Critique 261: Canada’s Guidance on Alcohol and Health: Final Report. Ottawa, Ont.: Canadian Centre on Substance Use and Addiction (2023).
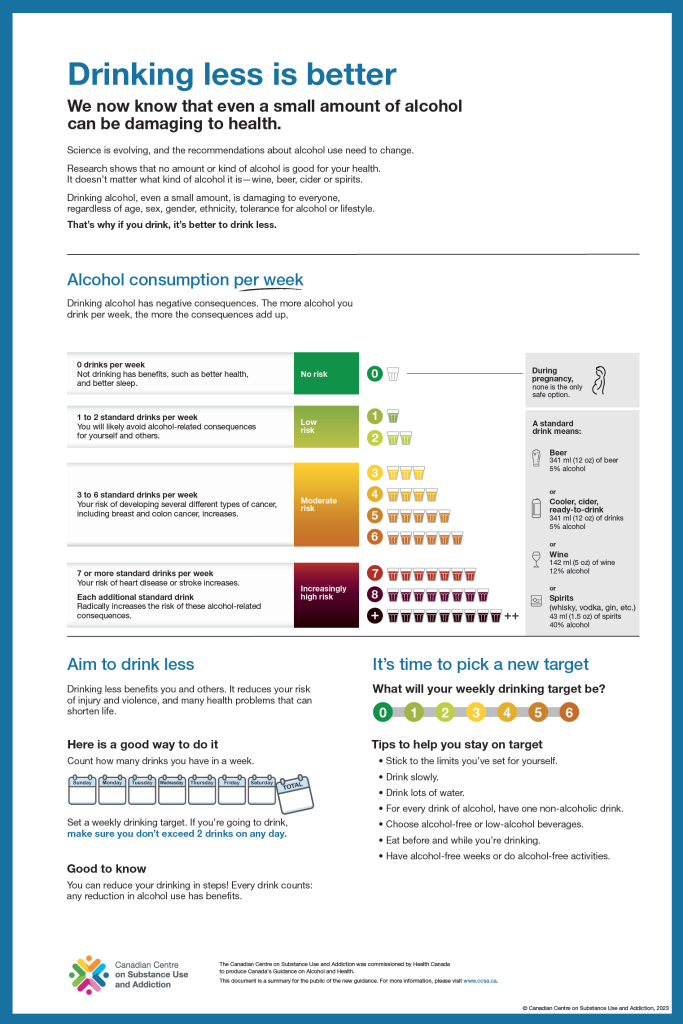
In January this year, the Canadian Centre on Substance Use and Addiction (CCSA) issued its recommendations entitled: Canada’s Guidance on Alcohol and Health: Final Report[1]. The Final Report contains three documents produced for three different target groups, namely one public summary for the general public, a technical summary for health professionals and a technical report for alcohol scientists. The public summary, entitled “drinking less is better” and subtitled “we know that even a small amount of alcohol can be damaging” states that science is evolving so that recommendations about alcohol need to change and that even a small amount of alcohol is damaging to everyone.
The recently issued Canada’s Guidance on Alcohol and Health by the CCSA focuses primarily on risk of death estimated by modelling twenty-one disease-alcohol consumption associations. The scientific evidence relating to both abusive and moderate alcohol consumption is itself not sufficiently consistent to produce precise recommendations for safe drinking for every alcohol consumer. There is no clear scientific evidence that uniformly applies to all population groups.
The accompanying Final Report suggests that “evidence has changed since the release of the 2011 Canadian Low Risk Drinking Guidelines”. This evidence includes the relationship between alcohol and cancer per se, stating that there is now no lower risk threshold for alcohol consumption; this contradicts 2022 data from 142,960 individuals from the population-based study MORGAM Project, that shows that there is indeed a nadir of the association. The authors also state that there is now no lower risk threshold for hypertension which was not shown in the reference that was used in the mathematical risk modelling. Additionally, they state that the potential cardioprotective effect of light to moderate alcohol consumption is more uncertain than previously estimated, which again was not shown in the reference selectively cited; this reference actually highlighted that relevance of drinking pattern in mathematical modelling. Other recent references cited are also considered contentious. This is not new data since 2011.
Forum members consider it a major omission not to take into account the association of alcohol consumption with overall mortality and only base their guidelines on an internationally criticized model. Moreover, the model mainly used evidence of low to very low quality. The authors also chose not to differentiate between gender and downplayed the reduced risk of cardiovascular disease and some other diseases like type II diabetes mellitus, nor did the authors take underreporting into account. Further, the authors neglected drinking pattern in their modelling which impacts risk of both short- and long-term alcohol-related harms and more importantly differentiates protective from harmful levels of alcohol consumption. The Forum also noticed several cases of misinterpretation of the input used for their modelling. Interestingly while these significant limitations were listed in the accompanying technical report, they were completely ignored in generating the long-term risk estimates for death and disability for Canadian alcohol consumers. In addition, the Forum noted that members of the Low-Risk Alcohol Drinking Guidelines Scientific Expert Panels and their associates are also authors of regularly cited references in the accompanying Final Report, certain of which are contentious and consistently use now widely debunked arguments around the ‘sick quitter’ hypothesis.
Accordingly, the Forum believes that these recommended guidelines do not contribute to their own intention to allow Canadians to make well-informed decisions on alcohol use and how it will affect their health. Furthermore, the evidence base assessing all-cause mortality and the risk of mortality from any cause at the 2011 alcohol level of 134.5 g/week for women, with no more than 27 g/day most days and 202 g/week for men, with no more than 40 g/day most days, remains robust and the hence the 2011 guidelines remain relevant to Canadians rather than the 2023 CCSA recommendations.
[1] https://www.ccsa.ca/canadas-guidance-alcohol-and-health-final-report
Forum comments
In January this year, the Canadian Centre on Substance Use and Addiction (CCSA) issued its recommendations entitled: Canada’s Guidance on Alcohol and Health: Final Report[1]. The Final Report contains three documents produced for three different target groups, namely one public summary for the general public, a technical summary for health professionals and a technical report for alcohol scientists. The public summary, entitled “drinking less is better” and subtitled “we know that even a small amount of alcohol can be damaging” states that science is evolving so that recommendations about alcohol need to change and that even a small amount of alcohol is damaging to everyone.
The CCSA 2023 Canadian drinking guidelines is the latest chapter in the never-ending story of sensible drinking advice. “Three bowls do I mix for temperate: one to health which they empty first, the second to love, the third to sleep. When this bowl is drunk up, wise guests go home” was the advice for sensible party-drinking by the Greek poet Eubulus (c. 375 B.C.) Anstie’s limit is the amount of alcohol that Dr. Francis Anstie (1833-1874) found could be consumed daily with no ill effects: 1.5 ounces of pure ethanol equivalent to two and one-half US standard drinks. A report by the Royal College of Psychiatrist (1979) was not that far from Anstie’s Limit: 56 drinks/week. However, with several reductions over the years the UK low risk guidelines in 2016 fell to 14 units (8 g alcohol/unit) per week with recommended alcohol-free days. With a suggested limit of two drinks (13.45 g alcohol/drink) per week, the 2023 CCSA recommended guidelines have reached a new low internationally.
According to the Final Report “… countries like the United Kingdom, France, Denmark, Holland and Australia recently reviewed new evidence on alcohol and health and released updated guidelines with limits significantly different from the 2011 Canadian guidelines, with weekly limits ranging from the equivalent of 5.2 to 8.3 Canadian standard drinks for women and men alike”. However, the Australian limit is 10 units per week (10 g alcohol/unit) per week equivalent to 7.41 Canadian standard drinks while the UK is equivalent to 8.29 Canadian standard drinks. In addition, the limit of new Danish guidelines from 2022 is 10 units (12 g alcohol/unit) per week equivalent to 8.92 Canadian standard drinks[2].
This critique will evaluate the methodology used to produce these recommendations and the data underlying these.
Basis of recommended guidelines
In their Final Report the authors state that the Canada’s Guidance on Alcohol and Health is informed by a public health perspective. It is unclear, however, what that perspective is. The perspective could be, when there is no alcohol consumed there is no harm or health harm due to alcohol. This may not be the right perspective since people, in general, do not drink for their health. An alternative perspective could be: how can a person, who enjoys the social and relaxing benefits from consuming an alcoholic drink from time to time have an acceptable risk level for his/her physical health. In that sense, one could question whether this guidance will help people making well-informed decisions, as intended.
Canadians drink more alcohol per capita than the worldwide average, according to the World Health Organization[3]. A 2017 report found that Canadians aged 15 and older drank 10 litres of pure alcohol per capita in 2016—3.6 more than the world average. Of the nearly 200 countries included in the report, Canada ranked 40th. More recent data from British Colombia indicate that per capita alcohol consumption may have been sustained at a level little over 9 litres of pure alcohol per capita for the past five years[4]. So, looking at a longer recent time period, Canadians tend to drink less.
The revision of the previous 2011 guidelines[5] is motivated by an overall insufficient quality of that report written by Canadian Centre on Substance Use and Addiction (CCSA) as assessed by the Public Health Agency of Canada. The group of scientists constructing the recommended 2023 guidelines did not change dramatically, however.
The CCSA strategy consists of selecting meta-analyses to provide data used in a model that calculates overall and specific risks. Risks considered acceptable were used to define the recommendations. Interestingly, the Final Report clearly states that the update of the Canadian guidelines was based on the modelling previously used to establish the 2011 Canadian guidelines, the 2020 Australian Alcohol Guidelines to Reduce Health Risks[6] and the 2016 UK Alcohol Guidelines[7]. Both the Australian and UK guidelines were widely criticised for their evidence-base and modelling[8]. One of the criticisms to the Australian guidelines was that no threshold effects were established for the risk curves used, whereas there seems to be no scientific justification for doing so[9].
The Canadian strategy is, however, different from strategies followed by other countries. The US, e.g., derived their recommendations based on meta-analyses (usually different ones) and other evidence, so to speak the totality of the evidence, rather than modelling estimated risks.
The Dutch guidelines (Dietary Guidelines) were revised in 2015[10] and have become stricter because the Health Council of the Netherlands did not focus on the risk similar to a non-drinker, but focused on those dietary conditions that would result in the best health (optimal health) rather than a specific risk level. This level was considered to be 5 g alcohol per day.
All-cause mortality omission
The recommended 2023 Canadian guidelines were constructed using a model integrating all known risks and benefits to derive at an overall risk assessment. The model was used to assess the alcohol-attributable deaths – a cause-specific approach to mortality risk from alcohol consumption. This scientific exercise is interesting, but data on the association between alcohol consumption and mortality risk do already exist. Advantage of considering overall mortality is that the association with alcohol consumption is irrespective of the cause of death and, therefore, includes all relevant causes of disease and disability leading to death. Surprisingly, no comparison was made between the model-generated attributable deaths and the real-life data on alcohol-associated deaths.
It is not clear why mathematical modelling is required at all when the mortality curves from the epidemiological literature can be used to identify a ‘low risk level’ of drinking. Similar to the Australian and UK guidelines, the recommended 2023 Canadian guidelines do not accept the logic of setting the guidelines at the point at which mortality risk is no higher than that of a non-drinker. This itself seems sensible and this level can be estimated this level by looking at the epidemiology, for example, a meta-analysis of 34 studies suggests that it is between 40 g and 60 g/day[11].
Overall mortality still shows a reduced risk with moderate consumptions also in various recent studies[12],[13],[14]. One way to take this notion into account is to look at the risk of dying of a non-drinker and calculate the non-drinker equivalence: level of alcohol consumed that generates the same or a similar risk level. This has recently been done in the Global Burden of Disease study. This study derived at low-risk drinking levels similar to the moderately risky levels in the recommended 2023 Canadian guidelines[15]. Unfortunately, the authors did not use the Canadian data from this Global Burden of Disease Study to calculate this alcohol consumption level; it may have been an opportunity to evaluate the comparability of the Canadian model to real life outcomes. We are of the opinion that the omission to review overall mortality is a limitation of the Canadian guidelines.
Concept of risk clarification
Furthermore, the concept of risk needs some consideration. Risk is of everyday and for everyone, but risk is different from safety. Safety is related to a level of risk and a level of risk is inherent to almost every activity. The level of risk is analysed by combining estimates of likelihood and consequences. Acceptability of a risk is primarily subjective and is generally viewed relative to other risks. Risk seems greater when put in terms of relative risk. A 100% increase in risk may seem enormous, but if the risk began as 1 in 100 people, the risk is increased to 2 in 100. To some people, this will seem like a large increase in risk but to others, it will not.
Some risk, therefore, needs to be accepted in our lives otherwise living is impossible. One risk may outweigh another, e.g., as Kiffer George Card explained in his article in the Conversation[16] “Those who drink alcohol report that these substances help them unwind — making it easier to come out of their shell and connect with friends and family. So, in short, people are taking risks with most things that they do, mainly because there is a benefit counterbalancing that risk. The benefit of drinking alcohol (in moderation) can be social engagement or a relaxation benefit which is not included in the risk models as indicated by the authors in their discussion. Therefore, the model produces a risk solely on specific physical health aspects. This may not have been clear to those for whom the recommendations are made.
In addition, the size of the risk needs some consideration. The risk in years of life lost (estimated and then modelled for the recommended 2023 Canadian guidelines) is considered “moderate” at a consumption level up to 6 drinks per week. Six Canadian drinks correspond to 6 x 13.5 g = 81 g/week which is 8 to 10 drinks per week in European and UK standard drinks, respectively. But what is that moderate risk? It is estimated at 17.5 YLLS (years of life lost) in 100 lifetimes. Assuming that a life time will consist of 75 years, 17.5 years are lost of the 7500 years in total which is 17.5/7500=0.00233 years lost per life, which would correspond to 0.23% of your life, which would be 64 days. Some people may consider this an acceptable risk.
Methodology
The methodology has been described with great care and is in general transparent, quite a number outcomes have been included, all of which were considered causally related to alcohol. Tables 1 and 2 show 21 diseases where their risk increases or risk decreases associated with weekly alcohol consumption. The paragraph “Diseases and Injuries Included in the Modelling” indicates that a total of 34 cause categories were included. The 21 diseases in Tables 1 and 2, which form the basis for the modelling performed, were based on various meta-analyses, in itself a well-accepted procedure.
However, 10 out of 16 of the meta-analyses used were considered of low to very low quality according to the criteria installed by the CCSA themselves. For instance, the review by Imitiaz et al. (2017) on tuberculosis, which is considered to be causally related to alcohol consumption, was based on an analysis of mostly case-control studies from small, high-risk populations. This meta-analysis cannot be considered representative for the Canadian population.
For cardiovascular disease, four meta-analyses were selected, three on atrial fibrillation incidence, various types of stroke, hypertension and one on the main cause of death, namely ischemic heart disease, also a meta-analysis of low quality according to CCSA’s grading system. This meta-analysis reports a very small negative relative risk (so a beneficial effect of 5%) for ischemic heart disease, which remains constant over a large range of drinking levels without any dose-response relationship. Other meta-analyses published[17],[18] come to other (more beneficial) associations[19],[20], namely beneficial effects of 25 to 40%. These meta-analyses were not selected nor evaluated.
Considering that most diabetics die of cardiovascular diseases like ischemic heart disease, the data used for type II diabetes mellitus are surprising: only females are beneficially affected for type II diabetes mellitus, whereas men are not (they have an increased risk). But still the risk relations for females and males for ischemic heart disease are the same. We believe that using only one single meta-analysis for major diseases like coronary heart disease and type II diabetes mellitus may introduce bias to the model. This paper will discussed further below.
Pancreatitis, also estimated based on a paper graded of low quality, is very different for males and females. This of course may be true, as females respond differently to alcohol as pointed out by the authors, but such large differences between males and females are hard to grasp. All-in-all, the accumulation of all estimated risks do not differ substantially between males and females. This is, however, not in agreement with the risk curves on total mortality observed in population-based studies[21].
The lack of quality in the underlying materials is acknowledged by the authors. They state: “In fact, in the field of alcohology most evidence is derived from cohort and observational studies that have inherent limitations that explain why many systematic reviews retained for this project did not receive a high-quality score. However, in no way does this mean that the quality of evidence is insufficient to provide guidance on alcohol and health to people living in Canada. In fact, there is a high level of confidence among members of the scientific expert panels and the Evidence Review Working Group that the identified reviews covered in this report are the latest and most high-quality evidence available to examine this public health issue”.
The authors also indicate: “Statistical models are only as good as their input. The relative risks were obtained from meta-analyses, which have been based on studies where participants may have underestimated their drinking, likely leading to higher guidelines”. So, the guidelines are based on evidence that is of insufficient quality to provide guidance, whereas the statistical models also have their drawbacks. In that sense we are dependent on the Working Group’s interpretation rather than on solid scientific evidence.
No gender differentiation
It is acknowledged in the recommended 2023 Canadian drinking guidelines that although detoxication is faster in men than in women where men can consume more alcohol before the risk of harm to their body’s organs and tissues increases, men generally exhibit more risk-taking behaviour over a lifetime than women and hence sustain more immediate injuries. It is, however, unclear how the committee derived at the notion that risk taking in a man´s lifetime results in a similar risk to the women´s higher sensitivity to alcohol. This assumption seems speculative.
Reduced risk of cardiovascular diseases from alcohol consumption disregarded or downplayed
In the author’s list of analytical limitations that disregards pattern of alcohol consumption, it is stated that “ for people engaged in heavy episodic drinking (consuming ≥ 60 g on at last one occasion monthly), there is no protective effect of alcohol consumption on ischemic heart diseases”, based on a meta-analysis[22] and a prospective cohort study[23]. The CCSA authors do not go on, however, to state that light to moderate has been found to be cardioprotective by the original authors22,23 who clearly also found a “cardioprotective effect of moderate alcohol consumption”.
Importance of pattern of alcohol consumption
A key limitation of the analysis which is actually recognised in the Final Report, is that drinking patterns were not considered. By their own admission, the relative risk estimates did not take into consideration the number of days during the week on which a person consumed alcohol because the authors claimed a “lack of evidence of the effect on drinking patterns of a person adopting abstinence days”. This is an obvious problem with the calculation and associated guideline as binge drinking is much more likely to lead to acute health conditions. Binge drinking or heavy episodic drinking is often defined as the consumption of 60 g or more of ethanol on one occasion.
No adjustment for underreporting
The issue of underreporting is not appreciated by the authors: “Although there is a hypothesis of a slight underestimation of alcohol use in medical epidemiology studies[24], the direction of alcohol use measurement bias in cohort studies is unknown[25],[26]”. The analysis of a total of 1 876 046 participants in 40 cohort studies from 18 countries on alcohol use and all-cause mortality24 found mean coverages of age 15+ per capita alcohol consumption of 62% ranging from 29% for Russia and 55% for western European countries to 66% for the USA and 97% for Japan25. To characterize those levels of underreporting as “a slight underestimation” is dismissal of a serious methodological problem in observational epidemiology.
Klatsky et al. (2014) also studied the role of underreporting in the moderate alcohol consumption and cancer association in a cohort of 127,176 persons: Individuals reporting light to moderate drinking had increased cancer risk in this cohort, however, the increased risk of cancer was concentrated in the stratum suspected of underreporting. For example, among persons reporting 1-2 drinks/day risk of any cancer was 1.33 (1.21–1.45) among those suspected of underreporting, 0.98 (0.87–1.09) among those not suspected, and 1.20 (1.10–1.31) among those of unsure status. These disparities were similar for the alcohol-related composite and for breast cancer[27].
Alcohol is not associated with all cancers, only certain cancers
In 2017, the American Society of Clinical Oncology (ASCO) published a position statement highlighting the connection between alcohol consumption and relative risk of cancer[28]. In a systematic review of international evidence, a World Cancer Research Fund/American Institute for Cancer Research (AICR) report[29] judged the evidence to be convincing that drinking alcohol was a cause of cancers of the oral cavity, pharynx, larynx, oesophagus, breast (in women), and colorectum (in men). Also, alcohol was judged to be a probable cause of increased risk of liver cancer and colorectal cancer (in women). An updated review of the evidence for liver cancer upgraded the conclusion for an association between alcohol drinking and liver cancer to convincing. The International Agency for Research on Cancer (IARC), a branch of World Health Organization (WHO), had assessed the evidence and come to similar conclusions. These cancers are referred to as alcohol-attributable cancers, and there is sufficient or convincing evidence of the attributions.30
Accordingly, alcohol consumption is associated with an increased risk of certain, but not of all, cancers, where multiple population studies have shown that the relationship between each cancer and alcohol differs. For example, there are stronger direct relationships in risk for cancers of the upper digestive tract from alcohol consumption but less strong direct relationships for cancers of the bowel and rectum, liver and breast, which is shown in the different relative risks and threshold effects estimated for each cancer. In addition, although the relative risk estimates for cancers between population studies differ, they consistently suggest that there is:
• no threshold for aerodigestive tract cancers, and risk increases linearly from approximately 1-2 g/day alcohol;
• no threshold for oesophageal cancer, and risk increases log linearly from approximately 1-2 g/day alcohol;
• a threshold of approximately 30 g/day alcohol for colorectal cancer;
• a threshold of approximately 45 g/day alcohol per day for liver cancer; and
• no threshold for breast cancer, and risk increases linearly from approximately <5 g/day alcohol.
These studies also consistently suggest that the risk of each cancer is low and relatively non-significant from light to moderate alcohol consumption. Risk becomes significant, however, with heavier alcohol consumption. Amount, pattern and lifetime alcohol consumption all influence the risk of these alcohol-attributable cancers. In addition, that while heavy, long-term drinkers are linked to the greatest risk of developing a cancer, even light and moderate drinkers have an increased risk relative to abstainers[30]. There are also alcohol thresholds for colorectum and liver cancers (World Cancer American Institute for Cancer Research 2007). For example, for both men and women, risk for these cancers only appears to increase when more than 30 and 45 g alcohol/day, respectively, is consumed[31],[32]). Risk of colorectal cancer increases by approximately 20% for alcohol consumption up 49.9 g alcohol/day and disproportionately increases to approximately 50% for more than 50 g alcohol/day[33]. Thus, with only heavy or high alcohol consumption is the risk high.
In addition, only approximately 10 to 15% of alcohol dependent drinkers develop cirrhosis of the liver and, of those, only 10% develop liver cancer[34]. Similarly, not all heavy drinkers develop cancer and some light-to-moderate drinkers develop cancer, suggests that an individual’s genetic predisposition influences their risk of developing cancer. This has also been suggested for colorectal cancers, such that there is a stronger relationship between alcohol consumption and colorectal cancers among individuals with a family history of colorectal cancer.33
Moderate alcohol consumption may, however, protect against Hodgkin’s and non-Hodgkin’s lymphomas and renal call cancers, and is not associated, positively or negatively, with other cancers32. A meta-analysis on the impact of alcohol consumption on the total risk contribution of the 20 most common cancer types in the Western world suggested that moderate alcohol consumption (up to 15 g /day) is not associated with an overall increased risk for cancer[35].
Model input
Of the 16 papers included in the modelling, 10 were of low to very low quality according to the criteria installed by the CCSA themselves. Some meta-analyses are discussed below, some previously critiqued by ISFAR and some discussed in the following:
Larsson SC, Orsini N, Wolk A. Alcohol consumption and risk of heart failure: a dose–response meta-analysis of prospective studies. European Journal of Heart Failure 2015;17:367–373. oi:10.1002/ejhf.228
In critique #163, the meta-analysis by Larsson et al. (2015) was evaluated. The authors concluded that there was actually a dose-response association between alcohol and heart failure; for example, a reduced risks of heart failure for consumers of 3 and 10 drinks/week, but not for those reporting the consumption of 21 drinks/week. Tables constructed by CCSA however, do not show how risks for heart failure were incorporated in their modelling. This Larsson paper scored a moderate quality by the CCSA. Also, Forum members considered this meta-analysis well-done[36].
Knott C, Bell S, Britton A. Alcohol Consumption and the Risk of Type 2 Diabetes: A Systematic Review and Dose-Response Meta-analysis of More Than 1.9 Million Individuals From 38 Observational Studies. Diabetes Care 2015;38:1804–1812 | DOI: 10.2337/dc15-0710.
In critique #172, the Knott et al. (2015) meta-analysis was evaluated. Prospective cohort studies and meta-analyses[37] have shown that the risk of developing type II diabetes mellitus (diabetes) is reduced among moderate drinkers by about 30%. Knott et al. (2015) carried out a multi-language search for studies on alcohol and diabetes and conducted a meta-analysis involving almost two million subjects from a final group of 38 cohort, case-cohort, case-control, or nested case-control studies. The main conclusions of the authors are that only females may show a significant inverse association between alcohol consumption and the risk of diabetes. Forum members had concerns about the analyses as the males in the study were primarily Asian (86%), and there were huge differences between the associations with alcohol for Asian and non-Asian populations. In general, many of the factors that relate to diabetes (diet, body size and adiposity, type of beverages consumed, etc.) are quite different between Asians and non-Asians; combining such groups when their analyses show opposite effects of alcohol on diabetes risk may not be a reasonable way of trying to develop results that apply globally. Forum members did not believe that this paper can support the conclusion of the authors that there is “no effect among males.” It could be unwise if the results of this study were used to develop alcohol guidelines for western populations.
Zhao J, Stockwell T, Roemer A, Naimi T, Chikritzhs T. Alcohol Consumption and Mortality From Coronary Heart Disease: An Updated Meta-Analysis of Cohort Studies. J Stud Alcohol Drugs. 2017 May;78(3):375-386. doi: 10.15288/jsad.2017.78.375. PMID: 28499102; PMCID: PMC5440363.
Zhao et al. (2017) meta-analysis has Tim Stockwell as co-author and he is co-author of seven of the papers referenced in the meta-analysis. The meta-analysis did not observe a reduced CHD mortality in studies “of higher quality” with exclusion of studies with “systematic selection bias”. The methods used to select “higher quality studies” with “rigorous criteria” used by Stockwell et al. (2016) to explore the presence of misclassifying of former and occasional drinkers as abstainers and other potentially confounding study characteristics left only five “higher quality” studies for analysis and neither partially nor fully adjusted estimates indicated significantly decreased risk for low- and medium-volume drinkers although the estimated relative risks for all current drinkers were less than unity. The wide confidence intervals with loss of significance might be due to loss of power as a consequence of exclusion of many solid studies due to the arguments by the authors that only lifelong, complete abstainers are the rightful reference group for alcohol consumption with exclusion of abstainers that “almost never” had consumed a drink.
Liu F, Liu Y, Sun X, Yin Z, Li H, Deng K, Zhao Y, Wang B, Ren Y, Liu X, Zhang D, Chen X, Cheng C, Liu L, Liu D, Chen G, Hong S, Wang C, Zhang M, Hu D. Race- and sex-specific association between alcohol consumption and hypertension in 22 cohort studies: A systematic review and meta-analysis. Nutr Metab Cardiovasc Dis. 2020 Jul 24;30(8):1249-1259. doi: 10.1016/j.numecd.2020.03.018. Epub 2020 Mar 27. PMID: 32446870.
The alcohol-hypertension relation among women was J-shaped and compared with non-drinkers: 10 g/day ethanol consumption did not increase the relative risk of hypertension for women. With that significant result from the meta-analysis by Liu et al. (2020) in mind, the risk calculations by the mathematical model showing increased risk of hypertension for females from 1.2% with one average drink per week up to 7.7% with an average use of seven drinks per week, raise questions on the reliability of the mathematical risk modelling employed by the Canadian guideline authors.
Larsson SC, Drca N, Wolk A. Alcohol consumption and risk of atrial fibrillation: a prospective study and dose-response meta-analysis. J Am Coll Cardiol. 2014 Jul 22;64(3):281-9. doi: 10.1016/j.jacc.2014.03.048. PMID: 25034065.
The authors of the recommended 2023 Canadian guidelines have selected a prospective study and a dose-response meta-analysis of seven studies (7245 cases) for evaluation of the risk of atrial fibrillation (AF) associated with alcohol consumption. Compared with current drinkers of less than 1 drink/week, the risk of AF did not increase for 1 to 6 drinks/week, nor for 7 to 14 drinks/week. Increases were observed at higher consumptions of 15 to 21 drinks/week, and for more than 21 drinks/week.
A 2017 meta-analysis with nine cohort studies (249,496 cases) found high levels of alcohol consumption associated with an increased incident AF risk. Moderate levels of alcohol consumption associated with a heightened AF risk in males, but in not females. Low alcohol consumption of up to 1 standard drink/day, however, was not associated with AF development[38]. Another 2022 meta-analysis which included a larger number of 16 cohort studies (305,433 cases), however, suggested a J-shaped relationship between alcohol consumption and incident AF: Up to 14 drinks per week seem to decrease the risk for developing AF although because of the substantial heterogeneity observed, no robust conclusion can be drawn[39]. Tables constructed by CCSA, however, only show increased risks for atrial fibrillation associated with alcohol consumption for both males and females.
Concluding comments
The scientific evidence relating to both abusive and moderate alcohol consumption is itself not sufficiently consistent to produce precise recommendations for safe drinking for every alcohol consumer. There is no clear scientific evidence that uniformly applies to all population groups.
The focus for recommendations has, however, changed. These changes could be described as follows:
- There has been a change in focus towards risk of death over a lifetime, adding the risk of death from short-term harms together with that from longer-term harms;
- The focus of long-term benefits (from cardiovascular diseases) has changed away towards long-term harms (from cancers);
- There has been a change in focus away from individual consumer factors, such as age, body mass index, gender and their associated effects on human health;
- There has also been change in focus away from pattern of consumption.
The WHO suggested that the four main non-communicable disease are cardiovascular diseases, cancers, diabetes mellitus and chronic lung diseases being responsible for the majority of all deaths globally. The association between lifetime alcohol consumption and death from cardiovascular diseases appears to be different from the association observed for alcohol-related cancers[40]. When all-cause mortality is considered, however, the data strongly suggested that light to moderate alcohol consumption reduces the risk of death from all causes12,[41],[42],[43]. The pattern of alcohol consumption, such as binge drinking, may modify this relationship[44],[45].
Forum member R. Curtis Ellison, who has been evaluating scientific data on the relationship of the consumption of alcoholic beverages to health outcomes for more than three decades, wrote: “I am appalled by the conclusions of the authors of this paper. They present a pseudo-scientific amalgamation of selected studies of low scientific validity that fit their preconceived notions and ignore many high-quality studies whose results may not support their own views”.
“The extensive critique by the Forum of the methods used in this paper have pointed out its weaknesses. In my opinion, it is especially regrettable that the authors ignore the pattern of drinking, so that they tend to group heavy week-end binge drinkers with regular moderate drinkers in their analyses. Their failure to adjust for under-reporting of intake further weakens the validity of their results, but of more importance is the failure to consider the type of beverage and the pattern of drinking, especially whether or not the beverage is consumed with food: these are the major determinants of whether the net health effects of drinking are favourable or harmful”.
“Current scientific data clearly indicate that, in comparison with abstainers, individuals who report the regular consumption of small to moderate amounts of an alcoholic beverage, when consumed with food markedly reduces their risk of coronary heart disease, type II diabetes mellitus, and total mortality. These relations have been found in essentially every well-done cohort study for many decades. By being very selective in choosing studies that support their preconceived ideas, by combining in their analyses data from many diverse cultures and populations with varying lifestyles, and especially by ignoring the pattern of drinking (regularly versus in binges, with or without food, etc.), the authors have created guidelines for drinking that do not apply to any single individual or population.”
Accordingly, the Forum believes that these recommended guidelines do not contribute to their own intention to allow Canadians to make well-informed decisions on alcohol use and how it will affect their health. Furthermore, the evidence base assessing all-cause mortality and the risk of mortality from any cause at the 2011 alcohol level of 135 g/week for women, with no more than 27 g/day most days and 202 g/week for men, with no more than 40 g/day most days, remains robust and the hence the 2011 guidelines remain relevant to Canadians rather than the 2023 CCSA recommendations.
[1] https://www.ccsa.ca/canadas-guidance-alcohol-and-health-final-report
[2] https://www.sst.dk/en/english/responsibilities-and-tasks/health-promotion/focus-areas/alcohol
[3] https://www.macleans.ca/society/canadians-drink-more-alcohol-than-the-global-average-says-report/
[4] https://www.uvic.ca/research/centres/cisur/stats/alcohol/index.php#:~:text=The%20most%20recent%20Statistics%20Canada,%25%20beer%20each%20per%20year).
[5] https://www.ccsa.ca/sites/default/files/2019-04/2011-Summary-of-Evidence-and-Guidelines-for-Low-Risk%20Drinking-en.pdf
[6] National Health & Medical Research Council (2020); Conigrave KM, Ali RL, Armstrong R, Chikritzhs TN, et al. (2021) Revision of the Australian guidelines to reduce health risks from drinking alcohol. Med J Aust. 215(11):518-524. doi: 10.5694/mja2.51336. Epub 2021 Nov 28. PMID: 34839537; PMCID: PMC9299166.
[7] U.K. Chief Medical Officers (2016); Holmes J, Beard E, Brown J, et al. Evaluating the promotion of revised UK alcohol drinking guidelines: a time series analysis using repeat cross-sectional survey data. NIHR J Lib. In press.
[8]https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/545743/list_of_resp.pdf; Holmes J, Beard E, Brown J, et al. (2020) Effects on alcohol consumption of announcing and implementing revised UK low-risk drinking guidelines: findings from an interrupted time series analysis. J Epidemiol Community Health 2020;74:942-949; https://www.abs.gov.au/statistics/health/health-conditions-and-risks/alcohol-consumption/latest-release; Holmes J, Brown J, Meier P, et al. (2016) Short-term effects of announcing revised lower risk national drinking guidelines on related awareness and knowledge: a trend analysis of monthly survey data in England. BMJ Open, 2016;6:e013804. doi:10.1136/bmjopen-2016- 013804; Stevely AK, Buykx P, Brown J et al. (2018) Exposure to revised drinking guidelines and ‘COM-B’ determinants of behaviour change: Descriptive analysis of a monthly cross-sectional survey in England. Public Health 18(1) DOI: 10.1186/s12889-018-5129-y; https://www.thetimes.co.uk/article/cut-in-drink-limit-ignored-findings-0mxjb0q6j; Searby A, Burr D, Redley B. (2022) Alcohol guideline awareness and beliefs among Australian nurses: A mixed-methods study. Collegian, Epub Nov 25 2022; https://doi.org/10.1016/j.colegn.2022.11.003; http://www.statsguy.co.uk/new-alcohol-guidelines/; Snowdon, C. (2022). Testing the total consumption model of alcohol. Economic Affairs, 42(3), 442– 452. https://doi.org/10.1111/ecaf.12545
[9] Snowdon, C. (2020) Submission to Public consultation: draft Australian guidelines to reduce the health risks from drinking alcohol. Submitted via NHMRC consultation form.
[10] https://www.healthcouncil.nl/documents/advisory-reports/2015/11/04/dutch-dietary-guidelines-2015
[11] Di Castelnuovo A, Costanzo S, Bagnardi V, et al. (2006) Alcohol Dosing and Total Mortality in Men and Women: An Updated Meta-analysis of 34 Prospective Studies. Arch Intern Med. 166(22):2437–2445. doi:10.1001/archinte.166.22.2437
[12] Corrao G, Bagnardi V, Zambon A, et al. (2004) A meta-analysis of alcohol consumption and the risk of 15 diseases. Prev Med. 38(5): 613-19
[13] Tolvanen E, Seppä K, Lintonen T, et al. (2005) Old people, alcohol use and mortality. A ten-year prospective study. Aging Clin. Exp. Res, 17(5): 426-433.
[14] Holahan CJ, Schutte KK, Brennan PL, et al. (2010) Late-Life Alcohol Consumption and 20-Year Mortality. Alcohol Clin Exp Res. 34(11): 1961-1971.
[15] GBD 2020 Alcohol Collaborators (2022) Population-level risks of alcohol consumption by amount, geography, age, sex, and year: a systematic analysis for the Global Burden of Disease Study 2020. Lancet 400(10347):185-235. doi: 10.1016/S0140-6736(22)00847-9.
[16] https://theconversation.com/canadas-new-drinking-guidelines-dont-consider-the-social-benefits-of-alcohol-but-should-they-198379
[17] Ronksley P, Brien S et al (2011) Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis BMJ 342:d671. doi: 10.1136/bmj.d671.
[18] Padilla H, Gaziano M, Djoussé L. (2010) Alcohol consumption and risk of heart failure: a meta-analysis. Phys Sportsmed. 2010; 38(3): 84-89.
[19] Roerecke M, Rehm J. (2012) The cardioprotective association of average alcohol consumption and ischaemic heart disease: a systematic review and meta-analysis. Addiction. 107(7): 1246-60.
[20] Roerecke M, Rehm J. (2014) Alcohol consumption, drinking patterns, and ischemic heart disease: a narrative review of meta-analyses and a systematic review and meta-analysis of the impact of heavy drinking occasions on risk for moderate drinkers. BMC Med., 12:182
[21] Di Castelnuovo A, Costanzo S, Bonaccio M, et al. (2022) Alcohol intake and total mortality in 142960 individuals from the MORGAM project: A population-based study. Addiction, 117: 312–25.
[22] Roerecke M, Rehm J. (2010) Irregular heavy drinking occasions and risk of ischemic heart disease: a systematic review and meta-analysis. Am J Epidemiol. 171:633-44.
[23] Sundell L, Salomaa V, Vartiainen E, et al. (2008) Increased stroke risk is related to a binge-drinking habit. Stroke. 39(12):3179–84.
[24] Stockwell T, Jinhui Z, Sherk, A et al. (2018). Underestimation of alcohol consumption in cohort studies and implications for alcohol’s contribution to the Global Burden of Disease. Addiction. 113. 10.1111/add.14392.
[25] Beimer PP (2004) Measurement Errors in Surveys. Paul P. Biemer (Ed), Robert M. Groves (Ed), Lars E. Lyberg (Ed), Nancy A. Mathiowetz (Ed), Seymour Sudman (Ed) ISBN: 978-0-471-69280-5 August 2004 760 Pages
[26] King AC. (1994) Enhancing the self-report of alcohol consumption in the community: two questionnaire formats. Am J Public Health. 84(2):294-6. doi: 10.2105/ajph.84.2.294. PMID: 8296958; PMCID: PMC1615001.
[27] Klatsky AL, Udaltsova N, Li Y, Baer D et al. (2014) Moderate alcohol intake and cancer: the role of underreporting. Cancer Causes Control. 25:693-9.
[28] LoConte NK, Brewster AM, Kaur JS, et al. (2018) Alcohol and Cancer: A Statement of the American Society of Clinical Oncology. J Clin Oncol. 36(1):83-93. doi: 10.1200/JCO.2017.76.1155. Epub 2017 Nov 7. PMID: 29112463.
[29] World Cancer Research Fund/American Institute for Cancer Research. Continuous Update Project Expert Report (2018). Alcoholic drinks and risk of cancer. Available at: https://www.wcrf.org/diet-activity-and-cancer/risk-factors/alcoholic-drinks-and-cancer-risk/
[30] LoConte, N.K., Brewster, A.M., Kaur, J.S, et al. (2017). Alcohol and Cancer: A Statement of the American Society of Clinical Oncology. 36(1): 83-93.
[31] Bagnardi, V., Rota, M., Botteri, E., et al. (2015) Alcohol consumption and site-specific cancer risk: a comprehensive dose-response meta-analysis. British Journal of Cancer. 112(3): 580-593.
[32] Cao, Y., Willett, W.C., Rimm, E.B., et al. (2015) Light to moderate intake of alcohol, drinking patterns, and risk of cancer: results from two prospective US cohort studies. BMJ (Clinical research ed.). 351(h4238): pp. 8
[33] Fedirko, V., Tramacere, I., Bagnardi, V, et al. (2011). Alcohol drinking and colorectal cancer risk: an overall and dose-response meta-analysis of published studies. Ann Oncol. 22(9):1958-1972.
[34] Hall, P. (1995) Pathological spectrum of alcoholic liver disease. Hall, P. (ed.) Alcoholic liver disease: pathobiology and pathogenesis. 2nd edition. London: Edward Arnold: pp. 41-68.
[35] Hendriks HFJ, Calame W (2018) The Contribution of Alcohol Consumption to Overall Cancer Incidence in the Western World: A Meta-Analysis. J Nutr Health, Sci 5(3): 311
[36] https://www.alcoholresearchforum.org/critique-163/
[37] Koppes LLJ, Dekker JM, Hendriks HFJ, et al. (2005) Moderate alcohol consumption lowers the risk of type 2 diabetes: a meta-analysis of prospective observational studies. Diabetes Care. 28(3):719-25. doi: 10.2337/diacare.28.3.719.
[38] Gallagher C et al. (2017) Alcohol and incident atrial fibrillation – A systematic review and meta-analysis. Int J Cardiol. 246:46-52.
[39] Giannopoulos G et al. (2022) Alcohol Consumption and the Risk of Incident Atrial Fibrillation: A Meta-Analysis. Diagnostics. 12:479.
[40] Bergmann, M.M., Rehm, J., Klipstein-Grobusch, K., et al. (2013) The association of pattern of lifetime alcohol use and cause of death in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Int J Epidemiol. 42: 1772-1790.
[41] Howie, E.K., Sui, X., Lee, D.C., et al. (2011). Alcohol consumption and risk of all-cause and cardiovascular disease mortality in men. J Aging Res. 2011; 805062. doi: 10.4061/2011/805062.
[42] Chiva-Blanch, G., Arranz, S., Lamuela-Raventos, R.M., et al (2013). Effects of wine, alcohol and polyphenols on cardiovascular disease risk factors: evidences from human studies. Alcohol Alcohol. 48: 270-277.
[43] Ferrari, P., Licaj, I., Muller, DC, et al. (2014). Lifetime alcohol use and overall and cause-specific mortality in the European Prospective Investigation into Cancer and nutrition (EPIC) study. BMJ Open. 4: e005245.
[44] Graff-Iversen, S., Jansen, M.D., Hoff, D.A., et al. (2013). Divergent associations of drinking frequency and binge consumption of alcohol with mortality within the same cohort. J Epidemiol Community Health. 67: 350-357.
[45] Bobak, M., Malyutina, S., Horvat, P., et al. (2016). Alcohol, drinking pattern and all-cause, cardiovascular and alcohol-related mortality in Eastern Europe. Eur J Epidemiol. 31: 21-30.
Forum Members
Forum Directors (Click on each name for link to a biographical sketch)
R. Curtis Ellison, MD, Section of Preventive Medicine/Epidemiology, Boston University School of Medicine, Boston, MA, USA (Chair)
Henk Hendriks, PhD, Netherlands (Co-Director)
Creina Stockley, PhD, MBA, Independent consultant and Adjunct Senior Lecturer in the School of Agriculture, Food and Wine at the University of Adelaide, Australia (Co-Director)
Forum Members (Click on each name for link to a biographical sketch)
Elizabeth Barrett-Connor, MD*, Distinguished Professor, Division of Epidemiology, Department of Family Medicine and Public Health and Department of Medicine, University of California, San Diego, La Jolla, CA USA (* Retired, 4 April 2019; died 9 June 2019)
Alberto Bertelli, MD, PhD, Institute of Human Anatomy, University of Milan, Italy
Dee Blackhurst, PhD, Lipid Laboratory, University of Cape Town, Cape Town, South Africa
Mladen Boban, MD, PhD, Professor and Head of the Department of Pharmacology, University of Split School of Medicine, Croatia
Marianne van den Bree, PhD. MRC Centre for Neuropsychiatric Genetics and Genomics, Institute of Psychological Medicine and Clinical Neurosciences, Cardiff University, UK
Giorgio Calabrese, MD, Docente di Dietetica e Nutrizione, Umana Università Cattolica del S. Cuore, Piacenza, Italy
Maria Isabel Covas, DPharm, PhD, Cardiovascular Risk and Nutrition Research Group, Institut Municipal d´Investigació Mèdica, Barcelona, Spain
Alan Crozier, PhD, Plant Biochemistry and Human Nutrition, University of Glasgow, Scotland, UK (* Retired 12 November 2019)
Giovanni de Gaetano, MD, PhD, Department of Epidemiology and Prevention, IRCCS Istituto Neurologico Mediterraneo NEUROMED, Pozzilli, Italy
Luc Djoussé, MD, DSc, Dept. of Medicine, Division of Aging, Brigham & Women’s Hospital and Harvard Medical School, Boston, MA, USA
Ramon Estruch, MD, PhD. Associate Professor of Medicine, University of Barcelona, Spain
Alun Evans, MD, Centre for Public Health, The Queen’s University of Belfast, Belfast, UK.
Harvey Finkel, MD, Hematology/Oncology, Retired (Formerly, Clinical Professor of Medicine, Boston University Medical Center, Boston, MA, USA)
Tedd Goldfinger, DO, FACC, Desert Cardiology of Tucson Heart Center, University of Arizona School of Medicine, Tucson, AZ, USA
Lynn Gretkowski, MD, Obstetrics/Gynecology, Mountainview, CA, Stanford University, Stanford, CA, USA (until 2022)
Dwight Heath, PhD, Dept. of Anthropology, Brown University, Providence, RI, USA
Oliver James, MD, Emeritus Professor of Hepatology, University of Newcastle, UK
Imke Janssen, PhD, Department of Preventive Medicine, Rush University Medical Centre, Chicago, IL, USA.
Ulrich Keil, MD, PhD, Professor Emeritus, Institute of Epidemiology & Social Medicine, University of Muenster, Germany
Arthur Klatsky, MD, Dept. of Cardiology, Kaiser Permanente Medical Center, Oakland, CA, USA
Maritha J. Kotze, PhD, Human Genetics, Dept of Pathology, University of Stellenbosch, Tygerberg, South Africa.
Rosa M. Lamuela-Raventos, PhD, Department of Nutrition and Food Science, University of Barcelona, Spain.
Dominique Lanzmann-Petithory,MD, PhD, Nutrition/Cardiology, Praticien Hospitalier Hôpital Emile Roux, Paris, France
Arduino A. Mangoni, PhD, Strategic Professor of Clinical Pharmacology and Senior Consultant in Clinical Pharmacology and Internal Medicine, Department of Clinical Pharmacology, Flinders University, Bedford Park, SA; Australia
Fulvio Mattivi, MSc, Head of the Department Food Quality and Nutrition, Research and Innovation Centre, Fondazione Edmund Mach, in San Michele all’Adige, Italy.
Ross McCormick, PhD, MSc, MBChB, Professor Emeritus, University of Auckland; former Associate Dean, Faculty of Medical and Health Sciences, The University of Auckland, Auckland, New Zealand
Linda McEvoy, PhD, Department of Radiology, University of California at San Diego (UCSD), La Jolla, CA, USA
Jean-Marc Orgogozo, MD, Professor of Neurology and Head of the Neurology Divisions, the University Hospital of Bordeaux, Pessac, France
Professor Andrzej Pajak, Epidemiology and Population Studies, Jagiellonian University Medical College, Kraków, Poland
Matilda Parente, MD, consultant in molecular pathology/genetics and emerging technologies, San Diego, CA, USA.
Lynda H. Powell, MEd, PhD, Chair, Dept. of Preventive Medicine, Rush University Medical School, Chicago, IL, USA
Ian Puddey, MD, Emeritus Professor, Faculty of Health & Medical Sciences, University of Western Australia, Nedlands, Australia
Cecilia Samieri, DVM, MSc, PhD, Senior Researcher, Epidemiology of Ageing and Cognitive Function, INSERM U897 and Université de Bordeaux, Bordeaux, France
Erik Skovenborg, MD, specialized in family medicine, member of the Scandinavian Medical Alcohol Board, Aarhus, Denmark
Diewertje Sluik, DrPH, Division of Human Nutrition, Wageningen University, NL
Jan Snel, PhD, Social and Behavioral Sciences, University of Amsterdam, Amsterdam, Holland
Jeremy P E Spencer, PhD, Reader in Biochemistry, The University of Reading, UK
Arne Svilaas, MD, PhD, general practice and lipidology, Oslo University Hospital, Oslo, Norway
Pierre-Louis Teissedre, PhD, Faculty of Oenology–ISVV, University Victor Segalen Bordeaux 2, Bordeaux, France
Dag S. Thelle, MD, PhD, Department of Biostatistics, Institute of Basic Medical Sciences, University of Oslo, Norway; Section for Epidemiology and Social Medicine, Sahlgrenska Academy, University of Gothenburg, Sweden
Nicole H. Tran, MD, PhD, Department of Internal Medicine, Director of Quality Improvement and Patient Safety, Kaiser Permanente Oakland Medical Center, Oakland, CA, USA
Fulvio Ursini, MD, Dept. of Biological Chemistry, University of Padova, Padova, Italy
Susan J van Rensburg, PhD, Senior Scientist, Department of Pathology, Stellenbosch University, Tygerberg, South Africa (* Retired, 12 November 2019)
David Van Velden, MD, Dept. of Pathology, Stellenbosch University, Stellenbosch, South Africa
David Vauzour, PhD, Senior Research Associate, Department of Nutrition, Norwich Medical School, University of East Anglia, Norwich, UK
Andrew L. Waterhouse, PhD, Department of Viticulture and Enology, University of California, Davis.
Yuqing Zhang, MD, DSc, Clinical Epidemiology, Boston University School of Medicine; Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA.
