Critiques of Recent Publications
Note: For an archive of critiques, by topic, CLICK HERE
======================================================
Critique 276 – Alcohol Consumption, High-Density Lipoprotein Particles and Subspecies, and Risk of Cardiovascular Disease: Findings from the PREVEND Prospective Study
A protective effect of moderate alcohol consumption for CVD has been reported by numerous studies over decades. This was a key finding of this study too. Further, it is also recognised that alcohol consumption increases high density lipoprotein cholesterol (HDL-C), and this was confirmed by this study too. HDL-C has been considered for years the “good” cholesterol, as suggested by the inverse correlation between its plasma levels and cardiovascular (CVD) risk, as shown by the epidemiology. However, the relationship between HDL and atherosclerosis has been found to be much more complex. This study failed to find an association between alcohol consumption and HDL parameters, suggesting that the clinical relevance of HDL is more related to reverse cholesterol transport in which an inverse relationship has been detected with the prevalence of atherosclerosis, inflammation, and the promotion of plaque stability, as well as the incidence of CV events such as acute myocardial infarction. The ability of HDL to promote reverse cholesterol transport therefore appears to be more related to its size and composition in terms of proteins and lipids, than to HDL-C plasma levels, where identifying efficacy should move to HDL function measurement, that is, reverse cholesterol transport, instead of plasma levels.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
======================================================
Critique 275 – Recovery of neuropsychological function following abstinence from alcohol in adults diagnosed with an alcohol use disorder: Systematic review of longitudinal studies
Alcohol use disorder (AUD) commonly is associated with compromise in neurobiological and/or neurobehavioral processes. The severity of this compromise varies across individuals and outcomes, as does the degree to which recovery of function is achieved. Clinicians have commented that some of the greatest recoveries are in AUD, where a potentially life-threatening situation has been turned around by clinical intervention coupled with an individual’s determination and peer support. This paper provides clear evidence that alcohol’s compromising effects on neuropsychological function can be improved with abstinence.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
======================================================
Critique 274 – Multi-ancestry study of the genetics of problematic alcohol use in over 1 million individuals
Problematic alcohol use (PAU) often seems to run in families, and genetics certainly influence our risk or likelihood of developing PAU. Research shows, however, that genes are responsible for about half of the risk for PAU, and hence do not alone determine whether someone will develop PAU. Environmental factors, as well as gene and environment interactions account for the remainder of the risk. Further, multiple genes play a role in a person’s risk for developing PAU and there are genes that increase a person’s risk, as well as those that may decrease that risk, directly or indirectly.
This study involving approximately 1 million individuals uncovered a shared genetic basis for PAU across diverse genetic backgrounds. One hundred and ten risk gene regions were identified, broadening our understanding of PAU’s genetic architecture and its consequences. For example, genetic correlations with other mental and neurological disorders were suggested as well as PAU’s role as a major cause of other health problems and death. Indeed, genome-wide data may pave the way for personalized risk assessments and innovative interventions and pharmacological treatments.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
======================================================
Critique 273 – Circulating metabolites may illustrate relationship of alcohol consumption with cardiovascular disease
Two papers were recently published which consider the complexity of liver and gut-generated circulating metabolites of alcoholic beverages, such as wine, and their specific roles in human health (referred to as metabolomics). These papers collectively suggest that the 60 or more alcohol-associated metabolites following consumption, may be related to the risk of cardiovascular and other diseases.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
======================================================
ISFAR reiterates its defence of moderate alcohol consumption’s health benefits by Stockley et al.
ISFAR was invited to provide a commentary on the paper, Apologizing for the alcohol industry? A comment on ISFAR’s defence of alcohol’s purported health benefits by Stockwell et al. (2024) which is available in the Journal of Studies in Alcohol (JSAD) site: doi.org/10.15288/jsad.23-00193. It was duly accepted for publication.
An excerpt from the text which is reproduced with the journal’s permission is available here.
======================================================
Critique 272 – New perspectives on how to formulate alcohol drinking guidelines
To encourage moderate alcohol consumption, many governments have developed guidelines for alcohol consumption. There has been, however, a remarkable lack of agreement about what constitutes an alcohol consumption that is associated with an acceptable risk, optimal health or safe (no risk) alcohol consumption. There is also no consensus on drinking on a daily basis, on a weekly basis and when driving and no consensus about the ratios of consumption guidelines for men and women. In addition, there is no consensus on a strategy with which to develop guidelines. The panel outlines a possible methodology for guideline development internationally to reduce the previously observed lack of consensus. The outlines discussed in the paper’s ‘propositions to debate’, however, are based on very complex non-transparent mathematical modelling of which the evidence base is flawed. The resulting guidance itself has been criticised as confusing for consumers, amongst other issues, and will thus not apply to any other country.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
======================================================
Critique 271 – Moderate alcohol consumption, types of beverages and drinking pattern with cardiometabolic biomarkers in three cohorts of US men and women
Cardiovascular diseases (CVDs) remain the leading cause of death globally, and leading risk factors for CHD and stroke include high blood pressure, high low-density lipoprotein (LDL) cholesterol, diabetes, smoking and second-hand smoke exposure, obesity, unhealthy diet, and physical inactivity.
Various randomized controlled trials have previously identified biomarkers that change with moderate alcohol consumption and which may explain its beneficial effects on CVDs. These biomarkers include HDL cholesterol, glycaemic control as HbA1c and adiponectin. Other relevant biomarkers changing with moderate alcohol consumption are fibrinogen, fibrinolysis, platelet aggregation, other lipoproteins, such as LDL cholesterol, HDL functionality, oxidative markers and triglycerides. This large epidemiological study provides further support for these beneficial effects but also highlights the beneficial effects on and inflammatory markers. The study also supports the importance of a regular and moderate pattern of alcohol consumption, not abstinence nor binge or heavy drinking, to maintain cardioprotection.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
======================================================
Critique 270 – Alcohol consumption and prognosis and survival in breast cancer survivors: the Pathways Study
Lifestyle in general appears to be very important in reducing the risk for breast cancer. There is a paucity of sound scientific information and advice available to women post-breast cancer diagnosis and treatment as to whether they could continue to consume alcohol without adversely affecting their health. This study adds to the existing evidence that pre- or post-diagnostic alcohol consumption is not positively associated with breast cancer re-occurrence. It also suggests that light to moderate alcohol consumption may in fact be beneficial to these women’s health, especially for those with an unhealthy BMI, allied with a healthy diet and regular exercise.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
======================================================
Critique 269 – Global prevalence, incidence, and outcomes of alcohol related liver diseases: a systematic review and meta‑analysis
In general terms, the risk of alcohol-related liver disease (ARLD) increases with how much you drink and how often you drink. Liver disease can take the form of fatty liver disease, alcoholic hepatitis and alcoholic cirrhosis.
A definitive threshold below which alcohol intake will not cause liver disease has not been established, but levels of around 20-30 g/day for men and 10-15 g/day for women are unlikely to cause ARLD in most individuals. As both quantity and frequency of influences the risk of ARLD, regular heavy drinkers and alcohol dependent drinkers are at risk of and die from ARLD at a much higher rate than the general population.
This extensive systematic review and meta‑analysis summarises the usually small-scale studies on ARLD to describe the ARLD population (Niu et al., 2023). Accordingly, it provides insight in the global prevalence of ARLD which is currently estimated at 4.8%, and the role of factors influencing the disease such as gender, ethnicity, tobacco smoking, obesity, and chronic viral hepatitis C. The relationship between ARLD prevalence or incidence and alcohol consumption data in a specific country were, however, not investigated.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
======================================================
Critique 268 – Alcohol intake including wine drinking is associated with decreased platelet reactivity in a large population sample – 1 August 2023
This study by Pashek et al. (2023) confirms previously observed associations between alcohol consumption and decreased platelet reactivity, but does not conclusively confirm differential beverage and gender effects.
Our knowledge regarding the health effects of alcohol consumption might best be grouped into two complementary approaches. Observational studies, for example, have now reached epic proportions in sample size and duration, and feeding studies have assessed the immediate and short-term effects of alcohol on behaviour, biochemical pathways, and similar social or physiological endpoints. Clearly, neither of these approaches represents gold-standard evidence in biomedical research, that is, only a long-term randomized trial of clinical endpoints would meet that standard. Existing clinical trial and epidemiological evidence as well as confirmatory studies such as Pashek et al. (2023) provide useful insight into the endpoints that a clinical trial of moderate alcohol consumption might be best poised to tackle (Mukamal et al. 2016).
These observational data have demonstrated a differential effect of the alcoholic beverages on haemostatic cardioprotective mechanisms. More data are required, however, to establish the degree of differentiation between alcoholic beverages in conferring cardio-protection, cancer-protection and protection against other degenerative diseases.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
======================================================
Critique 267 – Alcohol consumption and risks of more than 200 diseases in Chinese men – 11 July 2023
This paper essentially suggests that alcohol abuse leads into a broad array of diseases in a primarily unhealthy elderly population of Chinese men who consume large amounts of alcohol. In that sense, it may have been more appropriate to title the paper “Alcohol abuse and risks of more than 200 diseases in apparently unhealthy Chinese men. It adds little new insight in the already existing knowledge on alcohol consumption, and especially light to moderate alcohol consumption, and health in the Chinese populations, despite the additional Mendelian Randomisation (MR) analyses undertaken.
MR uses genetic variation as a natural experiment to investigate the causal relations between potentially modifiable risk factors such as alcohol and health outcomes in observational data.
Even though many more genetic factors have been identified for inclusion in these MR analyses it is clear that the results from many different types of studies must be considered when attempting to judge the health effects of alcohol. This is especially the case because type of beverage, drinking patterns, tobacco smoking and other lifestyle habits, diet, and many other environmental factors relate to the effects of alcohol consumption. Thus, the combination of data from observational studies, clinical trials, animal experiments, and MR analyses will be needed to improve our knowledge on the relationship between alcohol consumption to health and disease in all populations.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here
======================================================
Critique 266: Reduced stress-related neural network activity mediates the effect of alcohol on cardiovascular risk – 3 July 2023
Well-known and studied causes of cardiovascular diseases include genetic, environmental, dietary and lifestyle components. Stress can be considered as a lifestyle component and risk factor for cardiovascular disease. The amygdala region of the brain is associated with stress responses via the sympathetic nervous system, and duly increases blood pressure and heart rate, and triggers the release of inflammatory cells to stressors. This study has focused on the role of alcohol in mitigating these adverse effects from stress on the cardiovascular system. The study showed that light to moderate alcohol consumption of 1 to 2 standard drinks daily compared to abstinence potentially lowers cardiovascular risk as it leads to long-term reductions in the brain’s stress signalling in the amygdala. The relationship is also j-shaped where heavier alcohol consumption, however, increases the risk of stress-related cardiovascular disease events. This is a new plausible mechanism of action for alcohol on reducing cardiovascular risk which deserves further study.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here
======================================================
Critique 265 – Alcohol consumption and breast cancer prognosis after breast cancer diagnosis: a systematic review and meta‑analysis of the Japanese Breast Cancer Society Clinical Practice Guideline, 2022 edition – 14 June 2023
According to the WHO, there are more than 2.3 million cases of breast cancer diagnosed each year, which make it the most common cancer among adults. In 95% of countries, breast cancer is the first or second leading cause of female cancer deaths (https://www.who.int/news/item/03-02-2023-who-launches-new-roadmap-on-breast-cancer). Initial meta-analyses such as that of Longnecker et al. (1988) clearly showed risk at higher rates of alcohol consumption, but mixed results at moderate rates, depending on the model. This meta-analysis of 33 more recent studies, however, clearly shows no elevated risk at moderate consumption levels. In the absence of evidence to the contrary, we should continue to discourage heavy consumption because it is likely to be associated with an increased risk of breast cancer, not to mention many other health risks. This report, however, should relieve light to moderate alcohol drinkers of the fear of increasing their risk of breast cancer, and confirm that moderate consumption reduces overall mortality risk as also shown in this meta-analysis.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here
======================================================
Critique 264 – Association Between Daily Alcohol Intake and Risk of All-Cause Mortality. A Systematic Review and Meta-analyses – 26/4/2023
Zhao et al. (2023) again claims as did Stockwell et al. (2016) that “the importance of controlling for former drinker bias/misclassification is highlighted once more in our results which are consistent with prior studies showing that former drinkers have significantly elevated mortality risks compared with lifetime abstainers”. This statement clearly contradicts their e-Figure 4 which shows a J-shaped relationship between alcohol consumption and all-cause mortality, such that, as succinctly summarised by Forum Member Djousse, “scientific inference suffers greatly when objective reporting of data is ignored by some authors”. Zhao’s claim was made based on just 20 additional papers included in their analysis which carefully excluded hundreds of validated studies showing reduced disease and all-cause mortality among moderate drinkers, as well as choosing occasional drinkers as the reference group.
The key features that clearly demonstrate bias in the present paper are:
1. This is the third attempt by the same group of researchers to disprove the beneficial relationship between light to moderate alcohol consumption and cardiovascular health. The first attempt (Fillmore et al, in 2006) was discredited by reanalysis of the studies. Reanalysis showed that after adjusting for the claimed bias the cardioprotective effect for regular light to moderate alcohol consumption was still apparent.
2. Numerous meta-analyses have been undertaken over the past 15 years that have adjusted for this proposed bias and they have consistently shown that there is a cardioprotective effect for regular light to moderate alcohol consumption.
3. In this new paper, Zhao et al., (2023) have again biased their meta-analysis by ‘cherry picking’ a small number of studies for their meta-analysis – they discarded 3230 studies and analysed only 107. The 107 studies selected did relate consumption to disease and all-cause mortality but the authors carefully avoided hundreds of validated studies that showed reduced disease risk among light to moderate drinkers.
4. Countless animal and human studies over the past four decades have provided extensive evidence for the biological mechanisms supporting the findings that light to moderate alcohol consumption is cardioprotective. Zhao et al., (2023) seem to have deliberately pretended that they do not exist.
Forum Member Skovenborg succinctly summaries this flawed further meta-analysis by the Canadian Institute for Substance Use Research group to discredit the positive association between regular low to moderate alcohol consumption and all-cause mortality as follows: “a well-designed meta-analysis can provide valuable information for researchers, policymakers, and clinicians. However, there are many critical caveats in performing and interpreting them, and thus many ways in which meta-analyses can yield misleading information. Meta-analysis is powerful but also controversial— controversial because several conditions are critical to a sound meta-analysis, and small violations of those conditions can lead to misleading results (Walker et al. 2008).”
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here
======================================================
Critique 263 – Alcohol Drinking Patterns and Risk of Developing Acute and Chronic Pancreatitis – 17/04/2023
Alcohol consumption has often been found to be a risk factor for acute pancreatitis (AP) and a number of biologic mechanisms for such an association have been suggested. Overall, however, the risk is rather low, as only 1-3% of heavy drinkers develop AP after 10-20 years of follow up.
This is the second study of the Danish National Health Surveys group investigating the association between drinking pattern and pancreatitis. A prospective cohort study based on data from 316,751 men and women participating in the Danish National Health Surveys 2010 and 2013, it specifically assessed the effects of type of alcohol as well as drinking pattern on risk of acute and chronic pancreatitis.
A J-shaped association between the consumption of alcohol and development of pancreatitis was observed particularly for beer and spirits where drinking frequency such as daily, frequent binge drinking and problematic alcohol use were associated with increased development of pancreatitis. The study is important because of its large number of subjects, apparently good ascertainment of disease, appropriate and well-described methodology, and the fact that data on the type of beverage were available. Further, it was carried out using data from subjects in a single country, thus is less likely to be confounded by mixing data from very divergent cultures.
Placed in perspective, however, both acute and chronic pancreatitis risk was shown to increase at higher levels of alcohol consumption, at leveles well above the definitions for moderate alcohol consumption. Furthermore, beverage type does not seem to be an important modulator of this risk, whereas problematic alcohol use was, even for the alcohol consumption adjusted hazard ratios.
Forum Member Professor R Curtis Ellison suggested that “while this paper on the relation of alcohol to pancreatitis mainly supports previous research on the topic, it is important due to its large number of subjects, apparently good ascertainment of disease, appropriate and well-described methodology, and the fact that data on the type of beverage were available. Further, it was carried out using data from subjects in a single country, thus is less likely to be confounded by mixing data from very divergent cultures… The key findings of this well-done study are that heavy drinking is associated with increases in risk of pancreatitis, whereas drinking within recommended guidelines for any beverage appears to not increase the risk.”
Concluding comments
Altogether, an interesting study that shows that acute and chronic Pancreatitis increases at higher levels of alcohol consumption, at least well above the definitions for moderate alcohol consumption. Beverage type does not seem to be an important modulator of this risk, whereas problematic alcohol use was, even for the alcohol consumption adjusted hazard ratios.
Reference:
Alcohol Drinking Patterns and Risk of Developing Acute and Chronic Pancreatitis
Authors. Becker U, Timmermann A, Ekholm O, Grønbæk M, Drewes AM, Novovic S, Nøjgaard C, Olesen SS, Tolstrup JS. 2023. Alcohol and Alcoholism Mar 1;agad012. doi: 10.1093/alcalc/agad012. Online ahead of print, 10pp.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here
======================================================
Critique 262 – Changes in alcohol consumption and risk of dementia in a nationwide cohort in South Korea
Cognitive dysfunction eventually leads to a loss of independence that becomes a burden on families and society, as the individual requires more intense care and often institutionalisation. In the later stages, the cognitive impairment associated with dementias will create total dependency such that dementia is one the major causes of disability and disability burden overall among older adults globally (WHO 2023)[1].
As there is no cure, identification of factors associated with preservation of cognitive function could lead to substantial improvements in the quality of life in older adults, including simple dietary measures. Recent systematic review of health behaviours which maintain healthy cognitive function suggests that the consumption of fish and vegetables[2],[3], moderate physical activity and moderate alcohol consumption tend to be protective against cognitive decline and dementia. Studies have shown that alcohol acts directly and indirectly on the brain[4].
Consistent with the systematic review of 28 studies by Rehm et al. (2019)[5] where although causality could not be established, light to moderate alcohol consumption in middle to late adulthood was associated with a decreased risk of cognitive impairment and dementia. Conversely, heavy alcohol consumption was associated with changes in cognitive impairments, and an increased risk of all types of dementia.
Jeon et al. (2023) also showed in their massive retrospective cohort study of four million people followed for six years resulting in 24 million person-years, which is a significantly adds to the strength of the study outcomes that a decreased risk of dementia was associated with maintaining mild to moderate alcohol consumption. The study additionally showed that a decreased risk of dementia was associated with reducing alcohol consumption from a heavy to a moderate level, and with the initiation of mild alcohol consumption; collectively this data suggests that the threshold of alcohol consumption for dementia risk reduction is low.
Genetic profiles, standardized cognition, mood and behavioural assessments, as well as the quantification of structural and functional connectivity brain measures, which are all well established for dementia, if included in this study would have enabled the extrapolation of, and further added to the global relevance of the results from this huge South Korean population.
Forum members agreed with the conclusions of the authors which, simply stated, suggest that ‘sustained’ drinking up to 30 g/day is good for the brain, but non-drinkers who went from zero to moderate or heavy drinking did not show the same improvement as those who increased only to mild drinking. These observations are not new and indeed are generally consistent of those of past studies on alcohol consumption and cognitive decline, but the subject size is almost more significant than the sum of participants in past studies.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here
[2] Gardener SL, Rainey-Smith SR, Barnes MB, Sohrabi HR, Weinborn M, Lim YY, Harrington K, Taddei K, Gu Y, Rembach A, Szoeke C, Ellis KA, Masters CL, Macaulay SL, Rowe CC, Ames D, Keogh JB, Scarmeas N, Martins RN. Dietary patterns and cognitive decline in an Australian study of ageing. Mol Psychiatry. 2014 Jul 29. doi: 10.1038/mp.2014.79.
[3] van de Rest O, Berendsen AA, Haveman-Nies A, de Groot LC. Dietary patterns, cognitive decline, and dementia: a systematic review. Adv Nutr. 2015; 6(2):154-68.
[4] Brust JC. Ethanol and cognition: indirect effects, neurotoxicity and neuroprotection: a review. Int J Environ Res Pub Health. 2010; 7(4):1540-1557
[5] Rehm, J., Hasan, O.S.M., Black, S.E. et al. Alcohol use and dementia: a systematic scoping review. Alz Res Therapy 11, 1 (2019). https://doi.org/10.1186/s13195-018-0453-0
======================================================
Critique 261: Canada’s Guidance on Alcohol and Health: Final Report
Authors: Paradis, C., Butt, P., Shield, K., Poole, N., Wells, S., Naimi, T., Sherk, A., & the Low-Risk Alcohol Drinking Guidelines Scientific Expert Panels.
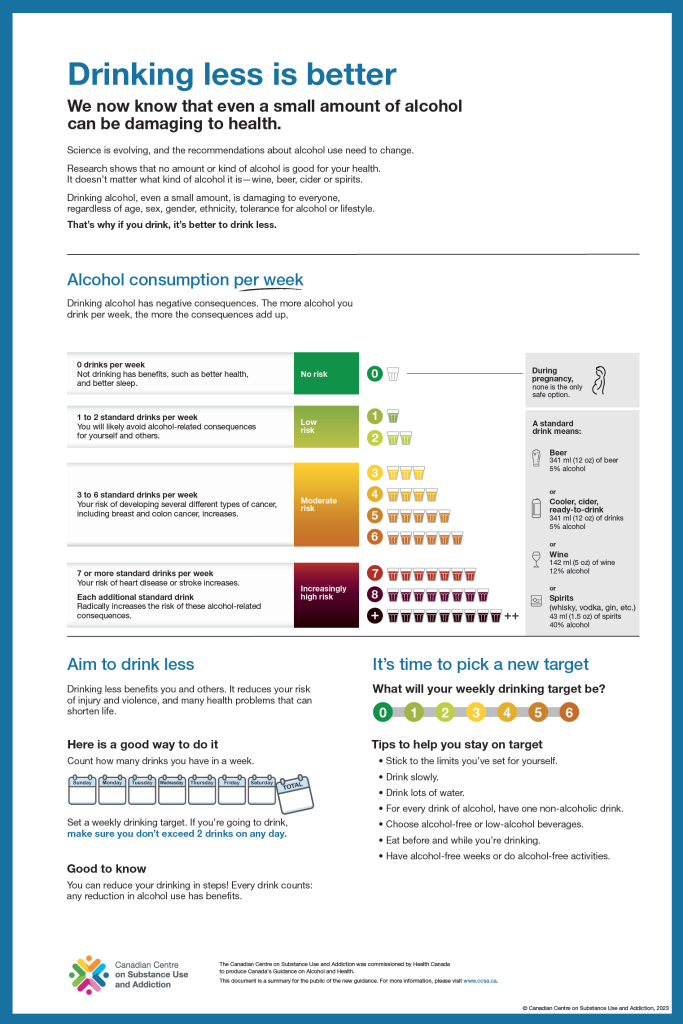
In January this year, the Canadian Centre on Substance Use and Addiction (CCSA) issued its recommendations entitled: Canada’s Guidance on Alcohol and Health: Final Report[1]. The Final Report contains three documents produced for three different target groups, namely one public summary for the general public, a technical summary for health professionals and a technical report for alcohol scientists. The public summary, entitled “drinking less is better” and subtitled “we know that even a small amount of alcohol can be damaging” states that science is evolving so that recommendations about alcohol need to change and that even a small amount of alcohol is damaging to everyone.
The recently issued Canada’s Guidance on Alcohol and Health by the CCSA focuses primarily on risk of death estimated by modelling twenty-one disease-alcohol consumption associations. The scientific evidence relating to both abusive and moderate alcohol consumption is itself not sufficiently consistent to produce precise recommendations for safe drinking for every alcohol consumer. There is no clear scientific evidence that uniformly applies to all population groups.
The accompanying Final Report suggests that “evidence has changed since the release of the 2011 Canadian Low Risk Drinking Guidelines”. This evidence includes the relationship between alcohol and cancer per se, stating that there is now no lower risk threshold for alcohol consumption; this contradicts 2022 data from 142,960 individuals from the population-based study MORGAM Project, that shows that there is indeed a nadir of the association. The authors also state that there is now no lower risk threshold for hypertension which was not shown in the reference that was used in the mathematical risk modelling. Additionally, they state that the potential cardioprotective effect of light to moderate alcohol consumption is more uncertain than previously estimated, which again was not shown in the reference selectively cited; this reference actually highlighted that relevance of drinking pattern in mathematical modelling. Other recent references cited are also considered contentious. This is not new data since 2011.
Forum members consider it a major omission not to take into account the association of alcohol consumption with overall mortality and only base their guidelines on an internationally criticized model. Moreover, the model mainly used evidence of low to very low quality. The authors also chose not to differentiate between gender and downplayed the reduced risk of cardiovascular disease and some other diseases like type II diabetes mellitus, nor did the authors take underreporting into account. Further, the authors neglected drinking pattern in their modelling which impacts risk of both short- and long-term alcohol-related harms and more importantly differentiates protective from harmful levels of alcohol consumption. The Forum also noticed several cases of misinterpretation of the input used for their modelling. Interestingly while these significant limitations were listed in the accompanying technical report, they were completely ignored in generating the long-term risk estimates for death and disability for Canadian alcohol consumers. In addition, the Forum noted that members of the Low-Risk Alcohol Drinking Guidelines Scientific Expert Panels and their associates are also authors of regularly cited references in the accompanying Final Report, certain of which are contentious and consistently use now widely debunked arguments around the ‘sick quitter’ hypothesis.
Accordingly, the Forum believes that these recommended guidelines do not contribute to their own intention to allow Canadians to make well-informed decisions on alcohol use and how it will affect their health. Furthermore, the evidence base assessing all-cause mortality and the risk of mortality from any cause at the 2011 alcohol level of 134.5 g/week for women, with no more than 27 g/day most days and 202 g/week for men, with no more than 40 g/day most days, remains robust and the hence the 2011 guidelines remain relevant to Canadians rather than the 2023 CCSA recommendations.
[1] https://www.ccsa.ca/canadas-guidance-alcohol-and-health-final-report
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here
======================================================
Critique 260: Two studies on the Mediterranean alcohol-drinking pattern and its association with hypertension and all cause mortality in the Seguimiento Universidad de Navarra” (SUN) cohort – 24 January 2023
Mediterranean Alcohol-Drinking Patterns and All-Cause Mortality in Women More Than 55 Years Old and Men More Than 50 Years Old in the “Seguimiento Universidad de Navarra” (SUN) Cohort – 14 December 2022
Mediterranean Alcohol-Drinking Pattern and Arterial Hypertension in the “Seguimiento Universidad de Navarra” (SUN) Prospective Cohort Study – 7 January 2023
The SUN (Seguimiento Universidad De Navarra) study represents one of the main cohorts in the European Mediterranean area aiming to explore the association between dietary factors and non-communicable diseases. The SUN study had previously shown that better adherence to the Mediterranean diet, which includes moderate alcohol consumption with meals, was significantly associated with a lower risk of all-cause mortality. It was also significantly associated with a lower risk of cardiovascular disease (CVD), which is the leading global cause of premature mortality.
These two new papers from the SUN study cohort concern alcohol and its potential beneficial effects when part of a Mediterranean diet and lifestyle. One paper is related to all-cause mortality in an older adult subset of the cohort, while the other related the pattern of drinking to the risk of an initial diagnosis of hypertension, which is a modifiable risk factor for atherosclerosis and therefore CVD.
Limitations of both studies include the relatively small number of events in some groups of drinkers and abstainers, where the latter group included both former drinkers and lifelong abstainer which are usually separated to reduce potential confounding. The all-cause mortality results may also be limited to a certain degree by a relatively small number of non-drinkers (n=35, for whom the degree of compliance with the Mediterranean diet was not shown), and the small number of drinkers who had low compliance with the Mediterranean Drinking Pattern (n=35), with the latter chosen as the reference group. Similarly, a weakness of the hypertension study is that the number of subjects in the low-adherence group was much smaller (n=156) compared with the other groups, yet it served as the referent category in the analyses. Further the low-adherence group was more likely to be younger, male, binged more, smoked more, consumed more alcohol and sugar-sweetened beverages, reported more recent weight gain, and had other unhealthy characteristics. While the investigators used multi-variable analyses that attempted to adjust for these factors, residual confounding is always a problem. Thus, it will be important that further studies with a larger number of subjects in the referent group confirm the observed relations shown in this study. According to their results, however, it seems clear that a drinking pattern of regular, moderate, wine consumption with food does not increase the risk of hypertension, an important message for the health of the population.
Overall, Forum members agreed with the conclusions of the authors that “Moderate red wine consumption at meals which is spread throughout the week, avoiding binge drinking, reduces the risk of all-cause mortality by 48%. These results are consistent with individual studies of each separate aspect of the pattern and with studies of a priori patterns.” Further, this paper strongly suggests that assessments of the relation of alcohol consumption to health should focus on the pattern of drinking, not just the total amount consumed.
References: Barbería-Latasa M, Bes-Rastrollo M, Pérez-Araluce R, Martínez-González MÁ, Gea A. Mediterranean Alcohol-Drinking Patterns and All-Cause Mortality in Women More Than 55 Years Old and Men More Than 50 Years Old in the “Seguimiento Universidad de Navarra” (SUN) Cohort. Nutrients. 2022 Dec 14;14(24):5310. doi: 10.3390/nu14245310. PMID: 36558468; PMCID: PMC9788476.
Hernández-Hernández A, Oliver D, Martínez-González MA, Ruiz-Canela M, Eguaras S, Toledo E, de la Rosa PA, Bes-Rastrollo M, Gea A. Mediterranean Alcohol-Drinking Pattern and Arterial Hypertension in the “Seguimiento Universidad de Navarra” (SUN) Prospective Cohort Study. Nutrients. 2023; 15(2):307. https://doi.org/10.3390/nu15020307
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here
======================================================
Critique 259: Importance of consuming alcohol (especially wine) with meals in relation to the risk of type 2 diabetes mellitus – 30 November 2022
Essentially all previous epidemiologic studies have shown that subjects who consume alcohol are at a lower risk than abstainers of developing Type 2 diabetes mellitus. The present analysis provides new information from more than 300,000 subjects in the UK BioBank who reported that they were consumers of alcohol; it demonstrates how the pattern of consuming alcohol plays an important role in the effect of alcohol on the risk of diabetes. Consuming an alcoholic beverage with food, versus drinking it at other times, is associated with a considerably lower risk of diabetes mellitus. This effect in independent of the amount of alcohol consumed, which suggests that all alcohol policy should be based only on research in which the pattern of drinking is known.
The study also demonstrated that the protective effects against diabetes was greater for consumers of wine rather than for those consuming beer or spirits. These associations are consistent with most previous epidemiologic studies, and now supported from these analyses of a very large cohort.
The authors had very reasonable estimates of alcohol intake as well as good ascertainment of health outcomes. They also had considerable data on many lifestyle and social factors that relate to the development of diabetes, so that confounding and modification of effect by them could be dealt with in the analyses. Forum members noted some limitations to the analytic methods regarding categorization of subjects by the type of alcohol they consumed, and the failure to adjust for diet. However, overall the results appear to support well the conclusions of the authors that there are key health advantages in terms of the risk of developing diabetes of consuming alcoholic beverages (especially wine) with meals, rather than on an empty stomach.
Reference: Ma H, Wang X, Li X, Heianza Y, Qi1 L. Moderate alcohol drinking with meals is related to lower incidence of type 2 diabetes. Am J Clin Nutr 2022;0:1–8.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here
Critique 258. Do the calories in alcoholic beverages increase the risk of obesity? 2 November 2022
This study was designed to determine if greater emphasis on the role of alcohol consumption as related to body weight might lead to less drinking and have a beneficial effect on subsequent weight and obesity. It was based on a survey of a select group of Australian adults who had previously volunteered to take part in medical research (not a population-based cohort). The authors took data from subjects who agreed with a question that asked if the subject ever thought about decreasing alcohol intake to lose weight, comparing them with those who did not answer the question in the affirmative. They compared the two groups (those answering yes versus those answering no to this question) and found some relation with body weight and with BMI (the latter of which was based on self-report of subjects regarding their height and weight).
Unfortunately, the premise that any alcohol increases body weight is erroneous, as the investigators ignored current scientific data that has consistently shown that light-to-moderate alcohol consumption does not increase body weight (which is seen generally only with excessive alcohol intake or binge drinking). While the authors had detailed data on the number of drinks reported by subjects, they ended up categorizing drinking levels into only two groups: ‘daily or weekly,’ or ‘monthly,’ which make it impossible to evaluate results of realistic drinking levels. They present no data on the pattern of drinking (e.g., with or without food, on a regular basis or in binges) or effects of different types of alcohol. They do not consider the complexity of factors related to obesity, and do not mention the effects of diet, exercise, smoking, or genetics on the risk of obesity. They misquoted the results of several previous studies to support their premise that lowering alcohol intake for everybody in the population would lead to less obesity, while a number of these studies actually showed the opposite.
Thus, the authors seem either oblivious to the data on alcohol calories and obesity or are deliberately ignoring it. Instead, their only concern appears to be to increase the incorrect perception that decreasing alcohol consumption among everybody, regardless of their intake, will lower the risk of obesity. Perhaps of even greater importance, they do not consider that a message to the entire population to decrease or stop alcohol consumption could result in increases in many diseases of ageing (e.g., coronary heart disease, ischemic stroke, diabetes, premature mortality risk) that are reduced by regular, moderate intake of alcohol, especially when consumed with food.
The authors end with conclusions that relate obesity to the culture of shame: the pervasive misconception that obesity is primarily a lifestyle-related condition and the simplistic belief that weight reduction is just adopting permanent caloric restriction, and the failure of a person with obesity to achieve and maintain weight loss is caused by a lack of discipline.
Overall, the present paper appears to the Forum as potentially misleading in the sense that it diverts the attention of experts, and potentially the population at risk, from the far more important and above all actionable effort to recommend moderation in drinking associated with a healthy and active lifestyle that does not lead to weight gain.
Reference: Bowden J, Harrison NJ, Caruso J, Room R, Pettigrew S, Olver I, Miller CWhich drinkers have changed their alcohol consumption due to energy content concerns? An Australian survey. BMC Public Health 20222; 22:1775. doi.org/10.1186/s12889-022-14159-9
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
======================================================
Critique 257: Does statin use modify potential beneficial effects of moderate alcohol consumption on cardiovascular risk? — 21 September 2022
The goal of this study was to determine if statin use (defined as the subject having been given a prescription for a statin, although actual consumption of statin was not ascertained) among a group of subjects who underwent cardiac catheterization modified the effects of alcohol consumption on subsequent cardiovascular events and total mortality. Their primary outcome was the occurrence during a follow-up period averaging 4.4 years of a Major Cardiac Adverse Event (MACE = documented myocardial infarction, ischemic stroke, heart failure hospitalization, or all-cause mortality).
From their adjusted analyses for “primary prevention” subjects MACE outcomes were 6.5% for alcohol users versus 14.2% for alcohol non-users (HR 0.50, CI 0.33, 0.78) for those not on a statin. If the subjects were on a statin, the protection from alcohol was less (19.5% for alcohol users versus 22.7% for alcohol non-users), not statistically significant. For subjects classified as ‘secondary prevention,’ alcohol users had only slightly lower risk of a MACE outcome, 18.2% versus 19.9% for no statin users and 19.9% versus 22.7% for statin users, not statistically significant. (In the Authors’ abstract, the HRs reported as greater than 1.0 are apparently for non-users of alcohol versus users of alcohol, as the reported adjusted risk of MACE was lower for alcohol users in all categories.)
There were several problems identified in the Forum review regarding the study design, analysis, and conclusions of the authors. Subjects were from the Intermountain Medical Center with patients primarily from Utah and several surrounding states. The characteristics of the subjects are quite different from those in most other areas of the United States in that the large majority reported that they consumed zero alcohol (between 66% and 75% in the categories of subjects); this is probably related to most being of the Mormon faith where alcohol use is not acceptable. (Religious affiliation of subjects is not reported in the paper.) Further, it would be expected that many Mormons who may have had consumed some alcohol in the previous year would deny it on a form being collected by the Intermountain Center, where they are being treated; this would lead to under-reporting of the exposure being studied and misclassification.
Further, all subjects were placed into categories classifying them as at “primary cardiovascular risk” or “secondary cardiovascular risk”; also if they reported any alcohol use (regardless of the amount or the drinking pattern) they were classified as alcohol users; otherwise they were in the no alcohol category. Subjects with zero coronary obstruction on angiography were classified as being at “primary risk” if they had not previously reported a myocardial infarction, coronary revascularization procedure, or an obstruction of a coronary artery of ≥ 70% identified on a prior angiogram (n=477). Otherwise, regardless of current findings of coronary obstruction of zero or of any amount of obstruction greater than zero, subjects with a previous cardiovascular event (including ≥70% obstruction of a coronary artery on a previous catheterization) were classified as being at secondary risk (n=2,108). Such complex and unusual categorizations could lead to misclassification of exposure and various types of bias. No data that are based on all patients, regardless of classification into primary or secondary risk, are presented.
Unfortunately, in their main analyses there were no distinctions according to the reported amount of alcohol. They do report “exploratory analyses” of reported amount: those consuming < 2 drinks/day seemed to have the most protection from alcohol – however, the numbers of subjects in the groups were inadequate for definitive results. Further, there were no data on the “pattern of drinking” (regularly or sporadically, with or without food, etc.) for subjects reporting any alcohol use. Having all subjects evaluated only within categories could lead to bias and limits the usefulness of the results.
In their analyses, the authors adjusted the effects of alcohol use on MACE with an extremely long list of potential confounders. Unfortunately, among these was the presence of diabetes, for which alcohol consumption has clearly been shown to reduce the risk of cardiovascular disease; diabetes is considered to be an important intermediary mechanism of the effect of alcohol. Thus, it would not be appropriate as a confounder. Also, others of the factors included as potential confounders were those that would be expected to be affected (either adversely or beneficially) by alcohol consumption, thus should not be used as potential confounders if one is seeking to determine the total effect of alcohol on cardiovascular disease.
Overall, a number of factors weaken the implications cited by the authors. These include the database used for this study (a majority of subjects reporting zero alcohol at baseline, unusual for Western populations), problems in categorization of subjects into primary or secondary risk, inappropriate factors adjusted for as “confounders” (including some directly affected by alcohol use), failure to discuss the law of diminishing results, and suggesting “no effect” when results were not statistically significant. Such problems make it difficult to support the authors’ conclusion that the prescription of a statin negates any effect of alcohol consumption on cardiovascular risk.
Reference: Anderson JL, Le VT, Bair TL, Muhlestein JB, Knowlton KU, Horne BD. Is Alcohol Consumption Associated with a Lower Risk of Cardiovascular Events in Patients Treated with Statins? An Observational Real-World Experience. J Clin Med 2022;11:4797. doi.org/10.3390/jcm11164797
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===========================================================
Critique 256: Alcohol consumption and health outcomes among 70 year olds in Sweden –22 August 2022
In a population-based cohort of 70-year-old men and women recruited in Gothenburg, Sweden, in 2014-2016, the authors of this paper have presented a detailed listing of many social, environmental, and biological factors that relate to non-drinking, former drinking, or current drinking of varying amounts of alcohol. Our Forum critique raises some questions about the traditional belief that the elderly should consume markedly less alcohol than younger subjects, and that the limitations placed on subjects related sorely to their age may often not be appropriate.
The paper emphasizes how a very large number of factors may modify the association between the amount of alcohol consumed and measures of health and disease. Many of these, such as indices of socio-economic state, are usually adjusted for in epidemiologic studies. Data on other factors that relate to alcohol consumption (such as self-related health, having a partner, grip strength, having others worried about their drinking, religiosity, gait speed, life satisfaction, etc.) represent data usually not collected in epidemiologic studies.
Forum members thought that these analyses show that subjects whose reported alcohol intake is only slightly above the recommended “safe” levels for subjects of this age should not be classified as “at-risk” drinkers. Most of their features match those of subjects reporting intake within current recommendations; certainly, they do not match the characteristics of heavier drinkers.
Forum members also pointed out that in addition to improved mortality associated with truly moderate drinking, as seen in essentially all epidemiologic studies, these analyses demonstrate that many other components of “successful ageing” are also associated with regular, moderate consumption of alcohol.
Reference: Ahlner F, Erhag HF, Johansson L, Fässberg MM, Sterner TR, Samuelsson J. Zettergren A, Waern M, Skoog I. Patterns of Alcohol Consumption and Associated Factors in a Population-Based Sample of 70-Year-Olds: Data from the Gothenburg H70 Birth Cohort Study 2014–16. Int J Environ Res Public Health 2022;19:8248; doi.org/10.3390/ijerph19148248
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
=====================================================
Critique 255: Wine consumption and the risk of cognitive decline in the elderly – 29 June 2022
The results of this systematic review and meta-analysis of longitudinal studies showed that, in almost every study, both wine consumption within the usual guidelines (no more than 2 drinks/day for men or 1 drink/day for women), as well as consumption in excess of these limits, were similarly associated with a lower risk of cognitive decline. For studies providing data on the amount of alcohol consumed, the risk of cognitive decline was reduced by 41% for both wine consumers drinking within the recommended guidelines as well as those reporting wine consumption in excess of the guidelines, when compared with abstainers. In studies where the amount of wine consumption was not reported, the estimate was an 18% reduction in the risk of cognitive decline for wine consumers versus abstainers.
Forum members noted that many potential confounders of the relation of alcoholic beverage consumption and cognition may modify the effects of alcohol on cognition, and were not evaluated very well in this study. Especially important may be the pattern of drinking (regularly or irregularly, with or without food, with associated binge drinking, etc), Forum members agreed that the calculations of the authors support a protective effect of wine consumption against cognitive decline, but their conclusions may be limited because of residual confounding by the pattern of drinking and other key factors not included in their analyses.
Forum members also noted another recent paper relating brain MRI markers to alcohol intake. However, changes in cognitive function were not assessed in the latter paper, and a direct comparison between the two papers cannot be done. However, we conclude that there remain questions regarding the effects of wine and other beverages containing alcohol on cognition. Other studies have shown divergent effects on the risk of dementia associated with wine consumption and the intake of spirits, so there may indeed be different effects on cognition with wine intake, the factor studied in the present paper. And, when compared with non-drinking or drinking of other beverages, extensive research supports health and mortality advantages when wine is consumed moderately, and especially with meals.
Reference:Lucerón-Lucas-Torres M, Cavero-Redondo I, Martínez-Vizcaíno V, Saz-Lara A, Pascual-Morena C, Álvarez-Bueno C. Association Between Wine Consumption and Cognitive Decline in Older People: A Systematic Review and Meta-Analysis of Longitudinal Studies. Frontiers in Nutrition 2022;9:863059
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
=====================================================
Critique 254: Adjusting for underreporting of alcohol intake in epidemiologic studies – 13 April 2022
It has been demonstrated repeatedly that the total population alcohol consumption based on self-reports by subjects in surveys and epidemiologic studies is lower than the amount of alcohol sold or taxed (disappearance data) within the population. This is assumed to relate to marked underreporting of individuals of their consumption, sometimes by one half or more. A key problem in attempting to adjust the self-reported values to more closely match the total alcohol disappearance data is that everyone does not underreport their intake, or may do so by different degrees.
The present study was based on data from US adults who responded to the 2011-2015 Behavioral Risk Factor Surveillance System (BRFSS; N = 2,198,089). The authors tested six methods for adjusting the self-reported data to provide what they hoped to be a more accurate value; some methods included adjustments based on differences in consumption by age and sex subgroups. From an unadjusted value of self-reported consumption of only 31.3% of that indicated by disappearance data, the various methods provided adjusted values ranging from 36.1% to 73%. The authors then used higher values to estimate the effect on alcohol-attributable deaths, using a population-attributable fraction approach.
While applauding the authors for attempting to obtain better estimates of alcohol consumption, Forum members were surprised that the authors did not even mention the method for identifying underreporting of individual subjects described by Klatsky and colleagues in the Kaiser Permanente Studies. The results of their method have been demonstrated to relate closely to alcohol’s effects on the risk of cancer, hypertension, and total mortality. Their method includes, in addition to self-reported data on alcohol consumption, adjustments for a variety of health conditions known to relate to excessive alcohol exposure, including alcoholic liver disease, hospitalizations for intoxication, mental problems associated with heavy drinking, etc. The presence of these conditions not only suggested that such subjects markedly underreported their intake (the exposure), but they also had much higher risk of adverse health effects (the outcome). When these conditions were not present at any of the study visits of subjects (allowing such subjects to be classified as being unlikely to be underreporting their alcohol consumption), adverse effects of low to moderate alcohol intake were generally not seen or their occurrences were markedly less frequent. This adjustment approach seems to be the only one previously described that gives reasonable results for individuals, and is clearly associated with the future health outcomes of subjects (and we realize that the occurrence of certain diseases or death happens for individual subjects, not for the population).
The Forum also raised questions about using “alcohol-attributable risk”. The authors base their calculations of population attributable risk on the hypothetic assumption of a rather low degree of underreporting in the population studies that are used as foundation of relative risk associations between alcohol intake and disease. Thus, risk is based mainly on self-reports of intake, even though their present paper indicates that adjustment for underreporting is so important. Further, throughout the paper, it appears that the authors tend to focus only on the adverse effects of alcohol without taking into regard the beneficial effects of light-to-moderate drinking, especially the regular consumption of wine with meals, which is found almost universally to be associated with lower risk of cardiovascular disease, diabetes, and total mortality.
While appropriate adjustment for underreporting could greatly improve the results of epidemiologic studies on alcohol and health, the goal would be to develop methods of determining the risk of individual subjects by including data on their own pattern of drinking and not assuming that the same adjustment formula applies to everyone in a population. By being able to identify subjects who underreport their intake, it would lead to some people changing categories of intake, and should result in estimates of either a lower risk, or greater risk, of adverse health effects of alcohol for that category of drinking. Further, more accurate and updated assessments of future health conditions that may be adversely (or beneficially) related to alcohol consumption should improve results and provide better data for setting drinking guidelines.
Reference: Esser MB, Sherk A, Subbaraman MS, Martinez P, Karriker-Jaffe KJ, Sacks JJ, Naimi TS. Improving Estimates of Alcohol-Attributable Deaths in the United States: Impact of Adjusting for the Underreporting of Alcohol Consumption. J Stud Alcohol Drugs 2022;83:134-144. https://doi.org/10.15288/jsad.2022.83.134.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 253 – The relation of alcohol consumption to the risk of glioma tumors of the brain – 5 January 2022
There appears to be an increase in the risk of glioma tumors of the brain, yet very few lifestyle or genetic factors shown to be true “risk factors” for the disease have been identified. The authors of this paper present the association between reported alcohol consumption from multiple assessments over decades and the diagnosis of such tumors, combining data from subjects in large cohort studies of nurses and male health care providers. Among the important strengths of this paper is the fact that the data were collected as part of a prospective study, difficult to do in cancer epidemiology except with very large cohorts. A total of 554 cases of glioma tumors were identified in these cohorts from a total sample of more than 200,000 subjects.
Forum reviewers agree with the conclusions of the authors that light-to-moderate alcohol consumption does not increase the risk of glioma; in fact, total alcohol consumption over many decades was found to reduce the risk. For example, a cumulative average consumption of total alcohol of >8 to 15 g/d (approximately 0.5 to 1.0 drink/day) was associated with a 25% lower risk of glioma when compared with the lowest category of intake (0 to 0.5 g/day) for both men and women. For consumers of > 15 g/d (just over 1 typical drink/day) versus the referent group, the risk for women was further significantly reduced to HR = 0.61; for men, the HR estimate was 0.79, but not statistically significant. (Some previous cohort studies have suggested an increase in risk for heavy drinkers.) There were no differences according to type of alcoholic beverage. For the subgroup of subjects with glioblastomas, findings were similar but less precise, due to smaller case counts.
The Forum concludes that light-to-moderate alcohol consumption, versus no alcohol intake or very occasional drinking, does not increase the risk; in this very well-done study, such consumption showed a significant reduction in the risk of glioma tumors of the brain.
Reference: Cote DJ, Samanic CM, Smith TR, Wang M, Smith‑Warner SA, Stampfer MJ, Egan KM. Alcohol intake and risk of glioma: results from three prospective cohort studies. Eur J Epidemiol 2021;36:965–974. https://doi.org/10.1007/s10654-021-00800-1
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 252: Dealing with previous alcohol exposure among “current non-drinkers” in epidemiologic studies testing the J-shaped curve – 3 December 2021
Most cohort studies have demonstrated a reduced risk of cardiovascular diseases, diabetes, and even dementia among light-to-moderate consumers of alcohol when compared with lifetime abstainers. This is often described as a “J-shaped curve,” a reduction in disease risk for light drinkers (compared with abstainers) but an increase in risk for heavy drinkers. Many criticisms of the J-shaped curve have been based on claims that many studies include “sick quitters” in their referent group. Such criticisms ignore most recent cohort studies in which only lifetime abstainers make up the referent group. Epidemiologists have known for decades that including ex-drinkers in the referent group for evaluating health effects of alcohol is an error; such a group cannot be used for comparisons with moderate drinkers.
While the present study from a large cohort in Germany clearly shows how previous alcohol excess and other unhealthy lifestyle factors and socio-economic factors influence the risk of many diseases, it creates a referent group made up of mixing lifetime abstainers and some ex-drinkers, and that their analyses show that this group does not have a higher risk of mortality than light drinkers (thus, the protection of light drinking leading to a decrease in risk of disease is erroneous). The authors of this paper apparently did this because they had such a small group of lifetime abstainers (only 42 subjects out of a cohort of 4,000!), a number grossly inadequate for comparisons with drinkers.
Forum members agreed that it was a serious error for the investigators; instead of admitting that their numbers were too low in this group for reliable comparisons, it appears that the authors augmented the comparison group with a group of ex-drinkers (that they considered to not be heavy drinkers) and reported that their analyses do not support a reduced risk among light drinkers. Thus, their claim that the lower risk of cardiovascular disease demonstrated in most studies among moderate drinkers is unrelated to alcohol consumption. However, this claim is based on an improper referent group used in their analyses. Forum members considered this to be a deeply flawed analysis, and of no merit for use in setting drinking guidelines.
Reference: John U, Rumpf H-J, Hanke M, Mayer C. Alcohol abstinence and mortality in a general population sample of adults in Germany: A cohort study. PLOS Med 2021;18:e1003819.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 251: Does moderate drinking increase, or decrease, the risk of falls in middle-age to elderly adults? 1 November 2021
To judge the relation of reported alcohol consumption to the risk of subsequent falls requiring hospitalization, the authors of this paper used data from the EPIC-Norfolk study, a prospective population-based cohort study in Norfolk, UK. In that study, there were a total of 25,637 community-dwelling adults, aged 40–79 years when recruited. The main outcome was the first hospital admission due to a fall over a follow-up period of about 11.5 years.
The key results of the study were that 19.2 % of non-drinkers were hospitalized for a fall during follow up, compared with 13.7% of low drinkers, 10.9 % of moderate drinkers, and 12.3% of heavy drinkers. In addition, the cumulative incident rates for falls at 121-180 months of follow up were 11.08% for teetotalers, 7.53% for low drinkers, 5.91% for moderate drinkers, and 8.20 % for heavy drinkers.
Forum members considered this to be a well-done study, with the analysis adjusting for a large number of factors that were potential confounders of the relation of alcohol intake to the risk of falls. We agree with the conclusions of the authors: “Moderate alcohol consumption appears to be associated with a reduced risk of falls hospitalization, and intake above the recommended limit is associated with an increased risk,” although we note that the increase in risk for heavier drinkers only appeared after essentially all covariates were added to the analysis. Obviously, residual confounding is always a possibility, but the present analyses indicating some protection against falls among light-to-moderate drinkers are supported by some well-done previous research.
The results of this study do not support the claim that any alcohol increases the risk of falls in older adults. It appears that this is not a concern for light-to-moderate drinkers who, in this study, had a lower risk of falls requiring hospitalization than did non-drinkers.
Reference: Tan GJ, Tan MP, Luben RN, Wareham NJ, Khaw K-T, Myint PK. The relationship between alcohol intake and falls hospitalization: Results from the EPIC-Norfolk. Geriatr Gerontol Int 2021;21:657-663.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 250: Importance of a favorable pattern of drinking (regularly, and with food) on risk of mortality – 28 July 2021
This is an analysis based on a very large data base of alcohol consumers (subjects reporting > 0 g of alcohol/week) from the UK Biobank (analyses based on 316,627 subjects with a median follow up of 8.9 years). The authors constructed categories of Drinking Habit Scores (DHS) for subjects; a “favorable” DHS was used for those subjects reporting a drinking frequency of 3 or more days/week and consuming alcohol with meals. The investigators then related the DHS categories to subsequent all-cause and cause-specific mortality, with adjustments for essentially all of the common known confounders/modifiers of alcohol effect.
Overall, Forum reviewers agreed with the main outcomes of the study, which indicate that subjects with a favorable DHS (in comparison with other drinkers) had significantly lower all-cause mortality (HR=0.82), CVD mortality (HR=0.84); cancer mortality (HR=0.82), and death from other causes (HR=0.77). In relation to the number of drinks consumed, the authors report that for all-cause, CVD, and other cause mortality, subjects with a favorable DHS showed a U-shaped or L-shaped curve (in that even for the heaviest drinkers, the mortality risk remained the same or lower than that of abstainers). Only for cancer mortality was there an increase in risk for subjects in the highest category of alcohol intake, leading to a J-shaped curve.
While the authors did not report specifically on the types of beverage being consumed in their favorable drinking pattern, it is the typical pattern generally found in southern Europe, and typically it is wine with meals. In these societies, wine is considered part of the meal, and is not consumed as “shots” that are usually being taken primarily as a way of getting drunk. As described in this paper, it is important to separate the health effects of these opposite approaches for consuming a beverage containing alcohol; putting all subjects into groups based only on the grams of alcohol consumed over a period, usually a week, does not take into account the important differences associated with the pattern of drinking.
We are finally appreciating that we are much further along in our research on alcohol and health than the innumerable studies that have focused just the amount of alcohol consumed, or on the J-shaped curve. We now realize the importance of the pattern of drinking. This constitutes not only the type of beverage and frequency of drinking, but also the consumption of alcohol with food and the absence of binge drinking. The pattern of drinking appears to be as important as, or even more important than, the quantity of alcohol consumed.
Reference: Ma H, Li X, Zhou T, Sun D, Shai I, Heianza Y, Rimm EB, Manson JE, Qi L. Alcohol Consumption Levels as Compared With Drinking Habits in Predicting All-Cause Mortality and Cause-Specific Mortality in Current Drinkers. Mayo Clin Proc 2021;96:1758-1769.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 249: Does light-to-moderate drinking increase the risk of atrial fibrillation? — 23 June 2021
While many epidemiologic studies have demonstrated an increase in the risk of AF for consumers of alcoholic beverages, there remains a question as to whether or not there is a threshold amount that would increase the risk. The present study concludes that “less than two alcohol units/day significantly increased the risk of incident AF, however, in men only. Reduction of even a moderate alcohol intake may thus reduce the risk of AF at the population level.”
While this may be the case, Forum members had a number of concerns about using the results of the present study to determine whether or not there is a threshold amount of alcohol necessary to increase the risk of AF. The methods used to judge alcohol consumption did not report the type of beverage or have a good estimate of the pattern of drinking, both of which factors are known to modify the health effects of alcohol. Further, the authors stated that there was evidence of considerable under-reporting of alcohol in their cohort, as the level of HDL noted in their “light” drinkers was above the level expected. This suggested to them that subjects in their lowest category of alcohol may actually have consumed more than they reported (probably about twice the reported amount of alcohol). This makes it difficult to determine if truly “light” drinking is associated with an increased risk of AF.
Overall, scientific data continue to show that light-to-moderate alcohol intake, especially when the pattern of drinking is found to be regular moderate consumption with food and without binge drinking, is associated with a lower risk of ischemic stroke and death. For the effects of alcohol intake on the risk of AF, the situation remains unclear. Unfortunately, the present study cannot answer the question as to whether there is, or is not, a clear threshold effect of alcohol intake on the risk of developing AF.
Reference: Ariansen I, Degerud E, Gjesdal K, Tell GS, Næss O. Examining the lower range of the association between alcohol intake and risk of incident hospitalization with atrial fibrillation. IJC Heart & Vasculature 2020;31:100679.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 248: Association of Alcohol Consumption with Cataract Surgery — 19 April 2021
This was a well-done analysis of a very large number of cases of cataract surgery in the UK; there were reasonable measures of the exposure (alcohol consumption), including the amount and type of beverage consumed, and appropriate potentially confounding factors were taken into consideration. However, data on the consumption of alcohol with or without food were not available. The use of national registries of cataract surgery provide an appropriate approach for estimating the main outcome of the analyses, and the results probably reflect the incidence of clinically significant cataract occurrence in these populations.
The key results were that there was a small but highly significant lower risk of cataract surgery among moderate drinkers. Red and white wine consumers showed more consistent and significantly lower risks of cataract surgery than consumers of other beverages. (In one of the two studies included in the analysis, small amounts of beer and spirits also showed a lower risk than that of non-drinkers.) There were too few heavy drinkers in these studies to determine the extent to which such drinking might affect risk. We appreciate that residual confounding, especially by factors that relate to subjects choosing to have surgical treatment of their cataracts, could still be present in these results.
Forum reviewers conclude that, in agreement with the investigators of this study, the data indicate a small but statistically and clinically significant decrease in the risk of cataract surgery for low-to-moderate drinkers, versus non-drinkers. A lowering of risk was especially clear for wine drinkers, in comparison with consumers of beer and spirits. There is an extensive literature regarding potential mechanisms by which constituents of the diet, especially those present in wine, may influence the development of cataracts. Among these are antioxidants or ROS scavengers, aldose reductase inhibitors, antiglycating agents, and inhibitors of lens epithelial cell apoptosis. However, the ultimate reason for the lower risk of cataract surgery associated with wine consumption found in this study has not been clearly delineated.
Reference: Chua SYL, Luben RN, Hayat S, Broadway DC, Khaw K-T, Warwick A, et al, on behalf of The UK Biobank Eye and Vision Consortium. Alcohol Consumption and Incident Cataract Surgery in Two Large UK Cohorts. Ophthalmology 2021, pre-publication.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 247: Effects of alcohol consumption on risk of stroke and systemic embolism among subjects with atrial fibrillation – 15 March 2021
The main aim of the current study was to investigate the associations of regular alcohol intake with incident stroke or systemic embolism in patients with established atrial fibrillation (AF), most of whom (84%) were on anti-coagulant therapy. The authors used combined data from two prospective studies of subjects with AF, followed for an average of 3 years. While they excluded subjects with “only short, potentially reversible AF episodes (e.g., as after cardiac surgery or sepsis)” about one half of subjects in the study were diagnosed as having paroxysmal AF. Reported alcohol at baseline and at subsequent examinations was classified as none, > 0 to < 1 drink/day, 1 to < 2 drinks/day, and ≥ 2 drinks/day.
The primary outcome was a composite of stroke and systemic embolism. Secondary outcomes were all-cause mortality, myocardial infarction, hospital admission for acute heart failure, and a composite of major and clinically relevant nonmajor bleeding. In their analyses, they adjusted for age, sex, education, hypertension, history of heart failure, history of diabetes, BMI, smoking status, physical activity, history of stroke, history of coronary heart disease, oral anticoagulation, history of renal failure, AF type, and health perception. With annual assessments, the investigators updated all covariates over time, if appropriate.
The main results indicated no significant effect of alcohol consumption on the risk of the major outcomes (stroke or systemic embolism). However, there were significant decreases in risk for several secondary outcomes. For hospital admissions for heart failure, in comparison with non-drinkers the HR for moderate drinkers was 0.60 (CI 0.41-0.87); further, among moderate drinkers the HR for myocardial infarction was 0.39 (CI 0.20 – 0.78), and for all-cause mortality the HR was 0.49 (CI 0.35-0.69).
Forum members had two major concerns with the paper. First, the authors failed to report specifically how alcohol consumption was associated with increased or decreased presence of AF during follow up, even though approximately one-half of subjects had only paroxysmal AF at baseline. Determining if alcohol consumption affected subsequent AF would be information of importance to practitioners who are advising their patients with AF regarding alcohol consumption.
Secondly, it was pointed out by Forum members that the results may have been affected by what is known as collider bias: as moderate drinking shows an inverse association with coronary heart disease (which is strongly related to the presence of AF), subjects who consumed alcohol prior to the baseline diagnosis of AF were probably different from those who had no prior alcohol exposure, and the results of combining these two groups (as was done in these analyses) may have been biased. Such bias usually tends to result in estimates of effect going toward the null.
While the reported results of no real effect of alcohol consumption on the risk of stroke or systemic embolism among patients with AF is encouraging, to decrease the risk of bias in future studies it will be important that such research attempts to separate subjects according to their prior use of alcohol before baseline measurements are assessed. The marked reduction in the risk of other major cardiovascular outcomes and total mortality, found in this study to be associated with light to moderate drinking, matches the results seen in most previous studies.
Reference: Reddiess P, Aeschbacher S, Meyre P, Coslovsky M, Kühne M, Rodondi N, et al, for the BEAT-AF and Swiss-AF investigators. Alcohol consumption and risk of cardiovascular outcomes and bleeding in patients with established atrial fibrillation. CMAJ 2020;193:E117-E123. doi: 10.1503/cmaj.200778
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 246: Light to moderate alcohol intake and the risk of cancer — 8 February 2021
The present paper attempts to use alcohol-attributable data, based on combining average alcohol intake from diverse European populations, to judge the effects of moderate alcohol consumption on the risk of cancer for all populations. It is based on earlier calculations of risk, extensively covered in previous publications by the senior author. The investigators conclude that the risk of a number of types of cancer are increased even among subjects reporting no more than 20 grams of alcohol per day (up to about 2 typical drinks), an amount they state to be within recommended levels of consumption (but exceed current US Drinking Guidelines for women of no more than 1 drink/day). The largest contribution to their calculated effects of alcohol was from breast cancer in women (which made up “68.7% of all alcohol attributable cancer for both sexes”). Breast cancer is a condition for which many factors other than just average alcohol intake are important: factors such as pattern of drinking, type of beverage, folate intake, smoking, obesity, physical activity, etc., all of which tend to confound the association.
Forum members had real concerns about their methodology of using an estimate of “alcohol-attributable cancer” based on reported average intake from 28 separate countries, including the large countries in western Europe (e.g., Germany, France, UK, Italy, Spain, Sweden), East-European countries (such as Poland and Hungary), and many smaller countries (e.g., Malta, Cyprus, Luxembourg, Latvia). Given the marked variation in culture and drinking patterns among these countries, it was considered that there are a large number of confounders and modifiers of alcohol effects that vary by country, and make it impossible to simply take the average alcohol intake from such diverse cultures to estimate causality of alcohol and cancer for everyone. By lumping data from all of these countries, the analyses end up with values that relate to a non-existent hypothetical population; different countries have different risk relationships, so the estimates of effect described in the paper apply to no single country.
Further, the investigators do not report rates of other outcomes, especially total mortality, associated with drinking. Taking only one outcome condition, without at least noting that moderate drinking has almost uniformly been found to decrease all-cause mortality, limits the usefulness of their results for setting alcohol guidelines. Heavy alcohol use is recognized by all as a serious impediment to the health of individuals, and to society at large. However, recommending lowering the intake of alcohol for everyone does not take into consideration that light drinkers might be more likely than heavy drinkers to follow such advice and might decrease their consumption to zero. Because of moderate drinking’s almost uniformly demonstrated beneficial effect on cardiovascular disease, if many light drinkers stopped drinking completely it would be expected to increase, rather than decrease, total mortality rates and the health of the population.
In their conclusions, the authors only mention the results of their actual analyses briefly, then start the usual chant of the need for extensive public health measures (warning labels, public information campaigns, increasing alcohol taxes, etc.) which tend to emphasize the dangers of any alcohol consumption. However, the analyses in this paper do not provide the data that are needed if one is to set appropriate drinking guidelines, which should be age-specific, sex-specific, and population-specific. Such factors would include not only the alcohol-disease relation but the particular characteristics of the population, the objective of guidelines (to influence and change behavior among target populations), the behavior that is thought to be in need of change, the culture and mindset of the target population, and the kind of message that is likely to be effective. Forum members realize that there are tensions between advice intended only to reduce the prevalence of misuse versus advice that takes into account the well demonstrated beneficial health effects of light-to-moderate consumption. When setting guidelines, it is important to take into account the prevailing drinking culture of a country or population, because only in that way is it possible to produce a public health message that is likely to be respected and regarded.
Reference: Rovira P, Rehm J. Estimation of cancers caused by light to moderate alcohol consumption in the European Union. European Journal of Public Health 2021; pre-publication. doi:10.1093/eurpub/ckaa236.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================
Critique 245: Effects of different patterns of alcohol consumption on risk of mortality, major cardiovascular events, cirrhosis, and cancer — 25 January 2021
This study was designed to determine factors that affect the pattern of alcohol consumption (including the frequency of consumption, type of beverage, with or without food, etc.), rather than just the reported average amount of alcohol, related to all-cause mortality, major cardiovascular events-MACE (MI/stroke/cardiovascular death), accidents/injuries, liver cirrhosis, all-cause and alcohol-related cancer incidence. It was based on a large prospective cohort study of UK Biobank (UKB) participants and included more than 300,000 subjects; outcomes were ascertained over a 9-year median follow-up period. Non-drinkers and only occasional drinkers were excluded from the analyses, so this paper does not judge the effects of light or moderate drinking versus not drinking, but only the effects of the pattern of reported alcohol consumption among regular drinkers.
The study showed that in comparison with subjects who consumed red wine more than 50% of the time (the reference group) there were lower risks of many adverse outcomes than among consumers of more than 50% of the time of spirits; the latter had 25% greater risk of all-cause mortality, 31% greater risk of MACE, and 48% higher risk of liver cirrhosis after controlling for total weekly alcohol consumption and relevant confounders. In comparison with red-wine drinkers, consumers of beer/cider showed an 18% higher risk for all-cause mortality, 16% higher risk of MACE, and 36% higher risk of liver cirrhosis. There were no statistically significant differences in outcomes between white wine drinkers and red wine drinkers.
Consumption of alcohol with food, versus not with food, showed a 10% (CI 2%-17%) lower risk of all-cause mortality. While consumers reporting alcohol consumption 3-4 days/week had lower risk of some adverse outcomes than subjects reporting intake on only 1-2 days/week, for some reasons subjects reporting daily or near-daily intake had an increased risk of liver cirrhosis, probably related to under-reporting by some heavy drinkers.
Forum members agree with the conclusions of this study as reported in the Authors’ Abstract: “Red wine drinking, consumption with food and spreading alcohol intake over 3–4 days were associated with lower risk of mortality and vascular events among regular alcohol drinkers, after adjusting for the effects of average amount consumed.” The results of this well-done study emphasize how inappropriate it is to use just the total average alcohol intake when relating the consumption of alcoholic beverages to the risk of adverse health outcomes.
Reference: Jani BD, McQueenie R, Nicholl BI, Field R, Hanlon P, Gallacher KI, Mair FS, Lewsey J. Association between patterns of alcohol consumption (beverage type, frequency and consumption with food) and risk of adverse health outcomes: a prospective cohort study. BMC Medicine 2021;19:8. https://doi.org/10.1186/s12916-020-01878-2.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 244: Is “ideal cardiovascular health” more common among consumers of wine than among drinkers of other beverages? — 18 December 2020
While a beneficial effect on cardiovascular disease of moderate drinking has been shown repeatedly in epidemiologic studies, the specific effects of different types of alcohol have not been well established. The authors examined the relation between alcohol type and an index of ideal cardiovascular health (CVH) as measured by the American Heart Association’s seven CVH metrics. Data from more than six thousand men and women, participants in the Multi-Ethnic Study of Atherosclerosis, were used to relate the association of the consumption of wine, beer, and liquor to the CVH score.
The authors report that participants who consumed 1-2 drinks/day of wine had higher odds of optimal CVH scores compared to those who never drank wine [adjusted prevalence odds ratio (POR) 1.64 (1.12-2.40)]. However, in comparison with participants who never drank beer or liquor, the odds of optimal CVH scores were lower for consumers of these beverages.
Forum members had some questions about the methodology for judging intake of the different beverages, as well as the statistical approach used in these analyses. However, they consider that the results (more favorable associations with wine consumption than from that of other beverages on indices of cardiovascular health) are in line with most previous studies.
It is important to realize that this study did not measure effects on the risk of disease occurrence or mortality, but just on the CVH index, a measure of overall cardiovascular health. Thus, we cannot tell specifically from this study whether the higher health indices among moderate wine drinkers was the result of the wine that they drink (even though this might be expected to some extent since, for example, moderate wine intake is known to favorably affect BMI, blood lipids, and blood glucose) or that their results relate to the fact that people with more moderate lifestyles and higher education, income, etc., tend to prefer moderate wine consumption and are less likely to be binge or heavy drinkers. It may be that wine drinkers make better decisions on all lifestyle behaviors than consumers of other beverages.
Reference: Ogunmoroti O, Osibogun O, McClelland RL, Lazo M, Mathews L, Okunrintemi V, Oni ET, Burke GL, Michos ED. Alcohol type and ideal cardiovascular health among adults of the Multi-Ethnic Study of Atherosclerosis. Drug and Alcohol Dependence 2020: Pre-publication release
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 243: Does the “quality” of the diet modify the relation of alcohol intake to the risk of hypertension? – 19 October 2020
The authors of this paper test the hypothesis that overall diet quality influences associations between alcohol consumption and the risk of hypertension, based on data from a study in the USA (NHANES) and two studies in China. In general, their designation of a “high-quality” diet for Chinese was one with greater amounts of fruit, vegetables, and beans, while for Caucasians and Hispanics it was one with more whole grains, fruit, vegetables and nuts; “low-quality” diets were mainly those with higher intakes of red meat products. For comparisons with abstainers, subjects reporting < 7 drinks/week for total alcohol were categorized as light and those reporting 7-21 drinks/week categorized as moderate drinkers, with those reporting more referred to as heavy drinkers.
The paper concludes that light alcohol consumption among subjects with a high-quality diet was significantly associated with a decreased risk of hypertension in Caucasians, and the risk of hypertension was not significantly increased with increasing alcohol consumption in Caucasians, Chinese, and Hispanics. On the contrary, in context of a diet calculated to be low quality the risk of hypertension was significantly increased in a linear fashion with increasing alcohol consumption in all groups except African Americans.
Forum reviewers considered this to be a generally well-done and interesting study, but had concern that the authors may not have adjusted adequately for a factor strongly related to diet quality: socio-economic status. The authors included in their analyses whether or not subjects had a high school diploma, but no adjustments were made for occupation, income, or other important indices of deprivation, which may be important since lower SES subjects have consistently been shown to have poorer diets. Thus, we are unsure whether or not it is the diet solely that is the reason that alcohol consumption was found to be associated with lower, higher, or no effect depending on the type of diet. Further, no results are shown indicating whether or not there were differences if the beverage consumed was beer, wine, or spirits, and there was insufficient data on the pattern of drinking. The authors begin their abstract saying that ‘Alcohol is commonly consumed around mealtimes,’ but apparently do not have any data on whether the beverage was consumed with or without food for the present analyses.” All of these factors may modify how alcohol affects the risk of developing hypertension.
Finally, some Forum members were uneasy with the term “quality of diet”, based on the inclusion or exclusion of certain foods, which may be very important to taste. Said one member, we trust that diets recommended as being of “high quality” are not those whose savor has been removed.
Reference: Jiang W, Meng X, Hou W, Wu X, Wang W, Wang M, Chu X, Wang P, Sun C, Han T, Li Y. Impact of overall diet quality on association between alcohol consumption and risk of hypertension: evidence from two national surveys with multiple ethnics. Eur J Clin Nutr 2020; doi.org/10.1038/s41430-020-00708-1.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
=========================================================================
Critique 242: The relation of light alcohol consumption to the risk of common cancers – 1 October 2020
In an attempt to assess the relation between light alcohol consumption (<12.5g per day) and the risk of a number of types of cancer, the authors carried out a review of meta-analyses published within the past 15 years. Using as keywords “light alcohol drinking,” “light alcohol consumption” and “cancer”, they found 29 meta-analyses on the subject. They report their results as indicating that “Light alcohol drinking was not associated with an increased risk of cancer occurrence, with the exception of breast and prostate cancer and melanoma. Furthermore, a possible protective role of light alcohol consumption on the development of bladder, kidney and ovarian cancer and Non Hodgkin Lymphoma was observed.”
Forum reviewers found a number of weaknesses in the paper. While their title focuses on “light alcohol drinking,” most of their reports of results and their discussion deal with harmful effects of heavier drinking; however, by not including papers on ‘heavy drinking’ in their original search, they may have left out many relevant papers. Further, the very brief reviews of each common cancer that they comment upon are sometimes based on only one or two meta-analyses, leaving out a huge amount of key data, especially that from single, well-done, long-term cohort studies with important information on the relation of alcohol to cancer; potential confounding by many factors could not be taken into consideration.
In the analyses in the present paper, the reported average level of alcohol consumed is used, but there is insufficient evaluation of possibly more important indices of alcohol exposure: the pattern of drinking (e.g., type of beverage consumed, in binges or on a regular basis, consumption with or without food, etc.). Further, there is probably inadequate control for important confounders or consideration of the effects of under-reporting, which may have been seen in single studies but not apparent in meta-analyses. In addition, a number of errors are present within the report, such as conflicting statements that may misrepresent the numeric data given. These problems make these results of limited use to professionals in health policy who are developing guidelines for alcohol use in the general public.
Reference: Caprio GG, Picascia D, Dallio M, Vitiello PP, Giunta EF, De Falco V, et al. Light Alcohol Drinking and the Risk of Cancer Development: A Controversial Relationship. Reviews on Recent Clinical Trials 2020;15:164-177
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 241: A Mendelian randomization study of alcohol consumption and the risk of breast cancer and ovarian cancer reveals no significant associations — 22 July 2020
The authors of this ambitious study used a Mendelian Randomization (MR) approach in an attempt to determine if alcohol consumption is causally associated with the risk of female hormone-dependent cancers. They used summary level genetic data from the hitherto largest genome-wide association study (GWAS) conducted on alcohol consumption (N = ~1.5 million individuals), breast cancer (N cases = 122,977) and ovarian cancer (N cases = 25,509). They examined three different alcohol intake exposures: drinks per week, alcohol use disorder (AUD) and age-adjusted alcohol use disorder identification test (AUDIT-C), to reflect general and harmful drinking behavior. For instrumental variables (IVs), they constructed updated and stronger genetic instruments using 99 SNPs related to drinks/week, 9 SNPs related to AUD, and 13 AUDIT-C-related SNPs, and estimated the causal relationship applying several two-sample MR methods.
The key result of these analyses was that the investigators did not find any evidence that alcohol intake increased the risk of breast cancer. For ovarian cancer, an initial inverse association with alcohol intake became null when adjustments were made for confounders. While members of our Forum agreed with the overall conclusions of the authors, who stated that they did not find “any compelling evidence in support for a causal relationship between genetically predicted alcohol consumption and risk of breast or ovarian cancer, consistent across three different alcohol-related exposures,” Forum members identified a number of weaknesses of the analyses. For example, there were very limited data on the pattern of drinking or the type of beverage consumed, and no data on smoking and other lifestyle habits, diet, and many other environmental factors that relate to the effects of alcohol consumption. Further, much of the data utilized to generate the IVs of alcohol exposure were from men, rather than women, although the two conditions being studied are present only in women.
Forum members agreed with the authors about the need to combine data from MR analyses with data from observational and experimental studies before making conclusions about the relation of alcohol consumption to health and disease. Given the rapid expansion of genetic studies, it is likely that MR analyses will be increasingly important in our research efforts, but we agree that the consideration of a combination of data from observational studies, clinical trials, animal experiments, and MR analyses will be needed as we seek to improve our knowledge on the relation of alcohol intake to health and disease; it is, and will remain, a continuing challenge.
Reference: Zhu J, Jiang X, Niu Z. Alcohol consumption and risk of breast and ovarian cancer: A Mendelian randomization study. Cancer Genetics 2020;245:35–41
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 240: Are there health risks from amounts of alcohol referred to as being within “low-risk drinking” guidelines? — 8 July 2020
The authors of this paper use very questionable data to suggest that drinking guidelines for all countries should be lowered to no more than 1 drink/day. In their analyses, they make a very large number of assumptions, including adding 80% to reported amounts of alcohol for all subjects to make up for alcohol disappearance data, and do not modify this according to their individual likelihood of being an under-reporter of intake. Further, they are not able to adjust for the pattern of drinking or type of beverage consumed, and it is considered bizarre that they grouped ex-drinkers (many of whom were apparently heavy drinkers) with current drinkers who report consuming within the guidelines to state that such subjects have a high risk of adverse effects. From the numbers presented in the tables in this paper, the risk of alcohol-attributable death for consumers of alcohol within-guidelines was fifty times lower than for those consuming above the guidelines. Such deficiencies in methodology, and especially possibly deliberate combinations of groups to support their premise, make it impossible to utilize their conclusions for setting guidelines for “low-risk” drinking.
Further, their conclusions do not reflect what the vast majority of well-done epidemiologic studies have shown for decades that light-to-moderate alcohol consumption (when defined as up to 1 drink/day for women and up to 2 drinks/day for men and not consumed in binges) is associated with a significant decrease in the risk of cardiovascular mortality as well as total mortality. The results of the current paper are not sufficient to warrant changing drinking guidelines.
Reference: Sherk A, Thomas G, Churchill S, Stockwell T. Does Drinking Within Low-Risk Guidelines Prevent Harm? Implications for High-Income Countries Using the International Model of Alcohol Harms and Policies. J Stud Alcohol Drugs 2020;81:352–361.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 239: Does the source of funding of epidemiologic studies on alcohol and health affect their results? – 28 May 2020
Funding of research by industry can lead to sponsorship bias. The aim of the current study was to evaluate for sponsorship bias in observational alcohol research by focusing on a spectrum of health outcomes related to moderate alcohol consumption. The authors utilized data from seven recent meta-analyses that included information from 386 observational studies of the relation of moderate alcohol consumption to a large number of health outcomes, including cardiovascular diseases, cancer, and mortality.
The authors report that only 5.4% of studies had some support from the alcohol industry, while 80.1% were funded by governments or other sources (non-industry-funded). Further, the results of moderate drinking on almost all health outcomes (including cardiovascular diseases and cancer) were essentially the same whether the study was funded by the beverage industry or not. Where there were slight differences, the results from non-alcohol-industry sources tended to have more favorable health results from moderate drinking than did those sponsored by the industry. The authors end their discussion stating: “In conclusion, only a small proportion of observational studies in meta-analyses, referred to by several international alcohol guidelines, are funded by the alcohol industry. Based on this selection of observational studies the association between moderate alcohol consumption and different health outcomes does not seem to be related to funding source.”
Forum members considered that the analyses were very complete, and detailed data were given in the very exhaustive supplementary material provided (exceeding 90 pages). (This makes it possible for a reevaluation of their results by others.) While Forum members noted that this analysis was apparently supported by the Dutch Beer Institute, the extensive data presented provide no evidence that there was bias in any of the analyses, upon which most international drinking guidelines have been based. The Forum concludes that the major studies that have shown that moderate drinking can have health benefits, especially for coronary heart disease and type 2 diabetes, are not based on bias because of support from the alcohol beverage industry.
Reference: Vos M, van Soest APM, Wingerden T, Janse ML, Dijk RM, Brouwer RJ, deKoning I, Feskens EJM, Sierksma A. Exploring the Influence of Alcohol Industry Funding in Observational Studies on Moderate Alcohol Consumption and Health. Adv Nutr 2020: pre-publication.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 238: Differences in evaluating confounding in epidemiologic studies when judging the effects of alcohol consumption on the risk of cardiovascular disease – 7 April 2020
The authors of the present paper compared studies included in a recent meta-analysis on alcohol consumption and the risk of coronary heart disease (CHD) for the number of potential confounding variables included in the analysis for each paper. While they found that most studies included adjustments for smoking, age, BMI, height and weight, physical activity, and education, many studies included adjustments for a multitude of other factors. They reach the conclusion that the large variation between studies in adjusting for confounding makes it impossible to accept the finding of a J-shaped curve between alcohol consumption and CHD (despite the consistency of such results).
Forum members agree that evaluating confounders in epidemiologic studies is extremely important. However, standardizing environmental confounders is not possible as there are so many, and so many yet undefined, and these confounders would be expected to vary in their influence among different populations. The authors did not focus on the key factor: the potential impact of each potential confounder. Limited research suggests that any “unknown confounder” would need to be extremely powerful to negate the reported protective effect of light-to-moderate consumption of alcohol, especially of wine, on the risk of CHD.
In addition, the authors were perturbed that many individual studies did not state specifically in their discussion that “residual confounding may be present in our results” or that “results of individual studies must be interpreted with caution.” Forum members assume that most readers of scientific reports realize that there should always be caution in making conclusions from a single study, especially observational studies, without the authors pointing in out in their paper. It may be analogous to stating that “further research is needed,” which should be assumed for any scientific paper.
Members of the Forum acknowledge that confounding makes it a difficult process to judge causality from observational studies, but point out that potential confounders in one study may be insignificant in another. It is not possible to generate a list of potential confounders that would apply to all epidemiologic studies. However, the consistency of the J-shaped curve between alcohol intake and risk of CHD in almost all epidemiologic studies, with support from a multitude of experimental studies, strongly supports the validity of such a relation.
Reference: Wallach JD, Serghiou S, Chu L, Egilman AC, Vasiliou V, Ross JS, Ioannidis JPA. Evaluation of confounding in epidemiologic studies assessing alcohol consumption on the risk of ischemic heart disease. BMC Medical Research Methodology 2020;20:64 https://doi.org/10.1186/s12874-020-0914-6
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 237: Relation of alcohol consumption in the elderly to the chances of reaching 90 years of age — 2 March 2020
An interesting and well-done study from a cohort of aging men in the Netherlands that evaluated how alcohol consumption data collected at 68 – 70 years of age related to the risk that the individual would survive to age 90. The authors report that “The highest probability of reaching 90 was found in those consuming 5–<15g/d alcohol, with RR=1.36 (95% CI, 1.20–1.55) when compared with abstainers.” Further, the authors noted that “Wine intake was positively associated with longevity (notably in women), whereas liquor was positively associated with longevity in men and inversely in women.” They also noted that there was a tendency for a lower chance of living to age 90 for subjects reporting binge drinking.
Forum members were unanimous in considering this to be an excellent study. It adds information on alcohol consumption collected in the elderly (ages 68-70 in this study) and subsequent longevity of life. It tends to counter fears expressed by some that the very elderly must be “protected” from alcohol, as it suggests that there are still health benefits from moderate drinking at all ages. Further, the reduction in risk of cardiovascular diseases is especially important in the elderly. This critique provides references to a multitude of research reports that strengthen the conclusions of the authors that, even among very elderly subjects, moderate drinking is associated with a greater longevity of life.
Reference: van den Brandt PA, Brandts L. Alcohol consumption in later life and reaching longevity: the Netherlands Cohort Study. Age and Ageing 2020;00:1–8 doi:10.1093/ageing/afaa003.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 236. Reasons for apparently diverse results from epidemiologic studies relating alcohol consumption to the risk of breast cancer 19 February 2020
The relation of alcohol consumption to the risk of breast of cancer has been the subject of innumerable epidemiologic studies over many decades, with most showing a slight increase in risk even for light drinking. However, it has been shown that this relation is attenuated when certain potential confounders are adjusted for, including folate levels, frequency of binge drinking, and the use of post-menopausal hormonal therapy. The present paper took the results of a recent large-scale meta-analysis and sought to try and explain why there is a large variability of results when the 97 studies included in that analysis were compared. The authors attempted to judge to what degree differences in exposure definitions, contrast levels, different study populations, different adjustment covariates, and different model approaches affected estimates of the effect of alcohol on cancer risk. The key factor the authors used in their analyses was the ratio between the most harmful and the most protective effects of estimated risk within each study.
All of the contrasts studied (different measures of alcohol consumption, different populations, different analytic approaches, etc.) had some effect on the estimates of effect of alcohol on the risk of cancer. As stated by the authors, “These findings suggest that whereas certain analytical and modelling choices, reflecting different types of alcohol and/or doses, can result in genuine differences, it is possible that many different analytical options, with different results, are pursued and selectively reported. Therefore, individual reported relative risk estimates from observational studies should be interpreted with caution.” Some Forum members disagreed with this conclusion, suggesting that due to marked variation in population, type of alcohol, analytic approaches, adjustment for confounding, etc., considerable error may be built in when combining data from heterogeneous studies. They felt that single large, long-term, well-done individual prospective studies may be preferable for judging the true effect of alcohol on the risk of breast cancer.
Thus, while Forum reviewers appreciated the attempt to explain differences in results of studies to get a more valid estimate of the true relation of alcohol consumption to the risk of breast cancer, and the analyses presented were done appropriately, some considered the approach described as not being a useful or valid one. Finding large differences in effects among sub-groups may not provide a reliable measure. Alternative approaches to scrutinize findings from observational studies, including Mendelian randomization or discussion centered on E-value (which assesses how strong an unmeasured confounder would have be to eliminate observed effect estimates), may be preferable. While such methods are imperfect, their use would be more interesting in informing the public and advancing scientific knowledge.
Reference: Chu L Ioannidis J PA, Egilman AC Vasiliou V, Ross JS, Wallach JD. Vibration of effects in epidemiologic studies of alcohol consumption and breast cancer risk. Inter J Epidemiol 2020;10:1–11. doi: 10.1093/ije/dyz271
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 235: Does type of alcohol or drinking pattern explain greater adverse effects of alcohol consumption among lower socio-economic subjects? 15 January 2020
The authors of this paper aimed to investigate whether and to what extent consumption by beverage type, BMI, smoking and other factors explain inequalities in alcohol-related harm evidenced though wholly attributable alcohol-related hospital admissions (ARHA). They especially evaluated levels of socio-economic status (SES) as determined by geographic and individual levels of deprivation. They based their analyses on data from 11,038 respondents to the Welsh Health Survey who answered questions on their health and lifestyle.
The results of this study support previous research on how factors associated with poor socio-economic status relate to poor health outcomes. It provides added information by providing an expanded definition for deprivation (assessed from geographic area of residence as well as from personal data), and for potential differences by type of beverage consumed. The definition of deprivation included many factors that, together, seem to be the primary reason why poorer, less educated people seem to have more adverse health effects that have been attributed to alcohol consumption.
Specifically, this study shows that the amount of alcohol consumed by people with low SES may be only a minor factor in explaining their increase in adverse effects that are usually classified as being “alcohol-related.” In this study, the frequency of alcohol consumption explained only 4% of the greater number of “wholly attributable alcohol-related hospital admissions.” Co-existing other behaviors and conditions, especially smoking, obesity, living in a deprived environment, poor health status, and mental health, appeared to have much greater effect. Thus, the conclusions of this study suggest that even for what are referred to as “wholly attributable .alcohol-related hospital admissions,” other factors associated with low SES may be more important than alcohol consumption itself as determinants of such adverse health outcomes.
Reference: Gartner A, Trefan L, Moore S, Akbari A, Paranjothy S, Farewell D. Drinking beer, wine or spirits – does it matter for inequalities in alcohol-related hospital admission? A record-linked longitudinal study in Wales. BMC Public Health 2019;19:1651. https://doi.org/10.1186/s12889-019-8015-3
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 234: Effects of red wine consumption on gut microbiota that affect health and disease – 14 November 2019
This brief paper supports earlier research relating wine consumption to gut microbiota, and the relation of the latter to obesity and to cardiovascular and other diseases. The authors report that “Red wine consumption was positively associated in a frequency-dependent manner with ɑ-diversity, but even rare consumption showed an effect. White wine also displayed a lesser but suggestive positive association with ɑ-diversity, while we saw no association with other alcohol categories.” They suggested that these effects of red wine on gut microbiota may play a role in the reduced risk of obesity, cardiovascular disease, and reduced total mortality associated with red wine intake that have been demonstrated in many cohort studies.
An increasing number of studies point to beneficial effects of wine, especially red wine, which may not be present for other types of beverages containing alcohol. However, we agree with the conclusions of the authors: “Red wine consumption should always be studied in the context of the overall dietary habits of individuals to take into account residual confounding and bias. The majority of observational studies fail to do this adequately; and thus, results from large scale clinical trials are needed in order to establish a cause and effect relationship between red wine polyphenols and gut microbiota.”
Forum members consider that the present analyses support a beneficial health effect of regular and moderate red wine, but also agree that much further research will be required to work out the complex relation between the consumption of red wine and gut microbiota and the effects on health.
Reference: Le Roy CI, Wells PM, Si J, Raes J, Bell JT, Spector TD. Red wine consumption associated with increased gut microbiota ɑ-diversity in 3 independent cohorts. Gastroenterology 2019. In press, doi.org/10.1053/j.gastro.2019.08.024
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 233: The relation of alcohol consumption to the development of dementia, with very extensive evaluations of the latter – 7 November 2019
This study was designed to assess the association between alcohol consumption and dementia and the roles of mild cognitive impairment (MCI) and apolipoproteinEε4 (APOEE4) genotype in modifying this association. It was based on data from the Ginkgo Evaluation of Memory Study, conducted from 2000 to 2008 among US community-dwelling participants (which did not demonstrate beneficial effects of ginkgo). The study analyzed 3,021 participants aged 72 years and older who were free of dementia at baseline.
The assessment of alcohol consumption included both the amount and frequency of intake, and the authors had a very broad assessment of potential confounders, including cardiovascular and other diseases, depression, race, ethnicity, educational level, social activity, medication use, and genotype for APOE-E4. There was a very complete and careful attention to the assessment of cognitive function, as subjects underwent numerous and repeated cognitive assessments. For example, if there was any suggestion of cognitive impairment, cerebral magnetic resonance imaging and referral to an expert panel of clinicians, who reviewed and validated presence of dementia, was carried out. No previous studies have had such an extensive assessment of cognition.
The main results include a finding that for the large majority of participants (the 2,548 without mild cognitive impairment at baseline), complete abstention from alcohol was associated with a slightly higher risk of dementia than seen in any of the groups consuming alcohol. For 473 subjects with MCI at baseline, there was no effect on risk of dementia for up to about 10 drinks/week, then a slight but insignificant increase in risk with greater intake. Daily low-quantity drinking was associated with more than 50% lower dementia risk than infrequent higher alcohol consumption. Many of the associations shown had a consistent pattern (a decrease in risk with light drinking) but did not reach statistical significance. The association was similar for all sub-groups, and was not modified by APOEE4 genotype.
The analyses seem well done, and Forum members agreed that, while some of the associations did not reach statistical significance, the data support most previous studies that show a J-shaped or U-shaped association for the relation of alcohol consumption to the risk of dementia. As has been shown in most previous studies, regular (even daily) light drinking was found to be preferable to infrequent higher levels of alcohol consumption in terms of the effect on the risk of dementia.
Reference: Koch M, Fitzpatrick AL, Rapp SR, Nahin RL, Williamson JD, Lopez OL, et al. Alcohol Consumption and Risk of Dementia and Cognitive Decline Among Older Adults With or Without Mild Cognitive Impairment. JAMA Network Open 2019:2(9):e1910319. doi: 10.1001/jamanetworkopen.2019.10319
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 232: Does moderate drinking of alcohol in later life reduce the risk of mortality? 3 September 2019
There are well-known problems inherent in most observational studies of alcohol and health. In addition to having to rely on self-report of intake, these include single-time point consumption assessments, inadequate confounder adjustments, accounting for reverse causation, selection bias, short follow up, residual confounding, and lacking information on chronic health conditions that may mediate the association between alcohol consumption and mortality. Further, there have been a lot of assumptions expounded about the generic fragility of older individuals in terms of alcohol consumption; they are generally without supportive clinical or experimental evidence. For light to moderate intake, the elderly tend to have similar benefits associated with alcohol as younger people, and they are at an age when the risk of mortality is at its peak.
The present study was able to adjust for many of these factors: it describes the risk of total mortality among a large group of older subjects, who were ≥ 56 years of age at the start of a 16 year follow up. They were participants in a nationally representative cohort of men and women in the USA, the Health and Retirement Study. Its strengths, in addition to its large size, is the fact that there were repeated assessments of alcohol so that changes of intake could be evaluated, and the authors were able to judge the potential importance of residual confounding.
The authors conclude that occasional drinking and moderate drinking among older subjects are associated with a lower risk of total mortality. The usual argument that light or moderate drinkers tend to have less severe or fewer common diseases and to enjoy better health and socioeconomic status is addressed in this study, which accounted for time-varying confounders that included smoking, body mass index, income, health/functioning, depression, and chronic diseases. From quantitative bias analysis studies they were able to estimate the effects of residual confounding on their results; the authors conclude that it is very unlikely that residual confounding by unrecorded variables would be the cause of the reduction in mortality associated with moderate drinking. Survival analyses supported notably decreased mortality for moderate drinkers. Forum members considered that this study adds important information about the effects on mortality of moderate drinking in the elderly.
Despite many decades of observational data, animal experiments, and limited clinical trials showing beneficial effects on many diseases and mortality from moderate drinking, it is noted that some researchers appear to be loath to admit to any positive health effects of alcohol. We all appreciate the serious adverse effects of heavy drinking and alcohol use disorders, both on the health of persons and on the community. However, when well-done analyses provide reliable data for light-to-moderate drinkers who do not binge drink, it is disturbing that, even then, some scientists question the observed beneficial results and appear to focus only on warnings about abuse.
There is evidence of a disinclination to admit to any beneficial effects of alcohol in many papers, including this one, which throughout the text seems to accentuate the negative aspects of alcohol. Such statements detract from an otherwise clear report suggesting, as one reviewer stated, that this paper is part research results, part polemic. In the opinion of the Forum, this paper provides strong evidence indicating that elderly people who are light-to-moderate drinkers tend to have a lower risk of mortality.
Reference: Keyes KM, Calvo E, Ornstein KA. Rutherford C. Fox MP, Staudinger UM, Fried LP. Alcohol Consumption in Later Life and Mortality in the United States: Results from 9 Waves of the Health and Retirement Study. Alcoholism: Clin Exper Res 2019;43:1734-1746.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 231: Association of alcohol consumption with obesity: Does moderate drinking increase or decrease the risk of obesity? 20 August 2019
While alcoholic beverages contain calories that are absorbed, the association between alcohol intake and body weight and obesity is unclear. Limited clinical trials have not confirmed a positive association between alcohol intake and weight, and some epidemiologic studies, including prospective cohort studies, show that regular moderate drinkers are less likely to be obese than are abstainers.
The present study uses data from National Health and Nutrition surveys between 2011 and 2016 to evaluate the association between reported amount and frequency of alcohol consumption and weight status. An estimated 78.1 % of males and 70.1% of females (who reported at least one drink in the past year) were classified as “drinkers.” A total of about 36% of US males and 41% of US females were described as “obese” (defined as BMI ≥ 30 kg/m2). The analyses included the level of obesity (Class 1, 2, or 3) as outcomes (with Class II defined as BMI 35-<40 kg/m2 and Class III as BMI ≥ 40 kg/m2) making it possible to judge the effects of alcohol on varying levels of obesity.
The present study reports that male current drinkers versus nondrinkers had 38% lower odds of Class 3 obesity versus subjects with a healthy weight; female current drinkers versus nondrinkers had more than 30% lower odds of Class I, Class II, or Class III obesity In both sexes, more frequent alcohol consumption was associated with less obesity, while heavy alcohol consumption was associated with increased risk of obesity. Females who reported that they were trying to lose weight consumed more than others, but there was not a strong relation between reported attempts to lose weight and outcomes.
Forum reviewers considered this to be a well-done analysis, with adjustments for most common potential confounding variables. It provides some support for previous findings of an inverse association with obesity for light-to-moderate alcohol consumption but an increase in obesity for heavy consumption. The authors state that this is the first study to be able to provide data showing that the magnitude of the inverse association is stronger for higher levels of weight status (Classes 1 to 3).
Forum members noted, however, that this study was based on assessments of different subjects in each wave of the national surveys, rather than on repeated assessments among the same individuals over time. It is clear that repeated recordings of alcohol intake in prospective cohort studies make it possible to obtain a reliable estimate of any changes in alcohol intake that may occur, rather than having to base results on a single measure, such as only a baseline value. Further, members caution that there are many genetic and lifestyle variables associated with the development of obesity, and residual confounding is always a potential problem in such analyses. Thus, while the present paper provides data indicating that more severe obesity may result from higher intake of alcohol, and that light-to-moderate intake may actually lead to a decrease in the risk of obesity, data from cohort studies with repeated assessments of alcohol and body size may provide more precise estimates of effect.
Reference: White GE, Mair C, Richardson GA, Courcoulas AP, King WC. Alcohol Use Among U.S. Adults by Weight Status and Weight Loss Attempt: NHANES, 2011−2016. Am J Prev Med 2019;57:220−230.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 230: An extensive review of the role of dietary constituents (foods, nutrients, and beverages) in the development of diabetes 1 August 2019
Of all lifestyle factors that relate to health and disease, probably the most difficult ones to evaluate are dietary factors, including foods, nutrients, and beverages. The present paper consists of a meta-analysis (an “umbrella” analysis) based on 53 previous meta-analyses from prospective cohort observational studies. This analysis includes 153 adjusted summary hazard ratios on dietary behaviors or diet quality indices, food groups and foods, beverages, alcoholic beverages, macronutrients, and micronutrients related to the incidence of type 2 diabetes. Data from previous meta-analyses on very few foods or nutrients are adequate to clearly determine their effects, but among those that have been identified as reducing the risk of diabetes, high-quality evidence was found only for whole grains, cereal fiber, and alcohol. As for dietary factors that have strong evidence of increasing the risk of diabetes, the authors of this paper identify only red meat, processed meat, bacon, and sugar-sweetened beverages.
Forum members considered this to be a well-done, appropriate analysis in a paper that summarizes well the current scientific literature. Some members were concerned about the number of assumptions that scientists must make when doing a simple meta-analysis, and especially when attempting an umbrella one; they consider it key to also evaluate single, large prospective studies where adjustments for many confounding socio-economic factors are less likely to be important.
Overall, the results of this paper strongly support most of the findings of previous meta-analyses and umbrella analyses and indicate only a few dietary factors for which “high-quality” evidence exists for an association with the risk of developing diabetes. The clearest evidence from the analyses in this paper, which was based only on prospective cohort studies, is that cereal grains and moderate alcohol lower the risk, while meats and sugar-sweetened beverages increase the risk of diabetes.
Given the complexity of evaluating dietary factors for their relation to disease outcomes, it will be useful for future studies to attempt to measure a multitude of foods, beverages, nutrients, and eating patterns, preferably over time, to evaluate further the association with disease. For now, current evidence suggests that cereals, grains, and moderate alcohol (that decrease risk) and meat and sugar-sweetened beverages (that increase risk) have the most consistent data for a relation to subsequent diabetes mellitus.
Reference: Neuenschwander M, Ballon A, Weber KS, Norat T, Aune D, Schwingshackl L, Schlesinger S. Role of diet in type 2 diabetes incidence: umbrella review of meta-analyses of prospective observational studies. BMJ 2019;365:l2368.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 229: A J-shaped curve for the relation of alcohol consumption to the risk of colorectal cancer — 10 July 2019
While heavy alcohol consumption is recognized as a contributor to the development of colorectal cancer (CRC), an increasing number of studies suggest that moderate alcohol consumption may not have an adverse effect on the risk of CRC, or even decrease the risk.
The present paper, a meta-analysis of 16 studies on the relation of alcohol consumption to invasive CRC, was conducted by leading investigators in the field. Forum members consider this to be a well-done study, with a large number of subjects, the ability to use individual level data in their meta-analysis, and the use of appropriate and complete analytic techniques.
The key finding of their study was that there was a J-shaped curve evident in all of their analytic approaches; their results strongly support a J-shaped association for the relation of alcohol intake to CRC: a slightly lower risk of cancer for light to moderate drinkers and an increased risk for subjects reporting an average of 3 or more drinks/day. Further, they found that their results did not vary by age, obesity, smoking, or family history of CRC. Overall, the effects of benefits/harms were somewhat more striking for cancers in the distal colon than in the proximal colon.
Potential mechanisms for heavy alcohol consumption being related to an increase in risk were discussed by the authors. As for moderate drinking decreasing the risk, potential mechanisms are discussed by a Forum member in this critique. He describes active, beverage-specific metabolites other than ethanol that reach the intestine. In particular, our attention goes to the several microbial catabolites which can be formed via our host microbiota in the colon.
The finding of a J-shaped curve between alcohol and CRC is similar to the relation seen for a number of other diseases, including coronary artery disease, ischemic stroke, dementia, and total mortality. While a linear relation between heavy drinking and certain upper aero-digestive tract cancers has been shown, for certain cancers there may be a J-shaped curve of effect, with reductions in risk for light-to-moderate drinkers.
Reference: McNabb S, Harrison TA, Albanes, Berndt S, Brenner H, Caan BJ, et al. Meta-analysis of 16 studies of the association of alcohol with colorectal cancer. Int J Cancer. 2019 Apr 29. doi: 10.1002/ijc.32377. [Epub ahead of print]
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
A Tribute to Elizabeth Barrett-Connor, MD (1935-2019)
It is with great sadness that we have learned of the death on 9 June 2019 of Elizabeth Barrett-Connor, a major contributor to the field of epidemiology for many decades and, especially, to a scientifically balanced and sound appraisal of the relation of alcohol consumption to health. Elizabeth was a member of our International Scientific Forum on Alcohol Research until April 2019, when she retired from the Forum because of ill health.
With degrees from Mount Holyoke College in Massachusetts, Cornell University Medical College, and London School of Hygiene and Tropical Medicine, Elizabeth also had medical training at the University of Texas Southwestern Medical School and the University of Miami in Florida. Joining the faculty at the University of California, San Diego, in 1970, she became a Distinguished Professor of Family Medicine and Public Health.
As described in the UCSD Faculty Profile from her university, “Dr. Barrett-Connor’s research concerned healthy aging with a focus on gender differences and women’s health. Dr. Barrett-Connor was founder and director of the Rancho Bernardo Heart and Chronic Disease Study, begun in 1972, with continuous support (4 MERIT awards) from the NIH. She served as a principal investigator of many multicenter clinical trials, including the Postmenopausal Estrogen/Progestin Interventions trial, the Heart and Estrogen-Progestin Replacement Study, the Raloxifene Use in the Heart study, and the Diabetes Prevention Program Observational Study. She was Past President of the Epidemiology Section of the American Public Health Association (APHA), the Epidemiology Council of the American Heart Association (AHA), the Society for Epidemiologic Research (SER), and the American Epidemiological Society (AES). She was a member of the Institute of Medicine (IOM), and a Master of the American College of Physicians (ACP).”
The author of more than 1,000 scientific publications (starting with articles on shigellosis and sickle cell anemia in the 1960s), during her career Dr. Barrett-Connor made important contributions to many fields, including epidemiology, gerontology, endocrinology, cardiology, gender effects, and lifestyle factors such as physical activity, diet, and alcohol consumption. She was the key individual responsible for maintaining and extracting data from the very long-term follow up of participants in the Rancho Bernardo Study of Healthy Aging. She was honored by the American Heart Association by the establishment of the annual Elizabeth Barrett-Connor Competition for young trainees in epidemiology.
Dr. Barrett-Connor was a highly respected mentor of young trainees and faculty. It is noteworthy that she was an author on at least 22 scientific publications during 2018-2019 that included, just in 2019, titles such as “Hearing impairment and cognitive decline in older, community-dwelling adults,” “Effects of APOE on cognitive aging in community-dwelling older adults,” “Genetic Ancestry Markers and Difference in A1c Between African American and White in the Diabetes Prevention Program,” “Cardiovascular Risk Factors Associated With Venous Thromboembolism,” and “Lifetime physical activity and late-life cognitive function: the Rancho Bernardo study.”
The obituary in the New York Times on 20 June 2019 by Karen Weintraub included a revealing anecdote about Elizabeth’s early days: “According to family lore, she was heading to the train station to take a nursing school entrance exam when she bumped into a friend. ‘You’d make a terrible nurse,’ the friend was said to have told her. ‘You can’t take orders from anybody.’ Acknowledging the truth of her friend’s comment, Dr. Barrett-Connor instead applied to medical school.”
Dr. Barrett-Connor was presented with a large number of awards. For example, all in one year she received awards from The University of Western Australia, the Society for the Advancement of Women’s Health Research, the Society for Epidemiologic Research, the Cleveland Clinic Foundation Department of Cardiology, and Scripps Clinic and Research Foundation.
In 2018, Dr. Barrett-Connor was awarded the Fred Conrad Koch Lifetime Achievement Award by the Endocrine Society with the following comments: “Elizabeth Barrett-Connor, MD, has made paradigm-shifting contributions in endocrine physiology and the role of hormones in disease pathogenesis (focus on gender differences) in cardiovascular disease, diabetes, osteoporosis, and breast cancer. It is hard to imagine the existence of any other individual whose work reflects such staggering impact. The hallmarks of Dr. Barrett-Connor’s enduring success — a driving quest for the truth, rigorous scientific discipline, and a joyful passion — have infused every aspect of her career, whether as investigator, lecturer, teacher, or mentor. She has helped make women more visible in the endocrinology field, not by example of her own shining star, but by her constant recognition of light coming from others.”
In a tribute to Dr. Barrett-Connor in Diabetes Care in April, 2019, former trainee and now Professor at the University of Cambridge in the UK, Kay-Tee Khaw noted: “When asked what her motto or philosophy of life was in an interview for her local newspaper, La Jolla Light, Elizabeth Barrett-Connor’s response was that she did not have any one particular philosophy so much as an attitude: ‘My defining principle is that I am a pathological optimist.’ Boundlessly curious, fearless, challenging, inspiring, and great fun to be with are some of the words her colleagues and mentees might use to describe her.”
In addition to her unbelievable contributions to the scientific literature and as a mentor to countless trainees and faculty, Elizabeth was a close friend to many of us in the Forum, who always enjoyed meeting with her at numerous conferences. She especially appreciated the contributions of good food, wine, and vibrant conversation on such occasions.
Among the number of comments received from Forum members were the following: “Dr. Barrett-Connor enjoyed critical debate, not only of scientific topics but also of politics and cultural issues. At a European conference, Elizabeth was one of the outstanding speakers with a talk on nutritional experiences in the US. When a female colleague from Finland was so moved by a certain theme and started crying Elizabeth commented very politely ‘I don`t like weeping women.’ Elizabeth was a strong woman with a lot of empathy and a lot of humour. She has truly been a wonderful and worldwide ambassador for public health and humanity.”
Stated another member: “Elizabeth argued against some of the best, was a clear, linear thinker, and never wavered in self-confidence. She strongly believed in the scientific method, as stated by Popper: ‘The only reason to have a hypothesis is to try to disprove it. If you couldn’t disprove it, you might be right—not guaranteed to be right, but you might be right.’ It teaches us about humility in science; something we need more of.”
We will sorely miss her
================================================================
Critique 227: A reduced risk of chronic obstructive pulmonary disease (COPD) associated with the intake of some alcoholic beverages – 29 May 2019
Chronic obstructive pulmonary disease (COPD) is a major health problem and cause of death throughout the world. While cigarette smoking is known to be the most important risk factor, there are limited data available on the relation of alcohol consumption to the condition. Given that moderate alcohol intake has been shown to decrease the risk of many inflammatory conditions, it may also affect the risk of COPD, which is associated with marked inflammation of lung tissues.
In the present study, the investigators related total alcohol consumption and intake of specific alcoholic beverages with the risk of COPD, based on data from more than 44,000 Swedish men in a population-based prospective cohort study. A total of 2,177 COPD cases were ascertained during follow up that extended up to 17 years. In their analyses, the authors had data permitting them to evaluate a number of demographic and lifestyle factors as potential confounders (including smoking status and pack-years of smoking, education, physical activity, BMI, and some indices of diet). However, there were very few ex-smokers or current smokers among the non-drinkers, making it somewhat difficult to adequate adjust for cigarette use as a cause of COPD.
Forum members thought that there are a number of deficiencies in this study that somewhat weaken its conclusions; especially important was the lack of ability to consider the pattern of drinking (regular, moderate versus binge drinking). Still, there is a strong consistency between the results of this study (indicating a “J-shaped” or “U-shaped” curve for alcohol intake and COPD) and results from extensive previous epidemiologic and experimental research.
Overall, the cumulative research findings now suggest that pulmonary disease might be included among the “diseases of ageing” that show a reduction in risk among moderate consumers of certain alcoholic beverages. Based on some previous epidemiologic studies and results from numerous experimental studies, data now suggest that, in addition to alcohol, the polyphenols present in wine and some beers may offer protection against COPD. While in the present study red wine consumption was associated with the lowest risk of COPD, Forum members acknowledge residual confounding by other lifestyle factors may still play a role.
Reference: Kaluza J, Harris HR, Linden A, Wolk A. Alcohol Consumption and Risk of Chronic Obstructive Pulmonary Disease: A Prospective Cohort Study of Men. Am J Epidemiol 2019;188:907–991.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 226: Consumption of red wine may lower the risk of lethal prostate cancer —- 16 May 2019
In an analysis from the Health Professionals Follow-up Study, the investigators evaluated the relation of alcohol consumption in their more than 45,000 study participants to the development of lethal prostate cancer. They related alcohol first to the overall risk of prostate cancer among all subjects, and then focused on the 5,182 men who developed non-metastatic prostate cancer to judge their risk of developing lethal prostate cancer or mortality. They judged the alcohol intake both prior to the diagnosis and after a diagnosis of prostate cancer. For reported alcohol consumption among subjects prior to the initial diagnosis of prostate cancer, there was a small (16%) but significant reduction in the risk of lethal prostate cancer among subjects reporting any alcohol consumption, but no significant effects of specific beverages on the risk of lethal prostate cancer. However, total mortality was lower for consumers of total alcohol intake and for most categories of intake for all types of beverage.
When they then related post-diagnosis alcohol intake (after the diagnosis of non-metastatic prostate cancer), the investigators found that red wine consumption was associated with a 50% reduction in the risk of developing lethal prostate cancer or mortality. There were no significant relations between total alcohol consumption or between the intake of other specific beverages and lethal disease.
The authors describe a number of hypotheses by which red wine, with its combination of high levels of polyphenols in addition to alcohol, may have lowered the risk of lethal prostate cancer. And there are numerous basic science experiments that have shown how polyphenols impede the development and growth of cancer cells. Presumably, it was not due to the alcohol in red wine, as similar amounts of alcohol in other beverages did not show a protective effect. While the effects of various polyphenols may play a role, at present the mechanisms of such an effect are not known.
Forum reviewers considered this to be a very well-done study and analysis, with repeated assessments of alcohol intake and essentially complete ascertainment of lethal prostate cancer and mortality. Forum members agree with the conclusions of the authors: “Our results indicate that moderate alcohol intake among men with prostate cancer is not associated with a higher risk of progression to lethal disease or overall mortality. The potential benefit of red wine on prostate cancer progression merits additional research.”
Reference: Downer MK, Kenfield SA, Stampfer MJ, Wilson KM, Dickerman BA, Giovannucci, EL, et al. Alcohol Intake and Risk of Lethal Prostate Cancer in the Health Professionals Follow-Up Study abstract. J Clin Oncology 2019 Pre-publication: : DOI https://doi. org/10.1200/JCO.18. 02462
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 225: Moderate alcohol consumption may lower the risk of chronic kidney disease — 8 April 2019
While numerous studies have found that moderate consumers of alcohol tend to be at a lower risk of developing chronic kidney disease (CKD), potential mechanisms for such an effect are unclear. The present large prospective, population-based, multi-cultural study provides important additional data on the effects of alcohol intake on the initial diagnosis of CKD over many years. It is based on data from the Atherosclerosis Risk in Communities Study and reports the relation of varying levels of alcohol consumption, versus non-drinking, to the incidence of CKD over a 24 year follow-up period.
Among the strengths of the study are the very large number of subjects (n=3,664) who developed CKD during follow up, using advanced methods for diagnosing the disease. Only baseline alcohol intake was used as the exposure and type of beverage or pattern of drinking could not be assessed; however, the authors considered multiple appropriate potentially confounding variables in the analyses, including total energy intake, age, sex, race-center, income, education level, health insurance, smoking, and physical activity. In comparison with the 25% of subjects in their analyses who were life-time abstainers, for subjects reporting all levels of alcohol consumption (≤1 drink per week, 2 to 7 drinks per week, 8 to 14 drinks per week, and ≥15 drinks per week), there was a statistically significant decrease in risk of incident CKD (from a 12% decrease in risk for the lowest category of alcohol intake to a 29% decrease for subjects reporting that they consumed 8-14 drinks/week).
The authors conclude: “Consuming a low or moderate amount of alcohol may lower the risk of developing CKD. Therefore, moderate consumption of alcohol may not likely be harmful to the kidneys.” Forum members agree that this study supports much earlier research showing a protective effect of moderate drinking on the risk of kidney disease. While mechanisms are not clear, effects of alcohol on renal vessels that are similar to those described for coronary and cerebrovascular arteries may play a role.
Reference: Hu EA, Lazo M, Rosenberg SD, Grams ME, Steffen LM, Coresh J, Rebholz CM. Alcohol Consumption and Incident Kidney Disease: Results From the Atherosclerosis Risk in Communities Study. J of Renal Nutrition, 2019, in press. DOI: https://doi.org/10.1053/j.jrn.2019.01.011
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 224: A brief summary of the association between wine/alcohol consumption and health in diabetics 12 March 2019
Diabetes mellitus is an increasingly common condition throughout the world, related closely to increases in obesity and ageing of populations. There are many, serious health conditions associated with diabetes, especially a marked increase in the risk of morbidity and mortality from cardiovascular disease. Scientific data from well-done cohort studies have demonstrated for decades that people who are moderate consumers of alcohol tend to have a considerably lower risk of developing diabetes in the first place, and diabetics who consume moderate amounts of alcohol are, in comparison with abstainers, at much lower risk of developing cardiovascular disease.
The present “mini-review” by scientists who have previously carried out the first large randomized clinical trial of wine and health outcomes among diabetics provides an interesting overview of the association of alcohol, particularly of wine, with health. The authors expand the implications of their research and conclude that “Initiating moderate alcohol consumption among well controlled persons with type 2 diabetes is apparently safe, in regard to changes in heart rate variability and carotid plaque formation.” Their findings have stimulated this critique by our Forum to also consider if available data now suggest that physicians should encourage the modest consumption of wine with food for selected patients with diabetes.
Our critique describes a number of risk factors (lipid levels, glucose, insulin, etc.) and intermediate conditions (such as endothelial function and arterial calcification) that have been shown to relate to the consumption of alcohol. Some Forum members believe that while all of these associations are important, the key information needed is the effect of alcohol consumption on disease outcomes themselves (coronary heart disease, stroke, dementia, etc.) and on mortality. At present, any recommendations regarding alcohol consumption must be based primarily on observational data from long-term cohort studies.
The key question we discuss in this critique is “Should physicians advise their older diabetic patients who are non-drinkers to begin to consume small amounts of an alcoholic beverage?” The consensus of Forum members is that current data suggest that, at a minimum, we should not advise such patients who currently consume alcohol moderately to stop their consumption. On the other hand, most members emphasize that we should discuss alcohol consumption with all patients. If they are at least occasional consumers of alcohol (the large majority of patients in most Western countries), our only advice might relate to the pattern of drinking. At present, the pattern commonly shown to be associated with the lowest risk of the usual diseases of ageing and mortality appears to be small amounts of alcohol, especially wine, with meals on a regular basis. For patients who indicate that they are drinking only in binges, we should emphasize the adverse health effects (for them as well as for society), and encourage a healthier pattern of drinking.
But what about current non-drinkers? For middle-aged or older non-drinkers who avoid alcohol because of religious prohibitions, previous misuse of alcohol, certain medical conditions, or a stated dislike of alcohol, our advice on prevention of disease should focus on not smoking, getting exercise, eating a healthy diet, and trying to avoid obesity. But for patients without such conditions that would indicate that they should avoid alcohol, many Forum members believe that they should at least be told of the current scientific evidence of possible beneficial health effects of regular, moderate intake. However, until considerably more data on its effects are available, we are not encouraging physicians to prescribe alcohol consumption for their diabetic patients.
Reference: Golan R, Gepner Y, Shai I. Wine and Health–New Evidence. Mini Review. European Journal of Clinical Nutrition. https://doi.org/10.1038/s41430-018-0309-5; 2019: in press.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 223: A new major review of the relation of alcohol consumption to the risk of dementia. 17 January 2019
While many studies have shown that excessive alcohol intake is associated with cognitive impairment and increased risk of dementia, most cohort studies have shown that the risks of these outcomes are lower among light-to-moderate drinkers than among abstainers. The authors of this paper conducted a scoping review on this topic, based on a systematic search of systematic reviews published from January 2000 to October 2017. A total of 28 systematic reviews were identified relating alcohol intake at various time periods to incidence of cognitive impairment/dementia, specific brain functions, or induced dementias. The authors report that light to moderate alcohol use in middle to late adulthood was associated with a decreased risk of cognitive impairment and dementia, but heavy alcohol use was associated with changes in brain structures, cognitive impairments, and an increased risk of all types of dementia.
Forum members considered this to be a well-done analysis, but were concerned that the focus was only on the potentially adverse effects of heavy drinking, with little regard or discussion of the findings of protection against such cognitive outcomes among light or moderate drinkers. Forum members point out that there are very many adverse health effects, both for the drinker and for society, resulting from heavy drinking. To them, the most interesting and provocative aspect of this paper was the conclusion of a protective effect against cognitive decline and dementia associated with light-to-moderate alcohol consumption.
Scientific data, including the results of the present systematic analysis, are very consistent in showing that cognitive decline, associated impairments in the functions of daily living, incident dementia, and survival are all associated favorably with light-to-moderate consumption of alcohol in middle age. The reasons and mechanisms that lead to these associations deserve further evaluation. With the increasing ageing of populations throughout the world, cognitive decline and dementia are expected to increase and create serious challenges for health care providers. Insight into ways of preventing or delaying the onset of such cognitive decline (in addition to decreasing the prevalence of heavy alcohol intake, the focus of this paper) could be extremely important in planning for the future.
Reference: Rehm J, Hasan OSM, Black SE, Shield KD, Schwarzinger M. Alcohol use and dementia: a systematic scoping review. Alzheimer’s Research & Therapy 2019; 11: pre-publication. https://doi.org/10.1186/s13195-018-0453-0
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 222. A new analysis relating alcohol intake to coronary heart disease – 20 December 2018
In an attempt to judge the effects of alcohol on the risk of coronary heart disease (CHD), the authors have carried out analyses using a sample of subjects from the National Epidemiologic Survey on Alcohol and Related Conditions III (NESARC-III). They based their exposure to current alcohol use on a single assessment at baseline of self-reported consumption during the past year, when the subjects were an average of 38.9 years of age. In addition they asked subjects if they had consumed larger amounts of alcohol when they were younger.
Their assessment of CHD was based on answers to questions at baseline as to having been told by a doctor that they had chest pain or CHD, apparently within the same 12-month period when they were asked about current alcohol consumption. Nothing in the paper indicates that the authors had data on the subsequent development of CHD during a follow-up period. When relating reported alcohol intake to CHD, they excluded 1,671 who reported “previous CHD,” although for this relatively young group it is questionable how many actually had CHD, as no data on validation of the diagnosis was done. For unclear reasons, for their comparison group they excluded any subjects with conditions that “may increase the risk of CHD (e.g., pneumonia, influenza, tuberculosis, liver disease, neurologic conditions, osteoporosis, arthritis, STD) and can be viewed as comorbid conditions related to alcohol consumption.”
Given that the exposure (alcohol) and outcome (CHD) were apparently from the same time period, there is reason to worry about reverse causation (i.e., subjects may have developed CHD and changed, either decreased or increased, their alcohol consumption during the same period).. As for using the self-reported amount of alcohol consumed at some time in the past as the exposure, there is a large chance of serious misclassification of exposure due to recall bias and bias according to current alcohol intake (as subjects currently reporting greater amounts of alcohol were more likely to report even higher intake in the past).
With only a single assessment of current alcohol intake, an inadequate assessment of long-term alcohol intake, a lack of data during a follow-up period for the main outcome, CHD, and no validation of the outcome, Forum members considered that this was an unusual cohort to use when attempting to judge the relation of changes in alcohol consumption to the development of CHD. The necessary elements for a useful analysis were not available to these investigators using this population sample.
In any case, results from many well-done long-term cohort studies with repeated assessments of alcohol and validated CHD outcomes during follow up have already provided key data on this topic: they almost uniformly demonstrate that light-to-moderate drinkers who do not binge drink have significantly lower risk of developing CHD. The present analysis does not provide data that would question such findings.
Reference: Fan AZ, Ruan WJ, Chou SP. Re-examining the relationship between alcohol consumption and coronary heart disease with a new lens. Pre-publication. Preventive Medicine 2019;118:336=343.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 221: The relation of alcohol intake to stomach cancer – 20 November 2018
There have been conflicting results from studies of the association between alcohol intake and the risk of gastric cancer. Some of the differences among studies have related to mixing subjects from Western countries with those from Asia, where dietary patterns, lifestyle factors, drinking patterns, and types of alcohol consumed differ from those among Western populations. Results usually differ between Asian and Western populations.
The present study is based on almost 500,000 subjects from the USA with follow up for a median of 15.5 years. The investigators identified a total of more than 1,300 cases of gastric cardia cancer (GCA) or gastric noncardia cancer (GNCA ). The authors report: “We found no association between higher alcohol consumption and GCA or GNCA, when examined as total alcoholic beverage intake or individual beverage types of beer, wine and liquor. Furthermore, we observed no association by stratum of sex, ethnic group, educational level or smoking status. We did, however, observe lower risk of GNCA among participants who drank up to one drink per day (HR = 0.81, 95% CI: 0.67–0.97) compared to nondrinkers.” They conclude: “Alcohol consumption was not associated with increased risk of GCA or GNCA in this large U.S. cohort.”
Forum members considered this to be a large, very well-done analysis; subjects were aged 50-71 years at baseline, appropriate for evaluating the risk of gastric cancer. Data on a large number of potential confounders were included in the analysis. Diagnosis of cancer was from state cancer registries, shown to be very accurate. The statistical analyses included restricted spine analysis to test for a dose-response curve (not found), and excluded the first two years after alcohol assessment to lower the risk of reverse causality. Further beverage-specific analyses were carried out, and did not show differences according to whether the consumption was of beer, wine, or spirits.
Weaknesses included only one assessment of alcohol intake, at baseline, and no data on binge drinking or other aspects of the pattern of drinking. Subjects were generally well-educated, white, and consumed alcohol moderately (75% reported one drink or less). Thus, these results may not pertain to other ethnic groups or to heavier consumers of alcohol.
Overall, these results provide further support for the lack of an association between light-to-moderate alcohol intake and the risk of gastric cancer. The significant decrease in risk of gastric non-cardia cancer associated with consumption of up to one drink/day should obviously be replicated, but the authors provide some potential mechanisms that could explain such a phenomenon. The study did not support previous data suggesting that wine consumption might have additional benefits to those of other beverages in terms of cancer risk.
Reference: Wang SM, Freedman ND, Loftfield E, Hua X, Abn CC. Alcohol consumption and risk of gastric cardia adenocarcinoma and gastric noncardia adenocarcinoma: A 16-year prospective analysis from the NIH-AARP diet and health cohort. Int J Cancer 2018; pre-publication.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 220: An unusual analysis relating alcohol intake to mortality – October 16, 2018
The authors of this treatise on alcohol consumption and mortality combined, for an unclear reason, results from two, very different studies: one from the Veterans’ Health Administration, based on outpatient clinical medical records, and the other from a national survey in the USA [The National Health Interview Survey (NHIS)]. Unfortunately, the VA data did not adjust for tobacco use or other important lifestyle habits, and are not useful in judging the effects of alcohol consumption on mortality.
While the NHIS survey included data on potential confounding, both it and the VA study based their analyses on a single estimate of alcohol consumption. The authors then created a variable that they stated was associated with the lowest risk of mortality and compared results from such alcohol intake with data from subjects reporting less or more alcohol. They combined data on all subjects reporting 1 to 2 drinks/week, so did not have the ability to provide a precise estimate of the association between low levels of intake and mortality risk. They did not comment on the effects that under-reporting of alcohol would have on their studies (and most investigators agree that the self-reported level of alcohol consumption is usually an under-estimate of actual consumption). Further, they did not point out the very much higher risk of mortality of non-drinkers, compared with moderate drinkers, demonstrated in their data.
To the extent that people accurately reported their past drinking status (never vs former), this study should put to rest concerns that protective associations of drinking versus non-drinking arise from inclusion of former drinkers into non-drinking groups. Never drinkers had higher risk of mortality than former drinkers in this study.
There are considerable data from many well-done cohort studies that have repeated assessments of alcohol intake over many decades and the subsequent risk of mortality. Such studies provide very clear and consistent results indicating a J-shaped curve: lower risk of mortality for light and moderate drinkers than for non-drinkers (even lifetime abstainers) and some increase in risk for heavy drinkers. These are the studies that can provide reliable information upon which drinking guidelines for different individuals and populations can be based.
Reference: Hartz SM, Oehlert M, Horton AC, Grucza RA, Fisher SL, et al. Daily Drinking Is Associated with Increased Mortality. Alcoholism: Clin & Experimental Research 2018; pre-publication. DOI: 10.1111/acer.13886.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 219: A global overview of alcohol consumption and health – 3 September 2018
Investigators working with data from the Global Burden of Diseases, Injuries, and Risk Factors Study 2016 have combined data from 195 locations around the world, from 1990 to 2016, for both sexes and for 5-year age groups between the ages of 15 years and 95 years and older. Their purpose was to determine how estimates of the prevalence of current drinking, abstention, the distribution of alcohol consumption among current drinkers in standard drinks daily (defined as 10 g of pure ethyl alcohol) relate to alcohol-attributable deaths and disability-adjusted lifeyears (DALYs). The paper does not present estimates of the effects of alcohol on a key outcome, total mortality.
The paper presents a huge number of analyses with data specific for each contributing center. However, the Forum considers that real problems emerge when they attempt to combine data from many divergent cultures to determine a single association between alcohol consumption and health. Many lifestyle and cultural factors strongly modify the relation of a given amount of alcohol to health and diseases. Such modifying factors include especially the socio-economic status of the individual, circumstances such as drinking with or without food, the pattern of drinking (regular moderate versus binge drinking), the type of beverage (e.g., wine versus spirits), the intention of the individual (drinking to get drunk versus drinking to enhance meals), level of physical activity, etc. When such modifying factors are not taken into consideration, the estimated intake of a given amount of alcohol (even if accurate), provides an incomplete assessment of the effects of alcohol on health.
The authors spend much of their paper focusing on their contention that these analyses have large implications for setting alcohol policy around the world. They then expand primarily on ways of decreasing alcohol intake world-wide through changes in guidelines. However, their failure to consider specifics of the culture for which the policy is being formulated, such as evaluating other lifestyle factors, the pattern of drinking, underreporting of alcohol intake, cultural factors, etc., negates their ability to provide useful information that is applicable to any single population: their guidelines end up applying to no one. And, their specific statement that zero consumption would be preferable everywhere is sharply contradicted by consistent reports from very large, well-done cohort studies (where individual data are available) which indicate that non-drinkers have higher risks of cardiovascular disease and total mortality than regular moderate drinkers who do not binge drink.
Setting guidelines for the public regarding alcohol consumption requires information not only on the reported intake but on other health conditions, as well as genetic, lifestyle, and cultural factors that may modify the effects of alcohol. Further, advice differs by age and the key problems within a country that the guidelines are directed toward improving. In the opinion of the Forum, despite the massive amount of work done by the investigators in the preparation of this paper, the overall combined results from such divergent populations have little applicability in setting guidelines that would lead to avoidance of alcohol abuse in any specific group of people around the world — they apply to no specific population.
Reference: GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. www.thelancet.com Published online August 23, 2018 http://dx.doi.org/10.1016/S0140-6736(18)31310-2
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here
================================================================
Critique 218: Long-term study of alcohol intake and the risk of Alzheimer Disease or other types of dementia – 21 August 2018
While there is general agreement that the moderate intake of alcohol is associated with a significantly lower risk of cardiovascular disease, there are less data on the relation of moderate alcohol consumption to dementia. However, the vast majority of well-done prospective studies indicate that, in comparison with non-drinkers, moderate, non-binge-drinking older adults have lower risk of Alzheimer Disease and other types of dementia. The present study provides important information on this association by monitoring for the development of dementia among subjects in a large cohort of British civil servants (the Whitehall Study) over more than two decades; there were repeated assessments of alcohol consumption.
The main results indicate that abstinence in middle life is associated with a significantly higher risk of dementia than the risk among moderate drinkers, while subjects reporting the intake of larger amounts of alcohol or evidence of an alcohol use disorder are at increased risk of dementia. Specifically, the study shows that among the 397 cases of dementia that were recorded over a mean follow up of 23 years, abstinence in midlife was associated with a 47% higher risk of dementia compared with consumption of 1-14 units/week (a British unit is the equivalent of 8 grams of alcohol). There was a 17% increase in risk of dementia for those reporting more than 14 units/week. With repeated assessments of alcohol the authors also calculated trajectories of alcohol consumption from midlife to early old age, with continued abstinence being associated with an increase in dementia of 74% and a decrease in consumption with an increase of 55% in comparison with subjects reporting continued moderate consumption. In several analyses, wine consumption was associated with more favorable effects than those of other beverages.
Forum members thought that this was a well-done analysis, but considered that the data presented do not allow for a firm determination of a cut-point for increased risk of dementia from alcohol intake. While the authors provide estimates of a linear increase in dementia risk for subjects reporting more than 14 units/week or reporting evidence of alcohol abuse, they do not give data that permits an estimate of the level of intake where the risk of dementia exceeds that of non-drinkers.
Overall, the results showing a decreased risk of dementia for moderate drinkers support the findings from most well-done prospective cohort studies. As for implications for policy, the study further shows that, in terms of the risk of dementia as well as cardiovascular disease, middle-aged and older individuals who are consuming alcohol moderately and without binge drinking should not be advised to stop drinking.
Reference: Sabia S, Fayosse A, Dumurgier J, Dugravot A, Akbaraly T, Britton A, Kivimäki M, Singh-Manoux A. Alcohol consumption and risk of dementia: 23 year follow-up of Whitehall II cohort study. BMJ 2018;362:k2927. http://dx.doi.org/10.1136/bmj.k2927
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================
Critique 217: Alcohol, cancer, and mortality: Further affirmation of the J-shaped curve for mortality and increase in incidence of cancer with larger intake of alcohol – 9 July 2018
Scientific studies have shown consistently that that the consumption of small amounts of alcohol on a regular basis is associated with a lower risk of total mortality, while consumption of large amounts is associated with an increased risk of certain cancers and mortality. The present report is from a population-based cohort study of almost 100,000 older subjects who were followed for a median of 8.9 years. There were large numbers of deaths (n=9,599) and incident cancers (n=12,763) diagnosed during follow up, which should lead to more precise estimates of effect.
The authors report that light-to-moderate drinking was associated with lower total mortality, but the risk of incident cancer increased with greater alcohol consumption, especially the intake of beer or spirits. However, the analyses indicate that the slightly increased risk of cancer associated with moderate alcohol consumption was less than the beneficial effect on mortality.
Specifically, in comparison with never drinkers or very light (< 1 drink/week) drinkers, the study shows lower mortality for “light-to-moderate” alcohol consumers (up to 2 drinks/day) but greater mortality among subjects classified as “heavy” (2 to < 3) or “very heavy” (3+ drinks/day) consumers. In beverage-specific analyses, there was a slight increase in total mortality for reported intake of spirits starting at the consumption of about 1 ½ drinks/day and for beer at or above about 2 drinks/day; no significant increase in cancer risk was associated with wine consumption, regardless of the amount. The authors conclude that “there is a J-shaped association between alcohol and mortality in older adults, which remains after adjustment for cancer risk.”
Forum member considered this to be a well-done analysis, and shows, essentially for the first time in a single study, how the beneficial effects of light and moderate drinking on cardiovascular disease and total mortality exceed the slight increase in cancer risk for alcohol consumption at this level. In other words, while even light-to-moderate drinking may be associated with a slight increase in the risk of certain cancers, such drinking still favorably affects the overall risk of mortality.
Reference: Kunzmann AT, Coleman HG, Huang W-Y, Berndt SI. The association of lifetime alcohol use with mortality and cancer risk in older adults: A cohort study. PLoS Med 2018;15:e1002585. https://doi.org/10.1371/journal.pmed.1002585.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================
Critique 216: Strong effects of five lifestyle factors on risk of mortality and longevity of life – 31 May 2018
It has long been known that a number of lifestyle factors – such as not smoking, being physically active, avoiding obesity – decrease the risk of many of the “diseases of ageing,” especially cardiovascular disease and cancer. The present paper from the Nurses’ Health Study and the Health Professionals Follow-up Study is especially important as it demonstrates the joint effects of five healthy factors on disease-specific and total mortality in very large cohorts of subjects. The “healthy lifestyle factors” evaluated were (1) never smoking, (2) body mass index of 18.5 to 24.9 kg/m2, (3) ≥30 min/d of moderate to vigorous physical activity, (4) moderate alcohol intake, and (5) a high diet quality score (upper 40%). The similarity in education and other socio-economic factors of the subjects in these studies tends to reduce potential confounding by such factors.
There were more than 42,000 deaths in their cohorts during follow-up periods extending up to 34 years. The effects of these factors on subsequent risk of mortality were striking: for subjects meeting criteria for all five factors versus none, there was an 84% reduction in all-cause mortality, 65% less cancer mortality, and 82% less cardiovascular disease mortality. The overall effect was associated with 12 to 14 additional years of life after age 50 for subjects meeting criteria for all five factors.
Forum members consider this to be an excellent study, as it was based on data from very large cohorts of well-monitored subjects over many decades, with essentially full ascertainment of mortality. This study strongly suggests that the leading causes of premature death throughout the developed world are, to a large extent, preventable.
Reference: Li Y, Pan A, Wang DD, Liu X, Dhana K, Franco OH, Kaptoge S, Di Angelantonio E, Stampfer M, Willett WC. Hu FB. Impact of Healthy Lifestyle Factors on Life Expectancies in the US Population. Circulation 2018;137:00–00. (Pre-publication). DOI: 10.1161/CIRCULATIONAHA.117.032047.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 215: Long-term effects of smoking and moderate drinking on the quality and longevity of life of elderly women — 9 May 2018
While essentially all epidemiologic studies have shown adverse health effects of cigarette smoking and beneficial effects of moderate alcohol consumption, the present study is important as it follows a cohort of elderly women into very old age. It is a prospective cohort study of 9,704 women at least 65 years of age, who were living independently at baseline and were not heavy drinkers; they had a mean baseline age of 71.7 years (range 65-99) and underwent repeated assessments of lifestyle habits starting in 1986 to 1988. They were followed longitudinally until death, loss to follow-up, or to April, 2016. Outcomes included grip strength, walking speed, prevalence of threshold scores for self-reported health, difficulty with three or more instrumental activities of daily living (IADLs), depression, prevalence of falls, living in a nursing home, and death after 10- or 20-year follow up. The main comparisons evaluated in this study were between women who were smokers and those who consumed alcohol moderately, with each analysis adjusted for the other exposure.
Forum members considered this to be a well-done study that provides some important data relating effects of smoking and moderate drinking on function and mortality in very elderly subjects (an age group where data are lacking). There were criticisms that the study does not report the effects of moderate drinking among smokers; previous studies have shown that the adverse effect of smoking is modified by moderate alcohol intake. Further, given that the reasons why some women quit drinking during follow up are not known, the article does not contribute to clarification of the problem of reverse causation (e.g., healthier women may tend to continue drinking whereas sicker women stop alcohol consumption). Also, the authors did not adjust for some strong confounders, especially those related to socio-economic status (SES).
Nevertheless, the results of this study make a real contribution to our knowledge of the effects of drinking on both quality of life and mortality among women who are 65 years or older. The follow up of subjects continued for a least 20 years, by which time almost 70% of the women had died. Hence, the effects on mortality should be excellent estimates. As expected, women who were smokers had greater risk for almost all adverse outcomes, while drinkers who continued to consume moderate alcohol into old age had the most favorable outcomes. While the authors report that women who reported drinking at baseline but quit later on had mortality risks that were intermediate between non-drinkers and persistent drinkers, the reasons why some women quit drinking were not known. Hence, it is appreciated that continued drinking could be only a marker of better health, and not the cause.
Reference: Nelson HD, Lui L, Ensrud K, Cummings SR, Cauley JA, Hillier TA. Associations of Smoking, Moderate Alcohol Use, and Function: A 20-Year Cohort Study of Older Women. Gerontology & Geriatric Medicine 2018;4:1–9. Pre-publication.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 214: Some methodologic problems in a recent paper urging changes in drinking guidelines – 23 April 2018
Using individual-participant data from a number of large studies, predominantly from the UK and other European countries, the authors of the present paper have estimated the association between the reported level of alcohol intake among drinkers with cardiovascular outcomes and mortality. They conclude that the lowest risk of these outcomes is from the intake of less than 100 g of alcohol per week, and that guidelines for the public should reduce the upper limits for the amount of alcohol that could be safely consumed.
Forum members identified a number of flaws in these analyses, including failure to separate advice for men versus women or for older adults versus young people. Further, the authors do not point out the effects of under-reporting of intake, the marked differences in many health effects according to type of alcoholic beverage (such differences are shown only in their supplement but not mentioned in the abstract); also, there is little discussion of the importance of the pattern of drinking on health results.
Most important, by excluding never-drinkers as a reference group in their main analyses, the authors essentially eliminated the ability to evaluate for any potentially beneficial (or adverse) effects of light-to-moderate drinking as compared with non-drinking. This is problematic, as in essentially all previous large studies, moderate drinkers are those for whom significant and large benefits have been reported for risk of cardiovascular disease and total mortality.
Guidelines for the public regarding alcohol intake relate to many factors, including the net overall physiologic effects on health as well as the particular needs of different countries and cultures. And, as in this study, the inclusion of results from so many different cultures is a problem for determining appropriate guidelines for alcohol intake. Given that culturally specific drinking patterns, type of beverage, and many other lifestyle factors modify the health effects of alcohol, mixing data from markedly different cultures may give results that may not be appropriate for any specific population.
Reference: Wood AM, Kaptoge S, Butterworth AS . . . John Danesh, et al, for the Emerging Risk Factors Collaboration/EPIC-CVD/UK Biobank Alcohol Study Group (120 authors). Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet 2018;391:1513-1523.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 213: A meta-analysis on lifestyle factors, cardiovascular disease, and total mortality for a very large number of middle-aged and elderly women – 27 March 2018
Overall, Forum members considered this to be a well-done paper that provides additional information on alcohol’s effects on CVD and mortality among a very large number of middle-aged or elderly women. Although women markedly increase their risk of CVD following menopause, this is a group of women for whom data are sparse. Weaknesses of the analysis include a lack of information on the pattern of drinking (binge versus regular), type of beverage, and drinking alcohol with or without food. It is of note that in some of the studies included in the meta-analysis, factors such as HDL-cholesterol and fibrinogen were adjusted for in the study; given that these are mechanisms of alcohol’s effects, overall results will surely underestimate the effects. Further, as the authors point out, this study provides little information on the physiologic mechanisms of alcohol’s effects on health.
Forum members praised the authors for this meta-analysis of a very large dataset. It strengthens previous analyses that show that each of the lifestyle factors considered – not smoking, not becoming obese, being physically active, and regularly consuming small to moderate amounts of alcohol – benefit health. The more healthy lifestyle factors a subject has, the greater the benefit.
It will be especially important that future research evaluates what happens if subjects change their lifestyle habits, as such results would help target specific behavioral changes. There are very limited data available on this at present, but such studies that have been done suggest that the onset of moderate drinking among non-drinkers, or a slight increase in alcohol consumption among light drinkers, have beneficial effects on health. Still, it is appreciated that moderate alcohol consumption is only one of a number of factors making up a “healthy lifestyle,” which is clearly associated with less cardiovascular and other diseases and a much lower risk of mortality.
Reference: Colpani V, Baena CP, Jaspers L, van Dijk GM, Farajzadegan Z, Dhana K, Tielemans MJ, Voortman T, Freak-Poli R, Veloso GGV, Chowdhury R, Kavousi M, Muka T. Franco OH. Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: a systematic review and metaanalysis. European Journal of Epidemiology 2018; pre-publication. https://doi.org/10.1007/s10654-018-0374-z
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 212: Is it the alcohol or other substances in wine that lead to beneficial health effects? — 15 March 2018
While epidemiologists have long noted that consumers of wine tend to have better health outcomes than consumers of other alcoholic beverages, it has always been of concern that we were comparing drinkers, and not the drink itself. In recent years, many basic scientists have evaluated the non-alcoholic constituents in wine, and most studies show beneficial health effects from polyphenols and other components in wine as well as beneficial health effects from the alcohol in wine.
The present study provides an excellent review of clinical trials that compared the effects of wine versus no intervention or versus the effects of other alcoholic beverages. The specified outcomes related to effects on lipids, glucose/insulin metabolism, hemostatic mechanisms, and inflammatory/endothelial systems. The authors conclude that “The most repeated result of wine consumption is on lipid metabolism, attributed mainly to ethanol, while wine micro-constituents seem to have an important role mainly in haemostatic and inflammatory/endothelial systems.” Forum members cite several other important effects of wine micro-constituents, including demonstrated effects of such components at the cellular, molecular, and gene levels to sustain increased fibrinolytic activity, which is closely related to the development of cardiovascular disease.
Forum members were unanimous is considering that this was an excellent review of human clinical trials on the topic; the paper does not, however, comment on the mechanisms by which micro-constituents may operate to improve health. Given that since virtually none of the wine micro-constituents circulates in the human biofluids in their native form, it is especially important that the catabolites of wine micro-constituents be better defined and evaluated.
Overall, current data indicate that wine may be especially effective in lowering the risk of cardiovascular disease not only through the alcohol it contains, but also from a number of its key polyphenols. Forum members also point out that, for beneficial health effects of any type of alcoholic beverage, the pattern of drinking is especially important: the consumption of small or moderate amounts on a regular basis, and preferably with food.
Reference: Fragopoulou E, Cholevaa M, Antonopoulou S, Demopoulos CA. Wine and its metabolic effects. A comprehensive review of clinical trials. Metabolism Clinical and Experimental 2018;83:102-119.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 211: Effects of alcohol and aldehydes on DNA and risk of cancer; potential implications from a study in mice — 22 January 2018
The authors of this paper, based on an extensive basic scientific experiment in mice, describe the features and mutational landscape of DNA damage caused by acetaldehyde, an endogenous and alcohol-derived metabolite. This damage results in DNA double-stranded breaks that, despite stimulating recombination repair, also cause chromosome rearrangements. Furthermore, the authors identify how the choice of DNA-repair pathway and a stringent p53 response limit the transmission of aldehyde-induced mutations in stem cells.
Forum members considered this to be a well-done series of experiments that add additional data on the effects of aldehyde on cellular damage, which could potentially lead to an increased risk of cancer. While interesting, these results in mice have limited applicability to the effects of alcohol in humans, as the study conditions do not correspond to that found in real life. For example, the levels of ethanol used to elicit the DNA changes were high and alcohol was directly injected into the animals, whereas in humans alcohol is orally absorbed and undergoes several types of metabolism that reduce maximum blood alcohol concentrations achieved. Further, the animal model was based on mice that had been genetically manipulated in that particular genes had been selectively ‘knocked out’ to make them unable to metabolize aldehyde or to repair DNA damage; while this was necessary to study the effects in a basic scientific experiment, it is in contrast to what would occur under non-manipulated conditions of alcohol consumption in humans
The damages shown in this experiment were to hematologic cells, and epidemiologic studies have generally not found an increase in the risk of hematologic cancers in humans to be associated with alcohol, especially from the moderate intake of alcohol (and many studies show instead a decrease in risk among drinkers). Thus, studies in humans have not provided support for these reported results from mice. Further, Forum members conclude that the polyphenols that are present in wine may play an important role in blocking a carcinogenic effect associated with alcohol intake.
Reference: Garaycoechea JI, Crossan GP, Langevin F, Mulderrig L, Louzada S, Yang F, Guilbaud G, Park N, Roerink S, Nik-Zainal S, Stratton MR, Patel1 KJ. Alcohol and endogenous aldehydes damage chromosomes and mature stem cells. Nature 2017;553:171-177. doi:10.1038/nature25154.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 210: Beer, wine, and spirits consumption and risk of gastric cancer – 8 January 2018
While heavy alcohol intake has been regularly found to increase the risk of upper aero-digestive tract (UADT) cancers (mouth, tongue, pharynx, larynx, etc.), results are less clear for gastric cancer. The present study is notable because it is based on a large number of subjects, uses appropriate analytic methods, and provides dose-dependent results according to type of beverage.
For total alcohol, the dose-response results in this meta-analysis show a curvilinear relation between alcohol intake and gastric cancer, with a minimal (4%) but significant increase per typical drink (12.5 g/alcohol). However, there were varying responses for different beverages. In beverage-specific analyses, for beer, a non-linear relation was found with a significant increase of 7%/drink (CI 1.01, 1.13); for liquor, there was a linear association, with RR=1.03 (CI 0.98, 109); and for wine, the RR was 0.99 (CI 0.93, 1.06).
While the authors show a figure of the dose-response curves for each beverage using a non-linear approach, they do not provide the specific values in a table or in the text; this makes it difficult to clearly determine threshold effects of beverages. The figures suggest that the risk associated with beer consumption shows a slight decrease for 1 to 2 drinks/day, then an increase; for spirits, no decrease with lighter intake is seen; for wine, the curve is continuously downward. The authors do state that “light, moderate, and wine drinking would not increase gastric cancer risk,” so it is presumed that significant increased risk was not noted for moderate drinking for any specific beverage when non-linear effects were evaluated. Thus, overall, it appears that this large meta-analysis shows no significant increases in risk for light to moderate consumption of an alcoholic beverage, but a slight increase in risk associated with greater intake of beer and spirits. For wine, no increase in the risk of gastric cancer was seen for any level of consumption.
In a number of sensitivity analyses, the authors found tendencies for a lower gastric cancer risk associated with alcohol for cohort versus case-control studies, for studies with larger numbers of subjects, for studies judged to be of higher quality, and for studies adjusting for confounding by SES & income; these types of studies would be expected to yield more precise estimates of effect. These results led the authors to state these sensitivity analyses “ . . . indicate that our results may be exaggerated to some degree, but it should be noted that the pooled risk estimates of high-quality studies yielded similar results to the original analysis.”
Overall, Forum members considered this to be a well-done analysis, and the data support an increase in gastric cancer risk for heavier drinking (of beer or spirits) but no significant effects for light or moderate drinking of any alcoholic beverage. Forum members considered that if the lack of increase in cancer risk from wine consumption seen in this analysis proves to be true, it might relate to the polyphenols in wine that block any adverse effects of alcohol on gastric cancer risk.
Reference: Wang P-L, Xiao F-T, Gong B-C, Liu F-N. Alcohol drinking and gastric cancer risk: a meta-analysis of observational studies. Oncotarget 2017;8:99013-99023.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 209: Does alcohol intake increase the risk of obesity? — 13 December 2017
The public, and scientists, have long been concerned about the relation between alcohol consumption and weight gain, as all alcoholic beverages contain calories. However, most epidemiologic studies do not find that light or moderate drinkers weigh more than their abstaining peers, and some even show lower weight among moderate drinkers than among abstainers. The reasons for this apparent effect are unclear.
The present study is important as it describes the effects on weight of changes in alcohol intake over repeated 4-year periods among a large cohort of health professionals, followed for 24 years. They found very slight increases in weight (mostly less than one-half pound over a four-year period) for subjects consuming alcoholic beverages; these were statistically significant for regular beer and liquor, but not for wine or light-beer. Overall, the largest increases in weight (still, only an increase of 0.6 pounds) were seen for subjects increasing their alcohol by an average of 2 or more drinks/day. For subjects decreasing their alcohol intake over the periods, there was a slight decrease in weight, still only about one-half pound or less.
The investigators conclude that any effects of drinking on weight are very minor, and probably of no clinical significance. While effects on weight gain were slightly lower among consumers of wine and light beer than for those consuming regular beer or spirits, the differences were not large. The study does not present data on the mechanisms of such associations.
Forum members considered this to be a very well-done analysis of repeatedly collected exposure and outcome data among health professionals over an extended period of time. Adjustments were made for known potential confounders associated with changes in weight and appropriate sensitivity analyses were done. While the paper indicates that calories from alcohol are metabolized similarly to those from other foods and do affect weight change, the changes associated with moderate alcohol intake appear to be very minor and would be expected to have very little effect on the development of obesity.
Reference: Downer MK, Bertoia ML, Mukamal KJ, Rimm EB, Stampfer MJ. Change in Alcohol Intake in Relation to Weight Change in a Cohort of US Men with 24 Years of Follow-Up. Obesity 2017;25:1988-1996. doi:10.1002/oby.21979
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 208: A statement on alcohol and cancer that ignores the net health effects of moderate drinking, such as increasing longevity of life — 16 November 2017
The present publication is an attempt by the American Society of Clinical Oncology to describe the relation between alcohol consumption and cancer, including the effects on the risk of developing cancer and effects among subjects currently being treated for cancer. It came to the conclusion that there is a need for the public to be warned about the use of alcohol because of its effects on cancer, and describes numerous approaches for decreasing alcohol use in the population.
Forum members considered this paper to markedly distort the associations between alcohol consumption, especially light drinking, and health outcomes. The authors were particularly remiss in not describing the net health effects of light to moderate consumption: longer longevity of life. Their long discussion of policy implications, and ways of decreasing alcohol use in the population, were unrelated to the data they presented, and failed to describe how complex and culturally specific such recommendations are. The authors describe many ways of decreasing alcohol consumption in the population, but do not provide any data about whether or not the measures they propose are successful.
While all Forum members agree that heavy alcohol consumption increases the risk of several cancers (information that oncologists should be aware of), light drinking has generally been associated only with a slight increase in breast cancer, but not with other types of cancer (especially when under-reporting of intake is considered). Further, factors such as dietary folate intake, patterns of drinking such as binge versus regular moderate drinking, and type of beverage generally consumed have been shown to modify even this relation. Also, regular light or moderate drinking has been consistently shown to decrease the risk of cardiovascular disease (the leading cause of death), diabetes, dementia, and even total mortality, associations largely ignored in this paper.
Our Forum considers that this publication from the American Society of Clinical Oncology misses an opportunity to provide, for oncologists and for the public, up-to-date and balanced information of the true relations of alcohol consumption to the risk of cancer and other health outcomes. They have especially ignored the effects of moderate drinking on the risk of total mortality.
Reference: LoConte NK, Brewster AM, Kaur JS, Merrill JK, Alberg AJ. Alcohol and Cancer: A Statement of the American Society of Clinical Oncology. J Clin Oncol 2017;35:pre-publication. DOI: https://doi.org/10.1200/JCO.2017. 76.1155
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 207: Effects on birth weight and risk of preterm birth of light-to-moderate drinking during pregnancy – 2 November 2017
There is no question that high levels of alcohol consumption during pregnancy can lead to severe adverse effects on the fetus, with the most serious condition known as fetal alcohol syndrome (FAS). Many studies have also related alcohol intake during pregnancy with premature birth, low birth weight, and the infant being small for gestational age (SGA). Data are not as clear on the effects just of occasional or light drinking, but most studies have not detected adverse effects.
The present paper, based on a pooled sample of almost 200,000 women from nine European cohorts, provides data indicating that premature birth, an infant being small for gestational age (SGA), or being of low birth weight do not appear to be associated with light-to-moderate intake (up to 6 drinks/week); these results are similar to those from many other recent studies. In this large study, mothers who consumed greater amounts of alcohol tended to have an increased risk of the infant being SGA or with low birth weight, but such a level of drinking had no effect on the risk of premature delivery. This cohort consisted almost exclusively of light drinkers; no data were available on other potentially harmful effects of excessive drinking.
An interesting additional finding was that the reported frequency of any alcohol consumption during pregnancy in the cohorts studied has decreased dramatically in recent decades (from approximately 50% of women studied prior to 2000, to 39% in 2000-2004, to 14% in 2005-2011). This suggests that most women are responding to guidelines recommending that a woman not drink during pregnancy.
Based on currently available information, the Forum considers that a recommendation to “avoid alcohol during pregnancy” is appropriate as part of drinking guidelines for the public. However, scientific data, including the present paper, do not suggest that women who may have an occasional drink or very light alcohol consumption during pregnancy should have undue concern about having a premature birth or a low-birth-weight infant.
Reference: Strandberg-Larsen K, Poulsen G, Bech BH, Chatzi L, Cordier S, et al. Association of light-to-moderate alcohol drinking in pregnancy with preterm birth and birth weight: elucidating bias by pooling data from nine European cohorts. Eur J Epidemiol 2017 pre-publication; DOI 10.1007/s10654-017-0323-2
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 206: Importance of considering cultural factors in determining effects on health of alcohol consumption – 3 October 2017
It has been clearly shown that presumably similar amounts of alcohol tend to have different health effects (both beneficial and adverse) in different cultures. Greater health benefits from moderate alcohol intake have been shown, for example, in southern European countries (where wine with meals is common) than in more northern European countries, where beer and spirits are more likely to be consumed and usually not with food. Some of these differences may relate to the beverage consumed, while others may relate especially to different patterns of consumption. Further, in certain cultures, intoxication after drinking is expected and even tends to not be condemned. In the typical Italian culture, however, it would not be socially acceptable for a guest at a family dinner to become overtly intoxicated, and such would probably be less often reported in an epidemiologic study even if it had occurred. Thus, similar rates of alcohol-use disorders would be ascertained differently in different countries.
We know that the net effect of alcohol consumption relates to the amount of alcohol, the type of beverage, the rapidity of consumption, whether drinking with or without food, and surely a number of genetic factors of the drinker. What we are often unsure about is what the cultural context of drinking is for an individual subject or subjects in a certain population: different cultures seem to help control, or not control, the risk of drinking excessively. As pointed out by the present paper, these factors complicate the comparison of results of epidemiologic studies from different cultures.
In planning and interpreting results of epidemiologic studies, investigators now realize that simply estimating the average alcohol consumption over a period of time, usually a week, is inadequate to quantify alcohol exposure. The pattern of consumption (especially whether with or without food and whether regularly or in binges) is especially important. And, as the present study points out, knowing about the cultural aspects of drinking for a specific population is also key to interpreting the results. How best to do this, so that studies in different countries can be compared, remains difficult.
Reference: Rehm J, Room R. The cultural aspect: How to measure and interpret epidemiological data on alcohol-use disorders across cultures. Nordic Studies on Alcohol and Drugs 2017;34:330–341. DOI: 10.1177/1455072517704795.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 205: A very large population-based study of the association of alcohol consumption with total and disease-specific mortality – 4 September 2017
The usual finding in longitudinal cohort studies has been that light-to-moderate consumers of alcohol tend to be at lower risk for total mortality and show greater longevity of life, even when other lifestyle/demographic factors known to affect longevity are adjusted for in the analysis. The present analysis is important as it presents data on the relation of alcohol intake to total mortality as well as to specific mortality from cardiovascular disease (CVD) and cancer for a very large number of subjects in the USA. It is based on data from more than 300,000 subjects, of whom almost 25,000 died during a follow-up period averaging 8.2 years. There was a very large number of lifetime abstainers which could serve as an appropriate reference group for their analyses. Further, by adjusting for a number of chronic diseases, and carrying out sensitivity analyses with a 2-year lag period for mortality, the investigators improved their ability to avoid having their results affected by “sick quitters.”
The authors conclude that their analysis shows that light and moderate drinkers have a lower risk of total mortality, as well as mortality from CVD, heart disease, and cerebrovascular disease. The protective effects of alcohol for such cardiovascular outcomes were not present for subjects who reported binge drinking or for those reporting what was defined as “heavy” drinking (>7 drinks/week for women and older men, 14 drinks/week for younger men). Interestingly, the mortality risk for light and moderate drinking was also significantly reduced for deaths attributed to cancer; Forum members thought that this may have possibly resulted from subjects with cancer who actually died from CVD having their deaths attributed to cancer. Subjects reporting heavy drinking and those with binge drinking showed increased risk of all-cause and cancer mortality, with no significant effect on CVD outcomes. The key results of the study are that there is a very clear J-shaped curve for the relation of alcohol to mortality, with lower total, cardiovascular, and even cancer mortality rates for light and moderate drinkers who do not binge drink. There was increased total mortality and cancer mortality for those classified as “heavy” drinkers.
Forum Members thought it unfortunate that beverage-specific data were not presented (as in many studies wine, and sometimes beer, drinkers have better outcomes than consumers of spirits), that subjects of all ages (≥ 18 years of age) were included in a single analysis (rather than also presenting results specifically for older subjects, when the outcome events studied usually occur), and especially that women and older men who consumed > 7 drinks/week, and younger men consuming >14 drinks/week were all combined into a “heavy” drinking category. It would have been preferable that the investigators also had a category for those consuming only slightly more than the recommended levels, who may well have had different outcomes than heavier drinkers.
Overall, Forum members considered this to be a well-done study providing additional data supporting a J-shaped curve for the association of alcohol consumption with mortality. Thus, data continue to indicate that light-to-moderate intake of alcoholic beverages without binge drinking reduces total mortality as well as death from CVD or cancer. The cumulative scientific data on this topic are well described in the accompanying Editorial Comment by de Gaetano and Constanzo in the same issue of the journal.
Reference: Xi B, Veeranki SP, Zhao M, Ma C, Yan Y, Mi J. Relationship of Alcohol Consumption to All-Cause, Cardiovascular, and Cancer-Related Mortality in U.S. Adults. J Am Coll Cardiol 2017;70:913–922
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 204: Moderate drinking improves the chances for healthy survival to age 85 – 21 August 2017
A number of studies have shown that the risk of cognitive impairment appears to be reduced among elderly subjects who consume moderate amounts of alcohol; most studies indicate that both light and moderate drinking are associated with a lower risk of dementia, but heavy drinking is often shown to be associated with higher cognitive risk for dementia and cognitive impairment. In some studies, a protective effect of light-to-moderate alcohol intake has been seen primarily among consumers of wine, or sometimes beer/wine. Further, almost all well-done cohort studies have shown that moderate drinkers tend to have longer lifespans.
The present study is based on a group of ageing subjects in California that had been observed closely for several decades; the average follow-up period for these particular analyses were about 14 years. Subjects in this cohort have had multiple assessments of cognitive ability and frailty. The authors conclude that their subjects who reported moderate alcohol consumption in the late 1980s were more likely than non-drinkers during follow up to survive to age 85 years of age, and also to be more likely to survive to age 85 cognitively intact (without evidence of dementia). Also, daily or near-daily drinkers had better health outcomes than those of non-drinkers or less-frequent drinkers.
The Forum considers this to be a well-done study; while it is not based on a large cohort, it provides new data by having extensive evaluation over time in a cohort of community-dwelling elderly subjects. The results support data from most other studies of survival and dementia among moderate drinkers, but adds specific information on survival to age 85 without cognitive impairment.
This study and the review of prior scientific data on this subject led Forum members to also raise a question about the typical guidelines for alcohol consumption for the elderly: generally less or no alcohol consumption is advised. Given that current scientific data show that the risks of the common disease outcomes of older subjects (e.g., coronary artery disease, ischemic stroke, osteoporosis, dementia, mortality) are lower among moderate drinkers than among non-drinkers, it may be time to reevaluate such restrictions that are based on age alone.
Reference: Richard EL, Kritz-Silverstein D, Laughlin GA, Fung TT, Barrett-Connor E, McEvoy LK. Alcohol Intake and Cognitively Healthy Longevity in Community-Dwelling Adults: The Rancho Bernardo Study. J Alzheimer’s Dis 2017;9:803–814. DOI 10.3233/JAD-161153
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 203: Moderate alcohol intake may reduce, not increase, the risk of falls in the elderly – 7 August 2017
Falls are common among the elderly, and markedly increase the subsequent risk of morbidity and mortality. There has been much written about the dangers of even light-to-moderate intake of alcohol among the elderly, with an increase in potential falls being one key reason cited. This may not be in the best interest of many elderly subjects; the demonstrated protection of light-to-moderate alcohol intake against many of the diseases of ageing (especially coronary heart disease, stroke, osteoporosis, dementia) could outweigh any dangers from falls if the latter risk is not great.
The present study examined the association between certain patterns of alcohol consumption, including the Mediterranean drinking pattern (MDP), and the risk of falls in more than 2,000 elderly subjects over 3.3 years; at the end of follow up, 21.4 % of subjects reported at least one fall in the previous year. The study found that up to moderate amounts of alcohol (defined as less than 40 grams of alcohol/day for men and less than 24 grams/day for women) did not increase the risk of falls, but actually resulted in a significant decrease of 20% or more in such risk. The risks for having multiple falls or those requiring medical care were also lower for moderate drinkers. The investigators report further that subjects with higher scores for a Mediterranean-type diet, that includes regular wine consumption, had similar or more impressive reduction in their risk of falls.
The specific reasons for such protection are not fully known, but a number of favorable effects on health of moderate drinking (e.g., less osteoporosis, less cardiovascular disease, less dementia, greater functional capacity, etc.) may play a role. While the investigators of this study were able to adjust for many factors known to be associated with falls, residual confounding is always a possibility to explain these results.
To summarize, while previous studies have often reported an increase in risk of falls for heavy drinkers, the present study supports results of many previous studies indicating that light-to-moderate alcohol intake does not increase the risk, and often is shown to decrease the risk of falls and fractures. In the present study, even with adjustments for most known lifestyle factors affecting risk, moderate drinking was associated with at least a 20% decrease in the risk of falls when compared with abstainers. This is a message that needs to be incorporated into drinking recommendations for the elderly.
Reference: Ortolá R, García-Esquinas E, Galán I, Guallar-Castillón P, López-García E, Banegas JR, Rodríguez-Artalejo F. Patterns of alcohol consumption and risk of falls in older adults: a prospective cohort study. Osteoporosis International 2017, on-line publication. DOI 10.1007/s00198-017-4157-2.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
==================================================================
Critique 202: Importance of folate intake for reducing breast cancer risk from alcohol consumption, especially for women with a positive family history of breast cancer – 17 July 2017
The strongest factor associated with the risk of a woman developing breast cancer appears to be a positive family history of such a diagnosis in a sibling or mother. Among environmental factors, almost all studies have shown that alcohol consumption relates to increased risk; a slight increase is often seen even among women who report only light drinking, e.g., an average of less than one drink per day. The present study evaluates how a positive family history of breast cancer in a first-degree relative and folate intake may modify the association between alcohol intake and breast cancer; the analysis is based on data from a large number of young women, aged 27-44 years at baseline, over a follow-up period of 20 years.
Forum members considered that this was a very well-done analysis from the large Nurses’ Health Study II, which followed young women for two decades. Alcohol consumption in total drinks/week was based on repeated assessments (but the pattern of drinking, binge versus regular drinking, was not evaluated). Repeated dietary questionnaires were used to estimate folate input. More than 2,800 incident invasive breast cancers were detected, essentially all being validated by a review of medical records.
The main results of this study were that without a positive family history of breast cancer, there was no significant increase in cancer risk for any level of alcohol intake. With a positive family history, however, there was a tendency for higher risk with increasing alcohol intake; this increase was not statistically significant for those with high folate, but a significant positive association (HR=1.82, 95% CI 1.06, 3.12; P-trend = 0.08) with cancer was seen for subjects with the highest level of alcohol intake plus low levels of folate.
Forum members conclude that the results from the present study should greatly relieve anxiety about breast cancer for women without a positive family history of breast cancer who choose to consume light-to-moderate amounts of alcohol. For women with a first-degree relative with breast cancer, the data indicate that if they maintain a high level of folate intake, it may attenuate an increase in risk associated with alcohol intake.
Reference: Kim HJ, Jung S, Eliassen AH, Chen WY, Willett WC, Cho E. Alcohol consumption and breast cancer risk by family history of breast cancer and folate intake in younger women. Am J Epidemiol 2017: pre-publication.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
==================================================================
Critique 201: The marked effect of lifestyle on mortality — 26 June 2017
The aim of the present study was to examine differences in the risk of mortality and in survival associated with a healthy lifestyle versus a less healthy lifestyle. The analyses were based on a total of more than 60,000 Swedish men and women who were followed in one of two studies; at baseline, the subjects were aged 45 to 83 years and were free of cancer and cardiovascular disease. The goal was to evaluate the effects of four “healthy” lifestyle factors: (1) nonsmoking; (2) physical activity at least 150 min/week; (3) alcohol consumption of 0–14 drinks/week; and (4) a healthy diet, with the latter defined as a modified Dietary Approaches to Stop Hypertension (DASH) Diet score above the median. Cox proportional hazards regression models and Laplace regression were used to estimate respectively hazard ratios of all-cause mortality and differences in survival time.
The authors report: “Compared with individuals with no or one healthy lifestyle factor, the multivariable hazard ratios of all-cause mortality for individuals with all four health behaviors were 0.47 (95% confidence interval [CI] 0.44-0.51) in men and 0.39 (95% CI 0.35-0.44) in women. This corresponded to a difference in survival time of 4.1 (95% CI 3.6-4.6) years in men and 4.9 (95% CI 4.3-5.6) years in women.”
Forum members considered this to be a well-done study on a large cohort with complete follow-up data on mortality. Notable weaknesses included the fact that never drinkers and consumers of 0 to 14 drinks/week were considered in one group (thus, including lifetime abstainers, ex-drinkers, and current moderate drinkers); these subjects were compared with consumers of >14 drinks/week. Thus potential differences between abstinence versus light/moderate consumption could not be determined. Further, there were incomplete data on the pattern of drinking, and no data on the type of beverage consumed were reported. Nevertheless, the reduction in mortality for subjects following a healthy lifestyle was impressive: a reduction by half, or more, in the risk of mortality and a 4- to 5-year longer lifespan.
Based on a number of previous studies that evaluated similar lifestyle factors and mortality, the results of this study were not unexpected. Still, they strongly support the remarkable effects on mortality and survival of these lifestyle factors. While not smoking was clearly the factor with the strongest effect on reducing mortality, having a healthy diet, exercising, and consuming light to moderate amounts of alcohol all make additional contributions. This is an important message in that even individuals who may be challenged by genetic or socioeconomic predispositions to earlier demise, adopting certain lifestyle habits can help them reach their greatest potential for a longer and healthier lifespan.
Reference: Larsson SC, Kaluza J, Wolk A. Combined impact of healthy lifestyle factors on lifespan: two prospective cohorts. J Int Med 2017. Pre-publication. Doi: 10.1111.joim.12637.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
Critique 200: Does Light Drinking Increase the Risk of Cancer? — 8 June 2017
The association between the consumption of alcohol and the risk of cancer has been of great interest for many decades. There are a number of types of cancer, especially those of the upper aero-digestive tract (such as mouth, tongue, pharynx, etc.) that are clearly increased among heavy drinkers, especially among subjects who are also heavy smokers. Cancer of the liver can be a result of alcoholic liver cirrhosis, related to long-term heavy drinking. Further, an increased risk for many other cancers have been shown for heavy drinkers, but generally not for light or moderate drinkers.
The risk of breast cancer in women, however, is usually found to be slightly higher in even light drinkers than it is among non-drinkers. This has been a common finding, although some studies suggest that the pattern of drinking, the estimated level of underreporting of alcohol intake, use of hormone replacement therapy, and level of folate intake may all affect this association. For colorectal cancer, some studies suggest an increase in risk even among light-to-moderate drinkers. This has led some to proclaim that no alcohol consumption is preferable for the prevention of cancer. Others suggest that it is important to consider not only cancer, but other diseases; for example, coronary heart disease, ischemic stroke, diabetes, and dementia (all of which are important causes of disability and death) occur less frequently among moderate drinkers than among non-drinkers. Further, the risk of total mortality is almost always found to be lower among light to moderate drinkers than among abstainers.
The present analysis was designed to help determine the association of light or moderate drinking with the risk of cancer. It consisted of a meta-analysis based on a total of 60 studies from 135 articles and included only cohort studies of high quality. The analysis focused on the association between very light (≤0.5 drink/day), light (≤1 drink/day), or moderate drinking (1-2 drinks/day) and the risk of cancer incidence and mortality.
The authors found that very-light drinking was not associated with the incidence of most cancers except for female breast cancer and male colorectal cancer, and was associated with a decreased incidence of both female and male lung cancer and both female and male thyroid cancer. Moderate drinking significantly increased the incidence of male colorectal cancer and female breast cancer, whereas it decreased the incidence of both female and male hematologic malignancy.
Forum members considered this to be a well-done meta-analysis, based on a large number of studies. The main weaknesses of the study related to the lack of ability of the authors to evaluate a number of known confounders: underreporting of alcohol intake, the pattern of drinking or the type of beverage consumed, socio-economic status, and folate intake or other dietary factors. Further, the authors did not describe the effects of alcohol consumption on total mortality.
The results of this study, obviously, support most previous epidemiologic evidence on the association between alcohol consumption and cancer. Larger amounts of alcohol are associated with increased risk of a number of cancers, and even light consumption is associated with the risk of breast cancer, and possibly colorectal cancer. However, given the inability to adjust for many confounders in this study, and lack of data on the net effects in terms of total mortality, it remains difficult for scientists to provide scientifically sound and balanced guidelines regarding the health consequences of alcohol consumption that are applicable to everyone in the population.
Reference: Choi Y-J, Myung S-K, Lee J-H. Light Alcohol Drinking and Risk of Cancer: A Meta-analysis of Cohort Studies. Cancer Research and Treatment 2017; pre-publication release.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=======================================================================
Critique 199: Potential mechanisms for the greater risk and fewer health advantages from alcohol consumption for subjects with low socio-economic status – 25 May 2017
The majority of epidemiologic studies have shown that both the positive and negative health effects of alcohol consumption are modified by the socio-economic status (SES) of individuals, with truly moderate drinkers who are from higher SES strata having better health outcomes and fewer adverse effects from alcohol than lower-SES subjects supposedly consuming similar amounts. One potential explanation for this has been that higher SES subjects (those with higher education, income, job status, etc.) are more likely to be regular moderate drinkers, more likely to be wine drinkers, and to drink primarily with meals, while lower SES subjects are more likely to binge drink (mainly beer or spirits), not with food, and may tend to under-report their alcohol intake. However, there are limited scientific data on the specific mechanisms by which such differences occur.
The authors of the present paper have used data on alcohol intake collected in the Scottish Health Surveys from more than 50,000 subjects to investigate whether the harmful effects of alcohol differ by socioeconomic status when accounting for a number of SES factors. They had very good measures of SES based on education, income, social class (professionals, skilled manual labor, unskilled labor, etc.), and a “measure of deprivation” of the geographic area of the subject (based on multiple measures of deprivation from government administrative data). Their health outcome measures were based on public records for deaths, admissions, and prescriptions; their primary outcome was alcohol-attributable admission or death. Their data show that, even without considering alcohol consumption, lower SES subjects were at much greater risk for poor health outcomes. And, while risks associated with increasing amounts of alcohol were present in all SES groups, they were much greater in the lower groups.
Forum members considered this to be a well-done study, but pointed out that there was limited information on the pattern of drinking and no data on the type of alcoholic beverage consumed or whether or not it was consumed with food. There was no dietary information or genetic information available, and little data on access to health care. While the study showed very marked differences in adverse health outcomes according to SES, the authors found that the factors they considered explained little of the health effects seen. They concluded: “Disadvantaged social groups have greater alcohol-attributable harms compared with individuals from advantaged areas for given levels of alcohol consumption, even after accounting for different drinking patterns, obesity, and smoking status at the individual level.”
Forum members agree that there may be many other lifestyle factors associated with poverty that scientists are unaware of, or unable to adequately control for, in their analyses. Differences by SES in the assessment of alcohol intake remains as a potential factor (especially given that higher SES subjects are usually found to consume alcohol regularly and moderately, less in binges, more often consuming wine with food, etc.). The authors of the present paper have evaluated a number of factors (including smoking status and obesity) as potential explanations for the poorer outcomes among lower SES subjects, and still found large differences in health effects despite adjusting for a number of such lifestyle factors. Thus, the specific reasons why lower SES subjects have worse health overall and poorer effects after alcohol consumption remain unclear.
Reference: Katikireddi SV, Whitley E, Lewsey J, Gray L, Leyland AH. Socioeconomic status as an effect modifier of alcohol consumption and harm: analysis of linked cohort data. Lancet Public Health 2017. Online publication May 10, 2017. http://dx.doi.org/10.1016/S2468-2667(17)30078-6
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================
Critique 198: A study of alcohol and cardiovascular disease based on “Big Data,” linked electronic medical records from the population — 24 April 2017
Essentially all observational cohort epidemiologic studies have shown a “J-shaped” curve for the association of moderate alcohol consumption with coronary heart disease and myocardial infarction, in that non-drinkers and heavy drinkers have higher risk than moderate drinkers. The present study presents a new approach for evaluating this relation by using electronic medical records for a very large number of patients (“big data”) in the UK to judge the relation between alcohol consumption and a variety of cardiovascular disease (CVD) outcomes. The study evaluated clinical data recorded by physicians from almost 2 million subjects, with about 115,000 CVD events recorded in public records. The exposures and outcomes came solely from the medical diagnoses given by individual physicians, and such diagnoses are known to often be inaccurate. For individual subjects, the exposure was based on codes for alcohol use or misuse in their medical records, and the cause of death was based on that recorded by the physician (which is not always consistent with diagnoses from autopsies or medical record reviews). Such problems would be expected to decrease the precision of the exposure and of outcome diagnoses.
Forum reviewers of this paper considered that the authors made a valiant effort in attempting to take into account the limiting factors of using big data for epidemiologic research. It is recognized that studies such as these cannot evaluate the pattern of drinking (regular versus binge) and the investigators were unable to evaluate different effects according to the type of beverage consumed (beer, wine, or spirits). It would be expected that both of these factors may have affected their results. Nevertheless, their conclusions strongly support the extensive observational data from cohort studies over many decades that have shown a higher risk among abstainers (versus moderate drinkers) for many CVD outcomes. In the present study, non-drinkers had significantly higher risk for unstable angina, myocardial infarction (MI), unheralded coronary death, heart failure, ischemic stroke, peripheral arterial disease, and abdominal aortic aneurysm. For most of these outcomes, heavy drinkers tended to have an increased risk (a J-shaped curve), but the risk for myocardial infarction and for stable angina remained decreased even for the heavy drinking category. For other manifestations of CVD, especially those related to cerebral artery disease (other than ischemic stroke), there was less of a clear pattern relating alcohol to disease. For their aggregate, overall outcome based on all manifestations of CVD, their analyses add further support for a J-shaped curve between alcohol intake and CVD.
Reference: Bell S, Daskalopoulou M, Rapsomaniki E, George J, Britton A, Bobak M, Casas JP, Dale CE, Denaxas S, Shah AD, Hemingway H. Association between clinically recorded alcohol consumption and initial presentation of 12 cardiovascular diseases: population based cohort study using linked health records. BMJ 2017;356:j909. http://dx.doi.org/10.1136/bmj.j909
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================
Critique 197: Alcohol consumption and the risk of developing dementia – 13 April 2017
A number of epidemiologic studies have found that light-to-moderate alcohol intake is associated with a lower risk of developing dementia and/or cognitive decline, while excessive drinking may increase the risk. The authors of the present paper carried out a meta-analysis of the current scientific literature that was based on data from 11 studies with 4,586 cases of all-cause dementia diagnosed among more than 70,000 subjects and two additional analyses of studies of approximately 50,000 subjects each for evaluating the association of alcohol intake with the diagnosis of Alzheimer’s disease or vascular dementia. Seven studies provided results according to type of alcoholic beverage consumed, while two provided results according to APOE 4 levels.
The conclusions of the authors are that, considering all sources of alcohol, light-to-moderate alcohol consumption was associated with a lower risk of all forms of dementia; the risk was reduced for up to 12.5 g/day (about one typical drink) and increased for consumers of more than 38 g/day (about 3 to 4 typical drinks). However, beverage-specific analyses indicated that the effect was only for wine, and not for consumption of beer or spirits. For moderate consumers of wine, the risk of dementia was reduced by 40% or more in comparison with that of non-drinkers. Little effect was noted among drinkers of spirits, and heavy beer drinkers appeared to have an increased risk of dementia. The presence or absence of APOE 4 did not appear to modify the effects.
Forum reviewers considered this to be a very well-done meta-analysis of the current literature on the topic. It was based only on prospective epidemiologic studies of very good quality, and sub-analyses evaluated the separate effects of each type of alcoholic beverage. While the authors were unable to include the pattern of drinking (binge versus regular moderate) in their analyses, and could not test for previous alcohol consumption among current non-drinkers, Forum members agreed with the primary findings of a J-shaped curve between alcohol consumption and all types of dementia (including vascular dementia and Alzheimer’s disease).
Most of this Forum critique deals with potential mechanisms by which wine consumption may reduce the risk of dementia and/or cognitive decline. In addition to the effects of both alcohol and polyphenols in wine on decreasing atherosclerosis and having beneficial effects on hematological factors (affecting cerebral as well as coronary arteries), there may also be anti-inflammatory effects and direct effects on brain structures that play a role. Given that the beneficial effects were primarily among wine consumers, this suggests that the polyphenols and other non-alcohol substances in wine (perhaps in interaction with alcohol) may be more important than the alcohol itself in reducing the risk of dementia.
The mechanistic studies described in the paper and in this critique provide considerable support for the epidemiologic findings of less dementia and cognitive decline among moderate drinkers. Forum member agree with the authors of this paper that light-to-moderate wine consumption may help lower the risk of dementia, an increasingly important condition in the world’s rapidly ageing populations.
Reference: Xu W, Wang H, Wan Y, Tan C, Li J, Tan L, Yu JT. Alcohol consumption and dementia risk: a dose-response meta-analysis of prospective studies. Eur J Epidemiol 2017;32:31-42. doi: 10.1007/s10654-017-0225-3. Epub 2017.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================
Critique 196: Adverse health effects of binge drinking on cardiovascular disease — 2 February 2017
This review paper on the effects of binge drinking on the risk of cardiovascular disease (CVD) provides considerable information on a topic of importance to public health. It clearly indicates that subjects who binge drink, however defined, tend to be at increased risk for hypertension, myocardial infarction, stroke, and cardiac arrhythmias. These adverse health outcomes are in addition to the well-known effects of binge drinking on drunkenness and many adverse health effects, both acute and chronic, as well as risk from violence and accidents to the drinker and to others.
While the members of the Forum applaud the efforts of the authors to present data on this relation, this paper failed to include many important previous research reports on the topic. Forum member Ian Puddey and others have prepared an extensive summary of many of the key research papers not addressed by the authors of this paper; their remarks are included in the full Forum critique. It describes how many factors, such as not only the amount but the rate at which alcohol is consumed, the type of beverage, whether or not food is being consumed, the prior drinking habits of the subjects, and many other factors can influence the effects of alcoholic beverages on health.
The Forum members conclude that a “comprehensive review” of binge drinking and other drinking patterns of alcohol in relation to the risk of CVD should include all of the available scientific data on the topic to be most useful. Taking into consideration the additional research results described in this critique provides a much better overview of the effects of binge drinking on CVD. The bottom line is that episodic heavy drinking, or binge drinking, has adverse influences on many health outcomes, including the risk of CVD.
Reference: Piano MR, Mazzuco A, Kang M, Phillips SA. Cardiovascular Consequences of Binge Drinking: An Integrative Review with Implications for Advocacy, Policy, and Research. Alcoholism: Clinical and Experimental Research 2017; Pre-publication. doi: 10.1111/acer.13329
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=========================================================================
Critique 195: How much of the “health benefits” of alcohol relate to higher socio-economic status of drinkers? — 19 December 2016
It has long been recognized from epidemiologic studies that both the positive and negative health effects of alcohol consumption are modified by the socio-economic status (SES) of individuals. Higher SES subjects (higher education, income, job status, etc.) are more likely to be regular moderate drinkers, while lower SES subjects are more likely to binge drink and under-report their alcohol intake. Truly moderate drinkers tend to have better health outcomes and fewer adverse effects from alcohol, and consistently show lower total mortality risks than non-drinkers or heavy drinkers.
The present study, from the New Zealand Longitudinal Study of Ageing, used data from the second examination of the cohort to do a cross-sectional analysis judging the relation of alcohol consumption to “health”. When controlling for age, income, and education (the latter two as measures of SES), they found a significant “J-shaped” association between reported alcohol intake and self-reported “physical health”. However, the authors state that they then used another measure of SES, the Living Standard Index-Short Forum (ELSI-SF), and found that the reported alcohol intake of subjects correlated with their measure of physical health almost exactly the same as with the results of the ELSI-SF. They conclude that there are no health benefits of moderate drinking, only that people with higher SES are more likely to drink moderately.
Forum members considered it unfortunate that the assessment of the exposure (alcohol intake) used in this study was based only on self-reported average intake and did not include data on the pattern of drinking (binge versus regular moderate intake, etc.). Further, their outcome was based only on a self-reported questionnaire of “physical health,” and did include any hard data; an overall index based on assessments of functional status, biomarkers of and the occurrence of disease, and mortality would be preferable when judging “health benefits” of alcohol. The Forum considered that the authors used inadequate indices of both the exposure to alcohol and their assessment of “health” (based on a questionnaire) to reach a conclusion that moderate drinking does not have any beneficial effects on health. This was done ignoring the massive amount of not only observational data but results from extensive experimental studies over more than four decades. Such research has found that moderate drinking not only has beneficial effects on assessments of physical health and disease occurrence, but results in significantly lower total mortality when moderate drinkers are compared with abstainers.
Regardless, given that this study, as have almost all epidemiologic studies, has shown the importance of SES on health outcomes, a key challenge to scientists is to seek to determine the mechanisms by which these differences occur. One potentially important factor is that the differing health outcomes relate to errors in judging the exposure, i.e., inadequate assessments of alcohol: not evaluating for binge drinking versus regular intake, consuming alcohol with or without food, type of beverage consumed, under-reporting of intake, etc. Also, much broader definitions of “health” are needed (rather than the results of a single self-administered questionnaire) that include the effects on functional status, disease states, and mortality. And, it is important that other lifestyle factors (smoking, drug use, etc.) that affect health be properly evaluated as determinants of health. Only with such data will we be able to fully judge the overall effects of alcohol consumption on health outcomes.
Reference: Towers A, Philipp M, Dulin P, Allen J. The “Health Benefits” of Moderate Drinking in Older Adults may be Better Explained by Socioeconomic Status. Pre-publication: J Gerontol B Psychol Sci Soc Sci 2016. doi:10.1093/geronb/gbw152
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 194: Long-term alcohol use and mortality among Swedish women – 22 November 2016
In a follow-up analysis of almost 50,000 young women, aged 30-49 at baseline, in the Swedish Women’s Lifestyle and Health cohort, the authors used self-reported information on alcohol consumption on two occasions, 12 years apart, to estimate the effects of alcohol on overall and cause-specific mortality. There were 2,100 deaths during follow up. Effects of alcohol on the two occasions, and changes between the two assessments among 33,000 women with available data, were related to mortality, as assessed from virtually complete national records.
Using “light” drinkers (0.1 – 1.49 grams of alcohol/day) as the referent group, the authors report an inverse association between greater amounts of alcohol consumption and mortality from cardiovascular disease. They report increased risk of cardiovascular and total mortality for abstainers. Despite the large number of total subjects, the authors report results separately for relatively narrow ranges of alcohol intake (none, 0.1-1.49, 1.5-4.9, 5-9.9, 10-14.9, 15+ g/day), which makes the numbers of subjects in many groups quite small. Given that the total mortality risks for most groups of drinkers were similar, it would have been interesting to see the effects of alcohol consumption (versus no consumption) using a broader definition of “moderate” drinking.
Forum members in general thought that this was a well-done study, using an excellent source of national records available in Sweden for determining mortality. They had concerns that the under-reporting of alcohol intake was not addressed; there is a high probability that some of the supposedly “light” drinkers may have actually consumed more alcohol, which would tend to decrease any differences between the referent group and the next groups of drinkers. This could help explain why, despite the strikingly lower risk ratios for cardiovascular disease for all drinkers when compared with the referent group, the inverse relation of alcohol was not statistically significant for any single group considered alone.
The Forum was also concerned that while the investigators had data on binge drinking and whether or not alcohol was usually consumed with meals, they chose not to include these data in their analyses. Given that drinking pattern plays a large role in determining favorable or unfavorable health effects of alcohol, the inclusion of such information may have better delineated the true effects of alcohol. Also, the authors “chose not to separately study the effects of different alcohol beverages;” reporting effects separately for beer, wine, and spirits could have provided key data on the effects of alcohol consumption.
The attempt of the authors to judge the effects of changes in alcohol intake during the study is laudable. Importantly, data on the reason that a woman may decide to increase or decrease her intake is not known; if due to the development of a serious disease, it may be the disease and not the change in alcohol intake that relates to subsequent mortality. However, given the inherent problems in assessing change, the results of this study are consistent with other studies that have suggested an increase in mortality risk for moderate drinkers who stop their alcohol consumption.
Reference: Licaj I, Sandin S, Skeie G, Adami H-O, Roswall N, Weiderpass E. Alcohol consumption over time and mortality in the Swedish Women’s Lifestyle and Health cohort. BMJ Open 2016;6:e012862. doi:10.1136/ bmjopen-2016-012862
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 193: The association of reported alcohol intake with the risk of subarachnoid hemorrhage: A meta-analysis – 1 November 2016
Data from epidemiologic studies are quite consistent for the relation of alcohol consumption with the different types of stroke: for ischemic stroke, an inverse association with moderate drinking and a possible increase with heavy drinking (a “j-shaped curve”); for hemorrhagic stroke, a direct positive association, although some studies suggest that there may be a threshold level for an increase in risk. Data are mixed on a possible association between the most uncommon type of stroke, subarachnoid hemorrhage (SAH). The present paper presents results of a meta-analysis relating reported intake of alcohol with subsequent risk of SAH. It was based on 14 observational studies reporting data on 483,553 individuals and 2,556 patients.
Forum members agree that this study suggests that alcohol intake, especially heavier drinking, increases the risk of SAH, although there was considerable heterogeneity among studies from different parts of the world, there were no countries from the Mediterranean area included, and there was no accounting for pattern of drinking (binge versus moderate regular) or type of beverage, all of which may affect risk.
The authors concluded that there was no relation between light (<15 g/day) or moderate alcohol consumption (15‑30 g/day) compared with abstaining individuals; this was based on statistically insignificant increases in RR of 1.27 (95% CI: 0.95, 1.68) and 1.33 (95% CI: 0.84, 2.09) for these two groups, respectively. However, Forum members suggest that there could be a slight increase in risk even for these two groups. For heavier drinkers (> 30 g/day, about 2 ½ to 3 typical drinks per day), the data indicate an increase in risk: RR=1.78 (95% CI: 1.46, 2.17).
It should be noted that the overall risk of total stroke is decreased from moderate drinking, as the most common type of stroke is ischemic, and moderate drinking has consistently been shown to lower such risk; this is especially related to lowering the risk of atherosclerotic or embolic clots. However, while rare, SAH is often a devastating disease, and the risk may be increased from alcohol consumption through its effects on decreasing coagulation.
Reference: Yao X, Zhang K, Bian J, Chen G. Alcohol consumption and risk of subarachnoid hemorrhage: A meta-analysis of 14 observational studies. Biomedical Reports 2016;5:428-436.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=========================================================================
Critique 192: The association of alcohol consumption with the risk of prostate cancer –- 12 September 2016
Scientific data are mixed on the association of alcohol consumption with the risk of prostate cancer. In the present paper, the authors have used data from 11, 372 subjects in the Older Finnish Twin Cohort who provided data on alcohol intake on two occasions. They were followed for the development of prostate cancer from 1981 to 2012, during which 601 incident cases of prostate cancer and 110 deaths from prostate cancer occurred. The authors relate reported average alcohol intake, and whether or not the subject reported binge drinking, to the risk of prostate cancer and prostate cancer-specific death. They also evaluated the risks of prostate cancer among alcohol-discordant twins. The authors used current abstainers and ex-drinkers as the referent group in their main analyses, but did sensitivity analyses using never drinkers as an alternative referent group.
The type of beverage consumed was not known, so whether or not wine or beer consumption may have a different relation with prostate cancer than spirits intake cannot be determined. However, overall the data indicated a higher risk of prostate cancer from heavy intake and binge drinking, but also a high risk among abstainers. The number of discordant twins (for alcohol consumption) was too small for definitive results in terms of the risk of prostate cancer among subjects with the same or a similar genetic background , but the lowest risk was among light drinkers who did not binge drink. Even among this subset of the population, abstainers had higher risk than light drinkers.
Thus, the results of this well-done study suggest that there may be a J-shaped relation between alcohol consumption and prostate cancer risk. Light drinkers appear to have the most favorable results for both incident prostate cancer and prostate cancer-specific mortality. The risk for subjects reporting heavy drinking and binge drinking was higher for both incidence and mortality than the risk of light drinkers; for unexplained reasons, abstainers also tended to have higher risk of prostate cancer and mortality.
Reference: Dickerman BA, Markt SC, Koskenvuo M, Pukkala E, Muccil LA, Kaprio J. Alcohol intake, drinking patterns, and prostate cancer risk and mortality: a 30-year prospective cohort study of Finnish twins. Cancer Causes Control 2016;27:1049–1058. DOI 10.1007/s10552-016-0778-6
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 191: A new study on the mechanisms of alcohol’s effects on health and disease – 25 August 2016
While observational epidemiologic studies for many decades have consistently shown that moderate drinkers have a lower risk of cardiovascular diseases than do non-drinkers or heavy drinkers, the specific metabolic effects of alcohol have been little studied. In the present analysis, among almost 10,000 young adults from three population-based cohorts in Finland, associations of alcohol intake with 86 metabolic measures were assessed. Circulating lipids, fatty acids and metabolites were quantified by high-throughput nuclear magnetic resonance metabolomics and biochemical assays. The investigators found that alcohol consumption was associated with a complex metabolic signature, including aberrations in multiple biomarkers for reduced as well as elevated cardiometabolic risk; many factors showed different associations according to the estimated amount of alcohol consumed.
Among key associations found for greater alcohol intake were increases in HDL-cholesterol and its subclasses, decreases in LDL size, an increase in monounsaturated fatty acids and a decrease in omega-6 fatty acids, and lower concentrations of glutamine and citrate. For unexplained reasons, the changes in fatty acids from alcohol in this study were similar to those occurring following the administration of canola oil in other research. Some Forum reviewers pointed out that the analyses were not theory driven, and should only be used to generate hypotheses that would need to be tested in future experiments. As stated by one reviewer, the major contribution from this paper could be that it ignites the interest for experimental studies and provides new variables to be evaluated in prospective studies. In any case, the findings of this study provide valuable clues to the biologic effects on health, both favorable and adverse, related to alcohol consumption.
While not discussed by the authors, Forum members considered that the results of this paper might also be useful in providing a new approach for judging the level of alcohol intake of individuals in epidemiologic studies. At present, alcohol intake is judged almost exclusively from self-reports by subjects. Previous attempts designed to identify subjects more likely to be under-reporting their intake have shown that they may sharpen relations between estimated intake and health outcomes. Forum members believe that approaches that identify sources of bias for self-reported data, whether based on genetic, behavioral, physiological, or other information (preferably on all), might allow epidemiologists to have more precise and accurate information on alcohol intake when relating such to disease outcomes. A new approach for providing more accurate and unbiased estimates of alcohol intake is suggested by this excellent analysis.
Reference: Würtz P, Cook S, Wang Q, Tiainen M, Tynkkynen T, Kangas AJ, et al. Metabolic profiling of alcohol consumption in 9778 young adults. Int J Epidemiol 2016; pre-publication: doi: 0.1093/ije/dyw175
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 190: Alcohol intake during middle age and later atherosclerosis – 11 August 2016
Carotid artery disease can be estimated by ultrasound from the thickness of the wall of the arteries (recorded as carotid artery intima/medial thickness, cIMT) and by evidence of atherosclerotic plaques within the carotid arteries. The association between alcohol intake and such lesions is unclear, as some studies show a positive association with cIMT and/or plaques while others show no association. Given that carotid disease relates to the subsequent risk of coronary artery disease, there is increasing use of carotid ultrasound measurements to help determine long-term risk.
The present large study from the UK provides valuable information by reporting the cross-sectional relation between alcohol consumption and cIMT as well as how the drinking pattern over 20 years in middle age may relate to cIMT later in life. While heavy alcohol intake was found to increase later cIMT measures, no clear differences were noted between subjects reporting abstinence and those reporting moderate drinking in middle age.
Forum reviewers considered this to be a well-done study. There were some concerns that only total average alcohol intake was considered, as there were no data on the type of beverage consumed, the pattern of drinking (binge versus regular moderate), whether the alcohol was consumed with food, etc., and there was an absence of data on diet, physical activity, adiposity, and other factors related to atherosclerosis. Further, only the thickness of the carotid artery was evaluated, and not the presence or absence of atherosclerotic plaques on the ultrasound readings.
Overall, current scientific data provide strong evidence that moderate alcohol consumption lowers the risk of most manifestations of cardiovascular disease; it appears to work through a combination of effects on lipids, inflammation, coagulation, fibrinolysis, glucose metabolism, and other paths. Further, heavy drinking is known to increase blood pressure, and is an important factor for developing hypertension (and a strong determinant of cIMT). The failure of the present study to find a significant association between moderate alcohol intake and later carotid thickness supports what has been shown in some, but not all, previous studies.
If indeed chronic alcohol use has little effect on atherosclerosis (using images from the carotids as an index of atherosclerosis in the coronary arteries and elsewhere in the body), it may indicate that the mechanisms for the protective effect of moderate alcohol consumption on cardiovascular disease are not so much related to preventing atherogenesis, but due primarily to the effects on coagulopathy. And it is known that clot formation within the arterial wall is often the precipitating event for an acute myocardial infarction or other cardiovascular event.
Reference: Britton A, Hardy R, Kuhf D, Deanfield J, Charakida M, Bell S. Twenty-year trajectories of alcohol consumption during midlife and atherosclerotic thickening in early old age: findings from two British population cohort studies. BMC Medicine 2016l;14:111. DOI 10.1186/s12916-016-0656-9.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 189: Importance of drinking pattern on the effects of wine on health — 26 July 2016
A review article appearing in Food & Function, a publication of the Royal Society of Chemistry in the United Kingdom, presents a summary of evidence-based scientific data relating the moderate consumption of wine and other alcoholic beverages to health. Forum members considered the paper to be a well-thought-out appraisal of the effects that the pattern of consumption (e.g., the type of beverage, regular versus binge drinking, consumption with meals, etc.) affects its risks and benefits. (It is recognized that some of the authors of this publication work primarily with wine, but the review article covers key behaviors that affect the relation of the consumption of all types of alcohol to health.)
The authors describe how the polyphenols and other non-alcoholic components of wine provide anti-oxidants and decrease post-prandial oxidative stress. These phenols can also scavenge free radicals in the mouth and throughout the gastro-intestinal tract, preventing lipid peroxidation as well as the absorption of cytotoxic lipid peroxidation products. Wine also favorably affects urate levels; thus, the antioxidant activity is apparently influenced by two separate mechanisms: wine-derived phenolic compounds and plasma urate. A further important biological property of wine is its potent antimicrobial activity that tends to decrease adverse effects of food-borne and oral pathogens.
The article summarizes the key differences in health effects when alcohol (especially wine) is consumed moderately, with food, and on a regular basis rather than in binges. These differences emphasize why evaluating only the total amount of alcohol consumed, and not how it is consumed, is inadequate when evaluating its effects on health and disease. Further, the authors emphasize how all medical and scientific information concerning the effects of wine and alcohol consumption on human health should be evidence-based and communicated in a competent, credible and unbiased manner.
Reference: Boban M, Stockley C, Teissedre P-L, Restani P, Fradera U, Stein-Hammer C, Ruf J-C. Drinking pattern of wine and effects on human health: why should we drink moderately and with meals? Food Funct 2016;7:2937–2942. DOI:10.1039/c6fo00218h
Note on potential conflict of interest: While several of the authors of this paper are members of our Forum, they have had no input into the review of the article.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 188: Alcohol-attributable cancer in New Zealand . . . 28 June 2016
Previous scientific research has shown that heavy alcohol consumption is a major risk factor for upper aero-digestive cancers, and even light drinking increases slightly the risk of breast cancer in women. The present study is based on a very small number of cases of cancer in New Zealand, tabulated separately for Māori and non-Māori subjects, and applies estimates of alcohol effects from other population-based studies. Besides having so few cases, the investigators had no individual data (on the pattern of alcohol consumption, type of beverage, smoking or other lifestyle habits, socio-economic status, etc.) on subjects who did, or did not, develop these cancers. It is not even known whether or not the specific subjects who developed these cancers consumed alcohol.
It has repeatedly been emphasized that disease-specific death rates must be interpreted in light of the effects of the exposure (in this case, alcohol consumption) on other causes of death as well, especially on total mortality risk. The large majority of studies have shown that moderate drinking clearly reduces the risk of most cardiovascular diseases, diabetes, and other of the diseases of ageing, as well as the risk of total mortality. However, the estimated effects of alcohol on total mortality are not included in this paper.
The very long Discussion in this paper is primarily a treatise on how the public must be told of the dangers of cancer from any alcohol consumption; it focuses on health policy recommendations and very little on the limitations of the data and the study. The authors end up making very broad recommendations based on very small numbers of subjects. Limitations to this study suggest that it adds little to our current understanding of the relation of alcohol consumption to the risk of cancer and other diseases.
Reference: Connor J, Kydd R, Maclennan B, Shield K, Rehm J. Alcohol-attributable cancer deaths under 80 years of age in New Zealand. Drug and Alcohol Review 2016; pre-publication. DOI: 10.1111/dar.12443
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 187: Alcohol and squamous cell carcinoma of the skin — 14 June 2016
Skin cancers, whether melanoma, basal cell, or squamous cell, are all increased by ultra-violet rays of the sun, and such cancers are much more common in areas of the world with more sun exposure. Further, the risk of such cancers is higher among individuals reporting excessive tanning (either from the sun or from tanning salons). The present study was undertaken to judge the relation between alcohol consumption and the risk of cutaneous squamous cell carcinoma (cSCC), an association that is unclear from earlier research. Determining the relation between alcohol and skin cancer is made difficult by the fact that excessive sun exposure has been shown to be greater among consumers of alcohol than among abstainers, thus the potential for confounding.
In the present analyses, combined data from three cohorts of subjects in the US, who had repeated assessments of alcohol intake over many years, were evaluated tor the relation of alcohol to the development of verified cSCC. Subjects included women in two cohorts of the Nurses’ Health Study and men in the Health Professionals’ Follow-up Study. Among subjects providing a total of more than 4 million person-years of follow up, 2,938 cases of cSCC were identified.
The results varied somewhat among the different cohorts, but in the meta-analysis of the three studies using continuous measures of alcohol, there was an increase in risk of cSCC with alcohol intake. Among women, there was a steep increase in risk of cancer for low levels of intake (up to 5 grams of alcohol/day, slightly less than ½ of a typical drink), then a gradual increase in risk thereafter, whereas among men there was more of a gradual increase in risk with larger reported alcohol intake.
Overall, the authors report an increase in risk per typical drink per day of 22% for invasive cSCC and 14% for in situ cSCC. In beverage-specific analyses, white wine consumption of >/= 5 times/week was associated with an increased risk of cSCC (RR 1.31, 95% confidence interval: 1.09-1.59), but an increased risk of cSCC was not seen for other alcoholic beverages. The population-attributable risk associated with alcohol intake of ≥ 20 grams/day (about 1 ½ typical drinks) was 3% of cSCCs.
Forum members considered that the analyses were well done, and the results of the study are consistent with increases in risk associated with alcohol consumption for other types of skin cancer. Given that sun exposure is by far the primary risk factor for skin cancer, and consumers of alcohol tend to have greater number of sunburns (also shown in this study), it is always difficult to determine if residual confounding by sun exposure is playing a role. The authors of this paper attempted to adjust for sun exposure by including in their analyses the typical exposure values in the area of the world where the subjects resided, by recording the frequency that subjects reported 5 or more severe sunburns, and several other measures. As expected, there were reductions in the estimated RR for invasive cSCC when going from age-adjusted RR (1.34) to multivariable-adjusted estimates (1.22) of risk. However, the magnitude of decrease in risk estimates when only those adjustments for sun-exposure were added to the equation cannot be determined from the data presented.
Forum reviewers consider that these analyses support results from many previous studies and indicate that consumers of alcohol have a greater risk than non-drinkers of all types of skin cancer. Attempts to judge how much of this association may be due to residual confounding related to sun exposure are less than conclusive. Various hypotheses have been raised for possible interactions between sun exposure and alcohol, but currently there are no experimental data to test these theories. While the authors conclude that “physicians may consider counseling their patients about the association between alcohol consumption and risk for cSCC,” it might be more advantageous for physicians to focus more on the much greater protection against this disease that would occur if they were able to limit their patient’s exposure to ultra-violet radiation.
Reference: Siiskonen S, Han J, Li T, Cho E, Nijsten T, Qureshi A, Alcohol intake is associated with increased risk of squamous cell carcinoma of the skin: three US prospective cohort studies. Nutrition and Cancer 2016;68:545-553.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 186: Changes in alcohol and effects on risk of breast cancer and heart disease — 19 May 2016
This large study from Denmark was designed to test the hypothesis that women who increase their alcohol intake over a five year period have a higher risk of breast cancer and a lower risk of coronary heart disease (CHD) compared with women who exhibit a stable alcohol intake. It consisted of more than 20.000 postmenopausal women who had two assessments of alcohol intake, about 5 years apart; changes during that period were related to their subsequent risk of developing breast cancer or CHD, or dying, during the subsequent follow-up period that averaged 8 years.
For the risk of breast cancer, the baseline alcohol consumption reported by the women showed that higher alcohol intake was associated with a greater risk of developing breast cancer during follow up, but a lower risk of developing CHD and for total mortality. For relating changes in alcohol intake in the 5 years between the two alcohol assessments, those who increased their reported alcohol intake showed an increased risk of subsequent breast cancer, while those who decreased their intake also had a tendency for greater breast cancer. In terms of CHD and total mortality, the data were consistent with an increase in consumption lowering risk, while there was a tendency for a decrease in consumption to increase risk. Hence, the directionality for risk from changes in intake reflected the risks associated with baseline risk, and the authors conclude that their results “ . . .support the hypotheses that alcohol intake is associated with increased risk of breast cancer and decreased risk of coronary heart disease.”
Forum reviewers considered this to be a very well-done study. They, and the authors, appreciated the innate difficulty in separating effects on health of usual alcohol intake over time and changes over a limited period of time. Reviewers were also concerned by these problems, suggesting that some of the reported changes in alcohol consumption in this study may have just reflected individuals replying differently to questions regarding their drinking at different points of time. Further, the reason why some women may have actually increased or decreased their intake are not known.
Nevertheless, Forum members applaud the attempt of the authors to judge if changes in alcohol intake relate to cancer, CHD, and total mortality. This is a difficult task given that baseline and life-time alcohol consumption clearly relate to these outcomes. Further, data on the pattern of drinking (regular versus binge), any estimate of underreporting of alcohol, the type of beverage consumed and, as stated by the authors, certain known risk factors of breast cancer, were not available to be included in their analyses. Thus while the results of this study add important information on the relation of alcohol to disease, there remain questions about the specific relevance of changes in intake for such outcomes.
Reference: Dam MK, Hvidtfeldt UA, Tjønneland A, Overvad K, Grønbæk M, Tolstrup JS. Five year change in alcohol intake and risk of breast cancer and coronary heart disease among postmenopausal women: prospective cohort study. BMJ 2016;353:i2314. http://dx.doi.org/10.1136/bmj.i2314
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 185: An innovative assessment of alcohol consumption and the risk of atrial fibrillation – 28 April 2016
A study from Denmark has been carried out to test the hypothesis that alcohol consumption, both observational (self-reported) and estimated by genetic instruments, is associated with the risk of atrial fibrillation (AF) and to determine whether people with high cardiovascular risk are more sensitive towards alcohol than people with low risk. It was based on a large cohort of subjects (more than 88,000) with a mean follow-up period of 6.1 years; there were almost 3,500 cases of AF diagnosed from hospital records during follow up. Unfortunately, the authors did not have data to identify binge drinkers, which tend to show greater adverse cardiovascular events than regular moderate drinkers whose weekly intake may be the same.
The main results of the study were that men consuming more than 14 drinks/week, especially those consuming more than 28 drinks/week, had an increase in risk of AF, but no significant increase in risk was seen for any level of alcohol intake among women. When genotypes affecting alcohol metabolism (AHD1B, ADH1C) were studied in a Mendelian randomization analysis, the authors state that they “found no evidence to support causality of the observational findings.”
Forum reviewers of this article considered it to be a well-done study with appropriate analyses. Its results reflect the findings of most previous prospective studies and meta-analyses of little effect of light drinking on AF, but an increase in risk for heavier drinkers. The study also showed that the effects of alcohol consumption on the risk of AF were not different between subjects who had cardiovascular disease or were at high-risk of cardiovascular disease than for other subjects.
While Mendelian randomization using genetic factors affecting alcohol metabolism has been touted as an unbiased approach for judging causal health effects of alcohol, there are questions about the adequacy of such instruments for judging effects. In the present study, their use did not suggest that the relations shown by the self-report of alcohol by subjects necessarily indicated a causal association of alcohol with AF.
Overall, current data suggest that heavy drinking may increase the risk of AF, but there is little evidence of a meaningful increase in risk from light drinking. Luckily, such levels of alcohol intake (some guidelines suggest no more than 2 drinks/day for men or 1 drink/day for women) have been shown from many previous studies to significantly lower the risk of cardiovascular disease and total mortality.
Reference: Tolstrup JS, Wium-Andersen MK, Ørsted DD, Nordestgaard BG. Alcohol consumption and risk of atrial fibrillation: Observational and genetic estimates of association. European Journal of Preventive Cardiology 2016; pre-publication. DOI: 10.1177/2047487316641804
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 184: A major new meta-analysis on alcohol consumption and the risk of pancreatic cancer — 4 April 2016
The present meta-analysis was based on data from more than four million subjects in prospective cohort studies, among whom 11,846 incident cases of pancreatic cancer were diagnosed. With the lowest intake group (non-drinkers or occasional drinkers) as the referent group, the authors defined “light” consumption as up to 12 grams/day (essentially one typical drink); 12-24 g/day as “moderate”; and ≥24 g/day as “heavy” drinking. The key results of the study were that, overall, neither light drinkers (RR = 0.97) nor moderate drinkers (RR = 0.98) showed an increase in risk of pancreatic cancer, while subjects classified as heavy drinkers had a slight increase (RR= 1.15, 95% CI 1.06 – 1.25). The increase in risk was due to heavy drinkers of liquor, as there was no significant increase in risk even for heavy drinkers of beer (RR = 1.08, CI 0.90 – 1.30) or wine (RR = 1.09, CI 0.79 -1.49).
Forum members considered this to be an excellent paper on the association between alcohol consumption and pancreatic cancer. The authors used appropriate methods and limited subjects to those in prospective cohort studies, which would tend to limit bias. The paper shows that the significant increase in risk occurred only among men, with no significant effect of alcohol being found among women. Among the weaknesses of the study were that there was a mixture of lifetime abstainers and ex-drinkers included in the referent group, and the same cut-points for category of alcohol intake was used for both men and women, whereas drinking guidelines are generally lower for women than for men. Further, data on the pattern of drinking (regular versus binge) were not available.
To summarize, this study showed no significant association with cancer risk for any level of consumption of beer or wine, which could relate to their lower concentration of alcohol per volume of the beverage, to non-alcoholic substances (such as polyphenols, present in wine and beer), or even to different drinking practices among subjects consuming different beverages. Thus, Forum members agree with the conclusions of the authors that heavy alcohol consumption, especially of liquor, increases the risk of pancreatic cancer, but the intake of beer or wine may not be associated with an increased risk.
Reference: Wang Y-T, Gou Y-W, Jin WW, Xiao M, Fang H-Y. Association between alcohol intake and the risk of pancreatic cancer: a dose–response meta-analysis of cohort studies. BMC Cancer 2016;16:212. DOI 10.1186/s12885-016-2241-1
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
==============================================================================
Critique 183: An unusual analysis of the association of alcohol consumption with mortality — 24 March 2016
The stated purpose of this new analysis was to determine whether misclassifying former and occasional drinkers as abstainers and other potentially confounding study characteristics underlie observed positive health outcomes for low volume drinkers in prospective studies of mortality. Unfortunately, the authors include in their analyses a number of old epidemiologic studies and do not acknowledge that when the “errors” that they have commented on in the past (such as including heavy ex-drinkers in the no-alcohol referent group) have been dealt with in the majority of studies over the past decade. The authors still exclude the vast majority of these well-done studies in their new meta-analysis. Results of essentially all studies that adjust for their concerns continue to show a significant and meaningful reduction in the risk of cardiovascular disease (CVD) and total mortality from the moderate intake of wine and alcohol.
Forum members note how very selective the authors are in choosing which papers to include in their new analyses: they identified 2,575 studies on the subject, analyzed 87, but then they found some reason to exclude almost all of these studies to reach a conclusion that “ . . . there was no significant protection for low-volume drinkers (RR = 1.04, 95% CI [0.95, 1.15])” based on what is apparently only 6 remaining studies! The paper ignores the comments by two other scientists (Roerecke & Rehm) who, like these authors, have in the past been very concerned that confounding and errors weaken the purported relation between alcohol and a lower risk of cardiovascular disease, but have more recently concluded: “For drinkers having one to two drinks per drinking day without episodic heavy drinking, there is substantial and consistent evidence from epidemiological and short-term experimental studies for a beneficial association with IHD risk when compared to lifetime abstainers. The alcohol-IHD relationship fulfills all criteria for a causal association proposed by Hill.”
The authors of the present paper also ignore the immense amount of experimental data, not only animal experiments but trials in humans, that have described the mechanisms by which moderate alcohol and wine intake have been shown to decrease essentially all of the risk factors for CVD, including low HDL-cholesterol, elevated LDL-cholesterol, endothelial dysfunction, coagulopathies, inflammation, abnormal glucose metabolism, and many others. The consistent finding of lower CVD risk among moderate drinkers in all well-done cohort studies is strongly supported by experimental evidence of the mechanisms.
In the opinion of Forum members, the present paper markedly distorts the accumulated scientific evidence on alcohol and CVD. As stated by one Forum member, “The biased selection of studies that are included undermines the value of the paper, but more importantly promulgates misinformation in the name of appropriate scientific method. Failure to acknowledge the robust body of knowledge that supports the opposite conclusion, and disqualification of extensive animal and cell culture studies that offer plausible biologic explanation of observed benefits, is unconscionable.”
The Forum concludes that the overwhelming body of observational scientific data, as well as an immense number of experimental studies, support the contention that, for most middle-aged and older men and women who choose to do so, the regular consumption of small amounts of an alcoholic beverage can be considered as one component of a “healthy lifestyle.” Such a habit has been shown to be associated with a lower risk of cardiovascular disease and of total mortality.
Reference: Stockwell T, Zhao J, Panwar S, Roemer A, Naimi T, Chikritzhs T. Do “Moderate” Drinkers Have Reduced Mortality Risk? A Systematic Review and Meta-Analysis of Alcohol Consumption and All-Cause Mortality. J Stud Alcohol Drugs 2016;77:185–198.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 182: A major meta-analysis on the association of alcohol consumption with the risk of diabetes mellitus — 8 March 2016
Most previous studies have shown that consumers of light-to-moderate amounts of alcoholic beverages tend to have a significant reduction in their subsequent risk of developing Type II diabetes mellitus (DM). The purpose of the present study was to explore and summarize the evidence on the strength of the association between alcohol consumption and the subsequent risk of DM by using a dose-response meta-analytic approach. The authors identified 26 prospective cohort studies providing data appropriate for a meta-analysis; their analyses were based on 706,716 individuals (275,711 men and 431,005 women) with 31,621 cases of DM.
This meta-analysis reports that light and moderate drinkers have a significantly reduced risk of developing DM. For “light” drinkers (defined as an average of ≤ 12 g/day of alcohol), in comparison with non-drinkers, the overall risk ratio for DM was 0.83, with 95% CIs of 0.73, 0.95 (P = 0.005). For “moderate” drinkers (>12- <24 g/day), the RR was 0.74, with 95% CIs of 0.67, 0.82 (P = 0.001). Thus, data from this meta-analysis indicate a 17% and 26% reduction in the risk of DM, respectively, for these two drinking categories.
For subjects classified as “heavy” users of alcohol (reported intake averaging ≥ 24 g/day), the RR was 0.98, with 95% CIs of 0.83, 1.09, P = 0.480), interpreted as no effect. In a figure in the paper showing the separate results for each individual study included, the point estimates for the risk of DM were 1.0 or less than 1.0 for light and moderate drinkers in essentially all studies. Thus, data from the individual studies support the overall finding of a decrease in risk of DM for light or moderate drinkers.
Sub-group analyses showed that when subjects were stratified by sex, age, BMI, smoking, physical activity, and family history of DM, the point estimates of the risk ratios associated with light or moderate alcohol consumption were less than 1.0 in all groups, adding further to the robustness of the overall conclusions of a reduction in risk of DM from alcohol intake. Similarly, for all subjects, as well as for men and women separately, there was a clear U-shaped curve for the association. The nadir of the effect was just over 20 grams of alcohol per day (about 2 typical drinks), and even the risk of heavy drinkers did not reach the estimated risk of non-drinkers.
Forum members considered this to be a well-done analysis that confirms most previous results from prospective studies indicating a reduction in the risk of developing DM associated with moderate drinking. Further, an increasing number of randomized clinical trials are supporting such beneficial effects on the development and clinical treatment of DM. The Forum thought it unfortunate that beverage-specific results were not available in this study, as increasingly it is being shown that, beyond alcohol effects, there are polyphenols and other substances in wine and beer that provide additional protection against diabetes. Further, the Forum felt it important to also emphasize the protective effects against cardiovascular disease among subjects who already have DM, who are especially vulnerable to coronary heart disease and other effects of atherosclerosis.
Overall, this meta-analysis based on a large number of subjects indicates that the risk of DM is considerable lower among light and moderate drinkers than among abstainers. This finding supports the contention that, for most middle-aged and older adults (with the exception of individuals with specific prohibitions against alcohol such as former drug or alcohol abuse, certain types of neurological or severe hepatic disease, etc.), moderate alcohol consumption should be considered as a component of a “healthy lifestyle” that reduces the risk of diabetes and most of the chronic diseases of ageing.
Reference: Li X-H, Yu F-F, Zhou Y-H, He J. Association between alcohol consumption and the risk of incident type 2 diabetes: a systematic review and dose-response meta-analysis. Pre-publication: Am J Clin Nutr 2016; doi: 10.3945/ajcn.115.114389.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 181: Support for a causal role of alcohol consumption in improving the lipid profile — 16 February 2016
The present paper is based on data from more than 10,000 Americans of European descent who were participants in the Atherosclerosis Risk in Communities (ARIC) study. Common and rare variants in alcohol dehydrogenase and acetaldehyde dehydrogenase genes were evaluated using Mendelian randomization (MR), and then a genetic score based on 5 SNPs was used in regression analyses for the association of alcohol with lipids. Results reported by the authors state: “Alcohol consumption significantly increased HDL2-c and reduced TG, total cholesterol, LDL-c, sdLDL-c, and apoB levels. For each of these lipids a non-linear trend was observed. Compared to the first quartile of alcohol consumption, the third quartile had a 12.3% lower level of TG (p < 0.001), a 7.71 mg/dL lower level of total cholesterol (p = 0.007), a 10.3% higher level of HDL2-c (p = 0.007), a 6.87 mg/dL lower level of LDL-c (p = 0.012), a 7.4% lower level of sdLDL-c (p = 0.037), and a 3.5% lower level of apoB (p = 0.058, P overall = 0.022).”
The authors thus conclude that “This study supports the causal role of regular low-to-moderate alcohol consumption in increasing HDL2-c, reducing TG, total cholesterol, and LDL-c, and provides evidence for the novel finding that low-to-moderate consumption of alcohol reduces apoB and sdLDL-c levels among European-Americans.”
Forum members considered this to be a well-done and important study, the results of which indicate favorable effects of moderate alcohol consumption on lipid factors. However, they doubt that the inclusion of the genetic score from MR played a large part in the results; the authors state that the genetic score used in this paper explained only approximately 0.1% variance of alcohol consumption, suggesting that it was a weak instrumental variable for the MR. Several Forum members stated that randomized control trials, especially cross-over trials, testing the effects of alcohol intake on risk factors, may provide even better evaluation of alcohol’s effects on lipids. Until large-scale RCTs of alcohol and disease occurrence can be are carried out, such RCTs may provide the most reliable data on mechanisms of alcohol’s effects on the risk of cardiovascular disease.
Overall, the present study provides important data indicating that light-to-moderate alcohol consumption has favorable effects on most lipid values. The effects shown for HDL-cholesterol support much earlier data, and the effects on small dense LDL-cholesterol and ApoB provide key new information. The effects on lipids are surely important factors in the protective effects of moderate drinking against cardiovascular disease that have been seen in almost all well-done cohort studies.
Reference: Vu KN, Ballantyne CM, Hoogeveen RC, Nambi V, Volcik KA, Boerwinkle E, Morrison AC. Causal Role of Alcohol Consumption in an Improved Lipid Profile: The Atherosclerosis Risk in Communities (ARIC) Study. PLoS One 2016;11:e0148765. doi: 10.1371/journal.pone.0148765. eCollection 2016.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 180: The association of alcohol intake with total mortality risk among women — 9 February 2016
The follow up of more than 6,000 women in a population-based cohort in an area of southern Sweden was used to estimate how baseline levels of alcohol consumption, at age 50-59 years, related to total mortality risk over the subsequent 17 years. At baseline, 26% of women reported no alcohol consumption while 13% reported an average of 12 or more grams of alcohol per day. Thus, the large majority (61%) were light drinkers, reporting the equivalent of no more than one drink per day. The authors report that, even when adjusting for education, marital status, smoking, BMI, physical fitness, diabetes and ischemic heart disease before screening, mortality risk during follow up was significantly higher among non-drinkers and heavier drinkers than among women reporting the equivalent no more than one typical drink per day. They state that their analyses thus support a “J-shaped” association between alcohol and total mortality risk, and that “The observed protective effect of light drinking (1–12 grams/day) could thus not be attributed to any of these known confounders.”
Forum members agreed this was a well-done study, but noted that the authors were unable to adjust for the pattern of drinking (regular versus binge), previous drinking among abstainers, or potential changes in drinking during follow up. Also, beverage-specific results are not presented. Further, the data presented in this study are not adequate to judge the specific level of alcohol consumption at which total mortality risk for drinkers reaches or exceeds the risk for non-drinkers; in other words, the “threshold” for adverse effects of alcohol on mortality cannot be determined very well. Nevertheless, the results of these analyses are very consistent with most long-term follow-up studies and support a “J-shaped” association between alcohol and the risk of total mortality.
Reference: Midlöv P, Calling S, Memon AA, Sundquist J, Sundquist K, Johansson S-E. Women’s health in the Lund area (WHILA) – Alcohol consumption and all-cause mortality among women – a 17 year follow-up study. Pre-publication: BMC Public Health 2016;16:22. DOI 10.1186/s12889-016-2700-2.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 179: Response to proposed guidelines regarding alcohol consumption in “Guidelines for a Healthy Diet” from the the Health Council of the Netherlands – 26 January 2016
The Health Council of the Netherlands has published “Guidelines for a Healthy Diet” that include a section related to alcohol consumption. Our Forum has been asked to provide comments on the alcohol guidelines (an English translation of certain sections related to alcohol consumption are attached as an appendix to the full review of these guidelines). The closing guidelines given in the Dutch document are as follows: “Do not drink alcohol, or at least no more than one glass per day. [The guidelines from 2006 recommended limiting one’s alcohol intake to one glass (women) or two glasses (men). The current data suggests that the guideline for men should be adjusted downwards.]”
Forum members were concerned that the guidelines were based on a very restricted number of the many hundreds of excellent epidemiologic and experimental publications in recent years that clearly indicate that moderate alcohol has favorable effects on most of the diseases of ageing, and on total mortality risk. For example, the proposed guidelines focus on adverse effects of alcohol on lung cancer, while current scientific knowledge suggests that it has negligible effect. Much of the discussion in the guidelines focusses on the dangers of alcohol on cancer, whereas data show that almost all of the risk (except for breast cancer) is from heavy drinking, not light-to-moderate drinking. Data strongly support a major role of alcohol abuse for upper aero-digestive cancers, but only minor effect on cancer in general from light-to-moderate drinking, especially when other lifestyle factors and under-reporting of intake are taken into account.
The findings for a benefit of moderate drinking on cardiovascular disease among middle-aged and older adults are very much under-played, despite overwhelming data showing a significant benefit. The “J-shaped” curve (lower risk of many diseases with light-to-moderate alcohol intake with higher risk for heavier drinking) is not presented in the guidelines, a major omission when presenting data on alcohol to the public. The additional protection against disease when moderate alcohol consumption occurs with meals was not mentioned. As one Forum member commented: “When professionals discuss alcohol consumption, what consumers want to know is first ‘how much,’ and then ‘when’ to drink.”
Overall Forum members considered that the proposed guidelines regarding alcohol consumption from the Health Council of the Netherlands in a number of sections do not reflect current scientific knowledge on the association of alcohol to health and disease. Forum members tend to agree with the statement of Boffetta and Hashibe who, in an extensive review of alcohol and cancer, stated that “Drinking, especially heavy drinking, increases cancer risk. However, total avoidance of alcohol, although optimum for cancer control, cannot be recommended in terms of a broad perspective of public health, in particular in countries with high incidence of cardiovascular disease.”
Forum members consider that it is important to describe both the potential harms and benefits for health associated with alcohol consumption, especially for middle-aged and older adults. The “J-shaped” curve should be an important concept in any guidelines on drinking that are presented to the public.
Reference: An English translation provided to the Forum includes parts of Section 8 of the Guidelines for a Healthy Diet, from the Health Council of the Netherlands; this material is included as an Appendix to the full report of this critique.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 178: The association of alcohol intake with health-related quality of life — 12 January 2016
Many studies have shown that moderate alcohol drinkers tend to have higher ratings of their quality of life (QOL) than non-drinkers. The directionality of this association has been difficult to ascertain: does moderate drinking improve someone’s QOL, or do people with higher QOL to begin with tend to drink alcohol moderately? The present study attempts to provide data designed to evaluate the directionality of these associations for both physical aspects of QOL as well as mental aspects.
Forum reviewers considered this to be a very well-done study from the Nurses’ Health Study II, with excellent and repeated measurements of both alcohol consumption and indices of QOL. It deals with the assessment of both physical and mental aspects of quality of life as well as the directionality of such an association: subjects were repeatedly assessed for the effects of alcohol intake on subsequent QOL as well as the effects of a given QOL measure on subsequent alcohol intake.
The key reported findings of this study were a positive association between alcohol and subsequent indices of physical QOL indices, with the poorest outcomes in abstainers and former drinkers; in spline analyses, the favorable effect appears to be up to about 2 drinks/day. Subjects with higher physical QOL also appeared to consume more alcohol in subsequent assessments. Somewhat surprising was the finding of little relation between alcohol and mental aspects of QOL, and even an apparent deleterious effect at the highest category of drinking. Thus, the study reports that physical aspects of QOL are positively associated with alcohol consumption, while mental aspects show little relation.
There was some concern by some Forum members about the methods used by the authors in adjusting, or not adjusting, for previous exposures (both alcohol and indices of QOL). Given that both baseline alcohol intake and QOL measures may tend to remain rather static over the period of the study (this “prevalent” exposures), adjusting for the effects of baseline values could attenuate any effect seen on subsequent outcomes. For example, if alcohol consumption indeed affects QOL and consumption remains roughly the same over the time period of the study, any effect of subsequent alcohol on QOL may be subsumed by the effects shown at baseline. In that situation, the net effect of adjustment for baseline alcohol may attenuate (or remove) the effect of the follow-up exposure on the outcome variable. The authors of this paper were aware of this problem, and attempted to deal with it. However, from the data presented, it is not possible to ascertain the specific analytic procedures used, and the final estimates of effect given for alcohol and QOL may still be biased.
Overall, the Forum considers this to be an important contribution to our understanding of how alcohol consumption may affect quality of life, and how quality of life affects alcohol consumption. As interpreted by the authors, physical aspects of QOL may be positively affected by alcohol consumption, but there is little effect on mental aspects of QOL.
Reference: Schrieks IC, Wei MY, Rimm EB, Okereke OI, Kawachi I, Hendriks HFJ, Mukamal KJ. Bidirectional associations between alcohol consumption and health-related quality of life amongst young and middle-aged women. J Intern Med 2015, pre-publication. doi:10.1111/joim.12453.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 177: A clinical trial testing the effects of alcohol on inflammatory markers — 21 December 2015
While there have been many observational studies of the relation of alcohol consumption to health risks and benefits, the number of clinical trials of alcohol administration for its health effects are limited. The present paper is based on a controlled diet cross-over trial among 53 postmenopausal women. A standard diet was provided for a period of 6 months; two meals each weekday were consumed at the study facility and food was provided for other meals. To the standard meal, during three 8-week interventions, either 0, 15 g, of 30 g of alcohol (ethanol) were added to the daily diet, with the two doses of alcohol the equivalent of a little over one typical drink and 2 ½ typical drinks. Weight remained stable and no adverse effects were reported.
The key results of the trial were that, during periods when alcohol was consumed, there were small but significant decreases in markers of cellular adhesion molecules and components in the hemostatic pathway; these are indices of inflammation and the effects are consistent with a decreased risk of cardiovascular disease (CVD). Specifically, reductions were seen when alcohol was administered for s-ICAM, fibrinogen, and D-dimer, all of which would be expected to lower CVD risk. PAI-1 increased with alcohol, and there were no effects on CRP, Factor VIIc or IL-6.
While there were a number of question about the study, Forum members considered that, overall, this was a very well-done, difficult-to-carry-out study that shows alcohol’s beneficial effects on a number of inflammatory and hemostatic factors. The results are in line with many observational studies, although some previous intervention studies have found such effects only after the administration wine (but not of gin), suggesting a key effect of the polyphenols in wine. This study indicates that ethanol itself may have similar beneficial effects on mechanisms that relate to the development of cardiovascular disease.
Reference: Stote KS, Tracy RP, Taylor PR, Baer DJ. The effect of moderate alcohol consumption on biomarkers of inflammation and hemostatic factors in postmenopausal women. European J Clin Nutrition 2015; advance online publication. doi:10.1038/ejcn.2015.182
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 176: A New Report on Alcohol Consumption and Total Mortality Risk — 14 December 2015
Most observational studies have found that moderate drinkers, in comparison with nondrinkers, tend to have lower risk of all-cause (total) mortality; this is probably related primarily to a reduction in the risk of cardiovascular disease, the leading cause of death among the elderly. This large study has conflicting findings, as the author claims that the present analyses do not demonstrate protection against mortality from light-to-moderate drinking. In this study, what were termed “occasional drinkers,” rather than nondrinkers, were used as the comparison group.
Forum members had two main concerns about this study that warrant an investigation of the author’s conclusions: there was no consideration of under-reporting of alcohol intake when declaring “occasional drinkers” as the referent group, and (2) the inclusion, and adjusting for as “confounders,” several factors that are actually mechanisms by which alcohol has been shown to reduce mortality.
The first concern could have led to many light drinkers being included in the referent group, and thus not evaluated for a potential protective effect of light drinking on mortality. In fact, presented only in the Appendix to the paper are data showing that when nondrinkers make up the referent group, consumers of 1-7 as well as 7-14 drinks per week show significant 20-30% reductions in the risk of mortality; these findings are very similar to those of most previous epidemiologic studies.
The second, and perhaps more important concern, is that some of the mechanisms by which moderate alcohol intake may lead to lower mortality, such as reducing the risk of diabetes and coronary heart disease, were “adjusted” for in the analyses. This would attenuate or even erase any true reduction in risk of mortality from moderate drinking.
Some Forum members also were concerned that some subjects were missing data on alcohol consumption but, rather than excluding them, an estimated value was imputed for them. Further, data on the pattern of drinking (regular moderate versus binge drinking) or on the type of beverage consumed were not included in the evaluation.
Forum members conclude that the results of this study will obviously be considered in conjunction with other scientific data when seeking to judge the relation of alcohol intake to mortality. However, concerns about the analysis raise questions about the conclusion of the author of no protective effect of alcohol on mortality, a finding that conflicts with the results of most previous studies.
Reference: Goulden R. Moderate Alcohol Consumption Is Not Associated with Reduced All-cause Mortality. Am J Med 2015; pre-publication. http://dx.doi.org/10.1016/j.amjmed.2015.10.013.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 175: An update on the association of alcohol consumption with breast cancer: Effects of BMI — 24 November 2015
Most observational epidemiologic studies have shown a slight increase in the risk of breast cancer for women who consume alcohol; the degree of increase is usually small for light-to-moderate drinkers (between 5% and 15% increase for consumers of no more than one drink/day), but the risk may be higher for women consuming greater amounts of alcohol. However, there are a number of factors that affect this relationship, including the type of study (cohort or case-control), the pattern of drinking (regular versus binge), the type of beverage consumed, folate intake, use of hormone replacement therapy, as well as genetic factors. It has also been shown that the risk of breast cancer among obese women tends to be higher than among non-obese women, but there are limited data on how obesity interacts with alcohol in affecting the risk of breast cancer. It is clear that alcohol consumption cannot be evaluated in isolation, without considering other factors that relate to the development of breast cancer.
The present study is based on a large cohort of Swedish women who were examined as part of the Women’s Lifestyle and Health Study in 1991 – 1992, then followed through 2009 for the development of breast cancer: 1,385 cases were ascertained among the more than 45,000 women in the study. Alcohol was assessed at baseline and again at the follow-up examination, and the diagnosis of breast cancer was gleaned through linkage to the nationwide health registries in Sweden. Almost all of the women were pre-menopausal at baseline.
Forum members considered this to be a very well-done study, with almost complete ascertainment of cancer cases. There were some concerns, however, including the fact that the height and weight of subjects was not measured but self-reported, perhaps resulting in less accurate estimates of BMI. Further there may have been residual confounding from other factors related to breast cancer that were not assessed. Finally, the reported levels of alcohol consumption among the women in this study were very low (72% of the cohort drank either zero alcohol or below 5 g per day), but it cannot be determined if these are indeed the levels in this population or whether there may have been under-reporting of consumption.
The key findings as reported by the authors were that, overall, there was “no statistically significant association between alcohol intake and breast cancer risk after adjustment for confounders.” While this is indeed supported by their data, Forum members warned that readers should also note that there was an increase in risk found in less-obese women (BMI ≤ 25 kg/m2), among whom there was a step-wise increase in the risk ratio for cancer from 1.0, to 1.05, to 1.19, to 1.32 with increasing category of alcohol intake. This association was not seen in the more obese women for total cancer or for any of the sub-categories of cancer.
While the overall results did not show an increase in risk from alcohol intake, the results among non-obese women are similar to those seen in many other studies, and suggest a slight increase in the risk of breast cancer associated with alcohol for at least some women. The differences in effect according to BMI reported by the investigators are interesting and add to our understanding of the association of alcohol with breast cancer which, however, remains unclear.
Reference: Shin A, Sandin S, Lof M, Margolis KL, Kim K, Couto E, Adami HO, Weiderpass E. Alcohol consumption, body mass index and breast cancer risk by hormone receptor status: Women’ Lifestyle and Health Study. BMC Cancer 2015;15:881 (DOI 10.1186/s12885-015-1896-3)
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 174: Two-year clinical trial of wine administration in diabetics who were previous abstainers or very-light drinkers — 19 October 2015
Observational epidemiologic studies have consistently found that moderate drinkers are at lower risk of cardiovascular disease (CVD); such alcohol consumption also lowers both the risk of diabetes as well as of CVD among diabetics. However, there have been few clinical trials of the administration of alcohol or wine among diabetics, and most have been for relatively short periods of time. Forum members welcomed the publication of the results of the present study, and consider that it provides valuable information on the relation between wine and cardiometabolic risk.
In this study, among 224 subjects with diabetes aged 40 to 75 years who were abstainers or very light drinkers (previously reported none or < 1 drink/week), the investigators carried out a randomized clinical trial of the effects of wine on cardiometabolic factors. The subjects were randomly assigned to 150 mL of mineral water, white wine, or red wine with dinner for 2 years; all groups followed a Mediterranean diet without caloric restriction. The study was described to subjects as a dietary intervention, and there were group sessions led by clinical dietitians each month for the first three months and then at 3-monthly intervals thereafter. The focus was on the Mediterranean diet, and wine was not discussed at these meetings. There was excellent compliance with the provided beverages (>80%) and excellent continued participation of subjects (94% for one year and 87% for the full two years).
The key results of this study were that the administration of 150 ml of red wine with dinner each evening, in comparison with mineral water, favorably affected many cardiometabolic factors, and especially led to an increase in HDL-cholesterol and apolipoprotein (a). The administration of similar amounts of white wine was also beneficial, and specifically improved measures of glycemic control.
Further, in 203 of the subjects, effects according to the genetic factors determining ADH were evaluated. In the study, 35.6% of subjects were homozygous for the polymorphism for “slow ethanol metabolism,” 21.3% were homozygous for that for “fast ethanol metabolism,” and 43% were heterozygous. Forum members agreed with the summary statement of the authors: “We found that diabetic patients who were slow alcohol metabolizers had improved glycemic control by initiating moderate wine consumption, which suggests that alcohol may play a role in glucose metabolism. In contrast, diabetic patients who were fast ethanol metabolizers benefited the most from the wine-induced BP-lowering effect, which suggests a mediatory role for ethanol metabolites.”
The study has important implications for advice to be given to diabetics. Most, but not all, Forum members agreed with the authors’ conclusion that “Initiating moderate wine intake, especially red wine, among well-controlled diabetics as part of a healthy diet is apparently safe and modestly decreases cardiometabolic risk.”
Reference: Gepner Y, Golan R, Harman-Boehm I, . . . Stampfer MJ, Shai I, et al. Effects of initiating moderate alcohol intake on cardiometabolic risk in adults with type 2 diabetes. A 2-year randomized, controlled trial. Ann Intern Med 2015; pre-publication. doi:10.7326/M14-1650
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 173: A Large Study of the Association of Alcohol with the Risk of Acute Myocardial Infarction — 15 October 2015
This paper presents prospective data from a large population-based cohort from rural Norway, a region with typically light alcohol drinking and many abstainers who were not ex-heavy drinkers. It relates reported alcohol intake, assessed on two occasions, with the risk of developing an acute myocardial infarction (AMI). Its key findings are that, even in this very light-drinking population, drinkers had significantly lower risk (about 20% to 30%) of developing a MI than non-drinkers. As the authors conclude: “Light-to-moderate alcohol consumption was linearly associated with a decreased risk of AMI in a population in which abstaining from alcohol is not socially stigmatized. Our results suggest that frequent alcohol consumption is most cardioprotective and that this association is not driven by misclassification of former drinkers.”
As this was a rather homogeneous rural cohort without huge differences among subjects in socioeconomic status, it allows much better control of confounding. The fact that these results show essentially a continuous inverse association (rather than the usually seen “J-shaped” curve) is not unexpected given the very few heavy drinking subjects in this cohort. In addition to cardiovascular disease, the investigators also reported effects on total mortality, which showed a “J-shaped” curve.
Forum members considered this to be a very well-done study, and supports almost all previous research showing a protective effect of moderate drinking on the risk of coronary heart disease. The authors had good data on alcohol exposure and the occurrence of AMI. A key result from this study is that frequent light drinking, even less than an average of one drink/day, is associated with a significant decrease in the risk of coronary heart disease. Based on this study and most previous research, the clear message to the public remains: if you have no contraindications to alcohol use and decide to consume an alcoholic beverage, the healthiest approach is to drink frequently but in small amounts.
Reference: Gémes K, Janszky I, Laugsand LE, Lászlo KD, Ahnve S, Vatten LJ, Mukamal KJ. Alcohol consumption is associated with a lower incidence of acute myocardial infarction: results from a large prospective population-based study in Norway. J Intern Med 2015; doi: 10.1111/joim.12428.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===========================================================================================================
Critique 172: Alcohol and the risk of developing diabetes — 7 October 2015
Prospective cohort studies for decades have tended to show that the risk of developing Type II diabetes mellitus is reduced among moderate drinkers in comparison with non-drinkers, with previous meta-analyses suggesting that moderate drinkers may have about 30% lower risk than that of abstainers. The present study carried out a multi-language search for studies on alcohol and diabetes and conducted a meta-analysis involving almost two million subjects from a final group of 38 cohort, case-cohort, case-control, or nested case-control studies. The main conclusions of the authors are that only females may show a significant inverse association between alcohol consumption and the risk of diabetes, and that previous studies may have overestimated the reduction in risk from moderate drinking.
Forum members had concerns about the analyses and the conclusions of the authors, as the males in the study were primarily Asian (86%), and there were huge differences between the associations with alcohol for Asian and non-Asian populations. There are always problems when the basic study data have a marked degree of heterogeneity. In general, many of the factors that relate to diabetes (diet, body size and adiposity, type of beverages consumed, etc.) are quite different between Asians and non-Asians; combining such groups when their analyses show opposite effects of alcohol on diabetes risk may not be a reasonable way of trying to develop results that apply globally. Forum members do not believe that the analyses presented in this paper can support the conclusion of the authors that there is “no effect among males.” It could be unwise if the results of this study were used to develop alcohol guidelines for western populations.
The authors could not take the pattern of drinking (regular versus binge) or the type of alcohol into consideration. Clinical trials have suggested that wine and its polyphenols may have effects above and beyond those seen with alcohol alone, and beneficial effects of such polyphenols have been demonstrated both for women and for men. Thus, while the analyses in this paper were all carried out accurately, attempting to use these data to develop guidelines that would apply globally, as was done by the authors, may not be appropriate.
Reference: Knott C, Bell S, Britton A. Alcohol Consumption and the Risk of Type 2 Diabetes: A Systematic Review and Dose-Response Meta-analysis of More Than 1.9 Million Individuals From 38 Observational Studies. Diabetes Care 2015;38:1804–1812 | DOI: 10.2337/dc15-0710
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 171: A global assessment of alcohol and health — 29 September 2015
The present publication is from the very large Prospective Urban Rural Epidemiological (PURE) study that focuses especially on middle-income and lower-income countries, for which previous data on the association of alcohol consumption with health outcomes are sparse. Included in this analysis are data from high-income countries (HICs: Sweden and Canada); upper-middle-income countries (UMICs: Argentina, Brazil, Chile, Poland, South Africa and Turkey); lower-middle-income countries (LMICs: China and Columbia); and low-income countries (LICs: India and Zimbabwe). The large majority of the subjects were from lower income countries.
It has long been recognized that, when evaluating the health effects of drinking, it is especially important to evaluate alcohol intake within a particular population, with its specific genetic, lifestyle, environmental, and cultural factors, and not study alcohol in isolation. While the PURE study is a very well-done study, Forum members were concerned that the authors have attempted to answer overall questions about alcohol and health by combining data from such diverse populations. For example, the issue of very different causes of mortality in different populations would lead to very different approaches to improving longevity. There are too many factors associated with health outcomes to attempt to determine the specific alcohol effects when considered in isolation.
The authors tried to adjust for confounders as far as that was possible, but one cannot exclude further confounding, especially as subjects from lower-income countries contained a much larger proportion of smokers than there were in higher-income countries. The authors also point at differences between countries not fully explained by drinking pattern (or other factors); this suggests that further confounding exists. Further, lumping all types of stroke into one category may be hiding associations, especially as lower-income countries might have a higher frequency of cerebral hemorrhages. Similarly, using a single grouping for all cancers may be inadequate. Other limitations of this study include the short duration of follow-up time (4.3 years) and the low number of cases of each outcome.
The Forum concluded that even though the study includes information from many countries, it is not possible from such data to determine net health effects of alcohol consumption that are applicable to people everywhere. Their analytic results cannot be used, as the authors suggest, to “support global health strategies,” although they may surely be useful for developing “national initiatives to reduce harmful alcohol use,” especially for lower-income countries.
Reference: Smyth A, Teo KK, Rangarajan S, O’Donnell M, Zhang X, Rana P, Leong DP, et al. Alcohol consumption and cardiovascular disease, cancer, injury, admission to hospital, and mortality: a prospective cohort study. Lancet 2015. Pre-publication. http://dx.doi.org/10.1016/ S0140-6736(15)00235-4. Online/Comment http://dx.doi.org/10.1016/ S0140-6736(15)00236-6.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 170: An update on the association of alcohol consumption with the risk of cancer — 1 September 2015
This well-done analysis based on data from two very large cohort studies, the Nurses’ Health Study and the Health Professionals’ Follow-up Study, evaluated the association of alcohol consumption over many years with the risk of cancer. The authors conclude that men reporting an average intake of more than 15 grams of alcohol per day, but not less, have a significant increase in risk of alcohol-related cancers. In women, however, even the consumption of an average of 5.0 – 14.9 grams of alcohol per day (the equivalent of between ½ and 1 ½ typical drinks) was associated with a slight increase in total cancer risk, stated to be primarily from an increase in the risk of breast cancer. For both genders, there seemed to be a dose-response increase in risk of cancer with larger amounts of alcohol. At the same time, smoking was identified as an even more important risk factor than alcohol for these cancers.
Forum members considered this to be an important study presenting data that are of relevance to individuals and agencies providing advice regarding alcohol consumption. There is little question that heavy drinking markedly increases the risk of upper aero-digestive cancers, and no physician or agency advises people to consume in excess of the typical limits of no more than one or two drinks/day. Hence the finding in this study of an increase in some cancers among women (especially breast cancer) even for lighter drinking has implications for alcohol policy.
The Forum was disappointed that all dietary and other lifestyle factors that have been shown to increase the risk of cancer (data that are known to be available to these investigators) were not included in their report. Members were especially concerned that the net effects on health and mortality of light-to-moderate alcohol consumption were not commented upon in the paper. Given that the risk of the most common causes of death, especially cardiovascular diseases, are reduced by moderate drinking, it seems that the authors should have included data, or at least mentioned, the effects of alcohol on cancer mortality and, especially, on total mortality. It has recently been emphasized that cohort studies that report on only one outcome (in this case, cancer) but do not mention other outcomes that are affected by the same exposure, especially total mortality, do not present the full picture, and can lead to biased recommendations. The inclusion of such information from these cohorts could provide even more valuable data upon which to develop appropriate guidelines for alcohol use by individual patients and the public.
Reference: Cao Y, Willett WC, Rimm EB, Stampfer MJ, Giovannucci EL. Light to moderate intake of alcohol, drinking patterns, and risk of cancer: results from two prospective US cohort studies. BMJ 2015;351:h4238; doi: 10.1136/bmj.h4238
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 169: Effects of IQ on risk of morbidity and mortality related to alcohol consumption — 25 August 2015
The present paper is based on a large cohort of subjects in Sweden who had IQ tests as children (when they were 13 years old) and were then followed for more than 30 years. The study reports an inverse association between childhood IQ and hospitalization for alcohol-related diseases or death. The association is strongly dose-dependent, with a marked increase in disease/mortality risk for each decrease in the childhood IQ score.
A key finding in this analysis is that the attained socio-economic status (SES) of the subjects at age 32 played a large role in explaining the association between IQ and alcohol-related disease and appeared to completely explain the association with death from alcohol-related causes. This suggests that much of the effect of IQ during childhood may be through its effect on later education, occupation, and income of the subjects, associations that have been noted in many previous epidemiologic studies to favor better health. It is reassuring that being born into a poor, uneducated family is not as important as a determinant of adverse effects of alcohol later in life as is the attained socio-economic status of the individual in young adulthood.
A possible explanation for the inverse relation of SES in young adulthood with adverse alcohol outcomes could relate to the type of beverage consumed, which was not evaluated in the present analysis. In a previous study from Denmark, it was shown that higher SES in young adults was associated with a strong preference for wine rather than for other types of alcoholic beverage. Wine consumption has been associated with better health in numerous studies, although it is unclear whether this is due primarily to the non-alcoholic constituents in wine or to confounding from associated lifestyle factors of wine drinkers.
Forum members agree with the authors that the underlying causes for an association between IQ (or SES) and adverse alcohol-related disease and death are not clearly defined. It could be that intelligence has effects on health through choices in lifestyle behavior or socioeconomic environment as an adult, or the relationship between intelligence and health is confounded by other factors such as biological or socioeconomic conditions early in life. As for now, we can only describe the association, but not explain it fully.
Reference: Sjölund S, Hemmingsson T, Gustafsson JE, Allebeck P. IQ and alcohol-related morbidity and mortality among Swedish men and women: the importance of socioeconomic position. Journal of Epidemiology and Community Health 2015;69:858-864.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 168: Effects of alcohol on blood pressure in women: A randomized trial — 5 August 2015
The present paper describes the effects among 24 normotensive pre-menopausal women, all of whom were regular drinkers (of an average of 2 to 3 drinks/day), of the administration of two levels of alcohol in the form of red wine in a randomized clinical trial. Subjects were given low amounts of wine and higher amounts of wine during two 4-week intervention periods, with the effects on blood pressure compared with changes when subjects were given similar amounts of dealcoholized red wine. Subjects were divided into a “lower level” usual intake group who previously consumed < 200 g/week of alcohol and a “higher level” group who previously consumed >200 g/week.
Previous “lower level” drinkers were given two levels of alcohol, in the form of 100 ml/day of red wine on 4 days per week (an average of 46 g/week of alcohol, or the equivalent of about ½ typical drink per day) and 200 ml/day of red wine daily (about 146 g/week of alcohol, the equivalent of about 1 ½ to 2 typical drinks/day) for another 4-week period. Subjects who were previous “higher level” drinkers were given 100 ml of red wine daily (about 73 g/d of alcohol per week, the equivalent of about one typical drink/day) for 4 weeks and 300 ml/d of red wine (about 218 g/week of alcohol, the equivalent of about 2 to 3 typical drinks/day) for another 4 weeks.
The main results are a small but significant increase in 24-hour average blood pressure (+2.0 mmHg systolic and +1.3 mmHg diastolic) with higher levels of red wine but no significant effects (+0.4 mmHg systolic, -0.3 mmHg diastolic) from lower levels of red wine administration, when compared with blood pressure levels during periods when dealcoholized red wine was given. The differences were predominantly due to slightly higher awake rather than asleep blood pressures. These findings are similar to results of a limited number of randomized controlled trials of alcohol in men.
Forum members considered this to be a well-conducted clinical trial, with important results. There were, however, some concern that the study focused only on regular drinkers; results may have been different if previous abstainers had also been studied. Further, while the slight increase in blood pressure from higher levels of alcohol support previous research, the finding of no significant findings for lower levels of intake (when subjects were given the equivalent of between ½ and 1 drink/day) may not support what the authors suggest: “Our results provide no support for the concept that regular low-level alcohol intake can lower BP, suggesting that the J-shaped relationship between alcohol and BP in several studies is more likely because of the presence of unmeasured confounders.” Forum members considered their results to be consistent with either a slight increase or a slight decrease in blood pressure among such drinkers and are not necessarily inconsistent with data from some previous cohort studies that showed a “J-shaped” relation between alcohol and blood pressure.
A number of Forum reviewers also raised the question as to whether or not the results of a 4-week intervention study can be extended to the effects of the regular intake of alcohol for many years. Further, the fact that the study group included previous drinkers of up to similar amounts of alcohol as given during the higher intervention (yet were still normotensive) might suggest that their blood pressure was not “sensitive” to alcohol, and could limit the applicability of these results to the general public. Nevertheless, this intervention study provides important trial data on the short-term effects of alcohol on blood pressure.
Reference: Mori TA, Burke V, Beilin LJ, Puddey IB. Randomized Controlled Intervention of the Effects of Alcohol on Blood Pressure in Premenopausal Women. Hypertension 2015;66:00-00. DOI: 10.1161/HYPERTENSIONAHA. 115.05773
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 167: What determines a person’s belief that “alcohol is heart-healthy?” — 22 July 2015
This paper, based on data from more than 5,000 adults participating in an internet-based survey, sought to determine what were the perceptions of subjects on the relation of alcohol to heart disease, and how these perceptions resulted in particular behaviors related to alcohol consumption. Partricipants for the survey were recruited by a variety of methods, including announcements “in the lay press, promotional events, word of mouth, social media, e-mail, and clinic visits.” While the goal of the study is commendable, the results of any such survey obviously depend on many social and cultural factors of the people who respond to the survey; it was not a random sample of the population used in this analysis. This is critical because an interpretation of the data requires an understanding of the population surveyed.
Forum members had other concerns about this paper, including the specific survey questions regarding the perceptions of alcohol effects. For example, the key question asked in the survey was “Do you believe alcohol is good for your heart?” Forum members pointed out that it is obvious to nearly everyone that this cannot be answered without quantifying the amount of alcohol or the pattern of drinking. They consisdered that a more appropriate quesiton might be something such as “Do you believe that the moderate consumption of alcoholic beverages can benefit your heart?”
The authors make statements such as “Participants perceiving alcohol as heart healthy consumed 47% more alcohol.” This may sound alarming until it is revealed that the observed difference was from a baseline of 0-3 to 1-5 glasses of wine/week and from 1-7 to 2-8 total drinks/week. These higher amounts are not ‘alarming’ at all, and in fact fall within usual guidelines for “sensible drinking.”
Forum members were particularly upset that the authors misquote a number of scientific papers to support their claim that even low levels of drinking increase the risk of certain diseases. The authors also use such misrepresentations of data to justify their concerns that current guidelines for alcohol consumption may not be appropriate. Forum reviewers found it especially disturbing that the peer review process by the journal failed to uncover such misrepresentations of data.
The authors repeatedly give the impression that they are against any amount of alcohol consumption. They do not comment on the consistent findings in almost all well-done prospective studies indicating that moderate drinkers live longer than abstainers. Further, statements by the authors that suggest that people who think that alcohol is heart healthy are misinformed does not stand up to scientific data, which indicate that moderate and responsible drinking is associated wtith better health and longevity.
It is interesting that the report indicates that older, higher-income, and more highly educated subjects are more likely to consider alcohol to be heart healthy than younger and less-educated subjects. While a question was asked by the investigators as to whether or not the responder’s perception of the health effects of alcohol influences their decision to drink or to not drink, the specific responses to this question are not presented in the paper. It remains unclear to what extent beliefs about alcohol’s potential health effects relate to alcohol use or, more importantly, to alcohol abuse.
Overall, Forum members thought that the idea behind this study was of interest, but emphasized that it is important to collect data based on a random and well described sample of the population if one is to provide significant and understandable results. Further, the report is compromised by what appears to be a deliberate misrepresentation of the prior scientific literature to support the authors’ contention that alcohol is not healthy; there are a number of obvious errors that should have been detected during the review process by the journal. In the opinion of the Forum, the most reliable result from these analyses relates to where people obtain their information regarding alcohol and health: it does not come from physicians or scientific publications, but primarily from the lay press.
Reference: Whitman IR, Pletcher MJ, Vittinghoff E, Imburgia KE, Maguire C, Bettencourt L, Sinha T, Parsnick T, Tison GH, Mulvanny CG, Olgin JE, Marcus GM. Perceptions, Information Sources, and Behavior Regarding Alcohol and Heart Health. Am J Cardiol 2015; pre-publication. http:// dx.doi.org./10-1016/j.amjcard/2015.05-029.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 166: The association between alcohol consumption and suicidal ideation and suicidal attempt — 1 July 2015
The present study evaluates the relation of alcohol consumption and the pattern of drinking with self-reports of suicidal ideation and suicidal attempts among more than 43,000 men and women in Korea, using data from a 2007-2011 survey. Overall, 11.3% of males and 21.2% of females reported that they had experienced suicidal ideation, and 0.8% of males and 1.1% of females had attempted suicide. High scores on the Alcohol Use Disorders Identification Test (AUDIT) and a history of alcoholic blackouts were associated with suicidal ideation among both men and women and, for males, with suicidal attempts.
There is little known about the epidemiology of suicidal tendencies, or the specific causes of suicide. It is generally agreed that depression is the most important risk factor for suicide, and depression can lead to alcohol abuse; however, alcohol abuse can also lead to depression. Unfortunately, with cross-sectional data, analyses such as those in this paper cannot sort out the confounding issues nor, more importantly, address the causality of alcohol consumption with suicidal tendencies. The egg and hen question has never been solved – whether the depression or the heavy drinking came first. Thus, whether alcohol abuse increases the risk of depression (that may lead to suicide) or whether depressed people turn to alcohol seeking relief, cannot be determined from analyses such as these. However, it is also noted that this study suggests that drinking alcohol according to the usual guidelines for “sensible drinking” (generally, advising no more than 1 to 2 drinks/day) is not associated with the risk of suicidal ideation or attempt.
Forum members also commented on the large differences between populations in suicidal tendencies, being much higher in Korea and Japan than in most of Europe and North America. This could limit the applicability of the conclusions of this study to western populations.
Reference: Bae H-C, Hong S, Jang S-I, Lee K-S, Park F-C. Patterns of Alcohol Consumption and Suicidal Behavior: Findings From the Fourth and Fifth Korea National Health and Nutritional Examination Survey (2007–2011). J Prev Med Public Health 2015;48:142-150 • http://dx.doi.org/10.3961/jpmph.14.027
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 165: Fiber intake may modify the association of alcohol consumption with certain hormone-dependent cancers — 4 June 2015
The positive association between alcohol intake and certain hormone-dependent cancers (especially breast cancer) noted in many studies has been attributed to an effect of alcohol through an increase in levels of estrogen and other hormones. The present study had extensive dietary data on more than 5,000 men and women in France, among whom comparisons were made between the sex-specific tertile of alcohol intake and the risk of hormone-related cancers (breast, prostate, ovarian, endometrial, and testicular).
The study found that, overall, the risk of some cancers (e.g., breast) but not others (e.g., prostate) were positively related to reported alcohol intake. The key results reported by the authors are that when the risks of cancer were related to alcohol while adjusting for fiber intake, subjects whose fiber intake was below the median value showed higher risks of cancer related to alcohol, but not subjects with higher fiber intake. For example, when the risk of breast cancer in women was related to the tertile of their alcohol intake, the 2nd tertile showed a HR of 1.55 (1.01 – 2.38) and the 3rd tertile (HR 1.70, CI 1.11 – 2.61), when compared with women in the lowest tertile.
For prostate cancer in men, however, the 2nd tertile showed a HR of 1.28 (CI 0.82 – 2.00) and the 3rd tertile a HR of 0.89 (CI 0.55 – 1.45). The interaction terms between alcohol intake and cancer were not significant for all hormone-dependent cancers or for breast cancer. Only the interaction term for prostate cancer reached statistical significance, but here the relationship between tertile of alcohol intake even among subjects with low dietary fiber did not show a clear dose-response relation.
Forum members had concerns about the large number of potential confounders in these analyses (e.g., different effects for different types of fiber, the intake of fiber being just a marker for folate intake or for other dietary or lifestyle factors), that made it difficult for the authors to reach firm conclusions. Unfortunately, the numbers of tumors for each of the sub-groups were often too small to give meaningful results. And there was no data on alcohol drinking pattern (regular moderate versus binge drinking) or type of beverage consumed. Thus, while this study indicates that alcohol intake may relate to certain hormone-dependent cancers, the analyses do not present a clear demonstration as to whether it is fiber intake or some other related factor that may modify the association.
Reference: Chhim A-S, Fassier P, Latino-Martel P, Druesne-Pecollo N, Zelek L, Duverger L, Hercberg S, Galan P, Deschasaux M, Touvier M. Prospective association between alcohol intake and hormone dependent cancer risk: modulation by dietary fiber intake. Amer J Clin Nutr 2015; pre-publication. Doi: 10.3945/ajcn.114.098418.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 164: Why are the harmful effects of alcohol consumption greater among people with low education and income? — 14 May 2015
Epidemiologists have noted for many years that one of the key factors that modifies the relation between alcohol intake and many diseases is the education, income, or other index of socio-economic status (SES) of subjects. While differences in drinking practices (regular moderate versus binge drinking), other more moderate lifestyle factors, better access to health care, etc., have been suggested as potential mechanisms, there has been little research directed at this relation.
The present study is a systematic review of published reports to investigate the relationship between SES and risk of mortality or morbidity for each alcohol-attributable condition and, where feasible, to explore alcohol consumption as a mediating or interacting variable in this relationship. It summarized data from 31 case-control or cohort studies, relating an overall measure of the effects of low SES (variously defined) to the risk of cancers related to alcohol, as well as to liver disease, hypertension, stroke, epilepsy, cardiac arrhythmias, and pancreatitis.
The key findings of the study demonstrate a tendency for greater risk for low-SES subjects than for high-SES subjects to develop a number of diseases that are associated with alcohol consumption. Specifically, the authors report higher and statistically significant increases in risk of head and neck cancer and of stroke associated with alcohol consumption among lower-SES subjects than among higher-SES subjects. There was a tendency for lower risk of breast cancer among lower-SES women, but differences were not significant when adjusted for known confounders. The authors suggest that some of the effects shown may relate to greater total amounts of alcohol consumption by lower-SES subjects, or due to their higher levels of smoking.
Forum members thought this was a valiant attempt of the authors to unravel what has been a mystery: why do people at lower levels of SES seem to have more adverse effects of alcohol consumption than subjects at higher levels of SES. Unfortunately, as the authors admit, current scientific data do not allow firm answers. Suggested theories for reasons why low-SES subjects may have more adverse effects from alcohol include (1) different drinking patterns, with more binge drinking, (2) clustering of poor lifestyle factors, and (3) less access to health care. In some studies, even though the reported total alcohol intake of low- and high-SES subjects may be similar, the latter seem more likely to drink moderate amounts of alcohol on a regular basis, while lower-SES subjects are more likely to binge drink on fewer days per week. However, other studies do not support such a finding. Further, there may be differences according to the type of alcoholic beverage consumed, which was not considered in this study.
Forum members pointed out that differences in factors other than drinking patterns probably contribute to the greater adverse effects among subjects with lower SES. One member suggested that lower SES affects susceptibility to many diseases, most likely due to effect modification of hitherto unrecognized factors. The Forum concluded that there are too many confounders to make a conclusion about this topic, and much more research will be needed to understand how socio-economic factors affect the risk of disease and may modify the relation between alcohol consumption and disease.
Reference: Jones L, Bates G, McCoy E, Bellis MA. Relationship between alcohol-attributable diseaseand socioeconomic status, and the role of alcohol consumption in this relationship: a systematic review and meta-analysis. BMC Public Health 2015;15:400. DOI 10.1186/s12889-015-1720-7.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 163: The association of alcohol consumption with the risk of developing heart failure — 5 May 2015
Two new papers have provided data on the association of alcohol consumption with the risk of developing heart failure (HF). The first is a meta-analysis by Larsson et al that is based on eight prospective studies, with more than 200,000 subjects and 6,211 cases of HF. Meta-analyses provide important information because they are usually based on very large numbers of subjects and cases, and can detect smaller increases in risk than seen in individual studies. However, single large prospective cohort studies tend to provide more detailed information on, and allow better adjustment for, potential confounders. The second paper discussed in this critique by Dorans et al, is based on 33,760 men who were followed for 14 years, with almost 3,000 cases of fatal or non-fatal HF.
There was a high degree of consistency between these two studies: both concluded that moderate alcohol consumption, in comparison with non-drinking, is associated with a lower risk of developing HF. The meta-analysis (Larsson et al) concluded that there was a dose-response association between alcohol and HF; for example, a reduced risks of HF for consumers of 3 and 10 drinks/week (a 10% and 17% decreased risk, respectively), but not for those reporting the consumption of 21 drinks/week (a RR of 1.07; 95% CI 0.77 – 1.48). In the report from the single large Swedish prospective study (Dorans et al), the risk of HF for most categories of drinkers tended to be lower than that of never drinkers, with the lowest risk among consumers of 7 – 14 drinks/week (HR=0.81, 95% CI 0.69 – 0.96).
Forum members considered both of these studies to have been very well done, and the similar results not unexpected. HF has many causes, but in developed countries the most common is coronary artery disease (CAD), and moderate drinking has long been known to be associated with a lower risk of developing CAD. In their critique, Forum members discuss other conditions that relate to the development of HF, including conditions (such as respiratory infection, excessive salt intake, non-compliance with prescribed medication, etc.) that may trigger an attack of symptomatic HF.
To summarize, based on previous research and these two excellent papers, current data suggest that the moderate intake of an alcoholic beverage lowers the risk of the development of symptomatic HF. This undoubtedly relates, as least to some extent, to the demonstrated protection of alcoholic beverages against CAD. As for giving advice regarding the consumption of alcohol, Forum members agree with the conclusions stated by Klatsky in his editorial accompanying one of the papers: “All persons should avoid heavy drinking and many persons should avoid all alcohol. However, it is the author’s opinion that many middle-aged and older persons at risk of CAD or HF should be told that he or she is better off as a light to moderate drinker. Dispassionate objectivity plus common sense should dictate advice about drinking.”
References:
- Larsson SC, Orsini N, Wolk A. Alcohol consumption and risk of heart failure: a dose–response meta-analysis of prospective studies. European Journal of Heart Failure 2015;17:367–373. doi:10.1002/ejhf.228
- Dorans KS, Mostofsky E, Levitan EB, Håkansson N, Wolk A, Mittleman MA. Alcohol and Incident Heart Failure Among Middle-Aged and Elderly Men: The Cohort of Swedish Men. Circulation Heart Failure 2015; pre-publication. DOI:10.1161/CIRCHEARTFAILURE.114.001787.
For the full critique of these papers, and general comments on the association of alcohol with heart failure, by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 162: What is the association between alcohol consumption and cancer? 13 April 2015
Three major papers on the association of alcohol consumption and cancer have recently been published. Forum members considered that all were well-done, and presented valuable new information on the topic. While the key findings in each study are similar, each brings specific information on how alcohol relates to the risk of developing cancer. In this critique, we present the authors’ abstracts of each paper, our comments on the paper, and then an overall discussion of the topic.
Problems can occur when combing case-control studies with prospective cohort studies, as was done in one of the papers reviewed, as risk estimates are usually higher in the former type of study and potential confounding may be less complete. Further, it is especially important to consider the interaction between alcohol consumption and smoking for upper aero-digestive tract cancer, as was not always done. And none of the studies covered in this critique emphasized the net effects of alcohol that, because of protective effects against cardiovascular disease, is almost always associated with lower total mortality among moderate drinkers than among abstainers.
In summary, the Forum considers that the three papers reviewed provide important data on one of very few lifestyle factors that have been shown to relate to the risk of cancer. And cumulative research data clearly show that heavy alcohol intake increases the risk of upper aero-digestive tract cancers and some other cancers. Further, in these and many previous reports, even light alcohol consumption was associated with an increase in risk of breast cancer in women. Unfortunately, the threshold level of drinking associated with an increase in risk is not clearly defined for most cancers.
Forum members agree with the conclusions of Klatsky et al, who stated: “At present, a possible increased cancer risk at moderate intake should enter into individual estimation of the overall risk-benefit equation for alcohol drinking, especially for young persons. For most persons older than age 50 years, the overall benefits of lighter drinking, especially the reduced risk of atherothrombotic disease, outweigh possible cancer risk.”
References:
-
-
-
- Klatsky AL, Li Y, Tran HN, Baer D, Udaltsova N, Armstrong MA, Friedman GD. Alcohol Intake, Beverage Choice, and Cancer: A Cohort Study in a Large Kaiser Permanente Population. Perm J 2015;19:March 1, 2015. http//dx.doi.org/10.7812/TPP/14-189
- Bagnardi V, Rota M, Botteri E, et al. Alcohol consumption and site-specific cancer risk: a comprehensive dose–response meta-analysis. British Journal of Cancer 2015;112:580–593. doi: 10.1038/bjc.2014.579
- Wienecke A, Barnes B, Neuhauser H, Kraywinkel K. Incident cancers attributable to alcohol consumption in Germany, 2010. Cancer Causes Control 2015;[Epub ahead of print].
-
-
For the full critique of these papers, and general comments on alcohol and cancer, by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 161: The effects of alcohol consumption on the risk of hip fracture — 31 March 2015
Among elderly people, falls leading to hip fracture are a major health problem, leading to severe morbidity and mortality. Underlying factors that increase the risk of hip and other fractures include osteoporosis and low bone mineral density, as well as an unsteady gait making falls more common. The role that alcohol consumption among the elderly may relate to hip fracture has been a topic of concern for many decades, but data from a number of prospective studies now suggest that light-to-moderate drinking may actually decrease the risk of such fractures, while heavy drinking may increase the risk.
The present meta-analysis is based on prospective studies that have yielded more than 26,000 incidences of hip fracture. It concludes that there is a “J-shaped” association between alcohol consumption, especially of wine, and the risk of hip fractures, with lower risk for a reported consumption of about 1 drink/day, no effect from drinking between 1 and 4 to 5 drinks, and an increased risk from heavier drinking. Part of the “protection” from light drinking is apparently from the effects of alcohol on increasing bone mineral density.
Forum reviewers considered this to be a very well-done meta-analysis that provides balanced information on the risk of this common public health problem. Noting that the major differences seen in this study were between light drinkers and heavy drinkers, it was commented that there are many differences between people who are moderate in their habits, including moderate drinking, and people who usually consume more than 4 or 5 drinks/day; thus, there is still the possibility of other lifestyle factors confounding this association. Also, it was noted that most of the subjects in this analysis were North American or European, so applicability to other racial/ethnic groups may be limited.
In summary, this large and very well-done meta-analysis supports a protective effect of light alcohol consumption on the risk of hip fracture, with an increase in bone density from alcohol being a probable important factor. Data suggest that wine consumption may have the most favorable effect, perhaps indicating that polyphenols and other compounds may also play a role. The study shows that heavy drinking (an average of 4 to 5 or more drinks/day) is associated with an increase in the risk of hip fracture.
Reference: Zhang X, Yu Z, Yu M, Qu X. Alcohol consumption and hip fracture risk. Osteoporos Int 2015;26:531–542. DOI 10.1007/s00198-014-2879-y
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 160: Do the calories in alcoholic beverages lead to increased obesity? — 23 March 2015
Among people who consume alcohol, it would be assumed that the excess calories provided by the alcohol would add to their risk of obesity; however, current data suggest that the association may be more complex. It is unclear to what extent people who consume alcohol may modify other aspects of their diets, either decreasing or increasing other sources of calories. Further, alcohol is metabolized differently from other foods, which suggests that its calories may not be as readily available as those from fat, carbohydrate, and protein to increase obesity. The present paper provides an update on scientific data on the association between alcohol consumption and obesity. The overall conclusions of the authors are that light-to-moderate drinking does not increase the risk of obesity, while heavier drinking (or even moderate drinking among obese subjects) may lead to weight gain.
Forum reviewers appreciated the excellent summary of scientific reports on this topic, and thought that the authors gave a sound and balanced update on the topic. However, mechanisms why numerous prospective epidemiologic studies show that moderate drinking does not increase the risk of obesity are unclear. Given that alcohol contains calories, and if drinking alcohol does not displace the intake of other foods, it would be assumed that such calories would increase the risk of obesity unless there are particular metabolic differences between alcohol calories and those from protein, fat, and carbohydrate.
Potential mechanisms suggested have included a decreased utilization of calories from alcohol due to what is known as ‘Non-exercise Activity Thermogenesis’ (NEAT), in which the metabolism of alcohol may create more heat than fat. Also, the Forum discussion included comments that alcohol could bring into play effects on insulin, glucose, and fat mobilization (however, in the laboratory, such mechanisms tend to increase, rather than decrease, body fat). Also, a reasonable interpretation of the fat tissue decrease related to ‘moderate’ ethanol intake seen in many studies could be an associated decrease in the intake of carbohydrates. One glass of wine substituting for approximately 50 g of glucose could be a reasonable mechanism for shifting the metabolism from lipogenesis to oxidation of lipids. Genetic factors undoubtedly play a role in the effects among individuals.
In summary, this update on the association of alcohol consumption and obesity concludes that most well-done prospective studies show that moderate drinkers do not have an increase in obesity, and in some studies there is even a slight decrease in weight. One possibility is that, especially for wine with meals, satiety may occur earlier and result in less intake of food. However, precise mechanisms for a lack of increase in weight are not known, and the effect could still result from drinkers compensating for their drinks by taking in fewer calories from other sources and perhaps also by being a little more physically active.
Reference: Traversy G, Chaput JP. Alcohol Consumption and Obesity: An Update. Curr Obes Rep 2015;4:122–130. DOI 10.1007/s13679-014-0129-4
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 159: Alcohol as a component of the Mediterranean-type diet; effects on the risk of mortality among diabetics — 17 March 2015
Many scientists have reported on health benefits associated with the traditional diet of much of the Mediterranean area: the primary basis of the diet is on plant-based foods (whole grains, vegetables, fruits), olive oil, moderate wine consumption, and limited intake of meat or dairy products. In 2003, Antonia Trichopoulou and her associates created a scoring system based on the number of components of the Mediterranean Diet (Med-Diet) consumed by subjects, giving a total score to judge the degree that individuals were following a Med-Diet pattern. The score is based on the intake of 7 items (cereal intake, ratio of monounsaturated to saturated fats, vegetables, fruits, nuts, fish, and moderate alcohol), considered to have positive effects, and 2 items (dairy products, meat and meat products) considered to have negative effects. Many groups have found that greater adherence to such a diet (a higher score) is associated with a lower risk of many diseases, and lower mortality. There are limited data on the relative merits of each component of the Med-Diet. In the present paper, the authors attempt to judge the proportion of the protection against mortality that can be attributed to each component of the score.
The authors’ calculations estimated that, in descending order of importance, moderate alcohol consumption (associated with a reduction of 14.7% in the protection against mortality when it was removed from the total score), cereal intake (12.2% reduction), ratio of monounsaturated to saturated fats (5.8%), and consumption of vegetables (5.8%), fruits and nuts (5.2%) and fish (5.0%) lowered mortality risk. Lower intakes of dairy products (reduction of 13.4%) and meat and meat products (3.4%) were also associated with lower mortality. Alcohol has long been known to relate to a lower risk of developing diabetes, and the present study indicates that it is an important factor in reducing the risk of mortality among subjects who have already developed diabetes, as has been shown in previous studies. This study indicates further that the full Med-Diet has very favorable effects on mortality among diabetics.
Forum members considered this to be a well-done attempt to tease apart the relative importance of each component of the Med-Diet as it relates to health outcomes among diabetics. They felt that these researchers from the MOLI-SANI study have published a convincing paper extending the known benefits of the Mediterranean diet to a cohort of type 2 diabetics, a group of subjects at high risk for cardiovascular and all-cause mortality.
There were some questions raised about the precision of the Med-Diet Score, as published and used in this study, in judging the relative contributions of the different dietary constituents, especially because of known complexities in judging the effects of avoiding one particular food when its absence may affect the intake of other foods. And for alcohol, the score used did not permit an evaluation of the role of the pattern of drinking or even the type of beverage consumed, which are known to affect the net effects of drinking on health.
Nevertheless, the results of this study add to an accumulating base of knowledge of the importance of the Mediterranean-type diet in reducing the risk of many health outcomes, including mortality among diabetics.
Reference: Bonaccio M, Di Castelnuovo A, Costanzo S, Persichillo M, De Curtis A, Donati MB, de Gaetano G, Iacoviello L, on behalf of the MOLI-SANI StudyInvestigators.
Adherence to the traditional Mediterranean diet and mortality in subjects with diabetes. Prospective results from the MOLI-SANI study. European Journal of Preventive Cardiology 2015. Pre-publication. DOI: 10.1177/2047487315569409.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 158: Comments on Alcohol Recommendations included in the Scientific Report of the 2015 Dietary Guidelines Advisory Committee – 4 March 2015
Note: The 2015 Dietary Guidelines Advisory Committee (Committee) submitted the Scientific Report of the 2015 Dietary Guidelines Advisory Committee (Advisory Report) to the Secretaries of the U.S. Department of Health and Human Services (HHS) and the U.S. Department of Agriculture (USDA) in February 2015. The purpose of the Advisory Report is to inform the Federal government of current scientific evidence on topics related to diet, nutrition, and health. It provides the Federal government with a foundation for developing national nutrition policy. However, the Advisory Report is not the Dietary Guidelines for Americans policy or a draft of the policy. The Federal government will determine how it will use the information in the Advisory Report as the government develops the 2015 version of the Dietary Guidelines for Americans. HHS and USDA will jointly release the Dietary Guidelines for Americans, 2015 later this year.
Sections of the Advisory Committee report related to alcohol are copied in the full Forum critique, which is available at www.bu.edu/alcohol-forum/critique-158. The full Advisory Committee report can be assessed at the following address: http://www.health.gov/dietaryguidelines/2015-scientific-report/PDFs/Scientific-Report-of-the-2015-Dietary-Guidelines-Advisory-Committee.pdf.
Forum Comments
Members of the International Scientific Forum on Alcohol Research (the Forum) have reviewed the sections of the Advisory Committee’s report that relate to the consumption of alcohol. They consider the report to be well written and a very clear statement on alcohol and health, one that generally reflects current scientific data.
Some Forum members thought that for dietary guidelines, there should have been more emphasis on the inclusion of moderate alcohol consumption as part of a Mediterranean-type diet, which is described in the report as being associated with very favorable health outcomes. The Forum found it interesting that the health problems associated with alcohol receive extensive detailed notice, but substantial favorable effects are barely mentioned. For example, while the comments on the increase in the risk of breast cancer are warranted, there is no mention that moderate alcohol consumption provides substantial protection against ischemic cardiovascular events, despite consistent and extensive data showing that the latter issue has a major public health benefit. Also, lacking any explanatory statements, the public and health professionals may be confused as to the basis for the recommendation that alcohol is “an important component of a healthy lifestyle.” So we recommend that some explanations for the statement, based on the relevant scientific literature, should be included. (Further, the report does not describe the favorable effects of moderate drinking on sociability, stress reduction, and relaxation, which are key reasons why most people consume alcohol in the first place.)
Despite our concerns, given that this is a statement that must get approval by a large number of governmental agencies and a variety of interested parties, it is consistent with current epidemiological data as well as mechanistic studies. The Forum strongly agrees that current scientific evidence indicates that, for mature adults without contraindications to alcohol use, moderate alcohol consumption can be included as a component of a balanced and healthy lifestyle.
For the full critique of the report by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 157: A mistaken interpretation of data relating alcohol to mortality – 20 February 2015
The authors of this paper have carried out a regression analysis to examine the association of reported alcohol consumption with all-cause mortality, dividing their sample into different age groups. They used data from Health Survey for England 1998-2008, linked to national mortality registration data. Their published results show lower risk of mortality (hazard ratios < 1.0 for mortality in comparison with recent non-drinkers and with never drinkers) for subjects in essentially all categories of moderate drinking. However, the authors have interpreted their analyses as indicating that moderate drinking is not associated with all-cause mortality for the vast majority of the population.
Forum members, and many other scientists, have been surprised by the conclusions of the authors, who apparently did not consider basic statistical principles (such as dealing with type-2 errors) in judging their results. The investigators appear to have looked only at p-values and ignored the estimates of effect in their own data, coming to the conclusion of no association between moderate alcohol and total mortality for most age groups. Focusing only on significance testing for estimating effects has been strongly condemned by epidemiologists and statisticians and can lead to inaccurate results.
The paper reflects a gross misinterpretation of the data, not what would be expected in a publication in a leading journal. In other words, the authors’ conclusions are not backed up by their data. A more appropriate headline based on this paper would be “Study supports a moderate protective effect of alcohol against all-cause mortality.” Given the wide media coverage of this article, with striking headlines indicating that moderate drinking does not affect mortality, one Forum reviewer wondered “How can more than 30 years of research in this field be undone by one misguided paper in the BMJ? Once in a while I reflect on how some doctors and journalists interpret scientific papers; they seem to rely more on abstracts and press releases.”
The Forum considers that the conclusions of the authors of this paper are simply not supported by the data provided. Rather, their findings are in accordance with those from previous prospective studies showing that, for all age groups, moderate alcohol consumption is associated with a decrease in all-cause mortality risk.
Reference: Knott CS, Coombs N, Stamatakis E, Biddulph JP. All cause mortality and the case for age specific alcohol consumption guidelines: pooled analyses of up to 10 population based cohorts. BMJ 2015;350:h384 doi: 10.1136/bmj.h384.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 156: The pattern of alcohol consumption and risk of cirrhosis — 10 February 2015
This paper, from a group of experienced investigators in Denmark using data from a large population-based cohort, attempted to judge how drinking pattern affects the risk of a subject developing alcoholic cirrhosis. From a cohort study of 55,917 participants (aged 50–64 years), the authors calculated hazard ratios (HRs) for alcoholic cirrhosis in relation to drinking frequency, lifetime alcohol amount, and beverage type. A total of 342 subjects developed alcoholic cirrhosis. The authors concluded that, in men, daily drinking was associated with an increased risk of alcoholic cirrhosis as compared with less frequent consumption; they also concluded that wine consumption might be associated with a lower risk of alcoholic cirrhosis that associated with the consumption of beer or liquor.
The major concern of Forum reviewers regarding this paper was the use of a diagnosis of “alcoholic cirrhosis” to judge the effects of alcohol on the disease; this was considered a type of circular reasoning. A diagnosis of alcoholic cirrhosis generally requires a history of alcoholism or heavy drinking, and subjects given that diagnosis would essentially be limited to those who were heavy drinkers. Thus, it would be no surprise to find a history of heavy drinking when evaluating alcohol as an exposure.
There was also concern about the implications of the author regarding frequency of drinking. The authors’ described in detail the relation of drinking pattern to liver cirrhosis, differentiating, in particular, effects associated with drinking daily versus drinking on 4-5, or 6 days a week. However, Forum members were concerned that as the overall average amount of alcohol for the daily drinkers exceeded that of those drinking less frequently, it was difficult to know if it was primarily the frequency of drinking (as concluded by the authors) or the total amount of alcohol consumed by subjects. The authors stated that they wanted to “execute evidence-based counselling,” which of course is praiseworthy, but Forum members had difficulty understanding why the effect of drinking 5-6 days/week should differ much from 7 days/week, especially if the usual amount was moderate. Indeed, the investigators state: “The mean alcohol amounts for daily drinkers were somewhat higher compared to those drinking less frequently in each category of alcohol amount, making it difficult to detangle the effect of drinking frequency and alcohol amount.” Forum members noted that the authors conclude that “daily drinking” was associated with increased cirrhosis, but they do not state daily drinking of how many drinks, which would be especially important. The study did not provide reliable data that would support alcohol-free days during the week.
The referent group in this study was made up of subjects reporting < 0 to 14 drinks/week, which would consist of light-to-moderate drinkers, those considered to be “sensible drinkers” in most cultures. Hence, it is no surprise that as subjects reported greater amounts of alcohol in the study, the risk of alcoholic cirrhosis increased. No one advises people to drink more than sensible limits. Further, there was a much higher risk of of cirrhosis among “current abstainers” than in the referent group, undoubtedly indicating that the current abstainers group included many former heavy drinkers.
Overall, the Forum thought that this paper raises, but does not answer, a number of questions about the relation of alcohol to the risk of cirrhosis: (1) Is wine really less liver-toxic than beer or liquor? (2) Should we really tell everyone to have one day each week without wine being included with their meal, or on which to avoid any alcohol? (3) Why is daily drinking, rather than 5 or 6 days per week dangerous for men but tends to be even slightly protective in women regarding liver disease? Because of concerns due to problems with bias from the diagnostic approach, the probability of under-reporting of alcohol consumption, and the lack of biological plausibility, we will need further scientific data to answer these important questions.
Reference: Askgaard G, Grønbæk M, Kjær MS, Tjønneland A, Tolstrup JS. Alcohol drinking pattern and risk of alcoholic liver cirrhosis: A prospective cohort study. Pre-publication. J Hepatol (2015) http://dx.doi.org/10.1016/j.jhep.2014.12.005.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 155: The effects of alcohol consumption on the risk of developing heart failure — 27 January 2015
An analysis of data from the large Atherosclerosis Risk in Communities (ARIC) study evaluated the effects of alcohol consumption at baseline, and the cumulative average intake based on several later assessments during a 24 year follow-up period, on the risk of the development of heart failure (HF). The authors conclude: “In this community, alcohol consumption of up to 7 drinks/week at early-middle age is associated with lower risk for future HF, with a similar but less definite association in women than in men. These findings suggest that despite the dangers of heavy drinking, modest alcohol consumption in early-middle age may be associated with a lower risk for HF.” The authors reported further that the risk of total mortality was higher than that of abstainers for former drinkers and for the heaviest drinkers, but did not demonstrate a “J-shaped” curve for total mortality (i.e., a lower risk for moderate drinkers in comparison with abstainers).
Forum members considered this to be a well-done analysis, with findings for a lower risk of HF among light-to-moderate drinkers consistent with many earlier reports. They noted that these findings may be somewhat affected by the inability of the investigators to include data on the pattern of alcohol consumption (regular moderate intake versus periodic binge drinking of similar total amounts) to disease. It would be expected that the relations between alcohol intake and HF (as well as with total mortality) would be stronger for regular moderate drinkers than for those who consumed their alcohol in binges (even if the total weekly average intake was the same). This could be one reason why a “J-shaped” curve was not seen for the relation of alcohol intake to total mortality in this study.
While coronary artery disease (CAD) is known to be a major precursor of HF, it is not clear from the data presented if the alcohol-HF relation may have differed between subjects with and those without CAD. For the effects of current heavy drinking, the implications from this study are limited because of the small number of such drinkers in this cohort; this was especially the case for women. The authors do not discuss the potential effects on their results of under-reporting of alcohol intake among their subjects; other studies have suggested means for identifying such subjects and ways of adjusting for such.
This study adds support to other large studies, including one just released as a pre-publication (see Addendum), that suggest that moderate alcohol consumption may reduce the risk of the development of heart failure. Some of this putative protective effect surely relates to a decrease in the risk of coronary artery disease among moderate drinkers. Heavy alcohol intake, especially among alcoholics, may increase the risk of both heart disease and heart failure.
Reference: Gonḉalves A, Claggett B, Jhund PS, Rosamond W, Deswal A, Aguilar D, Shah AM, Cheng S, Solomon SD. Alcohol consumption and risk of heart failure: the Atherosclerosis Risk in Communities Study. European Heart Journal, 2015, pre-publication; doi:10.1093/eurheartj/ehu514.
Addendum
Following the preparation of this critique, the pre-publication version of another paper has appeared: Larsson SC, Orsini N, Wolk A. Alcohol consumption and risk of heart failure: a dose–response meta‐analysis of prospective studies. European Journal of Heart Failure 2015; January, 2015. 10.1002/ejhf.228. According to its abstract, this paper is based on “a meta-analysis that included eight prospective studies, with a total of 202,378 participants and 6,211 cases of HF.”
While the Forum has not yet had an opportunity for a careful review of this new paper, the authors’ conclusions appear to provide strong support for the paper by Gonḉalves et al. The authors of the Larsson et al paper conclude their abstract by stating that when carrying out a dose-response meta-analysis, they “observed a non-linear relationship between alcohol consumption and risk of HF. Compared with non-drinkers, the RRs (95% CI) across levels of alcohol consumption were 0.90 (0.84–0.96) for 3 drinks/week, 0.83 (0.73–0.95) for 7 drinks/week, 0.84 (0.72–0.98) for 10 drinks/week, 0.90 (0.73–1.10) for 14 drinks/week, and 1.07 (0.77–1.48) for 21 drinks/week. Alcohol consumption in moderation is associated with a reduced risk of HF.”
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 154: Effects of changes in alcohol consumption on risk of dementia among elderly women — 12 January 2015
A number of prospective studies have shown that moderate drinkers are at lower risk of developing dementia or cognitive impairment than abstainers or heavy drinkers; possible mechanisms of a putative beneficial effect could relate to a reduction in the risk of cerebral atherosclerosis, a direct effect on cognition through the release of acetylcholine in the hippocampus, the antioxidant effects of alcohol and polyphenols, or from the down-regulation of inducible nitric synthase and up-regulation of endothelial nitric oxide synthase.
The present study is based on 1,309 women who were aged 65 years or greater at the beginning of a 20-year follow up, during which they had at least two assessments of cognitive function. At baseline, 42.1% of the women reported that they were “light” drinkers (>0 – < 3 drinks/week, 13.8% reported “moderate” consumption (3-7 drinks/week), and 3.6% reported “heavy” consumption (> 7 drinks/week). By the 20th year of follow up, 17.5% of the previously normal women had developed dementia (by several standard tests, a previous diagnosis of dementia, or nursing home residence), and 22.7% had developed mild cognitive impairment (MCI). Thus, a total of 40.2% of the women had developed some degree of cognitive impairment.
In this paper, there was no suggestion that the small percentage of women (5%) who increased their intake changed their risk of cognitive impairment (fully adjusted OR=1.04, 95% CI 0.56, 1.95), when compared with women who did not change their intake or decreased it only slightly. However, for women who decreased their intake by > 0.5 drinks/week, the authors suggest that there was an increase in risk of cognitive impairment, with unadjusted results showing an OR of 1.34, 95% CI: 1.05-1.70. However, with full adjustment for confounders, the effect was attenuated: OR = 1.26, 95% CI 0.98, 1.61; p = 0.07.
Forum members noted that the reasons that some women changed their drinking habits could not be ascertained (as is usually the case in observational studies). Alzheimer’s dementia has a long prodromal period and latent pathology could precede/contribute to a decrease in drinking. They were also concerned about the lack of cognitive characterization of the cohort at baseline. Thus, Forum members had some difficulty in knowing how to interpret the finding of a lack of association of baseline drinking with risk of cognitive impairment 20 years later given that we are not told whether the groups defined on baseline drinking differed from each other in age or other health risk factors. For those who changed their intake, decreasing drinking by > 0.5 glasses/week may be very different for someone drinking > 7 drinks/week than in someone drinking < 1 drink/week. It would have been better if the authors somehow took baseline drinking into account when assessing effects of change in drinking.
There was also the concern that any observational study that relates the effects of changes in alcohol intake on the risk of a disease without somehow taking earlier drinking into account may give paradoxical results. (An example is the relation of obesity to cardiovascular disease; overall, there is an increase in risk for obese individuals but when changes in intake among older people are evaluated, the result is often no effect or even a protective effect: the “obesity paradox.”) The same has been shown for the relation of usual alcohol intake and changes in intake to other diseases.
Thus, while the analyses were done appropriately, Forum members had concerns about whether the findings presented in this paper justify the wisdom of the authors in stating in their conclusion that “Women in their ninth and tenth decade of life who decrease alcohol use may be at risk of cognitive impairment.” As one reviewer stated: “Knowing from other studies that light to moderate alcohol consumption is good for the heart and the head, I would not advise elderly people to stop drinking. However, the conclusions of the authors that this paper shows that decreasing alcohol consumption increases the risk of cognitive impairment in elderly women may be true, but are not justified because the design, analysis, and results of the study do not permit such a statement.”
Reference: Hoang TD, Byers AL, Barnes DE, Yaffe K. Alcohol Consumption Patterns and Cognitive Impairment in Older Women. Am J Geriatr Psychiatry 2014; 22:1663-1667.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 153: Moderate alcohol intake may lower the risk of developing diabetes among obese subjects — 11 December 2014
This case-control study compared the risk of having a high level of hemoglobin A1c, a measure of hyperglycemia, and of the waist/height ratio, a measure of obesity, according to reported alcohol consumption. Overall, subjects reporting an average alcohol intake between 22 and 44 g/day (the equivalent of between about 2 and 4 typical drinks) had lower levels of hemoglobin A1c and lower weight/height values. The author concludes: “The associations between obesity and hyperglycemia were weaker in light-to-moderate drinkers than in nondrinkers. Thus, light-to-moderate drinking may reduce the impact of obesity on the risk for diabetes.”
While Forum reviewers had some concerns about the first analytic approach given in the paper, they agreed that the second approach, in which specific levels of A1c were reported according to alcohol intake and measures of obesity, had merit. These latter data clearly indicate that hyperglycemia is affected both by obesity (which increases the risk) and alcohol intake (which decreases the risk); hyperglycemia is the leading factor associated with the development of diabetes mellitus.
A therapeutic implication of this study may be that obese subjects who are moderate drinkers should not be advised to stop their alcohol consumption. The results, along with a large amount of other research currently available, also suggest that obese subjects who do not drink and have no contraindications to alcohol consumption should be informed that consuming moderate amounts of alcohol may be associated with a reduction in their risk of developing diabetes.
Reference: Wakabayashi U. Light-to-Moderate Alcohol Drinking Reduces the Impact of Obesity on the Risk of Diabetes Mellitus. J Stud Alcohol Drugs 2014;75:1032–1038.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 152: Specific genetic factors modify the reduction in heart disease risk from alcohol consumption — 27 November 2014
It has long been known that genetic and other environmental factors modify the association between alcohol consumption and a variety of diseases, especially coronary heart disease (CHD). Foremost among these modifying factors are genes that affect alcohol metabolism, age (effects seen only in older individuals), and drinking patterns (regular moderate versus binge drinking). Also, certain cholesteryl ester transfer protein (CETP TaqIB) polymorphisms, that relate to HDL-cholesterol activity, may interact with alcohol consumption for their effects on the risk of CHD. In the present study, the investigators have carried out a population-based case-control study among subjects in southwest Sweden to determine if there was an interaction between CETP genotypes and alcohol consumption for its effects on the risk of CHD. The authors conclude that a significant reduction in the risk of CHD from moderate drinking was seen only among the 18.6% of their subjects who had a particular CETP polymorphism.
Forum members considered this to be an interesting paper, but had some questions about the selection of cases, as they included not only new cases of CHD but subjects “who had an exacerbation of previously diagnosed coronary heart disease;” this makes it somewhat difficult to compare their results with other papers. Further, despite a large number of potential “control” subjects from their base population, the controls chosen were considerably younger than the cases and had different medical histories. While they adjusted for some of these factors in their analysis, residual confounding remains possible.
The major concern of Forum members was the broad conclusion of the authors (that only a small proportion of the population will show any cardio-protective effects of moderate drinking) based on such a small number of subjects. For example, among their “intermediate” category of drinkers with the supposedly “protective” CETP polymorphism, there were only 13 cases of CHD. Further, a number of previous large studies have had quite conflicting results regarding the effects of CETP polymorphisms on the alcohol-CHD association. While this paper adds information on one (of many) factors that affect the association between alcohol consumption and CHD, larger studies in different populations will be needed to determine the overall importance of this particular genetic polymorphism.
Reference: Mehlig K, Strandhagen E, Svensson P-A, Rosengren A, Torén K, Thelle DS, Lissner L. CETP TaqIB genotype modifies the association between alcohol and coronary heart disease: The INTERGENE case-control study. Alcohol 2014;48:695e700.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 151: “Fetal alcohol syndromes” result from multiple maternal factors during pregnancy — 20 November 2014
Excessive maternal alcohol consumption during pregnancy (especially among women with alcohol dependency) is known to markedly increase the risk of the fetus showing a group of developmental disorders defined as fetal alcohol spectrum syndrome (FASD), with the most serious form being fetal alcohol syndrome (FAS). The present paper attempts to identify maternal risk factors for FASD and FAS, but the authors report that there were not enough data to carry out a formal meta-analysis. They do, however, describe important maternal risk factors that have been reported in the literature to relate to these syndromes. The more frequent maternal conditions related to the risk of FASD or FAS include older age of mother, lower educational level, family relatives who abuse alcohol, little prenatal care, and a more severe pattern of alcohol consumption in general and particularly during pregnancy. They emphasize that “FAS is a multifactorial condition, and it is potentiated by complex relationships among several factors, social and biological.”
Forum reviewers considered this to be a well-done analysis presenting important and balanced information on these syndromes. Forum members agreed that many genetic and environmental factors, in addition to heavy alcohol consumption, may contribute to the development of these syndromes (e.g., certain genetic polymorphisms, inadequate pre-natal care, poverty, low education, familial alcoholism, use of illicit drugs, etc.).
Given the permanent nature of many of the defects found in FASD and FAS, and limited therapeutic options, it is important that the focus should be on the prevention of these syndromes. If they are to be prevented, it will be necessary to intervene among high-risk women, either prior to or early during pregnancy. Better knowledge of all the factors involved will help facilitate interventions that may help prevent these serious conditions.
Reference: Esper LH, Furtado EF. Identifying maternal risk factors associated with Fetal Alcohol Spectrum Disorders: a systematic review. Eur Child Adolesc Psychiatry (2014) 23:877–889; DOI 10.1007/s00787-014-0603-2.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 150: A new meta-analysis on the relation of alcohol consumption to the risk of ischemic heart disease — 6 November 2014
This meta-analysis is from authors who in the past have tended to argue that the demonstrated inverse association between moderate alcohol consumption and ischemic heart disease (IHD) shown in most studies is due to confounding by other lifestyle factors. However, in this paper, they come to the conclusion (in their words): “Results from our quantitative meta-analysis showed that drinkers with average intake of < 30 g/day and no episodic heavy drinking had the lowest IHD risk (relative risk = 0.64, 95% confidence interval 0.53 to 0.71). Drinkers with episodic heavy drinking occasions had a risk similar to lifetime abstainers (relative risk = 1.12, 95% confidence interval 0.91 to 1.37).”
The conclusions of the authors thus not only support a “J-shaped” curve for alcohol consumption and IHD but provide additional support suggesting that the effect may be causal, i.e., related to the alcohol consumption and not to other associated lifestyle factors. They state: “For drinkers having one to two drinks per drinking day without episodic heavy drinking, there is substantial and consistent evidence from epidemiological and short-term experimental studies for a beneficial association with IHD risk when compared to lifetime abstainers. The alcohol-IHD relationship fulfills all criteria for a causal association proposed by Hill.”
It is clear from epidemiologic studies that moderate drinkers may exhibit moderation in other lifestyle factors (such as not smoking, eating a healthy diet, etc.). Indeed, there is aggregation of healthy lifestyle factors that must be considered when judging how a single factor (such as moderate drinking) relates to disease outcomes. This meta-analysis suggests that other lifestyle factors do not explain the lower risk of IHD found to occur among moderate drinkers. In fact, increasingly, moderate drinking is found to be an independent (and rather important) lifestyle factor that lowers the risk of cardiovascular disease, regardless of other factors. Such protection is not seen when drinking is more than moderate, defined in this paper as an average of 30 grams or more of alcohol per day, the equivalent of about 2 ½ to 3 typical drinks.
Reference: Roerecke M, Rehm J. Alcohol consumption, drinking patterns, and ischemic heart disease: a narrative review of meta-analyses and a systematic review and meta-analysis of the impact of heavy drinking occasions on risk for moderate drinkers. BMC Medicine 2014;12:182.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 149: The association of alcohol consumption with the risk of death from colorectal cancer — 28 October 2014
Data from prospective cohort studies on the association between alcohol consumption and the occurrence of colorectal cancer (CRC) are conflicting, with some suggesting an increase in risk while others failing to show such an effect. There are little data on the effects of alcohol consumption on the risk of mortality from CRC. The present study is based on a meta-analysis of data from nine cohort studies (with a total of more than two million subjects) to judge how the level of alcohol intake relates to CRC mortality. A total of almost 4,000 deaths from CRC were recorded. The conclusions of the authors are that the consumption of ≥ 50 grams of alcohol (about 4 typical drinks or more) per day increases the risk of death from CRC modestly [RR 1.21 (95% CI 1.01, 1.46)], but “light” drinking (≤ 12.5 g/day) or “moderate” drinking (12.6-49.9 g/day) do not increase the risk of CRC death. In fact, they state that their data support a “J-shaped” relation between alcohol intake and CRC mortality (i.e., a slight decrease in mortality associated with light drinking but an increased risk with heavier drinking).
Forum members considered this to be a well-done analysis. They noted the inability of the authors to evaluate differences in effect according to type of beverage consumed, the pattern of drinking, or the underlying folate levels of subject, all of which probably modify such a relation. The results are in line with earlier reports on alcohol and breast cancer, where alcohol appears to increase the incidence of the disease but does not increase mortality. For most diseases, including colorectal cancer, there may a J-shaped effect on mortality: a reduction in risk for light-to-moderate drinking but an increase with heavier drinking.
Overall, the present meta-analysis supports a finding of increased risk of death from colorectal cancer from heavy drinking. However, it shows rather convincingly that light to moderate amounts of alcohol do not increase the risk of death from this disease, probably because of the protective effects of moderate drinking on cardiovascular disease, a more common cause of mortality.
Reference: Cai S, Li Y, Ding Y, Chen K, Jin M. Alcohol drinking and the risk of colorectal cancer death: a meta-analysis. European Journal of Cancer Prevention 2014;23:532–539.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 148: Alcohol and liver cancer — 24 September 2014
Hepatic cirrhosis frequently precedes the development of liver cancer, and excessive alcohol consumption is known to be one cause of cirrhosis. The investigators in the present study carried out a meta-analysis to evaluate the association of alcohol consumption with liver cancer. They used data from 19 prospectively studied cohorts with a large total number of cases: 4,445 incident cases and 5,550 deaths from liver cancer.
The analysis from this large study indicates that liver cancer is related to heavier alcohol intake, but not to light-to-moderate drinking (with the latter defined in this study as < 3 typical drinks per day). The authors conclude: “This systematic review suggests a moderate detrimental role of consumption of 3 or more alcoholic drinks per day on liver cancer, and a lack of association with moderate drinking.”
Forum reviewers considered this to be a well-done analysis with appropriate statistical methodology. While the authors were unable to test the potential effects of pattern of drinking (regular moderate versus binge drinking), the type of beverage (wine or other beverages), or potential effects of obesity (with the latter being a key factor associated with the most common type of liver disease in the US, non-alcoholic fatty liver disease), the results of this study support most other research indicating that more than moderate drinking increases the risk of cirrhosis and liver cancer. However, the findings of no effect from what the authors considered “moderate” drinking (< 3 drinks/day, which exceeds the guidelines for most countries), also fits with another recent meta-analysis showing no increase in risk of liver cancer to be associated with light drinking.
There are many adverse health effects of heavy alcohol consumption. Liver cirrhosis, which frequently precedes the development of liver cancer, is one such potential outcome. On the other hand, this study suggests that moderate alcohol intake does not increase the risk of liver cancer.
Reference: F. Turati, C. Galeone, M. Rota, C. Pelucchi, E. Negri, V. Bagnardi, G. Corrao, P. Boffetta, C. La Vecchia. Alcohol and liver cancer: a systematic review and meta-analysis of prospective studies. Annals of Oncology 2014; advance publication; doi:10.1093/annonc/mdu020
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 147: Association of alcohol intake with different types of breast cancer — 11 September 2014
The present study was based on a large number of women participating in a clinical trial (enhanced screening for certain cancers versus routine care) focusing on prostate, lung, colorectal, and ovarian cancer. During a follow-up period averaging about 9 years, a total of 1,905 women were diagnosed with invasive breast cancer. The analyses showed that an increase in cancer risk was associated with alcohol intake for estrogen and progestin positive (ER+/PR+) tumors, but not for other histologic types of breast cancer. The increased risk was predominantly seen among PR+ cancers, as there was no evidence of an increase in risk from alcohol for women with ER+/PR- tumors. An association with the highest category of alcohol intake was noted for ductal (the most prominent type), lobular, and mixed ductal/lobular tumors, but a clear dose-response curve was not present. The authors conclude that alcohol consumption is not associated with all breast cancer subtypes, and that future research should include precise definition of subtypes of cancer.
Forum reviewers considered this to be a well-done analysis. There were some questions about the characteristics of the participants in the study that could affect generalizability of the results. For example, the cohort of women in this study were more highly educated, more likely to have a positive family history of breast cancer, to be smokers, and perhaps more obese that the general population. Of more concern, however, was the lack of ability to evaluate a number of other potential risk factors for breast cancer: folate levels and other dietary factors, the pattern of drinking (regular versus binge), potential changes in drinking after the baseline measurement, type of beverage, or the HER2 status of tumors. The finding in the paper of an increase in breast cancer risk, in comparison with non-drinkers, even for women reporting less than ½ drink per week (RR 1.15, CI 0.97, 1.39) and 0.5 – < 1 drink per week (RR 1.25, CI 1.03, 1.53), suggests that residual confounding must also be considered; it is unlikely that such small amounts of alcohol would have a physiological effect.
Overall, the present study shows a significant increase in the risk of breast cancer among women in a cancer prevention trial who, at baseline, indicated that they were consuming even less than 1 drink/week. The increase was exclusively in ER+/PR+ tumors, but not in ER+/PR- or ER-/PR- tumors.
In future research on this association, information on folate levels and drinking pattern, and especially on type of beverage consumed and on evidence of under-reporting of alcohol intake, will be important in better defining how alcohol consumption relates to the risk of breast cancer. While the results of this study are important in studying the etiology of breast cancer (as alcohol appears to relate only to hormone receptor positive tumors), the findings may not necessarily help individual women know how their alcohol consumption by itself may relate to their overall risk of the disease.
Reference: Falk RT, Maas P, Schairer C, Chatterjee N, Mabie JE, Cunningham C, Buys SS, Isaacs C, Ziegler RG. Alcohol and Risk of Breast Cancer in Postmenopausal Women: An Analysis of Etiological Heterogeneity by Multiple Tumor Characteristics. Am J Epidemiol 2014; advance access; DOI: 10.1093/aje/kwu189.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 146: Alcohol and the risk of abdominal aortic aneurysm — 4 September 2014
The large majority of prospective epidemiologic studies on the effects of alcohol consumption and the risk of coronary heart disease and stroke have shown a significant reduction in risk for moderate drinkers. There have been few studies relating alcohol intake to the development of abdominal aortic aneurysm (AAA), and results have been inconsistent. The present study is based on two very large population-based cohorts in Sweden that were followed prospectively for the clinical development of AAA (identified by radiography, surgical repair, or death resulting from rupture). There were more than 1,200 cases identified during a 14-year follow-up period. The results of this study suggest that moderate drinking is associated with a lower risk of AAA, with the beneficial effects primarily among consumers of beer or wine.
Forum reviewers were unanimous in considering this to be a well-done analysis, with unbiased estimates of effect of alcohol on the risk of aneurysm. The reduced risk of AAA among moderate drinkers was similar to that seen for common manifestations of atherosclerosis, especially coronary heart disease and ischemic stroke. Reviewers were uncertain why only consumers of wine and beer showed a beneficial effect, but not consumers of spirits: this could be explained by the polyphenols present in wine and beer that have been shown to be anti-inflammatory, anti-oxidant, and anti-platelet aggregation (all mechanisms that may relate to the development of AAA). However, residual confounding could also play a role.
It was noted that the percentage of the population with hypertension, probably the most important risk factor for AAA, was much lower than is common in most industrialized countries, but the degree to which this affected the results cannot be known. While alcohol is known to increase blood pressure, some large studies suggest that an increase occurs only with more than light-to-moderate drinking. Further, there were few very heavy drinkers (the highest category of alcohol was an average consumption of ≥1 drink/day among women and ≥2 drinks/day among men), so this study could not assess whether or not large amounts of alcohol might increase risk of AAA.
There have been a very limited number of studies on alcohol intake and aortic aneurysm. While this study suggests a slight decrease in occurrence of AAA with moderate wine and beer intake, it will be important for other large studies to evaluate this association. Additional studies on polyphenol intake and occurrence of AAA will also be useful.
Reference: Stackelberg O, Björck M, Larsson SC, Orsini N, Wolk A. Alcohol Consumption, Specific Alcoholic Beverages, and Abdominal Aortic Aneurysm. Circulation 2014;130:646-652.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 145: Alcohol consumption and brain structure on MRI scans — 25 August 2014
While numerous prospective epidemiologic studies have provided evidence that light-to-moderate amounts of alcohol reduce the risk of dementia and heavy drinking increases the risk, there are few studies on the effects of alcohol on brain structure assessed by magnetic resonance imaging (MRI). The present study is a cross-sectional evaluation between reported alcohol intake and MRI-assessed brain structure among 589 multi-ethnic community residents of New York. Total brain volume (TBV), white matter hyperintensity volume (WMHV), and presence of infarcts were derived from MRI scans when subjects were, on average, 80 years of age..
A key finding of this analysis is that, in comparison with non-drinkers, light-to-moderate alcohol intake (up to an average of 1 drink/day for women or 2 drinks/day for men, which was reported in 31% of their subjects) was associated with larger TBV (i.e., less brain atrophy). The effect was primarily among consumers of wine rather than of beer or liquor. Significant associations were not found for alcohol or for specific beverages for other measures of brain structure (WMHV or presence of infarcts).
Forum reviewers considered this to be an appropriate analysis that was able to consider many of the potential confounders of such an association. On the other hand, it was not a large study and was based on a cross-sectional analysis; thus it cannot be used to judge causation (e.g., it is possible that people with larger brains to begin with were more likely to consume wine or total alcohol, rather than their alcohol intake increasing their brain size).
Data from many previous studies have shown that moderate alcohol intake lowers the risk of developing clinical signs of cognitive decline and of dementia. Such a finding has led Forum members to be of the opinion that instructing the elderly to refrain from light-to-moderate amounts of alcohol may not be wise. Although prospective studies may show that the decrease in the risk ratio for dementia (comparing drinking with abstainers) tends to be less among the elderly than among middle-aged subjects, the absolute risk of dementia increases markedly with age. Thus, any intervention that lowers the risk of cognitive impairment will have a much greater impact in older people as compared with younger people.
Given the inconsistences in previous reports on the effects of alcohol on brain structure, we must conclude that while this study suggests that there might be a beneficial association between alcohol (especially wine intake) and brain size, such a relation is not definitive. An inverse relation between moderate drinking and clinical evidence of dementia, however, has received support from a large number of prospective epidemiologic studies; it may be a better association for us to use when advising the elderly regarding alcohol consumption.
Overall, scientific data indicate that, for elderly subjects without contraindications to alcohol, small amounts of wine or other alcoholic beverage consumed regularly may reduce the risk of dementia and other diseases of ageing. As stated by Michel de Montaigne many centuries ago: “ . . . drinking is the almost last pleasure that the years steal from us.”
Reference: Gu Y, Scarmeas N, Eaton Short E, Luchsinger JA, DeCarli C, Stern Y, Manly JJ, Schupf N, Mayeux R, Brickman AM. Alcohol intake and brain structure in a multiethnic elderly cohort. Clinical Nutrition 2014;33:662e667.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 144: Alcohol consumption and risk of endometrial cancer — 18 August 2014
Most epidemiologic studies have shown that moderate alcohol consumption does not increase the risk of uterine cancer, and some have suggested an inverse or J-shaped relation. In a new analysis from the Nurses’ Health Study, with 68,067 female participants aged 34–59 years in 1980, investigators have related repeatedly assessed long-term alcohol intake, and related the cumulative average intake over time to the risk of invasive uterine cancer. A total of 794 cases of invasive endometrial adenocarcinoma were identified over a 30 year follow-up period.
The authors report an inverse association among alcohol drinkers (multivariable RR=0.81; 95% CI: 0.68–0.96) compared with nondrinkers. Women with an intake of <5 g per day (an average of approximately one-half drink per day) had a 22% lower risk of endometrial cancer (multivariable RR=0.78; 95% CI: 0.66–0.94), with no further decrease evident from larger amounts of alcohol. In comparison with non-drinkers, the relative risk was similarly reduced for consumers of more than 30 grams of alcohol per day, but the number of subjects in this category was small, and a potential increase in risk from heavy drinking could not be adequately assessed in this study.
Forum members considered this to be a very well-done prospective study, with clear and biologically plausible results. By having repeated assessments of alcohol, an estimate of long-term average consumption was possible. The approximately 20% lower risk of uterine cancer among subjects with light alcohol intake remained statistically significant after multivariate adjustments for known potential confounders. Reviewers agreed with the authors that a potential mechanism for the association could be a reduction in insulin concentrations and improved insulin sensitivity that have been shown to occur with moderate alcohol consumption. Further, the frequently demonstrated inverse relation for alcohol with obesity may also play a mechanistic role. Overall, this study adds to accumulating scientific data showing that moderate drinking does not increase the risk of uterine cancer, and probably is associated with a reduction in risk
Reference: Je Y, DeVivo I, Giovannucci E. Long-term alcohol intake and risk of endometrial cancer in the Nurses’ Health Study, 1980–2010. British Journal of Cancer 2014;111:186–194; doi: 10.1038/bjc.2014.257.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 143: A Mendelian randomization assessment of alcohol and cardiovascular disease — 20 July 2014
Using a very large dataset from subjects of European descent, the authors have carried out a Mendelian randomization analysis to estimate the effects of alcohol consumption on cardiovascular disease (CVD), using as the instrumental variable an uncommon allele affecting alcohol metabolism, the ADH1B rs1229984 variant. People with this variant are unusually sensitive to alcohol (developing flushing and other uncomfortable symptoms from alcohol) and it has been well demonstrated that they are less likely than people without this variant to consume alcohol, and are unlikely to be heavy drinkers. The authors conclude that since the 7% of their subjects with the uncommon allele had less cardiovascular disease, this indicates that alcohol consumption is unrelated to CVD.
Forum members agree that the analyses were done correctly, but strongly disagree with the premise of the study and the conclusions of the authors, and consider the genetic factor chosen as inappropriate to use as the instrumental variable in Mendelian randomization. The gene studied explains only a fraction of alcohol consumption in the population (not stated in the paper) and it may have effects on CVD beyond those explained by alcohol consumption. Thus, this ADH1b allele violates the assumptions required for a variable for Mendelian randomization and would be inappropriate for judging the effects of alcohol on CVD. Further, in the present study, the authors report little relation of their estimate of alcohol consumption with HDL-cholesterol, while essentially all observational studies, clinical trials, and experimental studies have shown that alcohol is an important determinant of HDL. This further suggests that the use of the ADH1B allele provides an inadequate estimate of alcohol consumption.
Even without the weakness of the allele chosen to reflect alcohol effects, conclusions derived from Mendelian randomization in general are heavily dependent on the assumption that the instrumental chosen is appropriate, of which you can rarely be confident. Forum reviewers consider this method to be a very blunt instrument and subject to considerable bias for variables that are weakly correlated with exposure and not true instruments.
Some reviewers were concerned by the conclusion of the authors that this Mendelian randomization paper shows that all persons should drink less; this does not necessarily mean for people to completely avoid drinking. The protection of moderate drinking against CVD that is generally observed shows a non-linear gradient: it is better manifested at a low alcohol consumption, while it is less strong as the consumption levels rise above optimum and finally disappears and is transformed into harm with heavy alcohol consumption. This would be in agreement with the conclusions of most prospective studies and meta-analyses that drinking alcohol at low doses offers the best protection against CVD, as there is a J-shaped curve.
Reference: Holmes MV, Dale CE, Zuccolo L, et al (a total of 155 authors). Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. BMJ 2014;349:g4164 doi: 10.1136/bmj.g4164.
For the full critique of this study by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 142: A large study of alcohol consumption and mortality — 14 July 2014
The large European Prospective Investigation into Cancer and Nutrition Study (EPIC) has released a new analysis of the relation of alcohol consumption to mortality. The study concluded that alcohol use was positively associated with overall mortality, alcohol-related cancers, and violent death and injuries, but marginally to cardiovascular disease, and that absolute risks of death observed in EPIC suggest that alcohol is an important determinant of total mortality.
There is no question that heavy alcohol consumption, especially when associated with smoking, increases the risk of a number of upper aero-digestive cancers that are commonly referred to as “alcohol-related cancers.” In the present study, the authors have also included in this group a number of other cancers that may be related less directly to the effects of alcohol; these include colorectal cancer and female breast cancer which, because they are so much more common, make up the large majority of cancers “related to alcohol.” Forum members consider the EPIC study to be an important source of data on cancer, but had a number of questions about the analysis and especially about the conclusions of the authors.
Major weaknesses of the study are that an assessment of alcohol intake was obtained only at a baseline visit, with no further assessments during a follow-up period averaging 12 years, and especially, no information was available on the pattern of drinking of subjects (e.g., regular moderate versus binge drinking). Further, Forum members noted that there was no discussion of the effects of under-reporting of alcohol, which has been shown to markedly affect health effects of alcohol intake in epidemiologic studies. In fact, recent large studies show that most of the cases of cancer that appear to relate to “light-to-moderate drinking” actually relate to underreporting of consumption by subjects who are found, from other collected medical data, to be heavy users or abusers of alcohol.
The authors focus on “extreme drinkers,” which consist of women who consume (≥30 g/day) or men who consume ≥60 g/day. They do not point out that only 2.4% of the women in this study consumed at this level, and little attention is given to the fact that almost all of the women were non-drinkers or light-moderate drinkers. From the data presented in the paper, there is a clear U-shaped curve among women: the highest risks for total mortality were in the abstainers (a 26% increase over the referent group of light drinkers) and the very small number of women in the highest drinking category (a 27% increase).
For men, 8.2% were in the highest drinking category, reporting an average consumption of ≥ 60 g/d (5 – 6 typical drinks). For men, there was generally a U-shaped curve, with lower death rates for light to moderate drinkers. However, the heaviest drinkers had the highest risk of death for overall mortality and for deaths from cancers and other causes of death. For both men and women, at every level of drinking, smokers had an increased risk of death in comparison with non-smokers.
Some reviewers were also concerned about the unusual categorization of alcohol intake used in the study. Referring to subjects reporting 0.1 – 4.9 g/day as “moderate drinkers” is a strange designation for an alcohol intake that in most other studies would be named as light or very modest, and may lead to confusion in interpreting results. (Most studies would define 5 – 14.9 g/day as light to moderate drinkers, and this group is not given a name in this study).
Overall, this study tends to show a U-shaped relation between alcohol consumption and mortality. The data presented focus primarily on the highest categories of drinking, levels that are well known to relate to many diseases and mortality. For truly light-to-moderate consumption, however, there is overwhelming epidemiologic data that such drinking relates to lower mortality risks, and the present study does not contradict such an association.
Reference: Ferrari P, Licaj I, Muller DC, et al (36 other authors). Lifetime alcohol use and overall and cause-specific mortality in the European Prospective Investigation into Cancer and nutrition (EPIC) study. Pre-publication; BMJ Open 2014;4:e005245. doi:10.1136/bmjopen-2014-005245
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 141: A world-wide study of alcohol consumption and the risk of myocardial infarction — 3 July 2014
The authors report on data collected in the INTERHEART Study, a large international collaborative project of individuals with a first myocardial infarction (MI) and age- and sex-matched controls from 52 countries in Asia, Europe, the Middle East, Africa, Australia, North and South America. Included were nations with very divergent lifestyles, religions, degrees of development, and drinking habits. The authors attempted to provide a “world-wide” overview of the relation of alcohol consumption to the risk of myocardial infarction (MI). However, they were forced to use a case-control design, a type of study with many opportunities for bias and one that prevents determination of a causal relation. Further, the lack of detailed data on the amount of alcohol consumed by individuals weakens their results.
While the authors state that their study shows that low levels of alcohol use are associated with a moderate reduction in the risk of MI, they point out differences in results in different countries. Forum members considered that these large differences severely limit their ability to use such a dataset to provide overall conclusions on alcohol and MI. For example, only 1% of the non-drinkers in this study came from W. Europe and 1% from North America, while more than 70% of the non-drinkers came from the Middle East or Asia. With such diversity (e.g., almost all the abstainers were from one area), it is not possible to adequately “adjust” for such regional differences in analysis.
The authors also studied how alcohol consumption shortly prior to (in the 24 hours before) the occurrence of a MI relate to the short-term risk of MI. While their results show an increased risk for heavy drinking immediately prior to an MI (a result that differs from that of some previous studies), they admit analytic problems, stating: “Thus there remains uncertainty over the risk of MI in the period immediately following alcohol intake.”
Previous large prospective cohort studies (a type of epidemiologic study that decreases the risk of recall bias regarding alcohol intake and certain types of confounding) have clearly shown an inverse relation between moderate alcohol consumption and MI. Most of the previous studies have provided much more detailed data on alcohol exposure than did the present study. The authors realized many of these problems, and warn against using their results to make overall conclusions about the association between alcohol and MI from their paper. They state: “The associations observed between alcohol use and MI may be accounted for by unmeasured confounders such as genetic differences between populations, variation in alcohol type or preparation, and heterogeneity of social context. The present analysis should therefore prompt further research to clarify the nature of the association between alcohol use and MI.” Unfortunately, the conclusions presented in the abstract and in the do not mention such problems.
Some Forum members worried that many readers of the paper will be left with a very misleading impression of the relation of alcohol consumption to myocardial infarction, and will not be aware that the conclusions trumpeted in the abstract are compromised by weak data. Overall, members considered that the present paper adds little to our knowledge about the risks and benefits of alcohol in relation to cardiovascular disease.
Reference: Leong DP, Smyth A. Teo KK, McKee M, Rangarajan S, Pais P, Liu L, Yusuf S, on behalf of the INTERHEART investigators. Patterns of Alcohol Consumption and Myocardial Infarction Risk: Observations from 52 Countries in the INTERHEART Case-Control Study. Circulation 2014 (pre-publication) DOI: 10.1161/CIRCULATIONAHA.113.007627.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 140: A meta-analysis shows that light alcohol consumption is associated with a reduced risk of stroke, while heavier drinking may increase risk — 5 June 2014
Most epidemiologic studies have shown a reduction in the risk of ischemic stroke (and total stroke, as ischemic stroke is by far the most common type in western countries) to be associated with light to moderate alcohol consumption. The present study, a meta-analysis, was based on 27 prospective studies; the authors categorized a reported intake of <15 g/day as light consumption, and 15-30 g/day as moderate consumption. The authors point out differences (greater smoking, larger amounts of alcohol) between Chinese subjects and those from other countries, which may explain some of the differences shown between alcohol’s effects in the different countries. They also point out that they had no data on the pattern of drinking (regular, moderate intake versus binge-drinking) or on the type of alcoholic beverage consumed.
The key results of the study are a significant 15% reduction in total stroke for low alcohol intake, no effect for moderate, and a 20% increased risk for heavy alcohol consumption (RR 1.20, 95% CI 1.01, 1.43). Analyses were also done according to type of stroke: for ischemic stroke and stroke mortality there were decreases for low alcohol intake, but no significant effects of either moderate or heavy intake. For hemorrhagic stroke, the RR for subjects reporting heavy alcohol intake was higher than that of abstainers, but none of the differences between drinkers and non-drinkers was statistically significant.
This meta-analysis supports previous findings of a decrease in the risk of most strokes with light drinking and possibly an increase in the risk for heavy drinking. Forum members generally agreed with the conclusions of the authors: “Low alcohol intake is associated with a reduced risk of stroke morbidity and mortality, whereas heavy alcohol intake is associated with an increased risk of total stroke. The association between alcohol intake and stroke morbidity and mortality is J-shaped. An alcohol intake of 0-20 grams/day is associated with decreased rates of stroke morbidity and mortality.”
Reference: Zhang C, Qin Y-Y,Chen Q, Jiang H, Chen X-Z, Xu C-L, Mao P-J, He J, Zhou Y-H. Alcohol intake and risk of stroke: A dose–response meta-analysis of prospective studies. Int J Cardiol 2014; pre-publication; http://dx.doi.org/10.1016/j.ijcard.2014.04.225.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 139: Does adjustment for stress levels explain the protective effect of moderate drinking on the risk of mortality? — 18 May 2014
An inverse association between moderate alcohol consumption and total mortality has been reported in most prospective epidemiologic studies, even after adjustments for all known potential confounders. The present analysis was carried out specifically to focus on the effects of psychosocial stressors on the association, using a large population-based German cohort from the WHO MONICA study. No alcohol intake was reported by 15.3% of males and 41.8% of females; “moderate drinking” was defined as an average intake of 0.1-39.9 g/day for men (making up 51.1% of the cohort) and 0.1 – 19.9 g/day for women (38.8% of the cohort). Although data are not presented, there were apparently few women in the higher drinking categories.
The authors related the effects of including, or not including, in their equations a large number of psychosocial stressors, including educational level, occupational status, several indices of social support, job strain symptoms, depressive symptoms, somatic symptoms, and self-perceived health status, in the estimation of the effects of alcohol consumption on risk of total mortality over an average follow-up period of 12 years. In their analyses, there was little effect on risk estimates for mortality when these factors were added to the multi-variable analysis. The authors conclude: “The observed protective effect of moderate drinking could not be attributed to misclassification or confounding by psychosocial stressors.”
The authors have demonstrated among men a “U-shaped” curve, with the risk for moderate drinkers being 25-30% lower than that of both non-drinkers and heavier drinkers. For women, there was a lower estimated mortality risk ratio for all drinkers than for non-drinkers, although the confidence intervals included 1.0 in all categories (perhaps, as the authors state, there were few women in their higher categories of alcohol intake).
Forum reviewers thought that this was a well-done analysis of a large population-based population. It did not support the hypothesis that social support, job strain, depressive symptoms, and other such psychosocial factors have a strong influence on the demonstrated inverse relation between moderate alcohol consumption and total mortality. Thus, this study provides additional evidence that the observed reduction in total mortality seen among moderate drinkers is not due to confounding by other lifestyle factors, including psychosocial stressors.
Reference: Ruf E, Baumert J, Meisinger C, Döring A, Ladwig K-H, and for the MONICA/KORA Investigators. Are psychosocial stressors associated with the relationship of alcohol consumption and all-cause mortality? BMC Public Health 2014, 14:312. http://www.biomedcentral.com/1471-2458/14/312.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 138: Underreporting of alcohol intake affects the relation of alcohol to the risk of cancer — 23 April 2014
Epidemiologists are often faced with reported adverse health effects of alcohol among subjects reporting very low levels of consumption, levels that physiologically should not cause diseases such as cancer. It is often assumed that at least some of the subjects reporting low levels of intake may be underreporting their actual intake, but heretofore it has been difficult to judge this.
In the present study, the authors used each subject’s computer-based data on conditions and diseases (including laboratory and social factors), related to alcohol misuse, collected over many years to identify subjects reporting “light-to-moderate” alcohol intake who were likely, or unlikely, to be underreporting their intake at a baseline examination. Overall, 18.4% of subjects were suspected of being underreporters while 46.5% had adequate data that suggested that they were not underreporters. (The remaining 35.1% of subjects had inadequate data stored in the computer to be classified.)
Among their cohort of more than 100,000 subjects, 14,880 developed cancer during an average follow-up period of 18 years. There were 23,363 subjects who reported that they were light (up to 1 drink/day) or moderate (1 to 2 drinks/day) drinkers. In all comparisons, subjects suspected of being underreporters of their alcohol intake had a higher risk of cancer than those not categorized as being underreporters. For example, among subjects reporting 1 to 2 drinks/day, in comparison with non-drinkers, the risk ratio of any type of cancer among those considered to not be underreporters was 0.98 (95% CI 0.87-1.09); in other words, no effect on cancer risk from alcohol. For those categorized underreporters, however, the relative risk of any cancer was 1.33 (95% CI 1.21–1.45). Similar results were seen for alcohol-related cancers as for any cancer. Also, the risk of breast cancer among women was less than one-half as high among moderate drinkers who were unlikely to be underreporters of their alcohol intake as among those considered likely to be underreporting their drinking.
Adjusting for confounding in prospective studies is an ever-present challenge for epidemiologists. One factor that has often been considered probable, but difficult to adjust for, is the underreporting of actual alcohol intake by subjects. Being able to adjust for such unerreporting would greatly improve studies relating alcohol consumption to the risk of cancer (and other chronic diseases). For epidemiologic studies that have extensive longitudinal data on all medical conditions (such as the Kaiser-Permanente Study, the basis for these analyses), the approach described in this paper could be an extremely valuable way of seeking the true relation between light-to-moderate alcohol intake and cancer as well as with a variety of other health outcomes. Based on the present study, an increase in the risk of cancer among light-to-moderate drinkers may occur primarily among those who underreport their alcohol intake.
Reference: Klatsky AL, Udaltsova N, Li Y, Baer D, Tran HN, Friedman GD. Moderate alcohol intake and cancer: the role of underreporting. Cancer Causes Control 2014; on-line publication; DOI 10.1007/s10552-014-0372-8 2014.
Potential Conflict of Interest: The first author of this paper, Dr. Klatsky, is a member of the International Scientific Forum on Alcohol Research. While he has not contributed to this critique, readers may wish to take this fact into account when interpreting the conclusions of the review.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 137: Alcohol intake prior to and during pregnancy and birth outcomes — 28 March 2014
The present analysis was carried out among 1,264 women from Leeds, UK, whose alcohol intake was estimated prior to and during pregnancy. The outcomes were birth weight of the infant and whether or not it was small for gestational age (SGA). In comparison with most previous research on this topic, this study is notable for being of a relatively small size. Further, it had a high percentage of women who consumed alcohol both prior to and during the first trimester, had a very low participation rate of eligible women (only 30%), failed to present estimated effects by ethnicity, and had some questions related to residual confounding. It is unclear how the results of this study increase our knowledge of maternal alcohol consumption and birth outcomes.
Forum members do not believe that the consumption of alcohol should be recommended for pregnant women. A certain percentage of newborns will be small for gestational age, have certain deformities, and have later emotional and behavioral abnormalities. If a woman has consumed any alcohol during the pregnancy, she (and perhaps even her doctor) may blame the abnormality on alcohol consumption, whether or not it had anything to do with it. Hence, the majority of Forum members agree that women should not be encouraged to consume alcohol during pregnancy.
Further, scientific data are very consistent on the potential risks of serious adverse health outcomes of the infant from heavy maternal drinking, especially among women who are alcoholics. Heavy-drinking women who become pregnant should be strongly urged to stop their drinking.
On the other hand, sound data indicating harmful effects on the fetus of light or occasional drinking by a pregnant woman are difficult to come by. Because of the epidemiologic concerns of the present paper, described in our Forum critique, we do not believe that this study adds materially to our understanding of the topic. The serious anxiety occurring among some women who may have ingested some alcohol prior to learning that they were pregnant seems, based on numerous studies, to generally be unnecessary; the need to abort a fetus because of previous light drinking by the mother cannot be justified.
There is a serious problem in interpreting all studies of prenatal alcohol exposure and the outcomes of pregnancy because of potential confounding, especially by ethnicity, education, smoking, coexisting use of illegal drugs, etc. Further, alcohol use by pregnant women has become an especially emotional and even a moral issue, and the entangled confounders make rational analysis most difficult. This means that there is a difficult challenge for epidemiologists and statisticians, as well as for public health officials and the general public, about how to interpret results of individual research projects. The literature can support varying views, from no alcohol at all for those who might soon be expectant mothers to being able to drink moderately throughout pregnancy.
Also, it should be pointed out that the potential health benefits of moderate alcohol consumption relate primarily to middle-aged and older people, so there is no reason for pregnant women to consume alcohol for its “health effects.” Thus, it is very reasonable that the majority of women choose to avoid alcohol during pregnancy. Further, heavy drinking during pregnancy has known potentially serious consequences, and should never be encouraged. Finally, there is insufficient scientific evidence that an occasional drink of alcohol during pregnancy leads to harm to the fetus, and should not cause undue alarm in a pregnant woman who may have consumed some alcohol before she realized she was pregnant.
Reference: Nykjaer C, Alwan NA, Greenwood DC, Simpson NAB, Hay AWM, White KLM, Cade JE. Maternal alcohol intake prior to and during pregnancy and risk of adverse birth outcomes: evidence from a British cohort. J Epidemiol Community Health 2014, pre-publication. doi:10.1136/jech-2013-202934
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 136: Alcohol’s effects on cardiovascular risk among subjects with diabetes mellitus — 18 March 2014
A U- or J-shaped curve for the relation of alcohol consumption to cardiovascular disease (CVD) among diabetics has been shown in most prospective epidemiologic studies for many years, and CVD is the leading cause of death among diabetics. A variety of potential mechanisms of protection against CVD have been described, including beneficial effects of moderate drinking on lipids, inflammatory markers, and insulin resistance. The current paper assesses the effects of alcohol use among participants in the Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified-Release Controlled Evaluation (ADVANCE) trial. It was based on more than 11,000 subjects with diabetes from 20 countries, including those in Eastern Europe, Asia, and established market economies in Western Europe, North America, and the Pacific region. The outcomes over 5 years of follow up were CVD events (death from CVD, non-fatal myocardial infarction, non-fatal stroke), microvascular disease (renal disease, diabetic eye disease), and all-cause mortality.
Key results of the analyses showed that during follow up, more than 1,000 subjects (about 10%) had a major CVD, with similar percentages experiencing a microvascular complication or dying. The authors report that “Compared with abstainers, any alcohol use was associated with a 17% lower risk of cardiovascular events, a 15% lower risk of microvascular complications, and a 13% lower risk of all-cause mortality.” While there were few heavy drinkers (<4% of subjects), their data indicated that there was no significant lowering of risk of the outcomes among such subjects. Subjects who consumed wine had lower estimates of cardiovascular disease outcomes and mortality than consumers of other beverages.
Forum reviewers considered this to be a well-done analysis based on a large cohort of subjects with diabetes mellitus, with an adequate number of non-drinkers to serve as a referent group. The results strongly support previous studies that have shown a lower risk of cardiovascular events and total mortality among diabetic subjects who consume moderate alcohol. The study also showed that the risks of microvascular complications (diabetic kidney disease, diabetic eye disease) were lower among moderate drinkers.
The Forum considers this to be an important message (to physicians and the public), as the vascular ravages of diabetes are very serious, and diabetes is such a common disease that is increasing throughout the world. Diabetic patients without contraindications to alcohol sorely need to know of the potential cardiovascular protection of moderate alcohol consumption.
Reference: Blomster JI, Zoungas S, Chalmers J, Li Q, Chow CK, Woodward M, Mancia G, Poulter N, Williams B, Harrap S, Neal B, Patel A, Hillis GS. The relationship between alcohol consumption and vascular complications and mortality in individuals with type 2 diabetes mellitus. Diabetes Care 2014; pre-publication: DOI: 10.2337/dc13-2727
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here
===============================================================================
Critique 135: Binge drinking greatly increases mortality risk among moderate drinkers — 11 March 2014
This study was based on a sample of “late-middle-aged” (55-65 years old at baseline) community residents who were recruited from the western part of the United States to participate in a study of late-life alcohol consumption and drinking problems. The present analyses evaluated association between episodic heavy drinking and total mortality among 446 adults who were considered to be “moderate” drinkers. The authors report that the 74 moderate drinkers who engaged in episodic heavy drinking (“binge drinking”) had more than two times higher odds of 20-year mortality than moderate drinkers who did not binge drink.
An association between binge drinking and health outcomes has been demonstrated in epidemiologic studies for decades. Many (but not all) studies have shown an approximately two-fold increase in the risk of adverse outcomes for binge drinkers, in comparison with moderate drinkers who do not binge drink. In reviewing the present study, Forum members commented on the small number of subjects (only 74 binge drinkers in the analysis), and some other analytic weaknesses (e.g., no data on potential changes in drinking habits over 20 years, inadequate control of some potential confounders, results not applicable to the general population as some subjects were recruited because of previous alcohol misuse). Nevertheless, the results of the study support adverse effects on mortality of such a drinking pattern.
There are now considerable scientific data indicating harmful health effects of episodic excessive drinking in terms of coronary heart disease, other diseases of ageing, and mortality. Simply knowing the average intake of subjects over a period of time is inadequate for classifying their alcohol consumption. For middle-aged and older subjects the drinking pattern that has been shown to be associated with the most favorable health outcomes (including greater longevity of life) is regular, light-to-moderate intake, especially when the alcoholic beverage is consumed with food.
Reference: Holahan CJ, Schutte KK, Brennan PL, Holahan CK, Moos RH. Episodic heavy drinking and 20-year total mortality among late-life moderate drinkers. Alcohol Clin Exp Res 2014; pre-publication; DOI: 10.1111/acer.12381.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 134: Comments on “Section 2.3, Alcohol Consumption,” from the “World Cancer Report 2014” issued by the World Health Organization – 11 February 2014
A recently released report by IARC (International Agency for Research on Cancer) of the World Health Organization, entitled “World Cancer Report 2014,” includes a section on alcohol consumption as a factor in the etiology of cancer. From reading this report, it is clear that the conclusion of the authors is that all alcohol consumption is harmful, regardless of the amount consumed, the type of beverage, or the pattern of drinking. The members of the International Scientific Forum on Alcohol Research (the Forum) have real concerns about the WHO report.
It appears that the authors have been very selective in choosing the data upon which they base their conclusions, often citing their own work and ignoring thousands of scientific articles relating alcohol consumption to cancer rates and mortality. The report fails to discuss potential lower risks of cancer associated with polyphenols in wine and some other beverages. It ignores the consistent finding in almost all prospective epidemiologic studies over many decades that total mortality rates are lower among light-to-moderate alcohol consumers (and recent evidence suggests that this may even be true among people with cancer).
Members of the Forum strongly agree that heavy alcohol consumption and “binge” drinking are associated with many adverse effects (and would never be advised by responsible agencies). However, the WHO report seriously undermines its credibility by publishing a report that seems to deliberately ignore overwhelming scientific evidence showing that light-to-moderate consumption of alcohol not only reduces overall mortality but is usually not associated with an increased risk of cancer.
Excessive and binge drinking in young people is a growing scourge in many parts of the world, and alcohol consumption (especially in conjunction with smoking) clearly increases the risk of upper aero-digestive cancers; further, even moderate consumption is associated with a slight increase in the risk of breast cancer in women. However, the scare tactics condemning all alcohol consumption in the WHO report tend to obscure those important messages.
It is the opinion of our Forum that WHO, in the alcohol section of its new publication World Cancer Report 2014, has not provided an objective statement on alcohol and cancer based on current scientific data. By doing so, WHO has lost credibility and, more importantly, has missed a key opportunity to convey important focused messages about alcohol and cancer that would be more likelty to improve the health of the public.
Reference: Rehm J, Shield K. Section 2.3, Alcohol Consumption, from World Cancer Report 2014, pp. 97-106, released 3 February 2014 by IARC (International Agency for Research on Cancer), of the World Health Organization.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 133: Alcohol intake may lower the risk of developing multiple sclerosis — 4 February 2014
Previous research has shown that alcohol consumption may be associated with a reduced risk of rheumatoid arthritis, lupus erythematosus, and other autoimmune diseases. There have also been reports that alcohol may lower the risk of multiple sclerosis (MS). The authors of the present paper have used data from two large Swedish case-control studies of MS to evaluate the relation of alcohol consumption to MS. Key results showed that in both of the case-control analyses, there was a dose-response inverse relation between alcohol consumption and the risk of developing MS. In comparison with subjects reporting no alcohol intake in the 5- or 10-year period during which the diagnosis of MS was first made, subjects in the highest alcohol consumption group (> 112 g/week, about 9 drinks per week for women; >168 g/week, about 14 drinks per week for men) had 30% to 50% lower risk of developing MS. A variety of potential confounders were included in the analysis, including smoking, education, and SES.
Forum members who reviewed this paper all thought that it reflected a well-done analysis. The main concerns were that, as are most studies of uncommon diseases, these were case-control comparisons (which may be associated with recall bias, reverse causation, and other potential confounding variables), and that the investigators could not determine if the “non-drinkers,” their referent group, were lifetime abstainers or former drinkers. Also, while earlier research has shown that the polyphenols in wine may provide protection beyond that of alcohol in combating inflammation, there were no data on beverage-specific results.
In general, however, Forum members welcomed this contribution to our knowledge on the subject, and thought that the authors did a good job in discussing the strengths and weaknesses of their study. There was a brief discussion of potential mechanisms by which alcoholic beverages could lower the risk of MS, but no discussion of the potential added effects related to polyphenolic substances. Forum members also thought that serum uric acid (which may increase with alcohol consumption) could play a role in an autoimmune disease, but this was not discussed by the authors.
Based on previous research and the results of this paper, it is probable that moderate alcohol intake, especially of wine, may lower the risk of developing MS, a neurological disease for which no cure is currently available. While MS is too uncommon a condition to use these findings to recommend alcohol consumption for the prevention of the disease, it would be useful if future research could help determine if, for subjects who already have MS, moderate drinking may affect the progression of their disease.
Reference: Hedström AK, Hillert J, Olsson T, Alfredsson L. Alcohol as a modifiable lifestyle factor affecting multiple sclerosis risk. JAMA Neurology 2014; doi:10.1001/jamaneurol.2013.5858; published online January 6, 2014.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 132: Pattern of alcohol consumption and cause of death in a large European prospective study — 21 January 2014
A large group of investigators participating in the European Prospective Investigation into Cancer and Nutrition (EPIC) study have reported on the association of alcohol consumption with disease-specific mortality over a 12-year period among a very large number of men and women. Alcohol intake over the past year (as well as estimates of earlier intake) was reported at baseline. A variety of approaches were used to identify deaths in the participating cohorts, but validation of the cause of death was not possible. No data were reported on certain key aspects of drinking pattern (frequency of alcohol intake, binge drinking, with meals, etc.) and beverage-specific effects were not reported.
The authors report that the risk of death from cardiovascular diseases was lower, and from cancer and certain other causes of death were higher, among drinkers than among their referent group of “lifetime light users” (men reporting ≤1 drink/week and women reporting ≤ 0.5 drinks/week). However, their graphs of alcohol intake and risk of total mortality (not included in the paper but in supplementary data they provide on the internet) show strong J-shaped curves for increasing alcohol intake for both men and women. For men, the risk among alcohol consumers of up to about 48 gr/day (the equivalent of approximately four “typical drinks”) was lower than that of the lifetime light users that made up the referent group; at higher intake, the risk increased above that of light drinkers. For women, the risk of total mortality for drinkers remained lower than that of the referent group at all reported levels of intake. Despite these findings, the entire paper focuses only on the increased risk of death from alcohol for certain diseases, and almost completely ignores the net, overall effects on total mortality.
Forum reviewers considered that while the analyses were done correctly, there were major weaknesses in the estimation of “lifetime alcohol intake,” no data on the pattern of intake, no validation of coexisting diseases and, especially, no validation of the specific cause of death, even though this was the primary outcome of the study. All of these factors weaken the strong assertions made by the authors in their conclusions.
Forum members were concerned that the authors seemed to obscure the total effects of light-to-moderate drinking (lower risk of all-cause mortality), and emphasize only the harmful effects. Some reviewers considered that the presentation appeared to be based more on ideology than on an unbiased assessment of the data, and one suggested that the paper appears to have been written starting from pre-conceived conclusions, then finding data to support them.
It is interesting that two Commentaries published with this article came to divergent views. One by Stockwell and Chikritzhs emphasized potential bias and confounding that cause concern when relating alcohol to mortality in observational studies. While they then pointed out how well the present authors adjusted for many of these factors, they nevertheless concluded their commentary repeating how such factors are difficult to control and stating that “ . . . a healthy dose of skepticism is warranted for the hypothesis that light/moderate alcohol consumption is beneficial to health.” (They do not mention that data on alcohol and mortality are far more robust that data supporting generally accepted beliefs of the beneficial effects of physical exercise, eating a healthy diet, maintaining a lean body mass, etc.)
On the other hand, the commentary on the present paper by Banks considered the data presented quite sound, and concluded: “If taken as causal, these findings are consistent with most public health advice about alcohol, except that most advice recommends an upper limit to alcohol consumption, but does not actually encourage drinking. In fact, the evidence goes further than this and indicates that, in later life, on average and bearing in mind the priorities and risks of specific individuals, drinking at least some alcohol, but not too much, is likely to minimize the overall risk of death.”
Reference: Bergmann MM, Rehm J, Klipstein-Grobusch K, et al (38 authors). The association of pattern of lifetime alcohol use and cause of death in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Int J Epidemiol 2013;42:1772-1790
Attached Commentaries:
Banks E. Commentary: Lifetime alcohol consumption and mortality: have some, but not too much. Int J Epidemiol 2013;42:1790–1792; doi:10.1093/ije/dyt218
Stockwell T, Chikritzhs T. Commentary: Another serious challenge to the hypothesis that moderate drinking is good for health? Int J Epidemiol 2013;42:1792–1794; doi:10.1093/ije/dyt217
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 131: Effects of alcohol consumption on the risk of gout — 23 December 2013
A new meta-analysis has been conducted to assess the effects of alcohol consumption on the risk of gout. A total of 12 articles with 17 studies involving 42,924 cases met the inclusion criteria. The authors report that the pooled RRs for light (≤1 drink/day), moderate (>1 to <3 drinks/day), and heavy drinking (≥3 drinks/day) vs. non/occasional alcohol drinking were 1.16 (95 % CI, 1.07–1.25), 1.58 (95 % CI, 1.50–1.66), and 2.64 (95 % CI, 2.26–3.09), respectively. The results suggested that alcohol consumption might be associated with increased risk of gout.
Forum reviewers agreed that the analytic methodology in this paper was appropriate. Considerable research has shown that alcohol intake, especially heavier drinking, increases serum uric acid levels and the risk of gout. There remain some questions about the relation of wine consumption with gout, and the present study did not have data to test beverage-specific responses.
Overall, data suggest that alcohol intake, especially heavier drinking, raises serum uric acid levels and may trigger an acute attack in persons with gout, especially those who are not controlling their disease with appropriate medication. A number of studies, including the present one, suggest that even light alcohol intake may increase the risk of developing gout. In any case, the risk appears to be rather low with light drinking, a level of alcohol intake that should reduce the risk of cardiovascular disease. Also, some studies suggest that the risk is lower for the consumption of wine than for the consumption of other beverages containing alcohol.
Reference: Wang M, Jiang X, Wu W, Zhang D. A meta-analysis of alcohol consumption and the risk of gout. Clin Rheumatol 2013;32:1641–1648.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 130: How alcohol consumption may interact with genetic factors that relate to health and disease — 10December 2013
Despite extensive research over the past few decades, our knowledge about the genes that underlie most chronic diseases remains incomplete. For example, even for alcohol-related diseases, it is not possible at present to determine how an individual person will respond over a lifetime to varying amounts of alcohol intake: not all heavy drinkers develop cirrhosis; not all moderate drinkers lower their risk of cardiovascular disease. While the underlying genetic pattern of a person undoubtedly plays a role in his/her health outcomes, environmental factors, including alcohol consumption, may modify the effects of genes. The modification of the effects of genes by environmental factors, such as alcohol intake, can be referred to as “epigenetics.”
A new paper on epigenetics, by a leading scientist who has worked at the National Institute of Alcohol Abuse and Alcoholism (NIAAA) for many years, provides important new insight into mechanisms by which alcohol intake, especially heavy consumption, may modify the activity of genes affecting health. Dr. Zakhari describes specific effects that heavy alcohol intake can have on the activities of enzymes involved in epigenetic modifications. In some cases, alcohol enhances genetically determined effects, in others it suppresses such activity. As stated by the author, “Metabolites, including those generated during ethanol metabolism, can impact disease states by binding to transcription factors and/or modifying chromatin structure, thereby altering gene expression patterns.”
Forum members consider this to be a very well-thought-out and well-done presentation of important new data. They agree with the author that these observations could help researchers to design model medications to treat or at least ameliorate alcohol-related organ damage, such as cirrhosis of the liver and alcohol-related cancers. While reviewers consider that these observations are important in our understanding of how alcohol affects health, they point out that they must be tested in further research, especially epidemiologic studies, to evaluate the extent that such interations between alcohol and genes actually affect health outcomes. Key problems that limit our ability to determine causality of disease from epidemiologic studies include not knowing the underlying genetic susceptibility of individual subjects and, as pointed out in the present paper, not accounting for environmental factors that may modify such genetic effects.
Reference: Zakhari S. Alcohol metabolism and epigenetics changes. Alcohol Research: Current Reviews 2013;35:9-16.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 129: Association of alcohol consumption with skin cancer; A report from the Women’s Health Initiative — 20 November 2013
A report from more than 59,000 women in the Women’s Health Initiative related reported alcohol consumption to the risk of melanoma (MM) and non-melanoma skin cancer (NMSC). This was a fairly large study, with 532 cases of melanoma and 9,593 cases of NMSC occurring over approximately 10 years of follow up. The key reported results were for a higher hazard of MM (HR 1.64) and NMSC (OR 1.23) for drinkers of 7 or more drinks/week, compared with non-drinkers. Lifetime alcohol consumption was also positively associated with hazard of MM and risk of NMSC, with the only significant increases for MM according to type of beverage being seen for women with a preference for white wine or liquor. As shown in many previous studies, the risk of these skin cancers was lower among smokers than among non-smokers.
Forum reviewers thought that this was a very well-done analysis. They did note that there were large decreases in the estimates of HRs related to alcohol consumption when adjustments were made for sun exposure and other known confounders. For example, the HR for MM decreased for total wine from 1.30 to 1.06 when adjusted; for red wine:1.71 to 1.34; for white wine: 1.93 to 1.52; for liquor: 1.87 to 1.65; for beer: 1.34 to 1.18. The magnitude of these changes, as well as the very different baseline characteristics of the women according to their drinking habits, raises the possibility that there may be residual confounding affecting the results. In addition, reviewer Zhang points out that by including subjects with these skin cancers prior to baseline in their main analyses, there could be a problems with bias in their results.
Forum member Klatsky has recently reported on this topic using several decades of follow-up data from the Kaiser-Permanente study, with more than 300,000 subjects and more than 1,000 cases of MM. In that study, he and his colleagues found that among persons preferring wine, the HR for MM at 3+ drinks per day was 1.7 (95% CI 1.2-2.5), while it was 1.2, 1.3, and 1.1 in persons with preference for liquor, beer, and no beverage type. However, at 1-2 drinks per day, wine drinkers had a HR of 0.9. Klatsky states “So maybe too much should not be made of the beverage type data in these analyses. However, the association with alcohol seems statistically solid.”
A previous study by Mukamal, with data from 300,000 subjects participating in a risk factor surveillance survey reports: “Approximately 33.5% of respondents reported a sunburn within the past year. Heavier average alcohol use and binge drinking were both positively associated with prevalence and number of sunburns within the past year. The adjusted odds ratios for prevalence and number of sunburns among binge drinkers were 1.39 (1.31-1.48) and 1.29 (1.20-1.38), respectively.” Klatsky wonders whether “possible confounding by sun is not only an artifact of SES and tropical vacations, but whether heavy imbibers at the beach may fall asleep when exposed or simply do not notice their sunburn until it is severe.” Other Forum reviewers also worry that there may be residual confounding in the present study from sun and ultraviolet exposure.
Klatsky adds: “However, even if the alcohol-melanoma association is due to confounding by sun exposure, the same explanation seems less plausible for the inverse association between smoking and melanoma. While there is obviously no public health utility in any ‘protective’ effects of smoking, that association is scientifically interesting and could be a clue to mechanisms.”
The bottom line is that there are considerable observational epidemiologic data suggesting that alcohol consumption may relate to an increase in the risk of MM and NMSCs. As mechanisms are not known, there is still concern that much of this relation may relate to residual confounding by ultraviolet sun exposure, the most important environmental factor for these diseases.
Rerference: Kubo JT, Henderson MT, Desai M, Wactawski-Wende J, Stefanick ML, Tang JY. Alcohol consumption and risk of melanoma and non-melanoma skin cancer in the Women’s Health Initiative. Cancer Causes Control 2013 (pre-publication) DOI 10.1007/s10552-013-0280-3
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 128: Little effect of alcohol consumption on breast cancer risk found among African-American women — 14 November 2013
Alcohol is known to be a risk factor for breast cancer in Caucasian women, but the evidence in African-American (AA) women is limited and results from previous studies are inconclusive. The present case-control study, based on 803 cases of breast cancer among African American women in the northeastern part of the USA, evaluated associations between recent and lifetime drinking and breast cancer risk. The authors report that there was no association between recent drinking and breast cancer risk, even when stratified by menopausal status or by hormone receptor status. Further, their analyses suggested a slight decrease in cancer risk with alcohol consumption among women who drank when under 20 years of age (OR = 0.65; 95% CI: 0.47–0.89), regardless of menopausal or hormone receptor status.
Forum reviewers point out that this was a case-control study of breast cancer, which always presents an opportunity for recall bias, and the number of cases was not large. Further, AA women generally drink very little, so it may be difficult to determine if larger amounts of alcohol may increase breast cancer risk.
On the other hand, the results were based on a very well-done and complete analysis, with appropriate control for known risk factors, similar results were obtained when recent (in last year) alcohol intake and long-term alcohol consumption were considered, and their finding of increased risk of breast cancer among subjects with a family history of breast cancer, a personal history of benign breast disease, and HRT use strengthen the results.
The results of this study are consistent with those from many previous studies showing little effect of alcohol consumption on breast cancer risk among AA women. However, given that few AA women in the USA drink alcohol, and those that do typically consume only small amounts, the study cannot estimate the potential effect on breast cancer among heavier drinkers. Further, Forum members believed that the decrease in the risk of breast cancer found in this study for drinking early in life (before age 20 years) may be due to residual confounding by socio-economic factors.
Overall, the present study supports previous research suggesting that the light alcohol consumption typically seen among AA women in the USA is not an important factor in their risk of breast cancer. On the other hand, this paper reports similar null results between alcohol and cancer risk among Caucasian women in their study. Current data do not necessarily indicate that there are ethnic differences in alcohol metabolism that may lead to differences between Caucasian and AA women in the association of alcohol consumption with breast cancer, and this study alone cannot be used to support such a premise.
Reference: Chandran U, Zirpoli G, Ciupak G, McCann SE, Gong Z, Pawlish K, Lin Y, Demissie K, Ambrosone CB, Bandera EV. Does alcohol increase breast cancer risk in African-American women? Findings from a case–control study. British J Cancer 2013;109:1945–1953 | doi: 10.1038/bjc.2013.513.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 127: Estimation of alcohol-attributable and alcohol-preventable mortality in Denmark — 6 November 2013
In an attempt to judge the harmful and beneficial health effects related to alcohol consumption, Danish scientists have carried out analyses comparing alcohol-attributable and alcohol-preventable mortality in Denmark. They have used estimates of the potentially harmful effects of alcohol use on more than 20 diseases, giving 100% values to “alcohol use disorders,” although the specific causes of death are not known for this category. Most of the other attributions for harm are realistic, but the alcohol preventable attributions for diabetes and ischemic heart disease appear to be low. The authors conclude that 5.0% of deaths among women and 9.5% of deaths among men were attributable to alcohol in Denmark in 2010, with the majority of all alcohol-attributable deaths caused by high consumption. They attribute only between 2 and 3% of deaths to be preventable by alcohol.
Previous estimates of alcohol-attributable and alcohol-preventable effects have varied widely, emphasizing the importance of the assumptions made by the investigators in any set of analyses. For example, an analysis of deaths in Germany by Konnopka et al (Konnopka A, Hans-Helmut König H-H. The health and economic consequences of moderate alcohol consumption in Germany 2002. Value in Health 2009;12:253-261) concluded that there were more alcohol-preventable deaths than alcohol-attributable deaths and a report from the UK also estimated much lower rates for alcohol-attributable deaths (White IR, Altmann DR, Nanchahal K. Mortality in England and Wales attributable to any drinking, drinking above sensible limits and drinking above lowest-risk level. Addiction 2004;99:749–756). Further, a previous report that included data for Denmark gave very different results for net alcohol effects, estimating that less than 1% of deaths were attributable to alcohol (Britton A, Nolte E, White IR, Gronbaek M, Powles J, Cavallo F, McPherson K. A comparison of the alcohol-attributable mortality in four European countries. Eur J Epidemiol. 2003;18:643–51). It is probable that different underlying assumptions of alcohol effects on various diseases are the prime reason for such differences.
There is no question that heavy alcohol consumption contributes to a large number of disease conditions, and the findings of this study emphasize the magnitude of the problem. On the other hand, if the potentially beneficial effects of moderate alcohol consumption on many common diseases are underestimated, a net unfavorable result, as in the present study, is unavoidable. It will be interesting to see what assumptions are made in other studies such as this, and how such assumptions affect the outcome of analyses.
Reference: Eliasen M, Becker U, Grønbæk M, Juel K, Tolstrup JS. Alcohol-attributable and alcohol-preventable mortality in Denmark: an analysis of which intake levels contribute most to alcohol’s harmful and beneficial effects. Eur J Epidemiol 2013; DOI 10.1007/s10654-013-9855-2
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 126: Moderate alcohol intake may lower the risk of rheumatoid arthritis — 11 October 2013
Moderate alcohol intake, compared with abstinence, has been related to lower inflammatory markers and a reduced risk of many auto-immune diseases, including rheumatoid arthritis (RA), systemic lupus erythematosus, autoimmure diabetes, and Graves hyperthyroidism. The present large meta-analysis relating alcohol to RA includes data from 5 prospective cohort studies and 3 nested case-control studies. Their analyses are based on prospective data from a total of almost 200,000 subjects, among whom 1,878 developed RA.
This meta-analysis concludes that low to moderate alcohol consumption is inversely associated with the development of RA. It suggests a “J-shaped” curve, with a lowered risk for an average intake of up to 15 g of alcohol (about 1 to 1 ½ typical drinks), in comparison with non-drinkers, and an increased risk for heavier drinking. While the immediate effects were greater for women in this study, for long-term effects the authors noted that “Regardless of sex, a consistent low to moderate alcohol consumption for a period of at least 10 years was found to have a 17% reduction in RA risk.”
Beneficial effects of alcohol on indices of inflammation have been shown repeatedly. The probable mechanism of alcohol’s effect on the risk of RA is down regulation of the immune response and a decrease in pro-inflammatory cytokines.
Reference: Jin Z, Xiang C, Cai Q, Wei X, He J. Alcohol consumption as a preventive factor for developing rheumatoid arthritis: a dose-response meta-analysis of prospective studies. Ann Rheum 2013. doi: 10.1136/annrheumdis-2013-203323
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 125: Effects of alcohol consumption on risk of colorectal cancer; potential modification by folate intake — 25 September 2013
Many epidemiologic studies have shown a small increase in the risk of breast cancer and colorectal cancer to be associated with alcohol consumption. Some have found that higher intakes of folic acid may attenuate such an increase in risk. The present study was designed to evaluate the influence of alcohol consumption on the risk of colorectal cancer according to folic acid fortification period in the United States. The relation of alcohol intake to colorectal cancer in two prospective studies (the Nurses’ Health Study and the Health Professionals Follow-up Study) was compared for a prefortification period (before 1998) with such risk estimates during the postfortification period, which began in 1998. A total of 2,793 cases of invasive colorectal cancer were documented.
The authors concluded that their data support an increase in colorectal cancer with high alcohol intake, and suggest that the risk may be lower in the postfortification period due to a higher folate intake in the US population. Forum reviewers had some concerns about these conclusions, as they point out that no dose-response relation between alcohol and colorectal cancer was shown in either period, and in data since 1998 no significant relation is seen between alcohol and such cancers. In fact, the authors of the present study state: “We also examined drinking pattern in relation to colorectal cancer risk; neither frequency of drinking nor quantity of drinking was associated with the risk of colorectal cancer;” they do not report their data upon which that statement is based.
Overall, the present paper does not answer the question as to the extent to which alcohol may relate to the risk of colorectal cancer, or if folate intake may modify any relation that may exist. Given that colorectal cancer (and breast cancer in women) are so common, it is important to evaluate how dietary folate and other nutrients may relate to such cancers. Further research on the relation of alcohol to these cancers, and potentially modifying factors, is greatly needed.
Reference: Nan H, Lee JE, Rimm EB, Fuchs CS, Giovannucci EL, Cho E. Prospective study of alcohol consumption and the risk of colorectal cancer before and after folic acid fortification in the United States. Annals of Epidemiology 2013;23:558-563.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 124: The J-shaped curve for the relation of alcohol consumption to mortality — 17 September 2013
An analysis based on data from more than 110,000 subjects in the USA, of whom 3,364 died during a follow-up period of up to 9 years, was used to evaluate the relation of “heavy drinking” and “nonheavy drinking” to the risk of all-cause mortality. The authors defined heavy drinking as 5 or more drinks/occasion, and recorded the frequency in which subjects consumed such amounts. Subjects consuming < 5 drinks/occasion were classified as nonheavy drinkers.
The key findings of the analyses were that there was a positive and linear increase in risk of mortality for subjects consuming heavy amounts of alcohol, with the risk increasing as drinking at this level was more frequent. For nonheavy drinkers, there was a J-shaped relation with mortality. The point at which the nonheavy drinkers’ risk of mortality exceeded that of abstainers was between 4 and 5 drinking occasions/week.
Forum reviewers thought that this was a well-done analysis that emphasizes the importance of the pattern of drinking, and not just the average weekly intake. Although the upper limits of drinks/occasion exceeded that usually considered as “moderate,” a J-shaped curve between alcohol and mortality for these drinkers was demonstrated. This is the pattern usually seen in prospective epidemiologic studies when “moderate” is defined at somewhat lower levels of alcohol intake.
Forum reviewers agreed with the conclusions of the authors regarding the importance of considering the pattern of drinking when evaluating the health effects of alcohol. The authors concluded: “Promoting less harmful drinking patterns by reducing heavy drinking frequency is an appropriate harm reduction strategy, and assessing drinking pattern by determining the frequency of heavy and nonheavy drinking is a simple and fast way to determine risk and promote less risky drinking behavior.”
Reference: Plunk AD, Syed-Mohammed H, Cavazos-Rehg P, Bierut LJ, Grucza RA. Alcohol consumption, heavy drinking, and mortality: Rethinking the J-shaped curve. Alcohol Clin Exp Res 2013;pre-publication: DOI: 10.1111/acer.12250
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 123: Alcohol consumption and lymphoid and myeloid neoplasms — 5 September 2013
Many prospective studies have shown that moderate drinkers are at lower risk of certain types of lymphoid cancer. For example, a report in 2009 from the Million Women’s Study in the UK found that alcohol consumption showed a significant inverse association with the occurrence of non-Hodgkin lymphoma (NHL). Further, a 2012 paper from that study based on 9,162 incident cases of haematological malignancy, including 7,047 lymphoid and 2,072 myeloid cancers, concluded: “Among predominantly moderate alcohol drinkers, higher intake was associated with lower risk of lymphoid malignancies.” Those investigators did not find a significant effect of alcohol on the risk of myeloid tumors, such as acute myeloid leukemia. Another 2012 paper based on almost 2,000 cases of Non-Hodgkin Lymphoma concluded: “In summary, findings from the prospective study presented here support the hypothesis that alcohol intake might be associated with a reduced risk of NHL.”
The authors of the present paper from the Netherlands, based on 17.3 years of follow up with 1,375 cases of lymphoid and 245 cases of myeloid neoplasms, did not find a statistically significant reduction in the risk of lymphoid cancers, and the authors suggest: “If any association between alcohol consumption and lymphoid neoplasms exists, our study suggests an increased risk rather than a decreased risk.”
While reasons for this difference in results of this study when compared with other recent studies may be used to better understand the association between alcohol and such cancers, Forum reviewers were concerned about a number of aspects of this study. For example, the authors had data on alcohol consumption only at baseline for this very long (17+ year) follow up, so changes (either increases or decreases in intake) were not known. Further, the key relations reported were not adjusted for a large number of potentially confounding variables, such as a positive family history of hematological cancer. (The authors state that they carried out such multivariable analyses but do not present the data.) Of even more concern was the apparent inverse effect of alcohol on cancer risk for a number of types of tumors when dose-response relations were shown.
Given the rather consistent findings in other very large studies of hematological malignancies that the risk of many types of lymphoid cancer may be reduced by alcohol, and inconsistencies in the results of the present analyses, it is difficult to conclude that the present paper should change our current interpretation of the association between alcohol and these types of cancer.
Forum members look forward to reports from other prospective studies on this topic. For the present, however, the overwhelming scientific evidence suggests that moderate alcohol consumption is associated with a decrease in the risk of many types of lymphoid malignancies, but has little effect on myeloid cancers.
Reference: Heinen MM, Verhage BAJ, Schouten LJ, Goldbohm RA, Schouten HC, van den Brandt PA. Alcohol consumption and risk of lymphoid and myeloid neoplasms: Results of the Netherlands cohort study. Int J Cancer 2013l133:1701–1713.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 122: Does moderate wine consumption lower the risk of developing depression? — 3 September 2013
There is a large literature relating heavy alcohol consumption to depression: most studies show that heavy drinkers tend to be depressed, and depressed people may self-medicate with large amounts of alcohol. This large prospective study of subjects at high risk of cardiovascular disease has shown that “moderate” drinkers, especially wine drinkers (the majority of their subjects), were at lower risk of developing depression during 7 years of follow up than were non-drinkers. An important aspect of this study is indeed that the analyses were based on moderate drinkers, as people exceeding certain amounts of alcohol or testing positive on the CAGE questionnaire (a measure of alcohol misuse) were excluded.
Strengths of the study include it being a large prospective study, with more than 5,000 subjects, aged 55-80 years at baseline, who were followed for up to 7 years for the initial development of clinical depression (which was diagnosed in 443 instances). Especially important was the ability of the investigators to have repeated assessments of alcohol consumption, every two years. A rather complete list of potentially confounding variables was available. The key findings of the study were that subjects reporting >5-15 grams/day of total alcohol intake, and wine drinkers of 2-7 drinks/week, were at a lower risk of developing depression than were non drinkers.
Some Forum members remained concerned that there may have been residual confounding by other lifestyle habits, and that the results may apply primarily to subjects who are also following a Mediterranean-type diet and lifestyle. Also, data were not available to evaluate the relation of heavy drinking or alcoholism to depression. However, the authors provide good scientific support for their conclusions that subjects reporting >5-15 grams/day of total alcohol intake (from about ½ to 1 ½ of a typical drink), and wine drinkers of 2-7 drinks/week, are at approximately 30% lower risk of developing depression than are abstainers of alcohol.
Reference: Gea A, Beunza JJ, Estruch R, et al (17 authors). Alcohol intake, wine consumption and the development of depression: the PREDIMED study. BMC Medicine 2013. Advanced publication, released 29 August 2013.
For the full critique of this paper by members of the International scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 121: Differences between wine and other alcoholic beverages in terms of adverse consequences of alcohol consumption – 22 August 2013
Questionnaire-based data on alcohol consumption were collected from more than 5,000 military recruits in Switzerland, who had a mean age of just over 19 years. There were very few drinkers who averaged more than 21 drinks/week, so the emphasis was on the effects of what is usually referred to as “binge drinking,” defined in this study as the consumption of 6 or more typical drinks (a drink containing 10-12 g of alcohol) on a single occasion. The “preference” of one particular type of beverage was based on the subject indicating that it made up more than two-thirds of his total alcohol consumption. The specific type of beverage preferred — beer, wine, or “other beverages” (the latter including apertifs, “pops,” chillers, and coolers) — was related to the pattern of drinking (frequency of binge drinking) and to the reported occurrence of adverse alcohol-related consequences (e.g., blackouts, driving after heavy drinking, missing work due to drinking, accidents, unprotected sex, encounters with police).
The authors report: “Preference for beer was associated with risky drinking patterns and, comparable with a preference for strong alcohol, with the use of illicit substances (cannabis and other illicit drugs). In contrast, a preference for wine was associated with low-risk alcohol consumption and a reduced likelihood of experiencing at least four negative alcohol-related consequences or of daily cigarette smoking.” More frequent binge drinking of any beverage was strongly associated with an increase in adverse alcohol-related consequences.
Forum reviewers thought that the adverse outcomes, especially those related to heavy beer intake, tend to characterize a particular subculture that demonstrates problematic substance use due to personal characteristics of the subjects. The unhealthy outcomes may be a feature more of the cultural habits of the subjects rather than just due to the type of beverage they consume most frequently.
The authors conclude that strategies for preventing problems with alcohol abuse should attempt to reduce excessive drinking of all types of beverages. However, they add: “to lessen the additional negative effects of beer and strong alcohol, which are particularly cheap in Switzerland, targeted strategies such as minimum pricing policies for these beverage types should be considered.” Forum members think that the extent to which such beverage-specific price restructuring would decrease unhealthy drinking practices among young people remains unclear.
Reference: Dey M, Gmel G, Studer J, Dermota P, Mohler-Kuo M. Beverage preferences and associated drinking patterns, consequences and other substance use behaviours. European Journal of Public Health 2013; advance access; doi:10.1093/eurpub/ckt109
For the full critique of this critique by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 120: Binge drinking impairs endothelial function in young people — 20 August 2013
The function of the vascular endothelium is a key process in the development of atherosclerosis and coronary heart disease, and extensive studies among middle-aged and elderly adults generally show beneficial effects of moderate drinking on vascular function. Whether or not alcohol consumption among young people has any lasting biological effects on cardiovascular risk is unclear: risk factors tend to track from childhood into adulthood, but specific long-lasting effects related only to drinking in young people are not known. Hence, data are currently not available to answer the question as to when during life people might consider beginning the moderate consumption of alcohol for the potential lowering of cardiovascular risk later in life.
The present study does not answer that question, as it only compares abstaining young people with binge drinkers, with the latter being defined as subjects reporting that they consumed ≥ 5 drinks in 2 hours for males, and ≥ 4 drinks in 2 hours for females. (The average number of binge-drinking episodes for these subjects was 6 ± 1 within the past month.) It does not compare abstainers with moderate drinkers. However, the paper does show that binge drinking among 18 – 25 year olds has adverse effects on endothelial function.
Forum reviewers were pleased to see this study, but point out that it is a cross-sectional analysis, and only compares binge drinkers with non-drinking young people. Further, inadequate data are presented to know the degree to which the results of the study may suffer from residual confounding from other factors.
The authors conclude that their study showed adverse effects on both microvascular and macrovascular function to be associated with frequent binge drinking in young people. It is hoped that these investigators, or others, will in the future provide data on the effects on vascular function of regular, moderate alcohol consumption among young people. It would also be interesting to learn if effects are different for high-polyphenol wine than for other beverages. Further, it will be important to determine how long beneficial or adverse effects on vascular function may persist, with or without continued alcohol intake.
Reference: Goslawski M, Piano MR, Bian J-T, Church EC, Szczurek M, Phillips SA. Binge drinking impairs vascular function in young adults. J Am Coll Cardiol 2013;62:201–207.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 119: A consensus statement on the association of moderate alcohol consumption and health — 13 August 2013
A group of Italian scientists has prepared a consensus paper to review the available evidence on the association between moderate alcohol use and health and disease. The report resulted from extensive discussions among 36 prominent Italian scientists, and provides a working document for the scientific and health professional communities. The report has been signed by 19 separate societies or federations in Italy, including societies in nutrition, cardiology, and general medicine, as well as organizations of scientists dealing with diabetes, hypertension, and obesity.
The consensus report ends with four conclusions:
“(1) In healthy adults and in the elderly, spontaneous consumption of alcoholic beverages within 30 g ethanol/d for men and 15 g/d for women is to be considered acceptable and do not deserve intervention by the primary care physician or the health professional in charge. In fact, there is no evidence to suggest complete abstention from alcohol drinking by moderate users.
(2) Patients with increased risk for specific diseases, for example women with familiar history of breast cancer, or subjects with familiar history of early CVD or cardiovascular patients should discuss their drinking habits with their physician.
(3) No abstainer should be advised to drink for health reasons.
(4) Alcohol use must be discouraged in specific physiological or personal situations or in selected age classes (children and adolescents, pregnant and lactating women and recovering alcoholics). Moreover, the possible interactions between alcohol and acute or chronic drug use must be discussed with the primary care physician.”
Forum reviewers considered this to be a well-done and generally well-balanced appraisal of the current literature on alcohol and health; it could help inform physicians and the general public about our current knowledge on this topic. However, Forum reviewers were concerned by several aspects of the report where it appeared that the conclusions were more “political” than “scientific” (perhaps necessary to gain the support of all of the societies endorsing the report).
The authors of the report provided good data to support their first two conclusions, and recent publications that were not available to the authors at the time they prepared their report strongly support these conclusions. However, Forum members found little data provided in the paper to support the third statement in their summary; in fact, the information the authors presented in the text would tend to support the opposite conclusion. Further, while it may be correct, their fourth conclusion was not supported by scientific data in the paper.
Forum members agreed that the importance of the effects of alcohol consumption on total mortality must always be considered, and agreed with the statement of the authors that “Low levels of alcohol intake (1-2 drinks per day for women and 2-4 drinks per day for men) are inversely associated with total mortality in both men and women.”
Key areas that the Forum believed could have been given more emphasis related to the association between alcohol and diabetes mellitus, where data strongly support an approximately 30% lower risk for moderate drinkers, in comparison with non-drinkers. And the risk of cardiovascular disease is considerably reduced among diabetics who consume alcohol moderately. And the potential effects of moderate drinking on reducing the risk of congestive heart failure, a rapidly increasing health problem related to ageing of the population, were not discussed. Forum members also wished that more emphasis had been given in the consensus report to the pattern of drinking: current data indicate that regular moderate drinking, rather than binge drinking, is the pattern associated with the most favorable health outcomes.
Overall, this consensus report is an important and useful addition to the scientific literature on the relation of moderate alcohol consumption to a variety of health outcomes. It could be of great values to physicians and policy makers when providing advice to the public regarding the effects of alcohol on health.
Reference: Poli A, Marangoni F, Avogaro A . . . de Gaetano G . . . et al (total of 36 authors). Moderate alcohol use and health: A consensus document. Nutrition, Metabolism, & Cardiovasular Disease 2013;23:487-504.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 118: Clustering of alcohol consumption with socioeconomic and biologic risk factors for cancer — 30 July 2013
It has been shown in most previous studies that moderate drinkers, especially those who generally consume wine, tend to have other “moderate” lifestyle factors. For example, they tend to be better educated, of higher socio-economic status, and generally are more active and eat a healthier diet than non-drinkers. An exception is cigarette smoking, which tends to be more common in drinkers than in abstainers. Epidemiologists studying alcohol and health are always striving to adjust appropriately for other lifestyle factors, attempting to assure that the difference in health outcomes among subjects relates to their drinking, and not to associated lifestyle factors.
In the present study, the investigators related alcohol consumption to a large number of socio-demographic and lifestyle factors that relate to the risk of cancer. They report that several factors were associated with alcohol consumption ≥10g/d in both genders: older age, smoking, higher socio-demographic category, higher income, and less healthy dietary intakes. Other factors were associated with alcohol consumption differently for men and women. The authors then report that the total number of such factors was higher among consumers of ≥10g/d of alcohol than among abstainers or lighter drinkers. They conclude: “The multiplicity of deleterious lifestyle behaviours combined with alcohol drinking must be taken into account in cancer prevention efforts. Gender-specific medical advice for people with personal or family history of alcohol-related diseases, including cancer, should be strengthened.”
While Forum reviewers found the data presented in this paper to be of interest, they did not believe that simply adding up all adverse risk factors provided useful information for the prevention of cancer. It is well known that smoking is a major risk factor for certain cancers, and in almost all studies alcohol consumers are more likely to be smokers; hence, drinkers should certainly be advised about the dangers of smoking. On the other hand, by simply summing the number of factors into a total score, the authors included a number of risk factors for which there is less of a scientific basis for their effect on cancer risk (e.g, the intake of supplements). Such factors should not be given the same weight as smoking as risk factors for cancer. Further, this study was carried out among computer-literate volunteers, so it may have limited relevance for the general population.
There have been extensive data showing that “healthy” and “unhealthy” lifestyle factors tend to cluster: for example, light-to-moderate drinkers tend to be leaner and eat a healthier diet than non-drinkers or heavy drinkers, as shown in this study. However, the prevention of chronic diseases relates to a large number of behaviors, and alcohol consumption cannot be considered as an isolated factor. Current epidemiologic data suggest that the combination of not smoking, being physically active, eating a healthy diet, avoiding obesity, and, unless contraindicated, regularly consuming small amounts of an alcoholic beverage, together make up what can be defined as a “healthy lifestyle.”
Reference: Touvier M, Druesne-Pecollo N, Kesse-Guyot E, Andreeva VA, Galan P, Hercberg S, Latino-Martel P. Demographic, socioeconomic, disease history, dietary and lifestyle cancer risk factors associated with alcohol consumption. Int J Cancer 2013;in press
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 117: Changes in alcohol intake modify levels of fibrinogen, an important risk factor for coronary heart disease — 18 July 2013
A prospective analysis of data from 2,520 subjects in the Coronary Artery Risk Development in Young Adults Study (CARDIA) cohort related reported alcohol intake at two examinations, 13 years apart, to levels of fibrinogen on the two occasions. Fibrinogen is a strong determinant of thrombosis, and is an important risk factor for coronary heart disease. The authors report that, in comparison with participants who never drank, those who became/stayed drinkers had smaller increases in fibrinogen, while those who quit drinking had the highest increase in fibrinogen over 13 years of follow-up. They conclude that lower levels of fibrinogen may be a key mechanism for the established protective effect of moderate alcohol intake on cardiovascular disease outcomes.
Forum reviewers considered this to be a potentially important paper, as the finding of higher fibrinogen among never drinkers and those who quit drinking may relate to the higher risk of coronary disease commonly reported from such subjects in prospective studies. However, the reviewers point out that the reasons that subjects quit drinking are not known (although the authors did adjust for conditions related to quitting drinking). Further, blood clotting factors other than fibrinogen may be affected by changes in alcohol consumption, and they were not reported in this paper. More research will be needed to determine if changes in fibrinogen levels are key elements in alcohol’s effects on cardiovascular disease.
Reference: Okwuosa TM, Klein O, Chan C, Schreiner P, Liu K, Green D. Long-term change in alcohol-consumption status and variations in fibrinogen levels: the coronary artery risk development in young adults (CARDIA) study. BMJ Open 2013;3:e002944. doi:10.1136/bmjopen-2013-002944
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 116: Effects of genetic factors on the metabolism of alcohol — 10 July 2013
A summary paper on genetically determined mechanisms related to the metabolism of alcohol and acetaldehyde describes numerous ways that the metabolism, especially of acetaldehyde, may be modified, both in the periphery of the body and in the brain. Individuals with a mutation of the aldehyde dehydrogenase gene (the ALDH2*2 allele), and certain other genetically determined enzymes, do not tolerate alcohol and are much less likely to become alcohol abusers. The authors state that their studies suggest possible therapeutic avenues in the treatment of alcoholism.
Reference: Israel Y, Rivera-Meza M, Karahanian E, Quintanilla ME, Tampier L, Morales P, Herrera-Marschitz M. Gene specific modifications unravel ethanol and acetaldehyde actions. Front Behav Neurosci 2013;7:80.doi:10.3389/fnbeh.2013.00080
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 115: Potential association of alcohol consumption with diverticulosis — 25 June 2013
The etiology of diverticulosis of the colon is poorly understood. Many, but not all, studies suggest that low fiber intake and obesity increase the risk; few studies have evaluated the relation of alcohol consumption and diverticulosis, with inconclusive results. This paper tests the cross-sectional association of alcohol consumption with diverticulosis among 746 asymptomatic consecutive subjects undergoing screening colonoscopies in Lebanon.
One-half of the subjects in this study were abstainers. Most of the “drinkers” stated that they consumed alcohol occasionally or < 1 drink/day; only about 10% reported 1 or more drinks/day, and no data on type of beverage or pattern of drinking were available. Nevertheless, from their analyses the authors conclude that alcohol consumption raises the risk of diverticulosis.
Forum members considered that this cross-sectional analysis provides little support for a causative effect of alcohol on the risk of diverticulosis. Most larger observational studies have not shown such an effect. In the present study, about 90% of subjects were either abstainers or consumed alcohol only occasionally or averaged < 1 drink/day. Further, the investigators did not evaluate the pattern of drinking (including binge drinking) and the results do not support an increase in risk with greater drinking (lack of a dose-response relation). Mechanisms for such an effect are largely unknown. Thus, few of the Hill criteria for “causality” are met.
The authors’ use of an inter-country comparison of per-capita alcohol intake and reported diverticulosis has no relevance: there are large cultural differences between nations with high and those with low per-capita alcohol intake, and alcohol use may well have been just a marker for a western-type culture. While the present study could be used to generate an hypothesis of a relation of alcohol intake to diverticulosis, attempts to validate such an association will require much additional research.
Reference: Sharara AI, El-Halabi MM, Mansour NM, Malli A, Ghaith OA, Hashash JG, Maasri K, Soweid A, Barada K, Mourad FH, El Zahabi L. Alcohol consumption is a risk factor for colonic diverticulosis. J Clin Gastroenterol 2013;47:420–425.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 113: Metabolic and biochemical mechanisms by which alcohol consumption affects health — 11 June 2013
A large study from Australia, that included a high percentage of current or former alcohol abusers, related alcohol consumption with a variety of metabolic and biologic parameters that relate to health. Included were markers of lipid function, inflammation, glucose metabolism, and liver function. As expected, there was a linear increase in HDL-cholesterol with increasing alcohol intake; somewhat surprisingly, there was a linear decrease in insulin levels with increasing alcohol consumption (which may relate to the typical finding of a significantly lower risk of diabetes mellitus among moderate drinkers). Essentially all of the other factors showed a “J-shaped” or “U-shaped” relation with alcohol: a decrease with small to moderate amounts of alcohol and an increase with larger intake.
In their association with alcohol, the lowest (most favorable) values of parameters varied by the measure: lowest triglycerides at about 1 to 2 drinks per day, lowest CRP at about 1 drink/day, lowest blood sugar and lowest alkaline phosphatase values at 1 to 3 drinks/day. Adverse effects on liver enzymes, blood glucose, and inflammatory markers showed a threshold level of intake that varied somewhat by marker. For example, reported non-drinkers had higher values of CRP, triglycerides, and alkaline phosphatase; among drinkers, significant increases were seen only in consumers of 40 or more drinks/week. Unfortunately, the investigators did not report on the pattern of drinking, which usually shows preferable results from regular, moderate intake of alcohol with no binge drinking.
The key findings of the study can be summarized as favorable effects of moderate alcohol intake on HDL-cholesterol and insulin levels, and for most other factors (including liver enzymes, triglycerides, blood glucose, and the inflammatory marker CRP), a “J-shaped” relation: lower values with light drinking and higher values with larger amounts of alcohol. For most of these, there was either no effect or a favorable effect until alcohol intake exceeded a “threshold value,” at which heavier drinking began to show adverse effects.
Forum reviewers agreed with the conclusion of the authors: “The pattern of potentially beneficial effects of alcohol on HDL-C and insulin increasing progressively as consumption increases, whereas the negative effects show thresholds, is consistent with net U- or J-shaped effects of alcohol on health.” While actual health outcomes were not evaluated in this study, overall it provides strong support for the results of most prospective epidemiologic studies that show lower rates of cardiovascular and other diseases among light-to-moderate drinkers than among abstainers or heavy drinkers.
Reference: Whitfield JB, Heath AC, Madden PAF, Pergadia ML, Montgomery GW, Martin NG. Metabolic and biochemical effects of low-to-moderate alcohol consumption. Alcohol Clin Exp Res 2013;37:575–586.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 112: Relation of alcohol intake to risk of dying from cancer — 23 May 2013
This paper presents a meta-analysis that related alcohol consumption to all-cancer mortality; it was based on almost 50,000 deaths reported in the literature from prospective cohort studies. Forum reviewers had some concerns about the conclusions of the paper, based on some discrepancies in the text, the lack of data on drinking pattern, no beverage-specific results, etc. Nevertheless, as expected, the reported average consumption of 50 or more grams of alcohol per day (equivalent to 4 or more typical drinks each day) was associated with an estimated 32% increased risk of dying from cancer.
However, there was no increase in the estimated risk of cancer death for subjects classified as “moderate” drinkers (defined by the authors using a wide range of intake: 12.6 to 49.9 grams/day, the equivalent of up to approximately 4 or more typical drinks). Further, Forum members were surprised that a slight but statistically significant decrease in cancer mortality risk was seen for “light” drinkers (those reporting an average of ≤ 12.5 grams/day, or about one typical drink). Forum members appreciated that misclassification of cause of death or residual confounding could have contributed to this latter result.
It is especially important that the only significant increase in risk in cancer mortality among the almost 50,000 cancer deaths reported in this meta-analysis was for consumers of 50 grams or more of alcohol. This suggests strongly that the overall risk of cancer mortality related to alcohol consumption is primarily (perhaps almost exclusively) from heavier drinking. Certainly, the findings from this study do not support the premise that “any amount of alcohol increases the overall risk of dying from cancer.”
Reference: Jin M, Cai S, Guo J, Zhu Y, Li M, Yu Y, Zhang S, Chen K. Alcohol drinking and all cancer mortality: a meta-analysis. Ann Oncol 2013;24:807-816. doi: 10.1093/annonc/mds508.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 111: Association of alcohol consumption with a measure of osteoporosis in elderly women — 7 May 2013
The density of bones, measured as bone mineral density (BMD), is strongly related to osteoporosis. Elderly women with osteoporosis, in particular, are at increased risk of fractures of the hip, arm, and spine; such fractures often relate to severe disability. With data on alcohol collected as part of a clinical trial on the prevention of osteoporosis, investigators in Finland have related alcohol consumption to changes over three years in BMD. After those excluded due to incomplete data, data on 300 women were available for analysis. The majority of women were abstainers or consumed little alcohol. Nevertheless, the results support much earlier research: regular, moderate drinking is associated with higher levels of BMD (i.e., lower risk of osteoporotic fractures) than is abstinence.
Forum reviewers, as did the authors, noted a number of limitations of the study: a rather small cohort with a very low intake of alcohol, a short duration of follow up, and rather small differences according to whether the women consumed alcohol or not.
Data from European surveys have shown that women in Finland tend to have high levels of osteoporosis and to drink very little; hence the increase in BMD associated with alcohol intake, even though slight, could be important in this population. Over the past three decades, there has been an increase in alcohol consumption in Finland, especially a marked increase in the consumption of wine. Hence, some Forum reviewers thought that the improvement in BMD among drinkers in this study may have been primarily from wine (which may have additional components, other than alcohol, that relate to BMD). However, the number of subjects was not large enough to test this hypothesis in the present study. Overall, this study supports the premise that moderate alcohol intake, along with an adequate calcium intake and vitamin D and exercise, may have a favorable influence on the risk of developing osteoporosis
Reference: Sommer I, Erkkilä AT, Järvinen R, Mursu J, Sirola J, Jurvelin JS, Kröger H, Tuppurainen M. Alcohol consumption and bone mineral density in elderly women. Public Health Nutr 2013;16:704-712. doi: 10.1017/S136898001200331X.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 110: Divergent effects of regular moderate and binge drinking – 30 April 2013
The present study relates alcohol consumption measured in young to middle-aged adults to mortality over a follow-up period of 20 years. The analyses are based on data from a large population in a region of Norway where the alcohol drinking pattern most commonly reported was binge drinking on infrequent occasions. Previous research has demonstrated that a very different drinking pattern – the frequent consumption of small amounts of alcohol – is generally considered to be the pattern associated with most health benefits.
In the present study, both men and women who reported consuming alcohol up to twice a month had about 20% lower mortality than did abstainers. All groups reporting binge drinking had higher mortality than non-binge drinkers (which was statistically significant for men and had a similar estimated effect among women). Cardiovascular and ischemic heart disease mortality had similar patterns as total mortality, being lower among drinkers but higher among those who reported binge drinking.
The key finding of this study is that there are divergent effects on mortality of the frequency of drinking and the amount of alcohol consumed per occasion. While the results for this study may reflect a certain Northern European pattern of drinking (not frequent but heavy on each occasion), they may not apply to other European or North American populations, where drinking is more frequent but binge drinking less common. Nevertheless, the results of this study support results typically found in more moderately drinking populations: more frequent drinking, but smaller amounts per occasion, is the pattern of alcohol consumption associated with the lowest risk of mortality. Both aspects of drinking must be considered when studying the relation of alcohol to mortality.
Reference: Graff-Iversen S, Jansen MD, Hoff DA, Høiseth G, Knudsen GP, Magnus P, Mørland J, Normann PT, Næss ØE, Tambs K. Divergent associations of drinking frequency and binge consumption of alcohol with mortality within the same cohort. J Epidemiol Community Health 2013;67:350-357. doi:10.1136/jech-2012-201564.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 109: In women developing breast cancer, moderate alcohol consumption before or after diagnosis does not increase breast cancer mortality and decreases total mortality — 16 April 2013
Most previous research has shown a slight increase in the risk of breast cancer (BrCa) among women who consume alcohol (versus nondrinkers), even among those whose average is only one drink/day. The association with death due to breast cancer is less clear, although overall total mortality among moderate drinkers is almost always lower than among non-drinkers; this reduction is generally attributed to a lower risk of cardiovascular disease.
The present study related alcohol consumption, both prior to the diagnosis of BrCa and after the diagnosis, with survival; deaths from BrCa and from cardiovascular disease, as well as total mortality, were related to alcohol intake. Specifically, in this study the authors assessed alcohol intake in a cohort of 22,890 women with incident invasive breast cancer (BrCa) who were residents of one of four US states and diagnosed at ages 20 to 79 years. During a median follow-up period of 11.3 years after diagnosis of BrCa, 7,780 deaths occurred, including 3,484 attributed to breast cancer.
Based on a quadratic analysis, moderate alcohol consumption before diagnosis showed a tendency towards lower risk of death from BrCa, and a significantly greater reduction in the risk of cardiovascular disease mortality and total mortality. Alcohol consumption after diagnosis was not associated with disease-specific survival, but was associated with a lower risk of total mortality. For women consuming alcohol prior to the diagnosis of BrCa, those who decreased their intake showed little effect on mortality, while those who increased their intake showed further lowering of their risk of cardiovascular and total mortality.
Forum reviewers considered this to be an excellent paper providing important new data on the association of alcohol consumption with survival after a diagnosis of invasive breast cancer. They thought that the statements of the authors accurately reflected their data, as they concluded: “Overall alcohol consumption before diagnosis was not associated with disease-specific survival, but we found a suggestion favoring moderate consumption. There was no evidence for an association with postdiagnosis alcohol intake and breast cancer survival. This study, however, does provide support for a benefit of limited alcohol intake for cardiovascular and overall survival in women with breast cancer.”
An accompanying editorial* agreed with the conclusions of the authors. The editorial stated, “Based on the best available evidence, including [the present report], it appears that modest alcohol consumption after breast cancer diagnosis, up to approximately one drink per day on average, may be associated with optimal overall survival, without compromising breast cancer-specific survival.”
*Demark-Wahnefried W. To your health: How does the latest research on alcohol and breast cancer inform clinical practice? jco.ascopubs.org/cgi/doi/10.1200/JCO.2013.490466),
Reference: Newcomb PA, Kampman E, Trentham-Dietz A, Egan KM, Titus LJ, Baron JA, Hampton JM, Passarelli MN, Willett WC. Alcohol consumption before and after breast cancer diagnosis: Associations with survival from breast cancer, cardiovascular disease, and other causes. J Clin Oncol 2013; pre-publication. Available at jco.ascopubs.org/cgi/doi/10.1200/JCO.2012.46.5765
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 108: An unusual paper relating alcohol consumption to the risk of stroke
Numerous well-done prospective epidemiologic studies have shown that while heavy drinking may increase the risk of stroke, light-to-moderate alcohol consumption is usually associated with a significant decrease in the risk of the most common type of stroke, ischemic stroke.
This paper from investigators in Finland states that it was designed to relate alcohol consumption and obesity to the risk of ischemic stroke. Unfortunately, even though it has clearly been shown that the amount and pattern of alcohol consumption strongly modify the effect on the risk of stroke, for some unknown reason the authors have grouped all consumers of alcohol into a single group. Specifically, there are no data given that describe the relation of light-to-moderate alcohol consumption with stroke. Hence, the conclusion of the authors that “alcohol increases the risk of stroke” is not supported by the data presented. In the opinion of members of the Forum, without reporting the effects according to the amount of alcohol consumed or the pattern of drinking, this is an unsupported and potentially dangerous statement to present in a scientific journal.
Reference: Rantakömi SH, Laukkanen JA, Sivenius J, Kauhanen J, Kurl S. Alcohol consumption and the risk of stroke among hypertensive and overweight men. J Neurol 2013;260:534–539. DOI 10.1007/s00415-012-6672-6
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 107: Little effect on child’s mental functioning associated with mother’s light, occasional drinking in early pregnancy – 25 March 2013
A new report from the prospective, population-based Avon Longitudinal Study of Parents and Children (ALSPAC) in the UK is based on investigation of the association between light drinking in pregnancy (<1 glass per week in the first trimester) and child mental health. Mental health was assessed in more than 6,000 children using both parent- and teacher-rated Strengths and Difficulties Questionnaires (SDQs) at age 11 years. Academic outcomes based on Key Stage 2 examination results were measured in more than 10,000 children.
Approximately 40% of women consumed some alcohol but less than 1 glass/week, while 16% reported consuming ≥1 glass per week during the first trimester. The authors report that after adjustment, relative to abstainers, there was no effect of light drinking on teacher-rated scores or examination results. In girls, although there was a suggestion of worse outcomes on the parent-rated total score in those exposed to light drinking compared to abstainers, no dose–response relationship was evident. The authors conclude: “Light drinking in pregnancy does not appear to be associated with clinically important adverse effects for mental health and academic outcomes at the age of 11 years.”
Forum reviewers considered this to be a well-done study, with a balanced assessment of results by the authors. Reviewers were surprised at the somewhat arbitrary separation of alcohol consumption: <1 drink per week versus ≥1 drink per week. Current guidance about alcohol consumption in pregnancy from the Department of Health in England (2009) allows for pregnant women to drink up to 1–2 units of alcohol once or twice a week, and it would have been preferable to have data presented for drinkers at this level.
Forum Co-Director Conibear considered that “The most important aspect of this study relates to the fact that 25% of babies in the UK are unplanned, and 17% of mothers do not know they are pregnant until eight weeks or more. Therefore balanced advice concerning the effect of alcohol use in early pregnancy is crucial to prevent unnecessary concern amongst this group of mothers to be. Although the best advice is to avoid alcohol if you are pregnant, the present research can reassure mothers who drank occasionally without realising that they were pregnant that they have not done long-term harm to their baby.”
Forum reviewer Stockley added: “I think that another important message is that if a woman decides to consume a small amount of alcohol during pregnancy, she should never binge drink or get drunk. This we know can have adverse effects on the developing fetus, especially in the first trimester, but interestingly, also in the third trimester of pregnancy.”
Reference: Sayal K, Draper ES, Fraser R, Barrow M, Davey Smith G, Gray R. Light drinking in pregnancy and mid-childhood mental health and learning outcomes. Arch Dis Child 2013;98:107–111. doi:10.1136/archdischild-2012-302436.
For the full critique of this publication by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 106: A clinical trial shows that glucose metabolism is improved more by red wine than by gin — 14 March 2013
To compare the effects of moderate consumption of red wine, dealcoholized red wine, and gin on glucose metabolism and the lipid profile, a group of Spanish investigators carried out a randomized control trial among 67 men at high cardiovascular risk. All received each of red wine (30 g alcohol/d), the equivalent amount of dealcoholized red wine, and gin (30 g alcohol/d) for 4 week periods, in a randomized order. While fasting glucose levels were not affected, mean adjusted plasma insulin and HOMA-IR decreased after red wine and dealcoholized red wine, but not after gin. HDL cholesterol, Apolipoprotein A-I and A-II increased after red wine and gin. Lipoprotein(a) decreased after the red wine intervention. The authors conclude that their results support a beneficial effect of the non-alcoholic fraction of red wine (mainly polyphenols) on insulin resistance, thus greater protective effects on cardiovascular disease from red wine than from other alcoholic beverages.
Forum members were unanimous in considering this to be a very well-done and important trial. It supports a huge amount of observational data from epidemiologic cohort studies that have shown that subjects who consume moderate amounts of alcohol tend to have much lower risk of developing diabetes. Further, patients with diabetes who drink moderately have much lower risk of subsequent cardiovascular disease and lower mortality. Studies such as this one help scientists understand the mechanisms by which moderate drinking, especially of wine, can reduce the risk of metabolic and vascular diseases.
Reference: Chiva-Blanch G, Urpi-Sarda M, Ros E, Valderas-Martinez P, Casas R, Arranz S, Guillén M, Lamuela-Raventós RM, Llorach R, Andres-Lacueva C, Estruch R. Effects of red wine polyphenols and alcohol on glucose metabolism and the lipid profile: A randomized clinical trial. Clinical Nutrition 2013. Pre-publication. dx.doi.org/10.1016/j.clnu.2012.08.022.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 105: For preventing cardiovascular disease, an unrestricted-calorie Mediterranean-type diet provides 30% more benefit than a low-fat diet: Results of a large population-based clinical trial — 6 March 2013
A large well-done clinical trial in Spain was carried out among 7,447 subjects at high-risk of cardiovascular disease (on the basis of diabetes, hypertension, dyslipidemia, and other risk factors). The trial compared the effects of two versions of an energy-unrestricted Mediterranean-type diet, one with large amounts of extra-virgin olive oil (EVOO) and one with a supplement of mixed nuts, with results among subjects in a “control group,” made up of subjects who were advised to follow a low-fat, low-cholesterol diet (that has typically been recommended for reducing the risk of cardiovascular disease).
Both of the groups advised to consume a Med-Diet showed an increase in total fat, from an average of 39.3 % of total calories to an average of more than 41%; the group advised to decrease their total fat lowered their intake from 39 to 37 % of calories. All three groups showed slight decreases in saturated fat and slight decreases in dietary cholesterol intake (but blood cholesterol levels were not reported). Only the Med-Diet + nuts group showed an increase in alpha-linolenic acid (ALA), the fatty acid related to the lowest risk of cardiovascular disease in the Cretan cohort of the Seven-Countries Study and in the Lyon Diet-Heart Study.
The large majority of subjects in all groups consumed wine at baseline, and about one-third of the Med-Diet groups and one-quarter of the control group reported consuming ≥ 7 glasses of wine/week during the trial. However, alcohol consumption was not evaluated specifically for its effects in the present study.
The study was ended early by its data and safety monitoring board due to marked advantages being shown in terms of the occurrence of the primary end-point (the occurrence of myocardial infarction, stroke, or death from cardiovascular causes) in both Med-Diet groups in comparison with the control group. The multivariable-adjusted hazard ratios were 0.70 and 0.72 for the Med-Diet with olive oil and the Med-Diet with added nuts, hence an approximately 30% decrease in risk among subjects assigned to a Med-Diet compared with those in the control group.
Forum members (as did the authors) had difficulty in determining which specific components of the Med-Diet may have been the primary reasons for its more favorable results, as significant dietary changes during the trial were mainly related to the supplementary olive oil or nuts given to subjects in the two Med-Diet groups. Among potential factors were increased mono-unsaturated fat and higher antioxidants from the added EVOO and an increase in ALA from the supplemental nuts. Forum members noted that the Med-Diet interventions apparently did not provide an increase in the intake of ALA, which could have led to even more protection against cardiovascular disease.
In any case, the striking reduction in risk shown in the study from the Med-Diet provide further evidence of the effectiveness of such a diet in reducing cardiovascular disease. It has been shown repeatedly that people advised to consume a Mediterranean-type diet tend to comply much better with such advice than do people advised mainly to decrease their intake of all fats and cholesterol. A very large amount of scientific data now support advice to follow a Mediterranean-type diet, one that does not restrict calories but encourages the intake of selected fats (which may include extra-virgin olive oil or canola oil), as well as more fruits, vegetables, grains, nuts, and wine; it may be the most effective dietary approach for reducing cardiovascular disease.
Reviewer Keil points out that many good prospective cohort studies have shown that an increase in adherence to components of a Mediterranean-type diet decreases the risk of many diseases and mortality. He adds: “The great thing about the present study is that when the skeptics raise their voice and argue that the proponents of the Mediterranean diet have only observational data available, we can now respond that we not only have RCT data on secondary prevention (Lyon Diet-Heart study) but also the present study on primary prevention of cardiovascular disease.”
Reference: Estruch R, Ros E, Salas-Salvadó J, Covas M-I, Corella D, Arós F, et al, for the PREDIMED Study Investigators. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 2013. DOI: 10.1056/NEJMoa1200303
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please clickhere.
===============================================================================
Critique 104: Moderate alcohol consumption is associated with a lower risk of diabetes — 26 February 2013
A population-based longitudinal study in Norway showed a lower risk of developing type II diabetes, and a tendency for less auto-immune diabetes, among subjects reporting moderate alcohol consumption. The lowest risk was among subjects reporting that they consumed alcohol 5-10 times during the previous two weeks or reporting a daily consumption of 10-15 grams of alcohol per day (slightly less than one to a little over one drink per day, using 12 g of alcohol per day as a “typical drink”).
The overall results from this study support most previous research showing a rather large (approximately 30% or more) reduction in the risk of Type II diabetes mellitus to be associated with moderate drinking. In this study, the strongest protective effect related to the consumption of wine, rather than beer or spirits. Unlike some previous research, the present study did not show an increased risk of diabetes among binge drinkers, heavier drinkers, those reporting episodes of intoxication, or those giving positive responses on a CAGE questionnaire (a measure of an alcohol use disorder). As it is likely that alcoholics were under-represented in the cohort, the ability to show the effects of very heavy drinking may have been limited.
While the numbers of subjects with auto-immune diabetes were small, there was a tendency seen for a similar reduction in risk with moderate drinking as with the much more common Type II diabetes. Overall, this study strongly supports much previous research showing that moderate alcohol consumption is associated with a lower risk of developing diabetes.
Reference: Rasouli B, Ahlbom A, Andersson T, Grill V, Midthjell K, Olsson L, Carlsson S. Alcohol consumption is associated with reduced risk of Type 2 diabetes and autoimmune diabetes in adults: results from the Nord-Trøndelag health study. Diabet Med 2013;30:56–64.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 103: Alcohol intake just prior to bed-time may affect your sleep patterns — 18 February 2013
A paper from experts in the science of sleep provides an excellent review of intervention studies since the 1980s on the effects of alcohol consumption on sleep. The study finds that the time required to fall asleep, and sleep patterns in the first part of the night, tend to be improved by alcohol. The authors conclude that “The onset of the first REM sleep period is significantly delayed at all doses and appears to be the most recognizable effect of alcohol on REM sleep, followed by the reduction in total night REM sleep.” Slow-wave sleep is more common and REM sleep less common after alcohol.
The studies reviewed in this report were intervention studies among mainly young normal subjects, not people with sleep disorders. Other studies have demonstrated that small amounts of alcohol given in the evening to the elderly may improve sleep, and reduce the need for sleep-inducing medications. Overall, the data reviewed in this paper suggest that small amounts of alcohol in the evening have few adverse effects on sleep, and relate to earlier onset of sleep and less awakening in the first part of the night. Larger amounts of alcohol tend to make the onset of sleep faster, but may have some adverse overall effects on sleep patterns, with a shorter duration of REM sleep throughout the night.
Reference: Ebrahim IO, Shapiro CM, Williams AJ, Fenwick PB. Alcohol and sleep I: Effects on normal sleep. Alcohol Clin Exp Res 2013;doi: 10.1111/acer.12006. [Epub ahead of print]
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Requested comments on paper by Nelson et al
by R. Curtis Ellison, MD, Professor of Medicine & Public Health,
Boston University School of Medicine
NOTE: These comments do not necessarily reflect the views of the members of the International Scientific Forum on Alcohol Research
Nelson DE, et al. Alcohol-attributable cancer deaths and years of potential life lost in the United States. Am J Pub Health, released February 14, 2013
We always welcome new scientific publications that help elucidate factors related to the development of cancer. The new paper by Nelson et al focuses on the role that alcohol consumption may play in the risk of a number of cancers.
Background: It has long been appreciated that there are a number of upper aero-digestive cancers, such as cancer of the mouth, throat, and esophagus, that occur much more frequently in heavy drinkers, especially alcoholics, than in abstainers. Physiologic studies suggest that these are not diseases of light to moderate drinkers, as a certain amount of alcohol is required to produce these diseases. Similarly, among people consuming enough alcohol to lead to liver cirrhosis, the risk of liver cancer is also markedly increased.
These “alcohol-related cancers” should be discussed separately from other more common cancers – especially colon cancer and female breast cancer – for which the risk may be only slightly increased by alcohol. In the case of breast cancer, there may be a slight increase in risk among some women consuming an average of only one drink/day (in some studies, such an increase in risk occurs primarily among women who binge drink, have an inadequate intake of folate, and/or are also on hormone replacement therapy.)
For these types of cancer, it is especially important to consider the net health effects of alcohol consumption. For example, it is estimated that if a woman at average risk of breast cancer (i.e., does not have such a cancer in a first-degree relative) decides to avoid drinking completely in hopes of reducing her risk of breast cancer, her risk of breast cancer would be expected to be slightly decreased, on average, by perhaps 5-10%; however, her risk would be increased of dying from much more common diseases such as heart attack, stroke, or other conditions for which small amounts of alcohol have been shown to reduce risk. And, importantly, her risk of dying of any cause (total mortality) would actually be increased by her avoiding light alcohol consumption.
The pattern of drinking has often been shown to be even more important than the average amount of alcohol consumed. A stronger association with beneficial effects is seen with the regular (up to daily) intake of small amounts of an alcoholic beverage; drinking larger amounts on fewer days (including binge drinking) is almost always associated with adverse health effects. For example, a man having up to 2 drinks each day would have an average of 14 drinks per week, generally considered to be within recommended guidelines. However, a man consuming 7 drinks on each of only two days each week, despite the same weekly average consumption, would not be considered to be a moderate drinker.
Comments on the present paper: There are a number of concerns about the analyses and conclusions of the authors of the present paper. These include the following:
(1) The authors have “corrected” the reported data on alcohol consumption to make up for presumed under-reporting, using a method not generally accepted by statisticians and other researchers. This means that even many “light” drinkers are listed as reporting greater amounts of alcohol.
(2) The authors do not clearly separate the effects of truly moderate drinking from heavier drinking in their conclusions. They use up to 20 grams of alcohol per day as their lowest drinking category; this is higher than the 14 g/day that is the current definition of responsible drinking for women in the US Guidelines. Further, as stated, if reported intakes are increased artificially, many more light drinkers would be bumped up into higher categories of drinking. The result of this mis-categorization is that bona fide moderate drinking, which has been shown by others to have no association with most types of cancer, is improperly associated in this study with increased cancer.
(3) The authors’ implications that even regular, moderate drinking increases the risk of many cancers is not consistent with most previous research. Further, by not having data on the pattern of drinking, the authors include binge drinkers in the same category as regular drinkers, further exaggerating the association of cancer with moderate drinking. Others have clearly shown that there are large differences in effect between these two patterns. (It is troubling also that in the paper, the estimated percentage of alcohol-attributable cancer risk among subjects reporting > 0 to 20 grams of alcohol per day is much higher than that of subjects reporting > 20 to 40 grams/day; while this partly relates to the large number of persons who drink only small amounts, such an association makes no sense biologically. It is difficult to understand who the subjects are in the lowest drinking group, but it may include a large percentage of ex-alcoholics or heavier drinkers underreporting their intake. However, this makes any conclusions in this paper regarding the risk of cancer among moderate drinkers highly suspect.)
(4) The authors do not point out the demonstrated effects of alcohol on total mortality; regular, light-to-moderate drinkers live longer. By focusing only on cancer risks, the authors fail to mention the effects on the risk of much more common conditions, such as coronary heart disease, stroke, dementia, other important health problems of ageing, and on total mortality. The study of the health benefits and problems of drinking is a very mature field — authors generally discuss their observations in the context of total mortality or other major diseases that would be affected by their experimental design. In nearly all cases, light drinking is shown to be beneficial; these studies are ignored here.
(5) Overall, a criticism of this paper relates to the failure of the authors to put their results into perspective. Statements such as “There is no safe threshold for alcohol and cancer risk” is more of a “scare” statement than a balanced discussion of their results. Given that almost all prospective studies show that regular moderate drinkers have better health as they age and live longer than lifetime abstainers, even papers focused on the effects of alcohol on any particular disease should present a balanced view on its net effects on health and disease.
(6) Finally, the authors of this paper have taken the results of their analyses (some of which are based on questionable assumptions) as “truth,” then expounding at length about the public health implications. There should always be a certain amount of doubt when presenting the results of an individual study, as no one analysis can possibly reveal everything about an association. (As stated by Voltaire: “Doubt is not a pleasant condition, but certainty is absurd!)
As the authors acknowledge, observational epidemiologic data can never reveal the full “truth” about the causation of disease from exposures, and each new study’s results must be interpreted taking into consideration previous research. However, the overall implications presented by the authors of this paper suggest that their goal may have been to support a presumed conclusion to discourage alcohol consumption, not to carefully interpret the available data to best advance the public health.
Key points of these comments
- There are a number of assumptions taken by the authors in their analyses that raise questions about their results. The authors present only “adjusted” data for reported alcohol intake (based on national sales, not on individual intake), making the relation of alcohol intake to the occurrence of cancer in individuals unclear.
- There is poor differentiation between regular moderate drinking and periodic heavy drinking (binge drinking) or alcoholism, although there are marked differences in health effects between these groups. Regular, moderate drinking is associated with net health benefits, whereas binge drinking and alcoholism have almost exclusively adverse effects (including increases in many types of cancer).
- There has been a huge amount of previous research in this field, but the authors do not put their own results into perspective or discuss the overall health effects of alcohol consumption. Previous data have clearly shown that regular moderate drinkers tend to have lower risk of cardiovascular disease, stroke, diabetes, and many other diseases, and have a lower overall risk of all-cause mortality.
Submitted by
- Curtis Ellison, MD, Professor of Medicine & Public Health; Director, Institute on Lifestyle & Health;l Boston University School of Medicine
Co-Director, International Scientific Forum on Alcohol Research
===============================================================================
Critique 102: Possible prevention of myocardial infarction from alcohol’s effects on periodontal disease: An hypothesis — 6 February 2013
A cross-sectional analysis among more than 5,000 Norwegian men was designed to determine if the frequency of alcohol consumption related to the risk of myocardial infarction associated with infectious periodontal disease. The authors hypothesized that because it is bactericidal, frequent alcohol consumption would decrease periodontal infection and lower the risk of tooth extraction related to periodontal infection. The authors state that their main finding was that frequent drinking lowers the risk of MI associated with periodontal disease.
Forum reviewers had real concern about the paper and the conclusions of the authors. Some stressed that the per cent of alcohol in most “drinks” is too low to be really bactericidal, that the key exposures (alcohol and oral infections) were based exclusively on self report and did not have information on type of beverage or pattern of drinking, that many confounders (especially related to socio-economic status) were not adequately taken into consideration, and that the authors did not really test the results of their study with appropriate statistical testing.
Current scientific data show an increase in the risk of cardiovascular disease to be associated with periodontitis. Further, data consistently show a decrease in the risk of cardiovascular disease from moderate drinking, and a very large number of mechanisms have been identified. However, the present study does not confirm that alcohol consumption plays an important role in preventing heart disease through its effect on periodontitis.
Reference: Håheim LL, Olsen I, Rønningen KS. Oral infection, regular alcohol drinking pattern, and myocardial infarction. Medical Hypotheses 2012;79:725–730.
For the full critique of this article by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 101: A review of the association of alcohol consumption with the risk of developing hypertension — 22 January 2013
A meta-analysis from investigators at Columbia University in New York evaluated the risk of developing hypertension according to the level of alcohol consumption previously recorded. The analyses were based on data from 16 prospective studies. The paper’s main results are that among men, there is little effect of alcohol consumption up to 30 grams of alcohol per day (the equivalent of about 2 ½ “typical drinks” by US standards or more than 3 drinks by UK standards), but evidence of an increased risk of hypertension for the intake of greater amounts of alcohol. For women, light drinking appears to be associated with a slightly lower risk of hypertension, but more than 20 grams/day of alcohol may increase the risk.
While Forum members thought that the analyses were done well, they had some concerns about the conclusions of the authors, some of which appear to not be in line with the data they presented. For example, their statement that “heavier alcohol consumption >20 g⁄d is associated with the risk of development of hypertension in both women and men” is not consistent with their findings of a significant increased risk of hypertension only with an intake of 31 – 40 grams of alcohol per day.
Similarly, the authors conclude: “Even for light drinkers, vigilant blood pressure monitoring is necessary,” which may not be appropriate given that their data show that intake below 30 grams per day has no significant association with hypertension in men and may actually reduce the risk of hypertension in women.
Overall, the results of this study, in line with findings from most previous research, indicate that people who consume alcohol according to most current drinking guidelines (no more than 2 typical drinks/day for men or 1/day for women) do not show an increase in their risk of hypertension, but heavier drinking appears to increase the risk. Not discussed in this paper, but especially important in terms of health, is that light drinking is associated with a significant and rather large decrease in the risk of the most serious sequelae of hypertension: coronary heart disease and ischemic stroke.
Reference: Briasoulis A, Agarwal V, Messerli FH. Alcohol consumption and the risk of hypertension in men and women: A systematic review and meta-analysis. J Clin Hypertens 2012;14:792-798.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 100: The effects of moderate drinking on cognitive function and dementia: An update — 15 January 2013
A paper from a group of Italian scientists provides an extensive review of the available research relating alcohol consumption to cognitive function. It presents brief summaries of results from most key epidemiologic studies dealing with this topic between 1987 and 2011. The large majority of these studies, and recent meta-analyses, support a finding of a lower risk of cognitive impairment from ageing and of dementia to be associated with moderate drinking.
Reviewers praised the authors for pointing out difficulties caused by having to develop guidelines for alcohol consumption based only on observational data, and not having large clinical trials for judging effect. A further problem faced in judging the numerous studies on this topic is that many lack data on beverage type and most lack detailed information on the pattern of drinking, which may be especially important in judging the effects of drinking.
Some reviewers stated that the paper does not present anything new, as previous meta-analyses have clearly shown a potentially protective effect of moderate alcohol consumption on the risk of cognitive decline and dementia. Given that recent large meta-analyses have shown that moderate drinking, is comparison with abstention, is usually associated with 20-35% lower risk of cognitive decline and dementia, Forum reviewers thought that the conclusions of the authors of this review paper were unnecessarily cautious. Overall, current scientific data support a conclusion that moderate consumption of alcoholic beverages, especially of wine, is neuroprotective.
Reference: Panza F, Frisardi V, Seripa D, Logroscino G, Santamato A, Imbimbo BP, Scafato E, Pilotto A, Solfrizzi V. Alcohol consumption in mild cognitive impairment and dementia: harmful or neuroprotective? Int J Geriatr Psychiatry 2012;27:1218-1238.
For the full review of this critique by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 099: Alcohol and survival after postmenopausal diagnosis of breast cancer — 20 December 2012
This paper assessed the association of pre-diagnostic alcohol consumption with disease recurrence and survival in a prospective cohort study in Germany based on 2,522 postmenopausal breast cancer patients, aged 50–74 years. The authors report that alcohol consumption was non-linearly associated with increased breast cancer-specific mortality, but not with breast cancer recurrence. Results were independent of estrogen receptor status. The authors also report a non-significantly decreased risk of mortality due to other causes.
Forum reviewers considered this to be a well-done analysis that was limited, however, by the lack of data on drinking patterns prior to breast cancer diagnosis and because no data were available on drinking after the diagnosis (the latter limits the applicability of its results to women who have already developed breast cancer). The comparisons were primarily between non-drinkers/light drinkers and women in the highest alcohol category; the authors state that when ex-drinkers were removed from the referent category, their results regarding breast cancer-specific mortality were no longer statistically significant. The authors do not describe the potential effects on their main results that could result from what is known as “index event bias,” which may occur when an exposure (e.g., alcohol) relates to the development of a disease, breast cancer in this study, and may also relate to sequelae (e.g., recurrence or death) from the same disease.
Forum reviewers conclude that current scientific data show that alcohol consumption may increase the risk of developing breast cancer. However, they believe that the effects on subsequent survival after such a diagnosis remain unclear.
Reference: Vrieling A, Buck K, Heinz J, Obi N, Benner A, Flesch-Janys D, Chang-Claude J. Pre-diagnostic alcohol consumption and postmenopausal breast cancer survival: a prospective patient cohort study. Breast Cancer Res Treat 2012;136:195–207. DOI 10.1007/s10549-012-2230-2
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 098: Moderate alcohol consumption may lower the risk of developing depression — 13 December 2012
Analyses from a prospective study of more than 13,000 adults in Spain related baseline alcohol intake (mainly wine) with the development of depression, with the outcome based on a physician’s diagnosis or on the habitual use of anti-depressant drugs for four or more years. Reported depression was much higher among women than men. Among women, the estimated hazard ratios for groups reporting an average alcohol intake of < 5 g/day of alcohol, 5-15 g/day, and > 15 g/day were 0.97, 0.62, and 0.84 (in comparison with subjects reporting no alcohol). The difference was statistically significant (CI = 0.43-0.89) for the group reporting 5-15 g/day.
Few men reported a diagnosis of depression; among moderately drinking men, the estimated risks of depression were similar to those of women, but none of the differences were statistically different from those of non-drinkers. The investigators found no differences according to the type of alcoholic beverage consumed.
The merits of this study include that the data were collected prospectively, that there were repeated questionnaires seeking data on depression, and that there were a large number of subjects, all of whom were college graduates. There were few men reporting depression, and few heavy drinkers, so results apply only to moderately drinking women. Among these women (those consuming between about ½ drink/day to about 1 or 1 ½ drinks per day) there was evidence of a lower risk of depression during a follow-up period extending up to 10 years.
Forum reviewers thought that this was a well-done analysis, and the use of cut-points for drinking groups according to spline analyses was appropriate. Some reviewers cautioned that moderate drinkers, especially regular wine drinkers, tend to have a large number of other healthy lifestyle habits that could relate to the risk of depression. While many of the recognized potential confounders were included in the Cox regression analysis in this paper, it will be important to determine if future studies support the conclusions of the authors.
Reference: Gea A, Martinez-Gonzalez MA, Toledo E, Sanchez-Villegas A, Bes-Rastrollo M, Nuñez-Cordoba JM, Sayon-Orea C, Beunza JJ. A longitudinal assessment of alcohol intake and incident depression: the SUN Project. BMC Public Health 2012, 12:954 doi:10.1186/1471-2458-12-954
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 097: Per-capita alcohol intake and all-cause mortality in Australia — 4 December 2012
An ecologic analysis from a group in Australia has related trends in the per-capita consumption of alcohol in Australia with rates of all-cause mortality. Unfortunately, the authors do not have data on individual consumption of alcohol (and no way of knowing if the people who drink or do not drink are those who die) and do not have data on many key factors that relate to both alcohol consumption and mortality (e.g., education, income, diet, occupation, etc.). Especially, they have no data on the patterns of consumption of members of the population (regular moderate intake or binge drinking). They “adjust” for death rates in women but do not report sex-specific mortality rates.
This paper illustrates many of the dangers of the so-called “ecologic fallacy,” in which comparisons are made between aggregate population data and biologic outcomes. It has been shown that such comparisons may be of interest in generating hypotheses, but not for answering questions of causation, for which different types of studies are required. As stated in a leading textbook of epidemiology: “Ecologic analysis poses major problems of interpretation when making ecologic inferences and especially when making biologic inferences. In contemporary epidemiology, the ‘ecologic fallacy’ reflects the failure of the investigator to recognize the need for biologic inference and thus for individual-level data. This need arises even when the primary exposure of interest is an ecologic measure and the outcome of interest is the health status of entire populations.”
With such serious limitations from the use of ecologic comparisons, this paper does not provide data upon which alcohol policy can be based. The authors of this paper appear to have ignored previous research providing very different interpretations of an inverse association between per-capita alcohol intake and mortality. A plethora of studies based on alcohol intake among individuals, and especially patterns of consumption, provide data needed for such policy decisions.
Reference: Livingston M, Wilkinson C. Per-capita alcohol consumption and all-cause male mortality in Australia, 1911–2006. Alcohol and Alcoholism 2012. Pre-publication: doi: 10.1093/alcalc/ags123
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 096: Frequency of alcohol consumption and cardiovascular risk factors: implications for drinking guidelines — 20 November 2012
As stated by the authors, “many observational studies suggest that increased drinking frequency is associated with reduced mortality among those with low-dose alcohol consumption. The purpose of this paper was to examine whether frequent drinkers consume lower-risk amounts during drinking days or have favorable risk factor profiles compared with those who drink less frequently, and discuss implications for the larger debate about the limitations of non-randomized studies about ‘moderate’ drinking and the development of low-risk drinking guidelines.” Indeed, previous epidemiologic research has clearly shown that the healthiest outcomes occur among regular, moderate drinkers who do not binge drink. Further, almost all studies have adjusted for a large number of socio-economic factors that are known to be potentially confounding factors for evaluating the association of alcohol consumption with health outcomes.
As expected, the present study shows that regular drinkers tend to consume less alcohol per occasion, and are less likely to binge drink. Further, such individuals tend to have better socio-economic status and lower levels of most cardiovascular risk factors. Most previous researchers have interpreted the better educational status and economic levels of moderate drinkers to be important causes of their more moderate lifestyle factors (including avoiding abusive drinking). Further, most previous research, including many basic science interventions and limited trials in humans, have shown that the administration (intake) of moderate amounts of an alcoholic beverage leads to more favorable cardiovascular risk factors, and numerous mechanisms have been identified (higher HDL-cholesterol, improved vascular reactivity, improved platelet and other coagulation factors, etc.).
The authors of this paper take an unusual turn when it comes to discussing the implications of their results. They tend to down-play any potential health benefits that may be caused by alcohol or the pattern of drinking and infer instead that the favorable risk factors themselves may lead to the drinking pattern. Forum members disagreed with the implications of the authors on a number of factors: (1) the lack of randomized trials of low-dose alcohol consumption; (2) levels of evidence; (3) drinking frequency and alcohol intake; (4) clustering of lifestyle behaviors; (5) alcohol consumption and CVD-related biomarkers; (6) alcohol intake, cancer and total mortality. Further, Forum reviewers cite a large body of scientific research that refutes some of the conclusions of the authors, e.g., that regular moderate alcohol intake does not relate to improved cardiovascular risk factors.
Forum reviewers agree with a concluding statement of the authors about using caution before recommending drinking to the general public. However, they believe that the arguments presented in this paper are not based on a balanced appraisal of available scientific data, and should not be used to support changes in guidelines for the public.
Reference: Naimi TS, Xuan Z, Brown DW, Saitz R. Confounding and studies of ‘moderate’ alcohol consumption: the case of drinking frequency and implications for low-risk drinking guidelines. Addiction 2012; pre-publication. doi:10.1111/j.1360-0443.2012.04074.x.
For the complete critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
A Tribute to Francesco Orlandi
(1927 – 2012)
It is with sadness that we have learned of the death on 12 November 2012 in Ancona, Italy, of Francesco Orlandi, MD. Francesco was a founding member of our International Scientific Forum on Alcohol Research, and a frequent and valuable contributor to our critiques. He will be sorely missed, both as a friend and as a respected scientist. Besides his strong passion for science, he was an extraordinarily cultivated man, rich in his sense of humor, and a sincere friend of many members of our Forum.
Francesco Orlandi was Professor of Gastroenterology at the University of Ancona from 1975 to 1999 and Direttore, Dottorato di ricerca Alimenti e Salute, 1997-99. He also served as Professor on wine and health at the Corso di Laurea Specialistica in Scienze Viticole ed Enologiche at the University of Turin.
Francesco was counselor and coordinator of the “wine and health” group of the Accademia Italiana della Vite e del Vino, and an OIV expert at the Italian Ministry of Agricultural, Food and Forestry Policies in Rome. In addition, he served as Visiting Professor in the Department of Medicine, Albert Einstein College of Medicine, New York, in 1977-8.
Francesco was always interested in the study of the health risks and benefits of alcohol consumption. In the 1990’s, he performed a number of experimental studies in rats on the mechanisms of early ethanol-induced liver damage, with particular attention to apoptosis and cell proliferation.
More recently Francesco became increasingly interested in the beneficial effects of moderate alcohol consumption on human health. He became convinced that only by working in a multi-disciplinary context could young investigators contribute to a new renaissance of alcohol and wine research in Italy. This is why in June, 2011, he organized the first seminar on responsible drinking in the context of the Mediterranean Diet, which was held in the ancient Pontignano Abbey, near Siena. There he brought together all young Italian scientists involved in this field of research; the abstracts of this meeting have been published (Eur J Nutr 2011;50:489–498).
As stated by a Forum member, Francesco was much more than a great doctor and an outstanding scientist. He was an old style gentleman, able to use the right words in every social context. He was an extremely educated person, cultivating interests from art, music, and sailing to science with the emotional motivation, intellectual freedom, and motivated curiosity that usually only young talents can have. Francesco will remain forever a young enthusiastic scientist for all of us who had the fortunate chance of interacting with him.
These comments provided by members of the International Scientific Forum on Alcohol Research (www.bu.edu/alcohol-forum)
15 November 2012
===============================================================================
Critique 095: Effects of alcohol on lymphoma, leukemia, and other types of hematological cancers —- 13 November 2012
Many observational epidemiologic studies have found an inverse association between alcohol consumption and hematological cancers (such as lymphoma and leukemia). This study, based on the Million Women’s Study in the UK, is large enough to permit an evaluation of associations with various types of such cancers. Further, it takes into account newer coding systems for morphology so that diseases associated with the lymphatic system can be separated from those of the myeloid system.
The key findings are that alcohol consumption appears to lower the risk of several types of lymphoma and plasma cell neoplasms, but has little effect on the risk of myeloid tumors such as acute myeloid leukemia. Smoking is associated with an increase in risk for most such cancers.
Forum reviewers considered this to be a very well-done analysis, and the ability of the authors to separate the effects on lymphoid and myeloid cancers is important. Forum members emphasize the strong differences in effect of smoking (an increase) and alcohol consumption (a decrease) on the risk of these cancers. They support future research to discover the mechanisms by which moderate drinking may lower such risk.
Reference: Kroll ME, Murphy F, Pirie K, Reeves GK, Green J, Beral V, for the Million Women Study Collaborators. Alcohol drinking, tobacco smoking and subtypes of haematological malignancy in the UK Million Women Study. British Journal of Cancer 2012;107:879–887.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
A Tribute to Serge Renaud
(1927 – 2012)
It is with sorrow that we have learned of the death in France on 28 October 2012 of Professor Serge Renaud at 84 years of age. In addition to being a colleague and close friend of many of us, he was celebrated as a pioneer in scientific research on the prevention of cardiovascular and other diseases. His innovative mind opened up new fields of inquiry that have greatly broadened research into the role of wine, alcohol, fatty acids, and other nutrients in preserving health and preventing disease. For his many contributions to science, on July 14, 2005, Serge received France’s highest distinction, the Legion d’Honneur.
Over many decades, Professor Renaud was the scientist who initiated much of the work relating the consumption of wine and other types of alcohol to cardiovascular disease and other of the diseases associated with ageing. He was the scientist most associated with the role of red wine in protecting the French from coronary artery disease (the “French Paradox”), and a leading figure in studying how other dietary factors relate to health. His innovative concepts have sometimes taken many years to be appreciated by other scientists. He made a major contribution with his research demonstrating how alpha-linolenic acid, monounsaturated fats, and other components of the “Cretan-type Mediterranean Diet,” play key roles in promoting health.
Serge Renaud was born in Cartelègue, Haute Gironde, France, and after starting his medical training in France moved to Montreal, Canada, and later to Boston, Massachusetts, USA. He returned to France in 1973 and became director of the INSERM unit in Lyon, France, where much of his research was carried out.
In an excellent tribute to Renaud in the Lancet in 2000, Bruno Simini pointed out his major contributions investigating the association between wine, diet, and thrombosis. Simini quotes Serge as saying: “If I hadn’t lived with my grandparents and great-grandparents on a vineyard near Bordeaux, perhaps this idea wouldn’t have occurred to me. When you see people reach the age of 80 or 90 years, who have been drinking small amounts of wine every day, you don’t believe wine in low doses is harmful.”1
In 1991, Serge Renaud appeared on the popular US television program, “60 Minutes,” in a segment entitled the “French Paradox.” When asked by Morley Safer, the host, what was the real reason that the French have rates of coronary artery disease so much lower than those in other developed nations, Renaud replied: “I think it is the alcohol.” And when Morley Safer closed the segment holding a glass of red wine and saying, “The protection of the French from heart disease may rest in this inviting glass,” the response in the US was remarkable – nothing such as this had ever been stated in the country that earlier in the century had made any alcohol consumption illegal through nation-wide prohibition. Following the television program, sales of red wine rose immediately by 40 per cent!
In addition to his studies on wine and alcohol, Professor Renaud, noting the very low rates of heart disease among participants from Crete in the “Seven Countries Study,” initiated the Lyon Diet Heart Study in 1985 to determine the effects of a diet based on that of Crete on the course of disease among patients who already had coronary disease. There were very dramatic reductions in subsequent coronary problems and in total mortality among subjects given the “Cretan-type diet,” which contained increased levels of an omega-3 fatty acid (alpha-linolenic acid) to replace some of the fats from meat and dairy products.
As quoted in the Lancet tribute by Simini, Professor Renaud said the results of these studies on heart disease and cardiac arrhythmias made him “wonder about the origins of civilisations. It is intriguing that ancient Asian and Mediterranean civilisations used natural oils in cooking—colza and olive—with similar fatty acid compositions.” [Colza oil is closely related to the widely used rapeseed oil and canola oil.] And because of his belief in ancient wisdom when it comes to diet and health, Renaud ends his book Le régime santé2 with a warning: “Don’t look for a pill that replaces [the Cretan diet]. There is no such thing.”
People around the world have profited, and will continue to profit, from the lifelong scientific work of Serge Renaud. For those of us who knew and worked with him, we cherish our memories of Serge the person, and of Serge the consummate scientist. As stated so well by a Forum member, “We are all in debt to Serge for the lesson he gave to our scientific community: curiosity as the sole reason to investigate, diligence in observing the facts, unbiased stringency in interpreting results, and, definitely not least, the modesty that only a great man can have. We shall keep him in our memory as an example and a mentor of the meaning of being a scientist.”
References
- Simini B. Serge Renaud: From French Paradox to Cretan miracle. The Lancet 2000;335:48. doi:10.1016/S0140-6736(05)71990-5.
- Renaud S. Le régime santé. Odile Jacob, Paris, 1998.
These comments provided by members of the International Scientific Forum on Alcohol Research (www.bu.edu/alcohol-forum)
31 October 2012
===============================================================================
Critique 094: The complex association between moderate alcohol consumption and breast cancer — 23 October 2012
An excellent review article from two scientists at the National Institue on Alcohol Abuse and Alcoholism describes the epidemiologic and basic scientific evidence linking alcohol consumption to the risk of breast cancer. The authors point out deficiencies in the epidemiologic data, especially that the pattern of drinking (regular moderate versus binge drinking) has generally not been taken into consideration (and the latter pattern can be associated with much higher blood alcohol concentrations). Further, epidemiologic studies usually provide data for only a short period of time, while the development of cancer may relate to exposures over many decades. The authors also comment upon the effect that under-reporting of alcohol by study participants could exaggerate effects on cancer risk from light drinking. They discuss two hypotheses that could relate alcohol to breast cancer risk: alcohol as a breast tumor promoter, and alcohol as a weak cumulative breast carcinogen, and present evidence from epidemiology and basic science that would relate to each hypothesis.
Overall, Forum reviewers were enthusiastic about this review paper, considering that it clearly outlined some of the difficulties scientists have in determining the causes of cancer. They agreed with the authors’ statements regarding the necessity to consider the overall net effects of moderate drinking, including reductions in the risk of cardiovascular disease and total mortality. They also agreed that future epidemiologic studies should focus on the pattern of drinking (and not just the average weekly amount of alcohol), and with their suggestions for future animal studies. One Forum reviewer cautioned that our understanding of the causes of breast cancer is still very incomplete, limiting our ability to provide well-founded recommendations to the public regarding moderate drinking as it relates to breast cancer risk.
Reference: Brooks PJ, Zakhari S. Moderate alcohol consumption and breast cancer in women: From epidemiology to mechanisms and interventions. Alcohol Clin Exp Res 2012; pre-publication: DOI: 10.1111/j.1530-0277.2012.01888.x.
For the full critique of this article by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 093: Is moderate alcohol consumption associated with an increased risk of atrial fibrillation among patients with cardiovascular disease? — 8 October 2012
An analysis of the association of alcohol consumption with the development of atrial fibrillation (AF) among subjects with coronary heart disease, stroke, diabetes, or other manifestations of cardiovascular disease (CVD) was based on subjects in two large antihypertensive drug treatment trials. Previous research in the general population has suggested an increase in the risk of the development of AF for heavy drinkers, and the present study shows such an association among subjects who already have CVD.
Among subjects in this study (all of whom had previous CVD), the authors also report that even “moderate” drinkers had a higher risk of AF than low-alcohol consumers, although the risk of death during follow up of moderate drinkers (9.9%) was lower than that of subjects reporting low-levels of drinking(12.5%). Excluding binge drinkers, the estimated risk of AF was about 13% higher in moderate drinkers than among subjects classified as low-alcohol consumers.
While the multiple analyses in this paper were done appropriately, Forum reviewers were concerned about two aspects of this study. First, there was concern about the wide range the authors chose for the category of “moderate” drinkers, which included subjects reporting from 1 drink per week up through those reporting 21 drinks per week for men and 14 drinks per week for women. It would have been useful to present results also for subjects who met more common definitions for moderate drinking: no more than 14 drinks/week for men and 7 drinks/week for women, the values used to define moderate drinking in the United States, Australia, and many other countries. Unfortunately, there is a conspicuous absence of data in this paper of the effects on the risk of AF of subjects consuming alcohol “moderately” by these standards.
Another major concern about these analyses relates to potential bias in the estimates from what is known as index event bias or collider bias. Given that alcohol intake prior to enrollment in this study may well have related to subjects’ development of cardiovascular disease, it is problematic to judge the effects of alcohol after a cardiovascular event on the subsequent risk of AF, a condition frequently associated with CVD.
All subjects in these analyses had already developed CVD (the prerequisite for being in the present study). Thus, the study included those who consumed alcohol prior to the diagnosis of CVD or diabetes and those who did not drink prior to these diagnoses. Given that moderate alcohol consumption has been shown to reduce substantially the risk of both CVD and diabetes, it can be assumed that subjects in this study who developed CVD despite being drinkers had other risk factors contributing to the disease that overcame any “protection” afforded by alcohol consumption. Unless adjusted for, these other risk factors could well affect the subsequent course of subjects following the onset of CVD, including the development of AF. A similar phenomenon has been seen for obesity (the “obesity paradox”), aspirin use (the “aspirin paradox”), and other exposures, where the associations with CVD seen prior to the initial development of the disease differ from those seen after the development of CVD.
It is clear from many previous studies in the general population that heavy alcohol intake and binge drinking increase the risk of developing atrial fibrillation. This cardiac arrhythmia is a common component of the “holiday heart” syndrome that may occur after very heavy bouts of drinking. As for the effects on the risk of atrial fibrillation from moderate drinking, as studied in this paper, there were a number of concerns from Forum reviewers about the analyses and results. They raise questions about the conclusions of the authors that even “moderate” drinking results in an increased risk of atrial fibrillation after the development of cardiovascular disease. Especially when defined as no more than 14 drinks per week for men or 7 drinks per week for women, the association between “moderate” alcohol consumption and atrial fibrillation remains unclear.
Reference: Liang Y, Mente A, Yusuf S, Gao P, Sleight P, Zhu J, Fagard R, Lonn E, Teo KK; for the ONTARGET and TRANSCEND Investigators. Alcohol consumption and the risk of incident atrial fibrillation among people with cardiovascular disease. CMAJ 2012. DOI:10.1503/cmaj.120412.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 092: The association of alcohol and tobacco with age at diagnosis among subjects with pancreatic cancer — 2 October 2012
This analysis from a group of distinguished scientists supports previous research showing that smoking is associated with an earlier onset of pancreatic adenocarcinoma. Other research has shown that smoking may also be a causative factor in the development of this type of cancer. For alcohol, this study shows that heavy drinking also appears to be associated with earlier diagnosis; previous research from some epidemiologic studies has suggested further that heavy intake of alcohol may be associated with the development of pancreatic cancer.
Forum reviewers were concerned, however, about potential bias in regards to the time of diagnosis of such cancer, and about many other limitations of the study. For example, the inability to separate drinkers by the pattern of drinking (binge drinking versus regular, moderate intake), by the socioeconomic status of subjects, and by a lack of information on chronic pancreatitis, a known risk factor, weaken the implications of this paper. Forum members do not think that the results of this study will have a large impact on clinical practice, or on measures for the prevention of pancreatic cancer.
Reference: Anderson MA; Zolotarevsky E; Cooper KL; Sherman S; Shats O; Whitcomb DC; Lynch HT; et al. Alcohol and tobacco lower the age of presentation in sporadic pancreatic cancer in a dose-dependent manner: A multicenter study. Am J Gastroenterol 2012; advance online publication, doi: 10.1038/ajg.2012.288
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 091: Light drinking may relate to increase in risk for certain cancers — 18 September 2012
A meta-analysis by a distinguished group of scientists was designed to determine if “light drinking” (defined as an average of up to 1 drink per day) was associated with the risk of certain cancers that have been shown in previous studies to be associated with the risk of cancer. The authors concluded that while the risk of these cancers was only slightly increased from such drinking, there were detectable increases in cancers of the oral cavity and pharynx, esophagus and female breast. They report no increase in the risk of cancers of the colorectum, liver, and larynx to be associated with such drinking.
Forum reviewers were concerned about a number of aspects of this study. While the statistical methodology was correct and done appropriately, the fact that the investigators (1) included both ex-drinkers and never drinkers in the reference group; (2) could not separate the effects of regular light drinking from binge drinking; (3) had no data on the duration of alcohol consumption at different levels; (4) did not adjust their analyses according to geographic region or type of study (both of which had large estimated effects on cancer risk); and (5) did not adjust their estimates of effect by other lifestyle habits, including smoking. All of these factors tend to weaken the implications of their results.
Forum reviewers were also concerned that despite the acknowledged limitations of their data, the authors present conclusions indicating that even light drinking increases the risk of certain cancers without commenting on the net health effects. They present only the effects on cancer (which was the topic of the meta-analysis) but do not comment on the overall or net health effects of light drinking: a marked reduction in the risk of much more common diseases, especially cardiovascular diseases, and a longer lifespan. Further, the lack of data on genetic patterns, folate intake, and other lifestyle factors makes it difficult to apply their findings to individual subjects. The Forum considers that while their analyses may be helpful in understanding associations between alcohol and cancer, the many limitations of this study indicate that it can provide only incomplete information on light alcohol consumption to be used as a basis for making recommendations to the public.
Reference: Bagnardi V, Rota M, Botteri E, Tramacere I, Islami F, Fedirko V, Scotti L, Jenab M, Turati F, Pasquali E, Pelucchi C, Bellocco R, Negri E, Corrao G, Rehm J, Boffetta P, La Vecchia C. Light alcohol drinking and cancer: a meta-analysis. Pre-publication: Annals of Oncology 2012; doi:10.1093/annonc/mds337
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 090: Effects of stopping alcohol consumption on subsequent risk of esophageal cancer — 13 September 2012
This paper provides an evaluation of the time following cessation of alcohol consumption that the risk of esophageal cancer returns to that of non-drinkers; it is based on 17 studies providing such information, 9 of which provided data for a meta-analysis. The authors conclude that an alcohol-related increased risk of esophageal cancer is reversible following drinking cessation, most likely requiring up to 16 years. The authors estimate that about one-half of the reduction in risk of cancer may occur within in a much shorter time, perhaps within about 4 or 5 years.
Forum reviewers considered this to be a well-done analysis. Forum members emphasized, as did the authors, a number of limitations of the study. Adjustments for smoking may not have been adequate: most upper aero-digestive cancers show a strong interaction between smoking and alcohol consumption in relation to cancer risk. (For many “alcohol-related” cancers, there is little effect of alcohol consumption among non-smokers.)
Further, large differences in the alcohol-cancer association were shown in this study for different geographical regions (some associations being much higher in Asia than in Europe or North America), but such differences were not adjusted for in the main analyses. The fact that the authors of this paper did not have data permitting the separation of ex-drinkers and never drinkers (both groups being included in the “non-drinker” category), and their inability to judge the effects of the baseline pattern of drinking (regular versus binge drinking), may also be limitations to the interpretation of their results. Adjustment for such factors may have influenced the effects of stopping drinking on subsequent cancer risk, and markedly changed the calculated effects on the numbers of cancers prevented worldwide.
In any case, the fact that cessation of drinking may reduce the risk of esophageal cancer is of importance. Other studies suggest further that just reducing the amount of alcohol consumed, rather than the complete cessation of drinking, may be associated with lowering of cancer risk, and low-level alcohol intake has been shown to have beneficial health effects on cardiovascular disease, diabetes, and other medical conditions.
Reference: Jarl J, Gerdtham Ulf-G. Time pattern of reduction in risk of oesophageal cancer following alcohol cessation — a meta-analysis. Addiction, 107, 1234–1243. doi:10.1111/j.1360-0443.2011.03772.x
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 089: Combination of hormone treatments and alcohol consumption influences the risk of breast cancer in women — 29 August 2012
An analysis among more than 40,000 postmenopausal women who were in the California Teachers Study was carried out to determine if there were differences in risk of breast cancer among women consuming alcohol according to their previous or current use of hormone therapy (HT). In the cohort, 660 women were diagnosed with invasive breast cancer during follow up.
Results from multivariate Cox proportional hazards regression models showed an increase in risk of breast cancer among alcohol consumers of more than 20 grams of alcohol per day (about 1 ½ to 2 typical drinks) who were current users of HT but not among those who were ex-users of HT. The authors conclude: “Following the cessation of HT use, alcohol consumption is not significantly associated with breast cancer risk, although a non-significant increased risk was observed among women who never used HT. Our findings confirm that concurrent exposure to HT and alcohol has a substantial adverse impact on breast cancer risk. However, after HT cessation, this risk is reduced.”
Forum reviewers considered this to be a very well-done analysis on a large group of post-menopausal women with repeated assessments of alcohol consumption and HT use. However, results from even very large studies on the relation between alcohol, HT, and breast cancer risk have often been conflicting. Even with numerous studies on this topic, we still have very poor predictors of which women will develop breast cancer. There is some increase in risk for women with a family history of such cancers and those who are obese. However, the percentage increases in risk associated with HT, alcohol consumption, and other environmental factors are generally small (unlike the many-fold increase in the risk of lung cancer among smokers in comparison with never smokers). This may explain why the results of individual studies may reach apparently conflicting conclusions. While the present study suggests that women who consume alcohol may have a decrease in their risk of breast cancer if they stop taking hormone replacement therapy, our current understanding of factors affecting breast cancer risk remains quite inadequate.
Reference: Horn-Ross PL, Canchola AJ, Bernstein L, Clarke CA, Lacey JV, Neuhausen SL, Reynolds P, Ursin G. Alcohol consumption and breast cancer risk among postmenopausal women following the cessation of hormone therapy use: the California Teachers Study. Cancer Epidemiol Biomarkers Prev 2012. [Epub ahead of print]
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 088: Higher levels of alcohol intake may slightly increase risk of age-related macular degeneration, with no effect from moderate drinking 22 August 2012
An analysis based on the follow up of more than 20,000 participants recruited in 1990-1994 for the Melbourne Collaborative Cohort Study in Australia related alcohol consumption at baseline to the subsequent development of age-related macular degeneration (AMD), a common cause of blindness in the elderly. At a follow-up examination between 2003 and 2007, digital macula photographs of both eyes were taken and evaluated for early and late AMD signs; there were 2,663 cases of early AMD and 121 cases of late AMD identified.
The authors report: “Drinking more than 20 g of alcohol per day was associated with an approximate 20% increase in the odds of early AMD (odds ratio = 1.21, 95% confidence interval: 1.06, 1.38; P = 0.004) when compared with those who reported no alcohol intake at baseline.” (An average of 20 grams/day of alcohol is the equivalent of about 2 daily drinks by British standards or 1 ½ drinks by US standards.) The analyses show that the increased risk was almost exclusively among smokers, with no significant effect among non-smokers who consumed any amount of alcohol.
Forum reviewers had some concern that approximately one-half of this “population-based” study did not have measurements for AMD; these included those who had died during the follow-up period (and deaths were more common among non-drinkers than among drinkers). Further, the authors focus only on the slight increase in risk of AMD seen for heavier drinkers, but do not emphasize that among never smokers there was no increase in risk for consumers of any amount of alcohol. Their results suggest a possible interaction between smoking and alcohol consumption in the etiology of this disease.
The findings of no effect (either positive or negative) from drinking < 20 g/day of alcohol in this study does not support some earlier reports of reduced risk of AMD among moderate wine drinkers. In the present study, there were no detectable differences in effect between the consumption of wine or of beer. A key point of this study may be that never-smokers do not show increased risk of AMD with alcohol consumption.
Reference: Adams MKM, Chong EW, Williamson E, Aung KZ, Makeyeva GA, Giles GG, English DR, Hopper J, Guymer RH, Baird PN, Robman LD, Simpson JA. 20/20—Alcohol and age-related macular degeneration: The Melbourne Collaborative Cohort Study. Am J Epidemiol 2012;176:289-298.
For the full critique of this article by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 087: Smoking increases, while alcohol consumption may decrease, the risk of amyotrophic lateral sclerosis (ALS) — 8 August 2012
Reference: de Jong SW, Huisman MHB, Sutedja NA, van der Kooi, AJ, de Visser M, Schelhaas HJ, Fischer K, Veldink JH, van den Berg LH. Smoking, alcohol consumption, and the risk of amyotrophic lateral sclerosis:A population-based study. Am J Epidemiol 2012;176:233–239
A population-based case-control study of the rare but devastating neurological disease amyotrophic lateral sclerosis (ALS) has shown that the risk of such disease is increased among smokers, as has been shown previously. However, surprisingly, the risk of ALS was found to be markedly lower among consumers of alcohol than among abstainers.
Forum reviewers thought that this was a well-done and important paper, as it is a population-based analysis, with almost 500 cases of ALS, a very large number of cases for this rare disease. They were especially struck by the magnitude of the difference in risk of ALS between alcohol consumers and never drinkers: the risk among drinkers was about one half that of non-drinkers. Said one reviewer: “The results in this study are astonishing in this mysterious disease. One should expect that alcohol, as a toxic agent, rather should contribute to the development of ALS than to prevent it. The lower risk among drinkers compared with non-drinkers is remarkable”
Forum reviewers cautioned that the results of this paper should not be used to prompt people to consume alcohol just to prevent ALS, as it is such a rare disease. However, this paper presents important data that could help scientists understand the etiology of ALS and perhaps other more common diseases.
For the full critique of this paper by members of the International Scientientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 086: Mechanisms for a beneficial effect of moderate alcohol consumption on osteoporosis in women — 1 August 2012
Women after menopause tend to develop weaker bones from what is known as osteoporosis, which may lead to fractures (especially hip fractures) from falling. The weakness of the bones results from an imbalance between the normal resorption (a type of dissolving of old bone) and the laying down of new bone, an ongoing process for both men and women referred to as “bone turnover.” For poorly understood reasons, after menopause the resorption of old bone in women continues but new bone is laid down less well, leading to a decrease in the density of bone. A variety of substances (calcium, vitamin D, various medications) have been used in an attempt to prevent the development of osteoporosis; in epidemiologic studies, moderate drinking of alcohol has been shown to lower this risk.
An intervention trial evaluating the association of alcohol intake with indices of bone metabolism shows beneficial effects of moderate alcohol intake on factors that relate to osteoporosis in post-menopausal women. The authors state that excessive bone turnover, combined with an imbalance whereby bone resorption exceeds bone formation, is the principal cause of post-menopausal bone loss. This study among 40 healthy post-menopausal women investigated the hypothesis that moderate alcohol intake (an average of 19 grams per day, or approximately 1 and ½ typical drinks per day in this study) attenuates bone turnover after menopause. Measurements were carried out while the women were consuming alcohol, after they had stopped drinking as part of the trial, and following resumption of alcohol. The study showed that abstinence from alcohol resulted in increased markers of bone turnover (hence, higher risk of developing osteoporosis), whereas resumption of alcohol reduced bone turnover markers.
Forum reviewers considered this to be an innovative and well-done study. The key questions raised were how alcohol may affect bone metabolism in a longer period of time than was tested in this study. Reviewers realized that such long-term intervention trials are very difficult and expensive to carry out. On the other hand, many prospective epidemiologic studies in the elderly have shown greater bone mineral density and a lower risk of fractures among regular moderate drinkers than among abstainers. The most important aspect of this study may be that it has helped identify cellular mechanisms for the increased bone density observed in post-menopausal women who are moderate alcohol consumers.
Reference: Marrone JA, Maddalozzo GF, Branscum AJ, Hardin K, Cialdella-Kam L, Philbrick KA, Breggia AC, Rosen CJ, Turner RT, Iwaniec UT. Moderate alcohol intake lowers biochemical markers of bone turnover in postmenopausal women. Menopause 2012;19: DOI: 10.1097/gme.0b013e31824ac071
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research and other invited scientists, please click here.
(Note: an ADDENDUM to the original Forum critique has been added on 15 August 2012.)
===============================================================================
Critique 085: Moderate alcohol intake is associated with a lower risk of kidney cancer — 19 July 2012
A majority of previous epidemiologic studies have shown that moderate drinking is associated with a lower risk of kidney cancer, which may affect about 1% of the general population. In published prospective cohort studies, the risk for such cancer among moderate drinkers is usually about 25% less than the risk seen among non-drinkers.
This well-done meta-analysis supports these findings: for the more-reliable prospective cohort studies (rather than case-control studies) the current study finds a 29% lower risk for subjects in the highest category of alcohol consumption in comparison with subjects in the lowest alcohol category. The findings suggest similar effects among men and women, and for all types of alcohol beverages. The effects are seen at a level of about one drink/day, with little further reduction in risk for greater alcohol consumption.
Reference: Song DY, Song S, Song Y, Lee JE. Alcohol intake and renal cell cancer risk: a meta-analysis. British Journal of Cancer 2012;106:1881–1890.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 084: Moderate drinking lowers risk of developing rheumatoid arthritis in women — 17 July 2012
A follow-up study of more than 34,000 women in Sweden has shown that moderate drinkers, in comparison with abstainers, were at significantly lower risk of developing rheumatoid arthritis (RA), an often serious and disabling type of arthritis. RA is known to relate to inflammation, and it is postulated that this is blocked to some degree by the consumption of alcohol. In this study, women who consumed at least 4 drinks per week (with a drink being defined as containing 15 grams of alcohol) had 37% lower risk of developing RA than subjects reporting never drinking or consuming less than 1 drink/week.
This large study is important as few prospective studies are of adequate size to have sufficient cases of RA to evaluate factors related to its development. The study supports previous research showing a lower risk of developing RA, or milder severity of the disease, among moderate drinkers than among abstainers.
Reference: Di Giuseppe D, Alfredsson L, Bottai M, Askling J, Wolk A. Long term alcohol intake and risk of rheumatoid arthritis in women: a population based cohort study. BMJ 2012;345:e4230 doi: 10.1136/bmj.e4230 (Published 10 July 2012)
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 083: Higher indices of quality of life are seen among persistent moderate drinkers than among abstainers — 20 June 2012
Data from a nationally representative sample of 5,404 community-dwelling Canadians ages 50 and older at baseline (1994/1995) was used to estimate the effects of alcohol drinking patterns on indices of quality of life, at baseline (when subjects were aged ≥50 years) and after a follow-up period. Health-related quality of life was assessed with the Health Utilities Index Mark 3 (HUI3). The authors report that most participants showed stable alcohol-consumption patterns over 6 years. Persistent regular moderate drinkers had the highest indices of quality of life at baseline, but subsequent changes in HUI3 were similar in all groups except those reporting decreasing alcohol consumption. The investigators conclude that persistent moderate drinkers had higher initial levels of health-related quality of life than persistent nonusers and those in other groups. However, rates of decline over time were similar for all groups except those decreasing their consumption, which had a greater decline in their level of health-related quality of life than persistent moderate users. While Forum reviewers admired the intent of this study, there were concerns about some of the statistical and epidemiologic aspects. The reasons that some people stopped drinking or decreased their intake were not known; while the authors state that subjects decreasing their alcohol consumption had a more rapid decline in quality of life measures, it is not known what percentage of such subjects decreased alcohol intake due to the development of serious iseases. If this were the case, such diseases may have been more important in their subsequent adverse health than the change in their drinking habits.
Further, the “baseline” quality of life measures in this study were obtained when subjects were aged 50 or older; this baseline value of quality of life was higher in moderate drinkers. However, there are statistical problems if adjustments are made for this when quality of life is assessed subsequently and related to drinking pattern. Peto has described this problem as a “horse-racing effect.” He states that in prospective studies, the correlation between exposures (e.g., drinking pattern) and outcomes (e.g., quality of life) assessments during follow up are likely to be the same as the outcome at the end of follow up. As an analogy he uses a race between ‘slow’ and ‘fast’ horses; it is likely that the fast horses will be ahead at the mid-point of the race as well as at the end. Environmental effects on quality of life begin early in life, and if one adjusts for the mid-life value (as done and referred to as “baseline” in the present study), you may end up disregarding much of the effect of subsequent alcohol intake.
Overall, this study shows a positive relation between moderate alcohol intake and quality of life in middle-aged adults. The effects on the subsequent quality of life as one ages of continued alccohol consumption, or of decreasing intake, remain unclear.
Reference: Kaplan MS, Huguet N, Feeny D, McFarland BH, Caetano R, Bernier J, Giesbrecht N, Oliver L, Ross N. Alcohol Use Patterns and Trajectories of Health-Related Quality of Life in Middle-Aged and Older Adults: A 14-Year Population-Based Study. J. Stud Alcohol Drugs 2012;73:581–590.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 082: A statistical model attempting to estimate the level of alcohol consumption that is “optimal” for health — 6 June 2012
Scientists from Australia and Oxford University have carried out a complex analysis in an attempt to determine the “optimal” level of alcohol consumption that is associated with the lowest rates of chronic disease in the UK. They conclude that the intake of about one-half of a typical drink per day would result in the healthiest outcomes, and the authors conclude that the recommended alcohol intake for the UK should be reduced from the current advised level of drinking.
There were a number of concerns by Forum members about the paper. It is based on an extremely complex statistical model that requires many assumptions, most of which cannot be validated. The parameters chosen to use in such a model determine the results, and a number of instances were identified where the values used in this analysis do not reflect current scientific knowledge. Further, the conclusions of the authors are based exclusively on the lowest point of the “J-shaped” curve for alcohol and disease, and disregard the findings that the risk of death, in comparison with non-drinkers, remains lower for drinkers of alcohol of up to several drinks per day.
There were other aspects of the paper that were of particular concern: (1) focusing only on the average amount of alcohol consumed, while the pattern of drinking (regular moderate versus binge drinking) has the greatest effect on health outcomes; (2) giving a single recommended level of alcohol intake irrespective of age; the greatest risks and lowest expected benefits of alcohol intake are among the young, whereas most of the putative health benefits relate to the diseases of ageing; (3) giving a single value for both men and women, since women are known to react (both adversely and beneficially) to lower levels of alcohol than do men; (4) the use of their estimated value alone for making recommendations for the population; guidelines should be based on a large number of social and behavioral factors, not just on the results of one scientific study.
The level of alcohol that is most likely to be associated with the lowest risk of adverse health outcomes and the most likely health benefits varies markedly among individuals. Middle-aged men and post-menopausal women are most likely to demonstrate enhanced health (e.g., lower risk of cardiovascular diseases, diabetes, dementia) from moderate drinking. For all ages, binge drinking is associated with predominantly adverse outcomes. In general, women should drink less than men. While the analyses presented in this paper are of scientific interest, they alone do not support changes in the current population recommendations for alcohol consumption.
Reference: Nichols M, Scarborough P, Allender S, Rayner M. What is the optimal level of population alcohol consumption for chronic disease prevention in England? Modelling the impact of changes in average consumption levels. BMJ Open 2012;2:e000957. doi:10.1136/bmjopen-2012-000957.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 081: Alcohol intake in the elderly affects risk of cognitive decline and dementia — 22 May 2012
A well-done review paper on the association between alcohol consumption and cognition in the elderly provides an excellent summary of potential mechanisms by which alcohol may affect cognitive function and the risk of dementia, both adversely and favorably. Current scientific data indicate that heavy drinking is associated with an increased risk of neurological disease and dysfunction, while regular light-to-moderate alcohol intake seems to be associated with a reduced risk of such dysfunction, including a lower risk of developing Alzheimer’s disease.
At present, the mechanisms by which the moderate intake of wine and other alcoholic beverages reduces the risk of cardiovascular diseases are much better defined than they are for cognition. Forum members agree with the authors that further research is needed to evaluate a potential role that wine and other alcoholic beverages may play in reducing the risk of dementia. Forum members also agree that, at present, the specific mechanisms of such putative protection are not well defined, and it would be premature to recommend light-to-moderate drinking for reducing the risk of dementia. On the other hand, current epidemiologic and biomedical data suggest that most elderly subjects who are responsible and moderate drinkers would not benefit from being advised to stop their alcohol consumption.
Reference: Kim JW, Lee DY, Lee BC, Jung MH, Kim H, Choi YS, Choi I-G. Alcohol and Cognition in the Elderly: A Review. Psychiatry Investig 2012;9:8-16; On-line: http://dx.doi.org/10.4306/pi.2012.9.1.8
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 080: Modest alcohol intake is associated with less inflammation among patients with the most common type of liver disease, non-alcoholic fatty liver disease (NAFLD) — 15 May 2012
NAFLD (non-alcoholic fatty liver disease) is the most common type of liver disease in the developed world, affecting up to one-third of the US population. NAFLD is often associated with obesity and other parameters of the so-called “metabolic syndrome,” which is a major risk factor for the development of cardiovascular disease. In a well-done study among subjects with NAFLD, the investigators have demonstrated that modest alcohol consumption (an average of up to 20 grams of alcohol per day and no binge drinking) is associated with less evidence of inflammation of the liver (steatohepatitis), a condition known to markedly increase the risk of progression of liver disease to cirrhosis.
Given that NAFLD and other conditions associated with the metabolic syndrome are so common, and are major risk factors for developing cardiovascular disease, the results of the present study are important. They show that modest drinking is associated with decreased, not increased, inflammation of the liver. Further, even among subjects with NAFLD, cardiovascular disease is a much more common cause of death than liver disease. The authors suggest that intervention studies should be done to support their findings; if confirmed, subjects with NAFLD should not be advised to avoid all alcohol, which is the current advice usually given to such patients.
Reference: Dunn W, Sanyal AJ, Brunt EM, Unalp-Arida A, Donohue M, McCullough AJ, Schwimmer JB. Modest alcohol consumption is associated with decreased prevalence of steatohepatitis in patients with non-alcoholic fatty liver disease (NAFLD). Journal of Hepatology 2012 (pre-publication release)
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
A Tribute to Federico Leighton Puga, MD — 8 May 2012
Frederico Leighton Puga, MD, Professor and Director of the Center for Molecular Nutrition and Chronic Diseases of the Catholic University of Chile in Santiago, died on 27 April 2012 at the age of 74 years. Dr. Leighton was a valued member of the International Scientific Forum on Alcohol Research, and was noted for his seminal work in nutrition, antioxidants, the health aspects of moderate wine consumption, and public health approaches for the prevention of chronic diseases.
Many Forum members knew and had worked with Dr. Leighton through many decades. All feel a deep loss, of a great scientist, a loyal and good friend, and someone very concerned with the health of people everywhere. As stated by one Forum member, “Federico was a great scientist motivated by curiosity and the desire to be useful for his country. His culture and education and intellectual rigor were well integrated into his humanity and the sweetness of his character.” Said another: “Federico had in abundance that indefinable quality known as ‘class.’” The world has lost an honest and honorable scientist.
For the full tribute to Dr. Leighton by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 079: Moderate alcohol consumption both prior to, and following, a myocardial infarction is associated with lower risk of mortality — 17 April 2012
In a very well-done analysis based on the follow up of more than 50,000 subjects from The Health Professionals Follow-up Study (HPFS), 1,818 men were confirmed with incident non-fatal myocardial infarction (MI). Among MI survivors, 468 deaths were documented during up to 20 years of follow up. Repeated reports were obtained on alcohol consumption throughout follow up. Average alcohol consumption was calculated prior to and then following the MI.
The overall results show that, in comparison with no alcohol consumption, the pre-MI and the post-MI intakes of light (0.1-9.9 g/day) and moderate (10.0-29.9 g/d) amounts of alcohol were both associated with lower risk of all-cause mortality and cardiovascular morality among these men. The significant reductions in all-cause mortality risk (22% lower for 0.1-9.9 g/day and 34% lower for 10.0 – 29.9 g/day, in comparison with non-drinkers) were no longer present for consumers of ≥ 30 g/day; for this highest consumer group, the adjusted hazard ratio was 0.87 with 95% CI of 0.61-1.25.
There are a number of other informative and interesting results described from this study. First, there was little change in reported alcohol prior to and following the MI: drinkers tended to remain drinkers of similar amounts. Few non-drinkers began to drink after their MI; among heavier drinkers, there was a tendency to decrease the amount somewhat (but very few stopped drinking completely). Further there were no significant differences in outcome according to type of beverage consumed although, interestingly, lower hazard ratios were seen for consumers of beer and liquor than of wine. While the authors state that the effects of alcohol were stronger for the association with non-anterior MIs, the HRs for all-cause mortality were little different: among the moderately drinking men the HRs were 0.58 for anterior MI and 0.51 for other types of MI.
Even though exposures (such as alcohol) for cardiovascular events (such as MI and cardiovascular mortality) may be different after a person has an event than it was before the event, in this study the reductions in risk were almost the same. For example, both for alcohol intake reported prior to a MI, and that after a non-fatal MI, the risk of mortality was about 30% lower for moderate drinkers than it was for abstainers. This suggests that, in terms of reducing cardiovascular disease, alcohol may have relatively short-term effects. Frequent consumption (of moderate amounts) may result in the best health outcomes.
Reference: Pai JK, Mukamal KJ, Rimm EB. Long-term alcohol consumption in relation to all-cause and cardiovascular mortality among survivors of myocardial infarction: the Health Professionals Follow-up Study. European Heart Journal 2012;doi:10.1093/eurheartj/ehs047
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 078: An update on the association of alcohol consumption with risk of breast cancer — 10 April 2012
An excellent review paper on the relation of alcohol consumption to the risk of breast cancer concludes that, overall, there is a positive dose-response relation between alcohol drinking and the risk of breast cancer. The analysis shows that an increase in risk is seen even among women reporting an average of only about one drink/day. Given the high prevalence of such light drinking in most female populations, the authors estimate that up to 1 to 2% of breast cancers in Europe and North America may be attributable to light drinking alone. Thus, while alcohol appears to be a risk factor for breast cancer, it does not explain a very high percentage of cases.
Forum members considered this to be a well-done analysis, with a good review not only of epidemiologic studies but of potential mechanisms of effect of alcohol on breast cancer risk. An increase in estrogen levels from alcohol seems to be the physiologic mechanism most commonly suggested for the increase in risk.
The meta-analysis is noteworthy in presenting risks specifically for women who consume up to one drink/day, which is the common pattern for a high proportion of women in western cultures. On the other hand, the authors herefailed to discuss the potential modification of alcohol effects on cancer risk from folate in the diet; in many studies, high folate levels tend to diminish or eliminate an increase in risk from alcohol. Further, the paper does not provide a discussion of the net effects of moderate drinking on mortality. In older women, the decrease in the risk of cardiovascular disease (a much more common cause of death than breast cancer), greatly exceeds the potential increase in risk of death from breast cancer.
Reference: Seitz HK, Pelucchi C, Bagnardi V, La Vecchia C. Epidemiology and Pathophysiology of Alcohol and Breast Cancer: Update 2012. Alcohol and Alcoholism 2012; doi: 10.1093/alcalc/ags011
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 077: Swedish study supports a “U-shaped” association of alcohol consumption with risk of pre-diabetes and diabetes mellitus — 29 March 2012
Subjects in a cohort in Sweden, some of whom had been exposed to a community intervention program to prevent diabetes, were evaluated 8-10 years after baseline for the presence of diabetes mellitus or impaired glucose metabolism (“pre-diabetes”) in relation to a baseline report of alcohol consumption. Approximately 2,000 men and 3,000 women had a normal glucose tolerance test at baseline; of these 105 men and 57 women developed type II diabetes. Of subjects with pre-diabetes at baseline, 175 men and 98 women progressed to diabetes. The authors report that total alcohol consumption and binge drinking increased the risk of pre-diabetes and diabetes in men, while low consumption decreased diabetes risk in women. However, the authors did not discuss the fact that in essentially all comparisons, the highest risk of diabetes or pre-diabetes was among abstainers.
Forum reviewers had some concerns about the study. For example, the study included some subjects who had been exposed to an intervention trial to prevent diabetes, yet no information is given on potential effects of the intervention. It was not a population-based group. Also, the sample was “enriched” with subjects who had a positive family history of diabetes, which may make it more difficult to judge the effects of environmental factors. Ex-drinkers and never drinkers were included in the abstainer group.
It appears that the authors focused only on the “statistically significant” results rather than commenting on the overall pattern of association (lower risk of developing diabetes for moderate drinkers than for abstainers and heavier drinkers). Further, the number of subjects in many of the sub-groups was very small, making it difficult to define specific cut-points for effects of alcohol on risk.
Nevertheless, reviewers considered that, overall, these analyses support the usual findings from previous research of a “U-shaped curve” for alcohol and diabetes for both men and women. There appears to be a reduction in risk with moderate alcohol intake and possibly an increased risk for heavier drinking.
Reference: Cullmann M, Hilding A, Östenson CG. Alcohol consumption and risk of pre-diabetes and type 2 diabetes development in a Swedish population. Diabet Med 2012;29:441–452. DOI: 10.1111/j.1464-5491.2011.03450.x
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 076: Evaluating the association of alcohol intake with cognitive functioning using a Mendelian randomization study design — 22 March 2012
Many observational cohort studies have shown that moderate alcohol use is associated with better cognitive function. However, since such studies are vulnerable to residual confounding by other lifestyle and physiologic factors, the authors conducted a Mendelian randomization study, using aldehyde dehydrogenase 2 (ALDH2) genotype (AA, GA, or GG) as an instrumental variable in 2-stage least squares analysis. Cognitive function was assessed from delayed 10-word recall score (n = 4,707) and Mini-Mental State Examination (MMSE) score (n = 2,284) among men from the Guangzhou Biobank Cohort Study (2003–2008). The authors had previously reported an association between reported alcohol intake and cognitive function from a larger group of subjects from the same study finding that women reporting occasional alcohol intake and men reporting occasional or moderate intake had better scores related to cognitive function than did abstainers.1
In the present Mendelian study, the authors found no significant association between groups defined by the ALDH2 genotype (as an “unbiased” estimate of alcohol consumption) and the two measures of cognitive functioning. A problem with the present analysis is that ALDH2 genotypes explained only 3% of the variance in reported alcohol intake, which weakens the conclusions of the authors. Further, differences in the predominant type of beverage consumed (rice wine), and probably marked differences in drinking patterns between these subjects and Europeans and Americans, make it difficult to know what the implications of this study are for western industrialized societies.
We agree with the authors that “Causality should be thoroughly verified in a variety of settings using different kinds of evidence, including experimental or genetic studies, rather than relying on simple observations in a particular setting.” We strongly support future attempts at using Mendelian randomization studies, hopefully using better instruments for estimating alcohol intake. On the other hand, as stated by recent evaluations of various study designs for determining causality,3 we appreciate that Mendelian randomization sounds good, but it is not the “Holy Grail.”
Reference: Au Yeung SL, Jiang CQ, Cheng KK, Liu B, Zhang WS, Lam TH, Leung GM, Schooling CM. Evaluation of moderate alcohol use and cognitive function among men using a Mendelian randomization design in the Guangzhou Biobank Cohort Study. Am J Epidemiol 2012; pre-publication release. DOI: 10.1093/aje/kwr462
Please click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 075: Moderate drinking associated with lower risk of stroke in women — 15 March 2012
A well-done analysis from the Nurses’ Health Study shows that the risk of total stroke is slightly lower among light-to-moderate consumers of alcohol than among subjects reporting no alcohol intake. In comparison with non-drinkers, the estimated risk is 17-21% lower for women averaging up to 15 grams of alcohol per day (a little over one drink/day by US definitions of approximately 12 grams of alcohol for a typical “drink.”). For consumers of larger amounts of alcohol, the risk of stroke has a tendency to be slightly increased, but not statistically significantly so.
Data on the pattern of drinking (regularly, binge, etc.) were not reported. Among these predominantly light drinkers, there were no differences between effects on the risk of the most common type of stroke, ischemic stroke (due to atherosclerotic obstruction of a artery or an embolic clot) or the less-common hemorrhagic stroke (bleeding into the brain).
The results, with full adjustment for other factors that may affect risk, suggest a “J-shaped” curve for total stroke, with reductions in risk for light-to-moderate drinking and possibly an increase with greater amounts. In this study, the point at which the risk of drinkers exceeds that of non-drinkers was about 38 grams of alcohol per day (the equivalent of about 3 typical “drinks”), with a 95% confidence interval of 28 to 57 grams/day.
The study supports many previous reports from observational epidemiologic studies that have shown a slight reduction in risk of the ischemic type of stroke from moderate alcohol intake. Some, but not all previous studies, show an increase in hemorrhagic stroke for any amounts of alcohol, but that was not seen in this study, possibly because there were few heavy drinkers in this group of nurses.
Reference: Jimenez M, Chiuve SE, Glynn RJ, Stampfer MJ, Camargo Jr CA, Willett WC, Manson JE, Rexrode KM. Alcohol Consumption and Risk of Stroke in Women. Stroke 2012, pre-publication. http://stroke.ahajournals.org. DOI: 10.1161/STROKEAHA.111.639435
Please click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 074: Does moderate wine consumption improve lung function? — 8 March 2012
An analysis based on a prospective study in the Netherlands assessed the impact of wine and resveratrol intake on lung function. It also studied genetic factors (affecting sirtuin) that have been found to be mechanisms by which resveratrol relates to metabolism and longevity of life. The authors report that resveratrol intake was associated with higher lung volumes and that white wine intake (but not red wine intake) was associated with lower risk of airway obstruction. They report that the genetic factors studied did not relate to the associations found.
While several previous studies (as does this one) have reported that wine intake improves lung function, Forum reviewers were concerned about several aspects of the paper, and especially with the conclusions of the authors that resveratrol was the key factor in improved lung function. A reviewer stated: “Resveratrol may well be just the bystander of something else present in wine.” The beneficial effects on lung function are probably related to many compounds present in wine, and not just resveratrol.
Based on a number of scientific studies, moderate wine intake appears to have a favorable effect on lung function. The doses of resveratrol seen in these epidemiologic studies are in the physiological range that could be expected from moderate wine consumption, unlike the huge doses of resveratrol being evaluated as a potential life-extending drug in pharmaceutical studies.
Reference: Siedlinski M, Boer JMA, Smit HA, Postma DS, Boezen HM. Dietary factors and lung function in the general population: wine and resveratrol intake. Eur Respir J 2012; 39: 385–391; DOI: 10.1183/09031936.00184110
Please click here for the full critique by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 073: The association of alcohol consumption with osteoporosis — 5 March 2012
Osteoporosis is a key underlying factor in fractures among the elderly, which are increasingly a major health problem. A review paper from France on the association between alcohol consumption and bone metabolism states that heavy alcohol intake may adversely affect bone mineral density and increase the risk of osteoporosis. It states that lighter drinking may actually improve bone density, but presents very limited data to support this statement. Forum members were disappointed that the paper did not carry out a meta-analysis or other synthesis of the data; further, data from a number of key epidemiologic studies on the subject were not discussed in the paper.
The paper provides important information on the mechanisms by which alcohol may affect bone metabolism. The authors describe effects of alcoholic beverages on bone density, bone microarchitecture, bone remodeling, and other mechanisms, which help explain how alcohol and polyphenols and other constituents of beer and wine may relate to the risk of fractures in the elderly.
Unfortunately, despite what the authors’ conclude, the paper does not provide a summation of the scientific data upon which public health policy can be based. Overall, current scientific data suggest that bone mineral density and the risk of fractures are favorably affected by light-to-moderate drinking, but adversely affected by heavy drinking and alcoholism.
Reference: Maurel DB, Boisseau N, Benhamou CL, Jaffre C. Alcohol and bone: review of dose effects and mechanisms. Osteoporos Int (2012) 23:1–16; DOI 10.1007/s00198-011-1787-7.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 072: Obesity may modify the association between alcohol consumption and the risk of colorectal cancer. 23 February 2012
A case-control study from Newfound/Labrador has reported that greater alcohol intake may increase the risk of colorectal cancer among obese subjects, but not among non-obese subjects. This is not a particularly large study, and only 45-60% of subjects who were recruited by telephone ended up providing data. Further, it is a case-control comparison, rather than a cohort analysis, making bias in the results more likely.
In this study, there was no relation of alcohol with the risk of CRC when considering the entire population. However, when subjects were stratified by BMI (<30 versus ≥ 30), the data indicate an increase in CRC risk for obese subjects who were “drinkers” (OR=2.2, 95% CI 1.2-4.0), especially among subjects reporting 5 or more drinks/daily (OR=3.7, CI 1.5-9.0). On the other hand, even among obese subjects there was not a clear dose-response effect noted, i.e., there was not a step-wise increase in CRC risk with greater number of drinks/day For example, the odds ratio (OR) was 2.3 times that of non-drinkers for obese subjects reporting 1-2 drinks/daily and 1.3 for those reporting 3-4 drinks/daily.
It will be interesting to determine if other studies show that there is modification of the association between alcohol intake and colorectal cancer by obesity. If such is the case, it could help understand some of the mechanisms for the development of cancer and provide better guidelines for screening for CRC.
Reference: Zhao J, Zhu Y, Wang PP, et al. Interaction between alcohol drinking and obesity in relation to colorectal cancer risk: a case-control study in Newfoundland and Labrador, Canada. BMC Public Health2012, 12:94 doi:10.1186/1471-2458-12-94
Please click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 071: Forum Comments on proposed new dietary guidelines for Australia — 16 February 2012
Members of the International Scientific Forum on Alcohol Research have provided comments on the chapter related to alcohol intake that has been included in “A review of the evidence to address targeted questions to inform the revision of the Australian Dietary Guidelines,” by the Australian Government Department of Health and Ageing and National Health and Medical Research Council (NHMRC), November 2011, ISBN Online 1864965304.
Forum members considered that the authors of the report should be commended on their work. Criticisms are primarily about the restriction in the time frame of the review, and minimal consideration of key nuances, such as quantity of alcohol consumed and its relation to risk or benefit, patterns of drinking, the balance between risks and benefits, and making statements at all when the evidence is too weak. More details (e.g. considering cardiovascular mechanisms to widen the search) would have added weight to the conclusions.
For the full comments of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 070: Potentially important new mechanisms found for the anti-aging effects of resveratrol, a phenolic compound found in red wine — 9 February 2012
A well-conducted experimental study in mice has provided potentially important new insights into the association of the intake of resveratrol and like compounds with health benefits. Resveratrol is a constituent of red wine and other vegetable products, and is being evaluated in high-doses as a pharmaceutical. The biologic mechanisms demonstrated in this study could provide key new approaches for the prevention or treatment of a number of chronic diseases in humans, especially those related to vascular and metabolic diseases and to the risk of mortality.
More than two decades ago, particularly through publicity related to the so-called “French Paradox,” the public became aware of the potential reduction in the risk of coronary heart disease from the moderate consumption of red wine, and the media focused on a single constituent in red wine, resveratrol, as being the “key” factor. We now know that resveratrol is only one of hundreds of phenolic compounds in wine, many of which have been shown to have beneficial effects on vascular function, and that alcohol itself (present in wine, beer or spirits) also provides considerable protection against heart disease. Still, there has remained considerable attention paid to resveratrol, and extensive scientific research on resveratrol and related substances have shown that, in high doses, they may increase longevity of life and reduce metabolic diseases of aging.
In general, Forum reviewers thought that this was a very well-done study. Their concerns related to the dose used in these experiments; while the levels of resveratrol and like compounds might be accessible with pharmaceutical doses, the suggestion that similar levels could be connected with wine consumption is misleading. Further, in humans, resveratrol in the diet will interact with many other chemicals to achieve an effect, as whole plant extracts consist of many active and inactive micronutrients that may play a role in health and disease. To ascribe a specific effect on health from one chemical found in wine or other plant products could be misleading.”
Still, the reviewers believed that this paper was an important contribution to our knowledge about the mechanisms by which resveratrol and other chemicals may play a role in cardiovascular and other diseases. Such knowledge could help develop approaches for the prevention and treatment of human disease and for increasing the longevity of a healthy life.
Reference: Park S-J, Ahmad F, Philp A, Baar K, Williams T, Luo H, Ke H, Rehmann H, Taussig R, Brown AL, Kim MK, Beaven MA, Burgin AB, Manganiello V, Chung JH. Resveratrol ameliorates aging-related metabolic phenotypes by inhibiting cAMP phosphodiesterases. Cell 2012;148:421-433. DOI 10.1016/j.cell.2012.01.017.
Click here for the full critique of this paper by the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 069: Little effect of binge drinking on heart disease or mortality among moderate drinkers in Denmark — 2 February 2012
In a well-done, population-based analysis from Denmark, it was found that subjects who were overall “light-to-moderate” drinkers but reported an episode of “binge drinking” (consumption >5 drinks on an occasion) did not show differences in risk of ischemic heart disease (coronary disease) or total mortality than did other moderate drinkers who did not report such an episode. These results are somewhat different from results of many other epidemiologic studies that have shown increased risk of health problems (even higher risk of coronary disease) to be associated with what was referred to as “binge drinking.”
Why there were no adverse effects of such drinking in the present study has provoked considerable discussion among members of the Forum. The general consensus of opinion has to do with inconsistencies in the definition of “binge drinking.” The rapid consumption of more than 5 drinks on an empty stomach surely has different effects than the consumption of alcohol over several hours with food, such as during a prolonged dinner. The rate of consumption strongly affects the consequences of alcohol; in fact, some have suggested that the consumption of more than 2 or 3 drinks in less than two hours may constitute a better definition of binge that the total number of drinks.
The Forum continues to suggest that “binge drinking,” however defined, is not a healthy pattern of alcohol consumption. But the circumstances of consumption (rate of consumption, with or without food, etc.) may also be important in its definition and in judging its effects on health.
Reference: Skov-Ettrup LS, Eliasen M, Ekholm O, Grønbaek M, Tolstrup JS. Binge drinking, drinking frequency, and risk of ischaemic heart disease: A population-based cohort study. Scandinavian Journal of Public Health 2011;39:880–887.
Click here for the full critique of this study by the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 068. Heavier alcohol consumption may increase risk of colon cancer in people with a family history of such cancer — 30 January 2012
An analysis based on a large number of subjects being followed in the Nurses’ Health Study and the Health Professionals Follow-up Study, relates alcohol consumption to the risk of colon cancer according to whether or not the subjects had a positive family history of colon cancer. Their results indicate that subjects with a family history whose average alcohol intake was 30 or more grams per day (about 2 ½ typical drinks by US standards) have an increase in their risk of colon cancer; there was not a significant association between alcohol and colon cancer among subjects without a positive family history.
Forum reviewers were somewhat concerned that the pattern of drinking (regularly or binge drinking) was not assessed, and that there was not a clear dose-response curve between the level of alcohol consumption and the risk of cancer (i.e., there was not a consistent increase in risk of cancer with greater alcohol intake). Further, folate intake was found to modify the association, with the highest risk for subjects with a positive family history of colon cancer, low levels of folate, and in the highest category of alcohol consumption.
The present study provides some support for an association between higher levels of alcohol intake and the risk of colon cancer among subjects with a positive family history of such cancer. However, there have been changes in the guidelines for screening for cancer (by endoscopy, with removal of pre-malignant tumors) and other preventive measures for people with a positive family history of colon cancer. Such measures could modify the effects of all risk factors for colon cancer in future analyses.
Reference: Cho E, Lee JE, Rimm EB, Fuchs CS, Giovannucci EL. Alcohol consumption and the risk of colon cancer by family history of colorectal cancer. Am J Clin Nutr 2012;95:413–419.
Click here for the full critique of this paper by the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 067: Comparison of effects of red wine versus white wine on hormones related to breast cancer risk 19 January 2012
Aromatase inhibitors (AIs) prevent the conversion of androgens to estrogens, and could play a role in the development of breast cancer. This study of 36 pre-menopausal women consisted of a cross-over intervention trial to determine if there were differences between red wine and white wine in their effects on AIs. Subjects sequentially consumed eight ounces of red wine, followed by white wine (or vice versa), each beverage for a one-month period. The investigators concluded that red wine, but not white wine, was associated with significant effects on some indices of estrogen metabolism; free testosterone and luteinizing hormone were increased, but no significant differences were noted in estrogen levels.
Forum reviewers considered the results interesting and that they contribute to our understanding of the relation of wine to hormonal levels. On the other hand, they were concerned about methodological problems, including a lack of baseline data and variations in the timing during the menstrual period of blood sampling (which could affect estrogen levels). Also, no significant effect of the interventions was seen on blood levels of estradiol.
Further, the Forum thought that it should be pointed out that data are inconsistent on the relation of red wine consumption to the risk of breast cancer; many studies do not show beverage-specific effects on risk. More research will be needed to determine if the polyphenols in red wine can play a role in lowering the risk of breast cancer.
Reference: Shufelt C, Bairey Merz CN, Yang YC, Kirschner J, Polk D, Stanczyk F, Paul-Labrador M, Braunstein GD. Red versus white wine as a nutritional aromatase inhibitor in premenopausal women. J Women’s Health, 2011;DOI: 10.1089/jwh.2011.3001
Click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 066: Is it the alcohol or the polyphenols in red wine (or both) that decrease cardiovascular disease in wine drinkers? 16 January 2012
Human randomized intervention trials of wine and alcohol are not common. This randomized, cross-over study was based on 67 male volunteers in Spain who were considered to be at “high-risk” of cardiovascular disease. The subjects agreed to not consume any alcohol for a baseline period, then for three one-month periods consumed 30 g/day of alcohol as red wine or as gin, or an equivalent amount of phenolics from dealcoholized red wine. The effects of each intervention on a large number of adhesion molecules and chemokines that affect inflammation and relate to the development of vascular disease were evaluated.
The key results of the study were that both ethanol and nonalcoholic compounds in red wine have potentially protective effects that may reduce the risk of vascular disease. Specifically, the authors conclude that “the phenolic content of red wine may modulate leukocyte adhesion molecules, whereas both ethanol and polyphenols of red wine may modulate soluble inflammatory mediators in patients at high risk of cardiovascular disease.” Thus, this study provides important new mechanistic evidence that the reduced risk of cardiovascular disease among red wine drinkers observed in most epidemiologic studies may result from a combination of both the alcohol and the polyphenols in the wine.
Reference: Chiva-Blanch G, Urpi-Sarda M, Llorach R, Rotches-Ribalta M, Guillèn M, Casas R, Arranz S, Valderas-Martinez P, Portoles O, Corella D, Tinahones F, Lamuela-Raventos RM, Andres-Lacueva C, Estruch R. Differential effects of polyphenols and alcohol of red wine on the expression of adhesion molecules and inflammatory cytokines related to atherosclerosis: a randomized clinical trial. Am J Clin Nutr 2012. doi: 10.3945/ajcn.111.022889.
Click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 065: Are there differences in mortality between people consuming wine and those consuming other types of alcoholic beverages? 20 December 2011
Wine consumers, especially in comparison with spirits drinkers, have been shown to have higher levels of education and income, to consume a healthier diet, be more physically active, and have other characteristics that are associated with better health outcomes. However, epidemiologic studies have been inconsistent in showing that, after adjustment for all associated lifestyle factors, consumers of wine have lower risk of cardiovascular disease and mortality than do consumers of other beverages.
A study based on the long-term follow up of a group of older Americans concluded that the associated lifestyle habits and environmental factors of wine consumers largely explained their better health outcomes. Forum reviewers were concerned about some of the methodological approaches used, and believed that the data presented in the paper were inadequate to support such a conclusion. This was a small study, had only a single estimate of alcohol intake (at baseline but not throughout 20 years of follow up), and the authors may have over-adjusted for large differences in lifestyle factors between what they termed as “low-wine” and “high-wine” consumers. The study did confirm a lower mortality risk for alcohol consumers than for non-drinkers.
Experimental studies have clearly indicated that the polyphenols and other constituents that are present in wine and some beers have independent protective effects against most cardiovascular risk factors. Whether or not such advantages are seen among moderate drinkers of wine (or beer) in epidemiologic studies is difficult to determine, as comparisons are not being made between wine, beer, and spirits but between humans who consume one or other such beverage. In almost all populations, drinkers of a specific beverage differ in many ways other than just the type of beverage they consume.
Reference: Holahan CJ, Schutte KK, Brennan PL, North RJ, Holahah CK, Moos BS, Moos RH. Wine consumption and 20-year mortality among late-life moderate drinkers. J Stud Alcohol Drug 2012; 73: 80–88.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 064: Association of lifestyle and environmental factors with the risk of cancer — 13 December 2111
It has been well established that certain lifestyle habits relate to the risk of certain cancers (e.g., smoking and lung cancer). In a well-done analysis, the authors estimate the proportion of cancer in the population associated with a variety of lifestyle and environmental factors. They find that smoking has, by far, the largest effect on the risk of cancer, with 19.4% of cancer cases in the UK attributable to tobacco use. A poor diet (less intake of fruits and vegetables and fiber and greater intake of meat and salt), obesity, and alcohol are the next most important factors that relate to cancer, with alcohol being calculated to relate to 4.0% of cancer cases in the UK.
Forum reviewers considered this to be a well-done paper that used epidemiologic methods that are preferable to those used in some previous such analyses. Generally, they disagreed with the authors that no alcohol consumption was the theoretical “optimum exposure level,” as the risk of certain cancers seems to increase primarily from heavy drinking. Further, they found reason to believe that the purported effects related to diet may have been over-estimated.
Nevertheless, this paper provides considerable new information on lifestyle and environmental factors that may relate to the risk of cancer. It puts into perspective the importance of targeting certain behaviors for the potential reduction in the risk of cancer.
Reference: Parkin DM, Boyd L, Walker LC. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. Summary and conclusions. British Journal of Cancer 2011;105:S77 – S81.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 063: Genes modify the risk of liver disease among alcoholics — 5 December 2011
It has been widely observed that only a small percentage of alcoholics develop cirrhosis of the liver, the most advanced form of alcoholic liver disease (ALD); the reason why all alcoholics do not develop such disease is not known. The present study from Spain, that includes original work and a meta-analysis, evaluates whether genetic polymorphisms that determine levels of glutathione-S-transferases (GST) relate to the risk of developing ALD among alcoholics. Alcoholics with certain genetic GST polymorphisms were found to be at significant excess risk for such liver disease in comparison with alcoholics without these polymorphisms.
As stated by the authors, the theory that these enzymes may affect risk is based on the ability of certain GST alleles to detoxify harmful ethanol metabolites in the liver by conjugating acetaldehyde and ROS to reduced glutathione. The specific polymorphisms that they found to be associated with increased liver disease are among those that would be expected to lower the activity of the corresponding GST enzymes; this would permit higher levels of toxic metabolites of alcohol and oxidative stress to be present for longer periods of time after excessive alcohol consumption.
Some Forum reviewers thought that while the study was well done, the authors were unclear as to how these data could directly lead to “potential therapeutic targets” for liver disease in alcoholics. Nevertheless, the original study and meta-analysis provide important data on how specific genetic factors relate to the development of liver disease among alcoholics and could theoretically lead to better strategies for the prevention and treatment of alcoholic liver disease.
Reference: Marcos M, Pastor I, Chamorro A-J, Ciria-Abad S, González-Sarmiento R, Laso F-J. Meta-analysis: glutathione-S-transferase allelic variants are associated with alcoholic liver disease. Aliment Pharmacol Ther 2011;34:1159–1172.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 062: Similar effects of beer and wine on the risk of cardiovascular disease and of total mortality — 22 November 2011
The authors carried out an updated meta-analysis on the relationship between wine, beer or spirit consumption and cardiovascular outcomes, using state-of-the-art statistical techniques. Their meta-analysis provides evidence of J-shaped relationships between both wine and beer intake and vascular risk, with maximal protection of about 33% at a level of 25 g/day of alcohol (approximately 2 drinks/day by US standards). A statistically significant association between spirits intake and vascular disease was not found.
The key result of this meta-analysis is the finding of a very similar inverse association between the consumption of beer and the consumption of wine in relation to cardiovascular outcomes. While a similar associationwas not seen for spirits consumption, the data presented do not permit the conclusion that the key effects on cardiovascular disease are primarily due to the polyphenols in beer and wine. Similarly, the results do not permit the conclusion that the effect on cardiovascular disease is due primarily to the alcohol in these beverages. The lack of a similar J-shaped association for spirits may have been due to different drinking patterns (e.g., more binge drinking among consumers of spirits), as the pattern of drinking was not included as a confounder in the analyses.
Reference: Costanzo S, Di Castelnuovo A, Donati MB, Iacoviello L, de Gaetano G. Wine, beer or spirit drinking in relation to fatal and non-fatal cardiovascular events: a meta-analysis. Eur J Epidemiol 2011;DOI 10.1007/s10654-011-9631-0
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
A response from the Alcohol Policy Coalition of Australia to the Forum Critique #058: “A misguided statement on alcohol and health from a coalition in Australia,” which was published on the Forum web-site on 28 September 2011.
The Alcohol Policy Coalition of Australia has provided a response to Forum critique #058, “A misguided statement on alcohol and health from a coalition in Australia,” that was published on the Forum web-site on 28 September 2011.
The original Forum critique is available under Recent Reviews, #058 (click Critique o58). A description of the Forum, its members, the goals of the Forum, a disclosure statement, etc., are available from the home page of the web-site.
The response from the Alcohol Policy Coalition is now published in full on our web-site, dated 18 November 2011. To read the response to our critique # 058 provided by the Alcohol Policy Coalition, please click here.
===============================================================================
Critique 061: The reduction in risk of coronary heart disease from alcohol consumption may involve mechanisms other than an increase in HDL-cholesterol. 10 November 2011
In a prospective, observational study of approximately 150,000 Norwegians, the investigators found that alcohol consumption was associated with a large decrease in the risk of death from coronary artery disease. For men, the fully adjusted hazard ratio for cardiac death was 0.52 (95% CI 0.39 – 0.69) when comparing subjects reporting more than one drink/week in comparison with those reporting never or rarely drinking; for women, it was 0.62 (0.32–1.23). There was little change in the hazard ratio when HDL-cholesterol (HDL) was added to the model, suggesting that very little of the lower risk of heart disease was due to an increase in HDL from alcohol consumption.
Forum members considered this a well-done analysis. They were surprised at the very low amounts of alcohol intake reported by the subjects, with only 16% of males and about 8% of females reporting more than one drink/week. It is possible that the low levels of drinking, or perhaps over-adjustment in the multivariable analysis, led to the lack of effect of HDL. Most other studies have shown a much larger proportion of the effect of alcohol on heart disease risk to be associated with an increase in HDL.
Reference: Magnus P, Bakke E, Hoff DA, Høiseth G, Graff-Iversen S, Knudsen GP, Myhre R, Normann PT, Næss Ø, Tambs K, Thelle DS, Mørland J. Controlling for High-Density Lipoprotein Cholesterol Does Not Affect the Magnitude of the Relationship Between Alcohol and Coronary Heart Disease. Circulation 2011;124: DOI: 10.1161/CIRCULATIONAHA.111.036491
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 060: A new analysis from the Nurses’ Health Study on the association of alcohol with risk of breast cancer 3 November 2011
In a well-done analysis using prospectively collected data from the Nurses’ Health Study, the risk of breast cancer was found to be modestly increased among consumers of alcohol, even those whose total alcohol consumption was reported to be in the range of 3 to 6 drinks/week. Similar small increases in the risk of breast cancer have been found from alcohol consumption in the majority of previous studies observational studies. A strength of this study was the very large number of subjects, permitting the investigators to attempt to determine if both the amount of alcohol and the frequency of consumption were important in this association; strong effects were not found for either. A weakness is the failure to report the effects of folate intake on the association between alcohol and cancer; the same investigators have previously shown that folate is a potential moderator of the effects of alcohol on breast cancer risk.
The authors describe well the dilemma that women face regarding alcohol intake, which may increase slightly the risk of breast cancer but markedly decrease the risk of other more common diseases, especially cardiovascular conditions. For example, the authors state that regarding breast cancer, “We did find an increased risk at low levels of use, but the risk was quite small.” Forum members agree with the statement of the authors that “An individual will need to weigh the modest risks of light to moderate alcohol use on breast cancer development against the beneficial effects on cardiovascular disease to make the best personal choice regarding alcohol consumption.”
Reference: Chen WY, Rosner B, Hankinson SE, Colditz GA, Willett WC. Moderate alcohol consumption during adult life, drinking patterns, and breast cancer risk. JAMA 2011;306:1884-1890.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 059: Association of quantity of alcohol and frequency of consumption with cancer mortality
20 October 2011
A paper from the National Institutes of Health in the United States attempts to evaluate the separate and combined effects of the frequency of alcohol consumption and the average quantity of alcohol per occasion as they relate to the risk of mortality from all cancers, as well as cancer-specific mortality. It is based on repeated administrations of the National Health Interview Survey in the United States, with a total of more than 300,000 subjects and over 8,000 deaths from cancer, and reports on total cancer deaths and deaths from lung, colorectal, prostate, and breast cancers.
For total alcohol consumption (frequency x quantity), the data indicate a significant reduction in the risk of all-site cancers (RR=0.87, CI 0.80-0.94) which, interestingly, is not emphasized by the authors and is not included in their abstract. Moderate drinking consistently shows no effect, and only heavier drinking is associated with an increase in all-site cancer risk. For site-specific cancers, an increase in risk of lung cancer was seen only for heavier drinkers, with a tendency for less cancer among light drinkers. There was no evidence of an effect of total alcohol consumption on colorectal, prostate, or breast cancer.
The authors excluded non-drinkers in a second analysis in which they used categories of usual daily quantity and of frequency of consumption in an attempt to investigate their separate effects. For all-site cancer and for lung cancer, these results again show an increase in risk only for drinkers reporting greater amounts of alcohol. The data also show an increase in cancer risk from more frequent drinking among women but not among men. For colorectal, prostate, and breast cancer, there is no clear pattern of an increase in risk from quantity of alcohol consumed. For frequency of drinking, again there is a suggestion of an increase in risk with more frequent drinking, although the trends are not statistically significant.
The overall message of this analysis is that light to moderate alcohol intake does not appear to increase the risk of all-site cancer (and light drinking was shown in this study to be associated with a significant decrease in risk). Similarly, light to moderate consumption was not associated with site-specific cancers of the lung, colorectum, breast, or prostate. Heavier drinking is known to be associated with a large number of adverse health effects, including certain cancers, as was shown in this study.
When considering cancer, alcohol consumption should not be considered in isolation, but in conjunction with, other lifestyle behaviors (especially smoking). We agree with the authors that both quantity and frequency of consumption need to be considered when evaluating the relation of alcohol to cancer; further, beverage-specific effects need to be further evaluated.
Reference: Rosalind A. Breslow RA, Chen CM, Graubard BI, Mukamal KJ. Prospective study of alcohol consumption quantity and frequency and cancer-specific mortality in the US population. Am J Epidemiol 2011; DOI: 10.1093/aje/kwr210.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 058: A misguided statement on alcohol and health from a coalition in Australia. 28 September 2011
A group known as the Alcohol Policy Coalition in Australia has released a document entitled Cancer, Cardiovascular Disease and Alcohol Consumption. Forum members agree that excessive alcohol use has many adverse effects on the individual and on society, and efforts to reduce such use are important. On the other hand, they were disturbed that the coalition statement was limited almost exclusively to the effects of abusive drinking, was based primarily on extremely limited sources of information (mainly position statements by other organizations, and not publications based on sound research), and indicated a strong bias against alcohol.
Forum members contend that the Australian report misrepresents the extensive scientific data available on alcohol and health. The report specifically ignores scientific data indicating that in all developed countries, moderate consumers of alcohol are at much lower risk of essentially all of the diseases of ageing: coronary heart disease, ischemic stroke, diabetes, and dementia. And conspicuously absent from the Australian report is a description of the lower total mortality among middle-aged and elderly people associated with moderate alcohol consumption, a finding that has been found consistently throughout the world. Further, there is no mention in the report of the key relevance of the pattern of drinking, although regular moderate drinking (versus binge drinking only on week-ends, even when the total volume of alcohol is the same) has been shown to be a strong determinant of beneficial effects of alcohol consumption.
Scientific data over many decades have shown that while excessive or irresponsible alcohol use has severe adverse health and societal effects, regular moderate drinking is associated with beneficial effects on health. And a very large number of experimental studies, including results from human trials, have described biological mechanisms for the protective effects of both alcohol and the polyphenolic components of wine.
There have been a number of comprehensive meta-analyses published that Forum members believe can provide much more accurate, up to date, and scientifically balanced views of the current status of the health effects of alcohol consumption. Such documents are better sources of data upon which policy decisions should be based.
Reference: Alcohol Policy Coalition Position Statement. “Cancer, Cardiovascular Disease and Alcohol Consumption.” Released in Australia, September 2011.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 057: Differences in effects on atherosclerosis of regular moderate drinking and binge drinking. An experimental study in mice. 20 September 2011
An excellent study among experimental animals has reported very dramatic differences between the effects of alcohol administered in moderation on a daily basis and the same total weekly amount of alcohol administered on only two days of the week: binge drinking. The mice used in the study that were given regular moderate amounts of alcohol showed no weight gain, improved lipid values, and much less development of atherosclerosis than did control animals. However, those given alcohol in a binge-drinking pattern showed worse outcomes than control animals, and much worse outcomes than those given regular moderate alcohol.
This experimental study provides strong support for the frequent finding among humans in epidemiologic studies: benefits from regular moderate drinking, adverse effects from binge drinking. It is especially important since, being an experimental study, the potential confounding effects of other lifestyle habits are not an issue, as is always the case for observational studies among humans.
Reference: Liu W, Redmond EM, Morrow D, Cullen JP. Differential effects of daily-moderate versus weekend-binge alcohol consumption on atherosclerotic plaque development in mice. Atherosclerosis 2010, doi:10.1016/j.atherosclerosis.2011.08.034
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 056: Relation of alcohol consumption to colorectal cancer 13 September 2011
A meta-analysis of case-control and cohort studies on the association of alcohol consumption with colorectal cancer was carried out, based on 22 studies from Asia, 2 from Australia, 13 from Western Europe, and 24 from North America. The paper provides evidence that alcohol, at least at higher levels of consumption, is associated with an increase in the risk of colorectal cancer. Overall, there was no increase in the risk for consumers reporting an average intake of up to 1 drink per day, but a modest increase (of 21%) for what the authors defined as “moderate drinking” (averaging up to 49.9 g of alcohol, or about 4 typical drinks, per day). The increase in risk was greater (52%) for consumers of 50 or more grams of alcohol per day.
Forum reviewers thought that this was, in general, a very well-done study that used appropriate statistical techniques for meta-analysis. There were some key concerns, however, including the following: (1) the authors’ definition of “moderate drinking” extended well above the usual recommended limits for sensible drinking; effects of consumption in categories of 1 to 2 drinks/day, 2 to 3 drinks/day, etc., were not given; (2) no results were provided according to type of beverage even though many previous studies have shown differences between health effects for consumers of wine, or wine/beer, and other beverages; and (3) no data were available on the pattern of drinking. Many studies have shown that regular, moderate drinking on most days of the week has very different health outcomes than drinking only on week-ends or binge drinking.
Despite these concerns, Forum members agreed that current data indicate that alcohol intake, especially heavier drinking, is associated with an increase in the risk of colorectal cancers. Future studies are needed to help determine if there is a threshold level of alcohol that increases the risk, if there are differences by type of beverage, and if the pattern of drinking (regular versus binge drinking) affects the risk.
Reference: FedirkoV, Tramacere I, Bagnardi V, Rota M, Scotti L, Islami F, et al. Alcohol drinking and colorectal cancer risk: an overall and dose–response meta-analysis of published studies. Annals of Oncology 22: 1958–1972, 2011, doi:10.1093/annonc/mdq653
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 055. Alcohol intake and “successful ageing” 8 September 2111
Among 13,894 women in the Nurses’ Health Study, investigators prospectively examined alcohol use assessed at midlife in relation to “successful ageing,” which was defined as survival to age 70 years, not having a major chronic disease (such as coronary disease, cancer, stroke, diabetes), and having no major cognitive impairment, physical impairment, or mental health problems. Only 11% of the women met these criteria.
The results indicate that moderate drinkers, especially those consuming wine and drinking regularly, were more likely to exhibit successful ageing. For average amount consumed, the largest benefit (an increase of 28%) was among women who reported 15.1 – 30 g of alcohol per day (an average of just over 1 to 2 ½ drinks per day), when compared with non-drinkers. The frequency of drinking was especially important: in comparison with nondrinkers, women who drank only on 1 to 2 days per week had little increase in their risk of successful ageing, but those drinking on at least 5 days per week had almost a 50% greater chance of successful ageing.
Forum reviewers had some questions about the definition of “successful ageing” used in this study. It is believed that a much greater percentage of people who may not meet these criteria make huge contributions to society and should be considered “successful.”
In summary, these results support the findings of earlier studies showing that many aspects of successful ageing, in addition to just survival, are favorably affected by regular, moderate consumption of alcohol.
Reference: Sun Q, Townsend MK, Okereke OI, Rimm EB, Hu FB, Stampfer MJ, Grodstein F. Alcohol consumption at midlife and successful ageing in women: A prospective cohort analysis in the Nurses’ Health Study. PLoS Med 8(9): e1001090. doi:10.1371/journal.pmed.1001090
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 054. Role of alcohol intake and smoking on upper aerodigestive cancers – 6 September 2011
This paper provies an extensive analysis of the proportion of the risk of upper aero-digestive tract (UADT) cancers in the population (the population attributable risk) may be due to alcohol consumption and/or smoking. The analyses provide strong evidence that smoking is the most important factor in the risk of these cancers, and the risk is enhanced among those who also consume 2 or more drinks per day. Alcohol alone (i.e., among non-smokers) has little effect on the risk.
The authors state that their observations “are consistent with the hypothesis that alcohol acts as a carcinogen primarily because of its promoting effect on tobacco smoke.” In terms of the population-attributable risk, the authors conclude that “Our findings confirm that tobacco and alcohol together explain 73% of total UADT cancer burden in Europe.” Overall, tobacco use alone explained 28.7%, the combination of smoking and drinking 43.9%, and alcohol use alone only 0.4% of the population attributable risk. Among women, the risk of these cancers was higher among smokers than among those who both smoked and consumed alcohol; this perhaps suggests that the moderate intake of wine, the most common beverage among European women, may play a role in reducing the risk associated with smoking.
Forum reviewers thought that this was a very good paper, but hoped that in the future we would have more studies that evaluated the effects on risk of varying levels of alcohol consumption, differential effects of various beverages, and even differential effects according to subjects’ genetically determined differences in alcohol metabolizing enzymes.
Reference: Anantharaman D, Marron M, Lagiou P, Samoli E, Ahrens W, Pohlabeln H, et al. Population attributable risk of tobacco and alcohol for upper aerodigestive tract cancer. Oral Oncology 2011;47:725–731.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 053: An extensive review of the effects of alcohol consumption on the risk of cognitive impairment and dementia 25 August 2011
The authors of this paper have carried out an excellent review of the relation of alcohol consumption to the risk of cognitive impairment and dementia. They reviewed a total of 143 previous publications on the topic. There were 74 studies, based on a total of more than 250,000 subjects, that provided risk estimates for varying levels of alcohol consumption which allowed the investigators to include them in a comprehensive meta-analysis. These papers were published mainly after 1998, were predominantly among older subjects (92% were ≥ 55 years of age and 70% ≥ 65 years of age), and almost all employed mental status examinations to define cognitive impairment/dementia.
As stated by the authors, “These studies overwhelmingly found that moderate drinking either reduced or had no effect on the risk of dementia or cognitive impairment.” Overall, in the new meta-analysis based on these studies, the average ratio of risk for cognitive risk associated with moderate drinking of alcohol was 0.77, with nondrinkers as the reference group. This estimate is close to the estimates of reduction in the risk of cognitive dysfunction (RR of 0.73 and 0.74) seen in other recent selective meta-analyses. The present study found that both light and moderate drinking provided a similar benefit, but heavy drinking was associated with non-significantly higher cognitive risk for dementia and cognitive impairment.
Forum reviewers of this paper were particularly pleased that the authors attempted to answer a number of specific questions on this topic that have been raised from previous research. Their results included finding no appreciable differences whether or not “sick quitters” were included in the reference group, little effect from adjustments for other lifestyle factors, and no significant differences between alcohol’s effects on dementia, Alzheimer’s dementia, or vascular dementia (but, based on a small number of studies, no significant reduction in risk of cognitive decline over time). The investigators concluded that there were no differences between results in men and women. Their analyses also led to the conclusion that wine is associated with more beneficial effects on cognition than beer or spirits, but the authors caution that these results are based on a limited number of reports, and that many studies show no significant differences according to type of beverage.
Forum reviewers agreed with the conclusions of the authors that “Overall, light to moderate drinking does not appear to impair cognition in younger subjects and actually seems to reduce the risk of dementia and cognitive decline in older subjects.”
Reference: Neafsey EJ, Collins MA. Moderate alcohol consumption and cognitive risk. Neuropsychiatric Disease and Treatment 2011:7:465–484.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 052: Does moderate alcohol consumption increase body weight? 16 August 2011
A paper from Spain provides an extensive review of the association between alcohol consumption and body weight. It includes descriptions of cross-sectional and prospective studies (and a few small intervention studies) among subjects who varied in age (adolescence to old age), culture (from Americans and Europeans to Asians), and principal type of beverage consumed and pattern of drinking. The authors state that many of the studies they reviewed appear to be contradictory in their results. However, based on their review, they conclude that “as positive associations between alcohol and weight gain were mainly found in studies with data on higher levels of drinking, it is possible that an effect on weight gain or abdominal adiposity may only be experienced by heavy drinkers.” A second conclusion of the authors is that “the type of alcoholic beverage might play an important role in modifying the effect of alcohol consumption on weight gain,” with more favorable effects generally seen among consumers of wine. A formal meta-analysis is not provided. Forum members were uncertain whether the higher risk seen for spirits drinkers in this study was due to the beverage they chose or to their consumption of larger amounts of alcohol.
The overall conclusions of the authors is that it is currently unclear whether alcohol consumption a risk factor for weight gain, but if so it appears to occur mainly among heavier drinkers. They also state that “light-to-moderate alcohol intake, especially of wine, may be more likely to protect against, rather than promote, weight gain.”
Forum reviewers agreed with most of the conclusions of the authors, especially that current data do not clearly indicate if moderate drinking increases weight; further, the biologic mechanisms relating alcohol to changes in body weight are not well understood. The Forum review comments on the strong protective effects of moderate drinking on the risk of metabolic syndrome and diabetes, both of which relate to increasing obesity. And some studies suggest that even very obese people may be at lower risk of diabetes if they are moderate drinkers. Forum members also reviewed some of the distinctive mechanisms by which alcohol is metabolized in the body (it provides calories that are rapidly absorbed and are not stored in fat) that could explain differences in the effects of calories from alcohol and from other foods.
Forum members agree with the authors of this paper that future research efforts should be directed towards assessing the specific roles of different types of alcoholic beverages, taking into account drinking patterns, and perhaps including in the analysis the propensity of individual subjects to gain weight in the past. For now, there is little evidence that someone consuming small to moderate amounts of alcohol on a regular basis is increasing his or her risk of becoming obese.
Reference: Sayon-Orea C, Martinez-Gonzalez MA, Bes-Rastrollo M. Alcohol consumption and body weight: a systematic review. Nutrition Reviews 2011;69:419-431.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 051: Types of alcohol in relation to acute pancreatitis 11 August 2011
A very well-done analysis from scientists in Sweden has related the type of alcoholic beverage, and the amount consumed per occasion, to the risk of acute pancreatitis. The study suggests that a greater number of drinks per occasion (“binge drinking”) of spirits increases the risk of acute pancreatitis, but no such relation was seen for the consumption of beer or wine. Forum reviewers suggested that a faster rate of drinking, with a greater rise in BAC, for spirits drinkers may be an important factor in the observed higher risk of pancreatitis; the increased risk may not necessarily be due to lower levels of antioxidants or to the presence of other toxic substances in spirits.
In any case, the average total alcohol consumption did not affect the risk of pancreatitis; instead, it was the number of drinks consumed per occasion (of spirits, in this study) that was associated with an increase in risk. Residual confounding by the pattern of drinking, diet, or by other lifestyle factors could still be operating, and it will require replication of these results in other studies to support the conclusions of the authors.
Reference: Azodi OS, Orsini N, Andrén-Sandberg Å, Wolk A. Effect of type of alcoholic beverage in causing acute pancreatitis. Brit J Surgery 2011;DOI: 10.1002/bjs.7632.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 050: Multiple maternal risk factors for fetal alcohol disorders 7 August 2011
An extremely well researched and written review on the relation of maternal drinking during pregnancy to adverse fetal outcomes has been published by scientists from the University of New Mexico Center on Alcoholism, Substance Abuse, and Addictions. It covers many factors (host, agent exposure, and environment) that have been found to relate to the occurrence of fetal alcohol spectrum disorders (FASD). Such factors modify the risk associated with alcohol consumption during pregnancy, although the risk of abnormalities is clearly increased with frequent consumption of large amounts of alcohol, and is greater among women who are alcoholics. While current data do not show that light or occasional alcohol consumption during pregnancy increases the risk of FASD, Forum members do not believe that pregnant women should be encouraged to drink.
Forum members agree with the authors that “More research is needed to more clearly define what type of individual behavioral, physical, and genetic factors are most likely to lead to having children with FASD.” Evaluating these multidimensional factors should help identify women at particular risk for having a child with FASD and lead to interventions to prevent such fetal abnormalities.
Reference: May PA, Gossage JP. Maternal risk factors for fetal alcohol spectrum disorders. Not as simple as it might seem. Alcohol Research & Health 2011;34:15-26.
For the full critique of this article by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 049: Effects of smoking and alcohol use on risk of upper aero-digestive cancers 1 August 2011
A case-control analysis from subjects living in areas of South America with high rates of upper aero-digestive tract cancers showed that both alcohol consumption and smoking tended to increase the risk of such cancers. However, the predominant cause of these cancers was the combination of smoking and alcohol consumption, with much higher risk than either exposure alone. The effects on risk were greater for smoking than for alcohol: for non-smokers, there was little effect of alcohol on risk. For non-drinkers, the risk of cancer associated with smoking was still increased, but was lower than it was for current drinkers.
An especially important finding in this study was that, among ex-drinkers and former smokers, the increased risks associated with alcohol and tobacco use decreased steadily as the time since quitting increased. As stated by the authors, most of these cancers “could be prevented by quitting the use of either of these two agents.”
Reference: Szymańska K, Hung RJ, Wűnsch-Filho V, Eluf-Neto J, Curado MP, Koifman S, Matos E, Menezes A, Fernandez L, Daudt AW, Boffetta P, Brennan P. Alcohol and tobacco, and the risk of cancers of the upper aerodigestive tract in Latin America: a case–control study. Cancer Causes Control (2011) 22:1037–1046. DOI 10.1007/s10552-011-9779-7
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 048: A new report on drinking guidelines and the association of alcohol with risk of cancer. 18 July 2011
The Canadian Medical Association Journal has published a commentary by some French scientists relating drinking guidelines to the association between alcohol and cancer. They conclude that the current guidelines for sensible drinking for the general population are not adequate for the prevention of cancer, and revisions and eventual exclusion of such guidelines are needed.
Forum reviewers agree that alcohol consumption, especially heavy intake, increases the risk of certain types of cancer. However, they consider that the opinions of the authors in the paper (labeled as an “Analysis” rather than an editorial or comments) do not reflect current sound scientific data, that the report is highly selective in citing a small number of papers that support their opinions, and that the authors have ignored a huge amount of recent data from more scientifically sound research that have largely discredited such studies. Further, the report provides no mention of the consistent finding from studies around the world that moderate drinkers tend to have lower all-cause mortality risk than do abstainers.
Scientific data over many decades have shown that excessive or irresponsible alcohol use has severe adverse health effects, including an increase in the risk of certain cancers. On the other hand, moderate drinking is associated with lower risk of cardiovascular disease and many other diseases of ageing and with all-cause mortality. A very large number of experimental studies, including results from human trials, have described biological mechanisms for the protective effects of alcoholic beverages against such diseases. A number of comprehensive meta-analyses provide much more accurate, up to date, and scientifically balanced views than does the current paper; such documents may be better sources of data upon which guidelines to the public regarding alcohol consumption should be based.
Reference: Latino-Martel P, Arwidson P, Ancellin R, Druesne-Pecollo N, Hercberg S, Le Quellec-Nathan M, Le-Luong T, Maraninchi D. Alcohol consumption and cancer risk: revisiting guidelines for sensible drinking. CMAJ 2011. DOI:10.1503. /cmaj.110363
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 047: Overall health effects of alcohol consumption. Comments on a WHO report 10 July 2011
The World Health Organization (WHO) has released its global status report on alcohol and health for 2011. Forum members largely agreed with the discussion in the report of the serious health and societal problems associated with the misuse of alcohol, which contributes to accidents, many diseases, and premature deaths. On the other hand, Forum members were disturbed that the report was limited almost exclusively to abusive drinking, was based primarily on out-dated information, and minimized the beneficial health effects associated with moderate drinking. The report ignored a massive amount of scientific data indicating that in all developed countries, moderate consumers of alcohol are at much lower risk of essentially all of the diseases of ageing: coronary heart disease, ischemic stroke, diabetes, dementia, and osteoporosis. And conspicuously absent from the WHO report is a description of the decrease in total mortality among middle-aged and elderly people associated with moderate alcohol consumption, a finding that has been found consistently throughout the world.
Epidemiologic studies over many decades have shown that while excessive or irresponsible alcohol use has severe adverse health and societal effects, moderate drinking is associated with lower risk of cardiovascular disease and other diseases of ageing. And a very large number of experimental studies, including results from human trials, have described biological mechanisms for the protective effects of both alcohol and the polyphenolic components of wine. A number of comprehensive meta-analyses are cited by Forum reviewers which they consider to provide much more accurate, up to date, and scientifically balanced views of the current “status” of the health effects of alcohol consumption. Such documents are better sources of data upon which policy decisions should be based.
Reference: Global status report on alcohol and health. World Health Organization 2011. ISBN 978 92 4 156415 1 (NLM classification: WM 274)
For the full critique of this publication by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 046: All-cause mortality rates are lower among moderate drinkers than among abstainers. 4 July 2011
The author of this paper set out to determine the extent to which potential “errors” in many early epidemiologic studies led to erroneous conclusions about an inverse association between moderate drinking and coronary heart disease (CHD). His analysis is based on prospective data for more than 124,000 persons interviewed in the U.S. National Health Interview Surveys of 1997 through 2000 and avoids the pitfalls of some earlier studies. He concludes that the so-called “errors” have not led to erroneous results, and that there is a strong protective effect of moderate drinking on CHD and all-cause mortality.
The results of this analysis support the vast majority of recent well-done prospective studies. In the present paper, non-drinkers had much higher risk of death than did almost all categories of subjects consuming alcohol. The author contends that these results lend credence to the argument that the relationship between alcohol and mortality is causal.
While some Forum reviewers felt that this analysis only replicates what has been shown in many other papers, it appears that erroneous information continues to be used by some policy groups. Thus, most reviewers believe that this new analysis provides important information on potential health effects of moderate drinking.
Reference: Fuller TD. Moderate alcohol consumption and the risk of mortality. Demography 2011. DOI 10.1007/s13524-011-0035-2
For the full review of this publication by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 045: Alcohol drinking in the elderly: Risks and benefits. 26 June 2011
The Royal College of Psychiatrists of London has published a report related primarily to problems of unrecognized alcohol misuse among the elderly. The report provides guidelines for psychiatrists and family physicians on how to find and how to treat elderly people with misuse of alcohol and drugs. The report also mentions lower “sensible limits” for older people in comparison with younger people. The Forum reviewers point out, however, inherent difficulties in providing guidelines for a very non-homogenous group of individuals whose only criterion for inclusion is being above the age of 65 years. Such a group includes individuals varying from marathon runners to very sick, frail people. Forum reviewers thought that advice to lower limits of drinking for everyone in this age group is not based on reliable research, and would certainly not apply to all in this age group.
The Forum reviewers were also struck by the absence in the Royal College report of any discussion of the strong positive effects of moderate drinking on most of the diseases of ageing, especially cardiovascular diseases, diabetes, and dementia, which are leading causes of morbidity and mortality in this age group. For healthy moderate and responsible drinkers, advice to reduce or stop all alcoholic beverage intake would not be in the best health interests of such individuals.
Reference: Royal College of Psychiatrists, London. Our invisible addicts. First Report of the Older Persons’ Substance Misuse Working Group of the Royal College of Psychiatrists, College Report CR165. June 2011
For the full review of this publication by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 044: The association of alcohol drinking with migraine headache 12 June 2011
An excellent paper from a headache center in Italy summarizes the scientific data relating alcohol ingestion to migraine headaches. The factors that trigger an attack of migraine, or of other headaches as well, are poorly understood. While retrospective studies tend to include alcohol as a trigger for an attack, the authors describe that in a recent prospective study (in which information on the factors that could potentially trigger an attack were collected prior to the migraine attack), menstruation, stress, and fatigue were found most commonly to relate to a subsequent attack, but not alcohol consumption (in fact, beer consumption on the previous day reduced the risk of a migraine attack). In the present paper, the authors reviewed the role and mechanism of action of alcohol or other components of alcoholic drinks in relation to alcohol-induced headache. They conclude from their review that reports overestimate the role of alcohol, as well as other foods, in the triggering of migraine.
Forum members thought that this was a very balanced review of the subject, and that it provided straightforward and sensible advice. Although some individuals surely have the onset of a migraine or other type of headache after the consumption of wine or alcohol, the findings are not consistent. Forum members suggest that given that subjects reporting migraine headaches have been found to be at increased risk of cardiovascular disease, it would not be appropriate to advise all such sufferers to avoid alcohol. As suggested by the authors of this paper, it may be reasonable for those subjects who had a desire to consume alcohol to drink small amounts of specific beverages to see if each beverage was tolerated or not. After seeing the effects, and factoring in symptoms versus potential benefits from moderate drinking, a reasonable discussion can be carried out with respect to continued alcohol use by subjects with migraine.
Reference: Panconesi A, Bartolozzi ML, Guidi L. Alcohol and migraine: What should we tell patients? Curr Pain Headache Rep 2011;15:177–184. DOI 10.1007/s11916-011-0184-4.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 043: Frequent moderate drinking of alcohol is associated with a lower risk of fatty liver disease. 23 May 2011
In a large study of men in Japan, the presence of fatty liver disease by ultrasonography showed an inverse association with the frequency of alcohol consumption; there was some suggestion of an increase in fatty liver disease with higher volume of alcohol consumed per day. Moderate drinkers had lower levels of obesity than did non-drinkers, and both obesity and metabolic abnormalities were positively associated with fatty liver disease.
These findings support the results of a number of other recent studies showing that moderate drinking does not increase the risk of this common type of liver disease; instead, it is associated with a lower risk of its occurrence. We agree with the implications of these studies as stated by the authors: “These results suggest that lifestyle modifications aimed at fighting central obesity and metabolic abnormalities should be the most important recommendations for the management of fatty liver. In addition, it seems unlikely that the risk of fatty liver can be reduced by the discontinuation and/or reduction of alcohol consumption alone.”
Reference: Hiramine Y, Imamura Y, Uto H, Koriyama C, Horiuchi M, Oketani M, Hosoyamada K, Kusano K, Ido A, Tsubouchi H. Alcohol drinking patterns and the risk of fatty liver in Japanese men. J Gastroenterol 2011 46:519–528. DOI 10.1007/s00535-010-0336-z.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 042: An increase in risk of certain types of gastric cancer from heavy drinking, but no increase from moderate alcohol consumption 17 May 2011
A very well-done meta-analysis supports other data generated on the risk of alcohol consumption and gastric cancer – that is – that the risk may be real for heavy alcohol consumption but not for moderate intake. The type of gastric cancer relating to heavier alcohol intake in this study tended to be tumors involving the noncardia, but differences between the association with tumors of the gastric cardia were not significant.
There was no increased risk of gastric cancer from alcohol among Asians; this may be due to lower alcohol intake; there is a greater prevalence among Asians of the inactive ALDH2 genotype that is associated with flushing and other adverse effects of alcohol, and such subjects tend to drink less alcohol. However, a number of studies have shown higher risk for upper aero-digestive cancers for subjects with this ALDH2 genotype, so the overall reason for the lower risk among Asians in this study remains unclear. The main outcome of the study is that there is no increase in the risk of gastric cancer associated with the moderate intake of alcohol.
Reference: Tramacere I, Negri E, Pelucchi C, Bagnardi V, Rota M, Scotti L, Islami F, Corrao G, La Vecchia C, Boffetta P. A meta-analysis on alcohol drinking and gastric cancer risk. Ann Oncology 2011;doi:10.1093/annonc/mdr135
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 041: Estimated health effects of changes in advice for alcohol consumption between the 2005 and 2010 Dietary Guidelines for Americans 6 May 2011
This paper from the National Institute on Alcohol Abuse and Alcoholism in the US suggests that the changes in wording of the alcohol recommendations in the Dietary Guidelines for Americans between 2005 and 2010 indicate that some at-risk drinkers could be classified as moderate drinkers. The authors carried out an analysis using data from a large, nationally representative sample of U.S. adults to estimate differences between subjects following the 2005 recommendations and a “gray zone” of subjects who exceed the 2005 recommendations but fall within the moderate guidelines according to the 2010 recommendations. The differences between these two groups were minimal; other than the gray zone subjects having an increased risk of alcohol dependence (which is unlikely to relate to their slight differences in consumption), the only other differences between the two groups related to alcohol-related interpersonal relations and job loss. And, as the authors state, “There were no associations with medical conditions or mental disorders.”
More importantly, the authors state that “Moreover, of the gray area drinkers who experienced incident alcohol dependence and interpersonal problems, 89% of the former and 94% of the latter had moved out of the gray area and into the highest-risk consumption group over the course of the follow-up interval.” Problems were thus very rare in those who remained in the gray zone of drinking during follow up.
Obviously, drinking 3 or 4 drinks/day (other than doing so only occasionally) should not be considered a healthy way to consume alcohol. But if, as the authors state, almost all of the estimated effects on health are due to subjects who increase their drinking above this “gray zone,” there is little support for their argument that the changes in guidelines make a difference.
Reference: Dawson DA, Grant BF. The “Gray Area” of consumption between moderate and risk drinking. J Stud Alcohol Drugs 2011;72:453–458.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 040: Lower risk of coronary heart disease from alcohol, even with heavy drinking 27 April 2011
Using data from The 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions study (the NESARC study, n = 43,093), the authors of this paper conclude that alcohol may have cardioprotective effects not only in moderate drinkers, but also in individuals with patterns of use traditionally considered as “hazardous.” While such a finding has been shown in some population studies, there were questions by Forum reviewers as to the adequacy of the method for diagnosing coronary artery disease: self-report, with most subjects listing angina pectoris, a “soft” criterion for coronary disease.
In addition, the categories of drinking used in this study were very broad: rare or only occasional drinkers were combined with regular drinkers up to 7 or 14 drinks per week in the “moderate” category; the “hazardous” category included a broad range of drinkers, from a minimal increase over the recommended limits to very heavy drinkers. The pattern of drinking (especially the number of days per week that alcohol was consumed) was not reported, making it difficult to separate regular from heavy week-end drinkers. The effects of heavier drinking on other conditions (such as alcohol-related liver disease, mortality, etc.) were not included in this analysis.
It is physiologically possible that even hazardous use of alcohol, like moderate use, may well lead to cleaner arteries and therefore lower rates of coronary artery disease. If this is the case, an explanation for the increases in cardiovascular mortality reported for heavy drinkers in many studies may relate not directly to coronary artery disease, but to conditions such as cardiomyopathy or cardiac arrhythmias. However, the rates of accidents, suicide and other morbidity associated with hazardous alcohol use may well overcome any protective effects on coronary disease.
Reference: Le Strat Y, Gorwood P. Hazardous drinking is associated with a lower risk of coronary heart disease: Results from a national representative sample. Am J Addict 2011;20:257–263.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 039: The role that alcohol drinking may play in the risk of cancer 17 April 2011
A large group of distinguished scientists have published a very detailed and rather complex paper describing the association between alcohol consumption and cancer. It is based on data from the EPIC study in Europe, with a mean follow up of 8.8 years for more than 300,000 subjects. The authors describe an increase in risk of many cancers from alcohol intake, but do not give data permitting the detection of a threshold of intake for an adverse effect on cancer risk. The investigators conclude that “In western Europe, an important proportion of cases of cancer can be attributable to alcohol consumption, especially consumption higher than the recommended upper limits.”
Members of the Forum were concerned that the authors did not separate moderate consumption from heavy consumption for their main analyses, ignored the demonstrated benefits of moderate drinking on total mortality, and did not point out other environmental influences (such as smoking, diet, obesity, etc.) that often have much larger effects on the risk of many cancers than does alcohol consumption. The authors make statements such as alcohol has negative effects on total mortality that are not supported by the data presented in their paper, and are contradicted by most large-scale population-based studies. Overall, while this paper supports the well-known association between heavy drinking and an increased risk of upper aero-digestive and certain other cancers, it adds little information useful for the prevention of most types of cancer.
Reference: Schűtze M, Boeing H, Pischon T, et al, Alcohol attributable burden of incidence of cancer in eight European countries based on results from prospective cohort study. BMJ 2011; 342:d1584 doi: 10.1136/bmj.d1584 (Published 7 April 2011)
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 038: Effects of a large reduction in alcohol prices on mortality in Finland 7 April 2011
Time series intervention analysis modeling was applied to the monthly aggregations of deaths in Finland for the period 1996–2006 to assess the impact of a reduction in alcohol prices in 2004. The authors report that alcohol-related deaths increased in men aged 40–49 years, and in men and women aged 50–69 years: the mean rate of alcohol-related mortality increased by 17%, 14%, and 40%, respectively, which implies 2.5, 2.9 and 1.6 additional monthly deaths per 100,000 person-years following the price reduction. In contrast to alcohol-related mortality, CVD and all-cause mortality decreased among men and women in the highest age category. The changes were consistent with 19 and 25 fewer monthly deaths per 100,000 person-years for CVD and 42 and 69 fewer monthly deaths for all-cause mortality.
Forum members agreed that both potentially harmful and beneficial effects resulting from changes in alcohol intake should be considered when estimating population effects. They were unsure whether all of the reported effects in the elderly should be attributed to changes in alcohol intake, as decreases in CVD and all-cause mortality rates were occurring prior to the change in alcohol intake.
Reference: Herttua K, Mäkelä P, Martikainen P. An evaluation of the impact of a large reduction in alcohol prices on alcohol-related and all-cause mortality: time series analysis of a population-based natural experiment. Int J Epidemiol 2011;40:441-454; doi:10.1093/ije/dyp336.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 037: Genes found to relate to level of alcohol consumption among Asians 27 March 2011
In a study of 1,721 Korean male drinkers aged 40–69 y in an urban population–based cohort, and another sample of 1,113 male drinkers from an independent rural cohort, information on average daily alcohol consumption was collected and DNA samples were collected for genotyping. In a genome-wide association (GWA) study, 12 single-nucleotide polymorphisms (SNPs) on chromosome 12q24 had genome-wide significant associations with alcohol consumption. These polymorphisms were closely related to genes that determine levels of ALDH, low levels of which relate to flushing after even small amounts of alcohol. Such enzymes are much more common among Asians than among westerners. Further, associations were tested only with the weekly amount of alcohol consumed, not the pattern of drinking; hence, these findings are not direct measures of alcoholism.
The editorial by Freedman et al states “epidemiologic literature suggests that those who begin drinking at an early age may be at greater risk for a maladaptive and more genetically pronounced form of alcohol consumption, and other environmental milieus affect the risk of alcoholism.” It will be important to investigate the interplay of genes and environmental factors when seeking the determinants of alcohol abuse. Despite the findings of this study, our understanding of factors associated with alcoholism remains very limited.
Reference: Baik I, Cho NH, Kim SH, Han B-G, Shin C. Genome-wide association studies identify genetic loci related to alcohol consumption in Korean men. Am J Clin Nutr 2011;93:809–816.
Accompanying Editorial: Agrawal A, Freedman ND, Bierut LJ. Genome-wide association studies of alcohol intake—a promising cocktail? Am J Clin Nutr 2011;93:681–683.
For the full critique of this article by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 036: Alcohol consumption after age 75 associated with lower risk of developing dementia
7 March 2011
A population-based study of elderly Germans, aged 75 and older, evaluated the association between alcohol consumption and incident overall dementia and Alzheimer dementia over 3 years. There was good ascertainment of the development of dementia, even among subjects who died during follow up.
Of 3,202 subjects free of dementia at baseline, 217 subjects met criteria of dementia during follow up. Subjects consuming alcohol had approximately 30% less overall dementia and 40% less Alzheimer dementia than did non-drinking subjects. Unlike many previous studies showing greater effects of wine on reducing risk of dementia, no significant differences were seen according to the type of alcoholic beverage consumed. Overall, these results are similar to several previous studies in the very elderly and suggest that moderate drinking is associated with less dementia, even among individuals aged 75 years and older.
Reference: Weyerer S, Schaufele M, Wiese B, Maier W, Tebarth F, van den Bussche H, Pentzek M, Bickel H, Luppa M, Riedel-Heller SG, for the German AgeCoDe Study Group (German Study on Ageing, Cognition and Dementia in Primary Care Patients). Current alcohol consumption and its relationship to incident dementia: results from a 3-year follow-up study among primary care attenders aged 75 years and older. Age and Ageing 2011; 0: 1–7; doi: 10.1093/ageing/afr007.
For the full critique of this article by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 035: A review of the association of alcohol consumption with cardiovascular disease outcomes 5 March 2011
In an excellent summary, the authors of this paper have synthesized results from longitudinal cohort studies comparing alcohol drinkers with non-drinkers for the outcomes of overall mortality and mortality from cardiovascular disease (CVD), incident coronary heart disease (CHD), mortality from CHD, incident stroke, and mortality from stroke. They conclude that light to moderate alcohol consumption is associated with a reduced risk of multiple cardiovascular outcomes. Further, they suggest that current scientific data satisfy Hill criteria indicating causality, that alcohol intake is the cause of the lower risk of cardiovascular disease among moderate drinkers.
Forum members thought that this was a very well-done, comprehensive summary of a large number of studies on alcohol and cardiovascular disease. Some believed that two topics were not adequately discussed: (1) greater benefits from wine than from other beverages, a result seen in many studies, and (2) the importance of the pattern of drinking on the health effects of alcohol. However, Forum members welcomed the discussion in the paper as to causality and regarding future directions in research, with more emphasis into how physicians and individual patients might respond to encouragement to consume alcohol for its potentially beneficial effects on cardiovascular disease. Most believe that there is no substitute for balanced judgment by a knowledgeable, objective health professional when discussing alcohol intake, and this requires is a synthesis of common sense and the best available scientific facts as they apply to the individual.
Reference: Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 2011;342:d671; doi:10.1136/bmj.d671
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 034: A review of interventional studies in humans showing effects of alcohol on risk factors for cardiovascular disease 5 March 2011
A summary paper on the effects of alcohol consumption on biologic mechanisms associated with coronary heart disease provides an excellent review of a large number of intervention studies in humans. Appropriate analyses were done and the results are presented in a very clear fashion, although there was little discussion of the separate, independent effects of alcohol and polyphenols on risk factors.
The trials the authors reviewed have demonstrated that the moderate intake of alcoholic beverages leads to increases in HDL-cholesterol, apolipoprotein A1, and adiponectin and decreases in fibrinogen, all factors associated with a lower risk of heart disease. The findings described in this paper strengthen the case for a causal link between alcohol intake and a reduced risk of coronary heart disease, suggesting that the lower risk of heart disease observed among moderate drinkers is caused by the alcoholic beverage itself, and not by other associated lifestyle factors.
Reference: Brien SE, Ronksley PE,Turner BJ, Mukamal KJ, Ghali WA. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ 2011;342:d636; doi:10.1136/bmj.d636.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 033: Moderate-to-heavy alcohol intake may increase risk of atrial fibrillation 12 February 2011
A number of well-done studies have shown an increase in the risk of atrial fibrillation to be associated with heavy alcohol intake or with alcoholism. Most previous studies suggest little if any increase in risk from light-to-moderate drinking. The present study was a meta-analysis based on 14 studies from Europe or North America. It showed an increase in risk with alcohol, but there were limited dose-response data to determine if there was a threshold above which the risk was increased.
Overall, the scientific evidence from many studies suggests that at least heavy drinking may increase the risk of atrial fibrillation, although whether light-to-moderate intake increases the risk seems unlikely. Previous basic scientific data of mechanisms of atrial fibrillation have suggested that alcohol has little effect on this arrhythmia.
Reference: Kodama S, Saito K, Tanaka S, Horikawa C, Saito A, Heianza Y, Anasako Y, Nishigaki Y, Yachi Y, Iida KT, Ohashi Y, Yamada N, Sone H. Alcohol consumption and risk of atrial fibrillation. A meta-analysis. J Am Coll Cardiol 2011;57:427–436.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 032: Comments on alcohol in newly released Dietary Guidelines for Americans, 2010 9 February 2011
The United States has released new Dietary Guidelines for Amercans, 2010. While the Key Recommendations regarding alcohol remain similar to those of earlier guidelines, there were some changes in the text that reflect increasing scientific data indicating potential health benefits of moderate drinking. The key recommendation is as follows:
“If alcohol is consumed, it should be consumed in moderation—up to one drink per day for women and two drinks per day for men—and only by adults of legal drinking age.”
Within the main body of the guidelines, comments on alcohol include the following:
“The consumption of alcohol can have beneficial or harmful effects, depending on the amount consumed, age, and other characteristics of the person consuming the alcohol. Alcohol consumption may have beneficial effects when consumed in moderation. Strong evidence from observational studies has shown that moderate alcohol consumption is associated with a lower risk of cardiovascular disease. Moderate alcohol consumption also is associated with reduced risk of all-cause mortality among middle-aged and older adults and may help to keep cognitive function intact with age. However, it is not recommended that anyone begin drinking or drink more frequently on the basis of potential health benefits because moderate alcohol intake also is associated with increased risk of breast cancer, violence, drowning, and injuries from falls and motor vehicle crashes.”
Reference: www.cnpp.usda.gov/Publications/DietaryGuidelines/2010/PolicyDoc/Chapter3.pdf
To see a copy of the section on alcohol from the new Dietary Guidelines, click here.
===============================================================================
Critique 031: Wine polyphenols have a variety of beneficial effects on health 30 January 2011
Much of the protection against cardiovascular disease attributed to wine intake may relate not only to the alcohol in wine, but to its polyphenolic constituents. This review article summarizes research into the chemistry, bioavailability, metabolism and excretion of polyphenols as well as mechanisms of their action. As stated by the authors, “These protective effects could be due to one or many components of the complex mixture of bioavailable and bioactive compounds present in red wine including ethanol, resveratrol, flavonols, flavan-3-ols, anthocyanins, phenolic acids as well as their metabolites formed either in the tissues or in the colon by the microflora.” The authors describe their cardioprotective effects, effects on vascular function and atherosclerosis, anti-platelet effects, effects on myocardial ischemia, and anti cancer and anti-diabetic effects.
The authors conclude that “Polyphenols are the most abundant antioxidants in the diet and are widespread constituents of wine, fruits and vegetables.” Their review provides an extensive scientific literature on polyphenols in wine; it suggests multiple mechanisms by which such substances may have beneficial effects on health.
Reference: Rodrigo R, Miranda A, Vergara L. Modulation of endogenous antioxidant system by wine polyphenols in human disease. Clin Chim Acta 2011;412:410-424
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research please click here.
===============================================================================
Critique 030: Young rats given red wine polyphenols show less deterioration in endothelial function with ageing. 30 January 2011
The gradual decrease in endothelial function over time is a key factor in the development of diseases associated with ageing, especially cardiovascular disease (CVD). Many epidemiologic studies suggest greater protection against CVD from wine than from other beverages containing alcohol, with at least one factor being the polyphenols in red wine (RWPs).
The present study in rats found that the administration of red wine polyphenols protected against ageing-induced endothelial dysfunction. As stated by the authors: “The present findings indicate that regular intake of RWPs in the drinking water starting at young age (16 week-old) prevented the aging-related endothelial dysfunction most likely by reducing the excessive oxidative stress in the arterial wall.” They further suggest an important role of NADPH oxidase and possibly also the angiotensin system in the abnormal vascular response in aging. Their study showed that, “RWPs intake had also a physiological beneficial effect since it improved the physical exercise capacity of old rats.”
Forum members thought that this was an excellent paper, as it begins to delve into mechanisms by which polyphenols improve health. A mechanism is addressed and results are consistent with the working hypothesis of a specific interaction between polyphenols and peculiar enzymes. There is a satisfying agreement between basic mechanisms and pathophysiology.
Some scientists believe that interventions to improve endothelial function (such as the consumption of red wine or other sources of polyphenols) should begin earlier in life to slow down the endothelial dysfunction that occurs with ageing. This study in rats tends to support such a belief.
Reference: Dal-Ros S, Zoll J, Lang AL, Auger C, Keller N, Bronner C, Geny B, Schini-Kerth VB. Chronic intake of red wine polyphenols by young rats prevents aging-induced endothelial dysfunction and decline in physical performance: Role of NADPH oxidase. Biochem Biophys Res Commun 2011;404:743-749
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 029: Differing opinions on the message to the public regarding alcohol consumption 16 January 2011
A Letter to the Editor entitled “What should we advise about alcohol consumption?” was recently published by Maurizio Ponz de Leon in Intern Emerg Med.1 Dr. de Leon argues that the message of health benefits of moderate drinking “seems to me hazardous and extremely dangerous to diffuse in the general population.” His reasons included (1) many people may be unable to distinguish between low–moderate and high consumption of wine, beer or spirits, and alcohol metabolism may differ remarkably from one subject to another; (2) alcohol remains a frequent cause of car crash, and governments (in almost all western countries) try to convince or force people to abstain from drinking before driving; and (3) to consider alcohol as a medication whose consumption may contribute to improved health is another source of concern. Dr. de Leon asks: “Are we truly at the point of prescribing alcohol consumption in order to reduce the risk of stroke and coronary damage?” He concluded that “more studies are needed before we can give sensible recommendations on alcohol consumption to the general population.”
The de Leon editorial has prompted considerable response from other scientists, including further Letters to the Editor of the journal by Di Castelnuovo, Costanzo, Donati, Iacoviello, and de Gaetano,2 and by Estruch and Lamuela-Raventos.3 In addition, the original editorial has stimulated considerable debate among members of the International Scientific Forum on Alcohol Research. Among key arguments presented by the Forum members, all experts in scientific research on alcohol, are that messages to the public should not be “paternalistic” (we will tell you what is best for you since you are not smart enough to understand the facts), and that guidelines must always be based on sound, balanced scientific data rather than on uninformed opinion. Forum members emphasized that there are certain people who should not drink at all (including former abusers of drugs or alcohol, people with certain medical conditions, children and adolescents, and people with religious or moral proscriptions against alcohol), and there can never be a general recommendation for everybody to consume alcohol. On the other hand, physicians should not withhold from their patients and the public scientifically sound and balanced data on alcohol and health. And the data are extremely strong supporting a role for moderate alcohol intake, for appropriate adults, for the reduction in risk of coronary artery disease and other diseases of ageing.
Several Forum members pointed out that it was unfortunate that the journal had chosen to publish the original letter that castigates alcohol from an author with good scientific credentials, but little to no apparent research expertise in the subject of alcohol and health. Many Forum members disagreed with the statement of de Leon that “Many people may be unable to distinguish between low–moderate and high consumption of wine, beer or spirits.” A leading scientist dealing with this subject for decades, Dr. Arthur Klatsky, has written: “Most people know very well what the difference is between light to moderate drinking and binge or excessive drinking. While some patients may rationalize their heavy drinking because of its purported health effects, I have yet to find someone who had developed alcohol abuse because of messages about the health effects of moderate drinking.” Medical practitioners, in his view, “have a ‘solemn duty’ to tell the truth about alcohol consumption, as they understand it, to all of their patients.” While pointing out that certain individuals will not benefit from the consumption of alcohol, several Forum members believed that it would be unethical for physicians to withhold from middle-aged or elderly subjects at risk of cardiovascular disease information on the potential benefits of light-to-moderate drinking
References:
- Maurizio Ponz de Leon. What should we advise about alcohol consumption? Intern Emerg Med, DOI 10.1007/s11739-010-0487-1.
- Augusto Di Castelnuovo, Simona Costanzo, Maria Benedetta Donati, Licia Iacoviello, Giovanni de Gaetano. What should we advise about alcohol consumption? Reply letter by A. Di Castelnuovo. Intern Emerg Med, DOI 10.1007/s11739-010-0502-6.
- Ramon Estruch • Rosa Ma Lamuela-Raventos. What should we advise about alcohol consumption: reply letter by R. Estruch. Intern Emerg Med; DOI 10.1007/s11739-010-0503-5.
For the full critique of these publications by members of the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 028: Changes over time in relation of social class to mortality from cirrhosis 9 January 2011
To explore the nature of the social class gradient of cirrhosis mortality in England and Wales across the 20th century, data on male cirrhosis mortality by social class were obtained from the Registrar General’s Decennial Supplements for the years 1921–1991. This paper describes a dramatic change during the 20th century in the association between social class and mortality from liver cirrhosis. While deaths from cirrhosis were more common among higher social classes in the early part of the century, the pattern changed so that deaths from cirrhosis were much more common among the lower social classes by the end of the century.
Suggested reasons for the lower current rates among subjects at higher social class include different patterns of alcohol consumption, with regular moderate consumption (especially of wine with meals) becoming more common with higher social class subjects while binge drinking (especially of beer and spirits) remaining more common in lower social classes. However, a number of other factors may relate to the class differences in rates of hepatic cirrhosis, including a less healthy diet and greater rates of obesity (associated with hepatic fatty liver and cirrhosis) among lower social class subjects and social class differences in hepatitis rates. Further, certain medications, coffee consumption, and many other lifestyle factors are associated with hepatic cirrhosis. The actual reasons for the changes over time reported in this paper remain unclear.
Reference: Crombie IK, Precious E. Changes in the social class gradient of cirrhosis mortality in England and Wales across the 20th century. Alcohol and Alcoholism 2011;46:80–82.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 027: Effects of resveratrol and quercetin on inflammation and insulin resistance – 20 December 2010
A study was carried out to examine the extent to which quercetin and trans-resveratrol (RSV) prevented inflammation or insulin resistance in primary cultures of human adipocytes treated with tumor necrosis factor-a (TNF-a)—an inflammatory cytokine elevated in the plasma and adipose tissue of obese, diabetic individuals. Cultures of human adipocytes were pretreated with quercetin and trans-RSV followed by treatment with TNF-a. Subsequently, gene and protein markers of inflammation and insulin resistance were measured. The authors report that quercetin, and to a lesser extent trans-RSV, attenuated the TNF-a–induced expression of inflammatory genes such as interleukin (IL)-6, IL-1b, IL-8, and monocyte chemoattractant protein-1 (MCP-1) and the secretion of IL-6, IL-8, and MCP-1.
Forum members were concerned about certain aspects of the study, especially the extrapolation of in vitro results to in vivo situations. The in vitro conditions the authors describe are minimally representative of an in vivo condition. In vivo, after consumption of quercetin or resveratrol, these compounds undergo extensive metabolism, leading to glucuronidated, sulphated or methylated compounds. In a previous study, quercetin 3-glucoside was transformed to 3,4-dihydroxyphenylacetic acid, acetate and butyrate in cells from human gut; only 3′-methylquercetin has been detected in human plasma, present at a concentration of 0.1 to 0.2 µM after 3 h. The authors of the current paper are using concentrations up to 60 µM, concentrations which have not been found in vivo.
There were also concerns with the work on cell uptake of quercetin and resveratrol. Primary adipocytes were incubated with the polyphenols, but it is not clear whether or not the concentrations used were subtoxic. Our current knowledge is limited about local concentration of the molecules we are studying in subcellular compartments, their interaction with alternative targets, and eventually their transformation into products that could be more or less active on a given specific pathway. The real difficult and important issue is the identification of a reasonable convergence — if not agreement — between data originating from extremely distant approaches. In this case, the notion that metabolic diseases are related to a homeostatic imbalance in adipose tissue, linked to a different redox status, linked to activation of specific pathways, and that different redox sensitive polyphenols do have a protective effect, encompasses the evidence produced by extremely distant approaches.
From a clinical point of view, the role of phytochemicals acting as antioxidants and anti-inflammatory agents could be extremely important in inflammation-associated chronic conditions such as cardiovascular disease, diabetes, and cancer. Quercetin and resveratrol may indeed play an important role in this regard, and need to be investigated further to establish the clinical importance of natural dietary compounds in the prevention of chronic degenerative conditions.
Reference: Chuang C-C, Martinez K, Xie G, Kennedy A, Bumrungpert A, Overman A, Jia W, McIntosh MK. Quercetin is equally or more effective than resveratrol in attenuating tumor necrosis factor-a–mediated inflammation and insulin resistance in primary human adipocytes. Am J Clin Nutr 2010;92:1511–1521.
For the full critique of this paper by the International Scientific Forum on Alcohol Research please click here.
===============================================================================
Critique 026: Chinese study suggests that alcohol increases angiographically significant coronary artery disease 8 December 2010
Among a large number of Chinese men presenting with chest pain or EKG changes, sequential subjects undergoing cardiac angiography were evaluated for obstructive coronary artery disease (CAD) lesions according to their reported recent alcohol intake. The study population consisted of 1,476 consecutive men 36 to 84 years of age; participants were categorized as nondrinkers, light drinkers, moderate drinkers, or heavy drinkers.
Adjusted odds ratios for angiographically proved CAD for light, moderate, and heavy drinking were 1.16 (95% confidence interval 0.68 to 1.94), 1.78 (1.35 to 2.27), and 2.18 (1.46 to 3.25). Compared to non-drinking, adjusted odds ratios were 1.03 (0.54 to 1.87) for drinking 0 to 15 years, 1.61 (1.28 to 2.14) for 16 to 30 years, and 1.98 (1.23 to 3.05) for >30 years. The authors concluded that moderate-to-heavy alcohol consumption increased the risk of CAD in Chinese men. CAD risk tended to increase with an increase in frequency and duration of drinking.
This was a very select group of patients (those presenting with chest pain or EKG changes), and not typical of the Chinese population. No information was available on drinking patterns or on previous alcohol intake. Further, a recent large population-based study from mainland China showed that consumers of alcohol were less likely to develop coronary disease, results similar to those in most Western populations. It is not possible from the present study to say that the association of alcohol intake with CAD is different between Chinese and Western populations, as the present study gives results only for a very select group of patients.
The most important outcome regarding CAD is the occurrence of clinical events (myocardial infarction, cardiac death, etc.). The detection of such events requires long-term follow-up studies to be able to judge the overall effects of alcohol drinking on CAD.
Reference: Zhou X, Li C, Xu W, Hong X, Chen J. Relation of alcohol consumption to angiographically proved coronary artery disease in Chinese men. Am J Cardiol 2010;106:1101–1103.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 025: Pattern of drinking and type of beverage affect the relation of alcohol intake to coronary heart disease 1 December 2010
Using cohort data from Belfast and France, investigators related weekly alcohol consumption, incidence of binge drinking (alcohol >50 g on at least one day a week), incidence of regular drinking (at least one day a week, and alcohol <50 g if on only one occasion), volume of alcohol intake, frequency of consumption, and types of beverage consumed to risk of coronary heart disease (CHD) events over a 10 year follow-up period. Overall, 60.5% of subjects from N. Ireland and 90.6% of French reported drinking alcohol at least once a week. Among drinkers, 12% of men in Belfast drank alcohol every day compared with 75% of men in France. Mean alcohol consumption was 22.1 g/ day in Belfast and 32.8 g/day in France. Binge drinkers comprised 9.4% and 0.5% of the Belfast and France samples, respectively.
Results showed that, after multivariate adjustment, the hazard ratio for hard coronary events compared with regular drinkers was 1.97 (95% CI 1.21 – 3.22) for binge drinkers, 2.03 (95% CI 1.41 – 2.94) for never drinkers, and 1.57 (95% CI 1.11 – 2.21) for former drinkers. The hazard ratio for hard coronary events in Belfast compared with in France was 1.76 (95% CI 1.37 to 2.67) before adjustment, and 1.09 (95% CI 0.79 to 1.50) after adjustment for alcohol patterns and wine drinking. Only wine drinking was associated with a lower risk of hard coronary events, irrespective of the country.
The authors conclude that regular and moderate alcohol intake throughout the week, the typical pattern in middle-aged men in France, is associated with a low risk of ischemic heart disease, whereas the binge drinking pattern more prevalent in Belfast confers a higher risk.
While a strong inverse association between moderate alcohol consumption and cardiovascular disease has been demonstrated for decades, more recent research has emphasized the importance of the pattern of drinking (regular moderate versus episodic or binge drinking). Further, there continues to be debate about the potential greater effect of wine versus other beverages containing alcohol. This study shows that regular moderate drinking (especially of wine) is associated with lower risk of MI, but episodic or binge drinking (especially of beer or whiskey) increases the risk. Lifetime abstinence has a similar adverse relation to CHD as does episodic or binge drinking.
Reference: Ruidavets J-B, Ducimetièere P, Evans A, Montaye M, Haas B, Bingham A, Yarnell J, Amouyel P, Arveiler D, Kee F, Bongard V, Ferrières J. Patterns of alcohol consumption and ischaemic heart disease in culturally divergent countries: the Prospective Epidemiological Study of Myocardial Infarction (PRIME). BMJ 2010;341:c6077 doi:10.1136/bmj.c6077.
For the detailed critique of this study by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 024: Moderate alcohol consumption lowers risk of metabolic diseases in a population with high mean alcohol intake. 28 November 2010
A cross-sectional analysis of data from subjects in Switzerland related varying levels of alcohol intake to the presence of diabetes mellitus, the “metabolic syndrome,” and an index of insulin resistance (HOMA-IR). The strengths of this paper include being population-based and having a large number of subjects who reported that they consumed 14 or more drinks/week. Also, there was a good percentage (27%) of subjects reporting no alcohol intake during the one week of assessment used for classifying subjects. Another strength is the careful confirmation of drinking status with state-of-the-art laboratory tests. In multivariate analysis, the prevalence of the metabolic syndrome, diabetes and mean HOMA-IR decreased with low-risk drinking and increased with high-risk drinking. No differences were noted according to the type of beverage consumed.
This is a cross-sectional analysis, so a causative relation between alcohol intake and the metabolic outcomes cannot be assessed. Still, the data support much that has been shown in prospective studies. Several Forum members commented on potential problems when considering a number of physiologic conditions as the “metabolic syndrome” and focusing therapy on the syndrome; they believed that each metabolic factor should be evaluated and treated singly.
Reference: Clerc O, Nanchen D, Cornuz J, Marques-Vidal P, Gmel G, Daeppen J-B, Paccaud F, Mooser V, Waeber G, Vollenweider P, Rodondi N. Alcohol drinking, the metabolic syndrome and diabetes in a population with high mean alcohol consumption. Diabet Med 2010;27:1241–1249.
For the detailed critique of this study by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 023: Evidence that PPAR-gamma is a mechanism for the effects of wine polyphenolics on cardiovascular risk. 27 November 2010
It is important that biological mechanisms are identified for the observed inverse relation between the moderate consumption of wine and cardiovascular disease shown in most epidemiologic studies. A paper by Zoechling et al is an elegant example of the needed effort to provide a biochemical mechanism for the biological effects of wine. Data on binding of different wine component were produced and this result is interpreted in light of epidemiological evidence.
It would have been appropriate to provide evidence also for the actual shift of gene expression primed by the same wine component in a cell or animal model. In this respect, results must be rated appropriate but still as preliminary; a ligand could have different effects. Further, biological evidence is not provided to support the contention that these polyphenols act through the PPAR-gamma receptor. The sort of evidence that should have been provided is a comparison with rosiglitazone in a cell population known to respond to PPAR-gamma agonists (e.g. adipocytes).
Further, the analytical data does not describe the amounts of any of the “active” substances. So while there is a lot of discussion of the active components, it is not possible to compare any wine’s “activity” with the amount of the key substances. Lacking such a comparison, it is very hard to conclude that these substances are in fact the responsible factors in the observed activity.
Nevertheless, this paper provides important data on potential mechanisms by which the constituents of wine and certain other beverages may act to reduce the risk of cardiovascular disease.
Reference: Zoechling A, Liebner F, Jungbauer A. Red wine: A source of potent ligands for peroxisome proliferator-activated receptor γ. Food & Function, Journal of the Royal Society of Chemistry, in press. DOI: 10.1039/c0fo00086h.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 022: Alcohol consumption decreases with the development of disease — 21 November 2010
In a cross-sectional study from the 2004 and 2007 Australian National Drug Strategy Household (NDSH) surveys, respondents were questioned about their current and past drinking, the presence of formal diagnosis for specific diseases (heart disease, type 2 diabetes, hypertension, cancer, anxiety, depression) and self-perceived general health status. The sample sizes for the 2004 and 2007 NDSH surveys were 24,109 and 23,356, respectively.
The authors report that respondents with a diagnosis of diabetes, hypertension, or anxiety were more likely to have reduced or stopped alcohol consumption in the past 12 months. The likelihood of having reduced or ceased alcohol consumption in the past 12 months increased as perceived general health status declined from excellent to poor (although the authors do not point out that lifetime abstainers were more likely than moderate drinkers to report less than excellent health status).
The authors conclude that the experience of ill health is associated with subsequent reduction or cessation of alcohol consumption (“sick quitters), which is consistent with most prospective epidemiologic studies. The authors also conclude that this may at least partly underlie the observed ‘J-shaped’ function relating alcohol consumption to premature mortality. On the other hand, most modern epidemiologic studies are careful not to include “sick quitters” within the non-drinking category, and relate health effects of drinkers with those of lifetime abstainers. Further, prospective studies in which alcohol intake is assessed at different times (rather than having “changes” based only on recall at one point in time, as was done in this study) usually indicate that subjects who decrease their intake are more likely to subsequently develop adverse health outcomes, especially related to cardiovascular disease, than those who continue moderate drinking.
Reference: Liang W, Chikritzhs T. Reduction in alcohol consumption and health status. Addiction 2010; in press (doi:10.1111/j.1360-0443.2010.03164.x).
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 021: Alcohol consumption affects risk of cataracts 25 October 2010
A population-based prospective study from Australia utilized repeated lens photographs over a period of 5 to 10 years to diagnose cataracts among more than 2,500 subjects. The investigators related the risk of their development, and the risk of cataract surgery, to the reported alcohol intake of subjects. Previous research has provided some biological mechanisms that make an association between alcohol and cataracts plausible.
Overall, the present study showed few statistically significant relations between alcohol and cataracts, although adjusted results suggested a “U-shaped” association between total alcohol intake and development of cataracts (a lower risk for moderate drinkers, higher risk for both abstainers and heavier drinkers). The U-shaped association with alcohol consumption was stronger for the risk of cataract surgery. These results are consistent with previous cohort studies. On inspection of the data presented, the potential reduction in risk of cataract was primarily for wine and beer. While some types of cataract may be reduced by moderate drinking, larger intake of alcohol may be associated with increased risk.
Reference: Kanthan GL, Mitchell P, Burlutsky G, Wang JJ. Alcohol Consumption and the Long-Term Incidence of Cataract and Cataract Surgery: The Blue Mountains Study. Am J Ophthalmol 2010;150:434–440.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 20: New data on effects of alcohol during pregnancy 12 October 2010
A very large population-based observational study from the UK found that at the age of 5 years, the children of women who reported light (no more than 1-2 units of alcohol per week or per occasion) drinking did not show any evidence of impairment on testing for behavioral and emotional problems or cognitive ability. There was a tendency for the male children of women reporting “heavy/binge” drinking during pregnancy (7 or more units per week or 6 or more units per occasion) to have poorer behavioral scores, but the effects were less clear among female offspring.
Scientific data continue to indicate that higher intake of alcohol during pregnancy may adversely affect the fetus, and could lead to very severe developmental or other problems in the child. However, most recent publications (as does this one) show little or no effects of occasional or light drinking by the mother during pregnancy. They also demonstrate how socio-economic, education, and other lifestyle factors of the mother may have large effects on the health of the fetus and child; these must be considered when evaluating the potential effects of alcohol during pregnancy.
Overall, current scientific data indicate that while drinking during pregnancy should not be encouraged, there is little evidence to suggest that an occasional drink or light drinking by the mother is associated with harm. Heavy drinking, however, may be associated with serious developmental defects in the fetus.
Reference: Kelly YJ, Sacker A, Gray R, Kelly J, Wolke D, Head J, Quigley MA. Light drinking during pregnancy: still no increased risk for socioemotional difficulties or cognitive deficits at 5 years of age? J Epidemiol Community Health 2010; doi:10.1136/jech.2009.103002
Addendum: After the above critique was prepared, a new paper has been published on the topic by O’Leary et al (O’Leary CM, Nassar N, Kurinczuk JJ, de Klerk N, Geelhoed E, Elliott EJ, Bower C. Prenatal Alcohol Exposure and Risk of Birth Defects Pediatrics 2010;126;e843-e850; DOI: 10.1542/peds.2010-0256). Overall, the results of that study are similar to those of the study by Kelly et al, with no increase in risk of birth defects in children born of women reporting low or moderate drinking during pregnancy but with an increased risk of defects among children of women reporting heavy drinking.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 019: Both alcohol and caffeinated coffee intake are associated with lower risk of diabetes in African-American women. 27 September 2010
In a very large cohort of African-American women in the US, the association between the consumption of alcohol, tea, and coffee was related to the development of type 2 diabetes mellitus over a follow-up period averaging 12 years. Tea and decaffeinated coffee showed no relation with diabetes, but the intake of both caffeinated coffee and alcohol showed a significant inverse association.
This paper is particularly important because some previous studies have not shown a strong association between alcohol and the risk of cardiovascular disease among African-Americans. African-Americans, especially women, tend to drink little alcohol, yet are at markedly increased risk of diabetes. In the present study, the approximately 30% lower risk for moderate alcohol drinkers was about the same in these African-American women as has been found in many previous studies of whites.
Reference
Boggs DA, Rosenberg L, Ruiz-Narvaez EA, Palmer JR. Coffee, tea, and alcohol intake in relation to risk of type 2 diabetes in African American women. Am J Clin Nutr 2010;92:960–966.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 018: Alcohol consumption following diagnosis of early-stage breast cancer may increase risk of recurrence of cancer but not total mortality risk 14 September 2010
In the Life After Cancer Epidemiology (LACE) study, 1,897 participants diagnosed with early-stage breast cancer between 1997 and 2000 and recruited on average 2 years post-breast cancer diagnosis were evaluated for the association between alcohol intake and breast cancer recurrence and death. The women, who were generally light drinkers, were followed for an average of 7.4 years. The study reported an increase in risk of breast cancer recurrence and breast cancer death, but no effect on total mortality, to be associated with consumption of 3 to 4 or more drinks per week when compared with women not drinking following their cancer diagnosis.
Previous research has been mixed on this topic. Almost all large studies have shown no increase in all-cause mortality for women who drink moderately following a diagnosis of breast cancer (as does this study). As for recurrence of breast cancer, most have shown no increase in risk, although one previous study of women with estrogen-receptor + tumors found an increased risk of a primary cancer developing in the contralateral breast to be associated with alcohol intake of more than 7 drinks per week.
Because of conflicting results among studies on this topic, further research will be needed to determine the extent to which alcohol following a diagnosis of breast cancer may relate to subsequent disease and death.
Reference: Kwan ML, Kushi LH, Weltzien E, Tam EK, Castillo A, Sweeney C, Caan BJ. Alcohol Consumption and Breast Cancer Recurrence and Survival Among Women With Early-Stage Breast Cancer:The Life After Cancer Epidemiology Study. J Clin Oncol 2010;28 (published ahead of print, 10.1200/JCO.2010.29.2730)
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 017: Moderate alcohol intake is associated with a lower risk of total mortality than are either abstinence or heavy drinking 5 September 2010
In a study based on data from 1,824 predominantly Caucasian Americans from the Western part of the United States, alcohol consumption at baseline was related to mortality risk during a 20-year follow-up period. Subjects were recruited into a longitudinal project that has examined late-life patterns of alcohol consumption and drinking problems. Lifetime abstainers were not included in the study, which focused on stress and coping processes among problem drinkers and non-problem drinkers. The sample at baseline included only subjects aged 55 to 65 years who had had outpatient contact with a health care facility in the previous 3 years.
The database at baseline included information on daily alcohol consumption, sociodemographic factors, former problem drinking status, health factors, and social-behavioral factors. Subjects who were not lifetime abstainers but did not report drinking at the time of the baseline examination were classified as “abstainers.” Data on potential changes in alcohol consumption during the course of the study were not collected. Death during follow up was confirmed primarily by death certificate.
The key results of the paper are that even when adjusting for sociodemographic factors, former problem drinking status, health factors, and social-behavioral factors, moderate drinking was associated with considerably lower risk of all-cause mortality. In comparison with “moderate drinkers” (subjects reporting up to 3 drinks/day), abstainers had 51 % higher mortality risk and heavy drinkers had 45% higher risk. The study supports most previous scientific studies showing that moderate drinking, in comparison with both abstinence and heavy drinking, is associated with lower risk of total mortality.
Reference: Holahan CJ, Schutte KK, Brennan PL, Holahan CK, Moos BS, Moos RH. Late-Life Alcohol Consumption and 20-Year Mortality. Alcoholism: Clinical and Experimental Research 2010;34:in press, November 2010
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 016: Association of alcohol with breast cancer risk varies according to subtype of tumor
29 August 2010
Most studies show a slight increase in the risk of breast cancer for women who consume alcohol. The association is thought to relate to alcohol’s effects on hormones, and alcohol use tends to be more strongly associated with hormonally sensitive breast cancers than tumors not sensitive to hormones. Few studies have evaluated how alcohol-related risk varies by breast cancer subtype. In the present study, follow-up data from 87,724 women in the Women’s Health Initiative Observational Study prospective cohort were evaluated for the relation of baseline alcohol consumption with subsequent breast cancer.
A total of 2,944 invasive breast cancer patients were diagnosed during follow up. In multivariable-adjusted analyses alcohol consumption was associated with an increase in the risk of lobular carcinoma (which makes up approximately 15-20% of breast cancers), but there was not a statistically significant association with the more-common ductal type of carcinoma. Hormone + cancers showed an association with alcohol intake, but not hormone – cancers. The findings support the importance of hormonal mechanisms in mediating the relation between alcohol use and breast cancer risk.
Reference Li CI, Chlebowski RT, Freiberg M, Johnson KC, Kuller L, Lane D, Lessin L, O’Sullivan MJ, Wactawski-Wende J, Yasmeen S, Prentice R. Alcohol consumption and risk of postmenopausal breast cancer by subtype: the Women’s Health Initiative Observational Study. J Natl Cancer Inst 2010 Aug 23. [Epub ahead of print]
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here : Critique 016.
===============================================================================
Critique 015: Moderate drinking does not appear to increase risk of breast cancer among women with a BRCA gene mutation 22 August 2010
A large study was carried out to assess the effects of alcohol consumption on breast cancer risk among women with a BRCA1 or a BRCA2 gene mutation, both of which markedly increase the risk of breast cancer. Comparisons were made between women with a gene mutation who had developed invasive breast cancer matched with women with the same gene mutation who had not developed breast cancer. After a number of appropriate exclusions, there were 1,480 matched pairs with BRCA1 mutations and 445 pairs with BRCA2 mutations.
Data from the study support an earlier report suggesting no increase in breast cancer risk from alcohol intake for women with either gene mutation. In the previous study on this topic, a slight lowering of breast cancer risk was noted with light drinking among women with the BRCA2 mutation but not among those with the BRCA1 mutation. In the present study, a possible reduction in risk of breast cancer was seen for moderately drinking women with the BRCA1 mutation, but not the BRCA2 mutation. Further, in the present study, the reduction is risk of breast cancer was seen only for wine consumers. While one should not over-interpret epidemiologic data in the absence of identified biologic mechanisms, there have been a very large number of experimental studies showing that certain polyphenols present in wine actively impede the initiation and growth of cancer cells.
Overall, current scientific data suggest that alcohol in moderation does not increase the risk of breast cancer among women with a BRCA mutation, and wine may be somewhat protective. If this is indeed the case and given the high risk associated with these genetic mutations, it would be important to inform women with such a mutation that moderate alcohol does not appear to increase their risk of breast cancer.
Reference: Dennis J, Ghadirian P, Little J, et al: The Hereditary Breast Cancer Clinical Study Group. Alcohol consumption and the risk of breast cancer among BRCA1 and BRCA2 mutation carriers. The Breast 2010; e-pub.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here.
=========================================================================
Critique 014: Moderate drinking, especially of wine, is associated with better cognitive function 13 August 2010
A large prospective study of men and women in northern Norway reported that moderate wine consumption was independently associated with better performance on cognitive tests after 7 years of follow up. There was no consistent association between consumption of beer or spirits and cognitive test results. The authors also reported that abstinence was associated with significantly lower cognitive performance in women. As noted by the authors, in any observational study there is the possibility of residual confounding by other lifestyle habits affecting cognitive function, and the present study was not able to adjust for certain ones (e.g., diet, income, or profession) but did adjust for age, education, body mass index, depression, and cardiovascular disease and its major risk factors.
The results of this study support findings from a number of observational, prospective studies that have shown that the moderate consumption of alcohol, especially of wine, may have favorable effects on cognitive function. Such effects could relate to the presence in wine of a number of polyphenols and other substances that reduce the risk of cognitive decline with ageing. Mechanisms that have been suggested for such protection against cognitive dysfunction include effects on atherosclerosis, coagulation, inflammation, as well as direct neuroprotective effects.
Reference: Arntzen KA, Schirmer H, Wilsgaard T, Mathiesen EB. Moderate wine consumption is associated with better cognitive test results: a 7 year follow up of 5033 subjects in the Tromsø Study. Acta Neurol Scandd 2010; Suppl 190:23-29.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 013: Greater than moderate alcohol intake increases the risk of liver cirrhosis 27 July 2010
A new meta-analysis shows that alcohol consumption is a strong factor in the development of cirrhosis of the liver. The study also supports the theory that there is a threshold of drinking above which the risk is increased, as some of their analyses suggest that the risk increases only with intake of more than 24 grams/day of alcohol for women (about 2 typical drinks by US standards) and 36 grams/day of alcohol for men (about 3 typical US drinks).
Despite some concerns about the approach used, our Forum agrees that the present meta-analysis supports previous studies indicating a strong role of heavy alcohol drinking in the development of cirrhosis. The differences found by the investigators between the effects of moderate alcohol intake on cirrhosis morbidity and on cirrhosis mortality are difficult to explain, but may relate to misclassification of alcohol intake (heavy drinkers reporting less alcohol), always a problem in observational studies of the effects of alcohol.
The results related to morbidity suggest that small amounts of alcohol are not associated with an increased risk of cirrhosis, and may be associated with lower risk of disease. Thus, the data provide evidence for a “threshold effect” of alcohol intake for the development of cirrhosis. Limited previous data are available suggesting that wine consumption may be associated with lower risk of cirrhosis than the intake of other beverages, but essentially all studies show heavy drinking of any type of beverage increases the risk.
Reference: Rehm J, Taylor B, Patra SM, Irving H, Baliunas D, Patra J, Roerecke M. Alcohol as a risk factor for liver cirrhosis: A systematic review and meta-analysis. Drug and Alcohol Review 2010,29,437–445. DOI: 10.1111/j.1465-3362.2009.00153.x
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 012: Moderate drinking in the elderly is associated with lower total mortality 23 July 2010
The effects of alcohol consumption in the elderly may be modified by a decreased ability to metabolize alcohol, an altered volume of distribution due to reduced lean body mass and total body water, and an increased prevalence of co-morbid conditions. These factors make this study of the net effects of drinking among a large number of community-dwelling elderly men and women especially important.
In large prospective studies from Australia of men aged 60-79 and women aged 70-75 years of age, men consuming up to 4 drinks/day and women up to 2 drinks/day had considerably lower risk of dying (total mortality) than did non-drinkers. For subjects reporting 1-2 drinks/day, their total mortality risk was about 20-30% lower than that of abstainers.
While the authors concluded that not consuming alcohol on 1 or 2 days per week was associated with better outcomes, this conclusion is not in accordance with their own data. The benefit of one or two “alcohol-free” days per week has never been substantiated with solid evidence from any large epidemiological study.
Our Forum review concludes that in terms of total mortality risk, recommendations for very low levels of drinking among the elderly may be overly restrictive, as this study showed lower total mortality for up to 4 drinks/day for elderly men and 2 drinks/day for elderly women. Further, this study does not provide support for the conclusion that mortality is lower for people who have 1 or 2 “alcohol-free” days per week.
Reference: McCaul KA, Almeida OP, Hankey GJ, Jamrozik K, Byles JE, Flicker L. Alcohol use and mortality in older men and women. Addiction 2010. On-line prior to publication: doi:10.1111/j.1360-0443.2010.02972.x
For the full critique of this paper by the International Scientific Forum on Alcohol Research, click here
===============================================================================
Critique 011: A Review of the Proposed New US Dietary Guidelines 14 July 2010
Members of our International Scientific Forum on Alcohol Research have submitted a detailed review of the draft recently circulated by the United States Department of Agriculture for proposed new US Dietary Guidelines for 2010. In general, Forum members were very pleased with the alcohol recommendations in the proposal, finding them interesting, balanced, and accurate. Many commented that, rather than just focusing on warnings against heavy drinking, the new Guidelines appear to take into account the large amount of recent epidemiologic and experimental data that support many potential beneficial health effects of moderate drinking.
Among specific recommendations from the Forum were the following:
■ A stronger statement is needed of the effects of light-to-moderate drinking on total mortality, in that recent prospective studies show a considerably lower of risk of death for moderate drinkers.
■ Additional emphasis is needed on the reduced risk of developing diabetes for moderate drinkers, and the much lower risk of cardiovascular disease among diabetics who consume some alcohol.
■ Further information should be presented on the consistent scientific data showing that women who drink moderately are at reduced, not increased, risk of weight gain in adult life.
There were a number of topics not discussed in the draft Guidelines that members of the Forum thought deserved consideration for inclusion.
■ Recent reports have consistently shown that among people who have already had a myocardial infarction or other cardiovascular event, moderate drinking is associated with a reduced risk of further cardiovascular events and death.
■ More emphasis in the Guidelines should be put on the pattern of drinking (regular moderate rather than occasional binge drinking) and also on the much lower blood alcohol levels after drinking when the beverage is consumed with food, rather than on an empty stomach.
■ It was also suggested to the Guidelines Committee that the beneficial effects on cardiovascular risk of polyphenols and other substances in wine and certain beers, in addition to alcohol, be discussed more adequately.
There were also some suggestions from ISFAR regarding future research needs in the field.
■ The Forum strongly supports the need for further research on the risks and benefits of light-to-moderate alcohol consumption, rather than focusing research only on alcohol abuse.
■ The Forum proposed emphasis on future research dealing with targeting recommendations for groups of people according to age, gender, other behaviors, etc., although there was some disagreement among Forum members as to whether or not moderate drinking has strong health effects in the young and not just in middle-aged and older adults.
■ ISFAR considers moderate drinking, unless contraindicated by certain conditions (e.g, former abuse, some types of severe liver disease), to be an important aspect of a healthy lifestyle. It should be a complement, not an alternative, to other lifestyle factors such as not smoking, getting exercise, eating a healthy diet, and avoiding obesity.
The draft of the proposed new Dietary Guidelines is available at http://www.cnpp.usda.gov/DGAs2010-DGACReport.htm.
For the full ISFAR critique of the proposed new Guidelines, click here
===============================================================================
Summary Critique 010 30 June 2010
Should moderate alcohol consumption be advised following a heart attack?
There has been considerable recent interest in the effects of alcohol consumption following an acute myocardial infarction (AMI). In an observational study among 325 subjects who were moderate drinkers prior to an AMI, 84% continued to drink and 16% quit. While most of the outcome measures showed no statistically significant effects between the two groups of patients, all outcomes showed a tendency towards better physical and mental health outcomes for persistent drinkers in comparison with those who quit drinking.
A key problem with this analysis, and with all observational epidemiologic studies on this topic, is that the reason that some subjects stopped drinking after having an AMI, while others continued to drink, is not known. Even though adjustments were made for many known related factors, there is always the possibility that subjects who stopped drinking were “sicker” in many ways than those who persisted in their alcohol consumption.
It may well require a randomized trial, in which some subjects having an AMI are randomly advised to continue to drink and others advised to stop drinking, to be able to determine reliably the effects on the clinical course of the persistence of alcohol intake following an AMI.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: Critique 010
===============================================================================
Summary: Critique 009 25 June 2010
Should moderate alcohol consumption be advised for its health effects?
A report from a conference that took place at the Medicine Grand Rounds at Beth Israel Deaconess Medical Center, Boston, Massachusetts, on January 15, 2009 has recently been published in the Journal of the American Medical Association, JAMA. It provides a discussion by an epidemiologist with a broad knowledge in the field in response to a theoretical question, as from a middle-aged patient, as to the advisability of consuming some alcohol “for his health.”
The paper provides an excellent discussion of a theoretical question about drinking and health. It focuses on the potential risks and benefits associated with moderate drinking for a middle-aged male patient. Most members of the International Scientific Forum on Alcohol Research (ISFAR) were pleased with the discussion of the topic. It was noted how uncommon it is that such knowledgeable, detailed, and mostly objective data appear in the mainstream medical literature. It was thought to be “readable, informative and thoughtful.”
The ISFAR critique points out a number of topics that were covered incompletely in the paper, including inadequate information on the importance of the pattern of drinking: moderate regular consumption versus binge drinking. Further, there was a notable lack of information on the beneficial effects on many pathophysiologic processes of polyphenols and other non-alcohol substances present in wine and certain other foods and beverages.
Overall, it was believed that the paper provided important information for physicians who may be discussing alcohol consumption with their patients.
Reference
Clinical Crossroads: Conferences with patients and doctors. A 42-year-old man considering whether to drink alcohol for his health. Kenneth J. Mukamal, MD, MPH, Discussant. JAMA 2010;303:2065-2073. (doi:10.1001/jama.2010.550)
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: Critique 009.
===============================================================================
Summary: Critique 008: 13 June 2010
Further evidence that moderate alcohol consumption may play a role in the prevention of Alzheimer’s Disease
In a case-control study from Spain on the effects of smoking and alcohol use on the risk of Alzheimer’s Disease (AD), the authors found that the risk of AD was unaffected by any measure of tobacco consumption. On the other hand, alcohol consumers showed a 47% lower risk of developing AD than did never consumers, with effects mainly among women and among never smokers. No differences were noted by type of alcoholic beverage consumed. The authors conclude that mean daily total consumption of alcohol showed increasingly protective dose-response relationships in women.
The numbers in this analysis were rather small, and there is always the possibility of confounding by other lifestyle factors. Still, the study supports a number of previous epidemiologic studies showing a lower risk of developing AD for moderate consumers of alcohol.
Reference
García AM, Ramón-Bou N, Porta M. Isolated and joint effects of tobacco and alcohol consumption on risk of Alzheimer’s Disease. Journal of Alzheimer’s Disease 2010;20:577–586. (DOI 10.3233/JAD-2010-1399).
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: Critique 08.
===============================================================================
Summary: Critique 007 9 June 2010
People may change to a “healthier” pattern of drinking as they age
In a prospective longitudinal study of a cohort of Americans in the “Baby Boomer” generation, subjects’ drinking habits were assessed at two points, when they were approximately 53 years of age and again when they were approximately 64 years of age. As the subjects got older, they began to consume fewer drinks per occasion but to consume alcohol more frequently; the net effect was little change in total alcohol intake for women but a slight increase for men.
In most epidemiologic studies, regular moderate drinking is the pattern associated with lower risk of many chronic diseases; hence, the described change in drinking pattern in this study (smaller amounts on more frequent occasions) can be considered a “healthy” change. Most long-term observational studies show a decrease in total alcohol intake with ageing, although reasons for such are poorly understood.
This paper emphasizes the importance of knowing the pattern of drinking, and not just the total number of drinks consumed over a week, when evaluating the impact of alcohol consumption on health and disease.
Reference
Molander RC, Yonker JA, Krahn DD. Age-related changes in drinking patterns from mid- to older age: results from the Wisconsin Longitudinal Study. Alcoholism: Clinical and Experimental Research 2010;34 (Published early online 7 May 2010).
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: Critique 07.
===============================================================================
Summary: Critique 006 2 June 2010
For patients who already have cardiovascular disease, continued moderate alcohol consumption may reduce their risk of death
This review paper in Circuation summarizes data from 8 epidemiologic studies of subjects with cardiovascular disease (CVD) as to their subsequent mortality (both CV and total-mortality) according to their alcohol consumption. Most studies showed significantly lower risk of both CV and total mortality for patients with CVD who were consumers of alcohol.
Despite these clear-cut findings, the authors were very cautious in their conclusions, focusing on the dangers of excessive drinking and not encouraging cardiovascular patients who do not drink to start regular drinking. They state that moderate consumers of alcohol who have CV disease should not be advised to stop drinking, but should be advised to not consume alcohol more heavily.
It is interesting that these authors published the meta-analysis upon which this review is largely based in the Journal of the American College of Cardiology earlier in 2010. In that paper, their conclusions were less restrained: “Cardiologists should be aware that regular, moderate alcohol consumption, in the context of a healthy lifestyle (increased physical activity, no smoking), dietary habits (decreased dietary fat intake, high consumption of fruit and vegetables), and adequate drug therapy, would put their patients at a level of cardiovascular or mortality risk substantially lower than either abstainers or heavy or binge drinkers.”
Reference
Costanzo S, Di Castelnuovo A, Donati MB, Iacoviello L, de Gaetano G. Contemporary Reviews in Cardiovascular Medicine. Cardiovascular and overall mortality risk in relation to alcohol consumption in patients with cardiovascular disease. Circulation 2010;121;1951-1959.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 006.
===============================================================================
Summary: Critique 005 27 May 2010
Alcohol in young women may increase their risk of benign breast disease
Among more than 6,000 young women being followed in a longitudinal study, 67 confirmed cases of benign breast disease (BBD) were diagnosed. Alcohol consumption was reported on 57 women who developed BBD when they were 16 – 23 years of age, with all but 8 subjects being 18 or older when they reported alcohol intake, and no data were presented on potential exposures earlier following menarche. A significant increase in the risk of BBD was associated with alcohol intake, although many key factors that have been shown to relate to BBD were not reported in the paper. Hence, while the number of cases is small, and a number of potential risk factors are not included, this study suggests that BBD may be increased by alcohol consumption in young women.
Reference
Berkey CS; Willett WC; Lindsay Frazier A; Rosner B; Colditz GA; Rockett RH; Helaine RM. Prospective study of adolescent alcohol consumption and risk of benign breast disease in young women. Pediatrics 2010;125:e1081-e1087.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 005.
===============================================================================
Summary: Critique 004 24 May 2010
Moderate alcohol consumption is associated with other healthy lifestyle factors
An analysis based on a very large number of subjects in France demonstrates, as have most other studies, that moderate consumers of alcohol have many associated healthy lifestyle habits: lower levels of body mass index, blood glucose, heart rate, stress and depression scores; higher subjective health status, HDL-cholesterol values, levels of physical activity and social status. The authors suggest that alcohol is not related causally to any of these factors, and that the other lifestyle factors, not alcohol consumption, are the reason that moderate drinkers have less cardiovascular disease. They chose a very narrow group of citations from the literature to support this contention.
The authors ignore a large number of well-conducted prospective epidemiologic studies showing that moderate drinkers are at lower risk over time of developing certain risk factors. Further, the authors of this paper ignore an immense basic science literature that suggests that alcohol is an important factor in the development of biological risk factors, atherosclerosis, and cardiovascular disease. Further, they do not describe a number of studies that have shown specifically that moderate drinking is associated with less cardiovascular disease and diabetes among subjects who are otherwise very healthy (non-smokers, not obese, physically active, and on a healthy diet).
There is no doubt that confounding by associated lifestyle factors can play a role in the lower risk of chronic diseases among moderate drinkers, who tend to also have other healthy behaviors. However, there is now a large body of scientific evidence that indicates that alcohol is an important factor in the lower rates of such diseases; current scientific data do not support the conclusions of the authors of this paper.
Reference
Hansel B, Thomas F, Pannier B, Bean K, Kontush A, Chapman MJ, Guize L, Bruckert E. Relationship between alcohol intake, health and social status and cardiovascular risk factors in the urban Paris-Ile-De-France Cohort: is the cardioprotective action of alcohol a myth? European J Clin Nutrition, advance online publication, doi:10:1038/ejcn.2010.61.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 004.
===================================================================================
Summary: Critique 003 17 May 2010
Moderate alcohol consumption markedly reduces the risk of diabetes mellitus, even among subjects with otherwise very healthy lifestyles
In a very well-done analysis from a large Dutch population, it was shown that moderate drinking considerably lowers the risk of developing type 2 diabetes even among subjects who are otherwise following a healthy lifestyle (not obese, non-smokers, physically active, eating a healthy diet). Thus, it indicates that the effect of moderate drinking on lowering the risk of diabetes cannot be explained by other healthy lifestyle habits of such drinkers. Moderate drinking should be considered as a complement, and not as an alternative, to other healthy lifestyle habits that lower the risk of chronic diseases such as diabetes and coronary heart disease.
Reference
Joosten MM, Grobbee DE, van der A DL, Verschuren WWM, Hendriks HFJ, Beulens JWJ. Combined effect of alcohol consumption and lifestyle behaviors on risk of type 2 diabetes. Am J Clin Nutr 2010;91: 1777-1783.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 003.
===============================================================================
Summary: Critique 002 26 April 2010
Red wine, but not other types of alcohol, improve endothelial function in a randomized trial
The healthy state of cells that form the lining of arteries, assessed by indices of endothelial function, is a key factor associated with preventing the development and progression of atherosclerosis and coronary heart disease. In a randomized trial among healthy young adults, the daily consumption of about 3 ounces of red wine for three weeks led to significant improvement in endothelial function. Such improvements were not seen with the consumption of water, or of beer or vodka containing similar amounts of alcohol.
Further, in a series of in-vitro studies, the authors showed very similar effects from red wine and from a high concentration of resveratrol (but not from beer or ethanol) on factors associated with improved endothelial function. The study supports many epidemiologic and animal experiments suggesting that certain non-alcoholic constituents of red wine have additional beneficial effects on cardiovascular risk over those of just the alcohol itself.
Reference
Huang PH, Chen YH, Tsai HY, Chen JS, Wu TC, Lin FY, Sata M, Chen JW, Lin SJ. Intake of red wine increases the number and functional capacity of circulating endothelial progenitor cells by enhancing nitric oxide bioavailability. Arteriosclerosis Thrombosis and Vascular Biology 2010;30:869-877.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 002.
===============================================================================
Summary: Critique 001 24 April 2010
Genetic effects on alcohol metabolism modify the relation of alcohol to breast cancer
A study from Germany compared the association between alcohol and breast cancer risk according to genetic variations affecting levels of alcohol dehydrogenase, an enzyme that clears alcohol from the blood stream. The authors conclude that genetic factors associated with the slow clearance of alcohol are associated with increased risk of breast cancer for drinkers; an increase in cancer risk was not seen for drinkers with genetic factors leading to fast clearance of alcohol. Such a finding would suggest that alcohol itself is the cause of an increase in breast cancer risk among drinkers.
Unfortunately, some previous studies have shown the opposite, that an increase in breast cancer risk occurs only among women who have genes associated with fast, rather than slow, alcohol metabolism. Overall, current scientific data indicate that breast cancer’s relation to drinking is not resolved, remaining murky and conflicted, and perhaps overemphasized. This facet of that murkiness is itself also conflicted. As of now, it is unclear the degree to which genes affecting alcohol dehydrogenase modify the association between alcohol and the risk of breast cancer and other diseases.
Reference
Larsen SB, Vogel U, Christensen J, Hansen RD, Wallin H, Overvad K, Tjønneland A, Tolstrup I. Interaction between ADH1C Arg272Gln and alcohol intake in relation to breast cancer risk suggests that ethanol is the causal factor in alcohol related breast cancer. Cancer Letters, 2010, in press.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 001.
=====================================================
Critique 256: Alcohol consumption and health outcomes among 70 year olds in Sweden –22 August 2022
In a population-based cohort of 70-year-old men and women recruited in Gothenburg, Sweden, in 2014-2016, the authors of this paper have presented a detailed listing of many social, environmental, and biological factors that relate to non-drinking, former drinking, or current drinking of varying amounts of alcohol. Our Forum critique raises some questions about the traditional belief that the elderly should consume markedly less alcohol than younger subjects, and that the limitations placed on subjects related sorely to their age may often not be appropriate.
The paper emphasizes how a very large number of factors may modify the association between the amount of alcohol consumed and measures of health and disease. Many of these, such as indices of socio-economic state, are usually adjusted for in epidemiologic studies. Data on other factors that relate to alcohol consumption (such as self-related health, having a partner, grip strength, having others worried about their drinking, religiosity, gait speed, life satisfaction, etc.) represent data usually not collected in epidemiologic studies.
Forum members thought that these analyses show that subjects whose reported alcohol intake is only slightly above the recommended “safe” levels for subjects of this age should not be classified as “at-risk” drinkers. Most of their features match those of subjects reporting intake within current recommendations; certainly, they do not match the characteristics of heavier drinkers.
Forum members also pointed out that in addition to improved mortality associated with truly moderate drinking, as seen in essentially all epidemiologic studies, these analyses demonstrate that many other components of “successful ageing” are also associated with regular, moderate consumption of alcohol.
Reference: Ahlner F, Erhag HF, Johansson L, Fässberg MM, Sterner TR, Samuelsson J. Zettergren A, Waern M, Skoog I. Patterns of Alcohol Consumption and Associated Factors in a Population-Based Sample of 70-Year-Olds: Data from the Gothenburg H70 Birth Cohort Study 2014–16.
Int J Environ Res Public Health 2022;19:8248; https://doi.org/10.3390/ijerph1914824
Comments on this critique by the International Scientific Forum on Alcohol Research have been provided by the following members:
Giovanni de Gaetano, MD, PhD, Department of Epidemiology and Prevention, IRCCS Istituto Neurologico Mediterraneo NEUROMED, Pozzilli, Italy
Curtis Ellison, MD, Professor of Medicine, Emeritus; Section of Preventive Medicine & Epidemiology, Boston University School of Medicine, Boston, MA, US
Harvey Finkel, MD, Hematology/Oncology, Retired (Formerly, Clinical Professor of Medicine, Boston University Medical Center, Boston, MA, USA)
Tedd Goldfinger, DO, FACC, Desert Cardiology of Tucson Heart Center, University of Arizona School of Medicine, Tucson, AZ, USA
Dominique Lanzmann-Petithory, MD, PhD, Nutrition Geriatrics, Hôpital Emile Roux, APHP Paris, Limeil-Brévannes, France
Linda McEvoy, PhD, Department of Radiology, University of California at San Diego (UCSD), La Jolla, CA, USA
Erik Skovenborg, MD, specialized in family medicine, member of the Scandinavian Medical Alcohol Board, Aarhus, Denmark
Creina Stockley, PhD, MSc Clinical Pharmacology, MBA; Principal, Stockley Health and Regulatory Solutions; Adjunct Senior Lecturer, The University of Adelaide, Adelaide, Australia
Arne Svilaas, MD, PhD, general practice and lipidology, Oslo University Hospital, Oslo, Norway
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please type in www.alcoholresearchforum.org/critique-256.
=====================================================
Critique 255: Wine consumption and the risk of cognitive decline in the elderly – 29 June 2022
The results of this systematic review and meta-analysis of longitudinal studies showed that, in almost every study, both wine consumption within the usual guidelines (no more than 2 drinks/day for men or 1 drink/day for women), as well as consumption in excess of these limits, were similarly associated with a lower risk of cognitive decline. For studies providing data on the amount of alcohol consumed, the risk of cognitive decline was reduced by 41% for both wine consumers drinking within the recommended guidelines as well as those reporting wine consumption in excess of the guidelines, when compared with abstainers. In studies where the amount of wine consumption was not reported, the estimate was an 18% reduction in the risk of cognitive decline for wine consumers versus abstainers.
Forum members noted that many potential confounders of the relation of alcoholic beverage consumption and cognition may modify the effects of alcohol on cognition, and were not evaluated very well in this study. Especially important may be the pattern of drinking (regularly or irregularly, with or without food, with associated binge drinking, etc), Forum members agreed that the calculations of the authors support a protective effect of wine consumption against cognitive decline, but their conclusions may be limited because of residual confounding by the pattern of drinking and other key factors not included in their analyses.
Forum members also noted another recent paper relating brain MRI markers to alcohol intake. However, changes in cognitive function were not assessed in the latter paper, and a direct comparison between the two papers cannot be done. However, we conclude that there remain questions regarding the effects of wine and other beverages containing alcohol on cognition. Other studies have shown divergent effects on the risk of dementia associated with wine consumption and the intake of spirits, so there may indeed be different effects on cognition with wine intake, the factor studied in the present paper. And, when compared with non-drinking or drinking of other beverages, extensive research supports health and mortality advantages when wine is consumed moderately, and especially with meals.
Reference:Lucerón-Lucas-Torres M, Cavero-Redondo I, Martínez-Vizcaíno V, Saz-Lara A, Pascual-Morena C, Álvarez-Bueno C. Association Between Wine Consumption and Cognitive Decline in Older People: A Systematic Review and Meta-Analysis of Longitudinal Studies. Frontiers in Nutrition 2022;9:863059
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
=====================================================
Critique 254: Adjusting for underreporting of alcohol intake in epidemiologic studies – 13 April 2022
It has been demonstrated repeatedly that the total population alcohol consumption based on self-reports by subjects in surveys and epidemiologic studies is lower than the amount of alcohol sold or taxed (disappearance data) within the population. This is assumed to relate to marked underreporting of individuals of their consumption, sometimes by one half or more. A key problem in attempting to adjust the self-reported values to more closely match the total alcohol disappearance data is that everyone does not underreport their intake, or may do so by different degrees.
The present study was based on data from US adults who responded to the 2011-2015 Behavioral Risk Factor Surveillance System (BRFSS; N = 2,198,089). The authors tested six methods for adjusting the self-reported data to provide what they hoped to be a more accurate value; some methods included adjustments based on differences in consumption by age and sex subgroups. From an unadjusted value of self-reported consumption of only 31.3% of that indicated by disappearance data, the various methods provided adjusted values ranging from 36.1% to 73%. The authors then used higher values to estimate the effect on alcohol-attributable deaths, using a population-attributable fraction approach.
While applauding the authors for attempting to obtain better estimates of alcohol consumption, Forum members were surprised that the authors did not even mention the method for identifying underreporting of individual subjects described by Klatsky and colleagues in the Kaiser Permanente Studies. The results of their method have been demonstrated to relate closely to alcohol’s effects on the risk of cancer, hypertension, and total mortality. Their method includes, in addition to self-reported data on alcohol consumption, adjustments for a variety of health conditions known to relate to excessive alcohol exposure, including alcoholic liver disease, hospitalizations for intoxication, mental problems associated with heavy drinking, etc. The presence of these conditions not only suggested that such subjects markedly underreported their intake (the exposure), but they also had much higher risk of adverse health effects (the outcome). When these conditions were not present at any of the study visits of subjects (allowing such subjects to be classified as being unlikely to be underreporting their alcohol consumption), adverse effects of low to moderate alcohol intake were generally not seen or their occurrences were markedly less frequent. This adjustment approach seems to be the only one previously described that gives reasonable results for individuals, and is clearly associated with the future health outcomes of subjects (and we realize that the occurrence of certain diseases or death happens for individual subjects, not for the population).
The Forum also raised questions about using “alcohol-attributable risk”. The authors base their calculations of population attributable risk on the hypothetic assumption of a rather low degree of underreporting in the population studies that are used as foundation of relative risk associations between alcohol intake and disease. Thus, risk is based mainly on self-reports of intake, even though their present paper indicates that adjustment for underreporting is so important. Further, throughout the paper, it appears that the authors tend to focus only on the adverse effects of alcohol without taking into regard the beneficial effects of light-to-moderate drinking, especially the regular consumption of wine with meals, which is found almost universally to be associated with lower risk of cardiovascular disease, diabetes, and total mortality.
While appropriate adjustment for underreporting could greatly improve the results of epidemiologic studies on alcohol and health, the goal would be to develop methods of determining the risk of individual subjects by including data on their own pattern of drinking and not assuming that the same adjustment formula applies to everyone in a population. By being able to identify subjects who underreport their intake, it would lead to some people changing categories of intake, and should result in estimates of either a lower risk, or greater risk, of adverse health effects of alcohol for that category of drinking. Further, more accurate and updated assessments of future health conditions that may be adversely (or beneficially) related to alcohol consumption should improve results and provide better data for setting drinking guidelines.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 253 – The relation of alcohol consumption to the risk of glioma tumors of the brain – 5 January 2022
There appears to be an increase in the risk of glioma tumors of the brain, yet very few lifestyle or genetic factors shown to be true “risk factors” for the disease have been identified. The authors of this paper present the association between reported alcohol consumption from multiple assessments over decades and the diagnosis of such tumors, combining data from subjects in large cohort studies of nurses and male health care providers. Among the important strengths of this paper is the fact that the data were collected as part of a prospective study, difficult to do in cancer epidemiology except with very large cohorts. A total of 554 cases of glioma tumors were identified in these cohorts from a total sample of more than 200,000 subjects.
Forum reviewers agree with the conclusions of the authors that light-to-moderate alcohol consumption does not increase the risk of glioma; in fact, total alcohol consumption over many decades was found to reduce the risk. For example, a cumulative average consumption of total alcohol of >8 to 15 g/d (approximately 0.5 to 1.0 drink/day) was associated with a 25% lower risk of glioma when compared with the lowest category of intake (0 to 0.5 g/day) for both men and women. For consumers of > 15 g/d (just over 1 typical drink/day) versus the referent group, the risk for women was further significantly reduced to HR = 0.61; for men, the HR estimate was 0.79, but not statistically significant. (Some previous cohort studies have suggested an increase in risk for heavy drinkers.) There were no differences according to type of alcoholic beverage. For the subgroup of subjects with glioblastomas, findings were similar but less precise, due to smaller case counts.
The Forum concludes that light-to-moderate alcohol consumption, versus no alcohol intake or very occasional drinking, does not increase the risk; in this very well-done study, such consumption showed a significant reduction in the risk of glioma tumors of the brain.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 252: Dealing with previous alcohol exposure among “current non-drinkers” in epidemiologic studies testing the J-shaped curve – 3 December 2021
Most cohort studies have demonstrated a reduced risk of cardiovascular diseases, diabetes, and even dementia among light-to-moderate consumers of alcohol when compared with lifetime abstainers. This is often described as a “J-shaped curve,” a reduction in disease risk for light drinkers (compared with abstainers) but an increase in risk for heavy drinkers. Many criticisms of the J-shaped curve have been based on claims that many studies include “sick quitters” in their referent group. Such criticisms ignore most recent cohort studies in which only lifetime abstainers make up the referent group. Epidemiologists have known for decades that including ex-drinkers in the referent group for evaluating health effects of alcohol is an error; such a group cannot be used for comparisons with moderate drinkers.
While the present study from a large cohort in Germany clearly shows how previous alcohol excess and other unhealthy lifestyle factors and socio-economic factors influence the risk of many diseases, it creates a referent group made up of mixing lifetime abstainers and some ex-drinkers, and that their analyses show that this group does not have a higher risk of mortality than light drinkers (thus, the protection of light drinking leading to a decrease in risk of disease is erroneous). The authors of this paper apparently did this because they had such a small group of lifetime abstainers (only 42 subjects out of a cohort of 4,000!), a number grossly inadequate for comparisons with drinkers.
Forum members agreed that it was a serious error for the investigators; instead of admitting that their numbers were too low in this group for reliable comparisons, it appears that the authors augmented the comparison group with a group of ex-drinkers (that they considered to not be heavy drinkers) and reported that their analyses do not support a reduced risk among light drinkers. Thus, their claim that the lower risk of cardiovascular disease demonstrated in most studies among moderate drinkers is unrelated to alcohol consumption. However, this claim is based on an improper referent group used in their analyses. Forum members considered this to be a deeply flawed analysis, and of no merit for use in setting drinking guidelines.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 251: Does moderate drinking increase, or decrease, the risk of falls in middle-age to elderly adults? 1 November 2021
To judge the relation of reported alcohol consumption to the risk of subsequent falls requiring hospitalization, the authors of this paper used data from the EPIC-Norfolk study, a prospective population-based cohort study in Norfolk, UK. In that study, there were a total of 25,637 community-dwelling adults, aged 40–79 years when recruited. The main outcome was the first hospital admission due to a fall over a follow-up period of about 11.5 years.
The key results of the study were that 19.2 % of non-drinkers were hospitalized for a fall during follow up, compared with 13.7% of low drinkers, 10.9 % of moderate drinkers, and 12.3% of heavy drinkers. In addition, the cumulative incident rates for falls at 121-180 months of follow up were 11.08% for teetotalers, 7.53% for low drinkers, 5.91% for moderate drinkers, and 8.20 % for heavy drinkers.
Forum members considered this to be a well-done study, with the analysis adjusting for a large number of factors that were potential confounders of the relation of alcohol intake to the risk of falls. We agree with the conclusions of the authors: “Moderate alcohol consumption appears to be associated with a reduced risk of falls hospitalization, and intake above the recommended limit is associated with an increased risk,” although we note that the increase in risk for heavier drinkers only appeared after essentially all covariates were added to the analysis. Obviously, residual confounding is always a possibility, but the present analyses indicating some protection against falls among light-to-moderate drinkers are supported by some well-done previous research.
The results of this study do not support the claim that any alcohol increases the risk of falls in older adults. It appears that this is not a concern for light-to-moderate drinkers who, in this study, had a lower risk of falls requiring hospitalization than did non-drinkers.
Reference: Tan GJ, Tan MP, Luben RN, Wareham NJ, Khaw K-T, Myint PK. The relationship between alcohol intake and falls hospitalization: Results from the EPIC-Norfolk. Geriatr Gerontol Int 2021;21:657-663.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 250: Importance of a favorable pattern of drinking (regularly, and with food) on risk of mortality – 28 July 2021
This is an analysis based on a very large data base of alcohol consumers (subjects reporting > 0 g of alcohol/week) from the UK Biobank (analyses based on 316,627 subjects with a median follow up of 8.9 years). The authors constructed categories of Drinking Habit Scores (DHS) for subjects; a “favorable” DHS was used for those subjects reporting a drinking frequency of 3 or more days/week and consuming alcohol with meals. The investigators then related the DHS categories to subsequent all-cause and cause-specific mortality, with adjustments for essentially all of the common known confounders/modifiers of alcohol effect.
Overall, Forum reviewers agreed with the main outcomes of the study, which indicate that subjects with a favorable DHS (in comparison with other drinkers) had significantly lower all-cause mortality (HR=0.82), CVD mortality (HR=0.84); cancer mortality (HR=0.82), and death from other causes (HR=0.77). In relation to the number of drinks consumed, the authors report that for all-cause, CVD, and other cause mortality, subjects with a favorable DHS showed a U-shaped or L-shaped curve (in that even for the heaviest drinkers, the mortality risk remained the same or lower than that of abstainers). Only for cancer mortality was there an increase in risk for subjects in the highest category of alcohol intake, leading to a J-shaped curve.
While the authors did not report specifically on the types of beverage being consumed in their favorable drinking pattern, it is the typical pattern generally found in southern Europe, and typically it is wine with meals. In these societies, wine is considered part of the meal, and is not consumed as “shots” that are usually being taken primarily as a way of getting drunk. As described in this paper, it is important to separate the health effects of these opposite approaches for consuming a beverage containing alcohol; putting all subjects into groups based only on the grams of alcohol consumed over a period, usually a week, does not take into account the important differences associated with the pattern of drinking.
We are finally appreciating that we are much further along in our research on alcohol and health than the innumerable studies that have focused just the amount of alcohol consumed, or on the J-shaped curve. We now realize the importance of the pattern of drinking. This constitutes not only the type of beverage and frequency of drinking, but also the consumption of alcohol with food and the absence of binge drinking. The pattern of drinking appears to be as important as, or even more important than, the quantity of alcohol consumed.
Reference: Ma H, Li X, Zhou T, Sun D, Shai I, Heianza Y, Rimm EB, Manson JE, Qi L. Alcohol Consumption Levels as Compared With Drinking Habits in Predicting All-Cause Mortality and Cause-Specific Mortality in Current Drinkers. Mayo Clin Proc 2021;96:1758-1769.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 249: Does light-to-moderate drinking increase the risk of atrial fibrillation? — 23 June 2021
While many epidemiologic studies have demonstrated an increase in the risk of AF for consumers of alcoholic beverages, there remains a question as to whether or not there is a threshold amount that would increase the risk. The present study concludes that “less than two alcohol units/day significantly increased the risk of incident AF, however, in men only. Reduction of even a moderate alcohol intake may thus reduce the risk of AF at the population level.”
While this may be the case, Forum members had a number of concerns about using the results of the present study to determine whether or not there is a threshold amount of alcohol necessary to increase the risk of AF. The methods used to judge alcohol consumption did not report the type of beverage or have a good estimate of the pattern of drinking, both of which factors are known to modify the health effects of alcohol. Further, the authors stated that there was evidence of considerable under-reporting of alcohol in their cohort, as the level of HDL noted in their “light” drinkers was above the level expected. This suggested to them that subjects in their lowest category of alcohol may actually have consumed more than they reported (probably about twice the reported amount of alcohol). This makes it difficult to determine if truly “light” drinking is associated with an increased risk of AF.
Overall, scientific data continue to show that light-to-moderate alcohol intake, especially when the pattern of drinking is found to be regular moderate consumption with food and without binge drinking, is associated with a lower risk of ischemic stroke and death. For the effects of alcohol intake on the risk of AF, the situation remains unclear. Unfortunately, the present study cannot answer the question as to whether there is, or is not, a clear threshold effect of alcohol intake on the risk of developing AF.
Reference: Ariansen I, Degerud E, Gjesdal K, Tell GS, Næss O. Examining the lower range of the association between alcohol intake and risk of incident hospitalization with atrial fibrillation. IJC Heart & Vasculature 2020;31:100679.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 248: Association of Alcohol Consumption with Cataract Surgery — 19 April 2021
This was a well-done analysis of a very large number of cases of cataract surgery in the UK; there were reasonable measures of the exposure (alcohol consumption), including the amount and type of beverage consumed, and appropriate potentially confounding factors were taken into consideration. However, data on the consumption of alcohol with or without food were not available. The use of national registries of cataract surgery provide an appropriate approach for estimating the main outcome of the analyses, and the results probably reflect the incidence of clinically significant cataract occurrence in these populations.
The key results were that there was a small but highly significant lower risk of cataract surgery among moderate drinkers. Red and white wine consumers showed more consistent and significantly lower risks of cataract surgery than consumers of other beverages. (In one of the two studies included in the analysis, small amounts of beer and spirits also showed a lower risk than that of non-drinkers.) There were too few heavy drinkers in these studies to determine the extent to which such drinking might affect risk. We appreciate that residual confounding, especially by factors that relate to subjects choosing to have surgical treatment of their cataracts, could still be present in these results.
Forum reviewers conclude that, in agreement with the investigators of this study, the data indicate a small but statistically and clinically significant decrease in the risk of cataract surgery for low-to-moderate drinkers, versus non-drinkers. A lowering of risk was especially clear for wine drinkers, in comparison with consumers of beer and spirits. There is an extensive literature regarding potential mechanisms by which constituents of the diet, especially those present in wine, may influence the development of cataracts. Among these are antioxidants or ROS scavengers, aldose reductase inhibitors, antiglycating agents, and inhibitors of lens epithelial cell apoptosis. However, the ultimate reason for the lower risk of cataract surgery associated with wine consumption found in this study has not been clearly delineated.
Reference: Chua SYL, Luben RN, Hayat S, Broadway DC, Khaw K-T, Warwick A, et al, on behalf of The UK Biobank Eye and Vision Consortium. Alcohol Consumption and Incident Cataract Surgery in Two Large UK Cohorts. Ophthalmology 2021, pre-publication.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 247: Effects of alcohol consumption on risk of stroke and systemic embolism among subjects with atrial fibrillation – 15 March 2021
The main aim of the current study was to investigate the associations of regular alcohol intake with incident stroke or systemic embolism in patients with established atrial fibrillation (AF), most of whom (84%) were on anti-coagulant therapy. The authors used combined data from two prospective studies of subjects with AF, followed for an average of 3 years. While they excluded subjects with “only short, potentially reversible AF episodes (e.g., as after cardiac surgery or sepsis)” about one half of subjects in the study were diagnosed as having paroxysmal AF. Reported alcohol at baseline and at subsequent examinations was classified as none, > 0 to < 1 drink/day, 1 to < 2 drinks/day, and ≥ 2 drinks/day.
The primary outcome was a composite of stroke and systemic embolism. Secondary outcomes were all-cause mortality, myocardial infarction, hospital admission for acute heart failure, and a composite of major and clinically relevant nonmajor bleeding. In their analyses, they adjusted for age, sex, education, hypertension, history of heart failure, history of diabetes, BMI, smoking status, physical activity, history of stroke, history of coronary heart disease, oral anticoagulation, history of renal failure, AF type, and health perception. With annual assessments, the investigators updated all covariates over time, if appropriate.
The main results indicated no significant effect of alcohol consumption on the risk of the major outcomes (stroke or systemic embolism). However, there were significant decreases in risk for several secondary outcomes. For hospital admissions for heart failure, in comparison with non-drinkers the HR for moderate drinkers was 0.60 (CI 0.41-0.87); further, among moderate drinkers the HR for myocardial infarction was 0.39 (CI 0.20 – 0.78), and for all-cause mortality the HR was 0.49 (CI 0.35-0.69).
Forum members had two major concerns with the paper. First, the authors failed to report specifically how alcohol consumption was associated with increased or decreased presence of AF during follow up, even though approximately one-half of subjects had only paroxysmal AF at baseline. Determining if alcohol consumption affected subsequent AF would be information of importance to practitioners who are advising their patients with AF regarding alcohol consumption.
Secondly, it was pointed out by Forum members that the results may have been affected by what is known as collider bias: as moderate drinking shows an inverse association with coronary heart disease (which is strongly related to the presence of AF), subjects who consumed alcohol prior to the baseline diagnosis of AF were probably different from those who had no prior alcohol exposure, and the results of combining these two groups (as was done in these analyses) may have been biased. Such bias usually tends to result in estimates of effect going toward the null.
While the reported results of no real effect of alcohol consumption on the risk of stroke or systemic embolism among patients with AF is encouraging, to decrease the risk of bias in future studies it will be important that such research attempts to separate subjects according to their prior use of alcohol before baseline measurements are assessed. The marked reduction in the risk of other major cardiovascular outcomes and total mortality, found in this study to be associated with light to moderate drinking, matches the results seen in most previous studies.
Reference: Reddiess P, Aeschbacher S, Meyre P, Coslovsky M, Kühne M, Rodondi N, et al, for the BEAT-AF and Swiss-AF investigators. Alcohol consumption and risk of cardiovascular outcomes and bleeding in patients with established atrial fibrillation. CMAJ 2020;193:E117-E123. doi: 10.1503/cmaj.200778
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 246: Light to moderate alcohol intake and the risk of cancer — 8 February 2021
The present paper attempts to use alcohol-attributable data, based on combining average alcohol intake from diverse European populations, to judge the effects of moderate alcohol consumption on the risk of cancer for all populations. It is based on earlier calculations of risk, extensively covered in previous publications by the senior author. The investigators conclude that the risk of a number of types of cancer are increased even among subjects reporting no more than 20 grams of alcohol per day (up to about 2 typical drinks), an amount they state to be within recommended levels of consumption (but exceed current US Drinking Guidelines for women of no more than 1 drink/day). The largest contribution to their calculated effects of alcohol was from breast cancer in women (which made up “68.7% of all alcohol attributable cancer for both sexes”). Breast cancer is a condition for which many factors other than just average alcohol intake are important: factors such as pattern of drinking, type of beverage, folate intake, smoking, obesity, physical activity, etc., all of which tend to confound the association.
Forum members had real concerns about their methodology of using an estimate of “alcohol-attributable cancer” based on reported average intake from 28 separate countries, including the large countries in western Europe (e.g., Germany, France, UK, Italy, Spain, Sweden), East-European countries (such as Poland and Hungary), and many smaller countries (e.g., Malta, Cyprus, Luxembourg, Latvia). Given the marked variation in culture and drinking patterns among these countries, it was considered that there are a large number of confounders and modifiers of alcohol effects that vary by country, and make it impossible to simply take the average alcohol intake from such diverse cultures to estimate causality of alcohol and cancer for everyone. By lumping data from all of these countries, the analyses end up with values that relate to a non-existent hypothetical population; different countries have different risk relationships, so the estimates of effect described in the paper apply to no single country.
Further, the investigators do not report rates of other outcomes, especially total mortality, associated with drinking. Taking only one outcome condition, without at least noting that moderate drinking has almost uniformly been found to decrease all-cause mortality, limits the usefulness of their results for setting alcohol guidelines. Heavy alcohol use is recognized by all as a serious impediment to the health of individuals, and to society at large. However, recommending lowering the intake of alcohol for everyone does not take into consideration that light drinkers might be more likely than heavy drinkers to follow such advice and might decrease their consumption to zero. Because of moderate drinking’s almost uniformly demonstrated beneficial effect on cardiovascular disease, if many light drinkers stopped drinking completely it would be expected to increase, rather than decrease, total mortality rates and the health of the population.
In their conclusions, the authors only mention the results of their actual analyses briefly, then start the usual chant of the need for extensive public health measures (warning labels, public information campaigns, increasing alcohol taxes, etc.) which tend to emphasize the dangers of any alcohol consumption. However, the analyses in this paper do not provide the data that are needed if one is to set appropriate drinking guidelines, which should be age-specific, sex-specific, and population-specific. Such factors would include not only the alcohol-disease relation but the particular characteristics of the population, the objective of guidelines (to influence and change behavior among target populations), the behavior that is thought to be in need of change, the culture and mindset of the target population, and the kind of message that is likely to be effective. Forum members realize that there are tensions between advice intended only to reduce the prevalence of misuse versus advice that takes into account the well demonstrated beneficial health effects of light-to-moderate consumption. When setting guidelines, it is important to take into account the prevailing drinking culture of a country or population, because only in that way is it possible to produce a public health message that is likely to be respected and regarded.
Reference: Rovira P, Rehm J. Estimation of cancers caused by light to moderate alcohol consumption in the European Union. European Journal of Public Health 2021; pre-publication. doi:10.1093/eurpub/ckaa236.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================
Critique 245: Effects of different patterns of alcohol consumption on risk of mortality, major cardiovascular events, cirrhosis, and cancer — 25 January 2021
This study was designed to determine factors that affect the pattern of alcohol consumption (including the frequency of consumption, type of beverage, with or without food, etc.), rather than just the reported average amount of alcohol, related to all-cause mortality, major cardiovascular events-MACE (MI/stroke/cardiovascular death), accidents/injuries, liver cirrhosis, all-cause and alcohol-related cancer incidence. It was based on a large prospective cohort study of UK Biobank (UKB) participants and included more than 300,000 subjects; outcomes were ascertained over a 9-year median follow-up period. Non-drinkers and only occasional drinkers were excluded from the analyses, so this paper does not judge the effects of light or moderate drinking versus not drinking, but only the effects of the pattern of reported alcohol consumption among regular drinkers.
The study showed that in comparison with subjects who consumed red wine more than 50% of the time (the reference group) there were lower risks of many adverse outcomes than among consumers of more than 50% of the time of spirits; the latter had 25% greater risk of all-cause mortality, 31% greater risk of MACE, and 48% higher risk of liver cirrhosis after controlling for total weekly alcohol consumption and relevant confounders. In comparison with red-wine drinkers, consumers of beer/cider showed an 18% higher risk for all-cause mortality, 16% higher risk of MACE, and 36% higher risk of liver cirrhosis. There were no statistically significant differences in outcomes between white wine drinkers and red wine drinkers.
Consumption of alcohol with food, versus not with food, showed a 10% (CI 2%-17%) lower risk of all-cause mortality. While consumers reporting alcohol consumption 3-4 days/week had lower risk of some adverse outcomes than subjects reporting intake on only 1-2 days/week, for some reasons subjects reporting daily or near-daily intake had an increased risk of liver cirrhosis, probably related to under-reporting by some heavy drinkers.
Forum members agree with the conclusions of this study as reported in the Authors’ Abstract: “Red wine drinking, consumption with food and spreading alcohol intake over 3–4 days were associated with lower risk of mortality and vascular events among regular alcohol drinkers, after adjusting for the effects of average amount consumed.” The results of this well-done study emphasize how inappropriate it is to use just the total average alcohol intake when relating the consumption of alcoholic beverages to the risk of adverse health outcomes.
Reference: Jani BD, McQueenie R, Nicholl BI, Field R, Hanlon P, Gallacher KI, Mair FS, Lewsey J. Association between patterns of alcohol consumption (beverage type, frequency and consumption with food) and risk of adverse health outcomes: a prospective cohort study. BMC Medicine 2021;19:8. https://doi.org/10.1186/s12916-020-01878-2.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 244: Is “ideal cardiovascular health” more common among consumers of wine than among drinkers of other beverages? — 18 December 2020
While a beneficial effect on cardiovascular disease of moderate drinking has been shown repeatedly in epidemiologic studies, the specific effects of different types of alcohol have not been well established. The authors examined the relation between alcohol type and an index of ideal cardiovascular health (CVH) as measured by the American Heart Association’s seven CVH metrics. Data from more than six thousand men and women, participants in the Multi-Ethnic Study of Atherosclerosis, were used to relate the association of the consumption of wine, beer, and liquor to the CVH score.
The authors report that participants who consumed 1-2 drinks/day of wine had higher odds of optimal CVH scores compared to those who never drank wine [adjusted prevalence odds ratio (POR) 1.64 (1.12-2.40)]. However, in comparison with participants who never drank beer or liquor, the odds of optimal CVH scores were lower for consumers of these beverages.
Forum members had some questions about the methodology for judging intake of the different beverages, as well as the statistical approach used in these analyses. However, they consider that the results (more favorable associations with wine consumption than from that of other beverages on indices of cardiovascular health) are in line with most previous studies.
It is important to realize that this study did not measure effects on the risk of disease occurrence or mortality, but just on the CVH index, a measure of overall cardiovascular health. Thus, we cannot tell specifically from this study whether the higher health indices among moderate wine drinkers was the result of the wine that they drink (even though this might be expected to some extent since, for example, moderate wine intake is known to favorably affect BMI, blood lipids, and blood glucose) or that their results relate to the fact that people with more moderate lifestyles and higher education, income, etc., tend to prefer moderate wine consumption and are less likely to be binge or heavy drinkers. It may be that wine drinkers make better decisions on all lifestyle behaviors than consumers of other beverages.
Reference: Ogunmoroti O, Osibogun O, McClelland RL, Lazo M, Mathews L, Okunrintemi V, Oni ET, Burke GL, Michos ED. Alcohol type and ideal cardiovascular health among adults of the Multi-Ethnic Study of Atherosclerosis. Drug and Alcohol Dependence 2020: Pre-publication release
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 243: Does the “quality” of the diet modify the relation of alcohol intake to the risk of hypertension? – 19 October 2020
The authors of this paper test the hypothesis that overall diet quality influences associations between alcohol consumption and the risk of hypertension, based on data from a study in the USA (NHANES) and two studies in China. In general, their designation of a “high-quality” diet for Chinese was one with greater amounts of fruit, vegetables, and beans, while for Caucasians and Hispanics it was one with more whole grains, fruit, vegetables and nuts; “low-quality” diets were mainly those with higher intakes of red meat products. For comparisons with abstainers, subjects reporting < 7 drinks/week for total alcohol were categorized as light and those reporting 7-21 drinks/week categorized as moderate drinkers, with those reporting more referred to as heavy drinkers.
The paper concludes that light alcohol consumption among subjects with a high-quality diet was significantly associated with a decreased risk of hypertension in Caucasians, and the risk of hypertension was not significantly increased with increasing alcohol consumption in Caucasians, Chinese, and Hispanics. On the contrary, in context of a diet calculated to be low quality the risk of hypertension was significantly increased in a linear fashion with increasing alcohol consumption in all groups except African Americans.
Forum reviewers considered this to be a generally well-done and interesting study, but had concern that the authors may not have adjusted adequately for a factor strongly related to diet quality: socio-economic status. The authors included in their analyses whether or not subjects had a high school diploma, but no adjustments were made for occupation, income, or other important indices of deprivation, which may be important since lower SES subjects have consistently been shown to have poorer diets. Thus, we are unsure whether or not it is the diet solely that is the reason that alcohol consumption was found to be associated with lower, higher, or no effect depending on the type of diet. Further, no results are shown indicating whether or not there were differences if the beverage consumed was beer, wine, or spirits, and there was insufficient data on the pattern of drinking. The authors begin their abstract saying that ‘Alcohol is commonly consumed around mealtimes,’ but apparently do not have any data on whether the beverage was consumed with or without food for the present analyses.” All of these factors may modify how alcohol affects the risk of developing hypertension.
Finally, some Forum members were uneasy with the term “quality of diet”, based on the inclusion or exclusion of certain foods, which may be very important to taste. Said one member, we trust that diets recommended as being of “high quality” are not those whose savor has been removed.
Reference: Jiang W, Meng X, Hou W, Wu X, Wang W, Wang M, Chu X, Wang P, Sun C, Han T, Li Y. Impact of overall diet quality on association between alcohol consumption and risk of hypertension: evidence from two national surveys with multiple ethnics. Eur J Clin Nutr 2020; doi.org/10.1038/s41430-020-00708-1.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
=========================================================================
Critique 242: The relation of light alcohol consumption to the risk of common cancers – 1 October 2020
In an attempt to assess the relation between light alcohol consumption (<12.5g per day) and the risk of a number of types of cancer, the authors carried out a review of meta-analyses published within the past 15 years. Using as keywords “light alcohol drinking,” “light alcohol consumption” and “cancer”, they found 29 meta-analyses on the subject. They report their results as indicating that “Light alcohol drinking was not associated with an increased risk of cancer occurrence, with the exception of breast and prostate cancer and melanoma. Furthermore, a possible protective role of light alcohol consumption on the development of bladder, kidney and ovarian cancer and Non Hodgkin Lymphoma was observed.”
Forum reviewers found a number of weaknesses in the paper. While their title focuses on “light alcohol drinking,” most of their reports of results and their discussion deal with harmful effects of heavier drinking; however, by not including papers on ‘heavy drinking’ in their original search, they may have left out many relevant papers. Further, the very brief reviews of each common cancer that they comment upon are sometimes based on only one or two meta-analyses, leaving out a huge amount of key data, especially that from single, well-done, long-term cohort studies with important information on the relation of alcohol to cancer; potential confounding by many factors could not be taken into consideration.
In the analyses in the present paper, the reported average level of alcohol consumed is used, but there is insufficient evaluation of possibly more important indices of alcohol exposure: the pattern of drinking (e.g., type of beverage consumed, in binges or on a regular basis, consumption with or without food, etc.). Further, there is probably inadequate control for important confounders or consideration of the effects of under-reporting, which may have been seen in single studies but not apparent in meta-analyses. In addition, a number of errors are present within the report, such as conflicting statements that may misrepresent the numeric data given. These problems make these results of limited use to professionals in health policy who are developing guidelines for alcohol use in the general public.
Reference: Caprio GG, Picascia D, Dallio M, Vitiello PP, Giunta EF, De Falco V, et al. Light Alcohol Drinking and the Risk of Cancer Development: A Controversial Relationship. Reviews on Recent Clinical Trials 2020;15:164-177
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 241: A Mendelian randomization study of alcohol consumption and the risk of breast cancer and ovarian cancer reveals no significant associations — 22 July 2020
The authors of this ambitious study used a Mendelian Randomization (MR) approach in an attempt to determine if alcohol consumption is causally associated with the risk of female hormone-dependent cancers. They used summary level genetic data from the hitherto largest genome-wide association study (GWAS) conducted on alcohol consumption (N = ~1.5 million individuals), breast cancer (N cases = 122,977) and ovarian cancer (N cases = 25,509). They examined three different alcohol intake exposures: drinks per week, alcohol use disorder (AUD) and age-adjusted alcohol use disorder identification test (AUDIT-C), to reflect general and harmful drinking behavior. For instrumental variables (IVs), they constructed updated and stronger genetic instruments using 99 SNPs related to drinks/week, 9 SNPs related to AUD, and 13 AUDIT-C-related SNPs, and estimated the causal relationship applying several two-sample MR methods.
The key result of these analyses was that the investigators did not find any evidence that alcohol intake increased the risk of breast cancer. For ovarian cancer, an initial inverse association with alcohol intake became null when adjustments were made for confounders. While members of our Forum agreed with the overall conclusions of the authors, who stated that they did not find “any compelling evidence in support for a causal relationship between genetically predicted alcohol consumption and risk of breast or ovarian cancer, consistent across three different alcohol-related exposures,” Forum members identified a number of weaknesses of the analyses. For example, there were very limited data on the pattern of drinking or the type of beverage consumed, and no data on smoking and other lifestyle habits, diet, and many other environmental factors that relate to the effects of alcohol consumption. Further, much of the data utilized to generate the IVs of alcohol exposure were from men, rather than women, although the two conditions being studied are present only in women.
Forum members agreed with the authors about the need to combine data from MR analyses with data from observational and experimental studies before making conclusions about the relation of alcohol consumption to health and disease. Given the rapid expansion of genetic studies, it is likely that MR analyses will be increasingly important in our research efforts, but we agree that the consideration of a combination of data from observational studies, clinical trials, animal experiments, and MR analyses will be needed as we seek to improve our knowledge on the relation of alcohol intake to health and disease; it is, and will remain, a continuing challenge.
Reference: Zhu J, Jiang X, Niu Z. Alcohol consumption and risk of breast and ovarian cancer: A Mendelian randomization study. Cancer Genetics 2020;245:35–41
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 240: Are there health risks from amounts of alcohol referred to as being within “low-risk drinking” guidelines? — 8 July 2020
The authors of this paper use very questionable data to suggest that drinking guidelines for all countries should be lowered to no more than 1 drink/day. In their analyses, they make a very large number of assumptions, including adding 80% to reported amounts of alcohol for all subjects to make up for alcohol disappearance data, and do not modify this according to their individual likelihood of being an under-reporter of intake. Further, they are not able to adjust for the pattern of drinking or type of beverage consumed, and it is considered bizarre that they grouped ex-drinkers (many of whom were apparently heavy drinkers) with current drinkers who report consuming within the guidelines to state that such subjects have a high risk of adverse effects. From the numbers presented in the tables in this paper, the risk of alcohol-attributable death for consumers of alcohol within-guidelines was fifty times lower than for those consuming above the guidelines. Such deficiencies in methodology, and especially possibly deliberate combinations of groups to support their premise, make it impossible to utilize their conclusions for setting guidelines for “low-risk” drinking.
Further, their conclusions do not reflect what the vast majority of well-done epidemiologic studies have shown for decades that light-to-moderate alcohol consumption (when defined as up to 1 drink/day for women and up to 2 drinks/day for men and not consumed in binges) is associated with a significant decrease in the risk of cardiovascular mortality as well as total mortality. The results of the current paper are not sufficient to warrant changing drinking guidelines.
Reference: Sherk A, Thomas G, Churchill S, Stockwell T. Does Drinking Within Low-Risk Guidelines Prevent Harm? Implications for High-Income Countries Using the International Model of Alcohol Harms and Policies. J Stud Alcohol Drugs 2020;81:352–361.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 239: Does the source of funding of epidemiologic studies on alcohol and health affect their results? – 28 May 2020
Funding of research by industry can lead to sponsorship bias. The aim of the current study was to evaluate for sponsorship bias in observational alcohol research by focusing on a spectrum of health outcomes related to moderate alcohol consumption. The authors utilized data from seven recent meta-analyses that included information from 386 observational studies of the relation of moderate alcohol consumption to a large number of health outcomes, including cardiovascular diseases, cancer, and mortality.
The authors report that only 5.4% of studies had some support from the alcohol industry, while 80.1% were funded by governments or other sources (non-industry-funded). Further, the results of moderate drinking on almost all health outcomes (including cardiovascular diseases and cancer) were essentially the same whether the study was funded by the beverage industry or not. Where there were slight differences, the results from non-alcohol-industry sources tended to have more favorable health results from moderate drinking than did those sponsored by the industry. The authors end their discussion stating: “In conclusion, only a small proportion of observational studies in meta-analyses, referred to by several international alcohol guidelines, are funded by the alcohol industry. Based on this selection of observational studies the association between moderate alcohol consumption and different health outcomes does not seem to be related to funding source.”
Forum members considered that the analyses were very complete, and detailed data were given in the very exhaustive supplementary material provided (exceeding 90 pages). (This makes it possible for a reevaluation of their results by others.) While Forum members noted that this analysis was apparently supported by the Dutch Beer Institute, the extensive data presented provide no evidence that there was bias in any of the analyses, upon which most international drinking guidelines have been based. The Forum concludes that the major studies that have shown that moderate drinking can have health benefits, especially for coronary heart disease and type 2 diabetes, are not based on bias because of support from the alcohol beverage industry.
Reference: Vos M, van Soest APM, Wingerden T, Janse ML, Dijk RM, Brouwer RJ, deKoning I, Feskens EJM, Sierksma A. Exploring the Influence of Alcohol Industry Funding in Observational Studies on Moderate Alcohol Consumption and Health. Adv Nutr 2020: pre-publication.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 238: Differences in evaluating confounding in epidemiologic studies when judging the effects of alcohol consumption on the risk of cardiovascular disease – 7 April 2020
The authors of the present paper compared studies included in a recent meta-analysis on alcohol consumption and the risk of coronary heart disease (CHD) for the number of potential confounding variables included in the analysis for each paper. While they found that most studies included adjustments for smoking, age, BMI, height and weight, physical activity, and education, many studies included adjustments for a multitude of other factors. They reach the conclusion that the large variation between studies in adjusting for confounding makes it impossible to accept the finding of a J-shaped curve between alcohol consumption and CHD (despite the consistency of such results).
Forum members agree that evaluating confounders in epidemiologic studies is extremely important. However, standardizing environmental confounders is not possible as there are so many, and so many yet undefined, and these confounders would be expected to vary in their influence among different populations. The authors did not focus on the key factor: the potential impact of each potential confounder. Limited research suggests that any “unknown confounder” would need to be extremely powerful to negate the reported protective effect of light-to-moderate consumption of alcohol, especially of wine, on the risk of CHD.
In addition, the authors were perturbed that many individual studies did not state specifically in their discussion that “residual confounding may be present in our results” or that “results of individual studies must be interpreted with caution.” Forum members assume that most readers of scientific reports realize that there should always be caution in making conclusions from a single study, especially observational studies, without the authors pointing in out in their paper. It may be analogous to stating that “further research is needed,” which should be assumed for any scientific paper.
Members of the Forum acknowledge that confounding makes it a difficult process to judge causality from observational studies, but point out that potential confounders in one study may be insignificant in another. It is not possible to generate a list of potential confounders that would apply to all epidemiologic studies. However, the consistency of the J-shaped curve between alcohol intake and risk of CHD in almost all epidemiologic studies, with support from a multitude of experimental studies, strongly supports the validity of such a relation.
Reference: Wallach JD, Serghiou S, Chu L, Egilman AC, Vasiliou V, Ross JS, Ioannidis JPA. Evaluation of confounding in epidemiologic studies assessing alcohol consumption on the risk of ischemic heart disease. BMC Medical Research Methodology 2020;20:64 https://doi.org/10.1186/s12874-020-0914-6
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 237: Relation of alcohol consumption in the elderly to the chances of reaching 90 years of age — 2 March 2020
An interesting and well-done study from a cohort of aging men in the Netherlands that evaluated how alcohol consumption data collected at 68 – 70 years of age related to the risk that the individual would survive to age 90. The authors report that “The highest probability of reaching 90 was found in those consuming 5–<15g/d alcohol, with RR=1.36 (95% CI, 1.20–1.55) when compared with abstainers.” Further, the authors noted that “Wine intake was positively associated with longevity (notably in women), whereas liquor was positively associated with longevity in men and inversely in women.” They also noted that there was a tendency for a lower chance of living to age 90 for subjects reporting binge drinking.
Forum members were unanimous in considering this to be an excellent study. It adds information on alcohol consumption collected in the elderly (ages 68-70 in this study) and subsequent longevity of life. It tends to counter fears expressed by some that the very elderly must be “protected” from alcohol, as it suggests that there are still health benefits from moderate drinking at all ages. Further, the reduction in risk of cardiovascular diseases is especially important in the elderly. This critique provides references to a multitude of research reports that strengthen the conclusions of the authors that, even among very elderly subjects, moderate drinking is associated with a greater longevity of life.
Reference: van den Brandt PA, Brandts L. Alcohol consumption in later life and reaching longevity: the Netherlands Cohort Study. Age and Ageing 2020;00:1–8 doi:10.1093/ageing/afaa003.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 236. Reasons for apparently diverse results from epidemiologic studies relating alcohol consumption to the risk of breast cancer 19 February 2020
The relation of alcohol consumption to the risk of breast of cancer has been the subject of innumerable epidemiologic studies over many decades, with most showing a slight increase in risk even for light drinking. However, it has been shown that this relation is attenuated when certain potential confounders are adjusted for, including folate levels, frequency of binge drinking, and the use of post-menopausal hormonal therapy. The present paper took the results of a recent large-scale meta-analysis and sought to try and explain why there is a large variability of results when the 97 studies included in that analysis were compared. The authors attempted to judge to what degree differences in exposure definitions, contrast levels, different study populations, different adjustment covariates, and different model approaches affected estimates of the effect of alcohol on cancer risk. The key factor the authors used in their analyses was the ratio between the most harmful and the most protective effects of estimated risk within each study.
All of the contrasts studied (different measures of alcohol consumption, different populations, different analytic approaches, etc.) had some effect on the estimates of effect of alcohol on the risk of cancer. As stated by the authors, “These findings suggest that whereas certain analytical and modelling choices, reflecting different types of alcohol and/or doses, can result in genuine differences, it is possible that many different analytical options, with different results, are pursued and selectively reported. Therefore, individual reported relative risk estimates from observational studies should be interpreted with caution.” Some Forum members disagreed with this conclusion, suggesting that due to marked variation in population, type of alcohol, analytic approaches, adjustment for confounding, etc., considerable error may be built in when combining data from heterogeneous studies. They felt that single large, long-term, well-done individual prospective studies may be preferable for judging the true effect of alcohol on the risk of breast cancer.
Thus, while Forum reviewers appreciated the attempt to explain differences in results of studies to get a more valid estimate of the true relation of alcohol consumption to the risk of breast cancer, and the analyses presented were done appropriately, some considered the approach described as not being a useful or valid one. Finding large differences in effects among sub-groups may not provide a reliable measure. Alternative approaches to scrutinize findings from observational studies, including Mendelian randomization or discussion centered on E-value (which assesses how strong an unmeasured confounder would have be to eliminate observed effect estimates), may be preferable. While such methods are imperfect, their use would be more interesting in informing the public and advancing scientific knowledge.
Reference: Chu L Ioannidis J PA, Egilman AC Vasiliou V, Ross JS, Wallach JD. Vibration of effects in epidemiologic studies of alcohol consumption and breast cancer risk. Inter J Epidemiol 2020;10:1–11. doi: 10.1093/ije/dyz271
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 235: Does type of alcohol or drinking pattern explain greater adverse effects of alcohol consumption among lower socio-economic subjects? 15 January 2020
The authors of this paper aimed to investigate whether and to what extent consumption by beverage type, BMI, smoking and other factors explain inequalities in alcohol-related harm evidenced though wholly attributable alcohol-related hospital admissions (ARHA). They especially evaluated levels of socio-economic status (SES) as determined by geographic and individual levels of deprivation. They based their analyses on data from 11,038 respondents to the Welsh Health Survey who answered questions on their health and lifestyle.
The results of this study support previous research on how factors associated with poor socio-economic status relate to poor health outcomes. It provides added information by providing an expanded definition for deprivation (assessed from geographic area of residence as well as from personal data), and for potential differences by type of beverage consumed. The definition of deprivation included many factors that, together, seem to be the primary reason why poorer, less educated people seem to have more adverse health effects that have been attributed to alcohol consumption.
Specifically, this study shows that the amount of alcohol consumed by people with low SES may be only a minor factor in explaining their increase in adverse effects that are usually classified as being “alcohol-related.” In this study, the frequency of alcohol consumption explained only 4% of the greater number of “wholly attributable alcohol-related hospital admissions.” Co-existing other behaviors and conditions, especially smoking, obesity, living in a deprived environment, poor health status, and mental health, appeared to have much greater effect. Thus, the conclusions of this study suggest that even for what are referred to as “wholly attributable .alcohol-related hospital admissions,” other factors associated with low SES may be more important than alcohol consumption itself as determinants of such adverse health outcomes.
Reference: Gartner A, Trefan L, Moore S, Akbari A, Paranjothy S, Farewell D. Drinking beer, wine or spirits – does it matter for inequalities in alcohol-related hospital admission? A record-linked longitudinal study in Wales. BMC Public Health 2019;19:1651. https://doi.org/10.1186/s12889-019-8015-3
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 234: Effects of red wine consumption on gut microbiota that affect health and disease – 14 November 2019
This brief paper supports earlier research relating wine consumption to gut microbiota, and the relation of the latter to obesity and to cardiovascular and other diseases. The authors report that “Red wine consumption was positively associated in a frequency-dependent manner with ɑ-diversity, but even rare consumption showed an effect. White wine also displayed a lesser but suggestive positive association with ɑ-diversity, while we saw no association with other alcohol categories.” They suggested that these effects of red wine on gut microbiota may play a role in the reduced risk of obesity, cardiovascular disease, and reduced total mortality associated with red wine intake that have been demonstrated in many cohort studies.
An increasing number of studies point to beneficial effects of wine, especially red wine, which may not be present for other types of beverages containing alcohol. However, we agree with the conclusions of the authors: “Red wine consumption should always be studied in the context of the overall dietary habits of individuals to take into account residual confounding and bias. The majority of observational studies fail to do this adequately; and thus, results from large scale clinical trials are needed in order to establish a cause and effect relationship between red wine polyphenols and gut microbiota.”
Forum members consider that the present analyses support a beneficial health effect of regular and moderate red wine, but also agree that much further research will be required to work out the complex relation between the consumption of red wine and gut microbiota and the effects on health.
Reference: Le Roy CI, Wells PM, Si J, Raes J, Bell JT, Spector TD. Red wine consumption associated with increased gut microbiota ɑ-diversity in 3 independent cohorts. Gastroenterology 2019. In press, doi.org/10.1053/j.gastro.2019.08.024
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 233: The relation of alcohol consumption to the development of dementia, with very extensive evaluations of the latter – 7 November 2019
This study was designed to assess the association between alcohol consumption and dementia and the roles of mild cognitive impairment (MCI) and apolipoproteinEε4 (APOEE4) genotype in modifying this association. It was based on data from the Ginkgo Evaluation of Memory Study, conducted from 2000 to 2008 among US community-dwelling participants (which did not demonstrate beneficial effects of ginkgo). The study analyzed 3,021 participants aged 72 years and older who were free of dementia at baseline.
The assessment of alcohol consumption included both the amount and frequency of intake, and the authors had a very broad assessment of potential confounders, including cardiovascular and other diseases, depression, race, ethnicity, educational level, social activity, medication use, and genotype for APOE-E4. There was a very complete and careful attention to the assessment of cognitive function, as subjects underwent numerous and repeated cognitive assessments. For example, if there was any suggestion of cognitive impairment, cerebral magnetic resonance imaging and referral to an expert panel of clinicians, who reviewed and validated presence of dementia, was carried out. No previous studies have had such an extensive assessment of cognition.
The main results include a finding that for the large majority of participants (the 2,548 without mild cognitive impairment at baseline), complete abstention from alcohol was associated with a slightly higher risk of dementia than seen in any of the groups consuming alcohol. For 473 subjects with MCI at baseline, there was no effect on risk of dementia for up to about 10 drinks/week, then a slight but insignificant increase in risk with greater intake. Daily low-quantity drinking was associated with more than 50% lower dementia risk than infrequent higher alcohol consumption. Many of the associations shown had a consistent pattern (a decrease in risk with light drinking) but did not reach statistical significance. The association was similar for all sub-groups, and was not modified by APOEE4 genotype.
The analyses seem well done, and Forum members agreed that, while some of the associations did not reach statistical significance, the data support most previous studies that show a J-shaped or U-shaped association for the relation of alcohol consumption to the risk of dementia. As has been shown in most previous studies, regular (even daily) light drinking was found to be preferable to infrequent higher levels of alcohol consumption in terms of the effect on the risk of dementia.
Reference: Koch M, Fitzpatrick AL, Rapp SR, Nahin RL, Williamson JD, Lopez OL, et al. Alcohol Consumption and Risk of Dementia and Cognitive Decline Among Older Adults With or Without Mild Cognitive Impairment. JAMA Network Open 2019:2(9):e1910319. doi: 10.1001/jamanetworkopen.2019.10319
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 232: Does moderate drinking of alcohol in later life reduce the risk of mortality? 3 September 2019
There are well-known problems inherent in most observational studies of alcohol and health. In addition to having to rely on self-report of intake, these include single-time point consumption assessments, inadequate confounder adjustments, accounting for reverse causation, selection bias, short follow up, residual confounding, and lacking information on chronic health conditions that may mediate the association between alcohol consumption and mortality. Further, there have been a lot of assumptions expounded about the generic fragility of older individuals in terms of alcohol consumption; they are generally without supportive clinical or experimental evidence. For light to moderate intake, the elderly tend to have similar benefits associated with alcohol as younger people, and they are at an age when the risk of mortality is at its peak.
The present study was able to adjust for many of these factors: it describes the risk of total mortality among a large group of older subjects, who were ≥ 56 years of age at the start of a 16 year follow up. They were participants in a nationally representative cohort of men and women in the USA, the Health and Retirement Study. Its strengths, in addition to its large size, is the fact that there were repeated assessments of alcohol so that changes of intake could be evaluated, and the authors were able to judge the potential importance of residual confounding.
The authors conclude that occasional drinking and moderate drinking among older subjects are associated with a lower risk of total mortality. The usual argument that light or moderate drinkers tend to have less severe or fewer common diseases and to enjoy better health and socioeconomic status is addressed in this study, which accounted for time-varying confounders that included smoking, body mass index, income, health/functioning, depression, and chronic diseases. From quantitative bias analysis studies they were able to estimate the effects of residual confounding on their results; the authors conclude that it is very unlikely that residual confounding by unrecorded variables would be the cause of the reduction in mortality associated with moderate drinking. Survival analyses supported notably decreased mortality for moderate drinkers. Forum members considered that this study adds important information about the effects on mortality of moderate drinking in the elderly.
Despite many decades of observational data, animal experiments, and limited clinical trials showing beneficial effects on many diseases and mortality from moderate drinking, it is noted that some researchers appear to be loath to admit to any positive health effects of alcohol. We all appreciate the serious adverse effects of heavy drinking and alcohol use disorders, both on the health of persons and on the community. However, when well-done analyses provide reliable data for light-to-moderate drinkers who do not binge drink, it is disturbing that, even then, some scientists question the observed beneficial results and appear to focus only on warnings about abuse.
There is evidence of a disinclination to admit to any beneficial effects of alcohol in many papers, including this one, which throughout the text seems to accentuate the negative aspects of alcohol. Such statements detract from an otherwise clear report suggesting, as one reviewer stated, that this paper is part research results, part polemic. In the opinion of the Forum, this paper provides strong evidence indicating that elderly people who are light-to-moderate drinkers tend to have a lower risk of mortality.
Reference: Keyes KM, Calvo E, Ornstein KA. Rutherford C. Fox MP, Staudinger UM, Fried LP. Alcohol Consumption in Later Life and Mortality in the United States: Results from 9 Waves of the Health and Retirement Study. Alcoholism: Clin Exper Res 2019;43:1734-1746.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 231: Association of alcohol consumption with obesity: Does moderate drinking increase or decrease the risk of obesity? 20 August 2019
While alcoholic beverages contain calories that are absorbed, the association between alcohol intake and body weight and obesity is unclear. Limited clinical trials have not confirmed a positive association between alcohol intake and weight, and some epidemiologic studies, including prospective cohort studies, show that regular moderate drinkers are less likely to be obese than are abstainers.
The present study uses data from National Health and Nutrition surveys between 2011 and 2016 to evaluate the association between reported amount and frequency of alcohol consumption and weight status. An estimated 78.1 % of males and 70.1% of females (who reported at least one drink in the past year) were classified as “drinkers.” A total of about 36% of US males and 41% of US females were described as “obese” (defined as BMI ≥ 30 kg/m2). The analyses included the level of obesity (Class 1, 2, or 3) as outcomes (with Class II defined as BMI 35-<40 kg/m2 and Class III as BMI ≥ 40 kg/m2) making it possible to judge the effects of alcohol on varying levels of obesity.
The present study reports that male current drinkers versus nondrinkers had 38% lower odds of Class 3 obesity versus subjects with a healthy weight; female current drinkers versus nondrinkers had more than 30% lower odds of Class I, Class II, or Class III obesity In both sexes, more frequent alcohol consumption was associated with less obesity, while heavy alcohol consumption was associated with increased risk of obesity. Females who reported that they were trying to lose weight consumed more than others, but there was not a strong relation between reported attempts to lose weight and outcomes.
Forum reviewers considered this to be a well-done analysis, with adjustments for most common potential confounding variables. It provides some support for previous findings of an inverse association with obesity for light-to-moderate alcohol consumption but an increase in obesity for heavy consumption. The authors state that this is the first study to be able to provide data showing that the magnitude of the inverse association is stronger for higher levels of weight status (Classes 1 to 3).
Forum members noted, however, that this study was based on assessments of different subjects in each wave of the national surveys, rather than on repeated assessments among the same individuals over time. It is clear that repeated recordings of alcohol intake in prospective cohort studies make it possible to obtain a reliable estimate of any changes in alcohol intake that may occur, rather than having to base results on a single measure, such as only a baseline value. Further, members caution that there are many genetic and lifestyle variables associated with the development of obesity, and residual confounding is always a potential problem in such analyses. Thus, while the present paper provides data indicating that more severe obesity may result from higher intake of alcohol, and that light-to-moderate intake may actually lead to a decrease in the risk of obesity, data from cohort studies with repeated assessments of alcohol and body size may provide more precise estimates of effect.
Reference: White GE, Mair C, Richardson GA, Courcoulas AP, King WC. Alcohol Use Among U.S. Adults by Weight Status and Weight Loss Attempt: NHANES, 2011−2016. Am J Prev Med 2019;57:220−230.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 230: An extensive review of the role of dietary constituents (foods, nutrients, and beverages) in the development of diabetes 1 August 2019
Of all lifestyle factors that relate to health and disease, probably the most difficult ones to evaluate are dietary factors, including foods, nutrients, and beverages. The present paper consists of a meta-analysis (an “umbrella” analysis) based on 53 previous meta-analyses from prospective cohort observational studies. This analysis includes 153 adjusted summary hazard ratios on dietary behaviors or diet quality indices, food groups and foods, beverages, alcoholic beverages, macronutrients, and micronutrients related to the incidence of type 2 diabetes. Data from previous meta-analyses on very few foods or nutrients are adequate to clearly determine their effects, but among those that have been identified as reducing the risk of diabetes, high-quality evidence was found only for whole grains, cereal fiber, and alcohol. As for dietary factors that have strong evidence of increasing the risk of diabetes, the authors of this paper identify only red meat, processed meat, bacon, and sugar-sweetened beverages.
Forum members considered this to be a well-done, appropriate analysis in a paper that summarizes well the current scientific literature. Some members were concerned about the number of assumptions that scientists must make when doing a simple meta-analysis, and especially when attempting an umbrella one; they consider it key to also evaluate single, large prospective studies where adjustments for many confounding socio-economic factors are less likely to be important.
Overall, the results of this paper strongly support most of the findings of previous meta-analyses and umbrella analyses and indicate only a few dietary factors for which “high-quality” evidence exists for an association with the risk of developing diabetes. The clearest evidence from the analyses in this paper, which was based only on prospective cohort studies, is that cereal grains and moderate alcohol lower the risk, while meats and sugar-sweetened beverages increase the risk of diabetes.
Given the complexity of evaluating dietary factors for their relation to disease outcomes, it will be useful for future studies to attempt to measure a multitude of foods, beverages, nutrients, and eating patterns, preferably over time, to evaluate further the association with disease. For now, current evidence suggests that cereals, grains, and moderate alcohol (that decrease risk) and meat and sugar-sweetened beverages (that increase risk) have the most consistent data for a relation to subsequent diabetes mellitus.
Reference: Neuenschwander M, Ballon A, Weber KS, Norat T, Aune D, Schwingshackl L, Schlesinger S. Role of diet in type 2 diabetes incidence: umbrella review of meta-analyses of prospective observational studies. BMJ 2019;365:l2368.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 229: A J-shaped curve for the relation of alcohol consumption to the risk of colorectal cancer — 10 July 2019
While heavy alcohol consumption is recognized as a contributor to the development of colorectal cancer (CRC), an increasing number of studies suggest that moderate alcohol consumption may not have an adverse effect on the risk of CRC, or even decrease the risk.
The present paper, a meta-analysis of 16 studies on the relation of alcohol consumption to invasive CRC, was conducted by leading investigators in the field. Forum members consider this to be a well-done study, with a large number of subjects, the ability to use individual level data in their meta-analysis, and the use of appropriate and complete analytic techniques.
The key finding of their study was that there was a J-shaped curve evident in all of their analytic approaches; their results strongly support a J-shaped association for the relation of alcohol intake to CRC: a slightly lower risk of cancer for light to moderate drinkers and an increased risk for subjects reporting an average of 3 or more drinks/day. Further, they found that their results did not vary by age, obesity, smoking, or family history of CRC. Overall, the effects of benefits/harms were somewhat more striking for cancers in the distal colon than in the proximal colon.
Potential mechanisms for heavy alcohol consumption being related to an increase in risk were discussed by the authors. As for moderate drinking decreasing the risk, potential mechanisms are discussed by a Forum member in this critique. He describes active, beverage-specific metabolites other than ethanol that reach the intestine. In particular, our attention goes to the several microbial catabolites which can be formed via our host microbiota in the colon.
The finding of a J-shaped curve between alcohol and CRC is similar to the relation seen for a number of other diseases, including coronary artery disease, ischemic stroke, dementia, and total mortality. While a linear relation between heavy drinking and certain upper aero-digestive tract cancers has been shown, for certain cancers there may be a J-shaped curve of effect, with reductions in risk for light-to-moderate drinkers.
Reference: McNabb S, Harrison TA, Albanes, Berndt S, Brenner H, Caan BJ, et al. Meta-analysis of 16 studies of the association of alcohol with colorectal cancer. Int J Cancer. 2019 Apr 29. doi: 10.1002/ijc.32377. [Epub ahead of print]
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
A Tribute to Elizabeth Barrett-Connor, MD (1935-2019)
It is with great sadness that we have learned of the death on 9 June 2019 of Elizabeth Barrett-Connor, a major contributor to the field of epidemiology for many decades and, especially, to a scientifically balanced and sound appraisal of the relation of alcohol consumption to health. Elizabeth was a member of our International Scientific Forum on Alcohol Research until April 2019, when she retired from the Forum because of ill health.
With degrees from Mount Holyoke College in Massachusetts, Cornell University Medical College, and London School of Hygiene and Tropical Medicine, Elizabeth also had medical training at the University of Texas Southwestern Medical School and the University of Miami in Florida. Joining the faculty at the University of California, San Diego, in 1970, she became a Distinguished Professor of Family Medicine and Public Health.
As described in the UCSD Faculty Profile from her university, “Dr. Barrett-Connor’s research concerned healthy aging with a focus on gender differences and women’s health. Dr. Barrett-Connor was founder and director of the Rancho Bernardo Heart and Chronic Disease Study, begun in 1972, with continuous support (4 MERIT awards) from the NIH. She served as a principal investigator of many multicenter clinical trials, including the Postmenopausal Estrogen/Progestin Interventions trial, the Heart and Estrogen-Progestin Replacement Study, the Raloxifene Use in the Heart study, and the Diabetes Prevention Program Observational Study. She was Past President of the Epidemiology Section of the American Public Health Association (APHA), the Epidemiology Council of the American Heart Association (AHA), the Society for Epidemiologic Research (SER), and the American Epidemiological Society (AES). She was a member of the Institute of Medicine (IOM), and a Master of the American College of Physicians (ACP).”
The author of more than 1,000 scientific publications (starting with articles on shigellosis and sickle cell anemia in the 1960s), during her career Dr. Barrett-Connor made important contributions to many fields, including epidemiology, gerontology, endocrinology, cardiology, gender effects, and lifestyle factors such as physical activity, diet, and alcohol consumption. She was the key individual responsible for maintaining and extracting data from the very long-term follow up of participants in the Rancho Bernardo Study of Healthy Aging. She was honored by the American Heart Association by the establishment of the annual Elizabeth Barrett-Connor Competition for young trainees in epidemiology.
Dr. Barrett-Connor was a highly respected mentor of young trainees and faculty. It is noteworthy that she was an author on at least 22 scientific publications during 2018-2019 that included, just in 2019, titles such as “Hearing impairment and cognitive decline in older, community-dwelling adults,” “Effects of APOE on cognitive aging in community-dwelling older adults,” “Genetic Ancestry Markers and Difference in A1c Between African American and White in the Diabetes Prevention Program,” “Cardiovascular Risk Factors Associated With Venous Thromboembolism,” and “Lifetime physical activity and late-life cognitive function: the Rancho Bernardo study.”
The obituary in the New York Times on 20 June 2019 by Karen Weintraub included a revealing anecdote about Elizabeth’s early days: “According to family lore, she was heading to the train station to take a nursing school entrance exam when she bumped into a friend. ‘You’d make a terrible nurse,’ the friend was said to have told her. ‘You can’t take orders from anybody.’ Acknowledging the truth of her friend’s comment, Dr. Barrett-Connor instead applied to medical school.”
Dr. Barrett-Connor was presented with a large number of awards. For example, all in one year she received awards from The University of Western Australia, the Society for the Advancement of Women’s Health Research, the Society for Epidemiologic Research, the Cleveland Clinic Foundation Department of Cardiology, and Scripps Clinic and Research Foundation.
In 2018, Dr. Barrett-Connor was awarded the Fred Conrad Koch Lifetime Achievement Award by the Endocrine Society with the following comments: “Elizabeth Barrett-Connor, MD, has made paradigm-shifting contributions in endocrine physiology and the role of hormones in disease pathogenesis (focus on gender differences) in cardiovascular disease, diabetes, osteoporosis, and breast cancer. It is hard to imagine the existence of any other individual whose work reflects such staggering impact. The hallmarks of Dr. Barrett-Connor’s enduring success — a driving quest for the truth, rigorous scientific discipline, and a joyful passion — have infused every aspect of her career, whether as investigator, lecturer, teacher, or mentor. She has helped make women more visible in the endocrinology field, not by example of her own shining star, but by her constant recognition of light coming from others.”
In a tribute to Dr. Barrett-Connor in Diabetes Care in April, 2019, former trainee and now Professor at the University of Cambridge in the UK, Kay-Tee Khaw noted: “When asked what her motto or philosophy of life was in an interview for her local newspaper, La Jolla Light, Elizabeth Barrett-Connor’s response was that she did not have any one particular philosophy so much as an attitude: ‘My defining principle is that I am a pathological optimist.’ Boundlessly curious, fearless, challenging, inspiring, and great fun to be with are some of the words her colleagues and mentees might use to describe her.”
In addition to her unbelievable contributions to the scientific literature and as a mentor to countless trainees and faculty, Elizabeth was a close friend to many of us in the Forum, who always enjoyed meeting with her at numerous conferences. She especially appreciated the contributions of good food, wine, and vibrant conversation on such occasions.
Among the number of comments received from Forum members were the following: “Dr. Barrett-Connor enjoyed critical debate, not only of scientific topics but also of politics and cultural issues. At a European conference, Elizabeth was one of the outstanding speakers with a talk on nutritional experiences in the US. When a female colleague from Finland was so moved by a certain theme and started crying Elizabeth commented very politely ‘I don`t like weeping women.’ Elizabeth was a strong woman with a lot of empathy and a lot of humour. She has truly been a wonderful and worldwide ambassador for public health and humanity.”
Stated another member: “Elizabeth argued against some of the best, was a clear, linear thinker, and never wavered in self-confidence. She strongly believed in the scientific method, as stated by Popper: ‘The only reason to have a hypothesis is to try to disprove it. If you couldn’t disprove it, you might be right—not guaranteed to be right, but you might be right.’ It teaches us about humility in science; something we need more of.”
We will sorely miss her
================================================================
Critique 227: A reduced risk of chronic obstructive pulmonary disease (COPD) associated with the intake of some alcoholic beverages – 29 May 2019
Chronic obstructive pulmonary disease (COPD) is a major health problem and cause of death throughout the world. While cigarette smoking is known to be the most important risk factor, there are limited data available on the relation of alcohol consumption to the condition. Given that moderate alcohol intake has been shown to decrease the risk of many inflammatory conditions, it may also affect the risk of COPD, which is associated with marked inflammation of lung tissues.
In the present study, the investigators related total alcohol consumption and intake of specific alcoholic beverages with the risk of COPD, based on data from more than 44,000 Swedish men in a population-based prospective cohort study. A total of 2,177 COPD cases were ascertained during follow up that extended up to 17 years. In their analyses, the authors had data permitting them to evaluate a number of demographic and lifestyle factors as potential confounders (including smoking status and pack-years of smoking, education, physical activity, BMI, and some indices of diet). However, there were very few ex-smokers or current smokers among the non-drinkers, making it somewhat difficult to adequate adjust for cigarette use as a cause of COPD.
Forum members thought that there are a number of deficiencies in this study that somewhat weaken its conclusions; especially important was the lack of ability to consider the pattern of drinking (regular, moderate versus binge drinking). Still, there is a strong consistency between the results of this study (indicating a “J-shaped” or “U-shaped” curve for alcohol intake and COPD) and results from extensive previous epidemiologic and experimental research.
Overall, the cumulative research findings now suggest that pulmonary disease might be included among the “diseases of ageing” that show a reduction in risk among moderate consumers of certain alcoholic beverages. Based on some previous epidemiologic studies and results from numerous experimental studies, data now suggest that, in addition to alcohol, the polyphenols present in wine and some beers may offer protection against COPD. While in the present study red wine consumption was associated with the lowest risk of COPD, Forum members acknowledge residual confounding by other lifestyle factors may still play a role.
Reference: Kaluza J, Harris HR, Linden A, Wolk A. Alcohol Consumption and Risk of Chronic Obstructive Pulmonary Disease: A Prospective Cohort Study of Men. Am J Epidemiol 2019;188:907–991.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 226: Consumption of red wine may lower the risk of lethal prostate cancer —- 16 May 2019
In an analysis from the Health Professionals Follow-up Study, the investigators evaluated the relation of alcohol consumption in their more than 45,000 study participants to the development of lethal prostate cancer. They related alcohol first to the overall risk of prostate cancer among all subjects, and then focused on the 5,182 men who developed non-metastatic prostate cancer to judge their risk of developing lethal prostate cancer or mortality. They judged the alcohol intake both prior to the diagnosis and after a diagnosis of prostate cancer. For reported alcohol consumption among subjects prior to the initial diagnosis of prostate cancer, there was a small (16%) but significant reduction in the risk of lethal prostate cancer among subjects reporting any alcohol consumption, but no significant effects of specific beverages on the risk of lethal prostate cancer. However, total mortality was lower for consumers of total alcohol intake and for most categories of intake for all types of beverage.
When they then related post-diagnosis alcohol intake (after the diagnosis of non-metastatic prostate cancer), the investigators found that red wine consumption was associated with a 50% reduction in the risk of developing lethal prostate cancer or mortality. There were no significant relations between total alcohol consumption or between the intake of other specific beverages and lethal disease.
The authors describe a number of hypotheses by which red wine, with its combination of high levels of polyphenols in addition to alcohol, may have lowered the risk of lethal prostate cancer. And there are numerous basic science experiments that have shown how polyphenols impede the development and growth of cancer cells. Presumably, it was not due to the alcohol in red wine, as similar amounts of alcohol in other beverages did not show a protective effect. While the effects of various polyphenols may play a role, at present the mechanisms of such an effect are not known.
Forum reviewers considered this to be a very well-done study and analysis, with repeated assessments of alcohol intake and essentially complete ascertainment of lethal prostate cancer and mortality. Forum members agree with the conclusions of the authors: “Our results indicate that moderate alcohol intake among men with prostate cancer is not associated with a higher risk of progression to lethal disease or overall mortality. The potential benefit of red wine on prostate cancer progression merits additional research.”
Reference: Downer MK, Kenfield SA, Stampfer MJ, Wilson KM, Dickerman BA, Giovannucci, EL, et al. Alcohol Intake and Risk of Lethal Prostate Cancer in the Health Professionals Follow-Up Study abstract. J Clin Oncology 2019 Pre-publication: : DOI https://doi. org/10.1200/JCO.18. 02462
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 225: Moderate alcohol consumption may lower the risk of chronic kidney disease — 8 April 2019
While numerous studies have found that moderate consumers of alcohol tend to be at a lower risk of developing chronic kidney disease (CKD), potential mechanisms for such an effect are unclear. The present large prospective, population-based, multi-cultural study provides important additional data on the effects of alcohol intake on the initial diagnosis of CKD over many years. It is based on data from the Atherosclerosis Risk in Communities Study and reports the relation of varying levels of alcohol consumption, versus non-drinking, to the incidence of CKD over a 24 year follow-up period.
Among the strengths of the study are the very large number of subjects (n=3,664) who developed CKD during follow up, using advanced methods for diagnosing the disease. Only baseline alcohol intake was used as the exposure and type of beverage or pattern of drinking could not be assessed; however, the authors considered multiple appropriate potentially confounding variables in the analyses, including total energy intake, age, sex, race-center, income, education level, health insurance, smoking, and physical activity. In comparison with the 25% of subjects in their analyses who were life-time abstainers, for subjects reporting all levels of alcohol consumption (≤1 drink per week, 2 to 7 drinks per week, 8 to 14 drinks per week, and ≥15 drinks per week), there was a statistically significant decrease in risk of incident CKD (from a 12% decrease in risk for the lowest category of alcohol intake to a 29% decrease for subjects reporting that they consumed 8-14 drinks/week).
The authors conclude: “Consuming a low or moderate amount of alcohol may lower the risk of developing CKD. Therefore, moderate consumption of alcohol may not likely be harmful to the kidneys.” Forum members agree that this study supports much earlier research showing a protective effect of moderate drinking on the risk of kidney disease. While mechanisms are not clear, effects of alcohol on renal vessels that are similar to those described for coronary and cerebrovascular arteries may play a role.
Reference: Hu EA, Lazo M, Rosenberg SD, Grams ME, Steffen LM, Coresh J, Rebholz CM. Alcohol Consumption and Incident Kidney Disease: Results From the Atherosclerosis Risk in Communities Study. J of Renal Nutrition, 2019, in press. DOI: https://doi.org/10.1053/j.jrn.2019.01.011
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 224: A brief summary of the association between wine/alcohol consumption and health in diabetics 12 March 2019
Diabetes mellitus is an increasingly common condition throughout the world, related closely to increases in obesity and ageing of populations. There are many, serious health conditions associated with diabetes, especially a marked increase in the risk of morbidity and mortality from cardiovascular disease. Scientific data from well-done cohort studies have demonstrated for decades that people who are moderate consumers of alcohol tend to have a considerably lower risk of developing diabetes in the first place, and diabetics who consume moderate amounts of alcohol are, in comparison with abstainers, at much lower risk of developing cardiovascular disease.
The present “mini-review” by scientists who have previously carried out the first large randomized clinical trial of wine and health outcomes among diabetics provides an interesting overview of the association of alcohol, particularly of wine, with health. The authors expand the implications of their research and conclude that “Initiating moderate alcohol consumption among well controlled persons with type 2 diabetes is apparently safe, in regard to changes in heart rate variability and carotid plaque formation.” Their findings have stimulated this critique by our Forum to also consider if available data now suggest that physicians should encourage the modest consumption of wine with food for selected patients with diabetes.
Our critique describes a number of risk factors (lipid levels, glucose, insulin, etc.) and intermediate conditions (such as endothelial function and arterial calcification) that have been shown to relate to the consumption of alcohol. Some Forum members believe that while all of these associations are important, the key information needed is the effect of alcohol consumption on disease outcomes themselves (coronary heart disease, stroke, dementia, etc.) and on mortality. At present, any recommendations regarding alcohol consumption must be based primarily on observational data from long-term cohort studies.
The key question we discuss in this critique is “Should physicians advise their older diabetic patients who are non-drinkers to begin to consume small amounts of an alcoholic beverage?” The consensus of Forum members is that current data suggest that, at a minimum, we should not advise such patients who currently consume alcohol moderately to stop their consumption. On the other hand, most members emphasize that we should discuss alcohol consumption with all patients. If they are at least occasional consumers of alcohol (the large majority of patients in most Western countries), our only advice might relate to the pattern of drinking. At present, the pattern commonly shown to be associated with the lowest risk of the usual diseases of ageing and mortality appears to be small amounts of alcohol, especially wine, with meals on a regular basis. For patients who indicate that they are drinking only in binges, we should emphasize the adverse health effects (for them as well as for society), and encourage a healthier pattern of drinking.
But what about current non-drinkers? For middle-aged or older non-drinkers who avoid alcohol because of religious prohibitions, previous misuse of alcohol, certain medical conditions, or a stated dislike of alcohol, our advice on prevention of disease should focus on not smoking, getting exercise, eating a healthy diet, and trying to avoid obesity. But for patients without such conditions that would indicate that they should avoid alcohol, many Forum members believe that they should at least be told of the current scientific evidence of possible beneficial health effects of regular, moderate intake. However, until considerably more data on its effects are available, we are not encouraging physicians to prescribe alcohol consumption for their diabetic patients.
Reference: Golan R, Gepner Y, Shai I. Wine and Health–New Evidence. Mini Review. European Journal of Clinical Nutrition. https://doi.org/10.1038/s41430-018-0309-5; 2019: in press.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 223: A new major review of the relation of alcohol consumption to the risk of dementia. 17 January 2019
While many studies have shown that excessive alcohol intake is associated with cognitive impairment and increased risk of dementia, most cohort studies have shown that the risks of these outcomes are lower among light-to-moderate drinkers than among abstainers. The authors of this paper conducted a scoping review on this topic, based on a systematic search of systematic reviews published from January 2000 to October 2017. A total of 28 systematic reviews were identified relating alcohol intake at various time periods to incidence of cognitive impairment/dementia, specific brain functions, or induced dementias. The authors report that light to moderate alcohol use in middle to late adulthood was associated with a decreased risk of cognitive impairment and dementia, but heavy alcohol use was associated with changes in brain structures, cognitive impairments, and an increased risk of all types of dementia.
Forum members considered this to be a well-done analysis, but were concerned that the focus was only on the potentially adverse effects of heavy drinking, with little regard or discussion of the findings of protection against such cognitive outcomes among light or moderate drinkers. Forum members point out that there are very many adverse health effects, both for the drinker and for society, resulting from heavy drinking. To them, the most interesting and provocative aspect of this paper was the conclusion of a protective effect against cognitive decline and dementia associated with light-to-moderate alcohol consumption.
Scientific data, including the results of the present systematic analysis, are very consistent in showing that cognitive decline, associated impairments in the functions of daily living, incident dementia, and survival are all associated favorably with light-to-moderate consumption of alcohol in middle age. The reasons and mechanisms that lead to these associations deserve further evaluation. With the increasing ageing of populations throughout the world, cognitive decline and dementia are expected to increase and create serious challenges for health care providers. Insight into ways of preventing or delaying the onset of such cognitive decline (in addition to decreasing the prevalence of heavy alcohol intake, the focus of this paper) could be extremely important in planning for the future.
Reference: Rehm J, Hasan OSM, Black SE, Shield KD, Schwarzinger M. Alcohol use and dementia: a systematic scoping review. Alzheimer’s Research & Therapy 2019; 11: pre-publication. https://doi.org/10.1186/s13195-018-0453-0
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 222. A new analysis relating alcohol intake to coronary heart disease – 20 December 2018
In an attempt to judge the effects of alcohol on the risk of coronary heart disease (CHD), the authors have carried out analyses using a sample of subjects from the National Epidemiologic Survey on Alcohol and Related Conditions III (NESARC-III). They based their exposure to current alcohol use on a single assessment at baseline of self-reported consumption during the past year, when the subjects were an average of 38.9 years of age. In addition they asked subjects if they had consumed larger amounts of alcohol when they were younger.
Their assessment of CHD was based on answers to questions at baseline as to having been told by a doctor that they had chest pain or CHD, apparently within the same 12-month period when they were asked about current alcohol consumption. Nothing in the paper indicates that the authors had data on the subsequent development of CHD during a follow-up period. When relating reported alcohol intake to CHD, they excluded 1,671 who reported “previous CHD,” although for this relatively young group it is questionable how many actually had CHD, as no data on validation of the diagnosis was done. For unclear reasons, for their comparison group they excluded any subjects with conditions that “may increase the risk of CHD (e.g., pneumonia, influenza, tuberculosis, liver disease, neurologic conditions, osteoporosis, arthritis, STD) and can be viewed as comorbid conditions related to alcohol consumption.”
Given that the exposure (alcohol) and outcome (CHD) were apparently from the same time period, there is reason to worry about reverse causation (i.e., subjects may have developed CHD and changed, either decreased or increased, their alcohol consumption during the same period).. As for using the self-reported amount of alcohol consumed at some time in the past as the exposure, there is a large chance of serious misclassification of exposure due to recall bias and bias according to current alcohol intake (as subjects currently reporting greater amounts of alcohol were more likely to report even higher intake in the past).
With only a single assessment of current alcohol intake, an inadequate assessment of long-term alcohol intake, a lack of data during a follow-up period for the main outcome, CHD, and no validation of the outcome, Forum members considered that this was an unusual cohort to use when attempting to judge the relation of changes in alcohol consumption to the development of CHD. The necessary elements for a useful analysis were not available to these investigators using this population sample.
In any case, results from many well-done long-term cohort studies with repeated assessments of alcohol and validated CHD outcomes during follow up have already provided key data on this topic: they almost uniformly demonstrate that light-to-moderate drinkers who do not binge drink have significantly lower risk of developing CHD. The present analysis does not provide data that would question such findings.
Reference: Fan AZ, Ruan WJ, Chou SP. Re-examining the relationship between alcohol consumption and coronary heart disease with a new lens. Pre-publication. Preventive Medicine 2019;118:336=343.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 221: The relation of alcohol intake to stomach cancer – 20 November 2018
There have been conflicting results from studies of the association between alcohol intake and the risk of gastric cancer. Some of the differences among studies have related to mixing subjects from Western countries with those from Asia, where dietary patterns, lifestyle factors, drinking patterns, and types of alcohol consumed differ from those among Western populations. Results usually differ between Asian and Western populations.
The present study is based on almost 500,000 subjects from the USA with follow up for a median of 15.5 years. The investigators identified a total of more than 1,300 cases of gastric cardia cancer (GCA) or gastric noncardia cancer (GNCA ). The authors report: “We found no association between higher alcohol consumption and GCA or GNCA, when examined as total alcoholic beverage intake or individual beverage types of beer, wine and liquor. Furthermore, we observed no association by stratum of sex, ethnic group, educational level or smoking status. We did, however, observe lower risk of GNCA among participants who drank up to one drink per day (HR = 0.81, 95% CI: 0.67–0.97) compared to nondrinkers.” They conclude: “Alcohol consumption was not associated with increased risk of GCA or GNCA in this large U.S. cohort.”
Forum members considered this to be a large, very well-done analysis; subjects were aged 50-71 years at baseline, appropriate for evaluating the risk of gastric cancer. Data on a large number of potential confounders were included in the analysis. Diagnosis of cancer was from state cancer registries, shown to be very accurate. The statistical analyses included restricted spine analysis to test for a dose-response curve (not found), and excluded the first two years after alcohol assessment to lower the risk of reverse causality. Further beverage-specific analyses were carried out, and did not show differences according to whether the consumption was of beer, wine, or spirits.
Weaknesses included only one assessment of alcohol intake, at baseline, and no data on binge drinking or other aspects of the pattern of drinking. Subjects were generally well-educated, white, and consumed alcohol moderately (75% reported one drink or less). Thus, these results may not pertain to other ethnic groups or to heavier consumers of alcohol.
Overall, these results provide further support for the lack of an association between light-to-moderate alcohol intake and the risk of gastric cancer. The significant decrease in risk of gastric non-cardia cancer associated with consumption of up to one drink/day should obviously be replicated, but the authors provide some potential mechanisms that could explain such a phenomenon. The study did not support previous data suggesting that wine consumption might have additional benefits to those of other beverages in terms of cancer risk.
Reference: Wang SM, Freedman ND, Loftfield E, Hua X, Abn CC. Alcohol consumption and risk of gastric cardia adenocarcinoma and gastric noncardia adenocarcinoma: A 16-year prospective analysis from the NIH-AARP diet and health cohort. Int J Cancer 2018; pre-publication.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 220: An unusual analysis relating alcohol intake to mortality – October 16, 2018
The authors of this treatise on alcohol consumption and mortality combined, for an unclear reason, results from two, very different studies: one from the Veterans’ Health Administration, based on outpatient clinical medical records, and the other from a national survey in the USA [The National Health Interview Survey (NHIS)]. Unfortunately, the VA data did not adjust for tobacco use or other important lifestyle habits, and are not useful in judging the effects of alcohol consumption on mortality.
While the NHIS survey included data on potential confounding, both it and the VA study based their analyses on a single estimate of alcohol consumption. The authors then created a variable that they stated was associated with the lowest risk of mortality and compared results from such alcohol intake with data from subjects reporting less or more alcohol. They combined data on all subjects reporting 1 to 2 drinks/week, so did not have the ability to provide a precise estimate of the association between low levels of intake and mortality risk. They did not comment on the effects that under-reporting of alcohol would have on their studies (and most investigators agree that the self-reported level of alcohol consumption is usually an under-estimate of actual consumption). Further, they did not point out the very much higher risk of mortality of non-drinkers, compared with moderate drinkers, demonstrated in their data.
To the extent that people accurately reported their past drinking status (never vs former), this study should put to rest concerns that protective associations of drinking versus non-drinking arise from inclusion of former drinkers into non-drinking groups. Never drinkers had higher risk of mortality than former drinkers in this study.
There are considerable data from many well-done cohort studies that have repeated assessments of alcohol intake over many decades and the subsequent risk of mortality. Such studies provide very clear and consistent results indicating a J-shaped curve: lower risk of mortality for light and moderate drinkers than for non-drinkers (even lifetime abstainers) and some increase in risk for heavy drinkers. These are the studies that can provide reliable information upon which drinking guidelines for different individuals and populations can be based.
Reference: Hartz SM, Oehlert M, Horton AC, Grucza RA, Fisher SL, et al. Daily Drinking Is Associated with Increased Mortality. Alcoholism: Clin & Experimental Research 2018; pre-publication. DOI: 10.1111/acer.13886.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 219: A global overview of alcohol consumption and health – 3 September 2018
Investigators working with data from the Global Burden of Diseases, Injuries, and Risk Factors Study 2016 have combined data from 195 locations around the world, from 1990 to 2016, for both sexes and for 5-year age groups between the ages of 15 years and 95 years and older. Their purpose was to determine how estimates of the prevalence of current drinking, abstention, the distribution of alcohol consumption among current drinkers in standard drinks daily (defined as 10 g of pure ethyl alcohol) relate to alcohol-attributable deaths and disability-adjusted lifeyears (DALYs). The paper does not present estimates of the effects of alcohol on a key outcome, total mortality.
The paper presents a huge number of analyses with data specific for each contributing center. However, the Forum considers that real problems emerge when they attempt to combine data from many divergent cultures to determine a single association between alcohol consumption and health. Many lifestyle and cultural factors strongly modify the relation of a given amount of alcohol to health and diseases. Such modifying factors include especially the socio-economic status of the individual, circumstances such as drinking with or without food, the pattern of drinking (regular moderate versus binge drinking), the type of beverage (e.g., wine versus spirits), the intention of the individual (drinking to get drunk versus drinking to enhance meals), level of physical activity, etc. When such modifying factors are not taken into consideration, the estimated intake of a given amount of alcohol (even if accurate), provides an incomplete assessment of the effects of alcohol on health.
The authors spend much of their paper focusing on their contention that these analyses have large implications for setting alcohol policy around the world. They then expand primarily on ways of decreasing alcohol intake world-wide through changes in guidelines. However, their failure to consider specifics of the culture for which the policy is being formulated, such as evaluating other lifestyle factors, the pattern of drinking, underreporting of alcohol intake, cultural factors, etc., negates their ability to provide useful information that is applicable to any single population: their guidelines end up applying to no one. And, their specific statement that zero consumption would be preferable everywhere is sharply contradicted by consistent reports from very large, well-done cohort studies (where individual data are available) which indicate that non-drinkers have higher risks of cardiovascular disease and total mortality than regular moderate drinkers who do not binge drink.
Setting guidelines for the public regarding alcohol consumption requires information not only on the reported intake but on other health conditions, as well as genetic, lifestyle, and cultural factors that may modify the effects of alcohol. Further, advice differs by age and the key problems within a country that the guidelines are directed toward improving. In the opinion of the Forum, despite the massive amount of work done by the investigators in the preparation of this paper, the overall combined results from such divergent populations have little applicability in setting guidelines that would lead to avoidance of alcohol abuse in any specific group of people around the world — they apply to no specific population.
Reference: GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. www.thelancet.com Published online August 23, 2018 http://dx.doi.org/10.1016/S0140-6736(18)31310-2
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here
================================================================
Critique 218: Long-term study of alcohol intake and the risk of Alzheimer Disease or other types of dementia – 21 August 2018
While there is general agreement that the moderate intake of alcohol is associated with a significantly lower risk of cardiovascular disease, there are less data on the relation of moderate alcohol consumption to dementia. However, the vast majority of well-done prospective studies indicate that, in comparison with non-drinkers, moderate, non-binge-drinking older adults have lower risk of Alzheimer Disease and other types of dementia. The present study provides important information on this association by monitoring for the development of dementia among subjects in a large cohort of British civil servants (the Whitehall Study) over more than two decades; there were repeated assessments of alcohol consumption.
The main results indicate that abstinence in middle life is associated with a significantly higher risk of dementia than the risk among moderate drinkers, while subjects reporting the intake of larger amounts of alcohol or evidence of an alcohol use disorder are at increased risk of dementia. Specifically, the study shows that among the 397 cases of dementia that were recorded over a mean follow up of 23 years, abstinence in midlife was associated with a 47% higher risk of dementia compared with consumption of 1-14 units/week (a British unit is the equivalent of 8 grams of alcohol). There was a 17% increase in risk of dementia for those reporting more than 14 units/week. With repeated assessments of alcohol the authors also calculated trajectories of alcohol consumption from midlife to early old age, with continued abstinence being associated with an increase in dementia of 74% and a decrease in consumption with an increase of 55% in comparison with subjects reporting continued moderate consumption. In several analyses, wine consumption was associated with more favorable effects than those of other beverages.
Forum members thought that this was a well-done analysis, but considered that the data presented do not allow for a firm determination of a cut-point for increased risk of dementia from alcohol intake. While the authors provide estimates of a linear increase in dementia risk for subjects reporting more than 14 units/week or reporting evidence of alcohol abuse, they do not give data that permits an estimate of the level of intake where the risk of dementia exceeds that of non-drinkers.
Overall, the results showing a decreased risk of dementia for moderate drinkers support the findings from most well-done prospective cohort studies. As for implications for policy, the study further shows that, in terms of the risk of dementia as well as cardiovascular disease, middle-aged and older individuals who are consuming alcohol moderately and without binge drinking should not be advised to stop drinking.
Reference: Sabia S, Fayosse A, Dumurgier J, Dugravot A, Akbaraly T, Britton A, Kivimäki M, Singh-Manoux A. Alcohol consumption and risk of dementia: 23 year follow-up of Whitehall II cohort study. BMJ 2018;362:k2927. http://dx.doi.org/10.1136/bmj.k2927
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================
Critique 217: Alcohol, cancer, and mortality: Further affirmation of the J-shaped curve for mortality and increase in incidence of cancer with larger intake of alcohol – 9 July 2018
Scientific studies have shown consistently that that the consumption of small amounts of alcohol on a regular basis is associated with a lower risk of total mortality, while consumption of large amounts is associated with an increased risk of certain cancers and mortality. The present report is from a population-based cohort study of almost 100,000 older subjects who were followed for a median of 8.9 years. There were large numbers of deaths (n=9,599) and incident cancers (n=12,763) diagnosed during follow up, which should lead to more precise estimates of effect.
The authors report that light-to-moderate drinking was associated with lower total mortality, but the risk of incident cancer increased with greater alcohol consumption, especially the intake of beer or spirits. However, the analyses indicate that the slightly increased risk of cancer associated with moderate alcohol consumption was less than the beneficial effect on mortality.
Specifically, in comparison with never drinkers or very light (< 1 drink/week) drinkers, the study shows lower mortality for “light-to-moderate” alcohol consumers (up to 2 drinks/day) but greater mortality among subjects classified as “heavy” (2 to < 3) or “very heavy” (3+ drinks/day) consumers. In beverage-specific analyses, there was a slight increase in total mortality for reported intake of spirits starting at the consumption of about 1 ½ drinks/day and for beer at or above about 2 drinks/day; no significant increase in cancer risk was associated with wine consumption, regardless of the amount. The authors conclude that “there is a J-shaped association between alcohol and mortality in older adults, which remains after adjustment for cancer risk.”
Forum member considered this to be a well-done analysis, and shows, essentially for the first time in a single study, how the beneficial effects of light and moderate drinking on cardiovascular disease and total mortality exceed the slight increase in cancer risk for alcohol consumption at this level. In other words, while even light-to-moderate drinking may be associated with a slight increase in the risk of certain cancers, such drinking still favorably affects the overall risk of mortality.
Reference: Kunzmann AT, Coleman HG, Huang W-Y, Berndt SI. The association of lifetime alcohol use with mortality and cancer risk in older adults: A cohort study. PLoS Med 2018;15:e1002585. https://doi.org/10.1371/journal.pmed.1002585.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================
Critique 216: Strong effects of five lifestyle factors on risk of mortality and longevity of life – 31 May 2018
It has long been known that a number of lifestyle factors – such as not smoking, being physically active, avoiding obesity – decrease the risk of many of the “diseases of ageing,” especially cardiovascular disease and cancer. The present paper from the Nurses’ Health Study and the Health Professionals Follow-up Study is especially important as it demonstrates the joint effects of five healthy factors on disease-specific and total mortality in very large cohorts of subjects. The “healthy lifestyle factors” evaluated were (1) never smoking, (2) body mass index of 18.5 to 24.9 kg/m2, (3) ≥30 min/d of moderate to vigorous physical activity, (4) moderate alcohol intake, and (5) a high diet quality score (upper 40%). The similarity in education and other socio-economic factors of the subjects in these studies tends to reduce potential confounding by such factors.
There were more than 42,000 deaths in their cohorts during follow-up periods extending up to 34 years. The effects of these factors on subsequent risk of mortality were striking: for subjects meeting criteria for all five factors versus none, there was an 84% reduction in all-cause mortality, 65% less cancer mortality, and 82% less cardiovascular disease mortality. The overall effect was associated with 12 to 14 additional years of life after age 50 for subjects meeting criteria for all five factors.
Forum members consider this to be an excellent study, as it was based on data from very large cohorts of well-monitored subjects over many decades, with essentially full ascertainment of mortality. This study strongly suggests that the leading causes of premature death throughout the developed world are, to a large extent, preventable.
Reference: Li Y, Pan A, Wang DD, Liu X, Dhana K, Franco OH, Kaptoge S, Di Angelantonio E, Stampfer M, Willett WC. Hu FB. Impact of Healthy Lifestyle Factors on Life Expectancies in the US Population. Circulation 2018;137:00–00. (Pre-publication). DOI: 10.1161/CIRCULATIONAHA.117.032047.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 215: Long-term effects of smoking and moderate drinking on the quality and longevity of life of elderly women — 9 May 2018
While essentially all epidemiologic studies have shown adverse health effects of cigarette smoking and beneficial effects of moderate alcohol consumption, the present study is important as it follows a cohort of elderly women into very old age. It is a prospective cohort study of 9,704 women at least 65 years of age, who were living independently at baseline and were not heavy drinkers; they had a mean baseline age of 71.7 years (range 65-99) and underwent repeated assessments of lifestyle habits starting in 1986 to 1988. They were followed longitudinally until death, loss to follow-up, or to April, 2016. Outcomes included grip strength, walking speed, prevalence of threshold scores for self-reported health, difficulty with three or more instrumental activities of daily living (IADLs), depression, prevalence of falls, living in a nursing home, and death after 10- or 20-year follow up. The main comparisons evaluated in this study were between women who were smokers and those who consumed alcohol moderately, with each analysis adjusted for the other exposure.
Forum members considered this to be a well-done study that provides some important data relating effects of smoking and moderate drinking on function and mortality in very elderly subjects (an age group where data are lacking). There were criticisms that the study does not report the effects of moderate drinking among smokers; previous studies have shown that the adverse effect of smoking is modified by moderate alcohol intake. Further, given that the reasons why some women quit drinking during follow up are not known, the article does not contribute to clarification of the problem of reverse causation (e.g., healthier women may tend to continue drinking whereas sicker women stop alcohol consumption). Also, the authors did not adjust for some strong confounders, especially those related to socio-economic status (SES).
Nevertheless, the results of this study make a real contribution to our knowledge of the effects of drinking on both quality of life and mortality among women who are 65 years or older. The follow up of subjects continued for a least 20 years, by which time almost 70% of the women had died. Hence, the effects on mortality should be excellent estimates. As expected, women who were smokers had greater risk for almost all adverse outcomes, while drinkers who continued to consume moderate alcohol into old age had the most favorable outcomes. While the authors report that women who reported drinking at baseline but quit later on had mortality risks that were intermediate between non-drinkers and persistent drinkers, the reasons why some women quit drinking were not known. Hence, it is appreciated that continued drinking could be only a marker of better health, and not the cause.
Reference: Nelson HD, Lui L, Ensrud K, Cummings SR, Cauley JA, Hillier TA. Associations of Smoking, Moderate Alcohol Use, and Function: A 20-Year Cohort Study of Older Women. Gerontology & Geriatric Medicine 2018;4:1–9. Pre-publication.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 214: Some methodologic problems in a recent paper urging changes in drinking guidelines – 23 April 2018
Using individual-participant data from a number of large studies, predominantly from the UK and other European countries, the authors of the present paper have estimated the association between the reported level of alcohol intake among drinkers with cardiovascular outcomes and mortality. They conclude that the lowest risk of these outcomes is from the intake of less than 100 g of alcohol per week, and that guidelines for the public should reduce the upper limits for the amount of alcohol that could be safely consumed.
Forum members identified a number of flaws in these analyses, including failure to separate advice for men versus women or for older adults versus young people. Further, the authors do not point out the effects of under-reporting of intake, the marked differences in many health effects according to type of alcoholic beverage (such differences are shown only in their supplement but not mentioned in the abstract); also, there is little discussion of the importance of the pattern of drinking on health results.
Most important, by excluding never-drinkers as a reference group in their main analyses, the authors essentially eliminated the ability to evaluate for any potentially beneficial (or adverse) effects of light-to-moderate drinking as compared with non-drinking. This is problematic, as in essentially all previous large studies, moderate drinkers are those for whom significant and large benefits have been reported for risk of cardiovascular disease and total mortality.
Guidelines for the public regarding alcohol intake relate to many factors, including the net overall physiologic effects on health as well as the particular needs of different countries and cultures. And, as in this study, the inclusion of results from so many different cultures is a problem for determining appropriate guidelines for alcohol intake. Given that culturally specific drinking patterns, type of beverage, and many other lifestyle factors modify the health effects of alcohol, mixing data from markedly different cultures may give results that may not be appropriate for any specific population.
Reference: Wood AM, Kaptoge S, Butterworth AS . . . John Danesh, et al, for the Emerging Risk Factors Collaboration/EPIC-CVD/UK Biobank Alcohol Study Group (120 authors). Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet 2018;391:1513-1523.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 213: A meta-analysis on lifestyle factors, cardiovascular disease, and total mortality for a very large number of middle-aged and elderly women – 27 March 2018
Overall, Forum members considered this to be a well-done paper that provides additional information on alcohol’s effects on CVD and mortality among a very large number of middle-aged or elderly women. Although women markedly increase their risk of CVD following menopause, this is a group of women for whom data are sparse. Weaknesses of the analysis include a lack of information on the pattern of drinking (binge versus regular), type of beverage, and drinking alcohol with or without food. It is of note that in some of the studies included in the meta-analysis, factors such as HDL-cholesterol and fibrinogen were adjusted for in the study; given that these are mechanisms of alcohol’s effects, overall results will surely underestimate the effects. Further, as the authors point out, this study provides little information on the physiologic mechanisms of alcohol’s effects on health.
Forum members praised the authors for this meta-analysis of a very large dataset. It strengthens previous analyses that show that each of the lifestyle factors considered – not smoking, not becoming obese, being physically active, and regularly consuming small to moderate amounts of alcohol – benefit health. The more healthy lifestyle factors a subject has, the greater the benefit.
It will be especially important that future research evaluates what happens if subjects change their lifestyle habits, as such results would help target specific behavioral changes. There are very limited data available on this at present, but such studies that have been done suggest that the onset of moderate drinking among non-drinkers, or a slight increase in alcohol consumption among light drinkers, have beneficial effects on health. Still, it is appreciated that moderate alcohol consumption is only one of a number of factors making up a “healthy lifestyle,” which is clearly associated with less cardiovascular and other diseases and a much lower risk of mortality.
Reference: Colpani V, Baena CP, Jaspers L, van Dijk GM, Farajzadegan Z, Dhana K, Tielemans MJ, Voortman T, Freak-Poli R, Veloso GGV, Chowdhury R, Kavousi M, Muka T. Franco OH. Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: a systematic review and metaanalysis. European Journal of Epidemiology 2018; pre-publication. https://doi.org/10.1007/s10654-018-0374-z
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 212: Is it the alcohol or other substances in wine that lead to beneficial health effects? — 15 March 2018
While epidemiologists have long noted that consumers of wine tend to have better health outcomes than consumers of other alcoholic beverages, it has always been of concern that we were comparing drinkers, and not the drink itself. In recent years, many basic scientists have evaluated the non-alcoholic constituents in wine, and most studies show beneficial health effects from polyphenols and other components in wine as well as beneficial health effects from the alcohol in wine.
The present study provides an excellent review of clinical trials that compared the effects of wine versus no intervention or versus the effects of other alcoholic beverages. The specified outcomes related to effects on lipids, glucose/insulin metabolism, hemostatic mechanisms, and inflammatory/endothelial systems. The authors conclude that “The most repeated result of wine consumption is on lipid metabolism, attributed mainly to ethanol, while wine micro-constituents seem to have an important role mainly in haemostatic and inflammatory/endothelial systems.” Forum members cite several other important effects of wine micro-constituents, including demonstrated effects of such components at the cellular, molecular, and gene levels to sustain increased fibrinolytic activity, which is closely related to the development of cardiovascular disease.
Forum members were unanimous is considering that this was an excellent review of human clinical trials on the topic; the paper does not, however, comment on the mechanisms by which micro-constituents may operate to improve health. Given that since virtually none of the wine micro-constituents circulates in the human biofluids in their native form, it is especially important that the catabolites of wine micro-constituents be better defined and evaluated.
Overall, current data indicate that wine may be especially effective in lowering the risk of cardiovascular disease not only through the alcohol it contains, but also from a number of its key polyphenols. Forum members also point out that, for beneficial health effects of any type of alcoholic beverage, the pattern of drinking is especially important: the consumption of small or moderate amounts on a regular basis, and preferably with food.
Reference: Fragopoulou E, Cholevaa M, Antonopoulou S, Demopoulos CA. Wine and its metabolic effects. A comprehensive review of clinical trials. Metabolism Clinical and Experimental 2018;83:102-119.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 211: Effects of alcohol and aldehydes on DNA and risk of cancer; potential implications from a study in mice — 22 January 2018
The authors of this paper, based on an extensive basic scientific experiment in mice, describe the features and mutational landscape of DNA damage caused by acetaldehyde, an endogenous and alcohol-derived metabolite. This damage results in DNA double-stranded breaks that, despite stimulating recombination repair, also cause chromosome rearrangements. Furthermore, the authors identify how the choice of DNA-repair pathway and a stringent p53 response limit the transmission of aldehyde-induced mutations in stem cells.
Forum members considered this to be a well-done series of experiments that add additional data on the effects of aldehyde on cellular damage, which could potentially lead to an increased risk of cancer. While interesting, these results in mice have limited applicability to the effects of alcohol in humans, as the study conditions do not correspond to that found in real life. For example, the levels of ethanol used to elicit the DNA changes were high and alcohol was directly injected into the animals, whereas in humans alcohol is orally absorbed and undergoes several types of metabolism that reduce maximum blood alcohol concentrations achieved. Further, the animal model was based on mice that had been genetically manipulated in that particular genes had been selectively ‘knocked out’ to make them unable to metabolize aldehyde or to repair DNA damage; while this was necessary to study the effects in a basic scientific experiment, it is in contrast to what would occur under non-manipulated conditions of alcohol consumption in humans
The damages shown in this experiment were to hematologic cells, and epidemiologic studies have generally not found an increase in the risk of hematologic cancers in humans to be associated with alcohol, especially from the moderate intake of alcohol (and many studies show instead a decrease in risk among drinkers). Thus, studies in humans have not provided support for these reported results from mice. Further, Forum members conclude that the polyphenols that are present in wine may play an important role in blocking a carcinogenic effect associated with alcohol intake.
Reference: Garaycoechea JI, Crossan GP, Langevin F, Mulderrig L, Louzada S, Yang F, Guilbaud G, Park N, Roerink S, Nik-Zainal S, Stratton MR, Patel1 KJ. Alcohol and endogenous aldehydes damage chromosomes and mature stem cells. Nature 2017;553:171-177. doi:10.1038/nature25154.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 210: Beer, wine, and spirits consumption and risk of gastric cancer – 8 January 2018
While heavy alcohol intake has been regularly found to increase the risk of upper aero-digestive tract (UADT) cancers (mouth, tongue, pharynx, larynx, etc.), results are less clear for gastric cancer. The present study is notable because it is based on a large number of subjects, uses appropriate analytic methods, and provides dose-dependent results according to type of beverage.
For total alcohol, the dose-response results in this meta-analysis show a curvilinear relation between alcohol intake and gastric cancer, with a minimal (4%) but significant increase per typical drink (12.5 g/alcohol). However, there were varying responses for different beverages. In beverage-specific analyses, for beer, a non-linear relation was found with a significant increase of 7%/drink (CI 1.01, 1.13); for liquor, there was a linear association, with RR=1.03 (CI 0.98, 109); and for wine, the RR was 0.99 (CI 0.93, 1.06).
While the authors show a figure of the dose-response curves for each beverage using a non-linear approach, they do not provide the specific values in a table or in the text; this makes it difficult to clearly determine threshold effects of beverages. The figures suggest that the risk associated with beer consumption shows a slight decrease for 1 to 2 drinks/day, then an increase; for spirits, no decrease with lighter intake is seen; for wine, the curve is continuously downward. The authors do state that “light, moderate, and wine drinking would not increase gastric cancer risk,” so it is presumed that significant increased risk was not noted for moderate drinking for any specific beverage when non-linear effects were evaluated. Thus, overall, it appears that this large meta-analysis shows no significant increases in risk for light to moderate consumption of an alcoholic beverage, but a slight increase in risk associated with greater intake of beer and spirits. For wine, no increase in the risk of gastric cancer was seen for any level of consumption.
In a number of sensitivity analyses, the authors found tendencies for a lower gastric cancer risk associated with alcohol for cohort versus case-control studies, for studies with larger numbers of subjects, for studies judged to be of higher quality, and for studies adjusting for confounding by SES & income; these types of studies would be expected to yield more precise estimates of effect. These results led the authors to state these sensitivity analyses “ . . . indicate that our results may be exaggerated to some degree, but it should be noted that the pooled risk estimates of high-quality studies yielded similar results to the original analysis.”
Overall, Forum members considered this to be a well-done analysis, and the data support an increase in gastric cancer risk for heavier drinking (of beer or spirits) but no significant effects for light or moderate drinking of any alcoholic beverage. Forum members considered that if the lack of increase in cancer risk from wine consumption seen in this analysis proves to be true, it might relate to the polyphenols in wine that block any adverse effects of alcohol on gastric cancer risk.
Reference: Wang P-L, Xiao F-T, Gong B-C, Liu F-N. Alcohol drinking and gastric cancer risk: a meta-analysis of observational studies. Oncotarget 2017;8:99013-99023.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 209: Does alcohol intake increase the risk of obesity? — 13 December 2017
The public, and scientists, have long been concerned about the relation between alcohol consumption and weight gain, as all alcoholic beverages contain calories. However, most epidemiologic studies do not find that light or moderate drinkers weigh more than their abstaining peers, and some even show lower weight among moderate drinkers than among abstainers. The reasons for this apparent effect are unclear.
The present study is important as it describes the effects on weight of changes in alcohol intake over repeated 4-year periods among a large cohort of health professionals, followed for 24 years. They found very slight increases in weight (mostly less than one-half pound over a four-year period) for subjects consuming alcoholic beverages; these were statistically significant for regular beer and liquor, but not for wine or light-beer. Overall, the largest increases in weight (still, only an increase of 0.6 pounds) were seen for subjects increasing their alcohol by an average of 2 or more drinks/day. For subjects decreasing their alcohol intake over the periods, there was a slight decrease in weight, still only about one-half pound or less.
The investigators conclude that any effects of drinking on weight are very minor, and probably of no clinical significance. While effects on weight gain were slightly lower among consumers of wine and light beer than for those consuming regular beer or spirits, the differences were not large. The study does not present data on the mechanisms of such associations.
Forum members considered this to be a very well-done analysis of repeatedly collected exposure and outcome data among health professionals over an extended period of time. Adjustments were made for known potential confounders associated with changes in weight and appropriate sensitivity analyses were done. While the paper indicates that calories from alcohol are metabolized similarly to those from other foods and do affect weight change, the changes associated with moderate alcohol intake appear to be very minor and would be expected to have very little effect on the development of obesity.
Reference: Downer MK, Bertoia ML, Mukamal KJ, Rimm EB, Stampfer MJ. Change in Alcohol Intake in Relation to Weight Change in a Cohort of US Men with 24 Years of Follow-Up. Obesity 2017;25:1988-1996. doi:10.1002/oby.21979
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 208: A statement on alcohol and cancer that ignores the net health effects of moderate drinking, such as increasing longevity of life — 16 November 2017
The present publication is an attempt by the American Society of Clinical Oncology to describe the relation between alcohol consumption and cancer, including the effects on the risk of developing cancer and effects among subjects currently being treated for cancer. It came to the conclusion that there is a need for the public to be warned about the use of alcohol because of its effects on cancer, and describes numerous approaches for decreasing alcohol use in the population.
Forum members considered this paper to markedly distort the associations between alcohol consumption, especially light drinking, and health outcomes. The authors were particularly remiss in not describing the net health effects of light to moderate consumption: longer longevity of life. Their long discussion of policy implications, and ways of decreasing alcohol use in the population, were unrelated to the data they presented, and failed to describe how complex and culturally specific such recommendations are. The authors describe many ways of decreasing alcohol consumption in the population, but do not provide any data about whether or not the measures they propose are successful.
While all Forum members agree that heavy alcohol consumption increases the risk of several cancers (information that oncologists should be aware of), light drinking has generally been associated only with a slight increase in breast cancer, but not with other types of cancer (especially when under-reporting of intake is considered). Further, factors such as dietary folate intake, patterns of drinking such as binge versus regular moderate drinking, and type of beverage generally consumed have been shown to modify even this relation. Also, regular light or moderate drinking has been consistently shown to decrease the risk of cardiovascular disease (the leading cause of death), diabetes, dementia, and even total mortality, associations largely ignored in this paper.
Our Forum considers that this publication from the American Society of Clinical Oncology misses an opportunity to provide, for oncologists and for the public, up-to-date and balanced information of the true relations of alcohol consumption to the risk of cancer and other health outcomes. They have especially ignored the effects of moderate drinking on the risk of total mortality.
Reference: LoConte NK, Brewster AM, Kaur JS, Merrill JK, Alberg AJ. Alcohol and Cancer: A Statement of the American Society of Clinical Oncology. J Clin Oncol 2017;35:pre-publication. DOI: https://doi.org/10.1200/JCO.2017. 76.1155
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 207: Effects on birth weight and risk of preterm birth of light-to-moderate drinking during pregnancy – 2 November 2017
There is no question that high levels of alcohol consumption during pregnancy can lead to severe adverse effects on the fetus, with the most serious condition known as fetal alcohol syndrome (FAS). Many studies have also related alcohol intake during pregnancy with premature birth, low birth weight, and the infant being small for gestational age (SGA). Data are not as clear on the effects just of occasional or light drinking, but most studies have not detected adverse effects.
The present paper, based on a pooled sample of almost 200,000 women from nine European cohorts, provides data indicating that premature birth, an infant being small for gestational age (SGA), or being of low birth weight do not appear to be associated with light-to-moderate intake (up to 6 drinks/week); these results are similar to those from many other recent studies. In this large study, mothers who consumed greater amounts of alcohol tended to have an increased risk of the infant being SGA or with low birth weight, but such a level of drinking had no effect on the risk of premature delivery. This cohort consisted almost exclusively of light drinkers; no data were available on other potentially harmful effects of excessive drinking.
An interesting additional finding was that the reported frequency of any alcohol consumption during pregnancy in the cohorts studied has decreased dramatically in recent decades (from approximately 50% of women studied prior to 2000, to 39% in 2000-2004, to 14% in 2005-2011). This suggests that most women are responding to guidelines recommending that a woman not drink during pregnancy.
Based on currently available information, the Forum considers that a recommendation to “avoid alcohol during pregnancy” is appropriate as part of drinking guidelines for the public. However, scientific data, including the present paper, do not suggest that women who may have an occasional drink or very light alcohol consumption during pregnancy should have undue concern about having a premature birth or a low-birth-weight infant.
Reference: Strandberg-Larsen K, Poulsen G, Bech BH, Chatzi L, Cordier S, et al. Association of light-to-moderate alcohol drinking in pregnancy with preterm birth and birth weight: elucidating bias by pooling data from nine European cohorts. Eur J Epidemiol 2017 pre-publication; DOI 10.1007/s10654-017-0323-2
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 206: Importance of considering cultural factors in determining effects on health of alcohol consumption – 3 October 2017
It has been clearly shown that presumably similar amounts of alcohol tend to have different health effects (both beneficial and adverse) in different cultures. Greater health benefits from moderate alcohol intake have been shown, for example, in southern European countries (where wine with meals is common) than in more northern European countries, where beer and spirits are more likely to be consumed and usually not with food. Some of these differences may relate to the beverage consumed, while others may relate especially to different patterns of consumption. Further, in certain cultures, intoxication after drinking is expected and even tends to not be condemned. In the typical Italian culture, however, it would not be socially acceptable for a guest at a family dinner to become overtly intoxicated, and such would probably be less often reported in an epidemiologic study even if it had occurred. Thus, similar rates of alcohol-use disorders would be ascertained differently in different countries.
We know that the net effect of alcohol consumption relates to the amount of alcohol, the type of beverage, the rapidity of consumption, whether drinking with or without food, and surely a number of genetic factors of the drinker. What we are often unsure about is what the cultural context of drinking is for an individual subject or subjects in a certain population: different cultures seem to help control, or not control, the risk of drinking excessively. As pointed out by the present paper, these factors complicate the comparison of results of epidemiologic studies from different cultures.
In planning and interpreting results of epidemiologic studies, investigators now realize that simply estimating the average alcohol consumption over a period of time, usually a week, is inadequate to quantify alcohol exposure. The pattern of consumption (especially whether with or without food and whether regularly or in binges) is especially important. And, as the present study points out, knowing about the cultural aspects of drinking for a specific population is also key to interpreting the results. How best to do this, so that studies in different countries can be compared, remains difficult.
Reference: Rehm J, Room R. The cultural aspect: How to measure and interpret epidemiological data on alcohol-use disorders across cultures. Nordic Studies on Alcohol and Drugs 2017;34:330–341. DOI: 10.1177/1455072517704795.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 205: A very large population-based study of the association of alcohol consumption with total and disease-specific mortality – 4 September 2017
The usual finding in longitudinal cohort studies has been that light-to-moderate consumers of alcohol tend to be at lower risk for total mortality and show greater longevity of life, even when other lifestyle/demographic factors known to affect longevity are adjusted for in the analysis. The present analysis is important as it presents data on the relation of alcohol intake to total mortality as well as to specific mortality from cardiovascular disease (CVD) and cancer for a very large number of subjects in the USA. It is based on data from more than 300,000 subjects, of whom almost 25,000 died during a follow-up period averaging 8.2 years. There was a very large number of lifetime abstainers which could serve as an appropriate reference group for their analyses. Further, by adjusting for a number of chronic diseases, and carrying out sensitivity analyses with a 2-year lag period for mortality, the investigators improved their ability to avoid having their results affected by “sick quitters.”
The authors conclude that their analysis shows that light and moderate drinkers have a lower risk of total mortality, as well as mortality from CVD, heart disease, and cerebrovascular disease. The protective effects of alcohol for such cardiovascular outcomes were not present for subjects who reported binge drinking or for those reporting what was defined as “heavy” drinking (>7 drinks/week for women and older men, 14 drinks/week for younger men). Interestingly, the mortality risk for light and moderate drinking was also significantly reduced for deaths attributed to cancer; Forum members thought that this may have possibly resulted from subjects with cancer who actually died from CVD having their deaths attributed to cancer. Subjects reporting heavy drinking and those with binge drinking showed increased risk of all-cause and cancer mortality, with no significant effect on CVD outcomes. The key results of the study are that there is a very clear J-shaped curve for the relation of alcohol to mortality, with lower total, cardiovascular, and even cancer mortality rates for light and moderate drinkers who do not binge drink. There was increased total mortality and cancer mortality for those classified as “heavy” drinkers.
Forum Members thought it unfortunate that beverage-specific data were not presented (as in many studies wine, and sometimes beer, drinkers have better outcomes than consumers of spirits), that subjects of all ages (≥ 18 years of age) were included in a single analysis (rather than also presenting results specifically for older subjects, when the outcome events studied usually occur), and especially that women and older men who consumed > 7 drinks/week, and younger men consuming >14 drinks/week were all combined into a “heavy” drinking category. It would have been preferable that the investigators also had a category for those consuming only slightly more than the recommended levels, who may well have had different outcomes than heavier drinkers.
Overall, Forum members considered this to be a well-done study providing additional data supporting a J-shaped curve for the association of alcohol consumption with mortality. Thus, data continue to indicate that light-to-moderate intake of alcoholic beverages without binge drinking reduces total mortality as well as death from CVD or cancer. The cumulative scientific data on this topic are well described in the accompanying Editorial Comment by de Gaetano and Constanzo in the same issue of the journal.
Reference: Xi B, Veeranki SP, Zhao M, Ma C, Yan Y, Mi J. Relationship of Alcohol Consumption to All-Cause, Cardiovascular, and Cancer-Related Mortality in U.S. Adults. J Am Coll Cardiol 2017;70:913–922
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 204: Moderate drinking improves the chances for healthy survival to age 85 – 21 August 2017
A number of studies have shown that the risk of cognitive impairment appears to be reduced among elderly subjects who consume moderate amounts of alcohol; most studies indicate that both light and moderate drinking are associated with a lower risk of dementia, but heavy drinking is often shown to be associated with higher cognitive risk for dementia and cognitive impairment. In some studies, a protective effect of light-to-moderate alcohol intake has been seen primarily among consumers of wine, or sometimes beer/wine. Further, almost all well-done cohort studies have shown that moderate drinkers tend to have longer lifespans.
The present study is based on a group of ageing subjects in California that had been observed closely for several decades; the average follow-up period for these particular analyses were about 14 years. Subjects in this cohort have had multiple assessments of cognitive ability and frailty. The authors conclude that their subjects who reported moderate alcohol consumption in the late 1980s were more likely than non-drinkers during follow up to survive to age 85 years of age, and also to be more likely to survive to age 85 cognitively intact (without evidence of dementia). Also, daily or near-daily drinkers had better health outcomes than those of non-drinkers or less-frequent drinkers.
The Forum considers this to be a well-done study; while it is not based on a large cohort, it provides new data by having extensive evaluation over time in a cohort of community-dwelling elderly subjects. The results support data from most other studies of survival and dementia among moderate drinkers, but adds specific information on survival to age 85 without cognitive impairment.
This study and the review of prior scientific data on this subject led Forum members to also raise a question about the typical guidelines for alcohol consumption for the elderly: generally less or no alcohol consumption is advised. Given that current scientific data show that the risks of the common disease outcomes of older subjects (e.g., coronary artery disease, ischemic stroke, osteoporosis, dementia, mortality) are lower among moderate drinkers than among non-drinkers, it may be time to reevaluate such restrictions that are based on age alone.
Reference: Richard EL, Kritz-Silverstein D, Laughlin GA, Fung TT, Barrett-Connor E, McEvoy LK. Alcohol Intake and Cognitively Healthy Longevity in Community-Dwelling Adults: The Rancho Bernardo Study. J Alzheimer’s Dis 2017;9:803–814. DOI 10.3233/JAD-161153
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 203: Moderate alcohol intake may reduce, not increase, the risk of falls in the elderly – 7 August 2017
Falls are common among the elderly, and markedly increase the subsequent risk of morbidity and mortality. There has been much written about the dangers of even light-to-moderate intake of alcohol among the elderly, with an increase in potential falls being one key reason cited. This may not be in the best interest of many elderly subjects; the demonstrated protection of light-to-moderate alcohol intake against many of the diseases of ageing (especially coronary heart disease, stroke, osteoporosis, dementia) could outweigh any dangers from falls if the latter risk is not great.
The present study examined the association between certain patterns of alcohol consumption, including the Mediterranean drinking pattern (MDP), and the risk of falls in more than 2,000 elderly subjects over 3.3 years; at the end of follow up, 21.4 % of subjects reported at least one fall in the previous year. The study found that up to moderate amounts of alcohol (defined as less than 40 grams of alcohol/day for men and less than 24 grams/day for women) did not increase the risk of falls, but actually resulted in a significant decrease of 20% or more in such risk. The risks for having multiple falls or those requiring medical care were also lower for moderate drinkers. The investigators report further that subjects with higher scores for a Mediterranean-type diet, that includes regular wine consumption, had similar or more impressive reduction in their risk of falls.
The specific reasons for such protection are not fully known, but a number of favorable effects on health of moderate drinking (e.g., less osteoporosis, less cardiovascular disease, less dementia, greater functional capacity, etc.) may play a role. While the investigators of this study were able to adjust for many factors known to be associated with falls, residual confounding is always a possibility to explain these results.
To summarize, while previous studies have often reported an increase in risk of falls for heavy drinkers, the present study supports results of many previous studies indicating that light-to-moderate alcohol intake does not increase the risk, and often is shown to decrease the risk of falls and fractures. In the present study, even with adjustments for most known lifestyle factors affecting risk, moderate drinking was associated with at least a 20% decrease in the risk of falls when compared with abstainers. This is a message that needs to be incorporated into drinking recommendations for the elderly.
Reference: Ortolá R, García-Esquinas E, Galán I, Guallar-Castillón P, López-García E, Banegas JR, Rodríguez-Artalejo F. Patterns of alcohol consumption and risk of falls in older adults: a prospective cohort study. Osteoporosis International 2017, on-line publication. DOI 10.1007/s00198-017-4157-2.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
==================================================================
Critique 202: Importance of folate intake for reducing breast cancer risk from alcohol consumption, especially for women with a positive family history of breast cancer – 17 July 2017
The strongest factor associated with the risk of a woman developing breast cancer appears to be a positive family history of such a diagnosis in a sibling or mother. Among environmental factors, almost all studies have shown that alcohol consumption relates to increased risk; a slight increase is often seen even among women who report only light drinking, e.g., an average of less than one drink per day. The present study evaluates how a positive family history of breast cancer in a first-degree relative and folate intake may modify the association between alcohol intake and breast cancer; the analysis is based on data from a large number of young women, aged 27-44 years at baseline, over a follow-up period of 20 years.
Forum members considered that this was a very well-done analysis from the large Nurses’ Health Study II, which followed young women for two decades. Alcohol consumption in total drinks/week was based on repeated assessments (but the pattern of drinking, binge versus regular drinking, was not evaluated). Repeated dietary questionnaires were used to estimate folate input. More than 2,800 incident invasive breast cancers were detected, essentially all being validated by a review of medical records.
The main results of this study were that without a positive family history of breast cancer, there was no significant increase in cancer risk for any level of alcohol intake. With a positive family history, however, there was a tendency for higher risk with increasing alcohol intake; this increase was not statistically significant for those with high folate, but a significant positive association (HR=1.82, 95% CI 1.06, 3.12; P-trend = 0.08) with cancer was seen for subjects with the highest level of alcohol intake plus low levels of folate.
Forum members conclude that the results from the present study should greatly relieve anxiety about breast cancer for women without a positive family history of breast cancer who choose to consume light-to-moderate amounts of alcohol. For women with a first-degree relative with breast cancer, the data indicate that if they maintain a high level of folate intake, it may attenuate an increase in risk associated with alcohol intake.
Reference: Kim HJ, Jung S, Eliassen AH, Chen WY, Willett WC, Cho E. Alcohol consumption and breast cancer risk by family history of breast cancer and folate intake in younger women. Am J Epidemiol 2017: pre-publication.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
==================================================================
Critique 201: The marked effect of lifestyle on mortality — 26 June 2017
The aim of the present study was to examine differences in the risk of mortality and in survival associated with a healthy lifestyle versus a less healthy lifestyle. The analyses were based on a total of more than 60,000 Swedish men and women who were followed in one of two studies; at baseline, the subjects were aged 45 to 83 years and were free of cancer and cardiovascular disease. The goal was to evaluate the effects of four “healthy” lifestyle factors: (1) nonsmoking; (2) physical activity at least 150 min/week; (3) alcohol consumption of 0–14 drinks/week; and (4) a healthy diet, with the latter defined as a modified Dietary Approaches to Stop Hypertension (DASH) Diet score above the median. Cox proportional hazards regression models and Laplace regression were used to estimate respectively hazard ratios of all-cause mortality and differences in survival time.
The authors report: “Compared with individuals with no or one healthy lifestyle factor, the multivariable hazard ratios of all-cause mortality for individuals with all four health behaviors were 0.47 (95% confidence interval [CI] 0.44-0.51) in men and 0.39 (95% CI 0.35-0.44) in women. This corresponded to a difference in survival time of 4.1 (95% CI 3.6-4.6) years in men and 4.9 (95% CI 4.3-5.6) years in women.”
Forum members considered this to be a well-done study on a large cohort with complete follow-up data on mortality. Notable weaknesses included the fact that never drinkers and consumers of 0 to 14 drinks/week were considered in one group (thus, including lifetime abstainers, ex-drinkers, and current moderate drinkers); these subjects were compared with consumers of >14 drinks/week. Thus potential differences between abstinence versus light/moderate consumption could not be determined. Further, there were incomplete data on the pattern of drinking, and no data on the type of beverage consumed were reported. Nevertheless, the reduction in mortality for subjects following a healthy lifestyle was impressive: a reduction by half, or more, in the risk of mortality and a 4- to 5-year longer lifespan.
Based on a number of previous studies that evaluated similar lifestyle factors and mortality, the results of this study were not unexpected. Still, they strongly support the remarkable effects on mortality and survival of these lifestyle factors. While not smoking was clearly the factor with the strongest effect on reducing mortality, having a healthy diet, exercising, and consuming light to moderate amounts of alcohol all make additional contributions. This is an important message in that even individuals who may be challenged by genetic or socioeconomic predispositions to earlier demise, adopting certain lifestyle habits can help them reach their greatest potential for a longer and healthier lifespan.
Reference: Larsson SC, Kaluza J, Wolk A. Combined impact of healthy lifestyle factors on lifespan: two prospective cohorts. J Int Med 2017. Pre-publication. Doi: 10.1111.joim.12637.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
Critique 200: Does Light Drinking Increase the Risk of Cancer? — 8 June 2017
The association between the consumption of alcohol and the risk of cancer has been of great interest for many decades. There are a number of types of cancer, especially those of the upper aero-digestive tract (such as mouth, tongue, pharynx, etc.) that are clearly increased among heavy drinkers, especially among subjects who are also heavy smokers. Cancer of the liver can be a result of alcoholic liver cirrhosis, related to long-term heavy drinking. Further, an increased risk for many other cancers have been shown for heavy drinkers, but generally not for light or moderate drinkers.
The risk of breast cancer in women, however, is usually found to be slightly higher in even light drinkers than it is among non-drinkers. This has been a common finding, although some studies suggest that the pattern of drinking, the estimated level of underreporting of alcohol intake, use of hormone replacement therapy, and level of folate intake may all affect this association. For colorectal cancer, some studies suggest an increase in risk even among light-to-moderate drinkers. This has led some to proclaim that no alcohol consumption is preferable for the prevention of cancer. Others suggest that it is important to consider not only cancer, but other diseases; for example, coronary heart disease, ischemic stroke, diabetes, and dementia (all of which are important causes of disability and death) occur less frequently among moderate drinkers than among non-drinkers. Further, the risk of total mortality is almost always found to be lower among light to moderate drinkers than among abstainers.
The present analysis was designed to help determine the association of light or moderate drinking with the risk of cancer. It consisted of a meta-analysis based on a total of 60 studies from 135 articles and included only cohort studies of high quality. The analysis focused on the association between very light (≤0.5 drink/day), light (≤1 drink/day), or moderate drinking (1-2 drinks/day) and the risk of cancer incidence and mortality.
The authors found that very-light drinking was not associated with the incidence of most cancers except for female breast cancer and male colorectal cancer, and was associated with a decreased incidence of both female and male lung cancer and both female and male thyroid cancer. Moderate drinking significantly increased the incidence of male colorectal cancer and female breast cancer, whereas it decreased the incidence of both female and male hematologic malignancy.
Forum members considered this to be a well-done meta-analysis, based on a large number of studies. The main weaknesses of the study related to the lack of ability of the authors to evaluate a number of known confounders: underreporting of alcohol intake, the pattern of drinking or the type of beverage consumed, socio-economic status, and folate intake or other dietary factors. Further, the authors did not describe the effects of alcohol consumption on total mortality.
The results of this study, obviously, support most previous epidemiologic evidence on the association between alcohol consumption and cancer. Larger amounts of alcohol are associated with increased risk of a number of cancers, and even light consumption is associated with the risk of breast cancer, and possibly colorectal cancer. However, given the inability to adjust for many confounders in this study, and lack of data on the net effects in terms of total mortality, it remains difficult for scientists to provide scientifically sound and balanced guidelines regarding the health consequences of alcohol consumption that are applicable to everyone in the population.
Reference: Choi Y-J, Myung S-K, Lee J-H. Light Alcohol Drinking and Risk of Cancer: A Meta-analysis of Cohort Studies. Cancer Research and Treatment 2017; pre-publication release.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=======================================================================
Critique 199: Potential mechanisms for the greater risk and fewer health advantages from alcohol consumption for subjects with low socio-economic status – 25 May 2017
The majority of epidemiologic studies have shown that both the positive and negative health effects of alcohol consumption are modified by the socio-economic status (SES) of individuals, with truly moderate drinkers who are from higher SES strata having better health outcomes and fewer adverse effects from alcohol than lower-SES subjects supposedly consuming similar amounts. One potential explanation for this has been that higher SES subjects (those with higher education, income, job status, etc.) are more likely to be regular moderate drinkers, more likely to be wine drinkers, and to drink primarily with meals, while lower SES subjects are more likely to binge drink (mainly beer or spirits), not with food, and may tend to under-report their alcohol intake. However, there are limited scientific data on the specific mechanisms by which such differences occur.
The authors of the present paper have used data on alcohol intake collected in the Scottish Health Surveys from more than 50,000 subjects to investigate whether the harmful effects of alcohol differ by socioeconomic status when accounting for a number of SES factors. They had very good measures of SES based on education, income, social class (professionals, skilled manual labor, unskilled labor, etc.), and a “measure of deprivation” of the geographic area of the subject (based on multiple measures of deprivation from government administrative data). Their health outcome measures were based on public records for deaths, admissions, and prescriptions; their primary outcome was alcohol-attributable admission or death. Their data show that, even without considering alcohol consumption, lower SES subjects were at much greater risk for poor health outcomes. And, while risks associated with increasing amounts of alcohol were present in all SES groups, they were much greater in the lower groups.
Forum members considered this to be a well-done study, but pointed out that there was limited information on the pattern of drinking and no data on the type of alcoholic beverage consumed or whether or not it was consumed with food. There was no dietary information or genetic information available, and little data on access to health care. While the study showed very marked differences in adverse health outcomes according to SES, the authors found that the factors they considered explained little of the health effects seen. They concluded: “Disadvantaged social groups have greater alcohol-attributable harms compared with individuals from advantaged areas for given levels of alcohol consumption, even after accounting for different drinking patterns, obesity, and smoking status at the individual level.”
Forum members agree that there may be many other lifestyle factors associated with poverty that scientists are unaware of, or unable to adequately control for, in their analyses. Differences by SES in the assessment of alcohol intake remains as a potential factor (especially given that higher SES subjects are usually found to consume alcohol regularly and moderately, less in binges, more often consuming wine with food, etc.). The authors of the present paper have evaluated a number of factors (including smoking status and obesity) as potential explanations for the poorer outcomes among lower SES subjects, and still found large differences in health effects despite adjusting for a number of such lifestyle factors. Thus, the specific reasons why lower SES subjects have worse health overall and poorer effects after alcohol consumption remain unclear.
Reference: Katikireddi SV, Whitley E, Lewsey J, Gray L, Leyland AH. Socioeconomic status as an effect modifier of alcohol consumption and harm: analysis of linked cohort data. Lancet Public Health 2017. Online publication May 10, 2017. http://dx.doi.org/10.1016/S2468-2667(17)30078-6
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================
Critique 198: A study of alcohol and cardiovascular disease based on “Big Data,” linked electronic medical records from the population — 24 April 2017
Essentially all observational cohort epidemiologic studies have shown a “J-shaped” curve for the association of moderate alcohol consumption with coronary heart disease and myocardial infarction, in that non-drinkers and heavy drinkers have higher risk than moderate drinkers. The present study presents a new approach for evaluating this relation by using electronic medical records for a very large number of patients (“big data”) in the UK to judge the relation between alcohol consumption and a variety of cardiovascular disease (CVD) outcomes. The study evaluated clinical data recorded by physicians from almost 2 million subjects, with about 115,000 CVD events recorded in public records. The exposures and outcomes came solely from the medical diagnoses given by individual physicians, and such diagnoses are known to often be inaccurate. For individual subjects, the exposure was based on codes for alcohol use or misuse in their medical records, and the cause of death was based on that recorded by the physician (which is not always consistent with diagnoses from autopsies or medical record reviews). Such problems would be expected to decrease the precision of the exposure and of outcome diagnoses.
Forum reviewers of this paper considered that the authors made a valiant effort in attempting to take into account the limiting factors of using big data for epidemiologic research. It is recognized that studies such as these cannot evaluate the pattern of drinking (regular versus binge) and the investigators were unable to evaluate different effects according to the type of beverage consumed (beer, wine, or spirits). It would be expected that both of these factors may have affected their results. Nevertheless, their conclusions strongly support the extensive observational data from cohort studies over many decades that have shown a higher risk among abstainers (versus moderate drinkers) for many CVD outcomes. In the present study, non-drinkers had significantly higher risk for unstable angina, myocardial infarction (MI), unheralded coronary death, heart failure, ischemic stroke, peripheral arterial disease, and abdominal aortic aneurysm. For most of these outcomes, heavy drinkers tended to have an increased risk (a J-shaped curve), but the risk for myocardial infarction and for stable angina remained decreased even for the heavy drinking category. For other manifestations of CVD, especially those related to cerebral artery disease (other than ischemic stroke), there was less of a clear pattern relating alcohol to disease. For their aggregate, overall outcome based on all manifestations of CVD, their analyses add further support for a J-shaped curve between alcohol intake and CVD.
Reference: Bell S, Daskalopoulou M, Rapsomaniki E, George J, Britton A, Bobak M, Casas JP, Dale CE, Denaxas S, Shah AD, Hemingway H. Association between clinically recorded alcohol consumption and initial presentation of 12 cardiovascular diseases: population based cohort study using linked health records. BMJ 2017;356:j909. http://dx.doi.org/10.1136/bmj.j909
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================
Critique 197: Alcohol consumption and the risk of developing dementia – 13 April 2017
A number of epidemiologic studies have found that light-to-moderate alcohol intake is associated with a lower risk of developing dementia and/or cognitive decline, while excessive drinking may increase the risk. The authors of the present paper carried out a meta-analysis of the current scientific literature that was based on data from 11 studies with 4,586 cases of all-cause dementia diagnosed among more than 70,000 subjects and two additional analyses of studies of approximately 50,000 subjects each for evaluating the association of alcohol intake with the diagnosis of Alzheimer’s disease or vascular dementia. Seven studies provided results according to type of alcoholic beverage consumed, while two provided results according to APOE 4 levels.
The conclusions of the authors are that, considering all sources of alcohol, light-to-moderate alcohol consumption was associated with a lower risk of all forms of dementia; the risk was reduced for up to 12.5 g/day (about one typical drink) and increased for consumers of more than 38 g/day (about 3 to 4 typical drinks). However, beverage-specific analyses indicated that the effect was only for wine, and not for consumption of beer or spirits. For moderate consumers of wine, the risk of dementia was reduced by 40% or more in comparison with that of non-drinkers. Little effect was noted among drinkers of spirits, and heavy beer drinkers appeared to have an increased risk of dementia. The presence or absence of APOE 4 did not appear to modify the effects.
Forum reviewers considered this to be a very well-done meta-analysis of the current literature on the topic. It was based only on prospective epidemiologic studies of very good quality, and sub-analyses evaluated the separate effects of each type of alcoholic beverage. While the authors were unable to include the pattern of drinking (binge versus regular moderate) in their analyses, and could not test for previous alcohol consumption among current non-drinkers, Forum members agreed with the primary findings of a J-shaped curve between alcohol consumption and all types of dementia (including vascular dementia and Alzheimer’s disease).
Most of this Forum critique deals with potential mechanisms by which wine consumption may reduce the risk of dementia and/or cognitive decline. In addition to the effects of both alcohol and polyphenols in wine on decreasing atherosclerosis and having beneficial effects on hematological factors (affecting cerebral as well as coronary arteries), there may also be anti-inflammatory effects and direct effects on brain structures that play a role. Given that the beneficial effects were primarily among wine consumers, this suggests that the polyphenols and other non-alcohol substances in wine (perhaps in interaction with alcohol) may be more important than the alcohol itself in reducing the risk of dementia.
The mechanistic studies described in the paper and in this critique provide considerable support for the epidemiologic findings of less dementia and cognitive decline among moderate drinkers. Forum member agree with the authors of this paper that light-to-moderate wine consumption may help lower the risk of dementia, an increasingly important condition in the world’s rapidly ageing populations.
Reference: Xu W, Wang H, Wan Y, Tan C, Li J, Tan L, Yu JT. Alcohol consumption and dementia risk: a dose-response meta-analysis of prospective studies. Eur J Epidemiol 2017;32:31-42. doi: 10.1007/s10654-017-0225-3. Epub 2017.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================
Critique 196: Adverse health effects of binge drinking on cardiovascular disease — 2 February 2017
This review paper on the effects of binge drinking on the risk of cardiovascular disease (CVD) provides considerable information on a topic of importance to public health. It clearly indicates that subjects who binge drink, however defined, tend to be at increased risk for hypertension, myocardial infarction, stroke, and cardiac arrhythmias. These adverse health outcomes are in addition to the well-known effects of binge drinking on drunkenness and many adverse health effects, both acute and chronic, as well as risk from violence and accidents to the drinker and to others.
While the members of the Forum applaud the efforts of the authors to present data on this relation, this paper failed to include many important previous research reports on the topic. Forum member Ian Puddey and others have prepared an extensive summary of many of the key research papers not addressed by the authors of this paper; their remarks are included in the full Forum critique. It describes how many factors, such as not only the amount but the rate at which alcohol is consumed, the type of beverage, whether or not food is being consumed, the prior drinking habits of the subjects, and many other factors can influence the effects of alcoholic beverages on health.
The Forum members conclude that a “comprehensive review” of binge drinking and other drinking patterns of alcohol in relation to the risk of CVD should include all of the available scientific data on the topic to be most useful. Taking into consideration the additional research results described in this critique provides a much better overview of the effects of binge drinking on CVD. The bottom line is that episodic heavy drinking, or binge drinking, has adverse influences on many health outcomes, including the risk of CVD.
Reference: Piano MR, Mazzuco A, Kang M, Phillips SA. Cardiovascular Consequences of Binge Drinking: An Integrative Review with Implications for Advocacy, Policy, and Research. Alcoholism: Clinical and Experimental Research 2017; Pre-publication. doi: 10.1111/acer.13329
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=========================================================================
Critique 195: How much of the “health benefits” of alcohol relate to higher socio-economic status of drinkers? — 19 December 2016
It has long been recognized from epidemiologic studies that both the positive and negative health effects of alcohol consumption are modified by the socio-economic status (SES) of individuals. Higher SES subjects (higher education, income, job status, etc.) are more likely to be regular moderate drinkers, while lower SES subjects are more likely to binge drink and under-report their alcohol intake. Truly moderate drinkers tend to have better health outcomes and fewer adverse effects from alcohol, and consistently show lower total mortality risks than non-drinkers or heavy drinkers.
The present study, from the New Zealand Longitudinal Study of Ageing, used data from the second examination of the cohort to do a cross-sectional analysis judging the relation of alcohol consumption to “health”. When controlling for age, income, and education (the latter two as measures of SES), they found a significant “J-shaped” association between reported alcohol intake and self-reported “physical health”. However, the authors state that they then used another measure of SES, the Living Standard Index-Short Forum (ELSI-SF), and found that the reported alcohol intake of subjects correlated with their measure of physical health almost exactly the same as with the results of the ELSI-SF. They conclude that there are no health benefits of moderate drinking, only that people with higher SES are more likely to drink moderately.
Forum members considered it unfortunate that the assessment of the exposure (alcohol intake) used in this study was based only on self-reported average intake and did not include data on the pattern of drinking (binge versus regular moderate intake, etc.). Further, their outcome was based only on a self-reported questionnaire of “physical health,” and did include any hard data; an overall index based on assessments of functional status, biomarkers of and the occurrence of disease, and mortality would be preferable when judging “health benefits” of alcohol. The Forum considered that the authors used inadequate indices of both the exposure to alcohol and their assessment of “health” (based on a questionnaire) to reach a conclusion that moderate drinking does not have any beneficial effects on health. This was done ignoring the massive amount of not only observational data but results from extensive experimental studies over more than four decades. Such research has found that moderate drinking not only has beneficial effects on assessments of physical health and disease occurrence, but results in significantly lower total mortality when moderate drinkers are compared with abstainers.
Regardless, given that this study, as have almost all epidemiologic studies, has shown the importance of SES on health outcomes, a key challenge to scientists is to seek to determine the mechanisms by which these differences occur. One potentially important factor is that the differing health outcomes relate to errors in judging the exposure, i.e., inadequate assessments of alcohol: not evaluating for binge drinking versus regular intake, consuming alcohol with or without food, type of beverage consumed, under-reporting of intake, etc. Also, much broader definitions of “health” are needed (rather than the results of a single self-administered questionnaire) that include the effects on functional status, disease states, and mortality. And, it is important that other lifestyle factors (smoking, drug use, etc.) that affect health be properly evaluated as determinants of health. Only with such data will we be able to fully judge the overall effects of alcohol consumption on health outcomes.
Reference: Towers A, Philipp M, Dulin P, Allen J. The “Health Benefits” of Moderate Drinking in Older Adults may be Better Explained by Socioeconomic Status. Pre-publication: J Gerontol B Psychol Sci Soc Sci 2016. doi:10.1093/geronb/gbw152
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 194: Long-term alcohol use and mortality among Swedish women – 22 November 2016
In a follow-up analysis of almost 50,000 young women, aged 30-49 at baseline, in the Swedish Women’s Lifestyle and Health cohort, the authors used self-reported information on alcohol consumption on two occasions, 12 years apart, to estimate the effects of alcohol on overall and cause-specific mortality. There were 2,100 deaths during follow up. Effects of alcohol on the two occasions, and changes between the two assessments among 33,000 women with available data, were related to mortality, as assessed from virtually complete national records.
Using “light” drinkers (0.1 – 1.49 grams of alcohol/day) as the referent group, the authors report an inverse association between greater amounts of alcohol consumption and mortality from cardiovascular disease. They report increased risk of cardiovascular and total mortality for abstainers. Despite the large number of total subjects, the authors report results separately for relatively narrow ranges of alcohol intake (none, 0.1-1.49, 1.5-4.9, 5-9.9, 10-14.9, 15+ g/day), which makes the numbers of subjects in many groups quite small. Given that the total mortality risks for most groups of drinkers were similar, it would have been interesting to see the effects of alcohol consumption (versus no consumption) using a broader definition of “moderate” drinking.
Forum members in general thought that this was a well-done study, using an excellent source of national records available in Sweden for determining mortality. They had concerns that the under-reporting of alcohol intake was not addressed; there is a high probability that some of the supposedly “light” drinkers may have actually consumed more alcohol, which would tend to decrease any differences between the referent group and the next groups of drinkers. This could help explain why, despite the strikingly lower risk ratios for cardiovascular disease for all drinkers when compared with the referent group, the inverse relation of alcohol was not statistically significant for any single group considered alone.
The Forum was also concerned that while the investigators had data on binge drinking and whether or not alcohol was usually consumed with meals, they chose not to include these data in their analyses. Given that drinking pattern plays a large role in determining favorable or unfavorable health effects of alcohol, the inclusion of such information may have better delineated the true effects of alcohol. Also, the authors “chose not to separately study the effects of different alcohol beverages;” reporting effects separately for beer, wine, and spirits could have provided key data on the effects of alcohol consumption.
The attempt of the authors to judge the effects of changes in alcohol intake during the study is laudable. Importantly, data on the reason that a woman may decide to increase or decrease her intake is not known; if due to the development of a serious disease, it may be the disease and not the change in alcohol intake that relates to subsequent mortality. However, given the inherent problems in assessing change, the results of this study are consistent with other studies that have suggested an increase in mortality risk for moderate drinkers who stop their alcohol consumption.
Reference: Licaj I, Sandin S, Skeie G, Adami H-O, Roswall N, Weiderpass E. Alcohol consumption over time and mortality in the Swedish Women’s Lifestyle and Health cohort. BMJ Open 2016;6:e012862. doi:10.1136/ bmjopen-2016-012862
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 193: The association of reported alcohol intake with the risk of subarachnoid hemorrhage: A meta-analysis – 1 November 2016
Data from epidemiologic studies are quite consistent for the relation of alcohol consumption with the different types of stroke: for ischemic stroke, an inverse association with moderate drinking and a possible increase with heavy drinking (a “j-shaped curve”); for hemorrhagic stroke, a direct positive association, although some studies suggest that there may be a threshold level for an increase in risk. Data are mixed on a possible association between the most uncommon type of stroke, subarachnoid hemorrhage (SAH). The present paper presents results of a meta-analysis relating reported intake of alcohol with subsequent risk of SAH. It was based on 14 observational studies reporting data on 483,553 individuals and 2,556 patients.
Forum members agree that this study suggests that alcohol intake, especially heavier drinking, increases the risk of SAH, although there was considerable heterogeneity among studies from different parts of the world, there were no countries from the Mediterranean area included, and there was no accounting for pattern of drinking (binge versus moderate regular) or type of beverage, all of which may affect risk.
The authors concluded that there was no relation between light (<15 g/day) or moderate alcohol consumption (15‑30 g/day) compared with abstaining individuals; this was based on statistically insignificant increases in RR of 1.27 (95% CI: 0.95, 1.68) and 1.33 (95% CI: 0.84, 2.09) for these two groups, respectively. However, Forum members suggest that there could be a slight increase in risk even for these two groups. For heavier drinkers (> 30 g/day, about 2 ½ to 3 typical drinks per day), the data indicate an increase in risk: RR=1.78 (95% CI: 1.46, 2.17).
It should be noted that the overall risk of total stroke is decreased from moderate drinking, as the most common type of stroke is ischemic, and moderate drinking has consistently been shown to lower such risk; this is especially related to lowering the risk of atherosclerotic or embolic clots. However, while rare, SAH is often a devastating disease, and the risk may be increased from alcohol consumption through its effects on decreasing coagulation.
Reference: Yao X, Zhang K, Bian J, Chen G. Alcohol consumption and risk of subarachnoid hemorrhage: A meta-analysis of 14 observational studies. Biomedical Reports 2016;5:428-436.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=========================================================================
Critique 192: The association of alcohol consumption with the risk of prostate cancer –- 12 September 2016
Scientific data are mixed on the association of alcohol consumption with the risk of prostate cancer. In the present paper, the authors have used data from 11, 372 subjects in the Older Finnish Twin Cohort who provided data on alcohol intake on two occasions. They were followed for the development of prostate cancer from 1981 to 2012, during which 601 incident cases of prostate cancer and 110 deaths from prostate cancer occurred. The authors relate reported average alcohol intake, and whether or not the subject reported binge drinking, to the risk of prostate cancer and prostate cancer-specific death. They also evaluated the risks of prostate cancer among alcohol-discordant twins. The authors used current abstainers and ex-drinkers as the referent group in their main analyses, but did sensitivity analyses using never drinkers as an alternative referent group.
The type of beverage consumed was not known, so whether or not wine or beer consumption may have a different relation with prostate cancer than spirits intake cannot be determined. However, overall the data indicated a higher risk of prostate cancer from heavy intake and binge drinking, but also a high risk among abstainers. The number of discordant twins (for alcohol consumption) was too small for definitive results in terms of the risk of prostate cancer among subjects with the same or a similar genetic background , but the lowest risk was among light drinkers who did not binge drink. Even among this subset of the population, abstainers had higher risk than light drinkers.
Thus, the results of this well-done study suggest that there may be a J-shaped relation between alcohol consumption and prostate cancer risk. Light drinkers appear to have the most favorable results for both incident prostate cancer and prostate cancer-specific mortality. The risk for subjects reporting heavy drinking and binge drinking was higher for both incidence and mortality than the risk of light drinkers; for unexplained reasons, abstainers also tended to have higher risk of prostate cancer and mortality.
Reference: Dickerman BA, Markt SC, Koskenvuo M, Pukkala E, Muccil LA, Kaprio J. Alcohol intake, drinking patterns, and prostate cancer risk and mortality: a 30-year prospective cohort study of Finnish twins. Cancer Causes Control 2016;27:1049–1058. DOI 10.1007/s10552-016-0778-6
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 191: A new study on the mechanisms of alcohol’s effects on health and disease – 25 August 2016
While observational epidemiologic studies for many decades have consistently shown that moderate drinkers have a lower risk of cardiovascular diseases than do non-drinkers or heavy drinkers, the specific metabolic effects of alcohol have been little studied. In the present analysis, among almost 10,000 young adults from three population-based cohorts in Finland, associations of alcohol intake with 86 metabolic measures were assessed. Circulating lipids, fatty acids and metabolites were quantified by high-throughput nuclear magnetic resonance metabolomics and biochemical assays. The investigators found that alcohol consumption was associated with a complex metabolic signature, including aberrations in multiple biomarkers for reduced as well as elevated cardiometabolic risk; many factors showed different associations according to the estimated amount of alcohol consumed.
Among key associations found for greater alcohol intake were increases in HDL-cholesterol and its subclasses, decreases in LDL size, an increase in monounsaturated fatty acids and a decrease in omega-6 fatty acids, and lower concentrations of glutamine and citrate. For unexplained reasons, the changes in fatty acids from alcohol in this study were similar to those occurring following the administration of canola oil in other research. Some Forum reviewers pointed out that the analyses were not theory driven, and should only be used to generate hypotheses that would need to be tested in future experiments. As stated by one reviewer, the major contribution from this paper could be that it ignites the interest for experimental studies and provides new variables to be evaluated in prospective studies. In any case, the findings of this study provide valuable clues to the biologic effects on health, both favorable and adverse, related to alcohol consumption.
While not discussed by the authors, Forum members considered that the results of this paper might also be useful in providing a new approach for judging the level of alcohol intake of individuals in epidemiologic studies. At present, alcohol intake is judged almost exclusively from self-reports by subjects. Previous attempts designed to identify subjects more likely to be under-reporting their intake have shown that they may sharpen relations between estimated intake and health outcomes. Forum members believe that approaches that identify sources of bias for self-reported data, whether based on genetic, behavioral, physiological, or other information (preferably on all), might allow epidemiologists to have more precise and accurate information on alcohol intake when relating such to disease outcomes. A new approach for providing more accurate and unbiased estimates of alcohol intake is suggested by this excellent analysis.
Reference: Würtz P, Cook S, Wang Q, Tiainen M, Tynkkynen T, Kangas AJ, et al. Metabolic profiling of alcohol consumption in 9778 young adults. Int J Epidemiol 2016; pre-publication: doi: 0.1093/ije/dyw175
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 190: Alcohol intake during middle age and later atherosclerosis – 11 August 2016
Carotid artery disease can be estimated by ultrasound from the thickness of the wall of the arteries (recorded as carotid artery intima/medial thickness, cIMT) and by evidence of atherosclerotic plaques within the carotid arteries. The association between alcohol intake and such lesions is unclear, as some studies show a positive association with cIMT and/or plaques while others show no association. Given that carotid disease relates to the subsequent risk of coronary artery disease, there is increasing use of carotid ultrasound measurements to help determine long-term risk.
The present large study from the UK provides valuable information by reporting the cross-sectional relation between alcohol consumption and cIMT as well as how the drinking pattern over 20 years in middle age may relate to cIMT later in life. While heavy alcohol intake was found to increase later cIMT measures, no clear differences were noted between subjects reporting abstinence and those reporting moderate drinking in middle age.
Forum reviewers considered this to be a well-done study. There were some concerns that only total average alcohol intake was considered, as there were no data on the type of beverage consumed, the pattern of drinking (binge versus regular moderate), whether the alcohol was consumed with food, etc., and there was an absence of data on diet, physical activity, adiposity, and other factors related to atherosclerosis. Further, only the thickness of the carotid artery was evaluated, and not the presence or absence of atherosclerotic plaques on the ultrasound readings.
Overall, current scientific data provide strong evidence that moderate alcohol consumption lowers the risk of most manifestations of cardiovascular disease; it appears to work through a combination of effects on lipids, inflammation, coagulation, fibrinolysis, glucose metabolism, and other paths. Further, heavy drinking is known to increase blood pressure, and is an important factor for developing hypertension (and a strong determinant of cIMT). The failure of the present study to find a significant association between moderate alcohol intake and later carotid thickness supports what has been shown in some, but not all, previous studies.
If indeed chronic alcohol use has little effect on atherosclerosis (using images from the carotids as an index of atherosclerosis in the coronary arteries and elsewhere in the body), it may indicate that the mechanisms for the protective effect of moderate alcohol consumption on cardiovascular disease are not so much related to preventing atherogenesis, but due primarily to the effects on coagulopathy. And it is known that clot formation within the arterial wall is often the precipitating event for an acute myocardial infarction or other cardiovascular event.
Reference: Britton A, Hardy R, Kuhf D, Deanfield J, Charakida M, Bell S. Twenty-year trajectories of alcohol consumption during midlife and atherosclerotic thickening in early old age: findings from two British population cohort studies. BMC Medicine 2016l;14:111. DOI 10.1186/s12916-016-0656-9.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 189: Importance of drinking pattern on the effects of wine on health — 26 July 2016
A review article appearing in Food & Function, a publication of the Royal Society of Chemistry in the United Kingdom, presents a summary of evidence-based scientific data relating the moderate consumption of wine and other alcoholic beverages to health. Forum members considered the paper to be a well-thought-out appraisal of the effects that the pattern of consumption (e.g., the type of beverage, regular versus binge drinking, consumption with meals, etc.) affects its risks and benefits. (It is recognized that some of the authors of this publication work primarily with wine, but the review article covers key behaviors that affect the relation of the consumption of all types of alcohol to health.)
The authors describe how the polyphenols and other non-alcoholic components of wine provide anti-oxidants and decrease post-prandial oxidative stress. These phenols can also scavenge free radicals in the mouth and throughout the gastro-intestinal tract, preventing lipid peroxidation as well as the absorption of cytotoxic lipid peroxidation products. Wine also favorably affects urate levels; thus, the antioxidant activity is apparently influenced by two separate mechanisms: wine-derived phenolic compounds and plasma urate. A further important biological property of wine is its potent antimicrobial activity that tends to decrease adverse effects of food-borne and oral pathogens.
The article summarizes the key differences in health effects when alcohol (especially wine) is consumed moderately, with food, and on a regular basis rather than in binges. These differences emphasize why evaluating only the total amount of alcohol consumed, and not how it is consumed, is inadequate when evaluating its effects on health and disease. Further, the authors emphasize how all medical and scientific information concerning the effects of wine and alcohol consumption on human health should be evidence-based and communicated in a competent, credible and unbiased manner.
Reference: Boban M, Stockley C, Teissedre P-L, Restani P, Fradera U, Stein-Hammer C, Ruf J-C. Drinking pattern of wine and effects on human health: why should we drink moderately and with meals? Food Funct 2016;7:2937–2942. DOI:10.1039/c6fo00218h
Note on potential conflict of interest: While several of the authors of this paper are members of our Forum, they have had no input into the review of the article.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 188: Alcohol-attributable cancer in New Zealand . . . 28 June 2016
Previous scientific research has shown that heavy alcohol consumption is a major risk factor for upper aero-digestive cancers, and even light drinking increases slightly the risk of breast cancer in women. The present study is based on a very small number of cases of cancer in New Zealand, tabulated separately for Māori and non-Māori subjects, and applies estimates of alcohol effects from other population-based studies. Besides having so few cases, the investigators had no individual data (on the pattern of alcohol consumption, type of beverage, smoking or other lifestyle habits, socio-economic status, etc.) on subjects who did, or did not, develop these cancers. It is not even known whether or not the specific subjects who developed these cancers consumed alcohol.
It has repeatedly been emphasized that disease-specific death rates must be interpreted in light of the effects of the exposure (in this case, alcohol consumption) on other causes of death as well, especially on total mortality risk. The large majority of studies have shown that moderate drinking clearly reduces the risk of most cardiovascular diseases, diabetes, and other of the diseases of ageing, as well as the risk of total mortality. However, the estimated effects of alcohol on total mortality are not included in this paper.
The very long Discussion in this paper is primarily a treatise on how the public must be told of the dangers of cancer from any alcohol consumption; it focuses on health policy recommendations and very little on the limitations of the data and the study. The authors end up making very broad recommendations based on very small numbers of subjects. Limitations to this study suggest that it adds little to our current understanding of the relation of alcohol consumption to the risk of cancer and other diseases.
Reference: Connor J, Kydd R, Maclennan B, Shield K, Rehm J. Alcohol-attributable cancer deaths under 80 years of age in New Zealand. Drug and Alcohol Review 2016; pre-publication. DOI: 10.1111/dar.12443
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 187: Alcohol and squamous cell carcinoma of the skin — 14 June 2016
Skin cancers, whether melanoma, basal cell, or squamous cell, are all increased by ultra-violet rays of the sun, and such cancers are much more common in areas of the world with more sun exposure. Further, the risk of such cancers is higher among individuals reporting excessive tanning (either from the sun or from tanning salons). The present study was undertaken to judge the relation between alcohol consumption and the risk of cutaneous squamous cell carcinoma (cSCC), an association that is unclear from earlier research. Determining the relation between alcohol and skin cancer is made difficult by the fact that excessive sun exposure has been shown to be greater among consumers of alcohol than among abstainers, thus the potential for confounding.
In the present analyses, combined data from three cohorts of subjects in the US, who had repeated assessments of alcohol intake over many years, were evaluated tor the relation of alcohol to the development of verified cSCC. Subjects included women in two cohorts of the Nurses’ Health Study and men in the Health Professionals’ Follow-up Study. Among subjects providing a total of more than 4 million person-years of follow up, 2,938 cases of cSCC were identified.
The results varied somewhat among the different cohorts, but in the meta-analysis of the three studies using continuous measures of alcohol, there was an increase in risk of cSCC with alcohol intake. Among women, there was a steep increase in risk of cancer for low levels of intake (up to 5 grams of alcohol/day, slightly less than ½ of a typical drink), then a gradual increase in risk thereafter, whereas among men there was more of a gradual increase in risk with larger reported alcohol intake.
Overall, the authors report an increase in risk per typical drink per day of 22% for invasive cSCC and 14% for in situ cSCC. In beverage-specific analyses, white wine consumption of >/= 5 times/week was associated with an increased risk of cSCC (RR 1.31, 95% confidence interval: 1.09-1.59), but an increased risk of cSCC was not seen for other alcoholic beverages. The population-attributable risk associated with alcohol intake of ≥ 20 grams/day (about 1 ½ typical drinks) was 3% of cSCCs.
Forum members considered that the analyses were well done, and the results of the study are consistent with increases in risk associated with alcohol consumption for other types of skin cancer. Given that sun exposure is by far the primary risk factor for skin cancer, and consumers of alcohol tend to have greater number of sunburns (also shown in this study), it is always difficult to determine if residual confounding by sun exposure is playing a role. The authors of this paper attempted to adjust for sun exposure by including in their analyses the typical exposure values in the area of the world where the subjects resided, by recording the frequency that subjects reported 5 or more severe sunburns, and several other measures. As expected, there were reductions in the estimated RR for invasive cSCC when going from age-adjusted RR (1.34) to multivariable-adjusted estimates (1.22) of risk. However, the magnitude of decrease in risk estimates when only those adjustments for sun-exposure were added to the equation cannot be determined from the data presented.
Forum reviewers consider that these analyses support results from many previous studies and indicate that consumers of alcohol have a greater risk than non-drinkers of all types of skin cancer. Attempts to judge how much of this association may be due to residual confounding related to sun exposure are less than conclusive. Various hypotheses have been raised for possible interactions between sun exposure and alcohol, but currently there are no experimental data to test these theories. While the authors conclude that “physicians may consider counseling their patients about the association between alcohol consumption and risk for cSCC,” it might be more advantageous for physicians to focus more on the much greater protection against this disease that would occur if they were able to limit their patient’s exposure to ultra-violet radiation.
Reference: Siiskonen S, Han J, Li T, Cho E, Nijsten T, Qureshi A, Alcohol intake is associated with increased risk of squamous cell carcinoma of the skin: three US prospective cohort studies. Nutrition and Cancer 2016;68:545-553.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 186: Changes in alcohol and effects on risk of breast cancer and heart disease — 19 May 2016
This large study from Denmark was designed to test the hypothesis that women who increase their alcohol intake over a five year period have a higher risk of breast cancer and a lower risk of coronary heart disease (CHD) compared with women who exhibit a stable alcohol intake. It consisted of more than 20.000 postmenopausal women who had two assessments of alcohol intake, about 5 years apart; changes during that period were related to their subsequent risk of developing breast cancer or CHD, or dying, during the subsequent follow-up period that averaged 8 years.
For the risk of breast cancer, the baseline alcohol consumption reported by the women showed that higher alcohol intake was associated with a greater risk of developing breast cancer during follow up, but a lower risk of developing CHD and for total mortality. For relating changes in alcohol intake in the 5 years between the two alcohol assessments, those who increased their reported alcohol intake showed an increased risk of subsequent breast cancer, while those who decreased their intake also had a tendency for greater breast cancer. In terms of CHD and total mortality, the data were consistent with an increase in consumption lowering risk, while there was a tendency for a decrease in consumption to increase risk. Hence, the directionality for risk from changes in intake reflected the risks associated with baseline risk, and the authors conclude that their results “ . . .support the hypotheses that alcohol intake is associated with increased risk of breast cancer and decreased risk of coronary heart disease.”
Forum reviewers considered this to be a very well-done study. They, and the authors, appreciated the innate difficulty in separating effects on health of usual alcohol intake over time and changes over a limited period of time. Reviewers were also concerned by these problems, suggesting that some of the reported changes in alcohol consumption in this study may have just reflected individuals replying differently to questions regarding their drinking at different points of time. Further, the reason why some women may have actually increased or decreased their intake are not known.
Nevertheless, Forum members applaud the attempt of the authors to judge if changes in alcohol intake relate to cancer, CHD, and total mortality. This is a difficult task given that baseline and life-time alcohol consumption clearly relate to these outcomes. Further, data on the pattern of drinking (regular versus binge), any estimate of underreporting of alcohol, the type of beverage consumed and, as stated by the authors, certain known risk factors of breast cancer, were not available to be included in their analyses. Thus while the results of this study add important information on the relation of alcohol to disease, there remain questions about the specific relevance of changes in intake for such outcomes.
Reference: Dam MK, Hvidtfeldt UA, Tjønneland A, Overvad K, Grønbæk M, Tolstrup JS. Five year change in alcohol intake and risk of breast cancer and coronary heart disease among postmenopausal women: prospective cohort study. BMJ 2016;353:i2314. http://dx.doi.org/10.1136/bmj.i2314
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 185: An innovative assessment of alcohol consumption and the risk of atrial fibrillation – 28 April 2016
A study from Denmark has been carried out to test the hypothesis that alcohol consumption, both observational (self-reported) and estimated by genetic instruments, is associated with the risk of atrial fibrillation (AF) and to determine whether people with high cardiovascular risk are more sensitive towards alcohol than people with low risk. It was based on a large cohort of subjects (more than 88,000) with a mean follow-up period of 6.1 years; there were almost 3,500 cases of AF diagnosed from hospital records during follow up. Unfortunately, the authors did not have data to identify binge drinkers, which tend to show greater adverse cardiovascular events than regular moderate drinkers whose weekly intake may be the same.
The main results of the study were that men consuming more than 14 drinks/week, especially those consuming more than 28 drinks/week, had an increase in risk of AF, but no significant increase in risk was seen for any level of alcohol intake among women. When genotypes affecting alcohol metabolism (AHD1B, ADH1C) were studied in a Mendelian randomization analysis, the authors state that they “found no evidence to support causality of the observational findings.”
Forum reviewers of this article considered it to be a well-done study with appropriate analyses. Its results reflect the findings of most previous prospective studies and meta-analyses of little effect of light drinking on AF, but an increase in risk for heavier drinkers. The study also showed that the effects of alcohol consumption on the risk of AF were not different between subjects who had cardiovascular disease or were at high-risk of cardiovascular disease than for other subjects.
While Mendelian randomization using genetic factors affecting alcohol metabolism has been touted as an unbiased approach for judging causal health effects of alcohol, there are questions about the adequacy of such instruments for judging effects. In the present study, their use did not suggest that the relations shown by the self-report of alcohol by subjects necessarily indicated a causal association of alcohol with AF.
Overall, current data suggest that heavy drinking may increase the risk of AF, but there is little evidence of a meaningful increase in risk from light drinking. Luckily, such levels of alcohol intake (some guidelines suggest no more than 2 drinks/day for men or 1 drink/day for women) have been shown from many previous studies to significantly lower the risk of cardiovascular disease and total mortality.
Reference: Tolstrup JS, Wium-Andersen MK, Ørsted DD, Nordestgaard BG. Alcohol consumption and risk of atrial fibrillation: Observational and genetic estimates of association. European Journal of Preventive Cardiology 2016; pre-publication. DOI: 10.1177/2047487316641804
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 184: A major new meta-analysis on alcohol consumption and the risk of pancreatic cancer — 4 April 2016
The present meta-analysis was based on data from more than four million subjects in prospective cohort studies, among whom 11,846 incident cases of pancreatic cancer were diagnosed. With the lowest intake group (non-drinkers or occasional drinkers) as the referent group, the authors defined “light” consumption as up to 12 grams/day (essentially one typical drink); 12-24 g/day as “moderate”; and ≥24 g/day as “heavy” drinking. The key results of the study were that, overall, neither light drinkers (RR = 0.97) nor moderate drinkers (RR = 0.98) showed an increase in risk of pancreatic cancer, while subjects classified as heavy drinkers had a slight increase (RR= 1.15, 95% CI 1.06 – 1.25). The increase in risk was due to heavy drinkers of liquor, as there was no significant increase in risk even for heavy drinkers of beer (RR = 1.08, CI 0.90 – 1.30) or wine (RR = 1.09, CI 0.79 -1.49).
Forum members considered this to be an excellent paper on the association between alcohol consumption and pancreatic cancer. The authors used appropriate methods and limited subjects to those in prospective cohort studies, which would tend to limit bias. The paper shows that the significant increase in risk occurred only among men, with no significant effect of alcohol being found among women. Among the weaknesses of the study were that there was a mixture of lifetime abstainers and ex-drinkers included in the referent group, and the same cut-points for category of alcohol intake was used for both men and women, whereas drinking guidelines are generally lower for women than for men. Further, data on the pattern of drinking (regular versus binge) were not available.
To summarize, this study showed no significant association with cancer risk for any level of consumption of beer or wine, which could relate to their lower concentration of alcohol per volume of the beverage, to non-alcoholic substances (such as polyphenols, present in wine and beer), or even to different drinking practices among subjects consuming different beverages. Thus, Forum members agree with the conclusions of the authors that heavy alcohol consumption, especially of liquor, increases the risk of pancreatic cancer, but the intake of beer or wine may not be associated with an increased risk.
Reference: Wang Y-T, Gou Y-W, Jin WW, Xiao M, Fang H-Y. Association between alcohol intake and the risk of pancreatic cancer: a dose–response meta-analysis of cohort studies. BMC Cancer 2016;16:212. DOI 10.1186/s12885-016-2241-1
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
==============================================================================
Critique 183: An unusual analysis of the association of alcohol consumption with mortality — 24 March 2016
The stated purpose of this new analysis was to determine whether misclassifying former and occasional drinkers as abstainers and other potentially confounding study characteristics underlie observed positive health outcomes for low volume drinkers in prospective studies of mortality. Unfortunately, the authors include in their analyses a number of old epidemiologic studies and do not acknowledge that when the “errors” that they have commented on in the past (such as including heavy ex-drinkers in the no-alcohol referent group) have been dealt with in the majority of studies over the past decade. The authors still exclude the vast majority of these well-done studies in their new meta-analysis. Results of essentially all studies that adjust for their concerns continue to show a significant and meaningful reduction in the risk of cardiovascular disease (CVD) and total mortality from the moderate intake of wine and alcohol.
Forum members note how very selective the authors are in choosing which papers to include in their new analyses: they identified 2,575 studies on the subject, analyzed 87, but then they found some reason to exclude almost all of these studies to reach a conclusion that “ . . . there was no significant protection for low-volume drinkers (RR = 1.04, 95% CI [0.95, 1.15])” based on what is apparently only 6 remaining studies! The paper ignores the comments by two other scientists (Roerecke & Rehm) who, like these authors, have in the past been very concerned that confounding and errors weaken the purported relation between alcohol and a lower risk of cardiovascular disease, but have more recently concluded: “For drinkers having one to two drinks per drinking day without episodic heavy drinking, there is substantial and consistent evidence from epidemiological and short-term experimental studies for a beneficial association with IHD risk when compared to lifetime abstainers. The alcohol-IHD relationship fulfills all criteria for a causal association proposed by Hill.”
The authors of the present paper also ignore the immense amount of experimental data, not only animal experiments but trials in humans, that have described the mechanisms by which moderate alcohol and wine intake have been shown to decrease essentially all of the risk factors for CVD, including low HDL-cholesterol, elevated LDL-cholesterol, endothelial dysfunction, coagulopathies, inflammation, abnormal glucose metabolism, and many others. The consistent finding of lower CVD risk among moderate drinkers in all well-done cohort studies is strongly supported by experimental evidence of the mechanisms.
In the opinion of Forum members, the present paper markedly distorts the accumulated scientific evidence on alcohol and CVD. As stated by one Forum member, “The biased selection of studies that are included undermines the value of the paper, but more importantly promulgates misinformation in the name of appropriate scientific method. Failure to acknowledge the robust body of knowledge that supports the opposite conclusion, and disqualification of extensive animal and cell culture studies that offer plausible biologic explanation of observed benefits, is unconscionable.”
The Forum concludes that the overwhelming body of observational scientific data, as well as an immense number of experimental studies, support the contention that, for most middle-aged and older men and women who choose to do so, the regular consumption of small amounts of an alcoholic beverage can be considered as one component of a “healthy lifestyle.” Such a habit has been shown to be associated with a lower risk of cardiovascular disease and of total mortality.
Reference: Stockwell T, Zhao J, Panwar S, Roemer A, Naimi T, Chikritzhs T. Do “Moderate” Drinkers Have Reduced Mortality Risk? A Systematic Review and Meta-Analysis of Alcohol Consumption and All-Cause Mortality. J Stud Alcohol Drugs 2016;77:185–198.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 182: A major meta-analysis on the association of alcohol consumption with the risk of diabetes mellitus — 8 March 2016
Most previous studies have shown that consumers of light-to-moderate amounts of alcoholic beverages tend to have a significant reduction in their subsequent risk of developing Type II diabetes mellitus (DM). The purpose of the present study was to explore and summarize the evidence on the strength of the association between alcohol consumption and the subsequent risk of DM by using a dose-response meta-analytic approach. The authors identified 26 prospective cohort studies providing data appropriate for a meta-analysis; their analyses were based on 706,716 individuals (275,711 men and 431,005 women) with 31,621 cases of DM.
This meta-analysis reports that light and moderate drinkers have a significantly reduced risk of developing DM. For “light” drinkers (defined as an average of ≤ 12 g/day of alcohol), in comparison with non-drinkers, the overall risk ratio for DM was 0.83, with 95% CIs of 0.73, 0.95 (P = 0.005). For “moderate” drinkers (>12- <24 g/day), the RR was 0.74, with 95% CIs of 0.67, 0.82 (P = 0.001). Thus, data from this meta-analysis indicate a 17% and 26% reduction in the risk of DM, respectively, for these two drinking categories.
For subjects classified as “heavy” users of alcohol (reported intake averaging ≥ 24 g/day), the RR was 0.98, with 95% CIs of 0.83, 1.09, P = 0.480), interpreted as no effect. In a figure in the paper showing the separate results for each individual study included, the point estimates for the risk of DM were 1.0 or less than 1.0 for light and moderate drinkers in essentially all studies. Thus, data from the individual studies support the overall finding of a decrease in risk of DM for light or moderate drinkers.
Sub-group analyses showed that when subjects were stratified by sex, age, BMI, smoking, physical activity, and family history of DM, the point estimates of the risk ratios associated with light or moderate alcohol consumption were less than 1.0 in all groups, adding further to the robustness of the overall conclusions of a reduction in risk of DM from alcohol intake. Similarly, for all subjects, as well as for men and women separately, there was a clear U-shaped curve for the association. The nadir of the effect was just over 20 grams of alcohol per day (about 2 typical drinks), and even the risk of heavy drinkers did not reach the estimated risk of non-drinkers.
Forum members considered this to be a well-done analysis that confirms most previous results from prospective studies indicating a reduction in the risk of developing DM associated with moderate drinking. Further, an increasing number of randomized clinical trials are supporting such beneficial effects on the development and clinical treatment of DM. The Forum thought it unfortunate that beverage-specific results were not available in this study, as increasingly it is being shown that, beyond alcohol effects, there are polyphenols and other substances in wine and beer that provide additional protection against diabetes. Further, the Forum felt it important to also emphasize the protective effects against cardiovascular disease among subjects who already have DM, who are especially vulnerable to coronary heart disease and other effects of atherosclerosis.
Overall, this meta-analysis based on a large number of subjects indicates that the risk of DM is considerable lower among light and moderate drinkers than among abstainers. This finding supports the contention that, for most middle-aged and older adults (with the exception of individuals with specific prohibitions against alcohol such as former drug or alcohol abuse, certain types of neurological or severe hepatic disease, etc.), moderate alcohol consumption should be considered as a component of a “healthy lifestyle” that reduces the risk of diabetes and most of the chronic diseases of ageing.
Reference: Li X-H, Yu F-F, Zhou Y-H, He J. Association between alcohol consumption and the risk of incident type 2 diabetes: a systematic review and dose-response meta-analysis. Pre-publication: Am J Clin Nutr 2016; doi: 10.3945/ajcn.115.114389.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 181: Support for a causal role of alcohol consumption in improving the lipid profile — 16 February 2016
The present paper is based on data from more than 10,000 Americans of European descent who were participants in the Atherosclerosis Risk in Communities (ARIC) study. Common and rare variants in alcohol dehydrogenase and acetaldehyde dehydrogenase genes were evaluated using Mendelian randomization (MR), and then a genetic score based on 5 SNPs was used in regression analyses for the association of alcohol with lipids. Results reported by the authors state: “Alcohol consumption significantly increased HDL2-c and reduced TG, total cholesterol, LDL-c, sdLDL-c, and apoB levels. For each of these lipids a non-linear trend was observed. Compared to the first quartile of alcohol consumption, the third quartile had a 12.3% lower level of TG (p < 0.001), a 7.71 mg/dL lower level of total cholesterol (p = 0.007), a 10.3% higher level of HDL2-c (p = 0.007), a 6.87 mg/dL lower level of LDL-c (p = 0.012), a 7.4% lower level of sdLDL-c (p = 0.037), and a 3.5% lower level of apoB (p = 0.058, P overall = 0.022).”
The authors thus conclude that “This study supports the causal role of regular low-to-moderate alcohol consumption in increasing HDL2-c, reducing TG, total cholesterol, and LDL-c, and provides evidence for the novel finding that low-to-moderate consumption of alcohol reduces apoB and sdLDL-c levels among European-Americans.”
Forum members considered this to be a well-done and important study, the results of which indicate favorable effects of moderate alcohol consumption on lipid factors. However, they doubt that the inclusion of the genetic score from MR played a large part in the results; the authors state that the genetic score used in this paper explained only approximately 0.1% variance of alcohol consumption, suggesting that it was a weak instrumental variable for the MR. Several Forum members stated that randomized control trials, especially cross-over trials, testing the effects of alcohol intake on risk factors, may provide even better evaluation of alcohol’s effects on lipids. Until large-scale RCTs of alcohol and disease occurrence can be are carried out, such RCTs may provide the most reliable data on mechanisms of alcohol’s effects on the risk of cardiovascular disease.
Overall, the present study provides important data indicating that light-to-moderate alcohol consumption has favorable effects on most lipid values. The effects shown for HDL-cholesterol support much earlier data, and the effects on small dense LDL-cholesterol and ApoB provide key new information. The effects on lipids are surely important factors in the protective effects of moderate drinking against cardiovascular disease that have been seen in almost all well-done cohort studies.
Reference: Vu KN, Ballantyne CM, Hoogeveen RC, Nambi V, Volcik KA, Boerwinkle E, Morrison AC. Causal Role of Alcohol Consumption in an Improved Lipid Profile: The Atherosclerosis Risk in Communities (ARIC) Study. PLoS One 2016;11:e0148765. doi: 10.1371/journal.pone.0148765. eCollection 2016.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 180: The association of alcohol intake with total mortality risk among women — 9 February 2016
The follow up of more than 6,000 women in a population-based cohort in an area of southern Sweden was used to estimate how baseline levels of alcohol consumption, at age 50-59 years, related to total mortality risk over the subsequent 17 years. At baseline, 26% of women reported no alcohol consumption while 13% reported an average of 12 or more grams of alcohol per day. Thus, the large majority (61%) were light drinkers, reporting the equivalent of no more than one drink per day. The authors report that, even when adjusting for education, marital status, smoking, BMI, physical fitness, diabetes and ischemic heart disease before screening, mortality risk during follow up was significantly higher among non-drinkers and heavier drinkers than among women reporting the equivalent no more than one typical drink per day. They state that their analyses thus support a “J-shaped” association between alcohol and total mortality risk, and that “The observed protective effect of light drinking (1–12 grams/day) could thus not be attributed to any of these known confounders.”
Forum members agreed this was a well-done study, but noted that the authors were unable to adjust for the pattern of drinking (regular versus binge), previous drinking among abstainers, or potential changes in drinking during follow up. Also, beverage-specific results are not presented. Further, the data presented in this study are not adequate to judge the specific level of alcohol consumption at which total mortality risk for drinkers reaches or exceeds the risk for non-drinkers; in other words, the “threshold” for adverse effects of alcohol on mortality cannot be determined very well. Nevertheless, the results of these analyses are very consistent with most long-term follow-up studies and support a “J-shaped” association between alcohol and the risk of total mortality.
Reference: Midlöv P, Calling S, Memon AA, Sundquist J, Sundquist K, Johansson S-E. Women’s health in the Lund area (WHILA) – Alcohol consumption and all-cause mortality among women – a 17 year follow-up study. Pre-publication: BMC Public Health 2016;16:22. DOI 10.1186/s12889-016-2700-2.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 179: Response to proposed guidelines regarding alcohol consumption in “Guidelines for a Healthy Diet” from the the Health Council of the Netherlands – 26 January 2016
The Health Council of the Netherlands has published “Guidelines for a Healthy Diet” that include a section related to alcohol consumption. Our Forum has been asked to provide comments on the alcohol guidelines (an English translation of certain sections related to alcohol consumption are attached as an appendix to the full review of these guidelines). The closing guidelines given in the Dutch document are as follows: “Do not drink alcohol, or at least no more than one glass per day. [The guidelines from 2006 recommended limiting one’s alcohol intake to one glass (women) or two glasses (men). The current data suggests that the guideline for men should be adjusted downwards.]”
Forum members were concerned that the guidelines were based on a very restricted number of the many hundreds of excellent epidemiologic and experimental publications in recent years that clearly indicate that moderate alcohol has favorable effects on most of the diseases of ageing, and on total mortality risk. For example, the proposed guidelines focus on adverse effects of alcohol on lung cancer, while current scientific knowledge suggests that it has negligible effect. Much of the discussion in the guidelines focusses on the dangers of alcohol on cancer, whereas data show that almost all of the risk (except for breast cancer) is from heavy drinking, not light-to-moderate drinking. Data strongly support a major role of alcohol abuse for upper aero-digestive cancers, but only minor effect on cancer in general from light-to-moderate drinking, especially when other lifestyle factors and under-reporting of intake are taken into account.
The findings for a benefit of moderate drinking on cardiovascular disease among middle-aged and older adults are very much under-played, despite overwhelming data showing a significant benefit. The “J-shaped” curve (lower risk of many diseases with light-to-moderate alcohol intake with higher risk for heavier drinking) is not presented in the guidelines, a major omission when presenting data on alcohol to the public. The additional protection against disease when moderate alcohol consumption occurs with meals was not mentioned. As one Forum member commented: “When professionals discuss alcohol consumption, what consumers want to know is first ‘how much,’ and then ‘when’ to drink.”
Overall Forum members considered that the proposed guidelines regarding alcohol consumption from the Health Council of the Netherlands in a number of sections do not reflect current scientific knowledge on the association of alcohol to health and disease. Forum members tend to agree with the statement of Boffetta and Hashibe who, in an extensive review of alcohol and cancer, stated that “Drinking, especially heavy drinking, increases cancer risk. However, total avoidance of alcohol, although optimum for cancer control, cannot be recommended in terms of a broad perspective of public health, in particular in countries with high incidence of cardiovascular disease.”
Forum members consider that it is important to describe both the potential harms and benefits for health associated with alcohol consumption, especially for middle-aged and older adults. The “J-shaped” curve should be an important concept in any guidelines on drinking that are presented to the public.
Reference: An English translation provided to the Forum includes parts of Section 8 of the Guidelines for a Healthy Diet, from the Health Council of the Netherlands; this material is included as an Appendix to the full report of this critique.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 178: The association of alcohol intake with health-related quality of life — 12 January 2016
Many studies have shown that moderate alcohol drinkers tend to have higher ratings of their quality of life (QOL) than non-drinkers. The directionality of this association has been difficult to ascertain: does moderate drinking improve someone’s QOL, or do people with higher QOL to begin with tend to drink alcohol moderately? The present study attempts to provide data designed to evaluate the directionality of these associations for both physical aspects of QOL as well as mental aspects.
Forum reviewers considered this to be a very well-done study from the Nurses’ Health Study II, with excellent and repeated measurements of both alcohol consumption and indices of QOL. It deals with the assessment of both physical and mental aspects of quality of life as well as the directionality of such an association: subjects were repeatedly assessed for the effects of alcohol intake on subsequent QOL as well as the effects of a given QOL measure on subsequent alcohol intake.
The key reported findings of this study were a positive association between alcohol and subsequent indices of physical QOL indices, with the poorest outcomes in abstainers and former drinkers; in spline analyses, the favorable effect appears to be up to about 2 drinks/day. Subjects with higher physical QOL also appeared to consume more alcohol in subsequent assessments. Somewhat surprising was the finding of little relation between alcohol and mental aspects of QOL, and even an apparent deleterious effect at the highest category of drinking. Thus, the study reports that physical aspects of QOL are positively associated with alcohol consumption, while mental aspects show little relation.
There was some concern by some Forum members about the methods used by the authors in adjusting, or not adjusting, for previous exposures (both alcohol and indices of QOL). Given that both baseline alcohol intake and QOL measures may tend to remain rather static over the period of the study (this “prevalent” exposures), adjusting for the effects of baseline values could attenuate any effect seen on subsequent outcomes. For example, if alcohol consumption indeed affects QOL and consumption remains roughly the same over the time period of the study, any effect of subsequent alcohol on QOL may be subsumed by the effects shown at baseline. In that situation, the net effect of adjustment for baseline alcohol may attenuate (or remove) the effect of the follow-up exposure on the outcome variable. The authors of this paper were aware of this problem, and attempted to deal with it. However, from the data presented, it is not possible to ascertain the specific analytic procedures used, and the final estimates of effect given for alcohol and QOL may still be biased.
Overall, the Forum considers this to be an important contribution to our understanding of how alcohol consumption may affect quality of life, and how quality of life affects alcohol consumption. As interpreted by the authors, physical aspects of QOL may be positively affected by alcohol consumption, but there is little effect on mental aspects of QOL.
Reference: Schrieks IC, Wei MY, Rimm EB, Okereke OI, Kawachi I, Hendriks HFJ, Mukamal KJ. Bidirectional associations between alcohol consumption and health-related quality of life amongst young and middle-aged women. J Intern Med 2015, pre-publication. doi:10.1111/joim.12453.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 177: A clinical trial testing the effects of alcohol on inflammatory markers — 21 December 2015
While there have been many observational studies of the relation of alcohol consumption to health risks and benefits, the number of clinical trials of alcohol administration for its health effects are limited. The present paper is based on a controlled diet cross-over trial among 53 postmenopausal women. A standard diet was provided for a period of 6 months; two meals each weekday were consumed at the study facility and food was provided for other meals. To the standard meal, during three 8-week interventions, either 0, 15 g, of 30 g of alcohol (ethanol) were added to the daily diet, with the two doses of alcohol the equivalent of a little over one typical drink and 2 ½ typical drinks. Weight remained stable and no adverse effects were reported.
The key results of the trial were that, during periods when alcohol was consumed, there were small but significant decreases in markers of cellular adhesion molecules and components in the hemostatic pathway; these are indices of inflammation and the effects are consistent with a decreased risk of cardiovascular disease (CVD). Specifically, reductions were seen when alcohol was administered for s-ICAM, fibrinogen, and D-dimer, all of which would be expected to lower CVD risk. PAI-1 increased with alcohol, and there were no effects on CRP, Factor VIIc or IL-6.
While there were a number of question about the study, Forum members considered that, overall, this was a very well-done, difficult-to-carry-out study that shows alcohol’s beneficial effects on a number of inflammatory and hemostatic factors. The results are in line with many observational studies, although some previous intervention studies have found such effects only after the administration wine (but not of gin), suggesting a key effect of the polyphenols in wine. This study indicates that ethanol itself may have similar beneficial effects on mechanisms that relate to the development of cardiovascular disease.
Reference: Stote KS, Tracy RP, Taylor PR, Baer DJ. The effect of moderate alcohol consumption on biomarkers of inflammation and hemostatic factors in postmenopausal women. European J Clin Nutrition 2015; advance online publication. doi:10.1038/ejcn.2015.182
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 176: A New Report on Alcohol Consumption and Total Mortality Risk — 14 December 2015
Most observational studies have found that moderate drinkers, in comparison with nondrinkers, tend to have lower risk of all-cause (total) mortality; this is probably related primarily to a reduction in the risk of cardiovascular disease, the leading cause of death among the elderly. This large study has conflicting findings, as the author claims that the present analyses do not demonstrate protection against mortality from light-to-moderate drinking. In this study, what were termed “occasional drinkers,” rather than nondrinkers, were used as the comparison group.
Forum members had two main concerns about this study that warrant an investigation of the author’s conclusions: there was no consideration of under-reporting of alcohol intake when declaring “occasional drinkers” as the referent group, and (2) the inclusion, and adjusting for as “confounders,” several factors that are actually mechanisms by which alcohol has been shown to reduce mortality.
The first concern could have led to many light drinkers being included in the referent group, and thus not evaluated for a potential protective effect of light drinking on mortality. In fact, presented only in the Appendix to the paper are data showing that when nondrinkers make up the referent group, consumers of 1-7 as well as 7-14 drinks per week show significant 20-30% reductions in the risk of mortality; these findings are very similar to those of most previous epidemiologic studies.
The second, and perhaps more important concern, is that some of the mechanisms by which moderate alcohol intake may lead to lower mortality, such as reducing the risk of diabetes and coronary heart disease, were “adjusted” for in the analyses. This would attenuate or even erase any true reduction in risk of mortality from moderate drinking.
Some Forum members also were concerned that some subjects were missing data on alcohol consumption but, rather than excluding them, an estimated value was imputed for them. Further, data on the pattern of drinking (regular moderate versus binge drinking) or on the type of beverage consumed were not included in the evaluation.
Forum members conclude that the results of this study will obviously be considered in conjunction with other scientific data when seeking to judge the relation of alcohol intake to mortality. However, concerns about the analysis raise questions about the conclusion of the author of no protective effect of alcohol on mortality, a finding that conflicts with the results of most previous studies.
Reference: Goulden R. Moderate Alcohol Consumption Is Not Associated with Reduced All-cause Mortality. Am J Med 2015; pre-publication. http://dx.doi.org/10.1016/j.amjmed.2015.10.013.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 175: An update on the association of alcohol consumption with breast cancer: Effects of BMI — 24 November 2015
Most observational epidemiologic studies have shown a slight increase in the risk of breast cancer for women who consume alcohol; the degree of increase is usually small for light-to-moderate drinkers (between 5% and 15% increase for consumers of no more than one drink/day), but the risk may be higher for women consuming greater amounts of alcohol. However, there are a number of factors that affect this relationship, including the type of study (cohort or case-control), the pattern of drinking (regular versus binge), the type of beverage consumed, folate intake, use of hormone replacement therapy, as well as genetic factors. It has also been shown that the risk of breast cancer among obese women tends to be higher than among non-obese women, but there are limited data on how obesity interacts with alcohol in affecting the risk of breast cancer. It is clear that alcohol consumption cannot be evaluated in isolation, without considering other factors that relate to the development of breast cancer.
The present study is based on a large cohort of Swedish women who were examined as part of the Women’s Lifestyle and Health Study in 1991 – 1992, then followed through 2009 for the development of breast cancer: 1,385 cases were ascertained among the more than 45,000 women in the study. Alcohol was assessed at baseline and again at the follow-up examination, and the diagnosis of breast cancer was gleaned through linkage to the nationwide health registries in Sweden. Almost all of the women were pre-menopausal at baseline.
Forum members considered this to be a very well-done study, with almost complete ascertainment of cancer cases. There were some concerns, however, including the fact that the height and weight of subjects was not measured but self-reported, perhaps resulting in less accurate estimates of BMI. Further there may have been residual confounding from other factors related to breast cancer that were not assessed. Finally, the reported levels of alcohol consumption among the women in this study were very low (72% of the cohort drank either zero alcohol or below 5 g per day), but it cannot be determined if these are indeed the levels in this population or whether there may have been under-reporting of consumption.
The key findings as reported by the authors were that, overall, there was “no statistically significant association between alcohol intake and breast cancer risk after adjustment for confounders.” While this is indeed supported by their data, Forum members warned that readers should also note that there was an increase in risk found in less-obese women (BMI ≤ 25 kg/m2), among whom there was a step-wise increase in the risk ratio for cancer from 1.0, to 1.05, to 1.19, to 1.32 with increasing category of alcohol intake. This association was not seen in the more obese women for total cancer or for any of the sub-categories of cancer.
While the overall results did not show an increase in risk from alcohol intake, the results among non-obese women are similar to those seen in many other studies, and suggest a slight increase in the risk of breast cancer associated with alcohol for at least some women. The differences in effect according to BMI reported by the investigators are interesting and add to our understanding of the association of alcohol with breast cancer which, however, remains unclear.
Reference: Shin A, Sandin S, Lof M, Margolis KL, Kim K, Couto E, Adami HO, Weiderpass E. Alcohol consumption, body mass index and breast cancer risk by hormone receptor status: Women’ Lifestyle and Health Study. BMC Cancer 2015;15:881 (DOI 10.1186/s12885-015-1896-3)
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 174: Two-year clinical trial of wine administration in diabetics who were previous abstainers or very-light drinkers — 19 October 2015
Observational epidemiologic studies have consistently found that moderate drinkers are at lower risk of cardiovascular disease (CVD); such alcohol consumption also lowers both the risk of diabetes as well as of CVD among diabetics. However, there have been few clinical trials of the administration of alcohol or wine among diabetics, and most have been for relatively short periods of time. Forum members welcomed the publication of the results of the present study, and consider that it provides valuable information on the relation between wine and cardiometabolic risk.
In this study, among 224 subjects with diabetes aged 40 to 75 years who were abstainers or very light drinkers (previously reported none or < 1 drink/week), the investigators carried out a randomized clinical trial of the effects of wine on cardiometabolic factors. The subjects were randomly assigned to 150 mL of mineral water, white wine, or red wine with dinner for 2 years; all groups followed a Mediterranean diet without caloric restriction. The study was described to subjects as a dietary intervention, and there were group sessions led by clinical dietitians each month for the first three months and then at 3-monthly intervals thereafter. The focus was on the Mediterranean diet, and wine was not discussed at these meetings. There was excellent compliance with the provided beverages (>80%) and excellent continued participation of subjects (94% for one year and 87% for the full two years).
The key results of this study were that the administration of 150 ml of red wine with dinner each evening, in comparison with mineral water, favorably affected many cardiometabolic factors, and especially led to an increase in HDL-cholesterol and apolipoprotein (a). The administration of similar amounts of white wine was also beneficial, and specifically improved measures of glycemic control.
Further, in 203 of the subjects, effects according to the genetic factors determining ADH were evaluated. In the study, 35.6% of subjects were homozygous for the polymorphism for “slow ethanol metabolism,” 21.3% were homozygous for that for “fast ethanol metabolism,” and 43% were heterozygous. Forum members agreed with the summary statement of the authors: “We found that diabetic patients who were slow alcohol metabolizers had improved glycemic control by initiating moderate wine consumption, which suggests that alcohol may play a role in glucose metabolism. In contrast, diabetic patients who were fast ethanol metabolizers benefited the most from the wine-induced BP-lowering effect, which suggests a mediatory role for ethanol metabolites.”
The study has important implications for advice to be given to diabetics. Most, but not all, Forum members agreed with the authors’ conclusion that “Initiating moderate wine intake, especially red wine, among well-controlled diabetics as part of a healthy diet is apparently safe and modestly decreases cardiometabolic risk.”
Reference: Gepner Y, Golan R, Harman-Boehm I, . . . Stampfer MJ, Shai I, et al. Effects of initiating moderate alcohol intake on cardiometabolic risk in adults with type 2 diabetes. A 2-year randomized, controlled trial. Ann Intern Med 2015; pre-publication. doi:10.7326/M14-1650
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 173: A Large Study of the Association of Alcohol with the Risk of Acute Myocardial Infarction — 15 October 2015
This paper presents prospective data from a large population-based cohort from rural Norway, a region with typically light alcohol drinking and many abstainers who were not ex-heavy drinkers. It relates reported alcohol intake, assessed on two occasions, with the risk of developing an acute myocardial infarction (AMI). Its key findings are that, even in this very light-drinking population, drinkers had significantly lower risk (about 20% to 30%) of developing a MI than non-drinkers. As the authors conclude: “Light-to-moderate alcohol consumption was linearly associated with a decreased risk of AMI in a population in which abstaining from alcohol is not socially stigmatized. Our results suggest that frequent alcohol consumption is most cardioprotective and that this association is not driven by misclassification of former drinkers.”
As this was a rather homogeneous rural cohort without huge differences among subjects in socioeconomic status, it allows much better control of confounding. The fact that these results show essentially a continuous inverse association (rather than the usually seen “J-shaped” curve) is not unexpected given the very few heavy drinking subjects in this cohort. In addition to cardiovascular disease, the investigators also reported effects on total mortality, which showed a “J-shaped” curve.
Forum members considered this to be a very well-done study, and supports almost all previous research showing a protective effect of moderate drinking on the risk of coronary heart disease. The authors had good data on alcohol exposure and the occurrence of AMI. A key result from this study is that frequent light drinking, even less than an average of one drink/day, is associated with a significant decrease in the risk of coronary heart disease. Based on this study and most previous research, the clear message to the public remains: if you have no contraindications to alcohol use and decide to consume an alcoholic beverage, the healthiest approach is to drink frequently but in small amounts.
Reference: Gémes K, Janszky I, Laugsand LE, Lászlo KD, Ahnve S, Vatten LJ, Mukamal KJ. Alcohol consumption is associated with a lower incidence of acute myocardial infarction: results from a large prospective population-based study in Norway. J Intern Med 2015; doi: 10.1111/joim.12428.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===========================================================================================================
Critique 172: Alcohol and the risk of developing diabetes — 7 October 2015
Prospective cohort studies for decades have tended to show that the risk of developing Type II diabetes mellitus is reduced among moderate drinkers in comparison with non-drinkers, with previous meta-analyses suggesting that moderate drinkers may have about 30% lower risk than that of abstainers. The present study carried out a multi-language search for studies on alcohol and diabetes and conducted a meta-analysis involving almost two million subjects from a final group of 38 cohort, case-cohort, case-control, or nested case-control studies. The main conclusions of the authors are that only females may show a significant inverse association between alcohol consumption and the risk of diabetes, and that previous studies may have overestimated the reduction in risk from moderate drinking.
Forum members had concerns about the analyses and the conclusions of the authors, as the males in the study were primarily Asian (86%), and there were huge differences between the associations with alcohol for Asian and non-Asian populations. There are always problems when the basic study data have a marked degree of heterogeneity. In general, many of the factors that relate to diabetes (diet, body size and adiposity, type of beverages consumed, etc.) are quite different between Asians and non-Asians; combining such groups when their analyses show opposite effects of alcohol on diabetes risk may not be a reasonable way of trying to develop results that apply globally. Forum members do not believe that the analyses presented in this paper can support the conclusion of the authors that there is “no effect among males.” It could be unwise if the results of this study were used to develop alcohol guidelines for western populations.
The authors could not take the pattern of drinking (regular versus binge) or the type of alcohol into consideration. Clinical trials have suggested that wine and its polyphenols may have effects above and beyond those seen with alcohol alone, and beneficial effects of such polyphenols have been demonstrated both for women and for men. Thus, while the analyses in this paper were all carried out accurately, attempting to use these data to develop guidelines that would apply globally, as was done by the authors, may not be appropriate.
Reference: Knott C, Bell S, Britton A. Alcohol Consumption and the Risk of Type 2 Diabetes: A Systematic Review and Dose-Response Meta-analysis of More Than 1.9 Million Individuals From 38 Observational Studies. Diabetes Care 2015;38:1804–1812 | DOI: 10.2337/dc15-0710
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 171: A global assessment of alcohol and health — 29 September 2015
The present publication is from the very large Prospective Urban Rural Epidemiological (PURE) study that focuses especially on middle-income and lower-income countries, for which previous data on the association of alcohol consumption with health outcomes are sparse. Included in this analysis are data from high-income countries (HICs: Sweden and Canada); upper-middle-income countries (UMICs: Argentina, Brazil, Chile, Poland, South Africa and Turkey); lower-middle-income countries (LMICs: China and Columbia); and low-income countries (LICs: India and Zimbabwe). The large majority of the subjects were from lower income countries.
It has long been recognized that, when evaluating the health effects of drinking, it is especially important to evaluate alcohol intake within a particular population, with its specific genetic, lifestyle, environmental, and cultural factors, and not study alcohol in isolation. While the PURE study is a very well-done study, Forum members were concerned that the authors have attempted to answer overall questions about alcohol and health by combining data from such diverse populations. For example, the issue of very different causes of mortality in different populations would lead to very different approaches to improving longevity. There are too many factors associated with health outcomes to attempt to determine the specific alcohol effects when considered in isolation.
The authors tried to adjust for confounders as far as that was possible, but one cannot exclude further confounding, especially as subjects from lower-income countries contained a much larger proportion of smokers than there were in higher-income countries. The authors also point at differences between countries not fully explained by drinking pattern (or other factors); this suggests that further confounding exists. Further, lumping all types of stroke into one category may be hiding associations, especially as lower-income countries might have a higher frequency of cerebral hemorrhages. Similarly, using a single grouping for all cancers may be inadequate. Other limitations of this study include the short duration of follow-up time (4.3 years) and the low number of cases of each outcome.
The Forum concluded that even though the study includes information from many countries, it is not possible from such data to determine net health effects of alcohol consumption that are applicable to people everywhere. Their analytic results cannot be used, as the authors suggest, to “support global health strategies,” although they may surely be useful for developing “national initiatives to reduce harmful alcohol use,” especially for lower-income countries.
Reference: Smyth A, Teo KK, Rangarajan S, O’Donnell M, Zhang X, Rana P, Leong DP, et al. Alcohol consumption and cardiovascular disease, cancer, injury, admission to hospital, and mortality: a prospective cohort study. Lancet 2015. Pre-publication. http://dx.doi.org/10.1016/ S0140-6736(15)00235-4. Online/Comment http://dx.doi.org/10.1016/ S0140-6736(15)00236-6.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 170: An update on the association of alcohol consumption with the risk of cancer — 1 September 2015
This well-done analysis based on data from two very large cohort studies, the Nurses’ Health Study and the Health Professionals’ Follow-up Study, evaluated the association of alcohol consumption over many years with the risk of cancer. The authors conclude that men reporting an average intake of more than 15 grams of alcohol per day, but not less, have a significant increase in risk of alcohol-related cancers. In women, however, even the consumption of an average of 5.0 – 14.9 grams of alcohol per day (the equivalent of between ½ and 1 ½ typical drinks) was associated with a slight increase in total cancer risk, stated to be primarily from an increase in the risk of breast cancer. For both genders, there seemed to be a dose-response increase in risk of cancer with larger amounts of alcohol. At the same time, smoking was identified as an even more important risk factor than alcohol for these cancers.
Forum members considered this to be an important study presenting data that are of relevance to individuals and agencies providing advice regarding alcohol consumption. There is little question that heavy drinking markedly increases the risk of upper aero-digestive cancers, and no physician or agency advises people to consume in excess of the typical limits of no more than one or two drinks/day. Hence the finding in this study of an increase in some cancers among women (especially breast cancer) even for lighter drinking has implications for alcohol policy.
The Forum was disappointed that all dietary and other lifestyle factors that have been shown to increase the risk of cancer (data that are known to be available to these investigators) were not included in their report. Members were especially concerned that the net effects on health and mortality of light-to-moderate alcohol consumption were not commented upon in the paper. Given that the risk of the most common causes of death, especially cardiovascular diseases, are reduced by moderate drinking, it seems that the authors should have included data, or at least mentioned, the effects of alcohol on cancer mortality and, especially, on total mortality. It has recently been emphasized that cohort studies that report on only one outcome (in this case, cancer) but do not mention other outcomes that are affected by the same exposure, especially total mortality, do not present the full picture, and can lead to biased recommendations. The inclusion of such information from these cohorts could provide even more valuable data upon which to develop appropriate guidelines for alcohol use by individual patients and the public.
Reference: Cao Y, Willett WC, Rimm EB, Stampfer MJ, Giovannucci EL. Light to moderate intake of alcohol, drinking patterns, and risk of cancer: results from two prospective US cohort studies. BMJ 2015;351:h4238; doi: 10.1136/bmj.h4238
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 169: Effects of IQ on risk of morbidity and mortality related to alcohol consumption — 25 August 2015
The present paper is based on a large cohort of subjects in Sweden who had IQ tests as children (when they were 13 years old) and were then followed for more than 30 years. The study reports an inverse association between childhood IQ and hospitalization for alcohol-related diseases or death. The association is strongly dose-dependent, with a marked increase in disease/mortality risk for each decrease in the childhood IQ score.
A key finding in this analysis is that the attained socio-economic status (SES) of the subjects at age 32 played a large role in explaining the association between IQ and alcohol-related disease and appeared to completely explain the association with death from alcohol-related causes. This suggests that much of the effect of IQ during childhood may be through its effect on later education, occupation, and income of the subjects, associations that have been noted in many previous epidemiologic studies to favor better health. It is reassuring that being born into a poor, uneducated family is not as important as a determinant of adverse effects of alcohol later in life as is the attained socio-economic status of the individual in young adulthood.
A possible explanation for the inverse relation of SES in young adulthood with adverse alcohol outcomes could relate to the type of beverage consumed, which was not evaluated in the present analysis. In a previous study from Denmark, it was shown that higher SES in young adults was associated with a strong preference for wine rather than for other types of alcoholic beverage. Wine consumption has been associated with better health in numerous studies, although it is unclear whether this is due primarily to the non-alcoholic constituents in wine or to confounding from associated lifestyle factors of wine drinkers.
Forum members agree with the authors that the underlying causes for an association between IQ (or SES) and adverse alcohol-related disease and death are not clearly defined. It could be that intelligence has effects on health through choices in lifestyle behavior or socioeconomic environment as an adult, or the relationship between intelligence and health is confounded by other factors such as biological or socioeconomic conditions early in life. As for now, we can only describe the association, but not explain it fully.
Reference: Sjölund S, Hemmingsson T, Gustafsson JE, Allebeck P. IQ and alcohol-related morbidity and mortality among Swedish men and women: the importance of socioeconomic position. Journal of Epidemiology and Community Health 2015;69:858-864.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 168: Effects of alcohol on blood pressure in women: A randomized trial — 5 August 2015
The present paper describes the effects among 24 normotensive pre-menopausal women, all of whom were regular drinkers (of an average of 2 to 3 drinks/day), of the administration of two levels of alcohol in the form of red wine in a randomized clinical trial. Subjects were given low amounts of wine and higher amounts of wine during two 4-week intervention periods, with the effects on blood pressure compared with changes when subjects were given similar amounts of dealcoholized red wine. Subjects were divided into a “lower level” usual intake group who previously consumed < 200 g/week of alcohol and a “higher level” group who previously consumed >200 g/week.
Previous “lower level” drinkers were given two levels of alcohol, in the form of 100 ml/day of red wine on 4 days per week (an average of 46 g/week of alcohol, or the equivalent of about ½ typical drink per day) and 200 ml/day of red wine daily (about 146 g/week of alcohol, the equivalent of about 1 ½ to 2 typical drinks/day) for another 4-week period. Subjects who were previous “higher level” drinkers were given 100 ml of red wine daily (about 73 g/d of alcohol per week, the equivalent of about one typical drink/day) for 4 weeks and 300 ml/d of red wine (about 218 g/week of alcohol, the equivalent of about 2 to 3 typical drinks/day) for another 4 weeks.
The main results are a small but significant increase in 24-hour average blood pressure (+2.0 mmHg systolic and +1.3 mmHg diastolic) with higher levels of red wine but no significant effects (+0.4 mmHg systolic, -0.3 mmHg diastolic) from lower levels of red wine administration, when compared with blood pressure levels during periods when dealcoholized red wine was given. The differences were predominantly due to slightly higher awake rather than asleep blood pressures. These findings are similar to results of a limited number of randomized controlled trials of alcohol in men.
Forum members considered this to be a well-conducted clinical trial, with important results. There were, however, some concern that the study focused only on regular drinkers; results may have been different if previous abstainers had also been studied. Further, while the slight increase in blood pressure from higher levels of alcohol support previous research, the finding of no significant findings for lower levels of intake (when subjects were given the equivalent of between ½ and 1 drink/day) may not support what the authors suggest: “Our results provide no support for the concept that regular low-level alcohol intake can lower BP, suggesting that the J-shaped relationship between alcohol and BP in several studies is more likely because of the presence of unmeasured confounders.” Forum members considered their results to be consistent with either a slight increase or a slight decrease in blood pressure among such drinkers and are not necessarily inconsistent with data from some previous cohort studies that showed a “J-shaped” relation between alcohol and blood pressure.
A number of Forum reviewers also raised the question as to whether or not the results of a 4-week intervention study can be extended to the effects of the regular intake of alcohol for many years. Further, the fact that the study group included previous drinkers of up to similar amounts of alcohol as given during the higher intervention (yet were still normotensive) might suggest that their blood pressure was not “sensitive” to alcohol, and could limit the applicability of these results to the general public. Nevertheless, this intervention study provides important trial data on the short-term effects of alcohol on blood pressure.
Reference: Mori TA, Burke V, Beilin LJ, Puddey IB. Randomized Controlled Intervention of the Effects of Alcohol on Blood Pressure in Premenopausal Women. Hypertension 2015;66:00-00. DOI: 10.1161/HYPERTENSIONAHA. 115.05773
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 167: What determines a person’s belief that “alcohol is heart-healthy?” — 22 July 2015
This paper, based on data from more than 5,000 adults participating in an internet-based survey, sought to determine what were the perceptions of subjects on the relation of alcohol to heart disease, and how these perceptions resulted in particular behaviors related to alcohol consumption. Partricipants for the survey were recruited by a variety of methods, including announcements “in the lay press, promotional events, word of mouth, social media, e-mail, and clinic visits.” While the goal of the study is commendable, the results of any such survey obviously depend on many social and cultural factors of the people who respond to the survey; it was not a random sample of the population used in this analysis. This is critical because an interpretation of the data requires an understanding of the population surveyed.
Forum members had other concerns about this paper, including the specific survey questions regarding the perceptions of alcohol effects. For example, the key question asked in the survey was “Do you believe alcohol is good for your heart?” Forum members pointed out that it is obvious to nearly everyone that this cannot be answered without quantifying the amount of alcohol or the pattern of drinking. They consisdered that a more appropriate quesiton might be something such as “Do you believe that the moderate consumption of alcoholic beverages can benefit your heart?”
The authors make statements such as “Participants perceiving alcohol as heart healthy consumed 47% more alcohol.” This may sound alarming until it is revealed that the observed difference was from a baseline of 0-3 to 1-5 glasses of wine/week and from 1-7 to 2-8 total drinks/week. These higher amounts are not ‘alarming’ at all, and in fact fall within usual guidelines for “sensible drinking.”
Forum members were particularly upset that the authors misquote a number of scientific papers to support their claim that even low levels of drinking increase the risk of certain diseases. The authors also use such misrepresentations of data to justify their concerns that current guidelines for alcohol consumption may not be appropriate. Forum reviewers found it especially disturbing that the peer review process by the journal failed to uncover such misrepresentations of data.
The authors repeatedly give the impression that they are against any amount of alcohol consumption. They do not comment on the consistent findings in almost all well-done prospective studies indicating that moderate drinkers live longer than abstainers. Further, statements by the authors that suggest that people who think that alcohol is heart healthy are misinformed does not stand up to scientific data, which indicate that moderate and responsible drinking is associated wtith better health and longevity.
It is interesting that the report indicates that older, higher-income, and more highly educated subjects are more likely to consider alcohol to be heart healthy than younger and less-educated subjects. While a question was asked by the investigators as to whether or not the responder’s perception of the health effects of alcohol influences their decision to drink or to not drink, the specific responses to this question are not presented in the paper. It remains unclear to what extent beliefs about alcohol’s potential health effects relate to alcohol use or, more importantly, to alcohol abuse.
Overall, Forum members thought that the idea behind this study was of interest, but emphasized that it is important to collect data based on a random and well described sample of the population if one is to provide significant and understandable results. Further, the report is compromised by what appears to be a deliberate misrepresentation of the prior scientific literature to support the authors’ contention that alcohol is not healthy; there are a number of obvious errors that should have been detected during the review process by the journal. In the opinion of the Forum, the most reliable result from these analyses relates to where people obtain their information regarding alcohol and health: it does not come from physicians or scientific publications, but primarily from the lay press.
Reference: Whitman IR, Pletcher MJ, Vittinghoff E, Imburgia KE, Maguire C, Bettencourt L, Sinha T, Parsnick T, Tison GH, Mulvanny CG, Olgin JE, Marcus GM. Perceptions, Information Sources, and Behavior Regarding Alcohol and Heart Health. Am J Cardiol 2015; pre-publication. http:// dx.doi.org./10-1016/j.amjcard/2015.05-029.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 166: The association between alcohol consumption and suicidal ideation and suicidal attempt — 1 July 2015
The present study evaluates the relation of alcohol consumption and the pattern of drinking with self-reports of suicidal ideation and suicidal attempts among more than 43,000 men and women in Korea, using data from a 2007-2011 survey. Overall, 11.3% of males and 21.2% of females reported that they had experienced suicidal ideation, and 0.8% of males and 1.1% of females had attempted suicide. High scores on the Alcohol Use Disorders Identification Test (AUDIT) and a history of alcoholic blackouts were associated with suicidal ideation among both men and women and, for males, with suicidal attempts.
There is little known about the epidemiology of suicidal tendencies, or the specific causes of suicide. It is generally agreed that depression is the most important risk factor for suicide, and depression can lead to alcohol abuse; however, alcohol abuse can also lead to depression. Unfortunately, with cross-sectional data, analyses such as those in this paper cannot sort out the confounding issues nor, more importantly, address the causality of alcohol consumption with suicidal tendencies. The egg and hen question has never been solved – whether the depression or the heavy drinking came first. Thus, whether alcohol abuse increases the risk of depression (that may lead to suicide) or whether depressed people turn to alcohol seeking relief, cannot be determined from analyses such as these. However, it is also noted that this study suggests that drinking alcohol according to the usual guidelines for “sensible drinking” (generally, advising no more than 1 to 2 drinks/day) is not associated with the risk of suicidal ideation or attempt.
Forum members also commented on the large differences between populations in suicidal tendencies, being much higher in Korea and Japan than in most of Europe and North America. This could limit the applicability of the conclusions of this study to western populations.
Reference: Bae H-C, Hong S, Jang S-I, Lee K-S, Park F-C. Patterns of Alcohol Consumption and Suicidal Behavior: Findings From the Fourth and Fifth Korea National Health and Nutritional Examination Survey (2007–2011). J Prev Med Public Health 2015;48:142-150 • http://dx.doi.org/10.3961/jpmph.14.027
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 165: Fiber intake may modify the association of alcohol consumption with certain hormone-dependent cancers — 4 June 2015
The positive association between alcohol intake and certain hormone-dependent cancers (especially breast cancer) noted in many studies has been attributed to an effect of alcohol through an increase in levels of estrogen and other hormones. The present study had extensive dietary data on more than 5,000 men and women in France, among whom comparisons were made between the sex-specific tertile of alcohol intake and the risk of hormone-related cancers (breast, prostate, ovarian, endometrial, and testicular).
The study found that, overall, the risk of some cancers (e.g., breast) but not others (e.g., prostate) were positively related to reported alcohol intake. The key results reported by the authors are that when the risks of cancer were related to alcohol while adjusting for fiber intake, subjects whose fiber intake was below the median value showed higher risks of cancer related to alcohol, but not subjects with higher fiber intake. For example, when the risk of breast cancer in women was related to the tertile of their alcohol intake, the 2nd tertile showed a HR of 1.55 (1.01 – 2.38) and the 3rd tertile (HR 1.70, CI 1.11 – 2.61), when compared with women in the lowest tertile.
For prostate cancer in men, however, the 2nd tertile showed a HR of 1.28 (CI 0.82 – 2.00) and the 3rd tertile a HR of 0.89 (CI 0.55 – 1.45). The interaction terms between alcohol intake and cancer were not significant for all hormone-dependent cancers or for breast cancer. Only the interaction term for prostate cancer reached statistical significance, but here the relationship between tertile of alcohol intake even among subjects with low dietary fiber did not show a clear dose-response relation.
Forum members had concerns about the large number of potential confounders in these analyses (e.g., different effects for different types of fiber, the intake of fiber being just a marker for folate intake or for other dietary or lifestyle factors), that made it difficult for the authors to reach firm conclusions. Unfortunately, the numbers of tumors for each of the sub-groups were often too small to give meaningful results. And there was no data on alcohol drinking pattern (regular moderate versus binge drinking) or type of beverage consumed. Thus, while this study indicates that alcohol intake may relate to certain hormone-dependent cancers, the analyses do not present a clear demonstration as to whether it is fiber intake or some other related factor that may modify the association.
Reference: Chhim A-S, Fassier P, Latino-Martel P, Druesne-Pecollo N, Zelek L, Duverger L, Hercberg S, Galan P, Deschasaux M, Touvier M. Prospective association between alcohol intake and hormone dependent cancer risk: modulation by dietary fiber intake. Amer J Clin Nutr 2015; pre-publication. Doi: 10.3945/ajcn.114.098418.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 164: Why are the harmful effects of alcohol consumption greater among people with low education and income? — 14 May 2015
Epidemiologists have noted for many years that one of the key factors that modifies the relation between alcohol intake and many diseases is the education, income, or other index of socio-economic status (SES) of subjects. While differences in drinking practices (regular moderate versus binge drinking), other more moderate lifestyle factors, better access to health care, etc., have been suggested as potential mechanisms, there has been little research directed at this relation.
The present study is a systematic review of published reports to investigate the relationship between SES and risk of mortality or morbidity for each alcohol-attributable condition and, where feasible, to explore alcohol consumption as a mediating or interacting variable in this relationship. It summarized data from 31 case-control or cohort studies, relating an overall measure of the effects of low SES (variously defined) to the risk of cancers related to alcohol, as well as to liver disease, hypertension, stroke, epilepsy, cardiac arrhythmias, and pancreatitis.
The key findings of the study demonstrate a tendency for greater risk for low-SES subjects than for high-SES subjects to develop a number of diseases that are associated with alcohol consumption. Specifically, the authors report higher and statistically significant increases in risk of head and neck cancer and of stroke associated with alcohol consumption among lower-SES subjects than among higher-SES subjects. There was a tendency for lower risk of breast cancer among lower-SES women, but differences were not significant when adjusted for known confounders. The authors suggest that some of the effects shown may relate to greater total amounts of alcohol consumption by lower-SES subjects, or due to their higher levels of smoking.
Forum members thought this was a valiant attempt of the authors to unravel what has been a mystery: why do people at lower levels of SES seem to have more adverse effects of alcohol consumption than subjects at higher levels of SES. Unfortunately, as the authors admit, current scientific data do not allow firm answers. Suggested theories for reasons why low-SES subjects may have more adverse effects from alcohol include (1) different drinking patterns, with more binge drinking, (2) clustering of poor lifestyle factors, and (3) less access to health care. In some studies, even though the reported total alcohol intake of low- and high-SES subjects may be similar, the latter seem more likely to drink moderate amounts of alcohol on a regular basis, while lower-SES subjects are more likely to binge drink on fewer days per week. However, other studies do not support such a finding. Further, there may be differences according to the type of alcoholic beverage consumed, which was not considered in this study.
Forum members pointed out that differences in factors other than drinking patterns probably contribute to the greater adverse effects among subjects with lower SES. One member suggested that lower SES affects susceptibility to many diseases, most likely due to effect modification of hitherto unrecognized factors. The Forum concluded that there are too many confounders to make a conclusion about this topic, and much more research will be needed to understand how socio-economic factors affect the risk of disease and may modify the relation between alcohol consumption and disease.
Reference: Jones L, Bates G, McCoy E, Bellis MA. Relationship between alcohol-attributable diseaseand socioeconomic status, and the role of alcohol consumption in this relationship: a systematic review and meta-analysis. BMC Public Health 2015;15:400. DOI 10.1186/s12889-015-1720-7.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 163: The association of alcohol consumption with the risk of developing heart failure — 5 May 2015
Two new papers have provided data on the association of alcohol consumption with the risk of developing heart failure (HF). The first is a meta-analysis by Larsson et al that is based on eight prospective studies, with more than 200,000 subjects and 6,211 cases of HF. Meta-analyses provide important information because they are usually based on very large numbers of subjects and cases, and can detect smaller increases in risk than seen in individual studies. However, single large prospective cohort studies tend to provide more detailed information on, and allow better adjustment for, potential confounders. The second paper discussed in this critique by Dorans et al, is based on 33,760 men who were followed for 14 years, with almost 3,000 cases of fatal or non-fatal HF.
There was a high degree of consistency between these two studies: both concluded that moderate alcohol consumption, in comparison with non-drinking, is associated with a lower risk of developing HF. The meta-analysis (Larsson et al) concluded that there was a dose-response association between alcohol and HF; for example, a reduced risks of HF for consumers of 3 and 10 drinks/week (a 10% and 17% decreased risk, respectively), but not for those reporting the consumption of 21 drinks/week (a RR of 1.07; 95% CI 0.77 – 1.48). In the report from the single large Swedish prospective study (Dorans et al), the risk of HF for most categories of drinkers tended to be lower than that of never drinkers, with the lowest risk among consumers of 7 – 14 drinks/week (HR=0.81, 95% CI 0.69 – 0.96).
Forum members considered both of these studies to have been very well done, and the similar results not unexpected. HF has many causes, but in developed countries the most common is coronary artery disease (CAD), and moderate drinking has long been known to be associated with a lower risk of developing CAD. In their critique, Forum members discuss other conditions that relate to the development of HF, including conditions (such as respiratory infection, excessive salt intake, non-compliance with prescribed medication, etc.) that may trigger an attack of symptomatic HF.
To summarize, based on previous research and these two excellent papers, current data suggest that the moderate intake of an alcoholic beverage lowers the risk of the development of symptomatic HF. This undoubtedly relates, as least to some extent, to the demonstrated protection of alcoholic beverages against CAD. As for giving advice regarding the consumption of alcohol, Forum members agree with the conclusions stated by Klatsky in his editorial accompanying one of the papers: “All persons should avoid heavy drinking and many persons should avoid all alcohol. However, it is the author’s opinion that many middle-aged and older persons at risk of CAD or HF should be told that he or she is better off as a light to moderate drinker. Dispassionate objectivity plus common sense should dictate advice about drinking.”
References:
- Larsson SC, Orsini N, Wolk A. Alcohol consumption and risk of heart failure: a dose–response meta-analysis of prospective studies. European Journal of Heart Failure 2015;17:367–373. doi:10.1002/ejhf.228
- Dorans KS, Mostofsky E, Levitan EB, Håkansson N, Wolk A, Mittleman MA. Alcohol and Incident Heart Failure Among Middle-Aged and Elderly Men: The Cohort of Swedish Men. Circulation Heart Failure 2015; pre-publication. DOI:10.1161/CIRCHEARTFAILURE.114.001787.
For the full critique of these papers, and general comments on the association of alcohol with heart failure, by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 162: What is the association between alcohol consumption and cancer? 13 April 2015
Three major papers on the association of alcohol consumption and cancer have recently been published. Forum members considered that all were well-done, and presented valuable new information on the topic. While the key findings in each study are similar, each brings specific information on how alcohol relates to the risk of developing cancer. In this critique, we present the authors’ abstracts of each paper, our comments on the paper, and then an overall discussion of the topic.
Problems can occur when combing case-control studies with prospective cohort studies, as was done in one of the papers reviewed, as risk estimates are usually higher in the former type of study and potential confounding may be less complete. Further, it is especially important to consider the interaction between alcohol consumption and smoking for upper aero-digestive tract cancer, as was not always done. And none of the studies covered in this critique emphasized the net effects of alcohol that, because of protective effects against cardiovascular disease, is almost always associated with lower total mortality among moderate drinkers than among abstainers.
In summary, the Forum considers that the three papers reviewed provide important data on one of very few lifestyle factors that have been shown to relate to the risk of cancer. And cumulative research data clearly show that heavy alcohol intake increases the risk of upper aero-digestive tract cancers and some other cancers. Further, in these and many previous reports, even light alcohol consumption was associated with an increase in risk of breast cancer in women. Unfortunately, the threshold level of drinking associated with an increase in risk is not clearly defined for most cancers.
Forum members agree with the conclusions of Klatsky et al, who stated: “At present, a possible increased cancer risk at moderate intake should enter into individual estimation of the overall risk-benefit equation for alcohol drinking, especially for young persons. For most persons older than age 50 years, the overall benefits of lighter drinking, especially the reduced risk of atherothrombotic disease, outweigh possible cancer risk.”
References:
-
-
-
- Klatsky AL, Li Y, Tran HN, Baer D, Udaltsova N, Armstrong MA, Friedman GD. Alcohol Intake, Beverage Choice, and Cancer: A Cohort Study in a Large Kaiser Permanente Population. Perm J 2015;19:March 1, 2015. http//dx.doi.org/10.7812/TPP/14-189
- Bagnardi V, Rota M, Botteri E, et al. Alcohol consumption and site-specific cancer risk: a comprehensive dose–response meta-analysis. British Journal of Cancer 2015;112:580–593. doi: 10.1038/bjc.2014.579
- Wienecke A, Barnes B, Neuhauser H, Kraywinkel K. Incident cancers attributable to alcohol consumption in Germany, 2010. Cancer Causes Control 2015;[Epub ahead of print].
-
-
For the full critique of these papers, and general comments on alcohol and cancer, by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 161: The effects of alcohol consumption on the risk of hip fracture — 31 March 2015
Among elderly people, falls leading to hip fracture are a major health problem, leading to severe morbidity and mortality. Underlying factors that increase the risk of hip and other fractures include osteoporosis and low bone mineral density, as well as an unsteady gait making falls more common. The role that alcohol consumption among the elderly may relate to hip fracture has been a topic of concern for many decades, but data from a number of prospective studies now suggest that light-to-moderate drinking may actually decrease the risk of such fractures, while heavy drinking may increase the risk.
The present meta-analysis is based on prospective studies that have yielded more than 26,000 incidences of hip fracture. It concludes that there is a “J-shaped” association between alcohol consumption, especially of wine, and the risk of hip fractures, with lower risk for a reported consumption of about 1 drink/day, no effect from drinking between 1 and 4 to 5 drinks, and an increased risk from heavier drinking. Part of the “protection” from light drinking is apparently from the effects of alcohol on increasing bone mineral density.
Forum reviewers considered this to be a very well-done meta-analysis that provides balanced information on the risk of this common public health problem. Noting that the major differences seen in this study were between light drinkers and heavy drinkers, it was commented that there are many differences between people who are moderate in their habits, including moderate drinking, and people who usually consume more than 4 or 5 drinks/day; thus, there is still the possibility of other lifestyle factors confounding this association. Also, it was noted that most of the subjects in this analysis were North American or European, so applicability to other racial/ethnic groups may be limited.
In summary, this large and very well-done meta-analysis supports a protective effect of light alcohol consumption on the risk of hip fracture, with an increase in bone density from alcohol being a probable important factor. Data suggest that wine consumption may have the most favorable effect, perhaps indicating that polyphenols and other compounds may also play a role. The study shows that heavy drinking (an average of 4 to 5 or more drinks/day) is associated with an increase in the risk of hip fracture.
Reference: Zhang X, Yu Z, Yu M, Qu X. Alcohol consumption and hip fracture risk. Osteoporos Int 2015;26:531–542. DOI 10.1007/s00198-014-2879-y
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 160: Do the calories in alcoholic beverages lead to increased obesity? — 23 March 2015
Among people who consume alcohol, it would be assumed that the excess calories provided by the alcohol would add to their risk of obesity; however, current data suggest that the association may be more complex. It is unclear to what extent people who consume alcohol may modify other aspects of their diets, either decreasing or increasing other sources of calories. Further, alcohol is metabolized differently from other foods, which suggests that its calories may not be as readily available as those from fat, carbohydrate, and protein to increase obesity. The present paper provides an update on scientific data on the association between alcohol consumption and obesity. The overall conclusions of the authors are that light-to-moderate drinking does not increase the risk of obesity, while heavier drinking (or even moderate drinking among obese subjects) may lead to weight gain.
Forum reviewers appreciated the excellent summary of scientific reports on this topic, and thought that the authors gave a sound and balanced update on the topic. However, mechanisms why numerous prospective epidemiologic studies show that moderate drinking does not increase the risk of obesity are unclear. Given that alcohol contains calories, and if drinking alcohol does not displace the intake of other foods, it would be assumed that such calories would increase the risk of obesity unless there are particular metabolic differences between alcohol calories and those from protein, fat, and carbohydrate.
Potential mechanisms suggested have included a decreased utilization of calories from alcohol due to what is known as ‘Non-exercise Activity Thermogenesis’ (NEAT), in which the metabolism of alcohol may create more heat than fat. Also, the Forum discussion included comments that alcohol could bring into play effects on insulin, glucose, and fat mobilization (however, in the laboratory, such mechanisms tend to increase, rather than decrease, body fat). Also, a reasonable interpretation of the fat tissue decrease related to ‘moderate’ ethanol intake seen in many studies could be an associated decrease in the intake of carbohydrates. One glass of wine substituting for approximately 50 g of glucose could be a reasonable mechanism for shifting the metabolism from lipogenesis to oxidation of lipids. Genetic factors undoubtedly play a role in the effects among individuals.
In summary, this update on the association of alcohol consumption and obesity concludes that most well-done prospective studies show that moderate drinkers do not have an increase in obesity, and in some studies there is even a slight decrease in weight. One possibility is that, especially for wine with meals, satiety may occur earlier and result in less intake of food. However, precise mechanisms for a lack of increase in weight are not known, and the effect could still result from drinkers compensating for their drinks by taking in fewer calories from other sources and perhaps also by being a little more physically active.
Reference: Traversy G, Chaput JP. Alcohol Consumption and Obesity: An Update. Curr Obes Rep 2015;4:122–130. DOI 10.1007/s13679-014-0129-4
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 159: Alcohol as a component of the Mediterranean-type diet; effects on the risk of mortality among diabetics — 17 March 2015
Many scientists have reported on health benefits associated with the traditional diet of much of the Mediterranean area: the primary basis of the diet is on plant-based foods (whole grains, vegetables, fruits), olive oil, moderate wine consumption, and limited intake of meat or dairy products. In 2003, Antonia Trichopoulou and her associates created a scoring system based on the number of components of the Mediterranean Diet (Med-Diet) consumed by subjects, giving a total score to judge the degree that individuals were following a Med-Diet pattern. The score is based on the intake of 7 items (cereal intake, ratio of monounsaturated to saturated fats, vegetables, fruits, nuts, fish, and moderate alcohol), considered to have positive effects, and 2 items (dairy products, meat and meat products) considered to have negative effects. Many groups have found that greater adherence to such a diet (a higher score) is associated with a lower risk of many diseases, and lower mortality. There are limited data on the relative merits of each component of the Med-Diet. In the present paper, the authors attempt to judge the proportion of the protection against mortality that can be attributed to each component of the score.
The authors’ calculations estimated that, in descending order of importance, moderate alcohol consumption (associated with a reduction of 14.7% in the protection against mortality when it was removed from the total score), cereal intake (12.2% reduction), ratio of monounsaturated to saturated fats (5.8%), and consumption of vegetables (5.8%), fruits and nuts (5.2%) and fish (5.0%) lowered mortality risk. Lower intakes of dairy products (reduction of 13.4%) and meat and meat products (3.4%) were also associated with lower mortality. Alcohol has long been known to relate to a lower risk of developing diabetes, and the present study indicates that it is an important factor in reducing the risk of mortality among subjects who have already developed diabetes, as has been shown in previous studies. This study indicates further that the full Med-Diet has very favorable effects on mortality among diabetics.
Forum members considered this to be a well-done attempt to tease apart the relative importance of each component of the Med-Diet as it relates to health outcomes among diabetics. They felt that these researchers from the MOLI-SANI study have published a convincing paper extending the known benefits of the Mediterranean diet to a cohort of type 2 diabetics, a group of subjects at high risk for cardiovascular and all-cause mortality.
There were some questions raised about the precision of the Med-Diet Score, as published and used in this study, in judging the relative contributions of the different dietary constituents, especially because of known complexities in judging the effects of avoiding one particular food when its absence may affect the intake of other foods. And for alcohol, the score used did not permit an evaluation of the role of the pattern of drinking or even the type of beverage consumed, which are known to affect the net effects of drinking on health.
Nevertheless, the results of this study add to an accumulating base of knowledge of the importance of the Mediterranean-type diet in reducing the risk of many health outcomes, including mortality among diabetics.
Reference: Bonaccio M, Di Castelnuovo A, Costanzo S, Persichillo M, De Curtis A, Donati MB, de Gaetano G, Iacoviello L, on behalf of the MOLI-SANI StudyInvestigators.
Adherence to the traditional Mediterranean diet and mortality in subjects with diabetes. Prospective results from the MOLI-SANI study. European Journal of Preventive Cardiology 2015. Pre-publication. DOI: 10.1177/2047487315569409.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 158: Comments on Alcohol Recommendations included in the Scientific Report of the 2015 Dietary Guidelines Advisory Committee – 4 March 2015
Note: The 2015 Dietary Guidelines Advisory Committee (Committee) submitted the Scientific Report of the 2015 Dietary Guidelines Advisory Committee (Advisory Report) to the Secretaries of the U.S. Department of Health and Human Services (HHS) and the U.S. Department of Agriculture (USDA) in February 2015. The purpose of the Advisory Report is to inform the Federal government of current scientific evidence on topics related to diet, nutrition, and health. It provides the Federal government with a foundation for developing national nutrition policy. However, the Advisory Report is not the Dietary Guidelines for Americans policy or a draft of the policy. The Federal government will determine how it will use the information in the Advisory Report as the government develops the 2015 version of the Dietary Guidelines for Americans. HHS and USDA will jointly release the Dietary Guidelines for Americans, 2015 later this year.
Sections of the Advisory Committee report related to alcohol are copied in the full Forum critique, which is available at www.bu.edu/alcohol-forum/critique-158. The full Advisory Committee report can be assessed at the following address: http://www.health.gov/dietaryguidelines/2015-scientific-report/PDFs/Scientific-Report-of-the-2015-Dietary-Guidelines-Advisory-Committee.pdf.
Forum Comments
Members of the International Scientific Forum on Alcohol Research (the Forum) have reviewed the sections of the Advisory Committee’s report that relate to the consumption of alcohol. They consider the report to be well written and a very clear statement on alcohol and health, one that generally reflects current scientific data.
Some Forum members thought that for dietary guidelines, there should have been more emphasis on the inclusion of moderate alcohol consumption as part of a Mediterranean-type diet, which is described in the report as being associated with very favorable health outcomes. The Forum found it interesting that the health problems associated with alcohol receive extensive detailed notice, but substantial favorable effects are barely mentioned. For example, while the comments on the increase in the risk of breast cancer are warranted, there is no mention that moderate alcohol consumption provides substantial protection against ischemic cardiovascular events, despite consistent and extensive data showing that the latter issue has a major public health benefit. Also, lacking any explanatory statements, the public and health professionals may be confused as to the basis for the recommendation that alcohol is “an important component of a healthy lifestyle.” So we recommend that some explanations for the statement, based on the relevant scientific literature, should be included. (Further, the report does not describe the favorable effects of moderate drinking on sociability, stress reduction, and relaxation, which are key reasons why most people consume alcohol in the first place.)
Despite our concerns, given that this is a statement that must get approval by a large number of governmental agencies and a variety of interested parties, it is consistent with current epidemiological data as well as mechanistic studies. The Forum strongly agrees that current scientific evidence indicates that, for mature adults without contraindications to alcohol use, moderate alcohol consumption can be included as a component of a balanced and healthy lifestyle.
For the full critique of the report by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 157: A mistaken interpretation of data relating alcohol to mortality – 20 February 2015
The authors of this paper have carried out a regression analysis to examine the association of reported alcohol consumption with all-cause mortality, dividing their sample into different age groups. They used data from Health Survey for England 1998-2008, linked to national mortality registration data. Their published results show lower risk of mortality (hazard ratios < 1.0 for mortality in comparison with recent non-drinkers and with never drinkers) for subjects in essentially all categories of moderate drinking. However, the authors have interpreted their analyses as indicating that moderate drinking is not associated with all-cause mortality for the vast majority of the population.
Forum members, and many other scientists, have been surprised by the conclusions of the authors, who apparently did not consider basic statistical principles (such as dealing with type-2 errors) in judging their results. The investigators appear to have looked only at p-values and ignored the estimates of effect in their own data, coming to the conclusion of no association between moderate alcohol and total mortality for most age groups. Focusing only on significance testing for estimating effects has been strongly condemned by epidemiologists and statisticians and can lead to inaccurate results.
The paper reflects a gross misinterpretation of the data, not what would be expected in a publication in a leading journal. In other words, the authors’ conclusions are not backed up by their data. A more appropriate headline based on this paper would be “Study supports a moderate protective effect of alcohol against all-cause mortality.” Given the wide media coverage of this article, with striking headlines indicating that moderate drinking does not affect mortality, one Forum reviewer wondered “How can more than 30 years of research in this field be undone by one misguided paper in the BMJ? Once in a while I reflect on how some doctors and journalists interpret scientific papers; they seem to rely more on abstracts and press releases.”
The Forum considers that the conclusions of the authors of this paper are simply not supported by the data provided. Rather, their findings are in accordance with those from previous prospective studies showing that, for all age groups, moderate alcohol consumption is associated with a decrease in all-cause mortality risk.
Reference: Knott CS, Coombs N, Stamatakis E, Biddulph JP. All cause mortality and the case for age specific alcohol consumption guidelines: pooled analyses of up to 10 population based cohorts. BMJ 2015;350:h384 doi: 10.1136/bmj.h384.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 156: The pattern of alcohol consumption and risk of cirrhosis — 10 February 2015
This paper, from a group of experienced investigators in Denmark using data from a large population-based cohort, attempted to judge how drinking pattern affects the risk of a subject developing alcoholic cirrhosis. From a cohort study of 55,917 participants (aged 50–64 years), the authors calculated hazard ratios (HRs) for alcoholic cirrhosis in relation to drinking frequency, lifetime alcohol amount, and beverage type. A total of 342 subjects developed alcoholic cirrhosis. The authors concluded that, in men, daily drinking was associated with an increased risk of alcoholic cirrhosis as compared with less frequent consumption; they also concluded that wine consumption might be associated with a lower risk of alcoholic cirrhosis that associated with the consumption of beer or liquor.
The major concern of Forum reviewers regarding this paper was the use of a diagnosis of “alcoholic cirrhosis” to judge the effects of alcohol on the disease; this was considered a type of circular reasoning. A diagnosis of alcoholic cirrhosis generally requires a history of alcoholism or heavy drinking, and subjects given that diagnosis would essentially be limited to those who were heavy drinkers. Thus, it would be no surprise to find a history of heavy drinking when evaluating alcohol as an exposure.
There was also concern about the implications of the author regarding frequency of drinking. The authors’ described in detail the relation of drinking pattern to liver cirrhosis, differentiating, in particular, effects associated with drinking daily versus drinking on 4-5, or 6 days a week. However, Forum members were concerned that as the overall average amount of alcohol for the daily drinkers exceeded that of those drinking less frequently, it was difficult to know if it was primarily the frequency of drinking (as concluded by the authors) or the total amount of alcohol consumed by subjects. The authors stated that they wanted to “execute evidence-based counselling,” which of course is praiseworthy, but Forum members had difficulty understanding why the effect of drinking 5-6 days/week should differ much from 7 days/week, especially if the usual amount was moderate. Indeed, the investigators state: “The mean alcohol amounts for daily drinkers were somewhat higher compared to those drinking less frequently in each category of alcohol amount, making it difficult to detangle the effect of drinking frequency and alcohol amount.” Forum members noted that the authors conclude that “daily drinking” was associated with increased cirrhosis, but they do not state daily drinking of how many drinks, which would be especially important. The study did not provide reliable data that would support alcohol-free days during the week.
The referent group in this study was made up of subjects reporting < 0 to 14 drinks/week, which would consist of light-to-moderate drinkers, those considered to be “sensible drinkers” in most cultures. Hence, it is no surprise that as subjects reported greater amounts of alcohol in the study, the risk of alcoholic cirrhosis increased. No one advises people to drink more than sensible limits. Further, there was a much higher risk of of cirrhosis among “current abstainers” than in the referent group, undoubtedly indicating that the current abstainers group included many former heavy drinkers.
Overall, the Forum thought that this paper raises, but does not answer, a number of questions about the relation of alcohol to the risk of cirrhosis: (1) Is wine really less liver-toxic than beer or liquor? (2) Should we really tell everyone to have one day each week without wine being included with their meal, or on which to avoid any alcohol? (3) Why is daily drinking, rather than 5 or 6 days per week dangerous for men but tends to be even slightly protective in women regarding liver disease? Because of concerns due to problems with bias from the diagnostic approach, the probability of under-reporting of alcohol consumption, and the lack of biological plausibility, we will need further scientific data to answer these important questions.
Reference: Askgaard G, Grønbæk M, Kjær MS, Tjønneland A, Tolstrup JS. Alcohol drinking pattern and risk of alcoholic liver cirrhosis: A prospective cohort study. Pre-publication. J Hepatol (2015) http://dx.doi.org/10.1016/j.jhep.2014.12.005.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 155: The effects of alcohol consumption on the risk of developing heart failure — 27 January 2015
An analysis of data from the large Atherosclerosis Risk in Communities (ARIC) study evaluated the effects of alcohol consumption at baseline, and the cumulative average intake based on several later assessments during a 24 year follow-up period, on the risk of the development of heart failure (HF). The authors conclude: “In this community, alcohol consumption of up to 7 drinks/week at early-middle age is associated with lower risk for future HF, with a similar but less definite association in women than in men. These findings suggest that despite the dangers of heavy drinking, modest alcohol consumption in early-middle age may be associated with a lower risk for HF.” The authors reported further that the risk of total mortality was higher than that of abstainers for former drinkers and for the heaviest drinkers, but did not demonstrate a “J-shaped” curve for total mortality (i.e., a lower risk for moderate drinkers in comparison with abstainers).
Forum members considered this to be a well-done analysis, with findings for a lower risk of HF among light-to-moderate drinkers consistent with many earlier reports. They noted that these findings may be somewhat affected by the inability of the investigators to include data on the pattern of alcohol consumption (regular moderate intake versus periodic binge drinking of similar total amounts) to disease. It would be expected that the relations between alcohol intake and HF (as well as with total mortality) would be stronger for regular moderate drinkers than for those who consumed their alcohol in binges (even if the total weekly average intake was the same). This could be one reason why a “J-shaped” curve was not seen for the relation of alcohol intake to total mortality in this study.
While coronary artery disease (CAD) is known to be a major precursor of HF, it is not clear from the data presented if the alcohol-HF relation may have differed between subjects with and those without CAD. For the effects of current heavy drinking, the implications from this study are limited because of the small number of such drinkers in this cohort; this was especially the case for women. The authors do not discuss the potential effects on their results of under-reporting of alcohol intake among their subjects; other studies have suggested means for identifying such subjects and ways of adjusting for such.
This study adds support to other large studies, including one just released as a pre-publication (see Addendum), that suggest that moderate alcohol consumption may reduce the risk of the development of heart failure. Some of this putative protective effect surely relates to a decrease in the risk of coronary artery disease among moderate drinkers. Heavy alcohol intake, especially among alcoholics, may increase the risk of both heart disease and heart failure.
Reference: Gonḉalves A, Claggett B, Jhund PS, Rosamond W, Deswal A, Aguilar D, Shah AM, Cheng S, Solomon SD. Alcohol consumption and risk of heart failure: the Atherosclerosis Risk in Communities Study. European Heart Journal, 2015, pre-publication; doi:10.1093/eurheartj/ehu514.
Addendum
Following the preparation of this critique, the pre-publication version of another paper has appeared: Larsson SC, Orsini N, Wolk A. Alcohol consumption and risk of heart failure: a dose–response meta‐analysis of prospective studies. European Journal of Heart Failure 2015; January, 2015. 10.1002/ejhf.228. According to its abstract, this paper is based on “a meta-analysis that included eight prospective studies, with a total of 202,378 participants and 6,211 cases of HF.”
While the Forum has not yet had an opportunity for a careful review of this new paper, the authors’ conclusions appear to provide strong support for the paper by Gonḉalves et al. The authors of the Larsson et al paper conclude their abstract by stating that when carrying out a dose-response meta-analysis, they “observed a non-linear relationship between alcohol consumption and risk of HF. Compared with non-drinkers, the RRs (95% CI) across levels of alcohol consumption were 0.90 (0.84–0.96) for 3 drinks/week, 0.83 (0.73–0.95) for 7 drinks/week, 0.84 (0.72–0.98) for 10 drinks/week, 0.90 (0.73–1.10) for 14 drinks/week, and 1.07 (0.77–1.48) for 21 drinks/week. Alcohol consumption in moderation is associated with a reduced risk of HF.”
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 154: Effects of changes in alcohol consumption on risk of dementia among elderly women — 12 January 2015
A number of prospective studies have shown that moderate drinkers are at lower risk of developing dementia or cognitive impairment than abstainers or heavy drinkers; possible mechanisms of a putative beneficial effect could relate to a reduction in the risk of cerebral atherosclerosis, a direct effect on cognition through the release of acetylcholine in the hippocampus, the antioxidant effects of alcohol and polyphenols, or from the down-regulation of inducible nitric synthase and up-regulation of endothelial nitric oxide synthase.
The present study is based on 1,309 women who were aged 65 years or greater at the beginning of a 20-year follow up, during which they had at least two assessments of cognitive function. At baseline, 42.1% of the women reported that they were “light” drinkers (>0 – < 3 drinks/week, 13.8% reported “moderate” consumption (3-7 drinks/week), and 3.6% reported “heavy” consumption (> 7 drinks/week). By the 20th year of follow up, 17.5% of the previously normal women had developed dementia (by several standard tests, a previous diagnosis of dementia, or nursing home residence), and 22.7% had developed mild cognitive impairment (MCI). Thus, a total of 40.2% of the women had developed some degree of cognitive impairment.
In this paper, there was no suggestion that the small percentage of women (5%) who increased their intake changed their risk of cognitive impairment (fully adjusted OR=1.04, 95% CI 0.56, 1.95), when compared with women who did not change their intake or decreased it only slightly. However, for women who decreased their intake by > 0.5 drinks/week, the authors suggest that there was an increase in risk of cognitive impairment, with unadjusted results showing an OR of 1.34, 95% CI: 1.05-1.70. However, with full adjustment for confounders, the effect was attenuated: OR = 1.26, 95% CI 0.98, 1.61; p = 0.07.
Forum members noted that the reasons that some women changed their drinking habits could not be ascertained (as is usually the case in observational studies). Alzheimer’s dementia has a long prodromal period and latent pathology could precede/contribute to a decrease in drinking. They were also concerned about the lack of cognitive characterization of the cohort at baseline. Thus, Forum members had some difficulty in knowing how to interpret the finding of a lack of association of baseline drinking with risk of cognitive impairment 20 years later given that we are not told whether the groups defined on baseline drinking differed from each other in age or other health risk factors. For those who changed their intake, decreasing drinking by > 0.5 glasses/week may be very different for someone drinking > 7 drinks/week than in someone drinking < 1 drink/week. It would have been better if the authors somehow took baseline drinking into account when assessing effects of change in drinking.
There was also the concern that any observational study that relates the effects of changes in alcohol intake on the risk of a disease without somehow taking earlier drinking into account may give paradoxical results. (An example is the relation of obesity to cardiovascular disease; overall, there is an increase in risk for obese individuals but when changes in intake among older people are evaluated, the result is often no effect or even a protective effect: the “obesity paradox.”) The same has been shown for the relation of usual alcohol intake and changes in intake to other diseases.
Thus, while the analyses were done appropriately, Forum members had concerns about whether the findings presented in this paper justify the wisdom of the authors in stating in their conclusion that “Women in their ninth and tenth decade of life who decrease alcohol use may be at risk of cognitive impairment.” As one reviewer stated: “Knowing from other studies that light to moderate alcohol consumption is good for the heart and the head, I would not advise elderly people to stop drinking. However, the conclusions of the authors that this paper shows that decreasing alcohol consumption increases the risk of cognitive impairment in elderly women may be true, but are not justified because the design, analysis, and results of the study do not permit such a statement.”
Reference: Hoang TD, Byers AL, Barnes DE, Yaffe K. Alcohol Consumption Patterns and Cognitive Impairment in Older Women. Am J Geriatr Psychiatry 2014; 22:1663-1667.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 153: Moderate alcohol intake may lower the risk of developing diabetes among obese subjects — 11 December 2014
This case-control study compared the risk of having a high level of hemoglobin A1c, a measure of hyperglycemia, and of the waist/height ratio, a measure of obesity, according to reported alcohol consumption. Overall, subjects reporting an average alcohol intake between 22 and 44 g/day (the equivalent of between about 2 and 4 typical drinks) had lower levels of hemoglobin A1c and lower weight/height values. The author concludes: “The associations between obesity and hyperglycemia were weaker in light-to-moderate drinkers than in nondrinkers. Thus, light-to-moderate drinking may reduce the impact of obesity on the risk for diabetes.”
While Forum reviewers had some concerns about the first analytic approach given in the paper, they agreed that the second approach, in which specific levels of A1c were reported according to alcohol intake and measures of obesity, had merit. These latter data clearly indicate that hyperglycemia is affected both by obesity (which increases the risk) and alcohol intake (which decreases the risk); hyperglycemia is the leading factor associated with the development of diabetes mellitus.
A therapeutic implication of this study may be that obese subjects who are moderate drinkers should not be advised to stop their alcohol consumption. The results, along with a large amount of other research currently available, also suggest that obese subjects who do not drink and have no contraindications to alcohol consumption should be informed that consuming moderate amounts of alcohol may be associated with a reduction in their risk of developing diabetes.
Reference: Wakabayashi U. Light-to-Moderate Alcohol Drinking Reduces the Impact of Obesity on the Risk of Diabetes Mellitus. J Stud Alcohol Drugs 2014;75:1032–1038.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 152: Specific genetic factors modify the reduction in heart disease risk from alcohol consumption — 27 November 2014
It has long been known that genetic and other environmental factors modify the association between alcohol consumption and a variety of diseases, especially coronary heart disease (CHD). Foremost among these modifying factors are genes that affect alcohol metabolism, age (effects seen only in older individuals), and drinking patterns (regular moderate versus binge drinking). Also, certain cholesteryl ester transfer protein (CETP TaqIB) polymorphisms, that relate to HDL-cholesterol activity, may interact with alcohol consumption for their effects on the risk of CHD. In the present study, the investigators have carried out a population-based case-control study among subjects in southwest Sweden to determine if there was an interaction between CETP genotypes and alcohol consumption for its effects on the risk of CHD. The authors conclude that a significant reduction in the risk of CHD from moderate drinking was seen only among the 18.6% of their subjects who had a particular CETP polymorphism.
Forum members considered this to be an interesting paper, but had some questions about the selection of cases, as they included not only new cases of CHD but subjects “who had an exacerbation of previously diagnosed coronary heart disease;” this makes it somewhat difficult to compare their results with other papers. Further, despite a large number of potential “control” subjects from their base population, the controls chosen were considerably younger than the cases and had different medical histories. While they adjusted for some of these factors in their analysis, residual confounding remains possible.
The major concern of Forum members was the broad conclusion of the authors (that only a small proportion of the population will show any cardio-protective effects of moderate drinking) based on such a small number of subjects. For example, among their “intermediate” category of drinkers with the supposedly “protective” CETP polymorphism, there were only 13 cases of CHD. Further, a number of previous large studies have had quite conflicting results regarding the effects of CETP polymorphisms on the alcohol-CHD association. While this paper adds information on one (of many) factors that affect the association between alcohol consumption and CHD, larger studies in different populations will be needed to determine the overall importance of this particular genetic polymorphism.
Reference: Mehlig K, Strandhagen E, Svensson P-A, Rosengren A, Torén K, Thelle DS, Lissner L. CETP TaqIB genotype modifies the association between alcohol and coronary heart disease: The INTERGENE case-control study. Alcohol 2014;48:695e700.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 151: “Fetal alcohol syndromes” result from multiple maternal factors during pregnancy — 20 November 2014
Excessive maternal alcohol consumption during pregnancy (especially among women with alcohol dependency) is known to markedly increase the risk of the fetus showing a group of developmental disorders defined as fetal alcohol spectrum syndrome (FASD), with the most serious form being fetal alcohol syndrome (FAS). The present paper attempts to identify maternal risk factors for FASD and FAS, but the authors report that there were not enough data to carry out a formal meta-analysis. They do, however, describe important maternal risk factors that have been reported in the literature to relate to these syndromes. The more frequent maternal conditions related to the risk of FASD or FAS include older age of mother, lower educational level, family relatives who abuse alcohol, little prenatal care, and a more severe pattern of alcohol consumption in general and particularly during pregnancy. They emphasize that “FAS is a multifactorial condition, and it is potentiated by complex relationships among several factors, social and biological.”
Forum reviewers considered this to be a well-done analysis presenting important and balanced information on these syndromes. Forum members agreed that many genetic and environmental factors, in addition to heavy alcohol consumption, may contribute to the development of these syndromes (e.g., certain genetic polymorphisms, inadequate pre-natal care, poverty, low education, familial alcoholism, use of illicit drugs, etc.).
Given the permanent nature of many of the defects found in FASD and FAS, and limited therapeutic options, it is important that the focus should be on the prevention of these syndromes. If they are to be prevented, it will be necessary to intervene among high-risk women, either prior to or early during pregnancy. Better knowledge of all the factors involved will help facilitate interventions that may help prevent these serious conditions.
Reference: Esper LH, Furtado EF. Identifying maternal risk factors associated with Fetal Alcohol Spectrum Disorders: a systematic review. Eur Child Adolesc Psychiatry (2014) 23:877–889; DOI 10.1007/s00787-014-0603-2.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 150: A new meta-analysis on the relation of alcohol consumption to the risk of ischemic heart disease — 6 November 2014
This meta-analysis is from authors who in the past have tended to argue that the demonstrated inverse association between moderate alcohol consumption and ischemic heart disease (IHD) shown in most studies is due to confounding by other lifestyle factors. However, in this paper, they come to the conclusion (in their words): “Results from our quantitative meta-analysis showed that drinkers with average intake of < 30 g/day and no episodic heavy drinking had the lowest IHD risk (relative risk = 0.64, 95% confidence interval 0.53 to 0.71). Drinkers with episodic heavy drinking occasions had a risk similar to lifetime abstainers (relative risk = 1.12, 95% confidence interval 0.91 to 1.37).”
The conclusions of the authors thus not only support a “J-shaped” curve for alcohol consumption and IHD but provide additional support suggesting that the effect may be causal, i.e., related to the alcohol consumption and not to other associated lifestyle factors. They state: “For drinkers having one to two drinks per drinking day without episodic heavy drinking, there is substantial and consistent evidence from epidemiological and short-term experimental studies for a beneficial association with IHD risk when compared to lifetime abstainers. The alcohol-IHD relationship fulfills all criteria for a causal association proposed by Hill.”
It is clear from epidemiologic studies that moderate drinkers may exhibit moderation in other lifestyle factors (such as not smoking, eating a healthy diet, etc.). Indeed, there is aggregation of healthy lifestyle factors that must be considered when judging how a single factor (such as moderate drinking) relates to disease outcomes. This meta-analysis suggests that other lifestyle factors do not explain the lower risk of IHD found to occur among moderate drinkers. In fact, increasingly, moderate drinking is found to be an independent (and rather important) lifestyle factor that lowers the risk of cardiovascular disease, regardless of other factors. Such protection is not seen when drinking is more than moderate, defined in this paper as an average of 30 grams or more of alcohol per day, the equivalent of about 2 ½ to 3 typical drinks.
Reference: Roerecke M, Rehm J. Alcohol consumption, drinking patterns, and ischemic heart disease: a narrative review of meta-analyses and a systematic review and meta-analysis of the impact of heavy drinking occasions on risk for moderate drinkers. BMC Medicine 2014;12:182.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 149: The association of alcohol consumption with the risk of death from colorectal cancer — 28 October 2014
Data from prospective cohort studies on the association between alcohol consumption and the occurrence of colorectal cancer (CRC) are conflicting, with some suggesting an increase in risk while others failing to show such an effect. There are little data on the effects of alcohol consumption on the risk of mortality from CRC. The present study is based on a meta-analysis of data from nine cohort studies (with a total of more than two million subjects) to judge how the level of alcohol intake relates to CRC mortality. A total of almost 4,000 deaths from CRC were recorded. The conclusions of the authors are that the consumption of ≥ 50 grams of alcohol (about 4 typical drinks or more) per day increases the risk of death from CRC modestly [RR 1.21 (95% CI 1.01, 1.46)], but “light” drinking (≤ 12.5 g/day) or “moderate” drinking (12.6-49.9 g/day) do not increase the risk of CRC death. In fact, they state that their data support a “J-shaped” relation between alcohol intake and CRC mortality (i.e., a slight decrease in mortality associated with light drinking but an increased risk with heavier drinking).
Forum members considered this to be a well-done analysis. They noted the inability of the authors to evaluate differences in effect according to type of beverage consumed, the pattern of drinking, or the underlying folate levels of subject, all of which probably modify such a relation. The results are in line with earlier reports on alcohol and breast cancer, where alcohol appears to increase the incidence of the disease but does not increase mortality. For most diseases, including colorectal cancer, there may a J-shaped effect on mortality: a reduction in risk for light-to-moderate drinking but an increase with heavier drinking.
Overall, the present meta-analysis supports a finding of increased risk of death from colorectal cancer from heavy drinking. However, it shows rather convincingly that light to moderate amounts of alcohol do not increase the risk of death from this disease, probably because of the protective effects of moderate drinking on cardiovascular disease, a more common cause of mortality.
Reference: Cai S, Li Y, Ding Y, Chen K, Jin M. Alcohol drinking and the risk of colorectal cancer death: a meta-analysis. European Journal of Cancer Prevention 2014;23:532–539.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 148: Alcohol and liver cancer — 24 September 2014
Hepatic cirrhosis frequently precedes the development of liver cancer, and excessive alcohol consumption is known to be one cause of cirrhosis. The investigators in the present study carried out a meta-analysis to evaluate the association of alcohol consumption with liver cancer. They used data from 19 prospectively studied cohorts with a large total number of cases: 4,445 incident cases and 5,550 deaths from liver cancer.
The analysis from this large study indicates that liver cancer is related to heavier alcohol intake, but not to light-to-moderate drinking (with the latter defined in this study as < 3 typical drinks per day). The authors conclude: “This systematic review suggests a moderate detrimental role of consumption of 3 or more alcoholic drinks per day on liver cancer, and a lack of association with moderate drinking.”
Forum reviewers considered this to be a well-done analysis with appropriate statistical methodology. While the authors were unable to test the potential effects of pattern of drinking (regular moderate versus binge drinking), the type of beverage (wine or other beverages), or potential effects of obesity (with the latter being a key factor associated with the most common type of liver disease in the US, non-alcoholic fatty liver disease), the results of this study support most other research indicating that more than moderate drinking increases the risk of cirrhosis and liver cancer. However, the findings of no effect from what the authors considered “moderate” drinking (< 3 drinks/day, which exceeds the guidelines for most countries), also fits with another recent meta-analysis showing no increase in risk of liver cancer to be associated with light drinking.
There are many adverse health effects of heavy alcohol consumption. Liver cirrhosis, which frequently precedes the development of liver cancer, is one such potential outcome. On the other hand, this study suggests that moderate alcohol intake does not increase the risk of liver cancer.
Reference: F. Turati, C. Galeone, M. Rota, C. Pelucchi, E. Negri, V. Bagnardi, G. Corrao, P. Boffetta, C. La Vecchia. Alcohol and liver cancer: a systematic review and meta-analysis of prospective studies. Annals of Oncology 2014; advance publication; doi:10.1093/annonc/mdu020
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 147: Association of alcohol intake with different types of breast cancer — 11 September 2014
The present study was based on a large number of women participating in a clinical trial (enhanced screening for certain cancers versus routine care) focusing on prostate, lung, colorectal, and ovarian cancer. During a follow-up period averaging about 9 years, a total of 1,905 women were diagnosed with invasive breast cancer. The analyses showed that an increase in cancer risk was associated with alcohol intake for estrogen and progestin positive (ER+/PR+) tumors, but not for other histologic types of breast cancer. The increased risk was predominantly seen among PR+ cancers, as there was no evidence of an increase in risk from alcohol for women with ER+/PR- tumors. An association with the highest category of alcohol intake was noted for ductal (the most prominent type), lobular, and mixed ductal/lobular tumors, but a clear dose-response curve was not present. The authors conclude that alcohol consumption is not associated with all breast cancer subtypes, and that future research should include precise definition of subtypes of cancer.
Forum reviewers considered this to be a well-done analysis. There were some questions about the characteristics of the participants in the study that could affect generalizability of the results. For example, the cohort of women in this study were more highly educated, more likely to have a positive family history of breast cancer, to be smokers, and perhaps more obese that the general population. Of more concern, however, was the lack of ability to evaluate a number of other potential risk factors for breast cancer: folate levels and other dietary factors, the pattern of drinking (regular versus binge), potential changes in drinking after the baseline measurement, type of beverage, or the HER2 status of tumors. The finding in the paper of an increase in breast cancer risk, in comparison with non-drinkers, even for women reporting less than ½ drink per week (RR 1.15, CI 0.97, 1.39) and 0.5 – < 1 drink per week (RR 1.25, CI 1.03, 1.53), suggests that residual confounding must also be considered; it is unlikely that such small amounts of alcohol would have a physiological effect.
Overall, the present study shows a significant increase in the risk of breast cancer among women in a cancer prevention trial who, at baseline, indicated that they were consuming even less than 1 drink/week. The increase was exclusively in ER+/PR+ tumors, but not in ER+/PR- or ER-/PR- tumors.
In future research on this association, information on folate levels and drinking pattern, and especially on type of beverage consumed and on evidence of under-reporting of alcohol intake, will be important in better defining how alcohol consumption relates to the risk of breast cancer. While the results of this study are important in studying the etiology of breast cancer (as alcohol appears to relate only to hormone receptor positive tumors), the findings may not necessarily help individual women know how their alcohol consumption by itself may relate to their overall risk of the disease.
Reference: Falk RT, Maas P, Schairer C, Chatterjee N, Mabie JE, Cunningham C, Buys SS, Isaacs C, Ziegler RG. Alcohol and Risk of Breast Cancer in Postmenopausal Women: An Analysis of Etiological Heterogeneity by Multiple Tumor Characteristics. Am J Epidemiol 2014; advance access; DOI: 10.1093/aje/kwu189.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 146: Alcohol and the risk of abdominal aortic aneurysm — 4 September 2014
The large majority of prospective epidemiologic studies on the effects of alcohol consumption and the risk of coronary heart disease and stroke have shown a significant reduction in risk for moderate drinkers. There have been few studies relating alcohol intake to the development of abdominal aortic aneurysm (AAA), and results have been inconsistent. The present study is based on two very large population-based cohorts in Sweden that were followed prospectively for the clinical development of AAA (identified by radiography, surgical repair, or death resulting from rupture). There were more than 1,200 cases identified during a 14-year follow-up period. The results of this study suggest that moderate drinking is associated with a lower risk of AAA, with the beneficial effects primarily among consumers of beer or wine.
Forum reviewers were unanimous in considering this to be a well-done analysis, with unbiased estimates of effect of alcohol on the risk of aneurysm. The reduced risk of AAA among moderate drinkers was similar to that seen for common manifestations of atherosclerosis, especially coronary heart disease and ischemic stroke. Reviewers were uncertain why only consumers of wine and beer showed a beneficial effect, but not consumers of spirits: this could be explained by the polyphenols present in wine and beer that have been shown to be anti-inflammatory, anti-oxidant, and anti-platelet aggregation (all mechanisms that may relate to the development of AAA). However, residual confounding could also play a role.
It was noted that the percentage of the population with hypertension, probably the most important risk factor for AAA, was much lower than is common in most industrialized countries, but the degree to which this affected the results cannot be known. While alcohol is known to increase blood pressure, some large studies suggest that an increase occurs only with more than light-to-moderate drinking. Further, there were few very heavy drinkers (the highest category of alcohol was an average consumption of ≥1 drink/day among women and ≥2 drinks/day among men), so this study could not assess whether or not large amounts of alcohol might increase risk of AAA.
There have been a very limited number of studies on alcohol intake and aortic aneurysm. While this study suggests a slight decrease in occurrence of AAA with moderate wine and beer intake, it will be important for other large studies to evaluate this association. Additional studies on polyphenol intake and occurrence of AAA will also be useful.
Reference: Stackelberg O, Björck M, Larsson SC, Orsini N, Wolk A. Alcohol Consumption, Specific Alcoholic Beverages, and Abdominal Aortic Aneurysm. Circulation 2014;130:646-652.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 145: Alcohol consumption and brain structure on MRI scans — 25 August 2014
While numerous prospective epidemiologic studies have provided evidence that light-to-moderate amounts of alcohol reduce the risk of dementia and heavy drinking increases the risk, there are few studies on the effects of alcohol on brain structure assessed by magnetic resonance imaging (MRI). The present study is a cross-sectional evaluation between reported alcohol intake and MRI-assessed brain structure among 589 multi-ethnic community residents of New York. Total brain volume (TBV), white matter hyperintensity volume (WMHV), and presence of infarcts were derived from MRI scans when subjects were, on average, 80 years of age..
A key finding of this analysis is that, in comparison with non-drinkers, light-to-moderate alcohol intake (up to an average of 1 drink/day for women or 2 drinks/day for men, which was reported in 31% of their subjects) was associated with larger TBV (i.e., less brain atrophy). The effect was primarily among consumers of wine rather than of beer or liquor. Significant associations were not found for alcohol or for specific beverages for other measures of brain structure (WMHV or presence of infarcts).
Forum reviewers considered this to be an appropriate analysis that was able to consider many of the potential confounders of such an association. On the other hand, it was not a large study and was based on a cross-sectional analysis; thus it cannot be used to judge causation (e.g., it is possible that people with larger brains to begin with were more likely to consume wine or total alcohol, rather than their alcohol intake increasing their brain size).
Data from many previous studies have shown that moderate alcohol intake lowers the risk of developing clinical signs of cognitive decline and of dementia. Such a finding has led Forum members to be of the opinion that instructing the elderly to refrain from light-to-moderate amounts of alcohol may not be wise. Although prospective studies may show that the decrease in the risk ratio for dementia (comparing drinking with abstainers) tends to be less among the elderly than among middle-aged subjects, the absolute risk of dementia increases markedly with age. Thus, any intervention that lowers the risk of cognitive impairment will have a much greater impact in older people as compared with younger people.
Given the inconsistences in previous reports on the effects of alcohol on brain structure, we must conclude that while this study suggests that there might be a beneficial association between alcohol (especially wine intake) and brain size, such a relation is not definitive. An inverse relation between moderate drinking and clinical evidence of dementia, however, has received support from a large number of prospective epidemiologic studies; it may be a better association for us to use when advising the elderly regarding alcohol consumption.
Overall, scientific data indicate that, for elderly subjects without contraindications to alcohol, small amounts of wine or other alcoholic beverage consumed regularly may reduce the risk of dementia and other diseases of ageing. As stated by Michel de Montaigne many centuries ago: “ . . . drinking is the almost last pleasure that the years steal from us.”
Reference: Gu Y, Scarmeas N, Eaton Short E, Luchsinger JA, DeCarli C, Stern Y, Manly JJ, Schupf N, Mayeux R, Brickman AM. Alcohol intake and brain structure in a multiethnic elderly cohort. Clinical Nutrition 2014;33:662e667.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 144: Alcohol consumption and risk of endometrial cancer — 18 August 2014
Most epidemiologic studies have shown that moderate alcohol consumption does not increase the risk of uterine cancer, and some have suggested an inverse or J-shaped relation. In a new analysis from the Nurses’ Health Study, with 68,067 female participants aged 34–59 years in 1980, investigators have related repeatedly assessed long-term alcohol intake, and related the cumulative average intake over time to the risk of invasive uterine cancer. A total of 794 cases of invasive endometrial adenocarcinoma were identified over a 30 year follow-up period.
The authors report an inverse association among alcohol drinkers (multivariable RR=0.81; 95% CI: 0.68–0.96) compared with nondrinkers. Women with an intake of <5 g per day (an average of approximately one-half drink per day) had a 22% lower risk of endometrial cancer (multivariable RR=0.78; 95% CI: 0.66–0.94), with no further decrease evident from larger amounts of alcohol. In comparison with non-drinkers, the relative risk was similarly reduced for consumers of more than 30 grams of alcohol per day, but the number of subjects in this category was small, and a potential increase in risk from heavy drinking could not be adequately assessed in this study.
Forum members considered this to be a very well-done prospective study, with clear and biologically plausible results. By having repeated assessments of alcohol, an estimate of long-term average consumption was possible. The approximately 20% lower risk of uterine cancer among subjects with light alcohol intake remained statistically significant after multivariate adjustments for known potential confounders. Reviewers agreed with the authors that a potential mechanism for the association could be a reduction in insulin concentrations and improved insulin sensitivity that have been shown to occur with moderate alcohol consumption. Further, the frequently demonstrated inverse relation for alcohol with obesity may also play a mechanistic role. Overall, this study adds to accumulating scientific data showing that moderate drinking does not increase the risk of uterine cancer, and probably is associated with a reduction in risk
Reference: Je Y, DeVivo I, Giovannucci E. Long-term alcohol intake and risk of endometrial cancer in the Nurses’ Health Study, 1980–2010. British Journal of Cancer 2014;111:186–194; doi: 10.1038/bjc.2014.257.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 143: A Mendelian randomization assessment of alcohol and cardiovascular disease — 20 July 2014
Using a very large dataset from subjects of European descent, the authors have carried out a Mendelian randomization analysis to estimate the effects of alcohol consumption on cardiovascular disease (CVD), using as the instrumental variable an uncommon allele affecting alcohol metabolism, the ADH1B rs1229984 variant. People with this variant are unusually sensitive to alcohol (developing flushing and other uncomfortable symptoms from alcohol) and it has been well demonstrated that they are less likely than people without this variant to consume alcohol, and are unlikely to be heavy drinkers. The authors conclude that since the 7% of their subjects with the uncommon allele had less cardiovascular disease, this indicates that alcohol consumption is unrelated to CVD.
Forum members agree that the analyses were done correctly, but strongly disagree with the premise of the study and the conclusions of the authors, and consider the genetic factor chosen as inappropriate to use as the instrumental variable in Mendelian randomization. The gene studied explains only a fraction of alcohol consumption in the population (not stated in the paper) and it may have effects on CVD beyond those explained by alcohol consumption. Thus, this ADH1b allele violates the assumptions required for a variable for Mendelian randomization and would be inappropriate for judging the effects of alcohol on CVD. Further, in the present study, the authors report little relation of their estimate of alcohol consumption with HDL-cholesterol, while essentially all observational studies, clinical trials, and experimental studies have shown that alcohol is an important determinant of HDL. This further suggests that the use of the ADH1B allele provides an inadequate estimate of alcohol consumption.
Even without the weakness of the allele chosen to reflect alcohol effects, conclusions derived from Mendelian randomization in general are heavily dependent on the assumption that the instrumental chosen is appropriate, of which you can rarely be confident. Forum reviewers consider this method to be a very blunt instrument and subject to considerable bias for variables that are weakly correlated with exposure and not true instruments.
Some reviewers were concerned by the conclusion of the authors that this Mendelian randomization paper shows that all persons should drink less; this does not necessarily mean for people to completely avoid drinking. The protection of moderate drinking against CVD that is generally observed shows a non-linear gradient: it is better manifested at a low alcohol consumption, while it is less strong as the consumption levels rise above optimum and finally disappears and is transformed into harm with heavy alcohol consumption. This would be in agreement with the conclusions of most prospective studies and meta-analyses that drinking alcohol at low doses offers the best protection against CVD, as there is a J-shaped curve.
Reference: Holmes MV, Dale CE, Zuccolo L, et al (a total of 155 authors). Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. BMJ 2014;349:g4164 doi: 10.1136/bmj.g4164.
For the full critique of this study by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 142: A large study of alcohol consumption and mortality — 14 July 2014
The large European Prospective Investigation into Cancer and Nutrition Study (EPIC) has released a new analysis of the relation of alcohol consumption to mortality. The study concluded that alcohol use was positively associated with overall mortality, alcohol-related cancers, and violent death and injuries, but marginally to cardiovascular disease, and that absolute risks of death observed in EPIC suggest that alcohol is an important determinant of total mortality.
There is no question that heavy alcohol consumption, especially when associated with smoking, increases the risk of a number of upper aero-digestive cancers that are commonly referred to as “alcohol-related cancers.” In the present study, the authors have also included in this group a number of other cancers that may be related less directly to the effects of alcohol; these include colorectal cancer and female breast cancer which, because they are so much more common, make up the large majority of cancers “related to alcohol.” Forum members consider the EPIC study to be an important source of data on cancer, but had a number of questions about the analysis and especially about the conclusions of the authors.
Major weaknesses of the study are that an assessment of alcohol intake was obtained only at a baseline visit, with no further assessments during a follow-up period averaging 12 years, and especially, no information was available on the pattern of drinking of subjects (e.g., regular moderate versus binge drinking). Further, Forum members noted that there was no discussion of the effects of under-reporting of alcohol, which has been shown to markedly affect health effects of alcohol intake in epidemiologic studies. In fact, recent large studies show that most of the cases of cancer that appear to relate to “light-to-moderate drinking” actually relate to underreporting of consumption by subjects who are found, from other collected medical data, to be heavy users or abusers of alcohol.
The authors focus on “extreme drinkers,” which consist of women who consume (≥30 g/day) or men who consume ≥60 g/day. They do not point out that only 2.4% of the women in this study consumed at this level, and little attention is given to the fact that almost all of the women were non-drinkers or light-moderate drinkers. From the data presented in the paper, there is a clear U-shaped curve among women: the highest risks for total mortality were in the abstainers (a 26% increase over the referent group of light drinkers) and the very small number of women in the highest drinking category (a 27% increase).
For men, 8.2% were in the highest drinking category, reporting an average consumption of ≥ 60 g/d (5 – 6 typical drinks). For men, there was generally a U-shaped curve, with lower death rates for light to moderate drinkers. However, the heaviest drinkers had the highest risk of death for overall mortality and for deaths from cancers and other causes of death. For both men and women, at every level of drinking, smokers had an increased risk of death in comparison with non-smokers.
Some reviewers were also concerned about the unusual categorization of alcohol intake used in the study. Referring to subjects reporting 0.1 – 4.9 g/day as “moderate drinkers” is a strange designation for an alcohol intake that in most other studies would be named as light or very modest, and may lead to confusion in interpreting results. (Most studies would define 5 – 14.9 g/day as light to moderate drinkers, and this group is not given a name in this study).
Overall, this study tends to show a U-shaped relation between alcohol consumption and mortality. The data presented focus primarily on the highest categories of drinking, levels that are well known to relate to many diseases and mortality. For truly light-to-moderate consumption, however, there is overwhelming epidemiologic data that such drinking relates to lower mortality risks, and the present study does not contradict such an association.
Reference: Ferrari P, Licaj I, Muller DC, et al (36 other authors). Lifetime alcohol use and overall and cause-specific mortality in the European Prospective Investigation into Cancer and nutrition (EPIC) study. Pre-publication; BMJ Open 2014;4:e005245. doi:10.1136/bmjopen-2014-005245
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 141: A world-wide study of alcohol consumption and the risk of myocardial infarction — 3 July 2014
The authors report on data collected in the INTERHEART Study, a large international collaborative project of individuals with a first myocardial infarction (MI) and age- and sex-matched controls from 52 countries in Asia, Europe, the Middle East, Africa, Australia, North and South America. Included were nations with very divergent lifestyles, religions, degrees of development, and drinking habits. The authors attempted to provide a “world-wide” overview of the relation of alcohol consumption to the risk of myocardial infarction (MI). However, they were forced to use a case-control design, a type of study with many opportunities for bias and one that prevents determination of a causal relation. Further, the lack of detailed data on the amount of alcohol consumed by individuals weakens their results.
While the authors state that their study shows that low levels of alcohol use are associated with a moderate reduction in the risk of MI, they point out differences in results in different countries. Forum members considered that these large differences severely limit their ability to use such a dataset to provide overall conclusions on alcohol and MI. For example, only 1% of the non-drinkers in this study came from W. Europe and 1% from North America, while more than 70% of the non-drinkers came from the Middle East or Asia. With such diversity (e.g., almost all the abstainers were from one area), it is not possible to adequately “adjust” for such regional differences in analysis.
The authors also studied how alcohol consumption shortly prior to (in the 24 hours before) the occurrence of a MI relate to the short-term risk of MI. While their results show an increased risk for heavy drinking immediately prior to an MI (a result that differs from that of some previous studies), they admit analytic problems, stating: “Thus there remains uncertainty over the risk of MI in the period immediately following alcohol intake.”
Previous large prospective cohort studies (a type of epidemiologic study that decreases the risk of recall bias regarding alcohol intake and certain types of confounding) have clearly shown an inverse relation between moderate alcohol consumption and MI. Most of the previous studies have provided much more detailed data on alcohol exposure than did the present study. The authors realized many of these problems, and warn against using their results to make overall conclusions about the association between alcohol and MI from their paper. They state: “The associations observed between alcohol use and MI may be accounted for by unmeasured confounders such as genetic differences between populations, variation in alcohol type or preparation, and heterogeneity of social context. The present analysis should therefore prompt further research to clarify the nature of the association between alcohol use and MI.” Unfortunately, the conclusions presented in the abstract and in the do not mention such problems.
Some Forum members worried that many readers of the paper will be left with a very misleading impression of the relation of alcohol consumption to myocardial infarction, and will not be aware that the conclusions trumpeted in the abstract are compromised by weak data. Overall, members considered that the present paper adds little to our knowledge about the risks and benefits of alcohol in relation to cardiovascular disease.
Reference: Leong DP, Smyth A. Teo KK, McKee M, Rangarajan S, Pais P, Liu L, Yusuf S, on behalf of the INTERHEART investigators. Patterns of Alcohol Consumption and Myocardial Infarction Risk: Observations from 52 Countries in the INTERHEART Case-Control Study. Circulation 2014 (pre-publication) DOI: 10.1161/CIRCULATIONAHA.113.007627.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 140: A meta-analysis shows that light alcohol consumption is associated with a reduced risk of stroke, while heavier drinking may increase risk — 5 June 2014
Most epidemiologic studies have shown a reduction in the risk of ischemic stroke (and total stroke, as ischemic stroke is by far the most common type in western countries) to be associated with light to moderate alcohol consumption. The present study, a meta-analysis, was based on 27 prospective studies; the authors categorized a reported intake of <15 g/day as light consumption, and 15-30 g/day as moderate consumption. The authors point out differences (greater smoking, larger amounts of alcohol) between Chinese subjects and those from other countries, which may explain some of the differences shown between alcohol’s effects in the different countries. They also point out that they had no data on the pattern of drinking (regular, moderate intake versus binge-drinking) or on the type of alcoholic beverage consumed.
The key results of the study are a significant 15% reduction in total stroke for low alcohol intake, no effect for moderate, and a 20% increased risk for heavy alcohol consumption (RR 1.20, 95% CI 1.01, 1.43). Analyses were also done according to type of stroke: for ischemic stroke and stroke mortality there were decreases for low alcohol intake, but no significant effects of either moderate or heavy intake. For hemorrhagic stroke, the RR for subjects reporting heavy alcohol intake was higher than that of abstainers, but none of the differences between drinkers and non-drinkers was statistically significant.
This meta-analysis supports previous findings of a decrease in the risk of most strokes with light drinking and possibly an increase in the risk for heavy drinking. Forum members generally agreed with the conclusions of the authors: “Low alcohol intake is associated with a reduced risk of stroke morbidity and mortality, whereas heavy alcohol intake is associated with an increased risk of total stroke. The association between alcohol intake and stroke morbidity and mortality is J-shaped. An alcohol intake of 0-20 grams/day is associated with decreased rates of stroke morbidity and mortality.”
Reference: Zhang C, Qin Y-Y,Chen Q, Jiang H, Chen X-Z, Xu C-L, Mao P-J, He J, Zhou Y-H. Alcohol intake and risk of stroke: A dose–response meta-analysis of prospective studies. Int J Cardiol 2014; pre-publication; http://dx.doi.org/10.1016/j.ijcard.2014.04.225.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 139: Does adjustment for stress levels explain the protective effect of moderate drinking on the risk of mortality? — 18 May 2014
An inverse association between moderate alcohol consumption and total mortality has been reported in most prospective epidemiologic studies, even after adjustments for all known potential confounders. The present analysis was carried out specifically to focus on the effects of psychosocial stressors on the association, using a large population-based German cohort from the WHO MONICA study. No alcohol intake was reported by 15.3% of males and 41.8% of females; “moderate drinking” was defined as an average intake of 0.1-39.9 g/day for men (making up 51.1% of the cohort) and 0.1 – 19.9 g/day for women (38.8% of the cohort). Although data are not presented, there were apparently few women in the higher drinking categories.
The authors related the effects of including, or not including, in their equations a large number of psychosocial stressors, including educational level, occupational status, several indices of social support, job strain symptoms, depressive symptoms, somatic symptoms, and self-perceived health status, in the estimation of the effects of alcohol consumption on risk of total mortality over an average follow-up period of 12 years. In their analyses, there was little effect on risk estimates for mortality when these factors were added to the multi-variable analysis. The authors conclude: “The observed protective effect of moderate drinking could not be attributed to misclassification or confounding by psychosocial stressors.”
The authors have demonstrated among men a “U-shaped” curve, with the risk for moderate drinkers being 25-30% lower than that of both non-drinkers and heavier drinkers. For women, there was a lower estimated mortality risk ratio for all drinkers than for non-drinkers, although the confidence intervals included 1.0 in all categories (perhaps, as the authors state, there were few women in their higher categories of alcohol intake).
Forum reviewers thought that this was a well-done analysis of a large population-based population. It did not support the hypothesis that social support, job strain, depressive symptoms, and other such psychosocial factors have a strong influence on the demonstrated inverse relation between moderate alcohol consumption and total mortality. Thus, this study provides additional evidence that the observed reduction in total mortality seen among moderate drinkers is not due to confounding by other lifestyle factors, including psychosocial stressors.
Reference: Ruf E, Baumert J, Meisinger C, Döring A, Ladwig K-H, and for the MONICA/KORA Investigators. Are psychosocial stressors associated with the relationship of alcohol consumption and all-cause mortality? BMC Public Health 2014, 14:312. http://www.biomedcentral.com/1471-2458/14/312.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 138: Underreporting of alcohol intake affects the relation of alcohol to the risk of cancer — 23 April 2014
Epidemiologists are often faced with reported adverse health effects of alcohol among subjects reporting very low levels of consumption, levels that physiologically should not cause diseases such as cancer. It is often assumed that at least some of the subjects reporting low levels of intake may be underreporting their actual intake, but heretofore it has been difficult to judge this.
In the present study, the authors used each subject’s computer-based data on conditions and diseases (including laboratory and social factors), related to alcohol misuse, collected over many years to identify subjects reporting “light-to-moderate” alcohol intake who were likely, or unlikely, to be underreporting their intake at a baseline examination. Overall, 18.4% of subjects were suspected of being underreporters while 46.5% had adequate data that suggested that they were not underreporters. (The remaining 35.1% of subjects had inadequate data stored in the computer to be classified.)
Among their cohort of more than 100,000 subjects, 14,880 developed cancer during an average follow-up period of 18 years. There were 23,363 subjects who reported that they were light (up to 1 drink/day) or moderate (1 to 2 drinks/day) drinkers. In all comparisons, subjects suspected of being underreporters of their alcohol intake had a higher risk of cancer than those not categorized as being underreporters. For example, among subjects reporting 1 to 2 drinks/day, in comparison with non-drinkers, the risk ratio of any type of cancer among those considered to not be underreporters was 0.98 (95% CI 0.87-1.09); in other words, no effect on cancer risk from alcohol. For those categorized underreporters, however, the relative risk of any cancer was 1.33 (95% CI 1.21–1.45). Similar results were seen for alcohol-related cancers as for any cancer. Also, the risk of breast cancer among women was less than one-half as high among moderate drinkers who were unlikely to be underreporters of their alcohol intake as among those considered likely to be underreporting their drinking.
Adjusting for confounding in prospective studies is an ever-present challenge for epidemiologists. One factor that has often been considered probable, but difficult to adjust for, is the underreporting of actual alcohol intake by subjects. Being able to adjust for such unerreporting would greatly improve studies relating alcohol consumption to the risk of cancer (and other chronic diseases). For epidemiologic studies that have extensive longitudinal data on all medical conditions (such as the Kaiser-Permanente Study, the basis for these analyses), the approach described in this paper could be an extremely valuable way of seeking the true relation between light-to-moderate alcohol intake and cancer as well as with a variety of other health outcomes. Based on the present study, an increase in the risk of cancer among light-to-moderate drinkers may occur primarily among those who underreport their alcohol intake.
Reference: Klatsky AL, Udaltsova N, Li Y, Baer D, Tran HN, Friedman GD. Moderate alcohol intake and cancer: the role of underreporting. Cancer Causes Control 2014; on-line publication; DOI 10.1007/s10552-014-0372-8 2014.
Potential Conflict of Interest: The first author of this paper, Dr. Klatsky, is a member of the International Scientific Forum on Alcohol Research. While he has not contributed to this critique, readers may wish to take this fact into account when interpreting the conclusions of the review.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 137: Alcohol intake prior to and during pregnancy and birth outcomes — 28 March 2014
The present analysis was carried out among 1,264 women from Leeds, UK, whose alcohol intake was estimated prior to and during pregnancy. The outcomes were birth weight of the infant and whether or not it was small for gestational age (SGA). In comparison with most previous research on this topic, this study is notable for being of a relatively small size. Further, it had a high percentage of women who consumed alcohol both prior to and during the first trimester, had a very low participation rate of eligible women (only 30%), failed to present estimated effects by ethnicity, and had some questions related to residual confounding. It is unclear how the results of this study increase our knowledge of maternal alcohol consumption and birth outcomes.
Forum members do not believe that the consumption of alcohol should be recommended for pregnant women. A certain percentage of newborns will be small for gestational age, have certain deformities, and have later emotional and behavioral abnormalities. If a woman has consumed any alcohol during the pregnancy, she (and perhaps even her doctor) may blame the abnormality on alcohol consumption, whether or not it had anything to do with it. Hence, the majority of Forum members agree that women should not be encouraged to consume alcohol during pregnancy.
Further, scientific data are very consistent on the potential risks of serious adverse health outcomes of the infant from heavy maternal drinking, especially among women who are alcoholics. Heavy-drinking women who become pregnant should be strongly urged to stop their drinking.
On the other hand, sound data indicating harmful effects on the fetus of light or occasional drinking by a pregnant woman are difficult to come by. Because of the epidemiologic concerns of the present paper, described in our Forum critique, we do not believe that this study adds materially to our understanding of the topic. The serious anxiety occurring among some women who may have ingested some alcohol prior to learning that they were pregnant seems, based on numerous studies, to generally be unnecessary; the need to abort a fetus because of previous light drinking by the mother cannot be justified.
There is a serious problem in interpreting all studies of prenatal alcohol exposure and the outcomes of pregnancy because of potential confounding, especially by ethnicity, education, smoking, coexisting use of illegal drugs, etc. Further, alcohol use by pregnant women has become an especially emotional and even a moral issue, and the entangled confounders make rational analysis most difficult. This means that there is a difficult challenge for epidemiologists and statisticians, as well as for public health officials and the general public, about how to interpret results of individual research projects. The literature can support varying views, from no alcohol at all for those who might soon be expectant mothers to being able to drink moderately throughout pregnancy.
Also, it should be pointed out that the potential health benefits of moderate alcohol consumption relate primarily to middle-aged and older people, so there is no reason for pregnant women to consume alcohol for its “health effects.” Thus, it is very reasonable that the majority of women choose to avoid alcohol during pregnancy. Further, heavy drinking during pregnancy has known potentially serious consequences, and should never be encouraged. Finally, there is insufficient scientific evidence that an occasional drink of alcohol during pregnancy leads to harm to the fetus, and should not cause undue alarm in a pregnant woman who may have consumed some alcohol before she realized she was pregnant.
Reference: Nykjaer C, Alwan NA, Greenwood DC, Simpson NAB, Hay AWM, White KLM, Cade JE. Maternal alcohol intake prior to and during pregnancy and risk of adverse birth outcomes: evidence from a British cohort. J Epidemiol Community Health 2014, pre-publication. doi:10.1136/jech-2013-202934
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 136: Alcohol’s effects on cardiovascular risk among subjects with diabetes mellitus — 18 March 2014
A U- or J-shaped curve for the relation of alcohol consumption to cardiovascular disease (CVD) among diabetics has been shown in most prospective epidemiologic studies for many years, and CVD is the leading cause of death among diabetics. A variety of potential mechanisms of protection against CVD have been described, including beneficial effects of moderate drinking on lipids, inflammatory markers, and insulin resistance. The current paper assesses the effects of alcohol use among participants in the Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified-Release Controlled Evaluation (ADVANCE) trial. It was based on more than 11,000 subjects with diabetes from 20 countries, including those in Eastern Europe, Asia, and established market economies in Western Europe, North America, and the Pacific region. The outcomes over 5 years of follow up were CVD events (death from CVD, non-fatal myocardial infarction, non-fatal stroke), microvascular disease (renal disease, diabetic eye disease), and all-cause mortality.
Key results of the analyses showed that during follow up, more than 1,000 subjects (about 10%) had a major CVD, with similar percentages experiencing a microvascular complication or dying. The authors report that “Compared with abstainers, any alcohol use was associated with a 17% lower risk of cardiovascular events, a 15% lower risk of microvascular complications, and a 13% lower risk of all-cause mortality.” While there were few heavy drinkers (<4% of subjects), their data indicated that there was no significant lowering of risk of the outcomes among such subjects. Subjects who consumed wine had lower estimates of cardiovascular disease outcomes and mortality than consumers of other beverages.
Forum reviewers considered this to be a well-done analysis based on a large cohort of subjects with diabetes mellitus, with an adequate number of non-drinkers to serve as a referent group. The results strongly support previous studies that have shown a lower risk of cardiovascular events and total mortality among diabetic subjects who consume moderate alcohol. The study also showed that the risks of microvascular complications (diabetic kidney disease, diabetic eye disease) were lower among moderate drinkers.
The Forum considers this to be an important message (to physicians and the public), as the vascular ravages of diabetes are very serious, and diabetes is such a common disease that is increasing throughout the world. Diabetic patients without contraindications to alcohol sorely need to know of the potential cardiovascular protection of moderate alcohol consumption.
Reference: Blomster JI, Zoungas S, Chalmers J, Li Q, Chow CK, Woodward M, Mancia G, Poulter N, Williams B, Harrap S, Neal B, Patel A, Hillis GS. The relationship between alcohol consumption and vascular complications and mortality in individuals with type 2 diabetes mellitus. Diabetes Care 2014; pre-publication: DOI: 10.2337/dc13-2727
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here
===============================================================================
Critique 135: Binge drinking greatly increases mortality risk among moderate drinkers — 11 March 2014
This study was based on a sample of “late-middle-aged” (55-65 years old at baseline) community residents who were recruited from the western part of the United States to participate in a study of late-life alcohol consumption and drinking problems. The present analyses evaluated association between episodic heavy drinking and total mortality among 446 adults who were considered to be “moderate” drinkers. The authors report that the 74 moderate drinkers who engaged in episodic heavy drinking (“binge drinking”) had more than two times higher odds of 20-year mortality than moderate drinkers who did not binge drink.
An association between binge drinking and health outcomes has been demonstrated in epidemiologic studies for decades. Many (but not all) studies have shown an approximately two-fold increase in the risk of adverse outcomes for binge drinkers, in comparison with moderate drinkers who do not binge drink. In reviewing the present study, Forum members commented on the small number of subjects (only 74 binge drinkers in the analysis), and some other analytic weaknesses (e.g., no data on potential changes in drinking habits over 20 years, inadequate control of some potential confounders, results not applicable to the general population as some subjects were recruited because of previous alcohol misuse). Nevertheless, the results of the study support adverse effects on mortality of such a drinking pattern.
There are now considerable scientific data indicating harmful health effects of episodic excessive drinking in terms of coronary heart disease, other diseases of ageing, and mortality. Simply knowing the average intake of subjects over a period of time is inadequate for classifying their alcohol consumption. For middle-aged and older subjects the drinking pattern that has been shown to be associated with the most favorable health outcomes (including greater longevity of life) is regular, light-to-moderate intake, especially when the alcoholic beverage is consumed with food.
Reference: Holahan CJ, Schutte KK, Brennan PL, Holahan CK, Moos RH. Episodic heavy drinking and 20-year total mortality among late-life moderate drinkers. Alcohol Clin Exp Res 2014; pre-publication; DOI: 10.1111/acer.12381.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 134: Comments on “Section 2.3, Alcohol Consumption,” from the “World Cancer Report 2014” issued by the World Health Organization – 11 February 2014
A recently released report by IARC (International Agency for Research on Cancer) of the World Health Organization, entitled “World Cancer Report 2014,” includes a section on alcohol consumption as a factor in the etiology of cancer. From reading this report, it is clear that the conclusion of the authors is that all alcohol consumption is harmful, regardless of the amount consumed, the type of beverage, or the pattern of drinking. The members of the International Scientific Forum on Alcohol Research (the Forum) have real concerns about the WHO report.
It appears that the authors have been very selective in choosing the data upon which they base their conclusions, often citing their own work and ignoring thousands of scientific articles relating alcohol consumption to cancer rates and mortality. The report fails to discuss potential lower risks of cancer associated with polyphenols in wine and some other beverages. It ignores the consistent finding in almost all prospective epidemiologic studies over many decades that total mortality rates are lower among light-to-moderate alcohol consumers (and recent evidence suggests that this may even be true among people with cancer).
Members of the Forum strongly agree that heavy alcohol consumption and “binge” drinking are associated with many adverse effects (and would never be advised by responsible agencies). However, the WHO report seriously undermines its credibility by publishing a report that seems to deliberately ignore overwhelming scientific evidence showing that light-to-moderate consumption of alcohol not only reduces overall mortality but is usually not associated with an increased risk of cancer.
Excessive and binge drinking in young people is a growing scourge in many parts of the world, and alcohol consumption (especially in conjunction with smoking) clearly increases the risk of upper aero-digestive cancers; further, even moderate consumption is associated with a slight increase in the risk of breast cancer in women. However, the scare tactics condemning all alcohol consumption in the WHO report tend to obscure those important messages.
It is the opinion of our Forum that WHO, in the alcohol section of its new publication World Cancer Report 2014, has not provided an objective statement on alcohol and cancer based on current scientific data. By doing so, WHO has lost credibility and, more importantly, has missed a key opportunity to convey important focused messages about alcohol and cancer that would be more likelty to improve the health of the public.
Reference: Rehm J, Shield K. Section 2.3, Alcohol Consumption, from World Cancer Report 2014, pp. 97-106, released 3 February 2014 by IARC (International Agency for Research on Cancer), of the World Health Organization.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 133: Alcohol intake may lower the risk of developing multiple sclerosis — 4 February 2014
Previous research has shown that alcohol consumption may be associated with a reduced risk of rheumatoid arthritis, lupus erythematosus, and other autoimmune diseases. There have also been reports that alcohol may lower the risk of multiple sclerosis (MS). The authors of the present paper have used data from two large Swedish case-control studies of MS to evaluate the relation of alcohol consumption to MS. Key results showed that in both of the case-control analyses, there was a dose-response inverse relation between alcohol consumption and the risk of developing MS. In comparison with subjects reporting no alcohol intake in the 5- or 10-year period during which the diagnosis of MS was first made, subjects in the highest alcohol consumption group (> 112 g/week, about 9 drinks per week for women; >168 g/week, about 14 drinks per week for men) had 30% to 50% lower risk of developing MS. A variety of potential confounders were included in the analysis, including smoking, education, and SES.
Forum members who reviewed this paper all thought that it reflected a well-done analysis. The main concerns were that, as are most studies of uncommon diseases, these were case-control comparisons (which may be associated with recall bias, reverse causation, and other potential confounding variables), and that the investigators could not determine if the “non-drinkers,” their referent group, were lifetime abstainers or former drinkers. Also, while earlier research has shown that the polyphenols in wine may provide protection beyond that of alcohol in combating inflammation, there were no data on beverage-specific results.
In general, however, Forum members welcomed this contribution to our knowledge on the subject, and thought that the authors did a good job in discussing the strengths and weaknesses of their study. There was a brief discussion of potential mechanisms by which alcoholic beverages could lower the risk of MS, but no discussion of the potential added effects related to polyphenolic substances. Forum members also thought that serum uric acid (which may increase with alcohol consumption) could play a role in an autoimmune disease, but this was not discussed by the authors.
Based on previous research and the results of this paper, it is probable that moderate alcohol intake, especially of wine, may lower the risk of developing MS, a neurological disease for which no cure is currently available. While MS is too uncommon a condition to use these findings to recommend alcohol consumption for the prevention of the disease, it would be useful if future research could help determine if, for subjects who already have MS, moderate drinking may affect the progression of their disease.
Reference: Hedström AK, Hillert J, Olsson T, Alfredsson L. Alcohol as a modifiable lifestyle factor affecting multiple sclerosis risk. JAMA Neurology 2014; doi:10.1001/jamaneurol.2013.5858; published online January 6, 2014.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 132: Pattern of alcohol consumption and cause of death in a large European prospective study — 21 January 2014
A large group of investigators participating in the European Prospective Investigation into Cancer and Nutrition (EPIC) study have reported on the association of alcohol consumption with disease-specific mortality over a 12-year period among a very large number of men and women. Alcohol intake over the past year (as well as estimates of earlier intake) was reported at baseline. A variety of approaches were used to identify deaths in the participating cohorts, but validation of the cause of death was not possible. No data were reported on certain key aspects of drinking pattern (frequency of alcohol intake, binge drinking, with meals, etc.) and beverage-specific effects were not reported.
The authors report that the risk of death from cardiovascular diseases was lower, and from cancer and certain other causes of death were higher, among drinkers than among their referent group of “lifetime light users” (men reporting ≤1 drink/week and women reporting ≤ 0.5 drinks/week). However, their graphs of alcohol intake and risk of total mortality (not included in the paper but in supplementary data they provide on the internet) show strong J-shaped curves for increasing alcohol intake for both men and women. For men, the risk among alcohol consumers of up to about 48 gr/day (the equivalent of approximately four “typical drinks”) was lower than that of the lifetime light users that made up the referent group; at higher intake, the risk increased above that of light drinkers. For women, the risk of total mortality for drinkers remained lower than that of the referent group at all reported levels of intake. Despite these findings, the entire paper focuses only on the increased risk of death from alcohol for certain diseases, and almost completely ignores the net, overall effects on total mortality.
Forum reviewers considered that while the analyses were done correctly, there were major weaknesses in the estimation of “lifetime alcohol intake,” no data on the pattern of intake, no validation of coexisting diseases and, especially, no validation of the specific cause of death, even though this was the primary outcome of the study. All of these factors weaken the strong assertions made by the authors in their conclusions.
Forum members were concerned that the authors seemed to obscure the total effects of light-to-moderate drinking (lower risk of all-cause mortality), and emphasize only the harmful effects. Some reviewers considered that the presentation appeared to be based more on ideology than on an unbiased assessment of the data, and one suggested that the paper appears to have been written starting from pre-conceived conclusions, then finding data to support them.
It is interesting that two Commentaries published with this article came to divergent views. One by Stockwell and Chikritzhs emphasized potential bias and confounding that cause concern when relating alcohol to mortality in observational studies. While they then pointed out how well the present authors adjusted for many of these factors, they nevertheless concluded their commentary repeating how such factors are difficult to control and stating that “ . . . a healthy dose of skepticism is warranted for the hypothesis that light/moderate alcohol consumption is beneficial to health.” (They do not mention that data on alcohol and mortality are far more robust that data supporting generally accepted beliefs of the beneficial effects of physical exercise, eating a healthy diet, maintaining a lean body mass, etc.)
On the other hand, the commentary on the present paper by Banks considered the data presented quite sound, and concluded: “If taken as causal, these findings are consistent with most public health advice about alcohol, except that most advice recommends an upper limit to alcohol consumption, but does not actually encourage drinking. In fact, the evidence goes further than this and indicates that, in later life, on average and bearing in mind the priorities and risks of specific individuals, drinking at least some alcohol, but not too much, is likely to minimize the overall risk of death.”
Reference: Bergmann MM, Rehm J, Klipstein-Grobusch K, et al (38 authors). The association of pattern of lifetime alcohol use and cause of death in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Int J Epidemiol 2013;42:1772-1790
Attached Commentaries:
Banks E. Commentary: Lifetime alcohol consumption and mortality: have some, but not too much. Int J Epidemiol 2013;42:1790–1792; doi:10.1093/ije/dyt218
Stockwell T, Chikritzhs T. Commentary: Another serious challenge to the hypothesis that moderate drinking is good for health? Int J Epidemiol 2013;42:1792–1794; doi:10.1093/ije/dyt217
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 131: Effects of alcohol consumption on the risk of gout — 23 December 2013
A new meta-analysis has been conducted to assess the effects of alcohol consumption on the risk of gout. A total of 12 articles with 17 studies involving 42,924 cases met the inclusion criteria. The authors report that the pooled RRs for light (≤1 drink/day), moderate (>1 to <3 drinks/day), and heavy drinking (≥3 drinks/day) vs. non/occasional alcohol drinking were 1.16 (95 % CI, 1.07–1.25), 1.58 (95 % CI, 1.50–1.66), and 2.64 (95 % CI, 2.26–3.09), respectively. The results suggested that alcohol consumption might be associated with increased risk of gout.
Forum reviewers agreed that the analytic methodology in this paper was appropriate. Considerable research has shown that alcohol intake, especially heavier drinking, increases serum uric acid levels and the risk of gout. There remain some questions about the relation of wine consumption with gout, and the present study did not have data to test beverage-specific responses.
Overall, data suggest that alcohol intake, especially heavier drinking, raises serum uric acid levels and may trigger an acute attack in persons with gout, especially those who are not controlling their disease with appropriate medication. A number of studies, including the present one, suggest that even light alcohol intake may increase the risk of developing gout. In any case, the risk appears to be rather low with light drinking, a level of alcohol intake that should reduce the risk of cardiovascular disease. Also, some studies suggest that the risk is lower for the consumption of wine than for the consumption of other beverages containing alcohol.
Reference: Wang M, Jiang X, Wu W, Zhang D. A meta-analysis of alcohol consumption and the risk of gout. Clin Rheumatol 2013;32:1641–1648.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 130: How alcohol consumption may interact with genetic factors that relate to health and disease — 10December 2013
Despite extensive research over the past few decades, our knowledge about the genes that underlie most chronic diseases remains incomplete. For example, even for alcohol-related diseases, it is not possible at present to determine how an individual person will respond over a lifetime to varying amounts of alcohol intake: not all heavy drinkers develop cirrhosis; not all moderate drinkers lower their risk of cardiovascular disease. While the underlying genetic pattern of a person undoubtedly plays a role in his/her health outcomes, environmental factors, including alcohol consumption, may modify the effects of genes. The modification of the effects of genes by environmental factors, such as alcohol intake, can be referred to as “epigenetics.”
A new paper on epigenetics, by a leading scientist who has worked at the National Institute of Alcohol Abuse and Alcoholism (NIAAA) for many years, provides important new insight into mechanisms by which alcohol intake, especially heavy consumption, may modify the activity of genes affecting health. Dr. Zakhari describes specific effects that heavy alcohol intake can have on the activities of enzymes involved in epigenetic modifications. In some cases, alcohol enhances genetically determined effects, in others it suppresses such activity. As stated by the author, “Metabolites, including those generated during ethanol metabolism, can impact disease states by binding to transcription factors and/or modifying chromatin structure, thereby altering gene expression patterns.”
Forum members consider this to be a very well-thought-out and well-done presentation of important new data. They agree with the author that these observations could help researchers to design model medications to treat or at least ameliorate alcohol-related organ damage, such as cirrhosis of the liver and alcohol-related cancers. While reviewers consider that these observations are important in our understanding of how alcohol affects health, they point out that they must be tested in further research, especially epidemiologic studies, to evaluate the extent that such interations between alcohol and genes actually affect health outcomes. Key problems that limit our ability to determine causality of disease from epidemiologic studies include not knowing the underlying genetic susceptibility of individual subjects and, as pointed out in the present paper, not accounting for environmental factors that may modify such genetic effects.
Reference: Zakhari S. Alcohol metabolism and epigenetics changes. Alcohol Research: Current Reviews 2013;35:9-16.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 129: Association of alcohol consumption with skin cancer; A report from the Women’s Health Initiative — 20 November 2013
A report from more than 59,000 women in the Women’s Health Initiative related reported alcohol consumption to the risk of melanoma (MM) and non-melanoma skin cancer (NMSC). This was a fairly large study, with 532 cases of melanoma and 9,593 cases of NMSC occurring over approximately 10 years of follow up. The key reported results were for a higher hazard of MM (HR 1.64) and NMSC (OR 1.23) for drinkers of 7 or more drinks/week, compared with non-drinkers. Lifetime alcohol consumption was also positively associated with hazard of MM and risk of NMSC, with the only significant increases for MM according to type of beverage being seen for women with a preference for white wine or liquor. As shown in many previous studies, the risk of these skin cancers was lower among smokers than among non-smokers.
Forum reviewers thought that this was a very well-done analysis. They did note that there were large decreases in the estimates of HRs related to alcohol consumption when adjustments were made for sun exposure and other known confounders. For example, the HR for MM decreased for total wine from 1.30 to 1.06 when adjusted; for red wine:1.71 to 1.34; for white wine: 1.93 to 1.52; for liquor: 1.87 to 1.65; for beer: 1.34 to 1.18. The magnitude of these changes, as well as the very different baseline characteristics of the women according to their drinking habits, raises the possibility that there may be residual confounding affecting the results. In addition, reviewer Zhang points out that by including subjects with these skin cancers prior to baseline in their main analyses, there could be a problems with bias in their results.
Forum member Klatsky has recently reported on this topic using several decades of follow-up data from the Kaiser-Permanente study, with more than 300,000 subjects and more than 1,000 cases of MM. In that study, he and his colleagues found that among persons preferring wine, the HR for MM at 3+ drinks per day was 1.7 (95% CI 1.2-2.5), while it was 1.2, 1.3, and 1.1 in persons with preference for liquor, beer, and no beverage type. However, at 1-2 drinks per day, wine drinkers had a HR of 0.9. Klatsky states “So maybe too much should not be made of the beverage type data in these analyses. However, the association with alcohol seems statistically solid.”
A previous study by Mukamal, with data from 300,000 subjects participating in a risk factor surveillance survey reports: “Approximately 33.5% of respondents reported a sunburn within the past year. Heavier average alcohol use and binge drinking were both positively associated with prevalence and number of sunburns within the past year. The adjusted odds ratios for prevalence and number of sunburns among binge drinkers were 1.39 (1.31-1.48) and 1.29 (1.20-1.38), respectively.” Klatsky wonders whether “possible confounding by sun is not only an artifact of SES and tropical vacations, but whether heavy imbibers at the beach may fall asleep when exposed or simply do not notice their sunburn until it is severe.” Other Forum reviewers also worry that there may be residual confounding in the present study from sun and ultraviolet exposure.
Klatsky adds: “However, even if the alcohol-melanoma association is due to confounding by sun exposure, the same explanation seems less plausible for the inverse association between smoking and melanoma. While there is obviously no public health utility in any ‘protective’ effects of smoking, that association is scientifically interesting and could be a clue to mechanisms.”
The bottom line is that there are considerable observational epidemiologic data suggesting that alcohol consumption may relate to an increase in the risk of MM and NMSCs. As mechanisms are not known, there is still concern that much of this relation may relate to residual confounding by ultraviolet sun exposure, the most important environmental factor for these diseases.
Rerference: Kubo JT, Henderson MT, Desai M, Wactawski-Wende J, Stefanick ML, Tang JY. Alcohol consumption and risk of melanoma and non-melanoma skin cancer in the Women’s Health Initiative. Cancer Causes Control 2013 (pre-publication) DOI 10.1007/s10552-013-0280-3
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 128: Little effect of alcohol consumption on breast cancer risk found among African-American women — 14 November 2013
Alcohol is known to be a risk factor for breast cancer in Caucasian women, but the evidence in African-American (AA) women is limited and results from previous studies are inconclusive. The present case-control study, based on 803 cases of breast cancer among African American women in the northeastern part of the USA, evaluated associations between recent and lifetime drinking and breast cancer risk. The authors report that there was no association between recent drinking and breast cancer risk, even when stratified by menopausal status or by hormone receptor status. Further, their analyses suggested a slight decrease in cancer risk with alcohol consumption among women who drank when under 20 years of age (OR = 0.65; 95% CI: 0.47–0.89), regardless of menopausal or hormone receptor status.
Forum reviewers point out that this was a case-control study of breast cancer, which always presents an opportunity for recall bias, and the number of cases was not large. Further, AA women generally drink very little, so it may be difficult to determine if larger amounts of alcohol may increase breast cancer risk.
On the other hand, the results were based on a very well-done and complete analysis, with appropriate control for known risk factors, similar results were obtained when recent (in last year) alcohol intake and long-term alcohol consumption were considered, and their finding of increased risk of breast cancer among subjects with a family history of breast cancer, a personal history of benign breast disease, and HRT use strengthen the results.
The results of this study are consistent with those from many previous studies showing little effect of alcohol consumption on breast cancer risk among AA women. However, given that few AA women in the USA drink alcohol, and those that do typically consume only small amounts, the study cannot estimate the potential effect on breast cancer among heavier drinkers. Further, Forum members believed that the decrease in the risk of breast cancer found in this study for drinking early in life (before age 20 years) may be due to residual confounding by socio-economic factors.
Overall, the present study supports previous research suggesting that the light alcohol consumption typically seen among AA women in the USA is not an important factor in their risk of breast cancer. On the other hand, this paper reports similar null results between alcohol and cancer risk among Caucasian women in their study. Current data do not necessarily indicate that there are ethnic differences in alcohol metabolism that may lead to differences between Caucasian and AA women in the association of alcohol consumption with breast cancer, and this study alone cannot be used to support such a premise.
Reference: Chandran U, Zirpoli G, Ciupak G, McCann SE, Gong Z, Pawlish K, Lin Y, Demissie K, Ambrosone CB, Bandera EV. Does alcohol increase breast cancer risk in African-American women? Findings from a case–control study. British J Cancer 2013;109:1945–1953 | doi: 10.1038/bjc.2013.513.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 127: Estimation of alcohol-attributable and alcohol-preventable mortality in Denmark — 6 November 2013
In an attempt to judge the harmful and beneficial health effects related to alcohol consumption, Danish scientists have carried out analyses comparing alcohol-attributable and alcohol-preventable mortality in Denmark. They have used estimates of the potentially harmful effects of alcohol use on more than 20 diseases, giving 100% values to “alcohol use disorders,” although the specific causes of death are not known for this category. Most of the other attributions for harm are realistic, but the alcohol preventable attributions for diabetes and ischemic heart disease appear to be low. The authors conclude that 5.0% of deaths among women and 9.5% of deaths among men were attributable to alcohol in Denmark in 2010, with the majority of all alcohol-attributable deaths caused by high consumption. They attribute only between 2 and 3% of deaths to be preventable by alcohol.
Previous estimates of alcohol-attributable and alcohol-preventable effects have varied widely, emphasizing the importance of the assumptions made by the investigators in any set of analyses. For example, an analysis of deaths in Germany by Konnopka et al (Konnopka A, Hans-Helmut König H-H. The health and economic consequences of moderate alcohol consumption in Germany 2002. Value in Health 2009;12:253-261) concluded that there were more alcohol-preventable deaths than alcohol-attributable deaths and a report from the UK also estimated much lower rates for alcohol-attributable deaths (White IR, Altmann DR, Nanchahal K. Mortality in England and Wales attributable to any drinking, drinking above sensible limits and drinking above lowest-risk level. Addiction 2004;99:749–756). Further, a previous report that included data for Denmark gave very different results for net alcohol effects, estimating that less than 1% of deaths were attributable to alcohol (Britton A, Nolte E, White IR, Gronbaek M, Powles J, Cavallo F, McPherson K. A comparison of the alcohol-attributable mortality in four European countries. Eur J Epidemiol. 2003;18:643–51). It is probable that different underlying assumptions of alcohol effects on various diseases are the prime reason for such differences.
There is no question that heavy alcohol consumption contributes to a large number of disease conditions, and the findings of this study emphasize the magnitude of the problem. On the other hand, if the potentially beneficial effects of moderate alcohol consumption on many common diseases are underestimated, a net unfavorable result, as in the present study, is unavoidable. It will be interesting to see what assumptions are made in other studies such as this, and how such assumptions affect the outcome of analyses.
Reference: Eliasen M, Becker U, Grønbæk M, Juel K, Tolstrup JS. Alcohol-attributable and alcohol-preventable mortality in Denmark: an analysis of which intake levels contribute most to alcohol’s harmful and beneficial effects. Eur J Epidemiol 2013; DOI 10.1007/s10654-013-9855-2
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 126: Moderate alcohol intake may lower the risk of rheumatoid arthritis — 11 October 2013
Moderate alcohol intake, compared with abstinence, has been related to lower inflammatory markers and a reduced risk of many auto-immune diseases, including rheumatoid arthritis (RA), systemic lupus erythematosus, autoimmure diabetes, and Graves hyperthyroidism. The present large meta-analysis relating alcohol to RA includes data from 5 prospective cohort studies and 3 nested case-control studies. Their analyses are based on prospective data from a total of almost 200,000 subjects, among whom 1,878 developed RA.
This meta-analysis concludes that low to moderate alcohol consumption is inversely associated with the development of RA. It suggests a “J-shaped” curve, with a lowered risk for an average intake of up to 15 g of alcohol (about 1 to 1 ½ typical drinks), in comparison with non-drinkers, and an increased risk for heavier drinking. While the immediate effects were greater for women in this study, for long-term effects the authors noted that “Regardless of sex, a consistent low to moderate alcohol consumption for a period of at least 10 years was found to have a 17% reduction in RA risk.”
Beneficial effects of alcohol on indices of inflammation have been shown repeatedly. The probable mechanism of alcohol’s effect on the risk of RA is down regulation of the immune response and a decrease in pro-inflammatory cytokines.
Reference: Jin Z, Xiang C, Cai Q, Wei X, He J. Alcohol consumption as a preventive factor for developing rheumatoid arthritis: a dose-response meta-analysis of prospective studies. Ann Rheum 2013. doi: 10.1136/annrheumdis-2013-203323
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 125: Effects of alcohol consumption on risk of colorectal cancer; potential modification by folate intake — 25 September 2013
Many epidemiologic studies have shown a small increase in the risk of breast cancer and colorectal cancer to be associated with alcohol consumption. Some have found that higher intakes of folic acid may attenuate such an increase in risk. The present study was designed to evaluate the influence of alcohol consumption on the risk of colorectal cancer according to folic acid fortification period in the United States. The relation of alcohol intake to colorectal cancer in two prospective studies (the Nurses’ Health Study and the Health Professionals Follow-up Study) was compared for a prefortification period (before 1998) with such risk estimates during the postfortification period, which began in 1998. A total of 2,793 cases of invasive colorectal cancer were documented.
The authors concluded that their data support an increase in colorectal cancer with high alcohol intake, and suggest that the risk may be lower in the postfortification period due to a higher folate intake in the US population. Forum reviewers had some concerns about these conclusions, as they point out that no dose-response relation between alcohol and colorectal cancer was shown in either period, and in data since 1998 no significant relation is seen between alcohol and such cancers. In fact, the authors of the present study state: “We also examined drinking pattern in relation to colorectal cancer risk; neither frequency of drinking nor quantity of drinking was associated with the risk of colorectal cancer;” they do not report their data upon which that statement is based.
Overall, the present paper does not answer the question as to the extent to which alcohol may relate to the risk of colorectal cancer, or if folate intake may modify any relation that may exist. Given that colorectal cancer (and breast cancer in women) are so common, it is important to evaluate how dietary folate and other nutrients may relate to such cancers. Further research on the relation of alcohol to these cancers, and potentially modifying factors, is greatly needed.
Reference: Nan H, Lee JE, Rimm EB, Fuchs CS, Giovannucci EL, Cho E. Prospective study of alcohol consumption and the risk of colorectal cancer before and after folic acid fortification in the United States. Annals of Epidemiology 2013;23:558-563.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 124: The J-shaped curve for the relation of alcohol consumption to mortality — 17 September 2013
An analysis based on data from more than 110,000 subjects in the USA, of whom 3,364 died during a follow-up period of up to 9 years, was used to evaluate the relation of “heavy drinking” and “nonheavy drinking” to the risk of all-cause mortality. The authors defined heavy drinking as 5 or more drinks/occasion, and recorded the frequency in which subjects consumed such amounts. Subjects consuming < 5 drinks/occasion were classified as nonheavy drinkers.
The key findings of the analyses were that there was a positive and linear increase in risk of mortality for subjects consuming heavy amounts of alcohol, with the risk increasing as drinking at this level was more frequent. For nonheavy drinkers, there was a J-shaped relation with mortality. The point at which the nonheavy drinkers’ risk of mortality exceeded that of abstainers was between 4 and 5 drinking occasions/week.
Forum reviewers thought that this was a well-done analysis that emphasizes the importance of the pattern of drinking, and not just the average weekly intake. Although the upper limits of drinks/occasion exceeded that usually considered as “moderate,” a J-shaped curve between alcohol and mortality for these drinkers was demonstrated. This is the pattern usually seen in prospective epidemiologic studies when “moderate” is defined at somewhat lower levels of alcohol intake.
Forum reviewers agreed with the conclusions of the authors regarding the importance of considering the pattern of drinking when evaluating the health effects of alcohol. The authors concluded: “Promoting less harmful drinking patterns by reducing heavy drinking frequency is an appropriate harm reduction strategy, and assessing drinking pattern by determining the frequency of heavy and nonheavy drinking is a simple and fast way to determine risk and promote less risky drinking behavior.”
Reference: Plunk AD, Syed-Mohammed H, Cavazos-Rehg P, Bierut LJ, Grucza RA. Alcohol consumption, heavy drinking, and mortality: Rethinking the J-shaped curve. Alcohol Clin Exp Res 2013;pre-publication: DOI: 10.1111/acer.12250
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 123: Alcohol consumption and lymphoid and myeloid neoplasms — 5 September 2013
Many prospective studies have shown that moderate drinkers are at lower risk of certain types of lymphoid cancer. For example, a report in 2009 from the Million Women’s Study in the UK found that alcohol consumption showed a significant inverse association with the occurrence of non-Hodgkin lymphoma (NHL). Further, a 2012 paper from that study based on 9,162 incident cases of haematological malignancy, including 7,047 lymphoid and 2,072 myeloid cancers, concluded: “Among predominantly moderate alcohol drinkers, higher intake was associated with lower risk of lymphoid malignancies.” Those investigators did not find a significant effect of alcohol on the risk of myeloid tumors, such as acute myeloid leukemia. Another 2012 paper based on almost 2,000 cases of Non-Hodgkin Lymphoma concluded: “In summary, findings from the prospective study presented here support the hypothesis that alcohol intake might be associated with a reduced risk of NHL.”
The authors of the present paper from the Netherlands, based on 17.3 years of follow up with 1,375 cases of lymphoid and 245 cases of myeloid neoplasms, did not find a statistically significant reduction in the risk of lymphoid cancers, and the authors suggest: “If any association between alcohol consumption and lymphoid neoplasms exists, our study suggests an increased risk rather than a decreased risk.”
While reasons for this difference in results of this study when compared with other recent studies may be used to better understand the association between alcohol and such cancers, Forum reviewers were concerned about a number of aspects of this study. For example, the authors had data on alcohol consumption only at baseline for this very long (17+ year) follow up, so changes (either increases or decreases in intake) were not known. Further, the key relations reported were not adjusted for a large number of potentially confounding variables, such as a positive family history of hematological cancer. (The authors state that they carried out such multivariable analyses but do not present the data.) Of even more concern was the apparent inverse effect of alcohol on cancer risk for a number of types of tumors when dose-response relations were shown.
Given the rather consistent findings in other very large studies of hematological malignancies that the risk of many types of lymphoid cancer may be reduced by alcohol, and inconsistencies in the results of the present analyses, it is difficult to conclude that the present paper should change our current interpretation of the association between alcohol and these types of cancer.
Forum members look forward to reports from other prospective studies on this topic. For the present, however, the overwhelming scientific evidence suggests that moderate alcohol consumption is associated with a decrease in the risk of many types of lymphoid malignancies, but has little effect on myeloid cancers.
Reference: Heinen MM, Verhage BAJ, Schouten LJ, Goldbohm RA, Schouten HC, van den Brandt PA. Alcohol consumption and risk of lymphoid and myeloid neoplasms: Results of the Netherlands cohort study. Int J Cancer 2013l133:1701–1713.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 122: Does moderate wine consumption lower the risk of developing depression? — 3 September 2013
There is a large literature relating heavy alcohol consumption to depression: most studies show that heavy drinkers tend to be depressed, and depressed people may self-medicate with large amounts of alcohol. This large prospective study of subjects at high risk of cardiovascular disease has shown that “moderate” drinkers, especially wine drinkers (the majority of their subjects), were at lower risk of developing depression during 7 years of follow up than were non-drinkers. An important aspect of this study is indeed that the analyses were based on moderate drinkers, as people exceeding certain amounts of alcohol or testing positive on the CAGE questionnaire (a measure of alcohol misuse) were excluded.
Strengths of the study include it being a large prospective study, with more than 5,000 subjects, aged 55-80 years at baseline, who were followed for up to 7 years for the initial development of clinical depression (which was diagnosed in 443 instances). Especially important was the ability of the investigators to have repeated assessments of alcohol consumption, every two years. A rather complete list of potentially confounding variables was available. The key findings of the study were that subjects reporting >5-15 grams/day of total alcohol intake, and wine drinkers of 2-7 drinks/week, were at a lower risk of developing depression than were non drinkers.
Some Forum members remained concerned that there may have been residual confounding by other lifestyle habits, and that the results may apply primarily to subjects who are also following a Mediterranean-type diet and lifestyle. Also, data were not available to evaluate the relation of heavy drinking or alcoholism to depression. However, the authors provide good scientific support for their conclusions that subjects reporting >5-15 grams/day of total alcohol intake (from about ½ to 1 ½ of a typical drink), and wine drinkers of 2-7 drinks/week, are at approximately 30% lower risk of developing depression than are abstainers of alcohol.
Reference: Gea A, Beunza JJ, Estruch R, et al (17 authors). Alcohol intake, wine consumption and the development of depression: the PREDIMED study. BMC Medicine 2013. Advanced publication, released 29 August 2013.
For the full critique of this paper by members of the International scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 121: Differences between wine and other alcoholic beverages in terms of adverse consequences of alcohol consumption – 22 August 2013
Questionnaire-based data on alcohol consumption were collected from more than 5,000 military recruits in Switzerland, who had a mean age of just over 19 years. There were very few drinkers who averaged more than 21 drinks/week, so the emphasis was on the effects of what is usually referred to as “binge drinking,” defined in this study as the consumption of 6 or more typical drinks (a drink containing 10-12 g of alcohol) on a single occasion. The “preference” of one particular type of beverage was based on the subject indicating that it made up more than two-thirds of his total alcohol consumption. The specific type of beverage preferred — beer, wine, or “other beverages” (the latter including apertifs, “pops,” chillers, and coolers) — was related to the pattern of drinking (frequency of binge drinking) and to the reported occurrence of adverse alcohol-related consequences (e.g., blackouts, driving after heavy drinking, missing work due to drinking, accidents, unprotected sex, encounters with police).
The authors report: “Preference for beer was associated with risky drinking patterns and, comparable with a preference for strong alcohol, with the use of illicit substances (cannabis and other illicit drugs). In contrast, a preference for wine was associated with low-risk alcohol consumption and a reduced likelihood of experiencing at least four negative alcohol-related consequences or of daily cigarette smoking.” More frequent binge drinking of any beverage was strongly associated with an increase in adverse alcohol-related consequences.
Forum reviewers thought that the adverse outcomes, especially those related to heavy beer intake, tend to characterize a particular subculture that demonstrates problematic substance use due to personal characteristics of the subjects. The unhealthy outcomes may be a feature more of the cultural habits of the subjects rather than just due to the type of beverage they consume most frequently.
The authors conclude that strategies for preventing problems with alcohol abuse should attempt to reduce excessive drinking of all types of beverages. However, they add: “to lessen the additional negative effects of beer and strong alcohol, which are particularly cheap in Switzerland, targeted strategies such as minimum pricing policies for these beverage types should be considered.” Forum members think that the extent to which such beverage-specific price restructuring would decrease unhealthy drinking practices among young people remains unclear.
Reference: Dey M, Gmel G, Studer J, Dermota P, Mohler-Kuo M. Beverage preferences and associated drinking patterns, consequences and other substance use behaviours. European Journal of Public Health 2013; advance access; doi:10.1093/eurpub/ckt109
For the full critique of this critique by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 120: Binge drinking impairs endothelial function in young people — 20 August 2013
The function of the vascular endothelium is a key process in the development of atherosclerosis and coronary heart disease, and extensive studies among middle-aged and elderly adults generally show beneficial effects of moderate drinking on vascular function. Whether or not alcohol consumption among young people has any lasting biological effects on cardiovascular risk is unclear: risk factors tend to track from childhood into adulthood, but specific long-lasting effects related only to drinking in young people are not known. Hence, data are currently not available to answer the question as to when during life people might consider beginning the moderate consumption of alcohol for the potential lowering of cardiovascular risk later in life.
The present study does not answer that question, as it only compares abstaining young people with binge drinkers, with the latter being defined as subjects reporting that they consumed ≥ 5 drinks in 2 hours for males, and ≥ 4 drinks in 2 hours for females. (The average number of binge-drinking episodes for these subjects was 6 ± 1 within the past month.) It does not compare abstainers with moderate drinkers. However, the paper does show that binge drinking among 18 – 25 year olds has adverse effects on endothelial function.
Forum reviewers were pleased to see this study, but point out that it is a cross-sectional analysis, and only compares binge drinkers with non-drinking young people. Further, inadequate data are presented to know the degree to which the results of the study may suffer from residual confounding from other factors.
The authors conclude that their study showed adverse effects on both microvascular and macrovascular function to be associated with frequent binge drinking in young people. It is hoped that these investigators, or others, will in the future provide data on the effects on vascular function of regular, moderate alcohol consumption among young people. It would also be interesting to learn if effects are different for high-polyphenol wine than for other beverages. Further, it will be important to determine how long beneficial or adverse effects on vascular function may persist, with or without continued alcohol intake.
Reference: Goslawski M, Piano MR, Bian J-T, Church EC, Szczurek M, Phillips SA. Binge drinking impairs vascular function in young adults. J Am Coll Cardiol 2013;62:201–207.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 119: A consensus statement on the association of moderate alcohol consumption and health — 13 August 2013
A group of Italian scientists has prepared a consensus paper to review the available evidence on the association between moderate alcohol use and health and disease. The report resulted from extensive discussions among 36 prominent Italian scientists, and provides a working document for the scientific and health professional communities. The report has been signed by 19 separate societies or federations in Italy, including societies in nutrition, cardiology, and general medicine, as well as organizations of scientists dealing with diabetes, hypertension, and obesity.
The consensus report ends with four conclusions:
“(1) In healthy adults and in the elderly, spontaneous consumption of alcoholic beverages within 30 g ethanol/d for men and 15 g/d for women is to be considered acceptable and do not deserve intervention by the primary care physician or the health professional in charge. In fact, there is no evidence to suggest complete abstention from alcohol drinking by moderate users.
(2) Patients with increased risk for specific diseases, for example women with familiar history of breast cancer, or subjects with familiar history of early CVD or cardiovascular patients should discuss their drinking habits with their physician.
(3) No abstainer should be advised to drink for health reasons.
(4) Alcohol use must be discouraged in specific physiological or personal situations or in selected age classes (children and adolescents, pregnant and lactating women and recovering alcoholics). Moreover, the possible interactions between alcohol and acute or chronic drug use must be discussed with the primary care physician.”
Forum reviewers considered this to be a well-done and generally well-balanced appraisal of the current literature on alcohol and health; it could help inform physicians and the general public about our current knowledge on this topic. However, Forum reviewers were concerned by several aspects of the report where it appeared that the conclusions were more “political” than “scientific” (perhaps necessary to gain the support of all of the societies endorsing the report).
The authors of the report provided good data to support their first two conclusions, and recent publications that were not available to the authors at the time they prepared their report strongly support these conclusions. However, Forum members found little data provided in the paper to support the third statement in their summary; in fact, the information the authors presented in the text would tend to support the opposite conclusion. Further, while it may be correct, their fourth conclusion was not supported by scientific data in the paper.
Forum members agreed that the importance of the effects of alcohol consumption on total mortality must always be considered, and agreed with the statement of the authors that “Low levels of alcohol intake (1-2 drinks per day for women and 2-4 drinks per day for men) are inversely associated with total mortality in both men and women.”
Key areas that the Forum believed could have been given more emphasis related to the association between alcohol and diabetes mellitus, where data strongly support an approximately 30% lower risk for moderate drinkers, in comparison with non-drinkers. And the risk of cardiovascular disease is considerably reduced among diabetics who consume alcohol moderately. And the potential effects of moderate drinking on reducing the risk of congestive heart failure, a rapidly increasing health problem related to ageing of the population, were not discussed. Forum members also wished that more emphasis had been given in the consensus report to the pattern of drinking: current data indicate that regular moderate drinking, rather than binge drinking, is the pattern associated with the most favorable health outcomes.
Overall, this consensus report is an important and useful addition to the scientific literature on the relation of moderate alcohol consumption to a variety of health outcomes. It could be of great values to physicians and policy makers when providing advice to the public regarding the effects of alcohol on health.
Reference: Poli A, Marangoni F, Avogaro A . . . de Gaetano G . . . et al (total of 36 authors). Moderate alcohol use and health: A consensus document. Nutrition, Metabolism, & Cardiovasular Disease 2013;23:487-504.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 118: Clustering of alcohol consumption with socioeconomic and biologic risk factors for cancer — 30 July 2013
It has been shown in most previous studies that moderate drinkers, especially those who generally consume wine, tend to have other “moderate” lifestyle factors. For example, they tend to be better educated, of higher socio-economic status, and generally are more active and eat a healthier diet than non-drinkers. An exception is cigarette smoking, which tends to be more common in drinkers than in abstainers. Epidemiologists studying alcohol and health are always striving to adjust appropriately for other lifestyle factors, attempting to assure that the difference in health outcomes among subjects relates to their drinking, and not to associated lifestyle factors.
In the present study, the investigators related alcohol consumption to a large number of socio-demographic and lifestyle factors that relate to the risk of cancer. They report that several factors were associated with alcohol consumption ≥10g/d in both genders: older age, smoking, higher socio-demographic category, higher income, and less healthy dietary intakes. Other factors were associated with alcohol consumption differently for men and women. The authors then report that the total number of such factors was higher among consumers of ≥10g/d of alcohol than among abstainers or lighter drinkers. They conclude: “The multiplicity of deleterious lifestyle behaviours combined with alcohol drinking must be taken into account in cancer prevention efforts. Gender-specific medical advice for people with personal or family history of alcohol-related diseases, including cancer, should be strengthened.”
While Forum reviewers found the data presented in this paper to be of interest, they did not believe that simply adding up all adverse risk factors provided useful information for the prevention of cancer. It is well known that smoking is a major risk factor for certain cancers, and in almost all studies alcohol consumers are more likely to be smokers; hence, drinkers should certainly be advised about the dangers of smoking. On the other hand, by simply summing the number of factors into a total score, the authors included a number of risk factors for which there is less of a scientific basis for their effect on cancer risk (e.g, the intake of supplements). Such factors should not be given the same weight as smoking as risk factors for cancer. Further, this study was carried out among computer-literate volunteers, so it may have limited relevance for the general population.
There have been extensive data showing that “healthy” and “unhealthy” lifestyle factors tend to cluster: for example, light-to-moderate drinkers tend to be leaner and eat a healthier diet than non-drinkers or heavy drinkers, as shown in this study. However, the prevention of chronic diseases relates to a large number of behaviors, and alcohol consumption cannot be considered as an isolated factor. Current epidemiologic data suggest that the combination of not smoking, being physically active, eating a healthy diet, avoiding obesity, and, unless contraindicated, regularly consuming small amounts of an alcoholic beverage, together make up what can be defined as a “healthy lifestyle.”
Reference: Touvier M, Druesne-Pecollo N, Kesse-Guyot E, Andreeva VA, Galan P, Hercberg S, Latino-Martel P. Demographic, socioeconomic, disease history, dietary and lifestyle cancer risk factors associated with alcohol consumption. Int J Cancer 2013;in press
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 117: Changes in alcohol intake modify levels of fibrinogen, an important risk factor for coronary heart disease — 18 July 2013
A prospective analysis of data from 2,520 subjects in the Coronary Artery Risk Development in Young Adults Study (CARDIA) cohort related reported alcohol intake at two examinations, 13 years apart, to levels of fibrinogen on the two occasions. Fibrinogen is a strong determinant of thrombosis, and is an important risk factor for coronary heart disease. The authors report that, in comparison with participants who never drank, those who became/stayed drinkers had smaller increases in fibrinogen, while those who quit drinking had the highest increase in fibrinogen over 13 years of follow-up. They conclude that lower levels of fibrinogen may be a key mechanism for the established protective effect of moderate alcohol intake on cardiovascular disease outcomes.
Forum reviewers considered this to be a potentially important paper, as the finding of higher fibrinogen among never drinkers and those who quit drinking may relate to the higher risk of coronary disease commonly reported from such subjects in prospective studies. However, the reviewers point out that the reasons that subjects quit drinking are not known (although the authors did adjust for conditions related to quitting drinking). Further, blood clotting factors other than fibrinogen may be affected by changes in alcohol consumption, and they were not reported in this paper. More research will be needed to determine if changes in fibrinogen levels are key elements in alcohol’s effects on cardiovascular disease.
Reference: Okwuosa TM, Klein O, Chan C, Schreiner P, Liu K, Green D. Long-term change in alcohol-consumption status and variations in fibrinogen levels: the coronary artery risk development in young adults (CARDIA) study. BMJ Open 2013;3:e002944. doi:10.1136/bmjopen-2013-002944
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 116: Effects of genetic factors on the metabolism of alcohol — 10 July 2013
A summary paper on genetically determined mechanisms related to the metabolism of alcohol and acetaldehyde describes numerous ways that the metabolism, especially of acetaldehyde, may be modified, both in the periphery of the body and in the brain. Individuals with a mutation of the aldehyde dehydrogenase gene (the ALDH2*2 allele), and certain other genetically determined enzymes, do not tolerate alcohol and are much less likely to become alcohol abusers. The authors state that their studies suggest possible therapeutic avenues in the treatment of alcoholism.
Reference: Israel Y, Rivera-Meza M, Karahanian E, Quintanilla ME, Tampier L, Morales P, Herrera-Marschitz M. Gene specific modifications unravel ethanol and acetaldehyde actions. Front Behav Neurosci 2013;7:80.doi:10.3389/fnbeh.2013.00080
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 115: Potential association of alcohol consumption with diverticulosis — 25 June 2013
The etiology of diverticulosis of the colon is poorly understood. Many, but not all, studies suggest that low fiber intake and obesity increase the risk; few studies have evaluated the relation of alcohol consumption and diverticulosis, with inconclusive results. This paper tests the cross-sectional association of alcohol consumption with diverticulosis among 746 asymptomatic consecutive subjects undergoing screening colonoscopies in Lebanon.
One-half of the subjects in this study were abstainers. Most of the “drinkers” stated that they consumed alcohol occasionally or < 1 drink/day; only about 10% reported 1 or more drinks/day, and no data on type of beverage or pattern of drinking were available. Nevertheless, from their analyses the authors conclude that alcohol consumption raises the risk of diverticulosis.
Forum members considered that this cross-sectional analysis provides little support for a causative effect of alcohol on the risk of diverticulosis. Most larger observational studies have not shown such an effect. In the present study, about 90% of subjects were either abstainers or consumed alcohol only occasionally or averaged < 1 drink/day. Further, the investigators did not evaluate the pattern of drinking (including binge drinking) and the results do not support an increase in risk with greater drinking (lack of a dose-response relation). Mechanisms for such an effect are largely unknown. Thus, few of the Hill criteria for “causality” are met.
The authors’ use of an inter-country comparison of per-capita alcohol intake and reported diverticulosis has no relevance: there are large cultural differences between nations with high and those with low per-capita alcohol intake, and alcohol use may well have been just a marker for a western-type culture. While the present study could be used to generate an hypothesis of a relation of alcohol intake to diverticulosis, attempts to validate such an association will require much additional research.
Reference: Sharara AI, El-Halabi MM, Mansour NM, Malli A, Ghaith OA, Hashash JG, Maasri K, Soweid A, Barada K, Mourad FH, El Zahabi L. Alcohol consumption is a risk factor for colonic diverticulosis. J Clin Gastroenterol 2013;47:420–425.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 113: Metabolic and biochemical mechanisms by which alcohol consumption affects health — 11 June 2013
A large study from Australia, that included a high percentage of current or former alcohol abusers, related alcohol consumption with a variety of metabolic and biologic parameters that relate to health. Included were markers of lipid function, inflammation, glucose metabolism, and liver function. As expected, there was a linear increase in HDL-cholesterol with increasing alcohol intake; somewhat surprisingly, there was a linear decrease in insulin levels with increasing alcohol consumption (which may relate to the typical finding of a significantly lower risk of diabetes mellitus among moderate drinkers). Essentially all of the other factors showed a “J-shaped” or “U-shaped” relation with alcohol: a decrease with small to moderate amounts of alcohol and an increase with larger intake.
In their association with alcohol, the lowest (most favorable) values of parameters varied by the measure: lowest triglycerides at about 1 to 2 drinks per day, lowest CRP at about 1 drink/day, lowest blood sugar and lowest alkaline phosphatase values at 1 to 3 drinks/day. Adverse effects on liver enzymes, blood glucose, and inflammatory markers showed a threshold level of intake that varied somewhat by marker. For example, reported non-drinkers had higher values of CRP, triglycerides, and alkaline phosphatase; among drinkers, significant increases were seen only in consumers of 40 or more drinks/week. Unfortunately, the investigators did not report on the pattern of drinking, which usually shows preferable results from regular, moderate intake of alcohol with no binge drinking.
The key findings of the study can be summarized as favorable effects of moderate alcohol intake on HDL-cholesterol and insulin levels, and for most other factors (including liver enzymes, triglycerides, blood glucose, and the inflammatory marker CRP), a “J-shaped” relation: lower values with light drinking and higher values with larger amounts of alcohol. For most of these, there was either no effect or a favorable effect until alcohol intake exceeded a “threshold value,” at which heavier drinking began to show adverse effects.
Forum reviewers agreed with the conclusion of the authors: “The pattern of potentially beneficial effects of alcohol on HDL-C and insulin increasing progressively as consumption increases, whereas the negative effects show thresholds, is consistent with net U- or J-shaped effects of alcohol on health.” While actual health outcomes were not evaluated in this study, overall it provides strong support for the results of most prospective epidemiologic studies that show lower rates of cardiovascular and other diseases among light-to-moderate drinkers than among abstainers or heavy drinkers.
Reference: Whitfield JB, Heath AC, Madden PAF, Pergadia ML, Montgomery GW, Martin NG. Metabolic and biochemical effects of low-to-moderate alcohol consumption. Alcohol Clin Exp Res 2013;37:575–586.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 112: Relation of alcohol intake to risk of dying from cancer — 23 May 2013
This paper presents a meta-analysis that related alcohol consumption to all-cancer mortality; it was based on almost 50,000 deaths reported in the literature from prospective cohort studies. Forum reviewers had some concerns about the conclusions of the paper, based on some discrepancies in the text, the lack of data on drinking pattern, no beverage-specific results, etc. Nevertheless, as expected, the reported average consumption of 50 or more grams of alcohol per day (equivalent to 4 or more typical drinks each day) was associated with an estimated 32% increased risk of dying from cancer.
However, there was no increase in the estimated risk of cancer death for subjects classified as “moderate” drinkers (defined by the authors using a wide range of intake: 12.6 to 49.9 grams/day, the equivalent of up to approximately 4 or more typical drinks). Further, Forum members were surprised that a slight but statistically significant decrease in cancer mortality risk was seen for “light” drinkers (those reporting an average of ≤ 12.5 grams/day, or about one typical drink). Forum members appreciated that misclassification of cause of death or residual confounding could have contributed to this latter result.
It is especially important that the only significant increase in risk in cancer mortality among the almost 50,000 cancer deaths reported in this meta-analysis was for consumers of 50 grams or more of alcohol. This suggests strongly that the overall risk of cancer mortality related to alcohol consumption is primarily (perhaps almost exclusively) from heavier drinking. Certainly, the findings from this study do not support the premise that “any amount of alcohol increases the overall risk of dying from cancer.”
Reference: Jin M, Cai S, Guo J, Zhu Y, Li M, Yu Y, Zhang S, Chen K. Alcohol drinking and all cancer mortality: a meta-analysis. Ann Oncol 2013;24:807-816. doi: 10.1093/annonc/mds508.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 111: Association of alcohol consumption with a measure of osteoporosis in elderly women — 7 May 2013
The density of bones, measured as bone mineral density (BMD), is strongly related to osteoporosis. Elderly women with osteoporosis, in particular, are at increased risk of fractures of the hip, arm, and spine; such fractures often relate to severe disability. With data on alcohol collected as part of a clinical trial on the prevention of osteoporosis, investigators in Finland have related alcohol consumption to changes over three years in BMD. After those excluded due to incomplete data, data on 300 women were available for analysis. The majority of women were abstainers or consumed little alcohol. Nevertheless, the results support much earlier research: regular, moderate drinking is associated with higher levels of BMD (i.e., lower risk of osteoporotic fractures) than is abstinence.
Forum reviewers, as did the authors, noted a number of limitations of the study: a rather small cohort with a very low intake of alcohol, a short duration of follow up, and rather small differences according to whether the women consumed alcohol or not.
Data from European surveys have shown that women in Finland tend to have high levels of osteoporosis and to drink very little; hence the increase in BMD associated with alcohol intake, even though slight, could be important in this population. Over the past three decades, there has been an increase in alcohol consumption in Finland, especially a marked increase in the consumption of wine. Hence, some Forum reviewers thought that the improvement in BMD among drinkers in this study may have been primarily from wine (which may have additional components, other than alcohol, that relate to BMD). However, the number of subjects was not large enough to test this hypothesis in the present study. Overall, this study supports the premise that moderate alcohol intake, along with an adequate calcium intake and vitamin D and exercise, may have a favorable influence on the risk of developing osteoporosis
Reference: Sommer I, Erkkilä AT, Järvinen R, Mursu J, Sirola J, Jurvelin JS, Kröger H, Tuppurainen M. Alcohol consumption and bone mineral density in elderly women. Public Health Nutr 2013;16:704-712. doi: 10.1017/S136898001200331X.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 110: Divergent effects of regular moderate and binge drinking – 30 April 2013
The present study relates alcohol consumption measured in young to middle-aged adults to mortality over a follow-up period of 20 years. The analyses are based on data from a large population in a region of Norway where the alcohol drinking pattern most commonly reported was binge drinking on infrequent occasions. Previous research has demonstrated that a very different drinking pattern – the frequent consumption of small amounts of alcohol – is generally considered to be the pattern associated with most health benefits.
In the present study, both men and women who reported consuming alcohol up to twice a month had about 20% lower mortality than did abstainers. All groups reporting binge drinking had higher mortality than non-binge drinkers (which was statistically significant for men and had a similar estimated effect among women). Cardiovascular and ischemic heart disease mortality had similar patterns as total mortality, being lower among drinkers but higher among those who reported binge drinking.
The key finding of this study is that there are divergent effects on mortality of the frequency of drinking and the amount of alcohol consumed per occasion. While the results for this study may reflect a certain Northern European pattern of drinking (not frequent but heavy on each occasion), they may not apply to other European or North American populations, where drinking is more frequent but binge drinking less common. Nevertheless, the results of this study support results typically found in more moderately drinking populations: more frequent drinking, but smaller amounts per occasion, is the pattern of alcohol consumption associated with the lowest risk of mortality. Both aspects of drinking must be considered when studying the relation of alcohol to mortality.
Reference: Graff-Iversen S, Jansen MD, Hoff DA, Høiseth G, Knudsen GP, Magnus P, Mørland J, Normann PT, Næss ØE, Tambs K. Divergent associations of drinking frequency and binge consumption of alcohol with mortality within the same cohort. J Epidemiol Community Health 2013;67:350-357. doi:10.1136/jech-2012-201564.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 109: In women developing breast cancer, moderate alcohol consumption before or after diagnosis does not increase breast cancer mortality and decreases total mortality — 16 April 2013
Most previous research has shown a slight increase in the risk of breast cancer (BrCa) among women who consume alcohol (versus nondrinkers), even among those whose average is only one drink/day. The association with death due to breast cancer is less clear, although overall total mortality among moderate drinkers is almost always lower than among non-drinkers; this reduction is generally attributed to a lower risk of cardiovascular disease.
The present study related alcohol consumption, both prior to the diagnosis of BrCa and after the diagnosis, with survival; deaths from BrCa and from cardiovascular disease, as well as total mortality, were related to alcohol intake. Specifically, in this study the authors assessed alcohol intake in a cohort of 22,890 women with incident invasive breast cancer (BrCa) who were residents of one of four US states and diagnosed at ages 20 to 79 years. During a median follow-up period of 11.3 years after diagnosis of BrCa, 7,780 deaths occurred, including 3,484 attributed to breast cancer.
Based on a quadratic analysis, moderate alcohol consumption before diagnosis showed a tendency towards lower risk of death from BrCa, and a significantly greater reduction in the risk of cardiovascular disease mortality and total mortality. Alcohol consumption after diagnosis was not associated with disease-specific survival, but was associated with a lower risk of total mortality. For women consuming alcohol prior to the diagnosis of BrCa, those who decreased their intake showed little effect on mortality, while those who increased their intake showed further lowering of their risk of cardiovascular and total mortality.
Forum reviewers considered this to be an excellent paper providing important new data on the association of alcohol consumption with survival after a diagnosis of invasive breast cancer. They thought that the statements of the authors accurately reflected their data, as they concluded: “Overall alcohol consumption before diagnosis was not associated with disease-specific survival, but we found a suggestion favoring moderate consumption. There was no evidence for an association with postdiagnosis alcohol intake and breast cancer survival. This study, however, does provide support for a benefit of limited alcohol intake for cardiovascular and overall survival in women with breast cancer.”
An accompanying editorial* agreed with the conclusions of the authors. The editorial stated, “Based on the best available evidence, including [the present report], it appears that modest alcohol consumption after breast cancer diagnosis, up to approximately one drink per day on average, may be associated with optimal overall survival, without compromising breast cancer-specific survival.”
*Demark-Wahnefried W. To your health: How does the latest research on alcohol and breast cancer inform clinical practice? jco.ascopubs.org/cgi/doi/10.1200/JCO.2013.490466),
Reference: Newcomb PA, Kampman E, Trentham-Dietz A, Egan KM, Titus LJ, Baron JA, Hampton JM, Passarelli MN, Willett WC. Alcohol consumption before and after breast cancer diagnosis: Associations with survival from breast cancer, cardiovascular disease, and other causes. J Clin Oncol 2013; pre-publication. Available at jco.ascopubs.org/cgi/doi/10.1200/JCO.2012.46.5765
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 108: An unusual paper relating alcohol consumption to the risk of stroke
Numerous well-done prospective epidemiologic studies have shown that while heavy drinking may increase the risk of stroke, light-to-moderate alcohol consumption is usually associated with a significant decrease in the risk of the most common type of stroke, ischemic stroke.
This paper from investigators in Finland states that it was designed to relate alcohol consumption and obesity to the risk of ischemic stroke. Unfortunately, even though it has clearly been shown that the amount and pattern of alcohol consumption strongly modify the effect on the risk of stroke, for some unknown reason the authors have grouped all consumers of alcohol into a single group. Specifically, there are no data given that describe the relation of light-to-moderate alcohol consumption with stroke. Hence, the conclusion of the authors that “alcohol increases the risk of stroke” is not supported by the data presented. In the opinion of members of the Forum, without reporting the effects according to the amount of alcohol consumed or the pattern of drinking, this is an unsupported and potentially dangerous statement to present in a scientific journal.
Reference: Rantakömi SH, Laukkanen JA, Sivenius J, Kauhanen J, Kurl S. Alcohol consumption and the risk of stroke among hypertensive and overweight men. J Neurol 2013;260:534–539. DOI 10.1007/s00415-012-6672-6
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 107: Little effect on child’s mental functioning associated with mother’s light, occasional drinking in early pregnancy – 25 March 2013
A new report from the prospective, population-based Avon Longitudinal Study of Parents and Children (ALSPAC) in the UK is based on investigation of the association between light drinking in pregnancy (<1 glass per week in the first trimester) and child mental health. Mental health was assessed in more than 6,000 children using both parent- and teacher-rated Strengths and Difficulties Questionnaires (SDQs) at age 11 years. Academic outcomes based on Key Stage 2 examination results were measured in more than 10,000 children.
Approximately 40% of women consumed some alcohol but less than 1 glass/week, while 16% reported consuming ≥1 glass per week during the first trimester. The authors report that after adjustment, relative to abstainers, there was no effect of light drinking on teacher-rated scores or examination results. In girls, although there was a suggestion of worse outcomes on the parent-rated total score in those exposed to light drinking compared to abstainers, no dose–response relationship was evident. The authors conclude: “Light drinking in pregnancy does not appear to be associated with clinically important adverse effects for mental health and academic outcomes at the age of 11 years.”
Forum reviewers considered this to be a well-done study, with a balanced assessment of results by the authors. Reviewers were surprised at the somewhat arbitrary separation of alcohol consumption: <1 drink per week versus ≥1 drink per week. Current guidance about alcohol consumption in pregnancy from the Department of Health in England (2009) allows for pregnant women to drink up to 1–2 units of alcohol once or twice a week, and it would have been preferable to have data presented for drinkers at this level.
Forum Co-Director Conibear considered that “The most important aspect of this study relates to the fact that 25% of babies in the UK are unplanned, and 17% of mothers do not know they are pregnant until eight weeks or more. Therefore balanced advice concerning the effect of alcohol use in early pregnancy is crucial to prevent unnecessary concern amongst this group of mothers to be. Although the best advice is to avoid alcohol if you are pregnant, the present research can reassure mothers who drank occasionally without realising that they were pregnant that they have not done long-term harm to their baby.”
Forum reviewer Stockley added: “I think that another important message is that if a woman decides to consume a small amount of alcohol during pregnancy, she should never binge drink or get drunk. This we know can have adverse effects on the developing fetus, especially in the first trimester, but interestingly, also in the third trimester of pregnancy.”
Reference: Sayal K, Draper ES, Fraser R, Barrow M, Davey Smith G, Gray R. Light drinking in pregnancy and mid-childhood mental health and learning outcomes. Arch Dis Child 2013;98:107–111. doi:10.1136/archdischild-2012-302436.
For the full critique of this publication by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 106: A clinical trial shows that glucose metabolism is improved more by red wine than by gin — 14 March 2013
To compare the effects of moderate consumption of red wine, dealcoholized red wine, and gin on glucose metabolism and the lipid profile, a group of Spanish investigators carried out a randomized control trial among 67 men at high cardiovascular risk. All received each of red wine (30 g alcohol/d), the equivalent amount of dealcoholized red wine, and gin (30 g alcohol/d) for 4 week periods, in a randomized order. While fasting glucose levels were not affected, mean adjusted plasma insulin and HOMA-IR decreased after red wine and dealcoholized red wine, but not after gin. HDL cholesterol, Apolipoprotein A-I and A-II increased after red wine and gin. Lipoprotein(a) decreased after the red wine intervention. The authors conclude that their results support a beneficial effect of the non-alcoholic fraction of red wine (mainly polyphenols) on insulin resistance, thus greater protective effects on cardiovascular disease from red wine than from other alcoholic beverages.
Forum members were unanimous in considering this to be a very well-done and important trial. It supports a huge amount of observational data from epidemiologic cohort studies that have shown that subjects who consume moderate amounts of alcohol tend to have much lower risk of developing diabetes. Further, patients with diabetes who drink moderately have much lower risk of subsequent cardiovascular disease and lower mortality. Studies such as this one help scientists understand the mechanisms by which moderate drinking, especially of wine, can reduce the risk of metabolic and vascular diseases.
Reference: Chiva-Blanch G, Urpi-Sarda M, Ros E, Valderas-Martinez P, Casas R, Arranz S, Guillén M, Lamuela-Raventós RM, Llorach R, Andres-Lacueva C, Estruch R. Effects of red wine polyphenols and alcohol on glucose metabolism and the lipid profile: A randomized clinical trial. Clinical Nutrition 2013. Pre-publication. dx.doi.org/10.1016/j.clnu.2012.08.022.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 105: For preventing cardiovascular disease, an unrestricted-calorie Mediterranean-type diet provides 30% more benefit than a low-fat diet: Results of a large population-based clinical trial — 6 March 2013
A large well-done clinical trial in Spain was carried out among 7,447 subjects at high-risk of cardiovascular disease (on the basis of diabetes, hypertension, dyslipidemia, and other risk factors). The trial compared the effects of two versions of an energy-unrestricted Mediterranean-type diet, one with large amounts of extra-virgin olive oil (EVOO) and one with a supplement of mixed nuts, with results among subjects in a “control group,” made up of subjects who were advised to follow a low-fat, low-cholesterol diet (that has typically been recommended for reducing the risk of cardiovascular disease).
Both of the groups advised to consume a Med-Diet showed an increase in total fat, from an average of 39.3 % of total calories to an average of more than 41%; the group advised to decrease their total fat lowered their intake from 39 to 37 % of calories. All three groups showed slight decreases in saturated fat and slight decreases in dietary cholesterol intake (but blood cholesterol levels were not reported). Only the Med-Diet + nuts group showed an increase in alpha-linolenic acid (ALA), the fatty acid related to the lowest risk of cardiovascular disease in the Cretan cohort of the Seven-Countries Study and in the Lyon Diet-Heart Study.
The large majority of subjects in all groups consumed wine at baseline, and about one-third of the Med-Diet groups and one-quarter of the control group reported consuming ≥ 7 glasses of wine/week during the trial. However, alcohol consumption was not evaluated specifically for its effects in the present study.
The study was ended early by its data and safety monitoring board due to marked advantages being shown in terms of the occurrence of the primary end-point (the occurrence of myocardial infarction, stroke, or death from cardiovascular causes) in both Med-Diet groups in comparison with the control group. The multivariable-adjusted hazard ratios were 0.70 and 0.72 for the Med-Diet with olive oil and the Med-Diet with added nuts, hence an approximately 30% decrease in risk among subjects assigned to a Med-Diet compared with those in the control group.
Forum members (as did the authors) had difficulty in determining which specific components of the Med-Diet may have been the primary reasons for its more favorable results, as significant dietary changes during the trial were mainly related to the supplementary olive oil or nuts given to subjects in the two Med-Diet groups. Among potential factors were increased mono-unsaturated fat and higher antioxidants from the added EVOO and an increase in ALA from the supplemental nuts. Forum members noted that the Med-Diet interventions apparently did not provide an increase in the intake of ALA, which could have led to even more protection against cardiovascular disease.
In any case, the striking reduction in risk shown in the study from the Med-Diet provide further evidence of the effectiveness of such a diet in reducing cardiovascular disease. It has been shown repeatedly that people advised to consume a Mediterranean-type diet tend to comply much better with such advice than do people advised mainly to decrease their intake of all fats and cholesterol. A very large amount of scientific data now support advice to follow a Mediterranean-type diet, one that does not restrict calories but encourages the intake of selected fats (which may include extra-virgin olive oil or canola oil), as well as more fruits, vegetables, grains, nuts, and wine; it may be the most effective dietary approach for reducing cardiovascular disease.
Reviewer Keil points out that many good prospective cohort studies have shown that an increase in adherence to components of a Mediterranean-type diet decreases the risk of many diseases and mortality. He adds: “The great thing about the present study is that when the skeptics raise their voice and argue that the proponents of the Mediterranean diet have only observational data available, we can now respond that we not only have RCT data on secondary prevention (Lyon Diet-Heart study) but also the present study on primary prevention of cardiovascular disease.”
Reference: Estruch R, Ros E, Salas-Salvadó J, Covas M-I, Corella D, Arós F, et al, for the PREDIMED Study Investigators. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 2013. DOI: 10.1056/NEJMoa1200303
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please clickhere.
===============================================================================
Critique 104: Moderate alcohol consumption is associated with a lower risk of diabetes — 26 February 2013
A population-based longitudinal study in Norway showed a lower risk of developing type II diabetes, and a tendency for less auto-immune diabetes, among subjects reporting moderate alcohol consumption. The lowest risk was among subjects reporting that they consumed alcohol 5-10 times during the previous two weeks or reporting a daily consumption of 10-15 grams of alcohol per day (slightly less than one to a little over one drink per day, using 12 g of alcohol per day as a “typical drink”).
The overall results from this study support most previous research showing a rather large (approximately 30% or more) reduction in the risk of Type II diabetes mellitus to be associated with moderate drinking. In this study, the strongest protective effect related to the consumption of wine, rather than beer or spirits. Unlike some previous research, the present study did not show an increased risk of diabetes among binge drinkers, heavier drinkers, those reporting episodes of intoxication, or those giving positive responses on a CAGE questionnaire (a measure of an alcohol use disorder). As it is likely that alcoholics were under-represented in the cohort, the ability to show the effects of very heavy drinking may have been limited.
While the numbers of subjects with auto-immune diabetes were small, there was a tendency seen for a similar reduction in risk with moderate drinking as with the much more common Type II diabetes. Overall, this study strongly supports much previous research showing that moderate alcohol consumption is associated with a lower risk of developing diabetes.
Reference: Rasouli B, Ahlbom A, Andersson T, Grill V, Midthjell K, Olsson L, Carlsson S. Alcohol consumption is associated with reduced risk of Type 2 diabetes and autoimmune diabetes in adults: results from the Nord-Trøndelag health study. Diabet Med 2013;30:56–64.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 103: Alcohol intake just prior to bed-time may affect your sleep patterns — 18 February 2013
A paper from experts in the science of sleep provides an excellent review of intervention studies since the 1980s on the effects of alcohol consumption on sleep. The study finds that the time required to fall asleep, and sleep patterns in the first part of the night, tend to be improved by alcohol. The authors conclude that “The onset of the first REM sleep period is significantly delayed at all doses and appears to be the most recognizable effect of alcohol on REM sleep, followed by the reduction in total night REM sleep.” Slow-wave sleep is more common and REM sleep less common after alcohol.
The studies reviewed in this report were intervention studies among mainly young normal subjects, not people with sleep disorders. Other studies have demonstrated that small amounts of alcohol given in the evening to the elderly may improve sleep, and reduce the need for sleep-inducing medications. Overall, the data reviewed in this paper suggest that small amounts of alcohol in the evening have few adverse effects on sleep, and relate to earlier onset of sleep and less awakening in the first part of the night. Larger amounts of alcohol tend to make the onset of sleep faster, but may have some adverse overall effects on sleep patterns, with a shorter duration of REM sleep throughout the night.
Reference: Ebrahim IO, Shapiro CM, Williams AJ, Fenwick PB. Alcohol and sleep I: Effects on normal sleep. Alcohol Clin Exp Res 2013;doi: 10.1111/acer.12006. [Epub ahead of print]
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Requested comments on paper by Nelson et al
by R. Curtis Ellison, MD, Professor of Medicine & Public Health,
Boston University School of Medicine
NOTE: These comments do not necessarily reflect the views of the members of the International Scientific Forum on Alcohol Research
Nelson DE, et al. Alcohol-attributable cancer deaths and years of potential life lost in the United States. Am J Pub Health, released February 14, 2013
We always welcome new scientific publications that help elucidate factors related to the development of cancer. The new paper by Nelson et al focuses on the role that alcohol consumption may play in the risk of a number of cancers.
Background: It has long been appreciated that there are a number of upper aero-digestive cancers, such as cancer of the mouth, throat, and esophagus, that occur much more frequently in heavy drinkers, especially alcoholics, than in abstainers. Physiologic studies suggest that these are not diseases of light to moderate drinkers, as a certain amount of alcohol is required to produce these diseases. Similarly, among people consuming enough alcohol to lead to liver cirrhosis, the risk of liver cancer is also markedly increased.
These “alcohol-related cancers” should be discussed separately from other more common cancers – especially colon cancer and female breast cancer – for which the risk may be only slightly increased by alcohol. In the case of breast cancer, there may be a slight increase in risk among some women consuming an average of only one drink/day (in some studies, such an increase in risk occurs primarily among women who binge drink, have an inadequate intake of folate, and/or are also on hormone replacement therapy.)
For these types of cancer, it is especially important to consider the net health effects of alcohol consumption. For example, it is estimated that if a woman at average risk of breast cancer (i.e., does not have such a cancer in a first-degree relative) decides to avoid drinking completely in hopes of reducing her risk of breast cancer, her risk of breast cancer would be expected to be slightly decreased, on average, by perhaps 5-10%; however, her risk would be increased of dying from much more common diseases such as heart attack, stroke, or other conditions for which small amounts of alcohol have been shown to reduce risk. And, importantly, her risk of dying of any cause (total mortality) would actually be increased by her avoiding light alcohol consumption.
The pattern of drinking has often been shown to be even more important than the average amount of alcohol consumed. A stronger association with beneficial effects is seen with the regular (up to daily) intake of small amounts of an alcoholic beverage; drinking larger amounts on fewer days (including binge drinking) is almost always associated with adverse health effects. For example, a man having up to 2 drinks each day would have an average of 14 drinks per week, generally considered to be within recommended guidelines. However, a man consuming 7 drinks on each of only two days each week, despite the same weekly average consumption, would not be considered to be a moderate drinker.
Comments on the present paper: There are a number of concerns about the analyses and conclusions of the authors of the present paper. These include the following:
(1) The authors have “corrected” the reported data on alcohol consumption to make up for presumed under-reporting, using a method not generally accepted by statisticians and other researchers. This means that even many “light” drinkers are listed as reporting greater amounts of alcohol.
(2) The authors do not clearly separate the effects of truly moderate drinking from heavier drinking in their conclusions. They use up to 20 grams of alcohol per day as their lowest drinking category; this is higher than the 14 g/day that is the current definition of responsible drinking for women in the US Guidelines. Further, as stated, if reported intakes are increased artificially, many more light drinkers would be bumped up into higher categories of drinking. The result of this mis-categorization is that bona fide moderate drinking, which has been shown by others to have no association with most types of cancer, is improperly associated in this study with increased cancer.
(3) The authors’ implications that even regular, moderate drinking increases the risk of many cancers is not consistent with most previous research. Further, by not having data on the pattern of drinking, the authors include binge drinkers in the same category as regular drinkers, further exaggerating the association of cancer with moderate drinking. Others have clearly shown that there are large differences in effect between these two patterns. (It is troubling also that in the paper, the estimated percentage of alcohol-attributable cancer risk among subjects reporting > 0 to 20 grams of alcohol per day is much higher than that of subjects reporting > 20 to 40 grams/day; while this partly relates to the large number of persons who drink only small amounts, such an association makes no sense biologically. It is difficult to understand who the subjects are in the lowest drinking group, but it may include a large percentage of ex-alcoholics or heavier drinkers underreporting their intake. However, this makes any conclusions in this paper regarding the risk of cancer among moderate drinkers highly suspect.)
(4) The authors do not point out the demonstrated effects of alcohol on total mortality; regular, light-to-moderate drinkers live longer. By focusing only on cancer risks, the authors fail to mention the effects on the risk of much more common conditions, such as coronary heart disease, stroke, dementia, other important health problems of ageing, and on total mortality. The study of the health benefits and problems of drinking is a very mature field — authors generally discuss their observations in the context of total mortality or other major diseases that would be affected by their experimental design. In nearly all cases, light drinking is shown to be beneficial; these studies are ignored here.
(5) Overall, a criticism of this paper relates to the failure of the authors to put their results into perspective. Statements such as “There is no safe threshold for alcohol and cancer risk” is more of a “scare” statement than a balanced discussion of their results. Given that almost all prospective studies show that regular moderate drinkers have better health as they age and live longer than lifetime abstainers, even papers focused on the effects of alcohol on any particular disease should present a balanced view on its net effects on health and disease.
(6) Finally, the authors of this paper have taken the results of their analyses (some of which are based on questionable assumptions) as “truth,” then expounding at length about the public health implications. There should always be a certain amount of doubt when presenting the results of an individual study, as no one analysis can possibly reveal everything about an association. (As stated by Voltaire: “Doubt is not a pleasant condition, but certainty is absurd!)
As the authors acknowledge, observational epidemiologic data can never reveal the full “truth” about the causation of disease from exposures, and each new study’s results must be interpreted taking into consideration previous research. However, the overall implications presented by the authors of this paper suggest that their goal may have been to support a presumed conclusion to discourage alcohol consumption, not to carefully interpret the available data to best advance the public health.
Key points of these comments
- There are a number of assumptions taken by the authors in their analyses that raise questions about their results. The authors present only “adjusted” data for reported alcohol intake (based on national sales, not on individual intake), making the relation of alcohol intake to the occurrence of cancer in individuals unclear.
- There is poor differentiation between regular moderate drinking and periodic heavy drinking (binge drinking) or alcoholism, although there are marked differences in health effects between these groups. Regular, moderate drinking is associated with net health benefits, whereas binge drinking and alcoholism have almost exclusively adverse effects (including increases in many types of cancer).
- There has been a huge amount of previous research in this field, but the authors do not put their own results into perspective or discuss the overall health effects of alcohol consumption. Previous data have clearly shown that regular moderate drinkers tend to have lower risk of cardiovascular disease, stroke, diabetes, and many other diseases, and have a lower overall risk of all-cause mortality.
Submitted by
- Curtis Ellison, MD, Professor of Medicine & Public Health; Director, Institute on Lifestyle & Health;l Boston University School of Medicine
Co-Director, International Scientific Forum on Alcohol Research
===============================================================================
Critique 102: Possible prevention of myocardial infarction from alcohol’s effects on periodontal disease: An hypothesis — 6 February 2013
A cross-sectional analysis among more than 5,000 Norwegian men was designed to determine if the frequency of alcohol consumption related to the risk of myocardial infarction associated with infectious periodontal disease. The authors hypothesized that because it is bactericidal, frequent alcohol consumption would decrease periodontal infection and lower the risk of tooth extraction related to periodontal infection. The authors state that their main finding was that frequent drinking lowers the risk of MI associated with periodontal disease.
Forum reviewers had real concern about the paper and the conclusions of the authors. Some stressed that the per cent of alcohol in most “drinks” is too low to be really bactericidal, that the key exposures (alcohol and oral infections) were based exclusively on self report and did not have information on type of beverage or pattern of drinking, that many confounders (especially related to socio-economic status) were not adequately taken into consideration, and that the authors did not really test the results of their study with appropriate statistical testing.
Current scientific data show an increase in the risk of cardiovascular disease to be associated with periodontitis. Further, data consistently show a decrease in the risk of cardiovascular disease from moderate drinking, and a very large number of mechanisms have been identified. However, the present study does not confirm that alcohol consumption plays an important role in preventing heart disease through its effect on periodontitis.
Reference: Håheim LL, Olsen I, Rønningen KS. Oral infection, regular alcohol drinking pattern, and myocardial infarction. Medical Hypotheses 2012;79:725–730.
For the full critique of this article by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 101: A review of the association of alcohol consumption with the risk of developing hypertension — 22 January 2013
A meta-analysis from investigators at Columbia University in New York evaluated the risk of developing hypertension according to the level of alcohol consumption previously recorded. The analyses were based on data from 16 prospective studies. The paper’s main results are that among men, there is little effect of alcohol consumption up to 30 grams of alcohol per day (the equivalent of about 2 ½ “typical drinks” by US standards or more than 3 drinks by UK standards), but evidence of an increased risk of hypertension for the intake of greater amounts of alcohol. For women, light drinking appears to be associated with a slightly lower risk of hypertension, but more than 20 grams/day of alcohol may increase the risk.
While Forum members thought that the analyses were done well, they had some concerns about the conclusions of the authors, some of which appear to not be in line with the data they presented. For example, their statement that “heavier alcohol consumption >20 g⁄d is associated with the risk of development of hypertension in both women and men” is not consistent with their findings of a significant increased risk of hypertension only with an intake of 31 – 40 grams of alcohol per day.
Similarly, the authors conclude: “Even for light drinkers, vigilant blood pressure monitoring is necessary,” which may not be appropriate given that their data show that intake below 30 grams per day has no significant association with hypertension in men and may actually reduce the risk of hypertension in women.
Overall, the results of this study, in line with findings from most previous research, indicate that people who consume alcohol according to most current drinking guidelines (no more than 2 typical drinks/day for men or 1/day for women) do not show an increase in their risk of hypertension, but heavier drinking appears to increase the risk. Not discussed in this paper, but especially important in terms of health, is that light drinking is associated with a significant and rather large decrease in the risk of the most serious sequelae of hypertension: coronary heart disease and ischemic stroke.
Reference: Briasoulis A, Agarwal V, Messerli FH. Alcohol consumption and the risk of hypertension in men and women: A systematic review and meta-analysis. J Clin Hypertens 2012;14:792-798.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 100: The effects of moderate drinking on cognitive function and dementia: An update — 15 January 2013
A paper from a group of Italian scientists provides an extensive review of the available research relating alcohol consumption to cognitive function. It presents brief summaries of results from most key epidemiologic studies dealing with this topic between 1987 and 2011. The large majority of these studies, and recent meta-analyses, support a finding of a lower risk of cognitive impairment from ageing and of dementia to be associated with moderate drinking.
Reviewers praised the authors for pointing out difficulties caused by having to develop guidelines for alcohol consumption based only on observational data, and not having large clinical trials for judging effect. A further problem faced in judging the numerous studies on this topic is that many lack data on beverage type and most lack detailed information on the pattern of drinking, which may be especially important in judging the effects of drinking.
Some reviewers stated that the paper does not present anything new, as previous meta-analyses have clearly shown a potentially protective effect of moderate alcohol consumption on the risk of cognitive decline and dementia. Given that recent large meta-analyses have shown that moderate drinking, is comparison with abstention, is usually associated with 20-35% lower risk of cognitive decline and dementia, Forum reviewers thought that the conclusions of the authors of this review paper were unnecessarily cautious. Overall, current scientific data support a conclusion that moderate consumption of alcoholic beverages, especially of wine, is neuroprotective.
Reference: Panza F, Frisardi V, Seripa D, Logroscino G, Santamato A, Imbimbo BP, Scafato E, Pilotto A, Solfrizzi V. Alcohol consumption in mild cognitive impairment and dementia: harmful or neuroprotective? Int J Geriatr Psychiatry 2012;27:1218-1238.
For the full review of this critique by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 099: Alcohol and survival after postmenopausal diagnosis of breast cancer — 20 December 2012
This paper assessed the association of pre-diagnostic alcohol consumption with disease recurrence and survival in a prospective cohort study in Germany based on 2,522 postmenopausal breast cancer patients, aged 50–74 years. The authors report that alcohol consumption was non-linearly associated with increased breast cancer-specific mortality, but not with breast cancer recurrence. Results were independent of estrogen receptor status. The authors also report a non-significantly decreased risk of mortality due to other causes.
Forum reviewers considered this to be a well-done analysis that was limited, however, by the lack of data on drinking patterns prior to breast cancer diagnosis and because no data were available on drinking after the diagnosis (the latter limits the applicability of its results to women who have already developed breast cancer). The comparisons were primarily between non-drinkers/light drinkers and women in the highest alcohol category; the authors state that when ex-drinkers were removed from the referent category, their results regarding breast cancer-specific mortality were no longer statistically significant. The authors do not describe the potential effects on their main results that could result from what is known as “index event bias,” which may occur when an exposure (e.g., alcohol) relates to the development of a disease, breast cancer in this study, and may also relate to sequelae (e.g., recurrence or death) from the same disease.
Forum reviewers conclude that current scientific data show that alcohol consumption may increase the risk of developing breast cancer. However, they believe that the effects on subsequent survival after such a diagnosis remain unclear.
Reference: Vrieling A, Buck K, Heinz J, Obi N, Benner A, Flesch-Janys D, Chang-Claude J. Pre-diagnostic alcohol consumption and postmenopausal breast cancer survival: a prospective patient cohort study. Breast Cancer Res Treat 2012;136:195–207. DOI 10.1007/s10549-012-2230-2
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 098: Moderate alcohol consumption may lower the risk of developing depression — 13 December 2012
Analyses from a prospective study of more than 13,000 adults in Spain related baseline alcohol intake (mainly wine) with the development of depression, with the outcome based on a physician’s diagnosis or on the habitual use of anti-depressant drugs for four or more years. Reported depression was much higher among women than men. Among women, the estimated hazard ratios for groups reporting an average alcohol intake of < 5 g/day of alcohol, 5-15 g/day, and > 15 g/day were 0.97, 0.62, and 0.84 (in comparison with subjects reporting no alcohol). The difference was statistically significant (CI = 0.43-0.89) for the group reporting 5-15 g/day.
Few men reported a diagnosis of depression; among moderately drinking men, the estimated risks of depression were similar to those of women, but none of the differences were statistically different from those of non-drinkers. The investigators found no differences according to the type of alcoholic beverage consumed.
The merits of this study include that the data were collected prospectively, that there were repeated questionnaires seeking data on depression, and that there were a large number of subjects, all of whom were college graduates. There were few men reporting depression, and few heavy drinkers, so results apply only to moderately drinking women. Among these women (those consuming between about ½ drink/day to about 1 or 1 ½ drinks per day) there was evidence of a lower risk of depression during a follow-up period extending up to 10 years.
Forum reviewers thought that this was a well-done analysis, and the use of cut-points for drinking groups according to spline analyses was appropriate. Some reviewers cautioned that moderate drinkers, especially regular wine drinkers, tend to have a large number of other healthy lifestyle habits that could relate to the risk of depression. While many of the recognized potential confounders were included in the Cox regression analysis in this paper, it will be important to determine if future studies support the conclusions of the authors.
Reference: Gea A, Martinez-Gonzalez MA, Toledo E, Sanchez-Villegas A, Bes-Rastrollo M, Nuñez-Cordoba JM, Sayon-Orea C, Beunza JJ. A longitudinal assessment of alcohol intake and incident depression: the SUN Project. BMC Public Health 2012, 12:954 doi:10.1186/1471-2458-12-954
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 097: Per-capita alcohol intake and all-cause mortality in Australia — 4 December 2012
An ecologic analysis from a group in Australia has related trends in the per-capita consumption of alcohol in Australia with rates of all-cause mortality. Unfortunately, the authors do not have data on individual consumption of alcohol (and no way of knowing if the people who drink or do not drink are those who die) and do not have data on many key factors that relate to both alcohol consumption and mortality (e.g., education, income, diet, occupation, etc.). Especially, they have no data on the patterns of consumption of members of the population (regular moderate intake or binge drinking). They “adjust” for death rates in women but do not report sex-specific mortality rates.
This paper illustrates many of the dangers of the so-called “ecologic fallacy,” in which comparisons are made between aggregate population data and biologic outcomes. It has been shown that such comparisons may be of interest in generating hypotheses, but not for answering questions of causation, for which different types of studies are required. As stated in a leading textbook of epidemiology: “Ecologic analysis poses major problems of interpretation when making ecologic inferences and especially when making biologic inferences. In contemporary epidemiology, the ‘ecologic fallacy’ reflects the failure of the investigator to recognize the need for biologic inference and thus for individual-level data. This need arises even when the primary exposure of interest is an ecologic measure and the outcome of interest is the health status of entire populations.”
With such serious limitations from the use of ecologic comparisons, this paper does not provide data upon which alcohol policy can be based. The authors of this paper appear to have ignored previous research providing very different interpretations of an inverse association between per-capita alcohol intake and mortality. A plethora of studies based on alcohol intake among individuals, and especially patterns of consumption, provide data needed for such policy decisions.
Reference: Livingston M, Wilkinson C. Per-capita alcohol consumption and all-cause male mortality in Australia, 1911–2006. Alcohol and Alcoholism 2012. Pre-publication: doi: 10.1093/alcalc/ags123
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 096: Frequency of alcohol consumption and cardiovascular risk factors: implications for drinking guidelines — 20 November 2012
As stated by the authors, “many observational studies suggest that increased drinking frequency is associated with reduced mortality among those with low-dose alcohol consumption. The purpose of this paper was to examine whether frequent drinkers consume lower-risk amounts during drinking days or have favorable risk factor profiles compared with those who drink less frequently, and discuss implications for the larger debate about the limitations of non-randomized studies about ‘moderate’ drinking and the development of low-risk drinking guidelines.” Indeed, previous epidemiologic research has clearly shown that the healthiest outcomes occur among regular, moderate drinkers who do not binge drink. Further, almost all studies have adjusted for a large number of socio-economic factors that are known to be potentially confounding factors for evaluating the association of alcohol consumption with health outcomes.
As expected, the present study shows that regular drinkers tend to consume less alcohol per occasion, and are less likely to binge drink. Further, such individuals tend to have better socio-economic status and lower levels of most cardiovascular risk factors. Most previous researchers have interpreted the better educational status and economic levels of moderate drinkers to be important causes of their more moderate lifestyle factors (including avoiding abusive drinking). Further, most previous research, including many basic science interventions and limited trials in humans, have shown that the administration (intake) of moderate amounts of an alcoholic beverage leads to more favorable cardiovascular risk factors, and numerous mechanisms have been identified (higher HDL-cholesterol, improved vascular reactivity, improved platelet and other coagulation factors, etc.).
The authors of this paper take an unusual turn when it comes to discussing the implications of their results. They tend to down-play any potential health benefits that may be caused by alcohol or the pattern of drinking and infer instead that the favorable risk factors themselves may lead to the drinking pattern. Forum members disagreed with the implications of the authors on a number of factors: (1) the lack of randomized trials of low-dose alcohol consumption; (2) levels of evidence; (3) drinking frequency and alcohol intake; (4) clustering of lifestyle behaviors; (5) alcohol consumption and CVD-related biomarkers; (6) alcohol intake, cancer and total mortality. Further, Forum reviewers cite a large body of scientific research that refutes some of the conclusions of the authors, e.g., that regular moderate alcohol intake does not relate to improved cardiovascular risk factors.
Forum reviewers agree with a concluding statement of the authors about using caution before recommending drinking to the general public. However, they believe that the arguments presented in this paper are not based on a balanced appraisal of available scientific data, and should not be used to support changes in guidelines for the public.
Reference: Naimi TS, Xuan Z, Brown DW, Saitz R. Confounding and studies of ‘moderate’ alcohol consumption: the case of drinking frequency and implications for low-risk drinking guidelines. Addiction 2012; pre-publication. doi:10.1111/j.1360-0443.2012.04074.x.
For the complete critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
A Tribute to Francesco Orlandi
(1927 – 2012)
It is with sadness that we have learned of the death on 12 November 2012 in Ancona, Italy, of Francesco Orlandi, MD. Francesco was a founding member of our International Scientific Forum on Alcohol Research, and a frequent and valuable contributor to our critiques. He will be sorely missed, both as a friend and as a respected scientist. Besides his strong passion for science, he was an extraordinarily cultivated man, rich in his sense of humor, and a sincere friend of many members of our Forum.
Francesco Orlandi was Professor of Gastroenterology at the University of Ancona from 1975 to 1999 and Direttore, Dottorato di ricerca Alimenti e Salute, 1997-99. He also served as Professor on wine and health at the Corso di Laurea Specialistica in Scienze Viticole ed Enologiche at the University of Turin.
Francesco was counselor and coordinator of the “wine and health” group of the Accademia Italiana della Vite e del Vino, and an OIV expert at the Italian Ministry of Agricultural, Food and Forestry Policies in Rome. In addition, he served as Visiting Professor in the Department of Medicine, Albert Einstein College of Medicine, New York, in 1977-8.
Francesco was always interested in the study of the health risks and benefits of alcohol consumption. In the 1990’s, he performed a number of experimental studies in rats on the mechanisms of early ethanol-induced liver damage, with particular attention to apoptosis and cell proliferation.
More recently Francesco became increasingly interested in the beneficial effects of moderate alcohol consumption on human health. He became convinced that only by working in a multi-disciplinary context could young investigators contribute to a new renaissance of alcohol and wine research in Italy. This is why in June, 2011, he organized the first seminar on responsible drinking in the context of the Mediterranean Diet, which was held in the ancient Pontignano Abbey, near Siena. There he brought together all young Italian scientists involved in this field of research; the abstracts of this meeting have been published (Eur J Nutr 2011;50:489–498).
As stated by a Forum member, Francesco was much more than a great doctor and an outstanding scientist. He was an old style gentleman, able to use the right words in every social context. He was an extremely educated person, cultivating interests from art, music, and sailing to science with the emotional motivation, intellectual freedom, and motivated curiosity that usually only young talents can have. Francesco will remain forever a young enthusiastic scientist for all of us who had the fortunate chance of interacting with him.
These comments provided by members of the International Scientific Forum on Alcohol Research (www.bu.edu/alcohol-forum)
15 November 2012
===============================================================================
Critique 095: Effects of alcohol on lymphoma, leukemia, and other types of hematological cancers —- 13 November 2012
Many observational epidemiologic studies have found an inverse association between alcohol consumption and hematological cancers (such as lymphoma and leukemia). This study, based on the Million Women’s Study in the UK, is large enough to permit an evaluation of associations with various types of such cancers. Further, it takes into account newer coding systems for morphology so that diseases associated with the lymphatic system can be separated from those of the myeloid system.
The key findings are that alcohol consumption appears to lower the risk of several types of lymphoma and plasma cell neoplasms, but has little effect on the risk of myeloid tumors such as acute myeloid leukemia. Smoking is associated with an increase in risk for most such cancers.
Forum reviewers considered this to be a very well-done analysis, and the ability of the authors to separate the effects on lymphoid and myeloid cancers is important. Forum members emphasize the strong differences in effect of smoking (an increase) and alcohol consumption (a decrease) on the risk of these cancers. They support future research to discover the mechanisms by which moderate drinking may lower such risk.
Reference: Kroll ME, Murphy F, Pirie K, Reeves GK, Green J, Beral V, for the Million Women Study Collaborators. Alcohol drinking, tobacco smoking and subtypes of haematological malignancy in the UK Million Women Study. British Journal of Cancer 2012;107:879–887.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
A Tribute to Serge Renaud
(1927 – 2012)
It is with sorrow that we have learned of the death in France on 28 October 2012 of Professor Serge Renaud at 84 years of age. In addition to being a colleague and close friend of many of us, he was celebrated as a pioneer in scientific research on the prevention of cardiovascular and other diseases. His innovative mind opened up new fields of inquiry that have greatly broadened research into the role of wine, alcohol, fatty acids, and other nutrients in preserving health and preventing disease. For his many contributions to science, on July 14, 2005, Serge received France’s highest distinction, the Legion d’Honneur.
Over many decades, Professor Renaud was the scientist who initiated much of the work relating the consumption of wine and other types of alcohol to cardiovascular disease and other of the diseases associated with ageing. He was the scientist most associated with the role of red wine in protecting the French from coronary artery disease (the “French Paradox”), and a leading figure in studying how other dietary factors relate to health. His innovative concepts have sometimes taken many years to be appreciated by other scientists. He made a major contribution with his research demonstrating how alpha-linolenic acid, monounsaturated fats, and other components of the “Cretan-type Mediterranean Diet,” play key roles in promoting health.
Serge Renaud was born in Cartelègue, Haute Gironde, France, and after starting his medical training in France moved to Montreal, Canada, and later to Boston, Massachusetts, USA. He returned to France in 1973 and became director of the INSERM unit in Lyon, France, where much of his research was carried out.
In an excellent tribute to Renaud in the Lancet in 2000, Bruno Simini pointed out his major contributions investigating the association between wine, diet, and thrombosis. Simini quotes Serge as saying: “If I hadn’t lived with my grandparents and great-grandparents on a vineyard near Bordeaux, perhaps this idea wouldn’t have occurred to me. When you see people reach the age of 80 or 90 years, who have been drinking small amounts of wine every day, you don’t believe wine in low doses is harmful.”1
In 1991, Serge Renaud appeared on the popular US television program, “60 Minutes,” in a segment entitled the “French Paradox.” When asked by Morley Safer, the host, what was the real reason that the French have rates of coronary artery disease so much lower than those in other developed nations, Renaud replied: “I think it is the alcohol.” And when Morley Safer closed the segment holding a glass of red wine and saying, “The protection of the French from heart disease may rest in this inviting glass,” the response in the US was remarkable – nothing such as this had ever been stated in the country that earlier in the century had made any alcohol consumption illegal through nation-wide prohibition. Following the television program, sales of red wine rose immediately by 40 per cent!
In addition to his studies on wine and alcohol, Professor Renaud, noting the very low rates of heart disease among participants from Crete in the “Seven Countries Study,” initiated the Lyon Diet Heart Study in 1985 to determine the effects of a diet based on that of Crete on the course of disease among patients who already had coronary disease. There were very dramatic reductions in subsequent coronary problems and in total mortality among subjects given the “Cretan-type diet,” which contained increased levels of an omega-3 fatty acid (alpha-linolenic acid) to replace some of the fats from meat and dairy products.
As quoted in the Lancet tribute by Simini, Professor Renaud said the results of these studies on heart disease and cardiac arrhythmias made him “wonder about the origins of civilisations. It is intriguing that ancient Asian and Mediterranean civilisations used natural oils in cooking—colza and olive—with similar fatty acid compositions.” [Colza oil is closely related to the widely used rapeseed oil and canola oil.] And because of his belief in ancient wisdom when it comes to diet and health, Renaud ends his book Le régime santé2 with a warning: “Don’t look for a pill that replaces [the Cretan diet]. There is no such thing.”
People around the world have profited, and will continue to profit, from the lifelong scientific work of Serge Renaud. For those of us who knew and worked with him, we cherish our memories of Serge the person, and of Serge the consummate scientist. As stated so well by a Forum member, “We are all in debt to Serge for the lesson he gave to our scientific community: curiosity as the sole reason to investigate, diligence in observing the facts, unbiased stringency in interpreting results, and, definitely not least, the modesty that only a great man can have. We shall keep him in our memory as an example and a mentor of the meaning of being a scientist.”
References
- Simini B. Serge Renaud: From French Paradox to Cretan miracle. The Lancet 2000;335:48. doi:10.1016/S0140-6736(05)71990-5.
- Renaud S. Le régime santé. Odile Jacob, Paris, 1998.
These comments provided by members of the International Scientific Forum on Alcohol Research (www.bu.edu/alcohol-forum)
31 October 2012
===============================================================================
Critique 094: The complex association between moderate alcohol consumption and breast cancer — 23 October 2012
An excellent review article from two scientists at the National Institue on Alcohol Abuse and Alcoholism describes the epidemiologic and basic scientific evidence linking alcohol consumption to the risk of breast cancer. The authors point out deficiencies in the epidemiologic data, especially that the pattern of drinking (regular moderate versus binge drinking) has generally not been taken into consideration (and the latter pattern can be associated with much higher blood alcohol concentrations). Further, epidemiologic studies usually provide data for only a short period of time, while the development of cancer may relate to exposures over many decades. The authors also comment upon the effect that under-reporting of alcohol by study participants could exaggerate effects on cancer risk from light drinking. They discuss two hypotheses that could relate alcohol to breast cancer risk: alcohol as a breast tumor promoter, and alcohol as a weak cumulative breast carcinogen, and present evidence from epidemiology and basic science that would relate to each hypothesis.
Overall, Forum reviewers were enthusiastic about this review paper, considering that it clearly outlined some of the difficulties scientists have in determining the causes of cancer. They agreed with the authors’ statements regarding the necessity to consider the overall net effects of moderate drinking, including reductions in the risk of cardiovascular disease and total mortality. They also agreed that future epidemiologic studies should focus on the pattern of drinking (and not just the average weekly amount of alcohol), and with their suggestions for future animal studies. One Forum reviewer cautioned that our understanding of the causes of breast cancer is still very incomplete, limiting our ability to provide well-founded recommendations to the public regarding moderate drinking as it relates to breast cancer risk.
Reference: Brooks PJ, Zakhari S. Moderate alcohol consumption and breast cancer in women: From epidemiology to mechanisms and interventions. Alcohol Clin Exp Res 2012; pre-publication: DOI: 10.1111/j.1530-0277.2012.01888.x.
For the full critique of this article by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 093: Is moderate alcohol consumption associated with an increased risk of atrial fibrillation among patients with cardiovascular disease? — 8 October 2012
An analysis of the association of alcohol consumption with the development of atrial fibrillation (AF) among subjects with coronary heart disease, stroke, diabetes, or other manifestations of cardiovascular disease (CVD) was based on subjects in two large antihypertensive drug treatment trials. Previous research in the general population has suggested an increase in the risk of the development of AF for heavy drinkers, and the present study shows such an association among subjects who already have CVD.
Among subjects in this study (all of whom had previous CVD), the authors also report that even “moderate” drinkers had a higher risk of AF than low-alcohol consumers, although the risk of death during follow up of moderate drinkers (9.9%) was lower than that of subjects reporting low-levels of drinking(12.5%). Excluding binge drinkers, the estimated risk of AF was about 13% higher in moderate drinkers than among subjects classified as low-alcohol consumers.
While the multiple analyses in this paper were done appropriately, Forum reviewers were concerned about two aspects of this study. First, there was concern about the wide range the authors chose for the category of “moderate” drinkers, which included subjects reporting from 1 drink per week up through those reporting 21 drinks per week for men and 14 drinks per week for women. It would have been useful to present results also for subjects who met more common definitions for moderate drinking: no more than 14 drinks/week for men and 7 drinks/week for women, the values used to define moderate drinking in the United States, Australia, and many other countries. Unfortunately, there is a conspicuous absence of data in this paper of the effects on the risk of AF of subjects consuming alcohol “moderately” by these standards.
Another major concern about these analyses relates to potential bias in the estimates from what is known as index event bias or collider bias. Given that alcohol intake prior to enrollment in this study may well have related to subjects’ development of cardiovascular disease, it is problematic to judge the effects of alcohol after a cardiovascular event on the subsequent risk of AF, a condition frequently associated with CVD.
All subjects in these analyses had already developed CVD (the prerequisite for being in the present study). Thus, the study included those who consumed alcohol prior to the diagnosis of CVD or diabetes and those who did not drink prior to these diagnoses. Given that moderate alcohol consumption has been shown to reduce substantially the risk of both CVD and diabetes, it can be assumed that subjects in this study who developed CVD despite being drinkers had other risk factors contributing to the disease that overcame any “protection” afforded by alcohol consumption. Unless adjusted for, these other risk factors could well affect the subsequent course of subjects following the onset of CVD, including the development of AF. A similar phenomenon has been seen for obesity (the “obesity paradox”), aspirin use (the “aspirin paradox”), and other exposures, where the associations with CVD seen prior to the initial development of the disease differ from those seen after the development of CVD.
It is clear from many previous studies in the general population that heavy alcohol intake and binge drinking increase the risk of developing atrial fibrillation. This cardiac arrhythmia is a common component of the “holiday heart” syndrome that may occur after very heavy bouts of drinking. As for the effects on the risk of atrial fibrillation from moderate drinking, as studied in this paper, there were a number of concerns from Forum reviewers about the analyses and results. They raise questions about the conclusions of the authors that even “moderate” drinking results in an increased risk of atrial fibrillation after the development of cardiovascular disease. Especially when defined as no more than 14 drinks per week for men or 7 drinks per week for women, the association between “moderate” alcohol consumption and atrial fibrillation remains unclear.
Reference: Liang Y, Mente A, Yusuf S, Gao P, Sleight P, Zhu J, Fagard R, Lonn E, Teo KK; for the ONTARGET and TRANSCEND Investigators. Alcohol consumption and the risk of incident atrial fibrillation among people with cardiovascular disease. CMAJ 2012. DOI:10.1503/cmaj.120412.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 092: The association of alcohol and tobacco with age at diagnosis among subjects with pancreatic cancer — 2 October 2012
This analysis from a group of distinguished scientists supports previous research showing that smoking is associated with an earlier onset of pancreatic adenocarcinoma. Other research has shown that smoking may also be a causative factor in the development of this type of cancer. For alcohol, this study shows that heavy drinking also appears to be associated with earlier diagnosis; previous research from some epidemiologic studies has suggested further that heavy intake of alcohol may be associated with the development of pancreatic cancer.
Forum reviewers were concerned, however, about potential bias in regards to the time of diagnosis of such cancer, and about many other limitations of the study. For example, the inability to separate drinkers by the pattern of drinking (binge drinking versus regular, moderate intake), by the socioeconomic status of subjects, and by a lack of information on chronic pancreatitis, a known risk factor, weaken the implications of this paper. Forum members do not think that the results of this study will have a large impact on clinical practice, or on measures for the prevention of pancreatic cancer.
Reference: Anderson MA; Zolotarevsky E; Cooper KL; Sherman S; Shats O; Whitcomb DC; Lynch HT; et al. Alcohol and tobacco lower the age of presentation in sporadic pancreatic cancer in a dose-dependent manner: A multicenter study. Am J Gastroenterol 2012; advance online publication, doi: 10.1038/ajg.2012.288
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 091: Light drinking may relate to increase in risk for certain cancers — 18 September 2012
A meta-analysis by a distinguished group of scientists was designed to determine if “light drinking” (defined as an average of up to 1 drink per day) was associated with the risk of certain cancers that have been shown in previous studies to be associated with the risk of cancer. The authors concluded that while the risk of these cancers was only slightly increased from such drinking, there were detectable increases in cancers of the oral cavity and pharynx, esophagus and female breast. They report no increase in the risk of cancers of the colorectum, liver, and larynx to be associated with such drinking.
Forum reviewers were concerned about a number of aspects of this study. While the statistical methodology was correct and done appropriately, the fact that the investigators (1) included both ex-drinkers and never drinkers in the reference group; (2) could not separate the effects of regular light drinking from binge drinking; (3) had no data on the duration of alcohol consumption at different levels; (4) did not adjust their analyses according to geographic region or type of study (both of which had large estimated effects on cancer risk); and (5) did not adjust their estimates of effect by other lifestyle habits, including smoking. All of these factors tend to weaken the implications of their results.
Forum reviewers were also concerned that despite the acknowledged limitations of their data, the authors present conclusions indicating that even light drinking increases the risk of certain cancers without commenting on the net health effects. They present only the effects on cancer (which was the topic of the meta-analysis) but do not comment on the overall or net health effects of light drinking: a marked reduction in the risk of much more common diseases, especially cardiovascular diseases, and a longer lifespan. Further, the lack of data on genetic patterns, folate intake, and other lifestyle factors makes it difficult to apply their findings to individual subjects. The Forum considers that while their analyses may be helpful in understanding associations between alcohol and cancer, the many limitations of this study indicate that it can provide only incomplete information on light alcohol consumption to be used as a basis for making recommendations to the public.
Reference: Bagnardi V, Rota M, Botteri E, Tramacere I, Islami F, Fedirko V, Scotti L, Jenab M, Turati F, Pasquali E, Pelucchi C, Bellocco R, Negri E, Corrao G, Rehm J, Boffetta P, La Vecchia C. Light alcohol drinking and cancer: a meta-analysis. Pre-publication: Annals of Oncology 2012; doi:10.1093/annonc/mds337
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 090: Effects of stopping alcohol consumption on subsequent risk of esophageal cancer — 13 September 2012
This paper provides an evaluation of the time following cessation of alcohol consumption that the risk of esophageal cancer returns to that of non-drinkers; it is based on 17 studies providing such information, 9 of which provided data for a meta-analysis. The authors conclude that an alcohol-related increased risk of esophageal cancer is reversible following drinking cessation, most likely requiring up to 16 years. The authors estimate that about one-half of the reduction in risk of cancer may occur within in a much shorter time, perhaps within about 4 or 5 years.
Forum reviewers considered this to be a well-done analysis. Forum members emphasized, as did the authors, a number of limitations of the study. Adjustments for smoking may not have been adequate: most upper aero-digestive cancers show a strong interaction between smoking and alcohol consumption in relation to cancer risk. (For many “alcohol-related” cancers, there is little effect of alcohol consumption among non-smokers.)
Further, large differences in the alcohol-cancer association were shown in this study for different geographical regions (some associations being much higher in Asia than in Europe or North America), but such differences were not adjusted for in the main analyses. The fact that the authors of this paper did not have data permitting the separation of ex-drinkers and never drinkers (both groups being included in the “non-drinker” category), and their inability to judge the effects of the baseline pattern of drinking (regular versus binge drinking), may also be limitations to the interpretation of their results. Adjustment for such factors may have influenced the effects of stopping drinking on subsequent cancer risk, and markedly changed the calculated effects on the numbers of cancers prevented worldwide.
In any case, the fact that cessation of drinking may reduce the risk of esophageal cancer is of importance. Other studies suggest further that just reducing the amount of alcohol consumed, rather than the complete cessation of drinking, may be associated with lowering of cancer risk, and low-level alcohol intake has been shown to have beneficial health effects on cardiovascular disease, diabetes, and other medical conditions.
Reference: Jarl J, Gerdtham Ulf-G. Time pattern of reduction in risk of oesophageal cancer following alcohol cessation — a meta-analysis. Addiction, 107, 1234–1243. doi:10.1111/j.1360-0443.2011.03772.x
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 089: Combination of hormone treatments and alcohol consumption influences the risk of breast cancer in women — 29 August 2012
An analysis among more than 40,000 postmenopausal women who were in the California Teachers Study was carried out to determine if there were differences in risk of breast cancer among women consuming alcohol according to their previous or current use of hormone therapy (HT). In the cohort, 660 women were diagnosed with invasive breast cancer during follow up.
Results from multivariate Cox proportional hazards regression models showed an increase in risk of breast cancer among alcohol consumers of more than 20 grams of alcohol per day (about 1 ½ to 2 typical drinks) who were current users of HT but not among those who were ex-users of HT. The authors conclude: “Following the cessation of HT use, alcohol consumption is not significantly associated with breast cancer risk, although a non-significant increased risk was observed among women who never used HT. Our findings confirm that concurrent exposure to HT and alcohol has a substantial adverse impact on breast cancer risk. However, after HT cessation, this risk is reduced.”
Forum reviewers considered this to be a very well-done analysis on a large group of post-menopausal women with repeated assessments of alcohol consumption and HT use. However, results from even very large studies on the relation between alcohol, HT, and breast cancer risk have often been conflicting. Even with numerous studies on this topic, we still have very poor predictors of which women will develop breast cancer. There is some increase in risk for women with a family history of such cancers and those who are obese. However, the percentage increases in risk associated with HT, alcohol consumption, and other environmental factors are generally small (unlike the many-fold increase in the risk of lung cancer among smokers in comparison with never smokers). This may explain why the results of individual studies may reach apparently conflicting conclusions. While the present study suggests that women who consume alcohol may have a decrease in their risk of breast cancer if they stop taking hormone replacement therapy, our current understanding of factors affecting breast cancer risk remains quite inadequate.
Reference: Horn-Ross PL, Canchola AJ, Bernstein L, Clarke CA, Lacey JV, Neuhausen SL, Reynolds P, Ursin G. Alcohol consumption and breast cancer risk among postmenopausal women following the cessation of hormone therapy use: the California Teachers Study. Cancer Epidemiol Biomarkers Prev 2012. [Epub ahead of print]
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 088: Higher levels of alcohol intake may slightly increase risk of age-related macular degeneration, with no effect from moderate drinking 22 August 2012
An analysis based on the follow up of more than 20,000 participants recruited in 1990-1994 for the Melbourne Collaborative Cohort Study in Australia related alcohol consumption at baseline to the subsequent development of age-related macular degeneration (AMD), a common cause of blindness in the elderly. At a follow-up examination between 2003 and 2007, digital macula photographs of both eyes were taken and evaluated for early and late AMD signs; there were 2,663 cases of early AMD and 121 cases of late AMD identified.
The authors report: “Drinking more than 20 g of alcohol per day was associated with an approximate 20% increase in the odds of early AMD (odds ratio = 1.21, 95% confidence interval: 1.06, 1.38; P = 0.004) when compared with those who reported no alcohol intake at baseline.” (An average of 20 grams/day of alcohol is the equivalent of about 2 daily drinks by British standards or 1 ½ drinks by US standards.) The analyses show that the increased risk was almost exclusively among smokers, with no significant effect among non-smokers who consumed any amount of alcohol.
Forum reviewers had some concern that approximately one-half of this “population-based” study did not have measurements for AMD; these included those who had died during the follow-up period (and deaths were more common among non-drinkers than among drinkers). Further, the authors focus only on the slight increase in risk of AMD seen for heavier drinkers, but do not emphasize that among never smokers there was no increase in risk for consumers of any amount of alcohol. Their results suggest a possible interaction between smoking and alcohol consumption in the etiology of this disease.
The findings of no effect (either positive or negative) from drinking < 20 g/day of alcohol in this study does not support some earlier reports of reduced risk of AMD among moderate wine drinkers. In the present study, there were no detectable differences in effect between the consumption of wine or of beer. A key point of this study may be that never-smokers do not show increased risk of AMD with alcohol consumption.
Reference: Adams MKM, Chong EW, Williamson E, Aung KZ, Makeyeva GA, Giles GG, English DR, Hopper J, Guymer RH, Baird PN, Robman LD, Simpson JA. 20/20—Alcohol and age-related macular degeneration: The Melbourne Collaborative Cohort Study. Am J Epidemiol 2012;176:289-298.
For the full critique of this article by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 087: Smoking increases, while alcohol consumption may decrease, the risk of amyotrophic lateral sclerosis (ALS) — 8 August 2012
Reference: de Jong SW, Huisman MHB, Sutedja NA, van der Kooi, AJ, de Visser M, Schelhaas HJ, Fischer K, Veldink JH, van den Berg LH. Smoking, alcohol consumption, and the risk of amyotrophic lateral sclerosis:A population-based study. Am J Epidemiol 2012;176:233–239
A population-based case-control study of the rare but devastating neurological disease amyotrophic lateral sclerosis (ALS) has shown that the risk of such disease is increased among smokers, as has been shown previously. However, surprisingly, the risk of ALS was found to be markedly lower among consumers of alcohol than among abstainers.
Forum reviewers thought that this was a well-done and important paper, as it is a population-based analysis, with almost 500 cases of ALS, a very large number of cases for this rare disease. They were especially struck by the magnitude of the difference in risk of ALS between alcohol consumers and never drinkers: the risk among drinkers was about one half that of non-drinkers. Said one reviewer: “The results in this study are astonishing in this mysterious disease. One should expect that alcohol, as a toxic agent, rather should contribute to the development of ALS than to prevent it. The lower risk among drinkers compared with non-drinkers is remarkable”
Forum reviewers cautioned that the results of this paper should not be used to prompt people to consume alcohol just to prevent ALS, as it is such a rare disease. However, this paper presents important data that could help scientists understand the etiology of ALS and perhaps other more common diseases.
For the full critique of this paper by members of the International Scientientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 086: Mechanisms for a beneficial effect of moderate alcohol consumption on osteoporosis in women — 1 August 2012
Women after menopause tend to develop weaker bones from what is known as osteoporosis, which may lead to fractures (especially hip fractures) from falling. The weakness of the bones results from an imbalance between the normal resorption (a type of dissolving of old bone) and the laying down of new bone, an ongoing process for both men and women referred to as “bone turnover.” For poorly understood reasons, after menopause the resorption of old bone in women continues but new bone is laid down less well, leading to a decrease in the density of bone. A variety of substances (calcium, vitamin D, various medications) have been used in an attempt to prevent the development of osteoporosis; in epidemiologic studies, moderate drinking of alcohol has been shown to lower this risk.
An intervention trial evaluating the association of alcohol intake with indices of bone metabolism shows beneficial effects of moderate alcohol intake on factors that relate to osteoporosis in post-menopausal women. The authors state that excessive bone turnover, combined with an imbalance whereby bone resorption exceeds bone formation, is the principal cause of post-menopausal bone loss. This study among 40 healthy post-menopausal women investigated the hypothesis that moderate alcohol intake (an average of 19 grams per day, or approximately 1 and ½ typical drinks per day in this study) attenuates bone turnover after menopause. Measurements were carried out while the women were consuming alcohol, after they had stopped drinking as part of the trial, and following resumption of alcohol. The study showed that abstinence from alcohol resulted in increased markers of bone turnover (hence, higher risk of developing osteoporosis), whereas resumption of alcohol reduced bone turnover markers.
Forum reviewers considered this to be an innovative and well-done study. The key questions raised were how alcohol may affect bone metabolism in a longer period of time than was tested in this study. Reviewers realized that such long-term intervention trials are very difficult and expensive to carry out. On the other hand, many prospective epidemiologic studies in the elderly have shown greater bone mineral density and a lower risk of fractures among regular moderate drinkers than among abstainers. The most important aspect of this study may be that it has helped identify cellular mechanisms for the increased bone density observed in post-menopausal women who are moderate alcohol consumers.
Reference: Marrone JA, Maddalozzo GF, Branscum AJ, Hardin K, Cialdella-Kam L, Philbrick KA, Breggia AC, Rosen CJ, Turner RT, Iwaniec UT. Moderate alcohol intake lowers biochemical markers of bone turnover in postmenopausal women. Menopause 2012;19: DOI: 10.1097/gme.0b013e31824ac071
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research and other invited scientists, please click here.
(Note: an ADDENDUM to the original Forum critique has been added on 15 August 2012.)
===============================================================================
Critique 085: Moderate alcohol intake is associated with a lower risk of kidney cancer — 19 July 2012
A majority of previous epidemiologic studies have shown that moderate drinking is associated with a lower risk of kidney cancer, which may affect about 1% of the general population. In published prospective cohort studies, the risk for such cancer among moderate drinkers is usually about 25% less than the risk seen among non-drinkers.
This well-done meta-analysis supports these findings: for the more-reliable prospective cohort studies (rather than case-control studies) the current study finds a 29% lower risk for subjects in the highest category of alcohol consumption in comparison with subjects in the lowest alcohol category. The findings suggest similar effects among men and women, and for all types of alcohol beverages. The effects are seen at a level of about one drink/day, with little further reduction in risk for greater alcohol consumption.
Reference: Song DY, Song S, Song Y, Lee JE. Alcohol intake and renal cell cancer risk: a meta-analysis. British Journal of Cancer 2012;106:1881–1890.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 084: Moderate drinking lowers risk of developing rheumatoid arthritis in women — 17 July 2012
A follow-up study of more than 34,000 women in Sweden has shown that moderate drinkers, in comparison with abstainers, were at significantly lower risk of developing rheumatoid arthritis (RA), an often serious and disabling type of arthritis. RA is known to relate to inflammation, and it is postulated that this is blocked to some degree by the consumption of alcohol. In this study, women who consumed at least 4 drinks per week (with a drink being defined as containing 15 grams of alcohol) had 37% lower risk of developing RA than subjects reporting never drinking or consuming less than 1 drink/week.
This large study is important as few prospective studies are of adequate size to have sufficient cases of RA to evaluate factors related to its development. The study supports previous research showing a lower risk of developing RA, or milder severity of the disease, among moderate drinkers than among abstainers.
Reference: Di Giuseppe D, Alfredsson L, Bottai M, Askling J, Wolk A. Long term alcohol intake and risk of rheumatoid arthritis in women: a population based cohort study. BMJ 2012;345:e4230 doi: 10.1136/bmj.e4230 (Published 10 July 2012)
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 083: Higher indices of quality of life are seen among persistent moderate drinkers than among abstainers — 20 June 2012
Data from a nationally representative sample of 5,404 community-dwelling Canadians ages 50 and older at baseline (1994/1995) was used to estimate the effects of alcohol drinking patterns on indices of quality of life, at baseline (when subjects were aged ≥50 years) and after a follow-up period. Health-related quality of life was assessed with the Health Utilities Index Mark 3 (HUI3). The authors report that most participants showed stable alcohol-consumption patterns over 6 years. Persistent regular moderate drinkers had the highest indices of quality of life at baseline, but subsequent changes in HUI3 were similar in all groups except those reporting decreasing alcohol consumption. The investigators conclude that persistent moderate drinkers had higher initial levels of health-related quality of life than persistent nonusers and those in other groups. However, rates of decline over time were similar for all groups except those decreasing their consumption, which had a greater decline in their level of health-related quality of life than persistent moderate users. While Forum reviewers admired the intent of this study, there were concerns about some of the statistical and epidemiologic aspects. The reasons that some people stopped drinking or decreased their intake were not known; while the authors state that subjects decreasing their alcohol consumption had a more rapid decline in quality of life measures, it is not known what percentage of such subjects decreased alcohol intake due to the development of serious iseases. If this were the case, such diseases may have been more important in their subsequent adverse health than the change in their drinking habits.
Further, the “baseline” quality of life measures in this study were obtained when subjects were aged 50 or older; this baseline value of quality of life was higher in moderate drinkers. However, there are statistical problems if adjustments are made for this when quality of life is assessed subsequently and related to drinking pattern. Peto has described this problem as a “horse-racing effect.” He states that in prospective studies, the correlation between exposures (e.g., drinking pattern) and outcomes (e.g., quality of life) assessments during follow up are likely to be the same as the outcome at the end of follow up. As an analogy he uses a race between ‘slow’ and ‘fast’ horses; it is likely that the fast horses will be ahead at the mid-point of the race as well as at the end. Environmental effects on quality of life begin early in life, and if one adjusts for the mid-life value (as done and referred to as “baseline” in the present study), you may end up disregarding much of the effect of subsequent alcohol intake.
Overall, this study shows a positive relation between moderate alcohol intake and quality of life in middle-aged adults. The effects on the subsequent quality of life as one ages of continued alccohol consumption, or of decreasing intake, remain unclear.
Reference: Kaplan MS, Huguet N, Feeny D, McFarland BH, Caetano R, Bernier J, Giesbrecht N, Oliver L, Ross N. Alcohol Use Patterns and Trajectories of Health-Related Quality of Life in Middle-Aged and Older Adults: A 14-Year Population-Based Study. J. Stud Alcohol Drugs 2012;73:581–590.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 082: A statistical model attempting to estimate the level of alcohol consumption that is “optimal” for health — 6 June 2012
Scientists from Australia and Oxford University have carried out a complex analysis in an attempt to determine the “optimal” level of alcohol consumption that is associated with the lowest rates of chronic disease in the UK. They conclude that the intake of about one-half of a typical drink per day would result in the healthiest outcomes, and the authors conclude that the recommended alcohol intake for the UK should be reduced from the current advised level of drinking.
There were a number of concerns by Forum members about the paper. It is based on an extremely complex statistical model that requires many assumptions, most of which cannot be validated. The parameters chosen to use in such a model determine the results, and a number of instances were identified where the values used in this analysis do not reflect current scientific knowledge. Further, the conclusions of the authors are based exclusively on the lowest point of the “J-shaped” curve for alcohol and disease, and disregard the findings that the risk of death, in comparison with non-drinkers, remains lower for drinkers of alcohol of up to several drinks per day.
There were other aspects of the paper that were of particular concern: (1) focusing only on the average amount of alcohol consumed, while the pattern of drinking (regular moderate versus binge drinking) has the greatest effect on health outcomes; (2) giving a single recommended level of alcohol intake irrespective of age; the greatest risks and lowest expected benefits of alcohol intake are among the young, whereas most of the putative health benefits relate to the diseases of ageing; (3) giving a single value for both men and women, since women are known to react (both adversely and beneficially) to lower levels of alcohol than do men; (4) the use of their estimated value alone for making recommendations for the population; guidelines should be based on a large number of social and behavioral factors, not just on the results of one scientific study.
The level of alcohol that is most likely to be associated with the lowest risk of adverse health outcomes and the most likely health benefits varies markedly among individuals. Middle-aged men and post-menopausal women are most likely to demonstrate enhanced health (e.g., lower risk of cardiovascular diseases, diabetes, dementia) from moderate drinking. For all ages, binge drinking is associated with predominantly adverse outcomes. In general, women should drink less than men. While the analyses presented in this paper are of scientific interest, they alone do not support changes in the current population recommendations for alcohol consumption.
Reference: Nichols M, Scarborough P, Allender S, Rayner M. What is the optimal level of population alcohol consumption for chronic disease prevention in England? Modelling the impact of changes in average consumption levels. BMJ Open 2012;2:e000957. doi:10.1136/bmjopen-2012-000957.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 081: Alcohol intake in the elderly affects risk of cognitive decline and dementia — 22 May 2012
A well-done review paper on the association between alcohol consumption and cognition in the elderly provides an excellent summary of potential mechanisms by which alcohol may affect cognitive function and the risk of dementia, both adversely and favorably. Current scientific data indicate that heavy drinking is associated with an increased risk of neurological disease and dysfunction, while regular light-to-moderate alcohol intake seems to be associated with a reduced risk of such dysfunction, including a lower risk of developing Alzheimer’s disease.
At present, the mechanisms by which the moderate intake of wine and other alcoholic beverages reduces the risk of cardiovascular diseases are much better defined than they are for cognition. Forum members agree with the authors that further research is needed to evaluate a potential role that wine and other alcoholic beverages may play in reducing the risk of dementia. Forum members also agree that, at present, the specific mechanisms of such putative protection are not well defined, and it would be premature to recommend light-to-moderate drinking for reducing the risk of dementia. On the other hand, current epidemiologic and biomedical data suggest that most elderly subjects who are responsible and moderate drinkers would not benefit from being advised to stop their alcohol consumption.
Reference: Kim JW, Lee DY, Lee BC, Jung MH, Kim H, Choi YS, Choi I-G. Alcohol and Cognition in the Elderly: A Review. Psychiatry Investig 2012;9:8-16; On-line: http://dx.doi.org/10.4306/pi.2012.9.1.8
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 080: Modest alcohol intake is associated with less inflammation among patients with the most common type of liver disease, non-alcoholic fatty liver disease (NAFLD) — 15 May 2012
NAFLD (non-alcoholic fatty liver disease) is the most common type of liver disease in the developed world, affecting up to one-third of the US population. NAFLD is often associated with obesity and other parameters of the so-called “metabolic syndrome,” which is a major risk factor for the development of cardiovascular disease. In a well-done study among subjects with NAFLD, the investigators have demonstrated that modest alcohol consumption (an average of up to 20 grams of alcohol per day and no binge drinking) is associated with less evidence of inflammation of the liver (steatohepatitis), a condition known to markedly increase the risk of progression of liver disease to cirrhosis.
Given that NAFLD and other conditions associated with the metabolic syndrome are so common, and are major risk factors for developing cardiovascular disease, the results of the present study are important. They show that modest drinking is associated with decreased, not increased, inflammation of the liver. Further, even among subjects with NAFLD, cardiovascular disease is a much more common cause of death than liver disease. The authors suggest that intervention studies should be done to support their findings; if confirmed, subjects with NAFLD should not be advised to avoid all alcohol, which is the current advice usually given to such patients.
Reference: Dunn W, Sanyal AJ, Brunt EM, Unalp-Arida A, Donohue M, McCullough AJ, Schwimmer JB. Modest alcohol consumption is associated with decreased prevalence of steatohepatitis in patients with non-alcoholic fatty liver disease (NAFLD). Journal of Hepatology 2012 (pre-publication release)
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
A Tribute to Federico Leighton Puga, MD — 8 May 2012
Frederico Leighton Puga, MD, Professor and Director of the Center for Molecular Nutrition and Chronic Diseases of the Catholic University of Chile in Santiago, died on 27 April 2012 at the age of 74 years. Dr. Leighton was a valued member of the International Scientific Forum on Alcohol Research, and was noted for his seminal work in nutrition, antioxidants, the health aspects of moderate wine consumption, and public health approaches for the prevention of chronic diseases.
Many Forum members knew and had worked with Dr. Leighton through many decades. All feel a deep loss, of a great scientist, a loyal and good friend, and someone very concerned with the health of people everywhere. As stated by one Forum member, “Federico was a great scientist motivated by curiosity and the desire to be useful for his country. His culture and education and intellectual rigor were well integrated into his humanity and the sweetness of his character.” Said another: “Federico had in abundance that indefinable quality known as ‘class.’” The world has lost an honest and honorable scientist.
For the full tribute to Dr. Leighton by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 079: Moderate alcohol consumption both prior to, and following, a myocardial infarction is associated with lower risk of mortality — 17 April 2012
In a very well-done analysis based on the follow up of more than 50,000 subjects from The Health Professionals Follow-up Study (HPFS), 1,818 men were confirmed with incident non-fatal myocardial infarction (MI). Among MI survivors, 468 deaths were documented during up to 20 years of follow up. Repeated reports were obtained on alcohol consumption throughout follow up. Average alcohol consumption was calculated prior to and then following the MI.
The overall results show that, in comparison with no alcohol consumption, the pre-MI and the post-MI intakes of light (0.1-9.9 g/day) and moderate (10.0-29.9 g/d) amounts of alcohol were both associated with lower risk of all-cause mortality and cardiovascular morality among these men. The significant reductions in all-cause mortality risk (22% lower for 0.1-9.9 g/day and 34% lower for 10.0 – 29.9 g/day, in comparison with non-drinkers) were no longer present for consumers of ≥ 30 g/day; for this highest consumer group, the adjusted hazard ratio was 0.87 with 95% CI of 0.61-1.25.
There are a number of other informative and interesting results described from this study. First, there was little change in reported alcohol prior to and following the MI: drinkers tended to remain drinkers of similar amounts. Few non-drinkers began to drink after their MI; among heavier drinkers, there was a tendency to decrease the amount somewhat (but very few stopped drinking completely). Further there were no significant differences in outcome according to type of beverage consumed although, interestingly, lower hazard ratios were seen for consumers of beer and liquor than of wine. While the authors state that the effects of alcohol were stronger for the association with non-anterior MIs, the HRs for all-cause mortality were little different: among the moderately drinking men the HRs were 0.58 for anterior MI and 0.51 for other types of MI.
Even though exposures (such as alcohol) for cardiovascular events (such as MI and cardiovascular mortality) may be different after a person has an event than it was before the event, in this study the reductions in risk were almost the same. For example, both for alcohol intake reported prior to a MI, and that after a non-fatal MI, the risk of mortality was about 30% lower for moderate drinkers than it was for abstainers. This suggests that, in terms of reducing cardiovascular disease, alcohol may have relatively short-term effects. Frequent consumption (of moderate amounts) may result in the best health outcomes.
Reference: Pai JK, Mukamal KJ, Rimm EB. Long-term alcohol consumption in relation to all-cause and cardiovascular mortality among survivors of myocardial infarction: the Health Professionals Follow-up Study. European Heart Journal 2012;doi:10.1093/eurheartj/ehs047
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 078: An update on the association of alcohol consumption with risk of breast cancer — 10 April 2012
An excellent review paper on the relation of alcohol consumption to the risk of breast cancer concludes that, overall, there is a positive dose-response relation between alcohol drinking and the risk of breast cancer. The analysis shows that an increase in risk is seen even among women reporting an average of only about one drink/day. Given the high prevalence of such light drinking in most female populations, the authors estimate that up to 1 to 2% of breast cancers in Europe and North America may be attributable to light drinking alone. Thus, while alcohol appears to be a risk factor for breast cancer, it does not explain a very high percentage of cases.
Forum members considered this to be a well-done analysis, with a good review not only of epidemiologic studies but of potential mechanisms of effect of alcohol on breast cancer risk. An increase in estrogen levels from alcohol seems to be the physiologic mechanism most commonly suggested for the increase in risk.
The meta-analysis is noteworthy in presenting risks specifically for women who consume up to one drink/day, which is the common pattern for a high proportion of women in western cultures. On the other hand, the authors herefailed to discuss the potential modification of alcohol effects on cancer risk from folate in the diet; in many studies, high folate levels tend to diminish or eliminate an increase in risk from alcohol. Further, the paper does not provide a discussion of the net effects of moderate drinking on mortality. In older women, the decrease in the risk of cardiovascular disease (a much more common cause of death than breast cancer), greatly exceeds the potential increase in risk of death from breast cancer.
Reference: Seitz HK, Pelucchi C, Bagnardi V, La Vecchia C. Epidemiology and Pathophysiology of Alcohol and Breast Cancer: Update 2012. Alcohol and Alcoholism 2012; doi: 10.1093/alcalc/ags011
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 077: Swedish study supports a “U-shaped” association of alcohol consumption with risk of pre-diabetes and diabetes mellitus — 29 March 2012
Subjects in a cohort in Sweden, some of whom had been exposed to a community intervention program to prevent diabetes, were evaluated 8-10 years after baseline for the presence of diabetes mellitus or impaired glucose metabolism (“pre-diabetes”) in relation to a baseline report of alcohol consumption. Approximately 2,000 men and 3,000 women had a normal glucose tolerance test at baseline; of these 105 men and 57 women developed type II diabetes. Of subjects with pre-diabetes at baseline, 175 men and 98 women progressed to diabetes. The authors report that total alcohol consumption and binge drinking increased the risk of pre-diabetes and diabetes in men, while low consumption decreased diabetes risk in women. However, the authors did not discuss the fact that in essentially all comparisons, the highest risk of diabetes or pre-diabetes was among abstainers.
Forum reviewers had some concerns about the study. For example, the study included some subjects who had been exposed to an intervention trial to prevent diabetes, yet no information is given on potential effects of the intervention. It was not a population-based group. Also, the sample was “enriched” with subjects who had a positive family history of diabetes, which may make it more difficult to judge the effects of environmental factors. Ex-drinkers and never drinkers were included in the abstainer group.
It appears that the authors focused only on the “statistically significant” results rather than commenting on the overall pattern of association (lower risk of developing diabetes for moderate drinkers than for abstainers and heavier drinkers). Further, the number of subjects in many of the sub-groups was very small, making it difficult to define specific cut-points for effects of alcohol on risk.
Nevertheless, reviewers considered that, overall, these analyses support the usual findings from previous research of a “U-shaped curve” for alcohol and diabetes for both men and women. There appears to be a reduction in risk with moderate alcohol intake and possibly an increased risk for heavier drinking.
Reference: Cullmann M, Hilding A, Östenson CG. Alcohol consumption and risk of pre-diabetes and type 2 diabetes development in a Swedish population. Diabet Med 2012;29:441–452. DOI: 10.1111/j.1464-5491.2011.03450.x
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 076: Evaluating the association of alcohol intake with cognitive functioning using a Mendelian randomization study design — 22 March 2012
Many observational cohort studies have shown that moderate alcohol use is associated with better cognitive function. However, since such studies are vulnerable to residual confounding by other lifestyle and physiologic factors, the authors conducted a Mendelian randomization study, using aldehyde dehydrogenase 2 (ALDH2) genotype (AA, GA, or GG) as an instrumental variable in 2-stage least squares analysis. Cognitive function was assessed from delayed 10-word recall score (n = 4,707) and Mini-Mental State Examination (MMSE) score (n = 2,284) among men from the Guangzhou Biobank Cohort Study (2003–2008). The authors had previously reported an association between reported alcohol intake and cognitive function from a larger group of subjects from the same study finding that women reporting occasional alcohol intake and men reporting occasional or moderate intake had better scores related to cognitive function than did abstainers.1
In the present Mendelian study, the authors found no significant association between groups defined by the ALDH2 genotype (as an “unbiased” estimate of alcohol consumption) and the two measures of cognitive functioning. A problem with the present analysis is that ALDH2 genotypes explained only 3% of the variance in reported alcohol intake, which weakens the conclusions of the authors. Further, differences in the predominant type of beverage consumed (rice wine), and probably marked differences in drinking patterns between these subjects and Europeans and Americans, make it difficult to know what the implications of this study are for western industrialized societies.
We agree with the authors that “Causality should be thoroughly verified in a variety of settings using different kinds of evidence, including experimental or genetic studies, rather than relying on simple observations in a particular setting.” We strongly support future attempts at using Mendelian randomization studies, hopefully using better instruments for estimating alcohol intake. On the other hand, as stated by recent evaluations of various study designs for determining causality,3 we appreciate that Mendelian randomization sounds good, but it is not the “Holy Grail.”
Reference: Au Yeung SL, Jiang CQ, Cheng KK, Liu B, Zhang WS, Lam TH, Leung GM, Schooling CM. Evaluation of moderate alcohol use and cognitive function among men using a Mendelian randomization design in the Guangzhou Biobank Cohort Study. Am J Epidemiol 2012; pre-publication release. DOI: 10.1093/aje/kwr462
Please click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 075: Moderate drinking associated with lower risk of stroke in women — 15 March 2012
A well-done analysis from the Nurses’ Health Study shows that the risk of total stroke is slightly lower among light-to-moderate consumers of alcohol than among subjects reporting no alcohol intake. In comparison with non-drinkers, the estimated risk is 17-21% lower for women averaging up to 15 grams of alcohol per day (a little over one drink/day by US definitions of approximately 12 grams of alcohol for a typical “drink.”). For consumers of larger amounts of alcohol, the risk of stroke has a tendency to be slightly increased, but not statistically significantly so.
Data on the pattern of drinking (regularly, binge, etc.) were not reported. Among these predominantly light drinkers, there were no differences between effects on the risk of the most common type of stroke, ischemic stroke (due to atherosclerotic obstruction of a artery or an embolic clot) or the less-common hemorrhagic stroke (bleeding into the brain).
The results, with full adjustment for other factors that may affect risk, suggest a “J-shaped” curve for total stroke, with reductions in risk for light-to-moderate drinking and possibly an increase with greater amounts. In this study, the point at which the risk of drinkers exceeds that of non-drinkers was about 38 grams of alcohol per day (the equivalent of about 3 typical “drinks”), with a 95% confidence interval of 28 to 57 grams/day.
The study supports many previous reports from observational epidemiologic studies that have shown a slight reduction in risk of the ischemic type of stroke from moderate alcohol intake. Some, but not all previous studies, show an increase in hemorrhagic stroke for any amounts of alcohol, but that was not seen in this study, possibly because there were few heavy drinkers in this group of nurses.
Reference: Jimenez M, Chiuve SE, Glynn RJ, Stampfer MJ, Camargo Jr CA, Willett WC, Manson JE, Rexrode KM. Alcohol Consumption and Risk of Stroke in Women. Stroke 2012, pre-publication. http://stroke.ahajournals.org. DOI: 10.1161/STROKEAHA.111.639435
Please click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 074: Does moderate wine consumption improve lung function? — 8 March 2012
An analysis based on a prospective study in the Netherlands assessed the impact of wine and resveratrol intake on lung function. It also studied genetic factors (affecting sirtuin) that have been found to be mechanisms by which resveratrol relates to metabolism and longevity of life. The authors report that resveratrol intake was associated with higher lung volumes and that white wine intake (but not red wine intake) was associated with lower risk of airway obstruction. They report that the genetic factors studied did not relate to the associations found.
While several previous studies (as does this one) have reported that wine intake improves lung function, Forum reviewers were concerned about several aspects of the paper, and especially with the conclusions of the authors that resveratrol was the key factor in improved lung function. A reviewer stated: “Resveratrol may well be just the bystander of something else present in wine.” The beneficial effects on lung function are probably related to many compounds present in wine, and not just resveratrol.
Based on a number of scientific studies, moderate wine intake appears to have a favorable effect on lung function. The doses of resveratrol seen in these epidemiologic studies are in the physiological range that could be expected from moderate wine consumption, unlike the huge doses of resveratrol being evaluated as a potential life-extending drug in pharmaceutical studies.
Reference: Siedlinski M, Boer JMA, Smit HA, Postma DS, Boezen HM. Dietary factors and lung function in the general population: wine and resveratrol intake. Eur Respir J 2012; 39: 385–391; DOI: 10.1183/09031936.00184110
Please click here for the full critique by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 073: The association of alcohol consumption with osteoporosis — 5 March 2012
Osteoporosis is a key underlying factor in fractures among the elderly, which are increasingly a major health problem. A review paper from France on the association between alcohol consumption and bone metabolism states that heavy alcohol intake may adversely affect bone mineral density and increase the risk of osteoporosis. It states that lighter drinking may actually improve bone density, but presents very limited data to support this statement. Forum members were disappointed that the paper did not carry out a meta-analysis or other synthesis of the data; further, data from a number of key epidemiologic studies on the subject were not discussed in the paper.
The paper provides important information on the mechanisms by which alcohol may affect bone metabolism. The authors describe effects of alcoholic beverages on bone density, bone microarchitecture, bone remodeling, and other mechanisms, which help explain how alcohol and polyphenols and other constituents of beer and wine may relate to the risk of fractures in the elderly.
Unfortunately, despite what the authors’ conclude, the paper does not provide a summation of the scientific data upon which public health policy can be based. Overall, current scientific data suggest that bone mineral density and the risk of fractures are favorably affected by light-to-moderate drinking, but adversely affected by heavy drinking and alcoholism.
Reference: Maurel DB, Boisseau N, Benhamou CL, Jaffre C. Alcohol and bone: review of dose effects and mechanisms. Osteoporos Int (2012) 23:1–16; DOI 10.1007/s00198-011-1787-7.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 072: Obesity may modify the association between alcohol consumption and the risk of colorectal cancer. 23 February 2012
A case-control study from Newfound/Labrador has reported that greater alcohol intake may increase the risk of colorectal cancer among obese subjects, but not among non-obese subjects. This is not a particularly large study, and only 45-60% of subjects who were recruited by telephone ended up providing data. Further, it is a case-control comparison, rather than a cohort analysis, making bias in the results more likely.
In this study, there was no relation of alcohol with the risk of CRC when considering the entire population. However, when subjects were stratified by BMI (<30 versus ≥ 30), the data indicate an increase in CRC risk for obese subjects who were “drinkers” (OR=2.2, 95% CI 1.2-4.0), especially among subjects reporting 5 or more drinks/daily (OR=3.7, CI 1.5-9.0). On the other hand, even among obese subjects there was not a clear dose-response effect noted, i.e., there was not a step-wise increase in CRC risk with greater number of drinks/day For example, the odds ratio (OR) was 2.3 times that of non-drinkers for obese subjects reporting 1-2 drinks/daily and 1.3 for those reporting 3-4 drinks/daily.
It will be interesting to determine if other studies show that there is modification of the association between alcohol intake and colorectal cancer by obesity. If such is the case, it could help understand some of the mechanisms for the development of cancer and provide better guidelines for screening for CRC.
Reference: Zhao J, Zhu Y, Wang PP, et al. Interaction between alcohol drinking and obesity in relation to colorectal cancer risk: a case-control study in Newfoundland and Labrador, Canada. BMC Public Health2012, 12:94 doi:10.1186/1471-2458-12-94
Please click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 071: Forum Comments on proposed new dietary guidelines for Australia — 16 February 2012
Members of the International Scientific Forum on Alcohol Research have provided comments on the chapter related to alcohol intake that has been included in “A review of the evidence to address targeted questions to inform the revision of the Australian Dietary Guidelines,” by the Australian Government Department of Health and Ageing and National Health and Medical Research Council (NHMRC), November 2011, ISBN Online 1864965304.
Forum members considered that the authors of the report should be commended on their work. Criticisms are primarily about the restriction in the time frame of the review, and minimal consideration of key nuances, such as quantity of alcohol consumed and its relation to risk or benefit, patterns of drinking, the balance between risks and benefits, and making statements at all when the evidence is too weak. More details (e.g. considering cardiovascular mechanisms to widen the search) would have added weight to the conclusions.
For the full comments of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 070: Potentially important new mechanisms found for the anti-aging effects of resveratrol, a phenolic compound found in red wine — 9 February 2012
A well-conducted experimental study in mice has provided potentially important new insights into the association of the intake of resveratrol and like compounds with health benefits. Resveratrol is a constituent of red wine and other vegetable products, and is being evaluated in high-doses as a pharmaceutical. The biologic mechanisms demonstrated in this study could provide key new approaches for the prevention or treatment of a number of chronic diseases in humans, especially those related to vascular and metabolic diseases and to the risk of mortality.
More than two decades ago, particularly through publicity related to the so-called “French Paradox,” the public became aware of the potential reduction in the risk of coronary heart disease from the moderate consumption of red wine, and the media focused on a single constituent in red wine, resveratrol, as being the “key” factor. We now know that resveratrol is only one of hundreds of phenolic compounds in wine, many of which have been shown to have beneficial effects on vascular function, and that alcohol itself (present in wine, beer or spirits) also provides considerable protection against heart disease. Still, there has remained considerable attention paid to resveratrol, and extensive scientific research on resveratrol and related substances have shown that, in high doses, they may increase longevity of life and reduce metabolic diseases of aging.
In general, Forum reviewers thought that this was a very well-done study. Their concerns related to the dose used in these experiments; while the levels of resveratrol and like compounds might be accessible with pharmaceutical doses, the suggestion that similar levels could be connected with wine consumption is misleading. Further, in humans, resveratrol in the diet will interact with many other chemicals to achieve an effect, as whole plant extracts consist of many active and inactive micronutrients that may play a role in health and disease. To ascribe a specific effect on health from one chemical found in wine or other plant products could be misleading.”
Still, the reviewers believed that this paper was an important contribution to our knowledge about the mechanisms by which resveratrol and other chemicals may play a role in cardiovascular and other diseases. Such knowledge could help develop approaches for the prevention and treatment of human disease and for increasing the longevity of a healthy life.
Reference: Park S-J, Ahmad F, Philp A, Baar K, Williams T, Luo H, Ke H, Rehmann H, Taussig R, Brown AL, Kim MK, Beaven MA, Burgin AB, Manganiello V, Chung JH. Resveratrol ameliorates aging-related metabolic phenotypes by inhibiting cAMP phosphodiesterases. Cell 2012;148:421-433. DOI 10.1016/j.cell.2012.01.017.
Click here for the full critique of this paper by the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 069: Little effect of binge drinking on heart disease or mortality among moderate drinkers in Denmark — 2 February 2012
In a well-done, population-based analysis from Denmark, it was found that subjects who were overall “light-to-moderate” drinkers but reported an episode of “binge drinking” (consumption >5 drinks on an occasion) did not show differences in risk of ischemic heart disease (coronary disease) or total mortality than did other moderate drinkers who did not report such an episode. These results are somewhat different from results of many other epidemiologic studies that have shown increased risk of health problems (even higher risk of coronary disease) to be associated with what was referred to as “binge drinking.”
Why there were no adverse effects of such drinking in the present study has provoked considerable discussion among members of the Forum. The general consensus of opinion has to do with inconsistencies in the definition of “binge drinking.” The rapid consumption of more than 5 drinks on an empty stomach surely has different effects than the consumption of alcohol over several hours with food, such as during a prolonged dinner. The rate of consumption strongly affects the consequences of alcohol; in fact, some have suggested that the consumption of more than 2 or 3 drinks in less than two hours may constitute a better definition of binge that the total number of drinks.
The Forum continues to suggest that “binge drinking,” however defined, is not a healthy pattern of alcohol consumption. But the circumstances of consumption (rate of consumption, with or without food, etc.) may also be important in its definition and in judging its effects on health.
Reference: Skov-Ettrup LS, Eliasen M, Ekholm O, Grønbaek M, Tolstrup JS. Binge drinking, drinking frequency, and risk of ischaemic heart disease: A population-based cohort study. Scandinavian Journal of Public Health 2011;39:880–887.
Click here for the full critique of this study by the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 068. Heavier alcohol consumption may increase risk of colon cancer in people with a family history of such cancer — 30 January 2012
An analysis based on a large number of subjects being followed in the Nurses’ Health Study and the Health Professionals Follow-up Study, relates alcohol consumption to the risk of colon cancer according to whether or not the subjects had a positive family history of colon cancer. Their results indicate that subjects with a family history whose average alcohol intake was 30 or more grams per day (about 2 ½ typical drinks by US standards) have an increase in their risk of colon cancer; there was not a significant association between alcohol and colon cancer among subjects without a positive family history.
Forum reviewers were somewhat concerned that the pattern of drinking (regularly or binge drinking) was not assessed, and that there was not a clear dose-response curve between the level of alcohol consumption and the risk of cancer (i.e., there was not a consistent increase in risk of cancer with greater alcohol intake). Further, folate intake was found to modify the association, with the highest risk for subjects with a positive family history of colon cancer, low levels of folate, and in the highest category of alcohol consumption.
The present study provides some support for an association between higher levels of alcohol intake and the risk of colon cancer among subjects with a positive family history of such cancer. However, there have been changes in the guidelines for screening for cancer (by endoscopy, with removal of pre-malignant tumors) and other preventive measures for people with a positive family history of colon cancer. Such measures could modify the effects of all risk factors for colon cancer in future analyses.
Reference: Cho E, Lee JE, Rimm EB, Fuchs CS, Giovannucci EL. Alcohol consumption and the risk of colon cancer by family history of colorectal cancer. Am J Clin Nutr 2012;95:413–419.
Click here for the full critique of this paper by the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 067: Comparison of effects of red wine versus white wine on hormones related to breast cancer risk 19 January 2012
Aromatase inhibitors (AIs) prevent the conversion of androgens to estrogens, and could play a role in the development of breast cancer. This study of 36 pre-menopausal women consisted of a cross-over intervention trial to determine if there were differences between red wine and white wine in their effects on AIs. Subjects sequentially consumed eight ounces of red wine, followed by white wine (or vice versa), each beverage for a one-month period. The investigators concluded that red wine, but not white wine, was associated with significant effects on some indices of estrogen metabolism; free testosterone and luteinizing hormone were increased, but no significant differences were noted in estrogen levels.
Forum reviewers considered the results interesting and that they contribute to our understanding of the relation of wine to hormonal levels. On the other hand, they were concerned about methodological problems, including a lack of baseline data and variations in the timing during the menstrual period of blood sampling (which could affect estrogen levels). Also, no significant effect of the interventions was seen on blood levels of estradiol.
Further, the Forum thought that it should be pointed out that data are inconsistent on the relation of red wine consumption to the risk of breast cancer; many studies do not show beverage-specific effects on risk. More research will be needed to determine if the polyphenols in red wine can play a role in lowering the risk of breast cancer.
Reference: Shufelt C, Bairey Merz CN, Yang YC, Kirschner J, Polk D, Stanczyk F, Paul-Labrador M, Braunstein GD. Red versus white wine as a nutritional aromatase inhibitor in premenopausal women. J Women’s Health, 2011;DOI: 10.1089/jwh.2011.3001
Click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 066: Is it the alcohol or the polyphenols in red wine (or both) that decrease cardiovascular disease in wine drinkers? 16 January 2012
Human randomized intervention trials of wine and alcohol are not common. This randomized, cross-over study was based on 67 male volunteers in Spain who were considered to be at “high-risk” of cardiovascular disease. The subjects agreed to not consume any alcohol for a baseline period, then for three one-month periods consumed 30 g/day of alcohol as red wine or as gin, or an equivalent amount of phenolics from dealcoholized red wine. The effects of each intervention on a large number of adhesion molecules and chemokines that affect inflammation and relate to the development of vascular disease were evaluated.
The key results of the study were that both ethanol and nonalcoholic compounds in red wine have potentially protective effects that may reduce the risk of vascular disease. Specifically, the authors conclude that “the phenolic content of red wine may modulate leukocyte adhesion molecules, whereas both ethanol and polyphenols of red wine may modulate soluble inflammatory mediators in patients at high risk of cardiovascular disease.” Thus, this study provides important new mechanistic evidence that the reduced risk of cardiovascular disease among red wine drinkers observed in most epidemiologic studies may result from a combination of both the alcohol and the polyphenols in the wine.
Reference: Chiva-Blanch G, Urpi-Sarda M, Llorach R, Rotches-Ribalta M, Guillèn M, Casas R, Arranz S, Valderas-Martinez P, Portoles O, Corella D, Tinahones F, Lamuela-Raventos RM, Andres-Lacueva C, Estruch R. Differential effects of polyphenols and alcohol of red wine on the expression of adhesion molecules and inflammatory cytokines related to atherosclerosis: a randomized clinical trial. Am J Clin Nutr 2012. doi: 10.3945/ajcn.111.022889.
Click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 065: Are there differences in mortality between people consuming wine and those consuming other types of alcoholic beverages? 20 December 2011
Wine consumers, especially in comparison with spirits drinkers, have been shown to have higher levels of education and income, to consume a healthier diet, be more physically active, and have other characteristics that are associated with better health outcomes. However, epidemiologic studies have been inconsistent in showing that, after adjustment for all associated lifestyle factors, consumers of wine have lower risk of cardiovascular disease and mortality than do consumers of other beverages.
A study based on the long-term follow up of a group of older Americans concluded that the associated lifestyle habits and environmental factors of wine consumers largely explained their better health outcomes. Forum reviewers were concerned about some of the methodological approaches used, and believed that the data presented in the paper were inadequate to support such a conclusion. This was a small study, had only a single estimate of alcohol intake (at baseline but not throughout 20 years of follow up), and the authors may have over-adjusted for large differences in lifestyle factors between what they termed as “low-wine” and “high-wine” consumers. The study did confirm a lower mortality risk for alcohol consumers than for non-drinkers.
Experimental studies have clearly indicated that the polyphenols and other constituents that are present in wine and some beers have independent protective effects against most cardiovascular risk factors. Whether or not such advantages are seen among moderate drinkers of wine (or beer) in epidemiologic studies is difficult to determine, as comparisons are not being made between wine, beer, and spirits but between humans who consume one or other such beverage. In almost all populations, drinkers of a specific beverage differ in many ways other than just the type of beverage they consume.
Reference: Holahan CJ, Schutte KK, Brennan PL, North RJ, Holahah CK, Moos BS, Moos RH. Wine consumption and 20-year mortality among late-life moderate drinkers. J Stud Alcohol Drug 2012; 73: 80–88.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 064: Association of lifestyle and environmental factors with the risk of cancer — 13 December 2111
It has been well established that certain lifestyle habits relate to the risk of certain cancers (e.g., smoking and lung cancer). In a well-done analysis, the authors estimate the proportion of cancer in the population associated with a variety of lifestyle and environmental factors. They find that smoking has, by far, the largest effect on the risk of cancer, with 19.4% of cancer cases in the UK attributable to tobacco use. A poor diet (less intake of fruits and vegetables and fiber and greater intake of meat and salt), obesity, and alcohol are the next most important factors that relate to cancer, with alcohol being calculated to relate to 4.0% of cancer cases in the UK.
Forum reviewers considered this to be a well-done paper that used epidemiologic methods that are preferable to those used in some previous such analyses. Generally, they disagreed with the authors that no alcohol consumption was the theoretical “optimum exposure level,” as the risk of certain cancers seems to increase primarily from heavy drinking. Further, they found reason to believe that the purported effects related to diet may have been over-estimated.
Nevertheless, this paper provides considerable new information on lifestyle and environmental factors that may relate to the risk of cancer. It puts into perspective the importance of targeting certain behaviors for the potential reduction in the risk of cancer.
Reference: Parkin DM, Boyd L, Walker LC. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. Summary and conclusions. British Journal of Cancer 2011;105:S77 – S81.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 063: Genes modify the risk of liver disease among alcoholics — 5 December 2011
It has been widely observed that only a small percentage of alcoholics develop cirrhosis of the liver, the most advanced form of alcoholic liver disease (ALD); the reason why all alcoholics do not develop such disease is not known. The present study from Spain, that includes original work and a meta-analysis, evaluates whether genetic polymorphisms that determine levels of glutathione-S-transferases (GST) relate to the risk of developing ALD among alcoholics. Alcoholics with certain genetic GST polymorphisms were found to be at significant excess risk for such liver disease in comparison with alcoholics without these polymorphisms.
As stated by the authors, the theory that these enzymes may affect risk is based on the ability of certain GST alleles to detoxify harmful ethanol metabolites in the liver by conjugating acetaldehyde and ROS to reduced glutathione. The specific polymorphisms that they found to be associated with increased liver disease are among those that would be expected to lower the activity of the corresponding GST enzymes; this would permit higher levels of toxic metabolites of alcohol and oxidative stress to be present for longer periods of time after excessive alcohol consumption.
Some Forum reviewers thought that while the study was well done, the authors were unclear as to how these data could directly lead to “potential therapeutic targets” for liver disease in alcoholics. Nevertheless, the original study and meta-analysis provide important data on how specific genetic factors relate to the development of liver disease among alcoholics and could theoretically lead to better strategies for the prevention and treatment of alcoholic liver disease.
Reference: Marcos M, Pastor I, Chamorro A-J, Ciria-Abad S, González-Sarmiento R, Laso F-J. Meta-analysis: glutathione-S-transferase allelic variants are associated with alcoholic liver disease. Aliment Pharmacol Ther 2011;34:1159–1172.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 062: Similar effects of beer and wine on the risk of cardiovascular disease and of total mortality — 22 November 2011
The authors carried out an updated meta-analysis on the relationship between wine, beer or spirit consumption and cardiovascular outcomes, using state-of-the-art statistical techniques. Their meta-analysis provides evidence of J-shaped relationships between both wine and beer intake and vascular risk, with maximal protection of about 33% at a level of 25 g/day of alcohol (approximately 2 drinks/day by US standards). A statistically significant association between spirits intake and vascular disease was not found.
The key result of this meta-analysis is the finding of a very similar inverse association between the consumption of beer and the consumption of wine in relation to cardiovascular outcomes. While a similar associationwas not seen for spirits consumption, the data presented do not permit the conclusion that the key effects on cardiovascular disease are primarily due to the polyphenols in beer and wine. Similarly, the results do not permit the conclusion that the effect on cardiovascular disease is due primarily to the alcohol in these beverages. The lack of a similar J-shaped association for spirits may have been due to different drinking patterns (e.g., more binge drinking among consumers of spirits), as the pattern of drinking was not included as a confounder in the analyses.
Reference: Costanzo S, Di Castelnuovo A, Donati MB, Iacoviello L, de Gaetano G. Wine, beer or spirit drinking in relation to fatal and non-fatal cardiovascular events: a meta-analysis. Eur J Epidemiol 2011;DOI 10.1007/s10654-011-9631-0
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
A response from the Alcohol Policy Coalition of Australia to the Forum Critique #058: “A misguided statement on alcohol and health from a coalition in Australia,” which was published on the Forum web-site on 28 September 2011.
The Alcohol Policy Coalition of Australia has provided a response to Forum critique #058, “A misguided statement on alcohol and health from a coalition in Australia,” that was published on the Forum web-site on 28 September 2011.
The original Forum critique is available under Recent Reviews, #058 (click Critique o58). A description of the Forum, its members, the goals of the Forum, a disclosure statement, etc., are available from the home page of the web-site.
The response from the Alcohol Policy Coalition is now published in full on our web-site, dated 18 November 2011. To read the response to our critique # 058 provided by the Alcohol Policy Coalition, please click here.
===============================================================================
Critique 061: The reduction in risk of coronary heart disease from alcohol consumption may involve mechanisms other than an increase in HDL-cholesterol. 10 November 2011
In a prospective, observational study of approximately 150,000 Norwegians, the investigators found that alcohol consumption was associated with a large decrease in the risk of death from coronary artery disease. For men, the fully adjusted hazard ratio for cardiac death was 0.52 (95% CI 0.39 – 0.69) when comparing subjects reporting more than one drink/week in comparison with those reporting never or rarely drinking; for women, it was 0.62 (0.32–1.23). There was little change in the hazard ratio when HDL-cholesterol (HDL) was added to the model, suggesting that very little of the lower risk of heart disease was due to an increase in HDL from alcohol consumption.
Forum members considered this a well-done analysis. They were surprised at the very low amounts of alcohol intake reported by the subjects, with only 16% of males and about 8% of females reporting more than one drink/week. It is possible that the low levels of drinking, or perhaps over-adjustment in the multivariable analysis, led to the lack of effect of HDL. Most other studies have shown a much larger proportion of the effect of alcohol on heart disease risk to be associated with an increase in HDL.
Reference: Magnus P, Bakke E, Hoff DA, Høiseth G, Graff-Iversen S, Knudsen GP, Myhre R, Normann PT, Næss Ø, Tambs K, Thelle DS, Mørland J. Controlling for High-Density Lipoprotein Cholesterol Does Not Affect the Magnitude of the Relationship Between Alcohol and Coronary Heart Disease. Circulation 2011;124: DOI: 10.1161/CIRCULATIONAHA.111.036491
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 060: A new analysis from the Nurses’ Health Study on the association of alcohol with risk of breast cancer 3 November 2011
In a well-done analysis using prospectively collected data from the Nurses’ Health Study, the risk of breast cancer was found to be modestly increased among consumers of alcohol, even those whose total alcohol consumption was reported to be in the range of 3 to 6 drinks/week. Similar small increases in the risk of breast cancer have been found from alcohol consumption in the majority of previous studies observational studies. A strength of this study was the very large number of subjects, permitting the investigators to attempt to determine if both the amount of alcohol and the frequency of consumption were important in this association; strong effects were not found for either. A weakness is the failure to report the effects of folate intake on the association between alcohol and cancer; the same investigators have previously shown that folate is a potential moderator of the effects of alcohol on breast cancer risk.
The authors describe well the dilemma that women face regarding alcohol intake, which may increase slightly the risk of breast cancer but markedly decrease the risk of other more common diseases, especially cardiovascular conditions. For example, the authors state that regarding breast cancer, “We did find an increased risk at low levels of use, but the risk was quite small.” Forum members agree with the statement of the authors that “An individual will need to weigh the modest risks of light to moderate alcohol use on breast cancer development against the beneficial effects on cardiovascular disease to make the best personal choice regarding alcohol consumption.”
Reference: Chen WY, Rosner B, Hankinson SE, Colditz GA, Willett WC. Moderate alcohol consumption during adult life, drinking patterns, and breast cancer risk. JAMA 2011;306:1884-1890.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 059: Association of quantity of alcohol and frequency of consumption with cancer mortality
20 October 2011
A paper from the National Institutes of Health in the United States attempts to evaluate the separate and combined effects of the frequency of alcohol consumption and the average quantity of alcohol per occasion as they relate to the risk of mortality from all cancers, as well as cancer-specific mortality. It is based on repeated administrations of the National Health Interview Survey in the United States, with a total of more than 300,000 subjects and over 8,000 deaths from cancer, and reports on total cancer deaths and deaths from lung, colorectal, prostate, and breast cancers.
For total alcohol consumption (frequency x quantity), the data indicate a significant reduction in the risk of all-site cancers (RR=0.87, CI 0.80-0.94) which, interestingly, is not emphasized by the authors and is not included in their abstract. Moderate drinking consistently shows no effect, and only heavier drinking is associated with an increase in all-site cancer risk. For site-specific cancers, an increase in risk of lung cancer was seen only for heavier drinkers, with a tendency for less cancer among light drinkers. There was no evidence of an effect of total alcohol consumption on colorectal, prostate, or breast cancer.
The authors excluded non-drinkers in a second analysis in which they used categories of usual daily quantity and of frequency of consumption in an attempt to investigate their separate effects. For all-site cancer and for lung cancer, these results again show an increase in risk only for drinkers reporting greater amounts of alcohol. The data also show an increase in cancer risk from more frequent drinking among women but not among men. For colorectal, prostate, and breast cancer, there is no clear pattern of an increase in risk from quantity of alcohol consumed. For frequency of drinking, again there is a suggestion of an increase in risk with more frequent drinking, although the trends are not statistically significant.
The overall message of this analysis is that light to moderate alcohol intake does not appear to increase the risk of all-site cancer (and light drinking was shown in this study to be associated with a significant decrease in risk). Similarly, light to moderate consumption was not associated with site-specific cancers of the lung, colorectum, breast, or prostate. Heavier drinking is known to be associated with a large number of adverse health effects, including certain cancers, as was shown in this study.
When considering cancer, alcohol consumption should not be considered in isolation, but in conjunction with, other lifestyle behaviors (especially smoking). We agree with the authors that both quantity and frequency of consumption need to be considered when evaluating the relation of alcohol to cancer; further, beverage-specific effects need to be further evaluated.
Reference: Rosalind A. Breslow RA, Chen CM, Graubard BI, Mukamal KJ. Prospective study of alcohol consumption quantity and frequency and cancer-specific mortality in the US population. Am J Epidemiol 2011; DOI: 10.1093/aje/kwr210.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 058: A misguided statement on alcohol and health from a coalition in Australia. 28 September 2011
A group known as the Alcohol Policy Coalition in Australia has released a document entitled Cancer, Cardiovascular Disease and Alcohol Consumption. Forum members agree that excessive alcohol use has many adverse effects on the individual and on society, and efforts to reduce such use are important. On the other hand, they were disturbed that the coalition statement was limited almost exclusively to the effects of abusive drinking, was based primarily on extremely limited sources of information (mainly position statements by other organizations, and not publications based on sound research), and indicated a strong bias against alcohol.
Forum members contend that the Australian report misrepresents the extensive scientific data available on alcohol and health. The report specifically ignores scientific data indicating that in all developed countries, moderate consumers of alcohol are at much lower risk of essentially all of the diseases of ageing: coronary heart disease, ischemic stroke, diabetes, and dementia. And conspicuously absent from the Australian report is a description of the lower total mortality among middle-aged and elderly people associated with moderate alcohol consumption, a finding that has been found consistently throughout the world. Further, there is no mention in the report of the key relevance of the pattern of drinking, although regular moderate drinking (versus binge drinking only on week-ends, even when the total volume of alcohol is the same) has been shown to be a strong determinant of beneficial effects of alcohol consumption.
Scientific data over many decades have shown that while excessive or irresponsible alcohol use has severe adverse health and societal effects, regular moderate drinking is associated with beneficial effects on health. And a very large number of experimental studies, including results from human trials, have described biological mechanisms for the protective effects of both alcohol and the polyphenolic components of wine.
There have been a number of comprehensive meta-analyses published that Forum members believe can provide much more accurate, up to date, and scientifically balanced views of the current status of the health effects of alcohol consumption. Such documents are better sources of data upon which policy decisions should be based.
Reference: Alcohol Policy Coalition Position Statement. “Cancer, Cardiovascular Disease and Alcohol Consumption.” Released in Australia, September 2011.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 057: Differences in effects on atherosclerosis of regular moderate drinking and binge drinking. An experimental study in mice. 20 September 2011
An excellent study among experimental animals has reported very dramatic differences between the effects of alcohol administered in moderation on a daily basis and the same total weekly amount of alcohol administered on only two days of the week: binge drinking. The mice used in the study that were given regular moderate amounts of alcohol showed no weight gain, improved lipid values, and much less development of atherosclerosis than did control animals. However, those given alcohol in a binge-drinking pattern showed worse outcomes than control animals, and much worse outcomes than those given regular moderate alcohol.
This experimental study provides strong support for the frequent finding among humans in epidemiologic studies: benefits from regular moderate drinking, adverse effects from binge drinking. It is especially important since, being an experimental study, the potential confounding effects of other lifestyle habits are not an issue, as is always the case for observational studies among humans.
Reference: Liu W, Redmond EM, Morrow D, Cullen JP. Differential effects of daily-moderate versus weekend-binge alcohol consumption on atherosclerotic plaque development in mice. Atherosclerosis 2010, doi:10.1016/j.atherosclerosis.2011.08.034
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 056: Relation of alcohol consumption to colorectal cancer 13 September 2011
A meta-analysis of case-control and cohort studies on the association of alcohol consumption with colorectal cancer was carried out, based on 22 studies from Asia, 2 from Australia, 13 from Western Europe, and 24 from North America. The paper provides evidence that alcohol, at least at higher levels of consumption, is associated with an increase in the risk of colorectal cancer. Overall, there was no increase in the risk for consumers reporting an average intake of up to 1 drink per day, but a modest increase (of 21%) for what the authors defined as “moderate drinking” (averaging up to 49.9 g of alcohol, or about 4 typical drinks, per day). The increase in risk was greater (52%) for consumers of 50 or more grams of alcohol per day.
Forum reviewers thought that this was, in general, a very well-done study that used appropriate statistical techniques for meta-analysis. There were some key concerns, however, including the following: (1) the authors’ definition of “moderate drinking” extended well above the usual recommended limits for sensible drinking; effects of consumption in categories of 1 to 2 drinks/day, 2 to 3 drinks/day, etc., were not given; (2) no results were provided according to type of beverage even though many previous studies have shown differences between health effects for consumers of wine, or wine/beer, and other beverages; and (3) no data were available on the pattern of drinking. Many studies have shown that regular, moderate drinking on most days of the week has very different health outcomes than drinking only on week-ends or binge drinking.
Despite these concerns, Forum members agreed that current data indicate that alcohol intake, especially heavier drinking, is associated with an increase in the risk of colorectal cancers. Future studies are needed to help determine if there is a threshold level of alcohol that increases the risk, if there are differences by type of beverage, and if the pattern of drinking (regular versus binge drinking) affects the risk.
Reference: FedirkoV, Tramacere I, Bagnardi V, Rota M, Scotti L, Islami F, et al. Alcohol drinking and colorectal cancer risk: an overall and dose–response meta-analysis of published studies. Annals of Oncology 22: 1958–1972, 2011, doi:10.1093/annonc/mdq653
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 055. Alcohol intake and “successful ageing” 8 September 2111
Among 13,894 women in the Nurses’ Health Study, investigators prospectively examined alcohol use assessed at midlife in relation to “successful ageing,” which was defined as survival to age 70 years, not having a major chronic disease (such as coronary disease, cancer, stroke, diabetes), and having no major cognitive impairment, physical impairment, or mental health problems. Only 11% of the women met these criteria.
The results indicate that moderate drinkers, especially those consuming wine and drinking regularly, were more likely to exhibit successful ageing. For average amount consumed, the largest benefit (an increase of 28%) was among women who reported 15.1 – 30 g of alcohol per day (an average of just over 1 to 2 ½ drinks per day), when compared with non-drinkers. The frequency of drinking was especially important: in comparison with nondrinkers, women who drank only on 1 to 2 days per week had little increase in their risk of successful ageing, but those drinking on at least 5 days per week had almost a 50% greater chance of successful ageing.
Forum reviewers had some questions about the definition of “successful ageing” used in this study. It is believed that a much greater percentage of people who may not meet these criteria make huge contributions to society and should be considered “successful.”
In summary, these results support the findings of earlier studies showing that many aspects of successful ageing, in addition to just survival, are favorably affected by regular, moderate consumption of alcohol.
Reference: Sun Q, Townsend MK, Okereke OI, Rimm EB, Hu FB, Stampfer MJ, Grodstein F. Alcohol consumption at midlife and successful ageing in women: A prospective cohort analysis in the Nurses’ Health Study. PLoS Med 8(9): e1001090. doi:10.1371/journal.pmed.1001090
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 054. Role of alcohol intake and smoking on upper aerodigestive cancers – 6 September 2011
This paper provies an extensive analysis of the proportion of the risk of upper aero-digestive tract (UADT) cancers in the population (the population attributable risk) may be due to alcohol consumption and/or smoking. The analyses provide strong evidence that smoking is the most important factor in the risk of these cancers, and the risk is enhanced among those who also consume 2 or more drinks per day. Alcohol alone (i.e., among non-smokers) has little effect on the risk.
The authors state that their observations “are consistent with the hypothesis that alcohol acts as a carcinogen primarily because of its promoting effect on tobacco smoke.” In terms of the population-attributable risk, the authors conclude that “Our findings confirm that tobacco and alcohol together explain 73% of total UADT cancer burden in Europe.” Overall, tobacco use alone explained 28.7%, the combination of smoking and drinking 43.9%, and alcohol use alone only 0.4% of the population attributable risk. Among women, the risk of these cancers was higher among smokers than among those who both smoked and consumed alcohol; this perhaps suggests that the moderate intake of wine, the most common beverage among European women, may play a role in reducing the risk associated with smoking.
Forum reviewers thought that this was a very good paper, but hoped that in the future we would have more studies that evaluated the effects on risk of varying levels of alcohol consumption, differential effects of various beverages, and even differential effects according to subjects’ genetically determined differences in alcohol metabolizing enzymes.
Reference: Anantharaman D, Marron M, Lagiou P, Samoli E, Ahrens W, Pohlabeln H, et al. Population attributable risk of tobacco and alcohol for upper aerodigestive tract cancer. Oral Oncology 2011;47:725–731.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 053: An extensive review of the effects of alcohol consumption on the risk of cognitive impairment and dementia 25 August 2011
The authors of this paper have carried out an excellent review of the relation of alcohol consumption to the risk of cognitive impairment and dementia. They reviewed a total of 143 previous publications on the topic. There were 74 studies, based on a total of more than 250,000 subjects, that provided risk estimates for varying levels of alcohol consumption which allowed the investigators to include them in a comprehensive meta-analysis. These papers were published mainly after 1998, were predominantly among older subjects (92% were ≥ 55 years of age and 70% ≥ 65 years of age), and almost all employed mental status examinations to define cognitive impairment/dementia.
As stated by the authors, “These studies overwhelmingly found that moderate drinking either reduced or had no effect on the risk of dementia or cognitive impairment.” Overall, in the new meta-analysis based on these studies, the average ratio of risk for cognitive risk associated with moderate drinking of alcohol was 0.77, with nondrinkers as the reference group. This estimate is close to the estimates of reduction in the risk of cognitive dysfunction (RR of 0.73 and 0.74) seen in other recent selective meta-analyses. The present study found that both light and moderate drinking provided a similar benefit, but heavy drinking was associated with non-significantly higher cognitive risk for dementia and cognitive impairment.
Forum reviewers of this paper were particularly pleased that the authors attempted to answer a number of specific questions on this topic that have been raised from previous research. Their results included finding no appreciable differences whether or not “sick quitters” were included in the reference group, little effect from adjustments for other lifestyle factors, and no significant differences between alcohol’s effects on dementia, Alzheimer’s dementia, or vascular dementia (but, based on a small number of studies, no significant reduction in risk of cognitive decline over time). The investigators concluded that there were no differences between results in men and women. Their analyses also led to the conclusion that wine is associated with more beneficial effects on cognition than beer or spirits, but the authors caution that these results are based on a limited number of reports, and that many studies show no significant differences according to type of beverage.
Forum reviewers agreed with the conclusions of the authors that “Overall, light to moderate drinking does not appear to impair cognition in younger subjects and actually seems to reduce the risk of dementia and cognitive decline in older subjects.”
Reference: Neafsey EJ, Collins MA. Moderate alcohol consumption and cognitive risk. Neuropsychiatric Disease and Treatment 2011:7:465–484.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 052: Does moderate alcohol consumption increase body weight? 16 August 2011
A paper from Spain provides an extensive review of the association between alcohol consumption and body weight. It includes descriptions of cross-sectional and prospective studies (and a few small intervention studies) among subjects who varied in age (adolescence to old age), culture (from Americans and Europeans to Asians), and principal type of beverage consumed and pattern of drinking. The authors state that many of the studies they reviewed appear to be contradictory in their results. However, based on their review, they conclude that “as positive associations between alcohol and weight gain were mainly found in studies with data on higher levels of drinking, it is possible that an effect on weight gain or abdominal adiposity may only be experienced by heavy drinkers.” A second conclusion of the authors is that “the type of alcoholic beverage might play an important role in modifying the effect of alcohol consumption on weight gain,” with more favorable effects generally seen among consumers of wine. A formal meta-analysis is not provided. Forum members were uncertain whether the higher risk seen for spirits drinkers in this study was due to the beverage they chose or to their consumption of larger amounts of alcohol.
The overall conclusions of the authors is that it is currently unclear whether alcohol consumption a risk factor for weight gain, but if so it appears to occur mainly among heavier drinkers. They also state that “light-to-moderate alcohol intake, especially of wine, may be more likely to protect against, rather than promote, weight gain.”
Forum reviewers agreed with most of the conclusions of the authors, especially that current data do not clearly indicate if moderate drinking increases weight; further, the biologic mechanisms relating alcohol to changes in body weight are not well understood. The Forum review comments on the strong protective effects of moderate drinking on the risk of metabolic syndrome and diabetes, both of which relate to increasing obesity. And some studies suggest that even very obese people may be at lower risk of diabetes if they are moderate drinkers. Forum members also reviewed some of the distinctive mechanisms by which alcohol is metabolized in the body (it provides calories that are rapidly absorbed and are not stored in fat) that could explain differences in the effects of calories from alcohol and from other foods.
Forum members agree with the authors of this paper that future research efforts should be directed towards assessing the specific roles of different types of alcoholic beverages, taking into account drinking patterns, and perhaps including in the analysis the propensity of individual subjects to gain weight in the past. For now, there is little evidence that someone consuming small to moderate amounts of alcohol on a regular basis is increasing his or her risk of becoming obese.
Reference: Sayon-Orea C, Martinez-Gonzalez MA, Bes-Rastrollo M. Alcohol consumption and body weight: a systematic review. Nutrition Reviews 2011;69:419-431.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 051: Types of alcohol in relation to acute pancreatitis 11 August 2011
A very well-done analysis from scientists in Sweden has related the type of alcoholic beverage, and the amount consumed per occasion, to the risk of acute pancreatitis. The study suggests that a greater number of drinks per occasion (“binge drinking”) of spirits increases the risk of acute pancreatitis, but no such relation was seen for the consumption of beer or wine. Forum reviewers suggested that a faster rate of drinking, with a greater rise in BAC, for spirits drinkers may be an important factor in the observed higher risk of pancreatitis; the increased risk may not necessarily be due to lower levels of antioxidants or to the presence of other toxic substances in spirits.
In any case, the average total alcohol consumption did not affect the risk of pancreatitis; instead, it was the number of drinks consumed per occasion (of spirits, in this study) that was associated with an increase in risk. Residual confounding by the pattern of drinking, diet, or by other lifestyle factors could still be operating, and it will require replication of these results in other studies to support the conclusions of the authors.
Reference: Azodi OS, Orsini N, Andrén-Sandberg Å, Wolk A. Effect of type of alcoholic beverage in causing acute pancreatitis. Brit J Surgery 2011;DOI: 10.1002/bjs.7632.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 050: Multiple maternal risk factors for fetal alcohol disorders 7 August 2011
An extremely well researched and written review on the relation of maternal drinking during pregnancy to adverse fetal outcomes has been published by scientists from the University of New Mexico Center on Alcoholism, Substance Abuse, and Addictions. It covers many factors (host, agent exposure, and environment) that have been found to relate to the occurrence of fetal alcohol spectrum disorders (FASD). Such factors modify the risk associated with alcohol consumption during pregnancy, although the risk of abnormalities is clearly increased with frequent consumption of large amounts of alcohol, and is greater among women who are alcoholics. While current data do not show that light or occasional alcohol consumption during pregnancy increases the risk of FASD, Forum members do not believe that pregnant women should be encouraged to drink.
Forum members agree with the authors that “More research is needed to more clearly define what type of individual behavioral, physical, and genetic factors are most likely to lead to having children with FASD.” Evaluating these multidimensional factors should help identify women at particular risk for having a child with FASD and lead to interventions to prevent such fetal abnormalities.
Reference: May PA, Gossage JP. Maternal risk factors for fetal alcohol spectrum disorders. Not as simple as it might seem. Alcohol Research & Health 2011;34:15-26.
For the full critique of this article by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 049: Effects of smoking and alcohol use on risk of upper aero-digestive cancers 1 August 2011
A case-control analysis from subjects living in areas of South America with high rates of upper aero-digestive tract cancers showed that both alcohol consumption and smoking tended to increase the risk of such cancers. However, the predominant cause of these cancers was the combination of smoking and alcohol consumption, with much higher risk than either exposure alone. The effects on risk were greater for smoking than for alcohol: for non-smokers, there was little effect of alcohol on risk. For non-drinkers, the risk of cancer associated with smoking was still increased, but was lower than it was for current drinkers.
An especially important finding in this study was that, among ex-drinkers and former smokers, the increased risks associated with alcohol and tobacco use decreased steadily as the time since quitting increased. As stated by the authors, most of these cancers “could be prevented by quitting the use of either of these two agents.”
Reference: Szymańska K, Hung RJ, Wűnsch-Filho V, Eluf-Neto J, Curado MP, Koifman S, Matos E, Menezes A, Fernandez L, Daudt AW, Boffetta P, Brennan P. Alcohol and tobacco, and the risk of cancers of the upper aerodigestive tract in Latin America: a case–control study. Cancer Causes Control (2011) 22:1037–1046. DOI 10.1007/s10552-011-9779-7
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 048: A new report on drinking guidelines and the association of alcohol with risk of cancer. 18 July 2011
The Canadian Medical Association Journal has published a commentary by some French scientists relating drinking guidelines to the association between alcohol and cancer. They conclude that the current guidelines for sensible drinking for the general population are not adequate for the prevention of cancer, and revisions and eventual exclusion of such guidelines are needed.
Forum reviewers agree that alcohol consumption, especially heavy intake, increases the risk of certain types of cancer. However, they consider that the opinions of the authors in the paper (labeled as an “Analysis” rather than an editorial or comments) do not reflect current sound scientific data, that the report is highly selective in citing a small number of papers that support their opinions, and that the authors have ignored a huge amount of recent data from more scientifically sound research that have largely discredited such studies. Further, the report provides no mention of the consistent finding from studies around the world that moderate drinkers tend to have lower all-cause mortality risk than do abstainers.
Scientific data over many decades have shown that excessive or irresponsible alcohol use has severe adverse health effects, including an increase in the risk of certain cancers. On the other hand, moderate drinking is associated with lower risk of cardiovascular disease and many other diseases of ageing and with all-cause mortality. A very large number of experimental studies, including results from human trials, have described biological mechanisms for the protective effects of alcoholic beverages against such diseases. A number of comprehensive meta-analyses provide much more accurate, up to date, and scientifically balanced views than does the current paper; such documents may be better sources of data upon which guidelines to the public regarding alcohol consumption should be based.
Reference: Latino-Martel P, Arwidson P, Ancellin R, Druesne-Pecollo N, Hercberg S, Le Quellec-Nathan M, Le-Luong T, Maraninchi D. Alcohol consumption and cancer risk: revisiting guidelines for sensible drinking. CMAJ 2011. DOI:10.1503. /cmaj.110363
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 047: Overall health effects of alcohol consumption. Comments on a WHO report 10 July 2011
The World Health Organization (WHO) has released its global status report on alcohol and health for 2011. Forum members largely agreed with the discussion in the report of the serious health and societal problems associated with the misuse of alcohol, which contributes to accidents, many diseases, and premature deaths. On the other hand, Forum members were disturbed that the report was limited almost exclusively to abusive drinking, was based primarily on out-dated information, and minimized the beneficial health effects associated with moderate drinking. The report ignored a massive amount of scientific data indicating that in all developed countries, moderate consumers of alcohol are at much lower risk of essentially all of the diseases of ageing: coronary heart disease, ischemic stroke, diabetes, dementia, and osteoporosis. And conspicuously absent from the WHO report is a description of the decrease in total mortality among middle-aged and elderly people associated with moderate alcohol consumption, a finding that has been found consistently throughout the world.
Epidemiologic studies over many decades have shown that while excessive or irresponsible alcohol use has severe adverse health and societal effects, moderate drinking is associated with lower risk of cardiovascular disease and other diseases of ageing. And a very large number of experimental studies, including results from human trials, have described biological mechanisms for the protective effects of both alcohol and the polyphenolic components of wine. A number of comprehensive meta-analyses are cited by Forum reviewers which they consider to provide much more accurate, up to date, and scientifically balanced views of the current “status” of the health effects of alcohol consumption. Such documents are better sources of data upon which policy decisions should be based.
Reference: Global status report on alcohol and health. World Health Organization 2011. ISBN 978 92 4 156415 1 (NLM classification: WM 274)
For the full critique of this publication by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 046: All-cause mortality rates are lower among moderate drinkers than among abstainers. 4 July 2011
The author of this paper set out to determine the extent to which potential “errors” in many early epidemiologic studies led to erroneous conclusions about an inverse association between moderate drinking and coronary heart disease (CHD). His analysis is based on prospective data for more than 124,000 persons interviewed in the U.S. National Health Interview Surveys of 1997 through 2000 and avoids the pitfalls of some earlier studies. He concludes that the so-called “errors” have not led to erroneous results, and that there is a strong protective effect of moderate drinking on CHD and all-cause mortality.
The results of this analysis support the vast majority of recent well-done prospective studies. In the present paper, non-drinkers had much higher risk of death than did almost all categories of subjects consuming alcohol. The author contends that these results lend credence to the argument that the relationship between alcohol and mortality is causal.
While some Forum reviewers felt that this analysis only replicates what has been shown in many other papers, it appears that erroneous information continues to be used by some policy groups. Thus, most reviewers believe that this new analysis provides important information on potential health effects of moderate drinking.
Reference: Fuller TD. Moderate alcohol consumption and the risk of mortality. Demography 2011. DOI 10.1007/s13524-011-0035-2
For the full review of this publication by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 045: Alcohol drinking in the elderly: Risks and benefits. 26 June 2011
The Royal College of Psychiatrists of London has published a report related primarily to problems of unrecognized alcohol misuse among the elderly. The report provides guidelines for psychiatrists and family physicians on how to find and how to treat elderly people with misuse of alcohol and drugs. The report also mentions lower “sensible limits” for older people in comparison with younger people. The Forum reviewers point out, however, inherent difficulties in providing guidelines for a very non-homogenous group of individuals whose only criterion for inclusion is being above the age of 65 years. Such a group includes individuals varying from marathon runners to very sick, frail people. Forum reviewers thought that advice to lower limits of drinking for everyone in this age group is not based on reliable research, and would certainly not apply to all in this age group.
The Forum reviewers were also struck by the absence in the Royal College report of any discussion of the strong positive effects of moderate drinking on most of the diseases of ageing, especially cardiovascular diseases, diabetes, and dementia, which are leading causes of morbidity and mortality in this age group. For healthy moderate and responsible drinkers, advice to reduce or stop all alcoholic beverage intake would not be in the best health interests of such individuals.
Reference: Royal College of Psychiatrists, London. Our invisible addicts. First Report of the Older Persons’ Substance Misuse Working Group of the Royal College of Psychiatrists, College Report CR165. June 2011
For the full review of this publication by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 044: The association of alcohol drinking with migraine headache 12 June 2011
An excellent paper from a headache center in Italy summarizes the scientific data relating alcohol ingestion to migraine headaches. The factors that trigger an attack of migraine, or of other headaches as well, are poorly understood. While retrospective studies tend to include alcohol as a trigger for an attack, the authors describe that in a recent prospective study (in which information on the factors that could potentially trigger an attack were collected prior to the migraine attack), menstruation, stress, and fatigue were found most commonly to relate to a subsequent attack, but not alcohol consumption (in fact, beer consumption on the previous day reduced the risk of a migraine attack). In the present paper, the authors reviewed the role and mechanism of action of alcohol or other components of alcoholic drinks in relation to alcohol-induced headache. They conclude from their review that reports overestimate the role of alcohol, as well as other foods, in the triggering of migraine.
Forum members thought that this was a very balanced review of the subject, and that it provided straightforward and sensible advice. Although some individuals surely have the onset of a migraine or other type of headache after the consumption of wine or alcohol, the findings are not consistent. Forum members suggest that given that subjects reporting migraine headaches have been found to be at increased risk of cardiovascular disease, it would not be appropriate to advise all such sufferers to avoid alcohol. As suggested by the authors of this paper, it may be reasonable for those subjects who had a desire to consume alcohol to drink small amounts of specific beverages to see if each beverage was tolerated or not. After seeing the effects, and factoring in symptoms versus potential benefits from moderate drinking, a reasonable discussion can be carried out with respect to continued alcohol use by subjects with migraine.
Reference: Panconesi A, Bartolozzi ML, Guidi L. Alcohol and migraine: What should we tell patients? Curr Pain Headache Rep 2011;15:177–184. DOI 10.1007/s11916-011-0184-4.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 043: Frequent moderate drinking of alcohol is associated with a lower risk of fatty liver disease. 23 May 2011
In a large study of men in Japan, the presence of fatty liver disease by ultrasonography showed an inverse association with the frequency of alcohol consumption; there was some suggestion of an increase in fatty liver disease with higher volume of alcohol consumed per day. Moderate drinkers had lower levels of obesity than did non-drinkers, and both obesity and metabolic abnormalities were positively associated with fatty liver disease.
These findings support the results of a number of other recent studies showing that moderate drinking does not increase the risk of this common type of liver disease; instead, it is associated with a lower risk of its occurrence. We agree with the implications of these studies as stated by the authors: “These results suggest that lifestyle modifications aimed at fighting central obesity and metabolic abnormalities should be the most important recommendations for the management of fatty liver. In addition, it seems unlikely that the risk of fatty liver can be reduced by the discontinuation and/or reduction of alcohol consumption alone.”
Reference: Hiramine Y, Imamura Y, Uto H, Koriyama C, Horiuchi M, Oketani M, Hosoyamada K, Kusano K, Ido A, Tsubouchi H. Alcohol drinking patterns and the risk of fatty liver in Japanese men. J Gastroenterol 2011 46:519–528. DOI 10.1007/s00535-010-0336-z.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 042: An increase in risk of certain types of gastric cancer from heavy drinking, but no increase from moderate alcohol consumption 17 May 2011
A very well-done meta-analysis supports other data generated on the risk of alcohol consumption and gastric cancer – that is – that the risk may be real for heavy alcohol consumption but not for moderate intake. The type of gastric cancer relating to heavier alcohol intake in this study tended to be tumors involving the noncardia, but differences between the association with tumors of the gastric cardia were not significant.
There was no increased risk of gastric cancer from alcohol among Asians; this may be due to lower alcohol intake; there is a greater prevalence among Asians of the inactive ALDH2 genotype that is associated with flushing and other adverse effects of alcohol, and such subjects tend to drink less alcohol. However, a number of studies have shown higher risk for upper aero-digestive cancers for subjects with this ALDH2 genotype, so the overall reason for the lower risk among Asians in this study remains unclear. The main outcome of the study is that there is no increase in the risk of gastric cancer associated with the moderate intake of alcohol.
Reference: Tramacere I, Negri E, Pelucchi C, Bagnardi V, Rota M, Scotti L, Islami F, Corrao G, La Vecchia C, Boffetta P. A meta-analysis on alcohol drinking and gastric cancer risk. Ann Oncology 2011;doi:10.1093/annonc/mdr135
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 041: Estimated health effects of changes in advice for alcohol consumption between the 2005 and 2010 Dietary Guidelines for Americans 6 May 2011
This paper from the National Institute on Alcohol Abuse and Alcoholism in the US suggests that the changes in wording of the alcohol recommendations in the Dietary Guidelines for Americans between 2005 and 2010 indicate that some at-risk drinkers could be classified as moderate drinkers. The authors carried out an analysis using data from a large, nationally representative sample of U.S. adults to estimate differences between subjects following the 2005 recommendations and a “gray zone” of subjects who exceed the 2005 recommendations but fall within the moderate guidelines according to the 2010 recommendations. The differences between these two groups were minimal; other than the gray zone subjects having an increased risk of alcohol dependence (which is unlikely to relate to their slight differences in consumption), the only other differences between the two groups related to alcohol-related interpersonal relations and job loss. And, as the authors state, “There were no associations with medical conditions or mental disorders.”
More importantly, the authors state that “Moreover, of the gray area drinkers who experienced incident alcohol dependence and interpersonal problems, 89% of the former and 94% of the latter had moved out of the gray area and into the highest-risk consumption group over the course of the follow-up interval.” Problems were thus very rare in those who remained in the gray zone of drinking during follow up.
Obviously, drinking 3 or 4 drinks/day (other than doing so only occasionally) should not be considered a healthy way to consume alcohol. But if, as the authors state, almost all of the estimated effects on health are due to subjects who increase their drinking above this “gray zone,” there is little support for their argument that the changes in guidelines make a difference.
Reference: Dawson DA, Grant BF. The “Gray Area” of consumption between moderate and risk drinking. J Stud Alcohol Drugs 2011;72:453–458.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 040: Lower risk of coronary heart disease from alcohol, even with heavy drinking 27 April 2011
Using data from The 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions study (the NESARC study, n = 43,093), the authors of this paper conclude that alcohol may have cardioprotective effects not only in moderate drinkers, but also in individuals with patterns of use traditionally considered as “hazardous.” While such a finding has been shown in some population studies, there were questions by Forum reviewers as to the adequacy of the method for diagnosing coronary artery disease: self-report, with most subjects listing angina pectoris, a “soft” criterion for coronary disease.
In addition, the categories of drinking used in this study were very broad: rare or only occasional drinkers were combined with regular drinkers up to 7 or 14 drinks per week in the “moderate” category; the “hazardous” category included a broad range of drinkers, from a minimal increase over the recommended limits to very heavy drinkers. The pattern of drinking (especially the number of days per week that alcohol was consumed) was not reported, making it difficult to separate regular from heavy week-end drinkers. The effects of heavier drinking on other conditions (such as alcohol-related liver disease, mortality, etc.) were not included in this analysis.
It is physiologically possible that even hazardous use of alcohol, like moderate use, may well lead to cleaner arteries and therefore lower rates of coronary artery disease. If this is the case, an explanation for the increases in cardiovascular mortality reported for heavy drinkers in many studies may relate not directly to coronary artery disease, but to conditions such as cardiomyopathy or cardiac arrhythmias. However, the rates of accidents, suicide and other morbidity associated with hazardous alcohol use may well overcome any protective effects on coronary disease.
Reference: Le Strat Y, Gorwood P. Hazardous drinking is associated with a lower risk of coronary heart disease: Results from a national representative sample. Am J Addict 2011;20:257–263.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 039: The role that alcohol drinking may play in the risk of cancer 17 April 2011
A large group of distinguished scientists have published a very detailed and rather complex paper describing the association between alcohol consumption and cancer. It is based on data from the EPIC study in Europe, with a mean follow up of 8.8 years for more than 300,000 subjects. The authors describe an increase in risk of many cancers from alcohol intake, but do not give data permitting the detection of a threshold of intake for an adverse effect on cancer risk. The investigators conclude that “In western Europe, an important proportion of cases of cancer can be attributable to alcohol consumption, especially consumption higher than the recommended upper limits.”
Members of the Forum were concerned that the authors did not separate moderate consumption from heavy consumption for their main analyses, ignored the demonstrated benefits of moderate drinking on total mortality, and did not point out other environmental influences (such as smoking, diet, obesity, etc.) that often have much larger effects on the risk of many cancers than does alcohol consumption. The authors make statements such as alcohol has negative effects on total mortality that are not supported by the data presented in their paper, and are contradicted by most large-scale population-based studies. Overall, while this paper supports the well-known association between heavy drinking and an increased risk of upper aero-digestive and certain other cancers, it adds little information useful for the prevention of most types of cancer.
Reference: Schűtze M, Boeing H, Pischon T, et al, Alcohol attributable burden of incidence of cancer in eight European countries based on results from prospective cohort study. BMJ 2011; 342:d1584 doi: 10.1136/bmj.d1584 (Published 7 April 2011)
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 038: Effects of a large reduction in alcohol prices on mortality in Finland 7 April 2011
Time series intervention analysis modeling was applied to the monthly aggregations of deaths in Finland for the period 1996–2006 to assess the impact of a reduction in alcohol prices in 2004. The authors report that alcohol-related deaths increased in men aged 40–49 years, and in men and women aged 50–69 years: the mean rate of alcohol-related mortality increased by 17%, 14%, and 40%, respectively, which implies 2.5, 2.9 and 1.6 additional monthly deaths per 100,000 person-years following the price reduction. In contrast to alcohol-related mortality, CVD and all-cause mortality decreased among men and women in the highest age category. The changes were consistent with 19 and 25 fewer monthly deaths per 100,000 person-years for CVD and 42 and 69 fewer monthly deaths for all-cause mortality.
Forum members agreed that both potentially harmful and beneficial effects resulting from changes in alcohol intake should be considered when estimating population effects. They were unsure whether all of the reported effects in the elderly should be attributed to changes in alcohol intake, as decreases in CVD and all-cause mortality rates were occurring prior to the change in alcohol intake.
Reference: Herttua K, Mäkelä P, Martikainen P. An evaluation of the impact of a large reduction in alcohol prices on alcohol-related and all-cause mortality: time series analysis of a population-based natural experiment. Int J Epidemiol 2011;40:441-454; doi:10.1093/ije/dyp336.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 037: Genes found to relate to level of alcohol consumption among Asians 27 March 2011
In a study of 1,721 Korean male drinkers aged 40–69 y in an urban population–based cohort, and another sample of 1,113 male drinkers from an independent rural cohort, information on average daily alcohol consumption was collected and DNA samples were collected for genotyping. In a genome-wide association (GWA) study, 12 single-nucleotide polymorphisms (SNPs) on chromosome 12q24 had genome-wide significant associations with alcohol consumption. These polymorphisms were closely related to genes that determine levels of ALDH, low levels of which relate to flushing after even small amounts of alcohol. Such enzymes are much more common among Asians than among westerners. Further, associations were tested only with the weekly amount of alcohol consumed, not the pattern of drinking; hence, these findings are not direct measures of alcoholism.
The editorial by Freedman et al states “epidemiologic literature suggests that those who begin drinking at an early age may be at greater risk for a maladaptive and more genetically pronounced form of alcohol consumption, and other environmental milieus affect the risk of alcoholism.” It will be important to investigate the interplay of genes and environmental factors when seeking the determinants of alcohol abuse. Despite the findings of this study, our understanding of factors associated with alcoholism remains very limited.
Reference: Baik I, Cho NH, Kim SH, Han B-G, Shin C. Genome-wide association studies identify genetic loci related to alcohol consumption in Korean men. Am J Clin Nutr 2011;93:809–816.
Accompanying Editorial: Agrawal A, Freedman ND, Bierut LJ. Genome-wide association studies of alcohol intake—a promising cocktail? Am J Clin Nutr 2011;93:681–683.
For the full critique of this article by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 036: Alcohol consumption after age 75 associated with lower risk of developing dementia
7 March 2011
A population-based study of elderly Germans, aged 75 and older, evaluated the association between alcohol consumption and incident overall dementia and Alzheimer dementia over 3 years. There was good ascertainment of the development of dementia, even among subjects who died during follow up.
Of 3,202 subjects free of dementia at baseline, 217 subjects met criteria of dementia during follow up. Subjects consuming alcohol had approximately 30% less overall dementia and 40% less Alzheimer dementia than did non-drinking subjects. Unlike many previous studies showing greater effects of wine on reducing risk of dementia, no significant differences were seen according to the type of alcoholic beverage consumed. Overall, these results are similar to several previous studies in the very elderly and suggest that moderate drinking is associated with less dementia, even among individuals aged 75 years and older.
Reference: Weyerer S, Schaufele M, Wiese B, Maier W, Tebarth F, van den Bussche H, Pentzek M, Bickel H, Luppa M, Riedel-Heller SG, for the German AgeCoDe Study Group (German Study on Ageing, Cognition and Dementia in Primary Care Patients). Current alcohol consumption and its relationship to incident dementia: results from a 3-year follow-up study among primary care attenders aged 75 years and older. Age and Ageing 2011; 0: 1–7; doi: 10.1093/ageing/afr007.
For the full critique of this article by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 035: A review of the association of alcohol consumption with cardiovascular disease outcomes 5 March 2011
In an excellent summary, the authors of this paper have synthesized results from longitudinal cohort studies comparing alcohol drinkers with non-drinkers for the outcomes of overall mortality and mortality from cardiovascular disease (CVD), incident coronary heart disease (CHD), mortality from CHD, incident stroke, and mortality from stroke. They conclude that light to moderate alcohol consumption is associated with a reduced risk of multiple cardiovascular outcomes. Further, they suggest that current scientific data satisfy Hill criteria indicating causality, that alcohol intake is the cause of the lower risk of cardiovascular disease among moderate drinkers.
Forum members thought that this was a very well-done, comprehensive summary of a large number of studies on alcohol and cardiovascular disease. Some believed that two topics were not adequately discussed: (1) greater benefits from wine than from other beverages, a result seen in many studies, and (2) the importance of the pattern of drinking on the health effects of alcohol. However, Forum members welcomed the discussion in the paper as to causality and regarding future directions in research, with more emphasis into how physicians and individual patients might respond to encouragement to consume alcohol for its potentially beneficial effects on cardiovascular disease. Most believe that there is no substitute for balanced judgment by a knowledgeable, objective health professional when discussing alcohol intake, and this requires is a synthesis of common sense and the best available scientific facts as they apply to the individual.
Reference: Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 2011;342:d671; doi:10.1136/bmj.d671
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 034: A review of interventional studies in humans showing effects of alcohol on risk factors for cardiovascular disease 5 March 2011
A summary paper on the effects of alcohol consumption on biologic mechanisms associated with coronary heart disease provides an excellent review of a large number of intervention studies in humans. Appropriate analyses were done and the results are presented in a very clear fashion, although there was little discussion of the separate, independent effects of alcohol and polyphenols on risk factors.
The trials the authors reviewed have demonstrated that the moderate intake of alcoholic beverages leads to increases in HDL-cholesterol, apolipoprotein A1, and adiponectin and decreases in fibrinogen, all factors associated with a lower risk of heart disease. The findings described in this paper strengthen the case for a causal link between alcohol intake and a reduced risk of coronary heart disease, suggesting that the lower risk of heart disease observed among moderate drinkers is caused by the alcoholic beverage itself, and not by other associated lifestyle factors.
Reference: Brien SE, Ronksley PE,Turner BJ, Mukamal KJ, Ghali WA. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ 2011;342:d636; doi:10.1136/bmj.d636.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 033: Moderate-to-heavy alcohol intake may increase risk of atrial fibrillation 12 February 2011
A number of well-done studies have shown an increase in the risk of atrial fibrillation to be associated with heavy alcohol intake or with alcoholism. Most previous studies suggest little if any increase in risk from light-to-moderate drinking. The present study was a meta-analysis based on 14 studies from Europe or North America. It showed an increase in risk with alcohol, but there were limited dose-response data to determine if there was a threshold above which the risk was increased.
Overall, the scientific evidence from many studies suggests that at least heavy drinking may increase the risk of atrial fibrillation, although whether light-to-moderate intake increases the risk seems unlikely. Previous basic scientific data of mechanisms of atrial fibrillation have suggested that alcohol has little effect on this arrhythmia.
Reference: Kodama S, Saito K, Tanaka S, Horikawa C, Saito A, Heianza Y, Anasako Y, Nishigaki Y, Yachi Y, Iida KT, Ohashi Y, Yamada N, Sone H. Alcohol consumption and risk of atrial fibrillation. A meta-analysis. J Am Coll Cardiol 2011;57:427–436.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 032: Comments on alcohol in newly released Dietary Guidelines for Americans, 2010 9 February 2011
The United States has released new Dietary Guidelines for Amercans, 2010. While the Key Recommendations regarding alcohol remain similar to those of earlier guidelines, there were some changes in the text that reflect increasing scientific data indicating potential health benefits of moderate drinking. The key recommendation is as follows:
“If alcohol is consumed, it should be consumed in moderation—up to one drink per day for women and two drinks per day for men—and only by adults of legal drinking age.”
Within the main body of the guidelines, comments on alcohol include the following:
“The consumption of alcohol can have beneficial or harmful effects, depending on the amount consumed, age, and other characteristics of the person consuming the alcohol. Alcohol consumption may have beneficial effects when consumed in moderation. Strong evidence from observational studies has shown that moderate alcohol consumption is associated with a lower risk of cardiovascular disease. Moderate alcohol consumption also is associated with reduced risk of all-cause mortality among middle-aged and older adults and may help to keep cognitive function intact with age. However, it is not recommended that anyone begin drinking or drink more frequently on the basis of potential health benefits because moderate alcohol intake also is associated with increased risk of breast cancer, violence, drowning, and injuries from falls and motor vehicle crashes.”
Reference: www.cnpp.usda.gov/Publications/DietaryGuidelines/2010/PolicyDoc/Chapter3.pdf
To see a copy of the section on alcohol from the new Dietary Guidelines, click here.
===============================================================================
Critique 031: Wine polyphenols have a variety of beneficial effects on health 30 January 2011
Much of the protection against cardiovascular disease attributed to wine intake may relate not only to the alcohol in wine, but to its polyphenolic constituents. This review article summarizes research into the chemistry, bioavailability, metabolism and excretion of polyphenols as well as mechanisms of their action. As stated by the authors, “These protective effects could be due to one or many components of the complex mixture of bioavailable and bioactive compounds present in red wine including ethanol, resveratrol, flavonols, flavan-3-ols, anthocyanins, phenolic acids as well as their metabolites formed either in the tissues or in the colon by the microflora.” The authors describe their cardioprotective effects, effects on vascular function and atherosclerosis, anti-platelet effects, effects on myocardial ischemia, and anti cancer and anti-diabetic effects.
The authors conclude that “Polyphenols are the most abundant antioxidants in the diet and are widespread constituents of wine, fruits and vegetables.” Their review provides an extensive scientific literature on polyphenols in wine; it suggests multiple mechanisms by which such substances may have beneficial effects on health.
Reference: Rodrigo R, Miranda A, Vergara L. Modulation of endogenous antioxidant system by wine polyphenols in human disease. Clin Chim Acta 2011;412:410-424
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research please click here.
===============================================================================
Critique 030: Young rats given red wine polyphenols show less deterioration in endothelial function with ageing. 30 January 2011
The gradual decrease in endothelial function over time is a key factor in the development of diseases associated with ageing, especially cardiovascular disease (CVD). Many epidemiologic studies suggest greater protection against CVD from wine than from other beverages containing alcohol, with at least one factor being the polyphenols in red wine (RWPs).
The present study in rats found that the administration of red wine polyphenols protected against ageing-induced endothelial dysfunction. As stated by the authors: “The present findings indicate that regular intake of RWPs in the drinking water starting at young age (16 week-old) prevented the aging-related endothelial dysfunction most likely by reducing the excessive oxidative stress in the arterial wall.” They further suggest an important role of NADPH oxidase and possibly also the angiotensin system in the abnormal vascular response in aging. Their study showed that, “RWPs intake had also a physiological beneficial effect since it improved the physical exercise capacity of old rats.”
Forum members thought that this was an excellent paper, as it begins to delve into mechanisms by which polyphenols improve health. A mechanism is addressed and results are consistent with the working hypothesis of a specific interaction between polyphenols and peculiar enzymes. There is a satisfying agreement between basic mechanisms and pathophysiology.
Some scientists believe that interventions to improve endothelial function (such as the consumption of red wine or other sources of polyphenols) should begin earlier in life to slow down the endothelial dysfunction that occurs with ageing. This study in rats tends to support such a belief.
Reference: Dal-Ros S, Zoll J, Lang AL, Auger C, Keller N, Bronner C, Geny B, Schini-Kerth VB. Chronic intake of red wine polyphenols by young rats prevents aging-induced endothelial dysfunction and decline in physical performance: Role of NADPH oxidase. Biochem Biophys Res Commun 2011;404:743-749
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 029: Differing opinions on the message to the public regarding alcohol consumption 16 January 2011
A Letter to the Editor entitled “What should we advise about alcohol consumption?” was recently published by Maurizio Ponz de Leon in Intern Emerg Med.1 Dr. de Leon argues that the message of health benefits of moderate drinking “seems to me hazardous and extremely dangerous to diffuse in the general population.” His reasons included (1) many people may be unable to distinguish between low–moderate and high consumption of wine, beer or spirits, and alcohol metabolism may differ remarkably from one subject to another; (2) alcohol remains a frequent cause of car crash, and governments (in almost all western countries) try to convince or force people to abstain from drinking before driving; and (3) to consider alcohol as a medication whose consumption may contribute to improved health is another source of concern. Dr. de Leon asks: “Are we truly at the point of prescribing alcohol consumption in order to reduce the risk of stroke and coronary damage?” He concluded that “more studies are needed before we can give sensible recommendations on alcohol consumption to the general population.”
The de Leon editorial has prompted considerable response from other scientists, including further Letters to the Editor of the journal by Di Castelnuovo, Costanzo, Donati, Iacoviello, and de Gaetano,2 and by Estruch and Lamuela-Raventos.3 In addition, the original editorial has stimulated considerable debate among members of the International Scientific Forum on Alcohol Research. Among key arguments presented by the Forum members, all experts in scientific research on alcohol, are that messages to the public should not be “paternalistic” (we will tell you what is best for you since you are not smart enough to understand the facts), and that guidelines must always be based on sound, balanced scientific data rather than on uninformed opinion. Forum members emphasized that there are certain people who should not drink at all (including former abusers of drugs or alcohol, people with certain medical conditions, children and adolescents, and people with religious or moral proscriptions against alcohol), and there can never be a general recommendation for everybody to consume alcohol. On the other hand, physicians should not withhold from their patients and the public scientifically sound and balanced data on alcohol and health. And the data are extremely strong supporting a role for moderate alcohol intake, for appropriate adults, for the reduction in risk of coronary artery disease and other diseases of ageing.
Several Forum members pointed out that it was unfortunate that the journal had chosen to publish the original letter that castigates alcohol from an author with good scientific credentials, but little to no apparent research expertise in the subject of alcohol and health. Many Forum members disagreed with the statement of de Leon that “Many people may be unable to distinguish between low–moderate and high consumption of wine, beer or spirits.” A leading scientist dealing with this subject for decades, Dr. Arthur Klatsky, has written: “Most people know very well what the difference is between light to moderate drinking and binge or excessive drinking. While some patients may rationalize their heavy drinking because of its purported health effects, I have yet to find someone who had developed alcohol abuse because of messages about the health effects of moderate drinking.” Medical practitioners, in his view, “have a ‘solemn duty’ to tell the truth about alcohol consumption, as they understand it, to all of their patients.” While pointing out that certain individuals will not benefit from the consumption of alcohol, several Forum members believed that it would be unethical for physicians to withhold from middle-aged or elderly subjects at risk of cardiovascular disease information on the potential benefits of light-to-moderate drinking
References:
- Maurizio Ponz de Leon. What should we advise about alcohol consumption? Intern Emerg Med, DOI 10.1007/s11739-010-0487-1.
- Augusto Di Castelnuovo, Simona Costanzo, Maria Benedetta Donati, Licia Iacoviello, Giovanni de Gaetano. What should we advise about alcohol consumption? Reply letter by A. Di Castelnuovo. Intern Emerg Med, DOI 10.1007/s11739-010-0502-6.
- Ramon Estruch • Rosa Ma Lamuela-Raventos. What should we advise about alcohol consumption: reply letter by R. Estruch. Intern Emerg Med; DOI 10.1007/s11739-010-0503-5.
For the full critique of these publications by members of the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 028: Changes over time in relation of social class to mortality from cirrhosis 9 January 2011
To explore the nature of the social class gradient of cirrhosis mortality in England and Wales across the 20th century, data on male cirrhosis mortality by social class were obtained from the Registrar General’s Decennial Supplements for the years 1921–1991. This paper describes a dramatic change during the 20th century in the association between social class and mortality from liver cirrhosis. While deaths from cirrhosis were more common among higher social classes in the early part of the century, the pattern changed so that deaths from cirrhosis were much more common among the lower social classes by the end of the century.
Suggested reasons for the lower current rates among subjects at higher social class include different patterns of alcohol consumption, with regular moderate consumption (especially of wine with meals) becoming more common with higher social class subjects while binge drinking (especially of beer and spirits) remaining more common in lower social classes. However, a number of other factors may relate to the class differences in rates of hepatic cirrhosis, including a less healthy diet and greater rates of obesity (associated with hepatic fatty liver and cirrhosis) among lower social class subjects and social class differences in hepatitis rates. Further, certain medications, coffee consumption, and many other lifestyle factors are associated with hepatic cirrhosis. The actual reasons for the changes over time reported in this paper remain unclear.
Reference: Crombie IK, Precious E. Changes in the social class gradient of cirrhosis mortality in England and Wales across the 20th century. Alcohol and Alcoholism 2011;46:80–82.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 027: Effects of resveratrol and quercetin on inflammation and insulin resistance – 20 December 2010
A study was carried out to examine the extent to which quercetin and trans-resveratrol (RSV) prevented inflammation or insulin resistance in primary cultures of human adipocytes treated with tumor necrosis factor-a (TNF-a)—an inflammatory cytokine elevated in the plasma and adipose tissue of obese, diabetic individuals. Cultures of human adipocytes were pretreated with quercetin and trans-RSV followed by treatment with TNF-a. Subsequently, gene and protein markers of inflammation and insulin resistance were measured. The authors report that quercetin, and to a lesser extent trans-RSV, attenuated the TNF-a–induced expression of inflammatory genes such as interleukin (IL)-6, IL-1b, IL-8, and monocyte chemoattractant protein-1 (MCP-1) and the secretion of IL-6, IL-8, and MCP-1.
Forum members were concerned about certain aspects of the study, especially the extrapolation of in vitro results to in vivo situations. The in vitro conditions the authors describe are minimally representative of an in vivo condition. In vivo, after consumption of quercetin or resveratrol, these compounds undergo extensive metabolism, leading to glucuronidated, sulphated or methylated compounds. In a previous study, quercetin 3-glucoside was transformed to 3,4-dihydroxyphenylacetic acid, acetate and butyrate in cells from human gut; only 3′-methylquercetin has been detected in human plasma, present at a concentration of 0.1 to 0.2 µM after 3 h. The authors of the current paper are using concentrations up to 60 µM, concentrations which have not been found in vivo.
There were also concerns with the work on cell uptake of quercetin and resveratrol. Primary adipocytes were incubated with the polyphenols, but it is not clear whether or not the concentrations used were subtoxic. Our current knowledge is limited about local concentration of the molecules we are studying in subcellular compartments, their interaction with alternative targets, and eventually their transformation into products that could be more or less active on a given specific pathway. The real difficult and important issue is the identification of a reasonable convergence — if not agreement — between data originating from extremely distant approaches. In this case, the notion that metabolic diseases are related to a homeostatic imbalance in adipose tissue, linked to a different redox status, linked to activation of specific pathways, and that different redox sensitive polyphenols do have a protective effect, encompasses the evidence produced by extremely distant approaches.
From a clinical point of view, the role of phytochemicals acting as antioxidants and anti-inflammatory agents could be extremely important in inflammation-associated chronic conditions such as cardiovascular disease, diabetes, and cancer. Quercetin and resveratrol may indeed play an important role in this regard, and need to be investigated further to establish the clinical importance of natural dietary compounds in the prevention of chronic degenerative conditions.
Reference: Chuang C-C, Martinez K, Xie G, Kennedy A, Bumrungpert A, Overman A, Jia W, McIntosh MK. Quercetin is equally or more effective than resveratrol in attenuating tumor necrosis factor-a–mediated inflammation and insulin resistance in primary human adipocytes. Am J Clin Nutr 2010;92:1511–1521.
For the full critique of this paper by the International Scientific Forum on Alcohol Research please click here.
===============================================================================
Critique 026: Chinese study suggests that alcohol increases angiographically significant coronary artery disease 8 December 2010
Among a large number of Chinese men presenting with chest pain or EKG changes, sequential subjects undergoing cardiac angiography were evaluated for obstructive coronary artery disease (CAD) lesions according to their reported recent alcohol intake. The study population consisted of 1,476 consecutive men 36 to 84 years of age; participants were categorized as nondrinkers, light drinkers, moderate drinkers, or heavy drinkers.
Adjusted odds ratios for angiographically proved CAD for light, moderate, and heavy drinking were 1.16 (95% confidence interval 0.68 to 1.94), 1.78 (1.35 to 2.27), and 2.18 (1.46 to 3.25). Compared to non-drinking, adjusted odds ratios were 1.03 (0.54 to 1.87) for drinking 0 to 15 years, 1.61 (1.28 to 2.14) for 16 to 30 years, and 1.98 (1.23 to 3.05) for >30 years. The authors concluded that moderate-to-heavy alcohol consumption increased the risk of CAD in Chinese men. CAD risk tended to increase with an increase in frequency and duration of drinking.
This was a very select group of patients (those presenting with chest pain or EKG changes), and not typical of the Chinese population. No information was available on drinking patterns or on previous alcohol intake. Further, a recent large population-based study from mainland China showed that consumers of alcohol were less likely to develop coronary disease, results similar to those in most Western populations. It is not possible from the present study to say that the association of alcohol intake with CAD is different between Chinese and Western populations, as the present study gives results only for a very select group of patients.
The most important outcome regarding CAD is the occurrence of clinical events (myocardial infarction, cardiac death, etc.). The detection of such events requires long-term follow-up studies to be able to judge the overall effects of alcohol drinking on CAD.
Reference: Zhou X, Li C, Xu W, Hong X, Chen J. Relation of alcohol consumption to angiographically proved coronary artery disease in Chinese men. Am J Cardiol 2010;106:1101–1103.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 025: Pattern of drinking and type of beverage affect the relation of alcohol intake to coronary heart disease 1 December 2010
Using cohort data from Belfast and France, investigators related weekly alcohol consumption, incidence of binge drinking (alcohol >50 g on at least one day a week), incidence of regular drinking (at least one day a week, and alcohol <50 g if on only one occasion), volume of alcohol intake, frequency of consumption, and types of beverage consumed to risk of coronary heart disease (CHD) events over a 10 year follow-up period. Overall, 60.5% of subjects from N. Ireland and 90.6% of French reported drinking alcohol at least once a week. Among drinkers, 12% of men in Belfast drank alcohol every day compared with 75% of men in France. Mean alcohol consumption was 22.1 g/ day in Belfast and 32.8 g/day in France. Binge drinkers comprised 9.4% and 0.5% of the Belfast and France samples, respectively.
Results showed that, after multivariate adjustment, the hazard ratio for hard coronary events compared with regular drinkers was 1.97 (95% CI 1.21 – 3.22) for binge drinkers, 2.03 (95% CI 1.41 – 2.94) for never drinkers, and 1.57 (95% CI 1.11 – 2.21) for former drinkers. The hazard ratio for hard coronary events in Belfast compared with in France was 1.76 (95% CI 1.37 to 2.67) before adjustment, and 1.09 (95% CI 0.79 to 1.50) after adjustment for alcohol patterns and wine drinking. Only wine drinking was associated with a lower risk of hard coronary events, irrespective of the country.
The authors conclude that regular and moderate alcohol intake throughout the week, the typical pattern in middle-aged men in France, is associated with a low risk of ischemic heart disease, whereas the binge drinking pattern more prevalent in Belfast confers a higher risk.
While a strong inverse association between moderate alcohol consumption and cardiovascular disease has been demonstrated for decades, more recent research has emphasized the importance of the pattern of drinking (regular moderate versus episodic or binge drinking). Further, there continues to be debate about the potential greater effect of wine versus other beverages containing alcohol. This study shows that regular moderate drinking (especially of wine) is associated with lower risk of MI, but episodic or binge drinking (especially of beer or whiskey) increases the risk. Lifetime abstinence has a similar adverse relation to CHD as does episodic or binge drinking.
Reference: Ruidavets J-B, Ducimetièere P, Evans A, Montaye M, Haas B, Bingham A, Yarnell J, Amouyel P, Arveiler D, Kee F, Bongard V, Ferrières J. Patterns of alcohol consumption and ischaemic heart disease in culturally divergent countries: the Prospective Epidemiological Study of Myocardial Infarction (PRIME). BMJ 2010;341:c6077 doi:10.1136/bmj.c6077.
For the detailed critique of this study by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 024: Moderate alcohol consumption lowers risk of metabolic diseases in a population with high mean alcohol intake. 28 November 2010
A cross-sectional analysis of data from subjects in Switzerland related varying levels of alcohol intake to the presence of diabetes mellitus, the “metabolic syndrome,” and an index of insulin resistance (HOMA-IR). The strengths of this paper include being population-based and having a large number of subjects who reported that they consumed 14 or more drinks/week. Also, there was a good percentage (27%) of subjects reporting no alcohol intake during the one week of assessment used for classifying subjects. Another strength is the careful confirmation of drinking status with state-of-the-art laboratory tests. In multivariate analysis, the prevalence of the metabolic syndrome, diabetes and mean HOMA-IR decreased with low-risk drinking and increased with high-risk drinking. No differences were noted according to the type of beverage consumed.
This is a cross-sectional analysis, so a causative relation between alcohol intake and the metabolic outcomes cannot be assessed. Still, the data support much that has been shown in prospective studies. Several Forum members commented on potential problems when considering a number of physiologic conditions as the “metabolic syndrome” and focusing therapy on the syndrome; they believed that each metabolic factor should be evaluated and treated singly.
Reference: Clerc O, Nanchen D, Cornuz J, Marques-Vidal P, Gmel G, Daeppen J-B, Paccaud F, Mooser V, Waeber G, Vollenweider P, Rodondi N. Alcohol drinking, the metabolic syndrome and diabetes in a population with high mean alcohol consumption. Diabet Med 2010;27:1241–1249.
For the detailed critique of this study by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 023: Evidence that PPAR-gamma is a mechanism for the effects of wine polyphenolics on cardiovascular risk. 27 November 2010
It is important that biological mechanisms are identified for the observed inverse relation between the moderate consumption of wine and cardiovascular disease shown in most epidemiologic studies. A paper by Zoechling et al is an elegant example of the needed effort to provide a biochemical mechanism for the biological effects of wine. Data on binding of different wine component were produced and this result is interpreted in light of epidemiological evidence.
It would have been appropriate to provide evidence also for the actual shift of gene expression primed by the same wine component in a cell or animal model. In this respect, results must be rated appropriate but still as preliminary; a ligand could have different effects. Further, biological evidence is not provided to support the contention that these polyphenols act through the PPAR-gamma receptor. The sort of evidence that should have been provided is a comparison with rosiglitazone in a cell population known to respond to PPAR-gamma agonists (e.g. adipocytes).
Further, the analytical data does not describe the amounts of any of the “active” substances. So while there is a lot of discussion of the active components, it is not possible to compare any wine’s “activity” with the amount of the key substances. Lacking such a comparison, it is very hard to conclude that these substances are in fact the responsible factors in the observed activity.
Nevertheless, this paper provides important data on potential mechanisms by which the constituents of wine and certain other beverages may act to reduce the risk of cardiovascular disease.
Reference: Zoechling A, Liebner F, Jungbauer A. Red wine: A source of potent ligands for peroxisome proliferator-activated receptor γ. Food & Function, Journal of the Royal Society of Chemistry, in press. DOI: 10.1039/c0fo00086h.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 022: Alcohol consumption decreases with the development of disease — 21 November 2010
In a cross-sectional study from the 2004 and 2007 Australian National Drug Strategy Household (NDSH) surveys, respondents were questioned about their current and past drinking, the presence of formal diagnosis for specific diseases (heart disease, type 2 diabetes, hypertension, cancer, anxiety, depression) and self-perceived general health status. The sample sizes for the 2004 and 2007 NDSH surveys were 24,109 and 23,356, respectively.
The authors report that respondents with a diagnosis of diabetes, hypertension, or anxiety were more likely to have reduced or stopped alcohol consumption in the past 12 months. The likelihood of having reduced or ceased alcohol consumption in the past 12 months increased as perceived general health status declined from excellent to poor (although the authors do not point out that lifetime abstainers were more likely than moderate drinkers to report less than excellent health status).
The authors conclude that the experience of ill health is associated with subsequent reduction or cessation of alcohol consumption (“sick quitters), which is consistent with most prospective epidemiologic studies. The authors also conclude that this may at least partly underlie the observed ‘J-shaped’ function relating alcohol consumption to premature mortality. On the other hand, most modern epidemiologic studies are careful not to include “sick quitters” within the non-drinking category, and relate health effects of drinkers with those of lifetime abstainers. Further, prospective studies in which alcohol intake is assessed at different times (rather than having “changes” based only on recall at one point in time, as was done in this study) usually indicate that subjects who decrease their intake are more likely to subsequently develop adverse health outcomes, especially related to cardiovascular disease, than those who continue moderate drinking.
Reference: Liang W, Chikritzhs T. Reduction in alcohol consumption and health status. Addiction 2010; in press (doi:10.1111/j.1360-0443.2010.03164.x).
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 021: Alcohol consumption affects risk of cataracts 25 October 2010
A population-based prospective study from Australia utilized repeated lens photographs over a period of 5 to 10 years to diagnose cataracts among more than 2,500 subjects. The investigators related the risk of their development, and the risk of cataract surgery, to the reported alcohol intake of subjects. Previous research has provided some biological mechanisms that make an association between alcohol and cataracts plausible.
Overall, the present study showed few statistically significant relations between alcohol and cataracts, although adjusted results suggested a “U-shaped” association between total alcohol intake and development of cataracts (a lower risk for moderate drinkers, higher risk for both abstainers and heavier drinkers). The U-shaped association with alcohol consumption was stronger for the risk of cataract surgery. These results are consistent with previous cohort studies. On inspection of the data presented, the potential reduction in risk of cataract was primarily for wine and beer. While some types of cataract may be reduced by moderate drinking, larger intake of alcohol may be associated with increased risk.
Reference: Kanthan GL, Mitchell P, Burlutsky G, Wang JJ. Alcohol Consumption and the Long-Term Incidence of Cataract and Cataract Surgery: The Blue Mountains Study. Am J Ophthalmol 2010;150:434–440.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 20: New data on effects of alcohol during pregnancy 12 October 2010
A very large population-based observational study from the UK found that at the age of 5 years, the children of women who reported light (no more than 1-2 units of alcohol per week or per occasion) drinking did not show any evidence of impairment on testing for behavioral and emotional problems or cognitive ability. There was a tendency for the male children of women reporting “heavy/binge” drinking during pregnancy (7 or more units per week or 6 or more units per occasion) to have poorer behavioral scores, but the effects were less clear among female offspring.
Scientific data continue to indicate that higher intake of alcohol during pregnancy may adversely affect the fetus, and could lead to very severe developmental or other problems in the child. However, most recent publications (as does this one) show little or no effects of occasional or light drinking by the mother during pregnancy. They also demonstrate how socio-economic, education, and other lifestyle factors of the mother may have large effects on the health of the fetus and child; these must be considered when evaluating the potential effects of alcohol during pregnancy.
Overall, current scientific data indicate that while drinking during pregnancy should not be encouraged, there is little evidence to suggest that an occasional drink or light drinking by the mother is associated with harm. Heavy drinking, however, may be associated with serious developmental defects in the fetus.
Reference: Kelly YJ, Sacker A, Gray R, Kelly J, Wolke D, Head J, Quigley MA. Light drinking during pregnancy: still no increased risk for socioemotional difficulties or cognitive deficits at 5 years of age? J Epidemiol Community Health 2010; doi:10.1136/jech.2009.103002
Addendum: After the above critique was prepared, a new paper has been published on the topic by O’Leary et al (O’Leary CM, Nassar N, Kurinczuk JJ, de Klerk N, Geelhoed E, Elliott EJ, Bower C. Prenatal Alcohol Exposure and Risk of Birth Defects Pediatrics 2010;126;e843-e850; DOI: 10.1542/peds.2010-0256). Overall, the results of that study are similar to those of the study by Kelly et al, with no increase in risk of birth defects in children born of women reporting low or moderate drinking during pregnancy but with an increased risk of defects among children of women reporting heavy drinking.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 019: Both alcohol and caffeinated coffee intake are associated with lower risk of diabetes in African-American women. 27 September 2010
In a very large cohort of African-American women in the US, the association between the consumption of alcohol, tea, and coffee was related to the development of type 2 diabetes mellitus over a follow-up period averaging 12 years. Tea and decaffeinated coffee showed no relation with diabetes, but the intake of both caffeinated coffee and alcohol showed a significant inverse association.
This paper is particularly important because some previous studies have not shown a strong association between alcohol and the risk of cardiovascular disease among African-Americans. African-Americans, especially women, tend to drink little alcohol, yet are at markedly increased risk of diabetes. In the present study, the approximately 30% lower risk for moderate alcohol drinkers was about the same in these African-American women as has been found in many previous studies of whites.
Reference
Boggs DA, Rosenberg L, Ruiz-Narvaez EA, Palmer JR. Coffee, tea, and alcohol intake in relation to risk of type 2 diabetes in African American women. Am J Clin Nutr 2010;92:960–966.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 018: Alcohol consumption following diagnosis of early-stage breast cancer may increase risk of recurrence of cancer but not total mortality risk 14 September 2010
In the Life After Cancer Epidemiology (LACE) study, 1,897 participants diagnosed with early-stage breast cancer between 1997 and 2000 and recruited on average 2 years post-breast cancer diagnosis were evaluated for the association between alcohol intake and breast cancer recurrence and death. The women, who were generally light drinkers, were followed for an average of 7.4 years. The study reported an increase in risk of breast cancer recurrence and breast cancer death, but no effect on total mortality, to be associated with consumption of 3 to 4 or more drinks per week when compared with women not drinking following their cancer diagnosis.
Previous research has been mixed on this topic. Almost all large studies have shown no increase in all-cause mortality for women who drink moderately following a diagnosis of breast cancer (as does this study). As for recurrence of breast cancer, most have shown no increase in risk, although one previous study of women with estrogen-receptor + tumors found an increased risk of a primary cancer developing in the contralateral breast to be associated with alcohol intake of more than 7 drinks per week.
Because of conflicting results among studies on this topic, further research will be needed to determine the extent to which alcohol following a diagnosis of breast cancer may relate to subsequent disease and death.
Reference: Kwan ML, Kushi LH, Weltzien E, Tam EK, Castillo A, Sweeney C, Caan BJ. Alcohol Consumption and Breast Cancer Recurrence and Survival Among Women With Early-Stage Breast Cancer:The Life After Cancer Epidemiology Study. J Clin Oncol 2010;28 (published ahead of print, 10.1200/JCO.2010.29.2730)
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 017: Moderate alcohol intake is associated with a lower risk of total mortality than are either abstinence or heavy drinking 5 September 2010
In a study based on data from 1,824 predominantly Caucasian Americans from the Western part of the United States, alcohol consumption at baseline was related to mortality risk during a 20-year follow-up period. Subjects were recruited into a longitudinal project that has examined late-life patterns of alcohol consumption and drinking problems. Lifetime abstainers were not included in the study, which focused on stress and coping processes among problem drinkers and non-problem drinkers. The sample at baseline included only subjects aged 55 to 65 years who had had outpatient contact with a health care facility in the previous 3 years.
The database at baseline included information on daily alcohol consumption, sociodemographic factors, former problem drinking status, health factors, and social-behavioral factors. Subjects who were not lifetime abstainers but did not report drinking at the time of the baseline examination were classified as “abstainers.” Data on potential changes in alcohol consumption during the course of the study were not collected. Death during follow up was confirmed primarily by death certificate.
The key results of the paper are that even when adjusting for sociodemographic factors, former problem drinking status, health factors, and social-behavioral factors, moderate drinking was associated with considerably lower risk of all-cause mortality. In comparison with “moderate drinkers” (subjects reporting up to 3 drinks/day), abstainers had 51 % higher mortality risk and heavy drinkers had 45% higher risk. The study supports most previous scientific studies showing that moderate drinking, in comparison with both abstinence and heavy drinking, is associated with lower risk of total mortality.
Reference: Holahan CJ, Schutte KK, Brennan PL, Holahan CK, Moos BS, Moos RH. Late-Life Alcohol Consumption and 20-Year Mortality. Alcoholism: Clinical and Experimental Research 2010;34:in press, November 2010
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 016: Association of alcohol with breast cancer risk varies according to subtype of tumor
29 August 2010
Most studies show a slight increase in the risk of breast cancer for women who consume alcohol. The association is thought to relate to alcohol’s effects on hormones, and alcohol use tends to be more strongly associated with hormonally sensitive breast cancers than tumors not sensitive to hormones. Few studies have evaluated how alcohol-related risk varies by breast cancer subtype. In the present study, follow-up data from 87,724 women in the Women’s Health Initiative Observational Study prospective cohort were evaluated for the relation of baseline alcohol consumption with subsequent breast cancer.
A total of 2,944 invasive breast cancer patients were diagnosed during follow up. In multivariable-adjusted analyses alcohol consumption was associated with an increase in the risk of lobular carcinoma (which makes up approximately 15-20% of breast cancers), but there was not a statistically significant association with the more-common ductal type of carcinoma. Hormone + cancers showed an association with alcohol intake, but not hormone – cancers. The findings support the importance of hormonal mechanisms in mediating the relation between alcohol use and breast cancer risk.
Reference Li CI, Chlebowski RT, Freiberg M, Johnson KC, Kuller L, Lane D, Lessin L, O’Sullivan MJ, Wactawski-Wende J, Yasmeen S, Prentice R. Alcohol consumption and risk of postmenopausal breast cancer by subtype: the Women’s Health Initiative Observational Study. J Natl Cancer Inst 2010 Aug 23. [Epub ahead of print]
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here : Critique 016.
===============================================================================
Critique 015: Moderate drinking does not appear to increase risk of breast cancer among women with a BRCA gene mutation 22 August 2010
A large study was carried out to assess the effects of alcohol consumption on breast cancer risk among women with a BRCA1 or a BRCA2 gene mutation, both of which markedly increase the risk of breast cancer. Comparisons were made between women with a gene mutation who had developed invasive breast cancer matched with women with the same gene mutation who had not developed breast cancer. After a number of appropriate exclusions, there were 1,480 matched pairs with BRCA1 mutations and 445 pairs with BRCA2 mutations.
Data from the study support an earlier report suggesting no increase in breast cancer risk from alcohol intake for women with either gene mutation. In the previous study on this topic, a slight lowering of breast cancer risk was noted with light drinking among women with the BRCA2 mutation but not among those with the BRCA1 mutation. In the present study, a possible reduction in risk of breast cancer was seen for moderately drinking women with the BRCA1 mutation, but not the BRCA2 mutation. Further, in the present study, the reduction is risk of breast cancer was seen only for wine consumers. While one should not over-interpret epidemiologic data in the absence of identified biologic mechanisms, there have been a very large number of experimental studies showing that certain polyphenols present in wine actively impede the initiation and growth of cancer cells.
Overall, current scientific data suggest that alcohol in moderation does not increase the risk of breast cancer among women with a BRCA mutation, and wine may be somewhat protective. If this is indeed the case and given the high risk associated with these genetic mutations, it would be important to inform women with such a mutation that moderate alcohol does not appear to increase their risk of breast cancer.
Reference: Dennis J, Ghadirian P, Little J, et al: The Hereditary Breast Cancer Clinical Study Group. Alcohol consumption and the risk of breast cancer among BRCA1 and BRCA2 mutation carriers. The Breast 2010; e-pub.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here.
=========================================================================
Critique 014: Moderate drinking, especially of wine, is associated with better cognitive function 13 August 2010
A large prospective study of men and women in northern Norway reported that moderate wine consumption was independently associated with better performance on cognitive tests after 7 years of follow up. There was no consistent association between consumption of beer or spirits and cognitive test results. The authors also reported that abstinence was associated with significantly lower cognitive performance in women. As noted by the authors, in any observational study there is the possibility of residual confounding by other lifestyle habits affecting cognitive function, and the present study was not able to adjust for certain ones (e.g., diet, income, or profession) but did adjust for age, education, body mass index, depression, and cardiovascular disease and its major risk factors.
The results of this study support findings from a number of observational, prospective studies that have shown that the moderate consumption of alcohol, especially of wine, may have favorable effects on cognitive function. Such effects could relate to the presence in wine of a number of polyphenols and other substances that reduce the risk of cognitive decline with ageing. Mechanisms that have been suggested for such protection against cognitive dysfunction include effects on atherosclerosis, coagulation, inflammation, as well as direct neuroprotective effects.
Reference: Arntzen KA, Schirmer H, Wilsgaard T, Mathiesen EB. Moderate wine consumption is associated with better cognitive test results: a 7 year follow up of 5033 subjects in the Tromsø Study. Acta Neurol Scandd 2010; Suppl 190:23-29.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 013: Greater than moderate alcohol intake increases the risk of liver cirrhosis 27 July 2010
A new meta-analysis shows that alcohol consumption is a strong factor in the development of cirrhosis of the liver. The study also supports the theory that there is a threshold of drinking above which the risk is increased, as some of their analyses suggest that the risk increases only with intake of more than 24 grams/day of alcohol for women (about 2 typical drinks by US standards) and 36 grams/day of alcohol for men (about 3 typical US drinks).
Despite some concerns about the approach used, our Forum agrees that the present meta-analysis supports previous studies indicating a strong role of heavy alcohol drinking in the development of cirrhosis. The differences found by the investigators between the effects of moderate alcohol intake on cirrhosis morbidity and on cirrhosis mortality are difficult to explain, but may relate to misclassification of alcohol intake (heavy drinkers reporting less alcohol), always a problem in observational studies of the effects of alcohol.
The results related to morbidity suggest that small amounts of alcohol are not associated with an increased risk of cirrhosis, and may be associated with lower risk of disease. Thus, the data provide evidence for a “threshold effect” of alcohol intake for the development of cirrhosis. Limited previous data are available suggesting that wine consumption may be associated with lower risk of cirrhosis than the intake of other beverages, but essentially all studies show heavy drinking of any type of beverage increases the risk.
Reference: Rehm J, Taylor B, Patra SM, Irving H, Baliunas D, Patra J, Roerecke M. Alcohol as a risk factor for liver cirrhosis: A systematic review and meta-analysis. Drug and Alcohol Review 2010,29,437–445. DOI: 10.1111/j.1465-3362.2009.00153.x
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 012: Moderate drinking in the elderly is associated with lower total mortality 23 July 2010
The effects of alcohol consumption in the elderly may be modified by a decreased ability to metabolize alcohol, an altered volume of distribution due to reduced lean body mass and total body water, and an increased prevalence of co-morbid conditions. These factors make this study of the net effects of drinking among a large number of community-dwelling elderly men and women especially important.
In large prospective studies from Australia of men aged 60-79 and women aged 70-75 years of age, men consuming up to 4 drinks/day and women up to 2 drinks/day had considerably lower risk of dying (total mortality) than did non-drinkers. For subjects reporting 1-2 drinks/day, their total mortality risk was about 20-30% lower than that of abstainers.
While the authors concluded that not consuming alcohol on 1 or 2 days per week was associated with better outcomes, this conclusion is not in accordance with their own data. The benefit of one or two “alcohol-free” days per week has never been substantiated with solid evidence from any large epidemiological study.
Our Forum review concludes that in terms of total mortality risk, recommendations for very low levels of drinking among the elderly may be overly restrictive, as this study showed lower total mortality for up to 4 drinks/day for elderly men and 2 drinks/day for elderly women. Further, this study does not provide support for the conclusion that mortality is lower for people who have 1 or 2 “alcohol-free” days per week.
Reference: McCaul KA, Almeida OP, Hankey GJ, Jamrozik K, Byles JE, Flicker L. Alcohol use and mortality in older men and women. Addiction 2010. On-line prior to publication: doi:10.1111/j.1360-0443.2010.02972.x
For the full critique of this paper by the International Scientific Forum on Alcohol Research, click here
===============================================================================
Critique 011: A Review of the Proposed New US Dietary Guidelines 14 July 2010
Members of our International Scientific Forum on Alcohol Research have submitted a detailed review of the draft recently circulated by the United States Department of Agriculture for proposed new US Dietary Guidelines for 2010. In general, Forum members were very pleased with the alcohol recommendations in the proposal, finding them interesting, balanced, and accurate. Many commented that, rather than just focusing on warnings against heavy drinking, the new Guidelines appear to take into account the large amount of recent epidemiologic and experimental data that support many potential beneficial health effects of moderate drinking.
Among specific recommendations from the Forum were the following:
■ A stronger statement is needed of the effects of light-to-moderate drinking on total mortality, in that recent prospective studies show a considerably lower of risk of death for moderate drinkers.
■ Additional emphasis is needed on the reduced risk of developing diabetes for moderate drinkers, and the much lower risk of cardiovascular disease among diabetics who consume some alcohol.
■ Further information should be presented on the consistent scientific data showing that women who drink moderately are at reduced, not increased, risk of weight gain in adult life.
There were a number of topics not discussed in the draft Guidelines that members of the Forum thought deserved consideration for inclusion.
■ Recent reports have consistently shown that among people who have already had a myocardial infarction or other cardiovascular event, moderate drinking is associated with a reduced risk of further cardiovascular events and death.
■ More emphasis in the Guidelines should be put on the pattern of drinking (regular moderate rather than occasional binge drinking) and also on the much lower blood alcohol levels after drinking when the beverage is consumed with food, rather than on an empty stomach.
■ It was also suggested to the Guidelines Committee that the beneficial effects on cardiovascular risk of polyphenols and other substances in wine and certain beers, in addition to alcohol, be discussed more adequately.
There were also some suggestions from ISFAR regarding future research needs in the field.
■ The Forum strongly supports the need for further research on the risks and benefits of light-to-moderate alcohol consumption, rather than focusing research only on alcohol abuse.
■ The Forum proposed emphasis on future research dealing with targeting recommendations for groups of people according to age, gender, other behaviors, etc., although there was some disagreement among Forum members as to whether or not moderate drinking has strong health effects in the young and not just in middle-aged and older adults.
■ ISFAR considers moderate drinking, unless contraindicated by certain conditions (e.g, former abuse, some types of severe liver disease), to be an important aspect of a healthy lifestyle. It should be a complement, not an alternative, to other lifestyle factors such as not smoking, getting exercise, eating a healthy diet, and avoiding obesity.
The draft of the proposed new Dietary Guidelines is available at http://www.cnpp.usda.gov/DGAs2010-DGACReport.htm.
For the full ISFAR critique of the proposed new Guidelines, click here
===============================================================================
Summary Critique 010 30 June 2010
Should moderate alcohol consumption be advised following a heart attack?
There has been considerable recent interest in the effects of alcohol consumption following an acute myocardial infarction (AMI). In an observational study among 325 subjects who were moderate drinkers prior to an AMI, 84% continued to drink and 16% quit. While most of the outcome measures showed no statistically significant effects between the two groups of patients, all outcomes showed a tendency towards better physical and mental health outcomes for persistent drinkers in comparison with those who quit drinking.
A key problem with this analysis, and with all observational epidemiologic studies on this topic, is that the reason that some subjects stopped drinking after having an AMI, while others continued to drink, is not known. Even though adjustments were made for many known related factors, there is always the possibility that subjects who stopped drinking were “sicker” in many ways than those who persisted in their alcohol consumption.
It may well require a randomized trial, in which some subjects having an AMI are randomly advised to continue to drink and others advised to stop drinking, to be able to determine reliably the effects on the clinical course of the persistence of alcohol intake following an AMI.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: Critique 010
===============================================================================
Summary: Critique 009 25 June 2010
Should moderate alcohol consumption be advised for its health effects?
A report from a conference that took place at the Medicine Grand Rounds at Beth Israel Deaconess Medical Center, Boston, Massachusetts, on January 15, 2009 has recently been published in the Journal of the American Medical Association, JAMA. It provides a discussion by an epidemiologist with a broad knowledge in the field in response to a theoretical question, as from a middle-aged patient, as to the advisability of consuming some alcohol “for his health.”
The paper provides an excellent discussion of a theoretical question about drinking and health. It focuses on the potential risks and benefits associated with moderate drinking for a middle-aged male patient. Most members of the International Scientific Forum on Alcohol Research (ISFAR) were pleased with the discussion of the topic. It was noted how uncommon it is that such knowledgeable, detailed, and mostly objective data appear in the mainstream medical literature. It was thought to be “readable, informative and thoughtful.”
The ISFAR critique points out a number of topics that were covered incompletely in the paper, including inadequate information on the importance of the pattern of drinking: moderate regular consumption versus binge drinking. Further, there was a notable lack of information on the beneficial effects on many pathophysiologic processes of polyphenols and other non-alcohol substances present in wine and certain other foods and beverages.
Overall, it was believed that the paper provided important information for physicians who may be discussing alcohol consumption with their patients.
Reference
Clinical Crossroads: Conferences with patients and doctors. A 42-year-old man considering whether to drink alcohol for his health. Kenneth J. Mukamal, MD, MPH, Discussant. JAMA 2010;303:2065-2073. (doi:10.1001/jama.2010.550)
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: Critique 009.
===============================================================================
Summary: Critique 008: 13 June 2010
Further evidence that moderate alcohol consumption may play a role in the prevention of Alzheimer’s Disease
In a case-control study from Spain on the effects of smoking and alcohol use on the risk of Alzheimer’s Disease (AD), the authors found that the risk of AD was unaffected by any measure of tobacco consumption. On the other hand, alcohol consumers showed a 47% lower risk of developing AD than did never consumers, with effects mainly among women and among never smokers. No differences were noted by type of alcoholic beverage consumed. The authors conclude that mean daily total consumption of alcohol showed increasingly protective dose-response relationships in women.
The numbers in this analysis were rather small, and there is always the possibility of confounding by other lifestyle factors. Still, the study supports a number of previous epidemiologic studies showing a lower risk of developing AD for moderate consumers of alcohol.
Reference
García AM, Ramón-Bou N, Porta M. Isolated and joint effects of tobacco and alcohol consumption on risk of Alzheimer’s Disease. Journal of Alzheimer’s Disease 2010;20:577–586. (DOI 10.3233/JAD-2010-1399).
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: Critique 08.
===============================================================================
Summary: Critique 007 9 June 2010
People may change to a “healthier” pattern of drinking as they age
In a prospective longitudinal study of a cohort of Americans in the “Baby Boomer” generation, subjects’ drinking habits were assessed at two points, when they were approximately 53 years of age and again when they were approximately 64 years of age. As the subjects got older, they began to consume fewer drinks per occasion but to consume alcohol more frequently; the net effect was little change in total alcohol intake for women but a slight increase for men.
In most epidemiologic studies, regular moderate drinking is the pattern associated with lower risk of many chronic diseases; hence, the described change in drinking pattern in this study (smaller amounts on more frequent occasions) can be considered a “healthy” change. Most long-term observational studies show a decrease in total alcohol intake with ageing, although reasons for such are poorly understood.
This paper emphasizes the importance of knowing the pattern of drinking, and not just the total number of drinks consumed over a week, when evaluating the impact of alcohol consumption on health and disease.
Reference
Molander RC, Yonker JA, Krahn DD. Age-related changes in drinking patterns from mid- to older age: results from the Wisconsin Longitudinal Study. Alcoholism: Clinical and Experimental Research 2010;34 (Published early online 7 May 2010).
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: Critique 07.
===============================================================================
Summary: Critique 006 2 June 2010
For patients who already have cardiovascular disease, continued moderate alcohol consumption may reduce their risk of death
This review paper in Circuation summarizes data from 8 epidemiologic studies of subjects with cardiovascular disease (CVD) as to their subsequent mortality (both CV and total-mortality) according to their alcohol consumption. Most studies showed significantly lower risk of both CV and total mortality for patients with CVD who were consumers of alcohol.
Despite these clear-cut findings, the authors were very cautious in their conclusions, focusing on the dangers of excessive drinking and not encouraging cardiovascular patients who do not drink to start regular drinking. They state that moderate consumers of alcohol who have CV disease should not be advised to stop drinking, but should be advised to not consume alcohol more heavily.
It is interesting that these authors published the meta-analysis upon which this review is largely based in the Journal of the American College of Cardiology earlier in 2010. In that paper, their conclusions were less restrained: “Cardiologists should be aware that regular, moderate alcohol consumption, in the context of a healthy lifestyle (increased physical activity, no smoking), dietary habits (decreased dietary fat intake, high consumption of fruit and vegetables), and adequate drug therapy, would put their patients at a level of cardiovascular or mortality risk substantially lower than either abstainers or heavy or binge drinkers.”
Reference
Costanzo S, Di Castelnuovo A, Donati MB, Iacoviello L, de Gaetano G. Contemporary Reviews in Cardiovascular Medicine. Cardiovascular and overall mortality risk in relation to alcohol consumption in patients with cardiovascular disease. Circulation 2010;121;1951-1959.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 006.
===============================================================================
Summary: Critique 005 27 May 2010
Alcohol in young women may increase their risk of benign breast disease
Among more than 6,000 young women being followed in a longitudinal study, 67 confirmed cases of benign breast disease (BBD) were diagnosed. Alcohol consumption was reported on 57 women who developed BBD when they were 16 – 23 years of age, with all but 8 subjects being 18 or older when they reported alcohol intake, and no data were presented on potential exposures earlier following menarche. A significant increase in the risk of BBD was associated with alcohol intake, although many key factors that have been shown to relate to BBD were not reported in the paper. Hence, while the number of cases is small, and a number of potential risk factors are not included, this study suggests that BBD may be increased by alcohol consumption in young women.
Reference
Berkey CS; Willett WC; Lindsay Frazier A; Rosner B; Colditz GA; Rockett RH; Helaine RM. Prospective study of adolescent alcohol consumption and risk of benign breast disease in young women. Pediatrics 2010;125:e1081-e1087.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 005.
===============================================================================
Summary: Critique 004 24 May 2010
Moderate alcohol consumption is associated with other healthy lifestyle factors
An analysis based on a very large number of subjects in France demonstrates, as have most other studies, that moderate consumers of alcohol have many associated healthy lifestyle habits: lower levels of body mass index, blood glucose, heart rate, stress and depression scores; higher subjective health status, HDL-cholesterol values, levels of physical activity and social status. The authors suggest that alcohol is not related causally to any of these factors, and that the other lifestyle factors, not alcohol consumption, are the reason that moderate drinkers have less cardiovascular disease. They chose a very narrow group of citations from the literature to support this contention.
The authors ignore a large number of well-conducted prospective epidemiologic studies showing that moderate drinkers are at lower risk over time of developing certain risk factors. Further, the authors of this paper ignore an immense basic science literature that suggests that alcohol is an important factor in the development of biological risk factors, atherosclerosis, and cardiovascular disease. Further, they do not describe a number of studies that have shown specifically that moderate drinking is associated with less cardiovascular disease and diabetes among subjects who are otherwise very healthy (non-smokers, not obese, physically active, and on a healthy diet).
There is no doubt that confounding by associated lifestyle factors can play a role in the lower risk of chronic diseases among moderate drinkers, who tend to also have other healthy behaviors. However, there is now a large body of scientific evidence that indicates that alcohol is an important factor in the lower rates of such diseases; current scientific data do not support the conclusions of the authors of this paper.
Reference
Hansel B, Thomas F, Pannier B, Bean K, Kontush A, Chapman MJ, Guize L, Bruckert E. Relationship between alcohol intake, health and social status and cardiovascular risk factors in the urban Paris-Ile-De-France Cohort: is the cardioprotective action of alcohol a myth? European J Clin Nutrition, advance online publication, doi:10:1038/ejcn.2010.61.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 004.
===================================================================================
Summary: Critique 003 17 May 2010
Moderate alcohol consumption markedly reduces the risk of diabetes mellitus, even among subjects with otherwise very healthy lifestyles
In a very well-done analysis from a large Dutch population, it was shown that moderate drinking considerably lowers the risk of developing type 2 diabetes even among subjects who are otherwise following a healthy lifestyle (not obese, non-smokers, physically active, eating a healthy diet). Thus, it indicates that the effect of moderate drinking on lowering the risk of diabetes cannot be explained by other healthy lifestyle habits of such drinkers. Moderate drinking should be considered as a complement, and not as an alternative, to other healthy lifestyle habits that lower the risk of chronic diseases such as diabetes and coronary heart disease.
Reference
Joosten MM, Grobbee DE, van der A DL, Verschuren WWM, Hendriks HFJ, Beulens JWJ. Combined effect of alcohol consumption and lifestyle behaviors on risk of type 2 diabetes. Am J Clin Nutr 2010;91: 1777-1783.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 003.
===============================================================================
Summary: Critique 002 26 April 2010
Red wine, but not other types of alcohol, improve endothelial function in a randomized trial
The healthy state of cells that form the lining of arteries, assessed by indices of endothelial function, is a key factor associated with preventing the development and progression of atherosclerosis and coronary heart disease. In a randomized trial among healthy young adults, the daily consumption of about 3 ounces of red wine for three weeks led to significant improvement in endothelial function. Such improvements were not seen with the consumption of water, or of beer or vodka containing similar amounts of alcohol.
Further, in a series of in-vitro studies, the authors showed very similar effects from red wine and from a high concentration of resveratrol (but not from beer or ethanol) on factors associated with improved endothelial function. The study supports many epidemiologic and animal experiments suggesting that certain non-alcoholic constituents of red wine have additional beneficial effects on cardiovascular risk over those of just the alcohol itself.
Reference
Huang PH, Chen YH, Tsai HY, Chen JS, Wu TC, Lin FY, Sata M, Chen JW, Lin SJ. Intake of red wine increases the number and functional capacity of circulating endothelial progenitor cells by enhancing nitric oxide bioavailability. Arteriosclerosis Thrombosis and Vascular Biology 2010;30:869-877.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 002.
===============================================================================
Summary: Critique 001 24 April 2010
Genetic effects on alcohol metabolism modify the relation of alcohol to breast cancer
A study from Germany compared the association between alcohol and breast cancer risk according to genetic variations affecting levels of alcohol dehydrogenase, an enzyme that clears alcohol from the blood stream. The authors conclude that genetic factors associated with the slow clearance of alcohol are associated with increased risk of breast cancer for drinkers; an increase in cancer risk was not seen for drinkers with genetic factors leading to fast clearance of alcohol. Such a finding would suggest that alcohol itself is the cause of an increase in breast cancer risk among drinkers.
Unfortunately, some previous studies have shown the opposite, that an increase in breast cancer risk occurs only among women who have genes associated with fast, rather than slow, alcohol metabolism. Overall, current scientific data indicate that breast cancer’s relation to drinking is not resolved, remaining murky and conflicted, and perhaps overemphasized. This facet of that murkiness is itself also conflicted. As of now, it is unclear the degree to which genes affecting alcohol dehydrogenase modify the association between alcohol and the risk of breast cancer and other diseases.
Reference
Larsen SB, Vogel U, Christensen J, Hansen RD, Wallin H, Overvad K, Tjønneland A, Tolstrup I. Interaction between ADH1C Arg272Gln and alcohol intake in relation to breast cancer risk suggests that ethanol is the causal factor in alcohol related breast cancer. Cancer Letters, 2010, in press.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 001.
===============================================================================
======================================================
Critique 260:Two studies on the Mediterranean alcohol-drinking pattern and its association with hypertension and all cause mortality in the Seguimiento Universidad de Navarra” (SUN) cohort – 24 January 2023
Mediterranean Alcohol-Drinking Patterns and All-Cause Mortality in Women More Than 55 Years Old and Men More Than 50 Years Old in the “Seguimiento Universidad de Navarra” (SUN) Cohort – 14 December 2022
Mediterranean Alcohol-Drinking Pattern and Arterial Hypertension in the “Seguimiento Universidad de Navarra” (SUN) Prospective Cohort Study – 7 January 2023
The SUN (Seguimiento Universidad De Navarra) study represents one of the main cohorts in the European Mediterranean area aiming to explore the association between dietary factors and non-communicable diseases. The SUN study had previously shown that better adherence to the Mediterranean diet, which includes moderate alcohol consumption with meals, was significantly associated with a lower risk of all-cause mortality. It was also significantly associated with a lower risk of cardiovascular disease (CVD), which is the leading global cause of premature mortality.
These two new papers from the SUN study cohort concern alcohol and its potential beneficial effects when part of a Mediterranean diet and lifestyle. One paper is related to all-cause mortality in an older adult subset of the cohort, while the other related the pattern of drinking to the risk of an initial diagnosis of hypertension, which is a modifiable risk factor for atherosclerosis and therefore CVD.
Limitations of both studies include the relatively small number of events in some groups of drinkers and abstainers, where the latter group included both former drinkers and lifelong abstainer which are usually separated to reduce potential confounding. The all-cause mortality results may also be limited to a certain degree by a relatively small number of non-drinkers (n=35, for whom the degree of compliance with the Mediterranean diet was not shown), and the small number of drinkers who had low compliance with the Mediterranean Drinking Pattern (n=35), with the latter chosen as the reference group. Similarly, a weakness of the hypertension study is that the number of subjects in the low-adherence group was much smaller (n=156) compared with the other groups, yet it served as the referent category in the analyses. Further the low-adherence group was more likely to be younger, male, binged more, smoked more, consumed more alcohol and sugar-sweetened beverages, reported more recent weight gain, and had other unhealthy characteristics. While the investigators used multi-variable analyses that attempted to adjust for these factors, residual confounding is always a problem. Thus, it will be important that further studies with a larger number of subjects in the referent group confirm the observed relations shown in this study. According to their results, however, it seems clear that a drinking pattern of regular, moderate, wine consumption with food does not increase the risk of hypertension, an important message for the health of the population.
Overall, Forum members agreed with the conclusions of the authors that “Moderate red wine consumption at meals which is spread throughout the week, avoiding binge drinking, reduces the risk of all-cause mortality by 48%. These results are consistent with individual studies of each separate aspect of the pattern and with studies of a priori patterns.” Further, this paper strongly suggests that assessments of the relation of alcohol consumption to health should focus on the pattern of drinking, not just the total amount consumed.
References: Barbería-Latasa M, Bes-Rastrollo M, Pérez-Araluce R, Martínez-González MÁ, Gea A. Mediterranean Alcohol-Drinking Patterns and All-Cause Mortality in Women More Than 55 Years Old and Men More Than 50 Years Old in the “Seguimiento Universidad de Navarra” (SUN) Cohort. Nutrients. 2022 Dec 14;14(24):5310. doi: 10.3390/nu14245310. PMID: 36558468; PMCID: PMC9788476.
Hernández-Hernández A, Oliver D, Martínez-González MA, Ruiz-Canela M, Eguaras S, Toledo E, de la Rosa PA, Bes-Rastrollo M, Gea A. Mediterranean Alcohol-Drinking Pattern and Arterial Hypertension in the “Seguimiento Universidad de Navarra” (SUN) Prospective Cohort Study. Nutrients. 2023; 15(2):307. https://doi.org/10.3390/nu15020307
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here
======================================================
Critique 259: Importance of consuming alcohol (especially wine) with meals in relation to the risk of type 2 diabetes mellitus – 30 November 2022
Essentially all previous epidemiologic studies have shown that subjects who consume alcohol are at a lower risk than abstainers of developing Type 2 diabetes mellitus. The present analysis provides new information from more than 300,000 subjects in the UK BioBank who reported that they were consumers of alcohol; it demonstrates how the pattern of consuming alcohol plays an important role in the effect of alcohol on the risk of diabetes. Consuming an alcoholic beverage with food, versus drinking it at other times, is associated with a considerably lower risk of diabetes mellitus. This effect in independent of the amount of alcohol consumed, which suggests that all alcohol policy should be based only on research in which the pattern of drinking is known.
The study also demonstrated that the protective effects against diabetes was greater for consumers of wine rather than for those consuming beer or spirits. These associations are consistent with most previous epidemiologic studies, and now supported from these analyses of a very large cohort.
The authors had very reasonable estimates of alcohol intake as well as good ascertainment of health outcomes. They also had considerable data on many lifestyle and social factors that relate to the development of diabetes, so that confounding and modification of effect by them could be dealt with in the analyses. Forum members noted some limitations to the analytic methods regarding categorization of subjects by the type of alcohol they consumed, and the failure to adjust for diet. However, overall the results appear to support well the conclusions of the authors that there are key health advantages in terms of the risk of developing diabetes of consuming alcoholic beverages (especially wine) with meals, rather than on an empty stomach.
Reference: Ma H, Wang X, Li X, Heianza Y, Qi1 L. Moderate alcohol drinking with meals is related to lower incidence of type 2 diabetes. Am J Clin Nutr 2022;0:1–8.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here
Critique 258. Do the calories in alcoholic beverages increase the risk of obesity? 2 November 2022
This study was designed to determine if greater emphasis on the role of alcohol consumption as related to body weight might lead to less drinking and have a beneficial effect on subsequent weight and obesity. It was based on a survey of a select group of Australian adults who had previously volunteered to take part in medical research (not a population-based cohort). The authors took data from subjects who agreed with a question that asked if the subject ever thought about decreasing alcohol intake to lose weight, comparing them with those who did not answer the question in the affirmative. They compared the two groups (those answering yes versus those answering no to this question) and found some relation with body weight and with BMI (the latter of which was based on self-report of subjects regarding their height and weight).
Unfortunately, the premise that any alcohol increases body weight is erroneous, as the investigators ignored current scientific data that has consistently shown that light-to-moderate alcohol consumption does not increase body weight (which is seen generally only with excessive alcohol intake or binge drinking). While the authors had detailed data on the number of drinks reported by subjects, they ended up categorizing drinking levels into only two groups: ‘daily or weekly,’ or ‘monthly,’ which make it impossible to evaluate results of realistic drinking levels. They present no data on the pattern of drinking (e.g., with or without food, on a regular basis or in binges) or effects of different types of alcohol. They do not consider the complexity of factors related to obesity, and do not mention the effects of diet, exercise, smoking, or genetics on the risk of obesity. They misquoted the results of several previous studies to support their premise that lowering alcohol intake for everybody in the population would lead to less obesity, while a number of these studies actually showed the opposite.
Thus, the authors seem either oblivious to the data on alcohol calories and obesity or are deliberately ignoring it. Instead, their only concern appears to be to increase the incorrect perception that decreasing alcohol consumption among everybody, regardless of their intake, will lower the risk of obesity. Perhaps of even greater importance, they do not consider that a message to the entire population to decrease or stop alcohol consumption could result in increases in many diseases of ageing (e.g., coronary heart disease, ischemic stroke, diabetes, premature mortality risk) that are reduced by regular, moderate intake of alcohol, especially when consumed with food.
The authors end with conclusions that relate obesity to the culture of shame: the pervasive misconception that obesity is primarily a lifestyle-related condition and the simplistic belief that weight reduction is just adopting permanent caloric restriction, and the failure of a person with obesity to achieve and maintain weight loss is caused by a lack of discipline.
Overall, the present paper appears to the Forum as potentially misleading in the sense that it diverts the attention of experts, and potentially the population at risk, from the far more important and above all actionable effort to recommend moderation in drinking associated with a healthy and active lifestyle that does not lead to weight gain.
Reference: Bowden J, Harrison NJ, Caruso J, Room R, Pettigrew S, Olver I, Miller CWhich drinkers have changed their alcohol consumption due to energy content concerns? An Australian survey. BMC Public Health 20222; 22:1775. doi.org/10.1186/s12889-022-14159-9
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
======================================================
Critique 257: Does statin use modify potential beneficial effects of moderate alcohol consumption on cardiovascular risk? — 21 September 2022
The goal of this study was to determine if statin use (defined as the subject having been given a prescription for a statin, although actual consumption of statin was not ascertained) among a group of subjects who underwent cardiac catheterization modified the effects of alcohol consumption on subsequent cardiovascular events and total mortality. Their primary outcome was the occurrence during a follow-up period averaging 4.4 years of a Major Cardiac Adverse Event (MACE = documented myocardial infarction, ischemic stroke, heart failure hospitalization, or all-cause mortality).
From their adjusted analyses for “primary prevention” subjects MACE outcomes were 6.5% for alcohol users versus 14.2% for alcohol non-users (HR 0.50, CI 0.33, 0.78) for those not on a statin. If the subjects were on a statin, the protection from alcohol was less (19.5% for alcohol users versus 22.7% for alcohol non-users), not statistically significant. For subjects classified as ‘secondary prevention,’ alcohol users had only slightly lower risk of a MACE outcome, 18.2% versus 19.9% for no statin users and 19.9% versus 22.7% for statin users, not statistically significant. (In the Authors’ abstract, the HRs reported as greater than 1.0 are apparently for non-users of alcohol versus users of alcohol, as the reported adjusted risk of MACE was lower for alcohol users in all categories.)
There were several problems identified in the Forum review regarding the study design, analysis, and conclusions of the authors. Subjects were from the Intermountain Medical Center with patients primarily from Utah and several surrounding states. The characteristics of the subjects are quite different from those in most other areas of the United States in that the large majority reported that they consumed zero alcohol (between 66% and 75% in the categories of subjects); this is probably related to most being of the Mormon faith where alcohol use is not acceptable. (Religious affiliation of subjects is not reported in the paper.) Further, it would be expected that many Mormons who may have had consumed some alcohol in the previous year would deny it on a form being collected by the Intermountain Center, where they are being treated; this would lead to under-reporting of the exposure being studied and misclassification.
Further, all subjects were placed into categories classifying them as at “primary cardiovascular risk” or “secondary cardiovascular risk”; also if they reported any alcohol use (regardless of the amount or the drinking pattern) they were classified as alcohol users; otherwise they were in the no alcohol category. Subjects with zero coronary obstruction on angiography were classified as being at “primary risk” if they had not previously reported a myocardial infarction, coronary revascularization procedure, or an obstruction of a coronary artery of ≥ 70% identified on a prior angiogram (n=477). Otherwise, regardless of current findings of coronary obstruction of zero or of any amount of obstruction greater than zero, subjects with a previous cardiovascular event (including ≥70% obstruction of a coronary artery on a previous catheterization) were classified as being at secondary risk (n=2,108). Such complex and unusual categorizations could lead to misclassification of exposure and various types of bias. No data that are based on all patients, regardless of classification into primary or secondary risk, are presented.
Unfortunately, in their main analyses there were no distinctions according to the reported amount of alcohol. They do report “exploratory analyses” of reported amount: those consuming < 2 drinks/day seemed to have the most protection from alcohol – however, the numbers of subjects in the groups were inadequate for definitive results. Further, there were no data on the “pattern of drinking” (regularly or sporadically, with or without food, etc.) for subjects reporting any alcohol use. Having all subjects evaluated only within categories could lead to bias and limits the usefulness of the results.
In their analyses, the authors adjusted the effects of alcohol use on MACE with an extremely long list of potential confounders. Unfortunately, among these was the presence of diabetes, for which alcohol consumption has clearly been shown to reduce the risk of cardiovascular disease; diabetes is considered to be an important intermediary mechanism of the effect of alcohol. Thus, it would not be appropriate as a confounder. Also, others of the factors included as potential confounders were those that would be expected to be affected (either adversely or beneficially) by alcohol consumption, thus should not be used as potential confounders if one is seeking to determine the total effect of alcohol on cardiovascular disease.
Overall, a number of factors weaken the implications cited by the authors. These include the database used for this study (a majority of subjects reporting zero alcohol at baseline, unusual for Western populations), problems in categorization of subjects into primary or secondary risk, inappropriate factors adjusted for as “confounders” (including some directly affected by alcohol use), failure to discuss the law of diminishing results, and suggesting “no effect” when results were not statistically significant. Such problems make it difficult to support the authors’ conclusion that the prescription of a statin negates any effect of alcohol consumption on cardiovascular risk.
Reference: Anderson JL, Le VT, Bair TL, Muhlestein JB, Knowlton KU, Horne BD. Is Alcohol Consumption Associated with a Lower Risk of Cardiovascular Events in Patients Treated with Statins? An Observational Real-World Experience. J Clin Med 2022;11:4797. doi.org/10.3390/jcm11164797
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===========================================================
Critique 256: Alcohol consumption and health outcomes among 70 year olds in Sweden –22 August 2022
In a population-based cohort of 70-year-old men and women recruited in Gothenburg, Sweden, in 2014-2016, the authors of this paper have presented a detailed listing of many social, environmental, and biological factors that relate to non-drinking, former drinking, or current drinking of varying amounts of alcohol. Our Forum critique raises some questions about the traditional belief that the elderly should consume markedly less alcohol than younger subjects, and that the limitations placed on subjects related sorely to their age may often not be appropriate.
The paper emphasizes how a very large number of factors may modify the association between the amount of alcohol consumed and measures of health and disease. Many of these, such as indices of socio-economic state, are usually adjusted for in epidemiologic studies. Data on other factors that relate to alcohol consumption (such as self-related health, having a partner, grip strength, having others worried about their drinking, religiosity, gait speed, life satisfaction, etc.) represent data usually not collected in epidemiologic studies.
Forum members thought that these analyses show that subjects whose reported alcohol intake is only slightly above the recommended “safe” levels for subjects of this age should not be classified as “at-risk” drinkers. Most of their features match those of subjects reporting intake within current recommendations; certainly, they do not match the characteristics of heavier drinkers.
Forum members also pointed out that in addition to improved mortality associated with truly moderate drinking, as seen in essentially all epidemiologic studies, these analyses demonstrate that many other components of “successful ageing” are also associated with regular, moderate consumption of alcohol.
Reference: Ahlner F, Erhag HF, Johansson L, Fässberg MM, Sterner TR, Samuelsson J. Zettergren A, Waern M, Skoog I. Patterns of Alcohol Consumption and Associated Factors in a Population-Based Sample of 70-Year-Olds: Data from the Gothenburg H70 Birth Cohort Study 2014–16. Int J Environ Res Public Health 2022;19:8248; doi.org/10.3390/ijerph19148248
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
=====================================================
Critique 255: Wine consumption and the risk of cognitive decline in the elderly – 29 June 2022
The results of this systematic review and meta-analysis of longitudinal studies showed that, in almost every study, both wine consumption within the usual guidelines (no more than 2 drinks/day for men or 1 drink/day for women), as well as consumption in excess of these limits, were similarly associated with a lower risk of cognitive decline. For studies providing data on the amount of alcohol consumed, the risk of cognitive decline was reduced by 41% for both wine consumers drinking within the recommended guidelines as well as those reporting wine consumption in excess of the guidelines, when compared with abstainers. In studies where the amount of wine consumption was not reported, the estimate was an 18% reduction in the risk of cognitive decline for wine consumers versus abstainers.
Forum members noted that many potential confounders of the relation of alcoholic beverage consumption and cognition may modify the effects of alcohol on cognition, and were not evaluated very well in this study. Especially important may be the pattern of drinking (regularly or irregularly, with or without food, with associated binge drinking, etc), Forum members agreed that the calculations of the authors support a protective effect of wine consumption against cognitive decline, but their conclusions may be limited because of residual confounding by the pattern of drinking and other key factors not included in their analyses.
Forum members also noted another recent paper relating brain MRI markers to alcohol intake. However, changes in cognitive function were not assessed in the latter paper, and a direct comparison between the two papers cannot be done. However, we conclude that there remain questions regarding the effects of wine and other beverages containing alcohol on cognition. Other studies have shown divergent effects on the risk of dementia associated with wine consumption and the intake of spirits, so there may indeed be different effects on cognition with wine intake, the factor studied in the present paper. And, when compared with non-drinking or drinking of other beverages, extensive research supports health and mortality advantages when wine is consumed moderately, and especially with meals.
Reference:Lucerón-Lucas-Torres M, Cavero-Redondo I, Martínez-Vizcaíno V, Saz-Lara A, Pascual-Morena C, Álvarez-Bueno C. Association Between Wine Consumption and Cognitive Decline in Older People: A Systematic Review and Meta-Analysis of Longitudinal Studies. Frontiers in Nutrition 2022;9:863059
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
=====================================================
Critique 254: Adjusting for underreporting of alcohol intake in epidemiologic studies – 13 April 2022
It has been demonstrated repeatedly that the total population alcohol consumption based on self-reports by subjects in surveys and epidemiologic studies is lower than the amount of alcohol sold or taxed (disappearance data) within the population. This is assumed to relate to marked underreporting of individuals of their consumption, sometimes by one half or more. A key problem in attempting to adjust the self-reported values to more closely match the total alcohol disappearance data is that everyone does not underreport their intake, or may do so by different degrees.
The present study was based on data from US adults who responded to the 2011-2015 Behavioral Risk Factor Surveillance System (BRFSS; N = 2,198,089). The authors tested six methods for adjusting the self-reported data to provide what they hoped to be a more accurate value; some methods included adjustments based on differences in consumption by age and sex subgroups. From an unadjusted value of self-reported consumption of only 31.3% of that indicated by disappearance data, the various methods provided adjusted values ranging from 36.1% to 73%. The authors then used higher values to estimate the effect on alcohol-attributable deaths, using a population-attributable fraction approach.
While applauding the authors for attempting to obtain better estimates of alcohol consumption, Forum members were surprised that the authors did not even mention the method for identifying underreporting of individual subjects described by Klatsky and colleagues in the Kaiser Permanente Studies. The results of their method have been demonstrated to relate closely to alcohol’s effects on the risk of cancer, hypertension, and total mortality. Their method includes, in addition to self-reported data on alcohol consumption, adjustments for a variety of health conditions known to relate to excessive alcohol exposure, including alcoholic liver disease, hospitalizations for intoxication, mental problems associated with heavy drinking, etc. The presence of these conditions not only suggested that such subjects markedly underreported their intake (the exposure), but they also had much higher risk of adverse health effects (the outcome). When these conditions were not present at any of the study visits of subjects (allowing such subjects to be classified as being unlikely to be underreporting their alcohol consumption), adverse effects of low to moderate alcohol intake were generally not seen or their occurrences were markedly less frequent. This adjustment approach seems to be the only one previously described that gives reasonable results for individuals, and is clearly associated with the future health outcomes of subjects (and we realize that the occurrence of certain diseases or death happens for individual subjects, not for the population).
The Forum also raised questions about using “alcohol-attributable risk”. The authors base their calculations of population attributable risk on the hypothetic assumption of a rather low degree of underreporting in the population studies that are used as foundation of relative risk associations between alcohol intake and disease. Thus, risk is based mainly on self-reports of intake, even though their present paper indicates that adjustment for underreporting is so important. Further, throughout the paper, it appears that the authors tend to focus only on the adverse effects of alcohol without taking into regard the beneficial effects of light-to-moderate drinking, especially the regular consumption of wine with meals, which is found almost universally to be associated with lower risk of cardiovascular disease, diabetes, and total mortality.
While appropriate adjustment for underreporting could greatly improve the results of epidemiologic studies on alcohol and health, the goal would be to develop methods of determining the risk of individual subjects by including data on their own pattern of drinking and not assuming that the same adjustment formula applies to everyone in a population. By being able to identify subjects who underreport their intake, it would lead to some people changing categories of intake, and should result in estimates of either a lower risk, or greater risk, of adverse health effects of alcohol for that category of drinking. Further, more accurate and updated assessments of future health conditions that may be adversely (or beneficially) related to alcohol consumption should improve results and provide better data for setting drinking guidelines.
Reference: Esser MB, Sherk A, Subbaraman MS, Martinez P, Karriker-Jaffe KJ, Sacks JJ, Naimi TS. Improving Estimates of Alcohol-Attributable Deaths in the United States: Impact of Adjusting for the Underreporting of Alcohol Consumption. J Stud Alcohol Drugs 2022;83:134-144. https://doi.org/10.15288/jsad.2022.83.134.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 253 – The relation of alcohol consumption to the risk of glioma tumors of the brain – 5 January 2022
There appears to be an increase in the risk of glioma tumors of the brain, yet very few lifestyle or genetic factors shown to be true “risk factors” for the disease have been identified. The authors of this paper present the association between reported alcohol consumption from multiple assessments over decades and the diagnosis of such tumors, combining data from subjects in large cohort studies of nurses and male health care providers. Among the important strengths of this paper is the fact that the data were collected as part of a prospective study, difficult to do in cancer epidemiology except with very large cohorts. A total of 554 cases of glioma tumors were identified in these cohorts from a total sample of more than 200,000 subjects.
Forum reviewers agree with the conclusions of the authors that light-to-moderate alcohol consumption does not increase the risk of glioma; in fact, total alcohol consumption over many decades was found to reduce the risk. For example, a cumulative average consumption of total alcohol of >8 to 15 g/d (approximately 0.5 to 1.0 drink/day) was associated with a 25% lower risk of glioma when compared with the lowest category of intake (0 to 0.5 g/day) for both men and women. For consumers of > 15 g/d (just over 1 typical drink/day) versus the referent group, the risk for women was further significantly reduced to HR = 0.61; for men, the HR estimate was 0.79, but not statistically significant. (Some previous cohort studies have suggested an increase in risk for heavy drinkers.) There were no differences according to type of alcoholic beverage. For the subgroup of subjects with glioblastomas, findings were similar but less precise, due to smaller case counts.
The Forum concludes that light-to-moderate alcohol consumption, versus no alcohol intake or very occasional drinking, does not increase the risk; in this very well-done study, such consumption showed a significant reduction in the risk of glioma tumors of the brain.
Reference: Cote DJ, Samanic CM, Smith TR, Wang M, Smith‑Warner SA, Stampfer MJ, Egan KM. Alcohol intake and risk of glioma: results from three prospective cohort studies. Eur J Epidemiol 2021;36:965–974. https://doi.org/10.1007/s10654-021-00800-1
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 252: Dealing with previous alcohol exposure among “current non-drinkers” in epidemiologic studies testing the J-shaped curve – 3 December 2021
Most cohort studies have demonstrated a reduced risk of cardiovascular diseases, diabetes, and even dementia among light-to-moderate consumers of alcohol when compared with lifetime abstainers. This is often described as a “J-shaped curve,” a reduction in disease risk for light drinkers (compared with abstainers) but an increase in risk for heavy drinkers. Many criticisms of the J-shaped curve have been based on claims that many studies include “sick quitters” in their referent group. Such criticisms ignore most recent cohort studies in which only lifetime abstainers make up the referent group. Epidemiologists have known for decades that including ex-drinkers in the referent group for evaluating health effects of alcohol is an error; such a group cannot be used for comparisons with moderate drinkers.
While the present study from a large cohort in Germany clearly shows how previous alcohol excess and other unhealthy lifestyle factors and socio-economic factors influence the risk of many diseases, it creates a referent group made up of mixing lifetime abstainers and some ex-drinkers, and that their analyses show that this group does not have a higher risk of mortality than light drinkers (thus, the protection of light drinking leading to a decrease in risk of disease is erroneous). The authors of this paper apparently did this because they had such a small group of lifetime abstainers (only 42 subjects out of a cohort of 4,000!), a number grossly inadequate for comparisons with drinkers.
Forum members agreed that it was a serious error for the investigators; instead of admitting that their numbers were too low in this group for reliable comparisons, it appears that the authors augmented the comparison group with a group of ex-drinkers (that they considered to not be heavy drinkers) and reported that their analyses do not support a reduced risk among light drinkers. Thus, their claim that the lower risk of cardiovascular disease demonstrated in most studies among moderate drinkers is unrelated to alcohol consumption. However, this claim is based on an improper referent group used in their analyses. Forum members considered this to be a deeply flawed analysis, and of no merit for use in setting drinking guidelines.
Reference: John U, Rumpf H-J, Hanke M, Mayer C. Alcohol abstinence and mortality in a general population sample of adults in Germany: A cohort study. PLOS Med 2021;18:e1003819.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 251: Does moderate drinking increase, or decrease, the risk of falls in middle-age to elderly adults? 1 November 2021
To judge the relation of reported alcohol consumption to the risk of subsequent falls requiring hospitalization, the authors of this paper used data from the EPIC-Norfolk study, a prospective population-based cohort study in Norfolk, UK. In that study, there were a total of 25,637 community-dwelling adults, aged 40–79 years when recruited. The main outcome was the first hospital admission due to a fall over a follow-up period of about 11.5 years.
The key results of the study were that 19.2 % of non-drinkers were hospitalized for a fall during follow up, compared with 13.7% of low drinkers, 10.9 % of moderate drinkers, and 12.3% of heavy drinkers. In addition, the cumulative incident rates for falls at 121-180 months of follow up were 11.08% for teetotalers, 7.53% for low drinkers, 5.91% for moderate drinkers, and 8.20 % for heavy drinkers.
Forum members considered this to be a well-done study, with the analysis adjusting for a large number of factors that were potential confounders of the relation of alcohol intake to the risk of falls. We agree with the conclusions of the authors: “Moderate alcohol consumption appears to be associated with a reduced risk of falls hospitalization, and intake above the recommended limit is associated with an increased risk,” although we note that the increase in risk for heavier drinkers only appeared after essentially all covariates were added to the analysis. Obviously, residual confounding is always a possibility, but the present analyses indicating some protection against falls among light-to-moderate drinkers are supported by some well-done previous research.
The results of this study do not support the claim that any alcohol increases the risk of falls in older adults. It appears that this is not a concern for light-to-moderate drinkers who, in this study, had a lower risk of falls requiring hospitalization than did non-drinkers.
Reference: Tan GJ, Tan MP, Luben RN, Wareham NJ, Khaw K-T, Myint PK. The relationship between alcohol intake and falls hospitalization: Results from the EPIC-Norfolk. Geriatr Gerontol Int 2021;21:657-663.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 250: Importance of a favorable pattern of drinking (regularly, and with food) on risk of mortality – 28 July 2021
This is an analysis based on a very large data base of alcohol consumers (subjects reporting > 0 g of alcohol/week) from the UK Biobank (analyses based on 316,627 subjects with a median follow up of 8.9 years). The authors constructed categories of Drinking Habit Scores (DHS) for subjects; a “favorable” DHS was used for those subjects reporting a drinking frequency of 3 or more days/week and consuming alcohol with meals. The investigators then related the DHS categories to subsequent all-cause and cause-specific mortality, with adjustments for essentially all of the common known confounders/modifiers of alcohol effect.
Overall, Forum reviewers agreed with the main outcomes of the study, which indicate that subjects with a favorable DHS (in comparison with other drinkers) had significantly lower all-cause mortality (HR=0.82), CVD mortality (HR=0.84); cancer mortality (HR=0.82), and death from other causes (HR=0.77). In relation to the number of drinks consumed, the authors report that for all-cause, CVD, and other cause mortality, subjects with a favorable DHS showed a U-shaped or L-shaped curve (in that even for the heaviest drinkers, the mortality risk remained the same or lower than that of abstainers). Only for cancer mortality was there an increase in risk for subjects in the highest category of alcohol intake, leading to a J-shaped curve.
While the authors did not report specifically on the types of beverage being consumed in their favorable drinking pattern, it is the typical pattern generally found in southern Europe, and typically it is wine with meals. In these societies, wine is considered part of the meal, and is not consumed as “shots” that are usually being taken primarily as a way of getting drunk. As described in this paper, it is important to separate the health effects of these opposite approaches for consuming a beverage containing alcohol; putting all subjects into groups based only on the grams of alcohol consumed over a period, usually a week, does not take into account the important differences associated with the pattern of drinking.
We are finally appreciating that we are much further along in our research on alcohol and health than the innumerable studies that have focused just the amount of alcohol consumed, or on the J-shaped curve. We now realize the importance of the pattern of drinking. This constitutes not only the type of beverage and frequency of drinking, but also the consumption of alcohol with food and the absence of binge drinking. The pattern of drinking appears to be as important as, or even more important than, the quantity of alcohol consumed.
Reference: Ma H, Li X, Zhou T, Sun D, Shai I, Heianza Y, Rimm EB, Manson JE, Qi L. Alcohol Consumption Levels as Compared With Drinking Habits in Predicting All-Cause Mortality and Cause-Specific Mortality in Current Drinkers. Mayo Clin Proc 2021;96:1758-1769.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 249: Does light-to-moderate drinking increase the risk of atrial fibrillation? — 23 June 2021
While many epidemiologic studies have demonstrated an increase in the risk of AF for consumers of alcoholic beverages, there remains a question as to whether or not there is a threshold amount that would increase the risk. The present study concludes that “less than two alcohol units/day significantly increased the risk of incident AF, however, in men only. Reduction of even a moderate alcohol intake may thus reduce the risk of AF at the population level.”
While this may be the case, Forum members had a number of concerns about using the results of the present study to determine whether or not there is a threshold amount of alcohol necessary to increase the risk of AF. The methods used to judge alcohol consumption did not report the type of beverage or have a good estimate of the pattern of drinking, both of which factors are known to modify the health effects of alcohol. Further, the authors stated that there was evidence of considerable under-reporting of alcohol in their cohort, as the level of HDL noted in their “light” drinkers was above the level expected. This suggested to them that subjects in their lowest category of alcohol may actually have consumed more than they reported (probably about twice the reported amount of alcohol). This makes it difficult to determine if truly “light” drinking is associated with an increased risk of AF.
Overall, scientific data continue to show that light-to-moderate alcohol intake, especially when the pattern of drinking is found to be regular moderate consumption with food and without binge drinking, is associated with a lower risk of ischemic stroke and death. For the effects of alcohol intake on the risk of AF, the situation remains unclear. Unfortunately, the present study cannot answer the question as to whether there is, or is not, a clear threshold effect of alcohol intake on the risk of developing AF.
Reference: Ariansen I, Degerud E, Gjesdal K, Tell GS, Næss O. Examining the lower range of the association between alcohol intake and risk of incident hospitalization with atrial fibrillation. IJC Heart & Vasculature 2020;31:100679.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 248: Association of Alcohol Consumption with Cataract Surgery — 19 April 2021
This was a well-done analysis of a very large number of cases of cataract surgery in the UK; there were reasonable measures of the exposure (alcohol consumption), including the amount and type of beverage consumed, and appropriate potentially confounding factors were taken into consideration. However, data on the consumption of alcohol with or without food were not available. The use of national registries of cataract surgery provide an appropriate approach for estimating the main outcome of the analyses, and the results probably reflect the incidence of clinically significant cataract occurrence in these populations.
The key results were that there was a small but highly significant lower risk of cataract surgery among moderate drinkers. Red and white wine consumers showed more consistent and significantly lower risks of cataract surgery than consumers of other beverages. (In one of the two studies included in the analysis, small amounts of beer and spirits also showed a lower risk than that of non-drinkers.) There were too few heavy drinkers in these studies to determine the extent to which such drinking might affect risk. We appreciate that residual confounding, especially by factors that relate to subjects choosing to have surgical treatment of their cataracts, could still be present in these results.
Forum reviewers conclude that, in agreement with the investigators of this study, the data indicate a small but statistically and clinically significant decrease in the risk of cataract surgery for low-to-moderate drinkers, versus non-drinkers. A lowering of risk was especially clear for wine drinkers, in comparison with consumers of beer and spirits. There is an extensive literature regarding potential mechanisms by which constituents of the diet, especially those present in wine, may influence the development of cataracts. Among these are antioxidants or ROS scavengers, aldose reductase inhibitors, antiglycating agents, and inhibitors of lens epithelial cell apoptosis. However, the ultimate reason for the lower risk of cataract surgery associated with wine consumption found in this study has not been clearly delineated.
Reference: Chua SYL, Luben RN, Hayat S, Broadway DC, Khaw K-T, Warwick A, et al, on behalf of The UK Biobank Eye and Vision Consortium. Alcohol Consumption and Incident Cataract Surgery in Two Large UK Cohorts. Ophthalmology 2021, pre-publication.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 247: Effects of alcohol consumption on risk of stroke and systemic embolism among subjects with atrial fibrillation – 15 March 2021
The main aim of the current study was to investigate the associations of regular alcohol intake with incident stroke or systemic embolism in patients with established atrial fibrillation (AF), most of whom (84%) were on anti-coagulant therapy. The authors used combined data from two prospective studies of subjects with AF, followed for an average of 3 years. While they excluded subjects with “only short, potentially reversible AF episodes (e.g., as after cardiac surgery or sepsis)” about one half of subjects in the study were diagnosed as having paroxysmal AF. Reported alcohol at baseline and at subsequent examinations was classified as none, > 0 to < 1 drink/day, 1 to < 2 drinks/day, and ≥ 2 drinks/day.
The primary outcome was a composite of stroke and systemic embolism. Secondary outcomes were all-cause mortality, myocardial infarction, hospital admission for acute heart failure, and a composite of major and clinically relevant nonmajor bleeding. In their analyses, they adjusted for age, sex, education, hypertension, history of heart failure, history of diabetes, BMI, smoking status, physical activity, history of stroke, history of coronary heart disease, oral anticoagulation, history of renal failure, AF type, and health perception. With annual assessments, the investigators updated all covariates over time, if appropriate.
The main results indicated no significant effect of alcohol consumption on the risk of the major outcomes (stroke or systemic embolism). However, there were significant decreases in risk for several secondary outcomes. For hospital admissions for heart failure, in comparison with non-drinkers the HR for moderate drinkers was 0.60 (CI 0.41-0.87); further, among moderate drinkers the HR for myocardial infarction was 0.39 (CI 0.20 – 0.78), and for all-cause mortality the HR was 0.49 (CI 0.35-0.69).
Forum members had two major concerns with the paper. First, the authors failed to report specifically how alcohol consumption was associated with increased or decreased presence of AF during follow up, even though approximately one-half of subjects had only paroxysmal AF at baseline. Determining if alcohol consumption affected subsequent AF would be information of importance to practitioners who are advising their patients with AF regarding alcohol consumption.
Secondly, it was pointed out by Forum members that the results may have been affected by what is known as collider bias: as moderate drinking shows an inverse association with coronary heart disease (which is strongly related to the presence of AF), subjects who consumed alcohol prior to the baseline diagnosis of AF were probably different from those who had no prior alcohol exposure, and the results of combining these two groups (as was done in these analyses) may have been biased. Such bias usually tends to result in estimates of effect going toward the null.
While the reported results of no real effect of alcohol consumption on the risk of stroke or systemic embolism among patients with AF is encouraging, to decrease the risk of bias in future studies it will be important that such research attempts to separate subjects according to their prior use of alcohol before baseline measurements are assessed. The marked reduction in the risk of other major cardiovascular outcomes and total mortality, found in this study to be associated with light to moderate drinking, matches the results seen in most previous studies.
Reference: Reddiess P, Aeschbacher S, Meyre P, Coslovsky M, Kühne M, Rodondi N, et al, for the BEAT-AF and Swiss-AF investigators. Alcohol consumption and risk of cardiovascular outcomes and bleeding in patients with established atrial fibrillation. CMAJ 2020;193:E117-E123. doi: 10.1503/cmaj.200778
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 246: Light to moderate alcohol intake and the risk of cancer — 8 February 2021
The present paper attempts to use alcohol-attributable data, based on combining average alcohol intake from diverse European populations, to judge the effects of moderate alcohol consumption on the risk of cancer for all populations. It is based on earlier calculations of risk, extensively covered in previous publications by the senior author. The investigators conclude that the risk of a number of types of cancer are increased even among subjects reporting no more than 20 grams of alcohol per day (up to about 2 typical drinks), an amount they state to be within recommended levels of consumption (but exceed current US Drinking Guidelines for women of no more than 1 drink/day). The largest contribution to their calculated effects of alcohol was from breast cancer in women (which made up “68.7% of all alcohol attributable cancer for both sexes”). Breast cancer is a condition for which many factors other than just average alcohol intake are important: factors such as pattern of drinking, type of beverage, folate intake, smoking, obesity, physical activity, etc., all of which tend to confound the association.
Forum members had real concerns about their methodology of using an estimate of “alcohol-attributable cancer” based on reported average intake from 28 separate countries, including the large countries in western Europe (e.g., Germany, France, UK, Italy, Spain, Sweden), East-European countries (such as Poland and Hungary), and many smaller countries (e.g., Malta, Cyprus, Luxembourg, Latvia). Given the marked variation in culture and drinking patterns among these countries, it was considered that there are a large number of confounders and modifiers of alcohol effects that vary by country, and make it impossible to simply take the average alcohol intake from such diverse cultures to estimate causality of alcohol and cancer for everyone. By lumping data from all of these countries, the analyses end up with values that relate to a non-existent hypothetical population; different countries have different risk relationships, so the estimates of effect described in the paper apply to no single country.
Further, the investigators do not report rates of other outcomes, especially total mortality, associated with drinking. Taking only one outcome condition, without at least noting that moderate drinking has almost uniformly been found to decrease all-cause mortality, limits the usefulness of their results for setting alcohol guidelines. Heavy alcohol use is recognized by all as a serious impediment to the health of individuals, and to society at large. However, recommending lowering the intake of alcohol for everyone does not take into consideration that light drinkers might be more likely than heavy drinkers to follow such advice and might decrease their consumption to zero. Because of moderate drinking’s almost uniformly demonstrated beneficial effect on cardiovascular disease, if many light drinkers stopped drinking completely it would be expected to increase, rather than decrease, total mortality rates and the health of the population.
In their conclusions, the authors only mention the results of their actual analyses briefly, then start the usual chant of the need for extensive public health measures (warning labels, public information campaigns, increasing alcohol taxes, etc.) which tend to emphasize the dangers of any alcohol consumption. However, the analyses in this paper do not provide the data that are needed if one is to set appropriate drinking guidelines, which should be age-specific, sex-specific, and population-specific. Such factors would include not only the alcohol-disease relation but the particular characteristics of the population, the objective of guidelines (to influence and change behavior among target populations), the behavior that is thought to be in need of change, the culture and mindset of the target population, and the kind of message that is likely to be effective. Forum members realize that there are tensions between advice intended only to reduce the prevalence of misuse versus advice that takes into account the well demonstrated beneficial health effects of light-to-moderate consumption. When setting guidelines, it is important to take into account the prevailing drinking culture of a country or population, because only in that way is it possible to produce a public health message that is likely to be respected and regarded.
Reference: Rovira P, Rehm J. Estimation of cancers caused by light to moderate alcohol consumption in the European Union. European Journal of Public Health 2021; pre-publication. doi:10.1093/eurpub/ckaa236.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================
Critique 245: Effects of different patterns of alcohol consumption on risk of mortality, major cardiovascular events, cirrhosis, and cancer — 25 January 2021
This study was designed to determine factors that affect the pattern of alcohol consumption (including the frequency of consumption, type of beverage, with or without food, etc.), rather than just the reported average amount of alcohol, related to all-cause mortality, major cardiovascular events-MACE (MI/stroke/cardiovascular death), accidents/injuries, liver cirrhosis, all-cause and alcohol-related cancer incidence. It was based on a large prospective cohort study of UK Biobank (UKB) participants and included more than 300,000 subjects; outcomes were ascertained over a 9-year median follow-up period. Non-drinkers and only occasional drinkers were excluded from the analyses, so this paper does not judge the effects of light or moderate drinking versus not drinking, but only the effects of the pattern of reported alcohol consumption among regular drinkers.
The study showed that in comparison with subjects who consumed red wine more than 50% of the time (the reference group) there were lower risks of many adverse outcomes than among consumers of more than 50% of the time of spirits; the latter had 25% greater risk of all-cause mortality, 31% greater risk of MACE, and 48% higher risk of liver cirrhosis after controlling for total weekly alcohol consumption and relevant confounders. In comparison with red-wine drinkers, consumers of beer/cider showed an 18% higher risk for all-cause mortality, 16% higher risk of MACE, and 36% higher risk of liver cirrhosis. There were no statistically significant differences in outcomes between white wine drinkers and red wine drinkers.
Consumption of alcohol with food, versus not with food, showed a 10% (CI 2%-17%) lower risk of all-cause mortality. While consumers reporting alcohol consumption 3-4 days/week had lower risk of some adverse outcomes than subjects reporting intake on only 1-2 days/week, for some reasons subjects reporting daily or near-daily intake had an increased risk of liver cirrhosis, probably related to under-reporting by some heavy drinkers.
Forum members agree with the conclusions of this study as reported in the Authors’ Abstract: “Red wine drinking, consumption with food and spreading alcohol intake over 3–4 days were associated with lower risk of mortality and vascular events among regular alcohol drinkers, after adjusting for the effects of average amount consumed.” The results of this well-done study emphasize how inappropriate it is to use just the total average alcohol intake when relating the consumption of alcoholic beverages to the risk of adverse health outcomes.
Reference: Jani BD, McQueenie R, Nicholl BI, Field R, Hanlon P, Gallacher KI, Mair FS, Lewsey J. Association between patterns of alcohol consumption (beverage type, frequency and consumption with food) and risk of adverse health outcomes: a prospective cohort study. BMC Medicine 2021;19:8. https://doi.org/10.1186/s12916-020-01878-2.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 244: Is “ideal cardiovascular health” more common among consumers of wine than among drinkers of other beverages? — 18 December 2020
While a beneficial effect on cardiovascular disease of moderate drinking has been shown repeatedly in epidemiologic studies, the specific effects of different types of alcohol have not been well established. The authors examined the relation between alcohol type and an index of ideal cardiovascular health (CVH) as measured by the American Heart Association’s seven CVH metrics. Data from more than six thousand men and women, participants in the Multi-Ethnic Study of Atherosclerosis, were used to relate the association of the consumption of wine, beer, and liquor to the CVH score.
The authors report that participants who consumed 1-2 drinks/day of wine had higher odds of optimal CVH scores compared to those who never drank wine [adjusted prevalence odds ratio (POR) 1.64 (1.12-2.40)]. However, in comparison with participants who never drank beer or liquor, the odds of optimal CVH scores were lower for consumers of these beverages.
Forum members had some questions about the methodology for judging intake of the different beverages, as well as the statistical approach used in these analyses. However, they consider that the results (more favorable associations with wine consumption than from that of other beverages on indices of cardiovascular health) are in line with most previous studies.
It is important to realize that this study did not measure effects on the risk of disease occurrence or mortality, but just on the CVH index, a measure of overall cardiovascular health. Thus, we cannot tell specifically from this study whether the higher health indices among moderate wine drinkers was the result of the wine that they drink (even though this might be expected to some extent since, for example, moderate wine intake is known to favorably affect BMI, blood lipids, and blood glucose) or that their results relate to the fact that people with more moderate lifestyles and higher education, income, etc., tend to prefer moderate wine consumption and are less likely to be binge or heavy drinkers. It may be that wine drinkers make better decisions on all lifestyle behaviors than consumers of other beverages.
Reference: Ogunmoroti O, Osibogun O, McClelland RL, Lazo M, Mathews L, Okunrintemi V, Oni ET, Burke GL, Michos ED. Alcohol type and ideal cardiovascular health among adults of the Multi-Ethnic Study of Atherosclerosis. Drug and Alcohol Dependence 2020: Pre-publication release
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 243: Does the “quality” of the diet modify the relation of alcohol intake to the risk of hypertension? – 19 October 2020
The authors of this paper test the hypothesis that overall diet quality influences associations between alcohol consumption and the risk of hypertension, based on data from a study in the USA (NHANES) and two studies in China. In general, their designation of a “high-quality” diet for Chinese was one with greater amounts of fruit, vegetables, and beans, while for Caucasians and Hispanics it was one with more whole grains, fruit, vegetables and nuts; “low-quality” diets were mainly those with higher intakes of red meat products. For comparisons with abstainers, subjects reporting < 7 drinks/week for total alcohol were categorized as light and those reporting 7-21 drinks/week categorized as moderate drinkers, with those reporting more referred to as heavy drinkers.
The paper concludes that light alcohol consumption among subjects with a high-quality diet was significantly associated with a decreased risk of hypertension in Caucasians, and the risk of hypertension was not significantly increased with increasing alcohol consumption in Caucasians, Chinese, and Hispanics. On the contrary, in context of a diet calculated to be low quality the risk of hypertension was significantly increased in a linear fashion with increasing alcohol consumption in all groups except African Americans.
Forum reviewers considered this to be a generally well-done and interesting study, but had concern that the authors may not have adjusted adequately for a factor strongly related to diet quality: socio-economic status. The authors included in their analyses whether or not subjects had a high school diploma, but no adjustments were made for occupation, income, or other important indices of deprivation, which may be important since lower SES subjects have consistently been shown to have poorer diets. Thus, we are unsure whether or not it is the diet solely that is the reason that alcohol consumption was found to be associated with lower, higher, or no effect depending on the type of diet. Further, no results are shown indicating whether or not there were differences if the beverage consumed was beer, wine, or spirits, and there was insufficient data on the pattern of drinking. The authors begin their abstract saying that ‘Alcohol is commonly consumed around mealtimes,’ but apparently do not have any data on whether the beverage was consumed with or without food for the present analyses.” All of these factors may modify how alcohol affects the risk of developing hypertension.
Finally, some Forum members were uneasy with the term “quality of diet”, based on the inclusion or exclusion of certain foods, which may be very important to taste. Said one member, we trust that diets recommended as being of “high quality” are not those whose savor has been removed.
Reference: Jiang W, Meng X, Hou W, Wu X, Wang W, Wang M, Chu X, Wang P, Sun C, Han T, Li Y. Impact of overall diet quality on association between alcohol consumption and risk of hypertension: evidence from two national surveys with multiple ethnics. Eur J Clin Nutr 2020; doi.org/10.1038/s41430-020-00708-1.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
=========================================================================
Critique 242: The relation of light alcohol consumption to the risk of common cancers – 1 October 2020
In an attempt to assess the relation between light alcohol consumption (<12.5g per day) and the risk of a number of types of cancer, the authors carried out a review of meta-analyses published within the past 15 years. Using as keywords “light alcohol drinking,” “light alcohol consumption” and “cancer”, they found 29 meta-analyses on the subject. They report their results as indicating that “Light alcohol drinking was not associated with an increased risk of cancer occurrence, with the exception of breast and prostate cancer and melanoma. Furthermore, a possible protective role of light alcohol consumption on the development of bladder, kidney and ovarian cancer and Non Hodgkin Lymphoma was observed.”
Forum reviewers found a number of weaknesses in the paper. While their title focuses on “light alcohol drinking,” most of their reports of results and their discussion deal with harmful effects of heavier drinking; however, by not including papers on ‘heavy drinking’ in their original search, they may have left out many relevant papers. Further, the very brief reviews of each common cancer that they comment upon are sometimes based on only one or two meta-analyses, leaving out a huge amount of key data, especially that from single, well-done, long-term cohort studies with important information on the relation of alcohol to cancer; potential confounding by many factors could not be taken into consideration.
In the analyses in the present paper, the reported average level of alcohol consumed is used, but there is insufficient evaluation of possibly more important indices of alcohol exposure: the pattern of drinking (e.g., type of beverage consumed, in binges or on a regular basis, consumption with or without food, etc.). Further, there is probably inadequate control for important confounders or consideration of the effects of under-reporting, which may have been seen in single studies but not apparent in meta-analyses. In addition, a number of errors are present within the report, such as conflicting statements that may misrepresent the numeric data given. These problems make these results of limited use to professionals in health policy who are developing guidelines for alcohol use in the general public.
Reference: Caprio GG, Picascia D, Dallio M, Vitiello PP, Giunta EF, De Falco V, et al. Light Alcohol Drinking and the Risk of Cancer Development: A Controversial Relationship. Reviews on Recent Clinical Trials 2020;15:164-177
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 241: A Mendelian randomization study of alcohol consumption and the risk of breast cancer and ovarian cancer reveals no significant associations — 22 July 2020
The authors of this ambitious study used a Mendelian Randomization (MR) approach in an attempt to determine if alcohol consumption is causally associated with the risk of female hormone-dependent cancers. They used summary level genetic data from the hitherto largest genome-wide association study (GWAS) conducted on alcohol consumption (N = ~1.5 million individuals), breast cancer (N cases = 122,977) and ovarian cancer (N cases = 25,509). They examined three different alcohol intake exposures: drinks per week, alcohol use disorder (AUD) and age-adjusted alcohol use disorder identification test (AUDIT-C), to reflect general and harmful drinking behavior. For instrumental variables (IVs), they constructed updated and stronger genetic instruments using 99 SNPs related to drinks/week, 9 SNPs related to AUD, and 13 AUDIT-C-related SNPs, and estimated the causal relationship applying several two-sample MR methods.
The key result of these analyses was that the investigators did not find any evidence that alcohol intake increased the risk of breast cancer. For ovarian cancer, an initial inverse association with alcohol intake became null when adjustments were made for confounders. While members of our Forum agreed with the overall conclusions of the authors, who stated that they did not find “any compelling evidence in support for a causal relationship between genetically predicted alcohol consumption and risk of breast or ovarian cancer, consistent across three different alcohol-related exposures,” Forum members identified a number of weaknesses of the analyses. For example, there were very limited data on the pattern of drinking or the type of beverage consumed, and no data on smoking and other lifestyle habits, diet, and many other environmental factors that relate to the effects of alcohol consumption. Further, much of the data utilized to generate the IVs of alcohol exposure were from men, rather than women, although the two conditions being studied are present only in women.
Forum members agreed with the authors about the need to combine data from MR analyses with data from observational and experimental studies before making conclusions about the relation of alcohol consumption to health and disease. Given the rapid expansion of genetic studies, it is likely that MR analyses will be increasingly important in our research efforts, but we agree that the consideration of a combination of data from observational studies, clinical trials, animal experiments, and MR analyses will be needed as we seek to improve our knowledge on the relation of alcohol intake to health and disease; it is, and will remain, a continuing challenge.
Reference: Zhu J, Jiang X, Niu Z. Alcohol consumption and risk of breast and ovarian cancer: A Mendelian randomization study. Cancer Genetics 2020;245:35–41
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 240: Are there health risks from amounts of alcohol referred to as being within “low-risk drinking” guidelines? — 8 July 2020
The authors of this paper use very questionable data to suggest that drinking guidelines for all countries should be lowered to no more than 1 drink/day. In their analyses, they make a very large number of assumptions, including adding 80% to reported amounts of alcohol for all subjects to make up for alcohol disappearance data, and do not modify this according to their individual likelihood of being an under-reporter of intake. Further, they are not able to adjust for the pattern of drinking or type of beverage consumed, and it is considered bizarre that they grouped ex-drinkers (many of whom were apparently heavy drinkers) with current drinkers who report consuming within the guidelines to state that such subjects have a high risk of adverse effects. From the numbers presented in the tables in this paper, the risk of alcohol-attributable death for consumers of alcohol within-guidelines was fifty times lower than for those consuming above the guidelines. Such deficiencies in methodology, and especially possibly deliberate combinations of groups to support their premise, make it impossible to utilize their conclusions for setting guidelines for “low-risk” drinking.
Further, their conclusions do not reflect what the vast majority of well-done epidemiologic studies have shown for decades that light-to-moderate alcohol consumption (when defined as up to 1 drink/day for women and up to 2 drinks/day for men and not consumed in binges) is associated with a significant decrease in the risk of cardiovascular mortality as well as total mortality. The results of the current paper are not sufficient to warrant changing drinking guidelines.
Reference: Sherk A, Thomas G, Churchill S, Stockwell T. Does Drinking Within Low-Risk Guidelines Prevent Harm? Implications for High-Income Countries Using the International Model of Alcohol Harms and Policies. J Stud Alcohol Drugs 2020;81:352–361.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 239: Does the source of funding of epidemiologic studies on alcohol and health affect their results? – 28 May 2020
Funding of research by industry can lead to sponsorship bias. The aim of the current study was to evaluate for sponsorship bias in observational alcohol research by focusing on a spectrum of health outcomes related to moderate alcohol consumption. The authors utilized data from seven recent meta-analyses that included information from 386 observational studies of the relation of moderate alcohol consumption to a large number of health outcomes, including cardiovascular diseases, cancer, and mortality.
The authors report that only 5.4% of studies had some support from the alcohol industry, while 80.1% were funded by governments or other sources (non-industry-funded). Further, the results of moderate drinking on almost all health outcomes (including cardiovascular diseases and cancer) were essentially the same whether the study was funded by the beverage industry or not. Where there were slight differences, the results from non-alcohol-industry sources tended to have more favorable health results from moderate drinking than did those sponsored by the industry. The authors end their discussion stating: “In conclusion, only a small proportion of observational studies in meta-analyses, referred to by several international alcohol guidelines, are funded by the alcohol industry. Based on this selection of observational studies the association between moderate alcohol consumption and different health outcomes does not seem to be related to funding source.”
Forum members considered that the analyses were very complete, and detailed data were given in the very exhaustive supplementary material provided (exceeding 90 pages). (This makes it possible for a reevaluation of their results by others.) While Forum members noted that this analysis was apparently supported by the Dutch Beer Institute, the extensive data presented provide no evidence that there was bias in any of the analyses, upon which most international drinking guidelines have been based. The Forum concludes that the major studies that have shown that moderate drinking can have health benefits, especially for coronary heart disease and type 2 diabetes, are not based on bias because of support from the alcohol beverage industry.
Reference: Vos M, van Soest APM, Wingerden T, Janse ML, Dijk RM, Brouwer RJ, deKoning I, Feskens EJM, Sierksma A. Exploring the Influence of Alcohol Industry Funding in Observational Studies on Moderate Alcohol Consumption and Health. Adv Nutr 2020: pre-publication.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 238: Differences in evaluating confounding in epidemiologic studies when judging the effects of alcohol consumption on the risk of cardiovascular disease – 7 April 2020
The authors of the present paper compared studies included in a recent meta-analysis on alcohol consumption and the risk of coronary heart disease (CHD) for the number of potential confounding variables included in the analysis for each paper. While they found that most studies included adjustments for smoking, age, BMI, height and weight, physical activity, and education, many studies included adjustments for a multitude of other factors. They reach the conclusion that the large variation between studies in adjusting for confounding makes it impossible to accept the finding of a J-shaped curve between alcohol consumption and CHD (despite the consistency of such results).
Forum members agree that evaluating confounders in epidemiologic studies is extremely important. However, standardizing environmental confounders is not possible as there are so many, and so many yet undefined, and these confounders would be expected to vary in their influence among different populations. The authors did not focus on the key factor: the potential impact of each potential confounder. Limited research suggests that any “unknown confounder” would need to be extremely powerful to negate the reported protective effect of light-to-moderate consumption of alcohol, especially of wine, on the risk of CHD.
In addition, the authors were perturbed that many individual studies did not state specifically in their discussion that “residual confounding may be present in our results” or that “results of individual studies must be interpreted with caution.” Forum members assume that most readers of scientific reports realize that there should always be caution in making conclusions from a single study, especially observational studies, without the authors pointing in out in their paper. It may be analogous to stating that “further research is needed,” which should be assumed for any scientific paper.
Members of the Forum acknowledge that confounding makes it a difficult process to judge causality from observational studies, but point out that potential confounders in one study may be insignificant in another. It is not possible to generate a list of potential confounders that would apply to all epidemiologic studies. However, the consistency of the J-shaped curve between alcohol intake and risk of CHD in almost all epidemiologic studies, with support from a multitude of experimental studies, strongly supports the validity of such a relation.
Reference: Wallach JD, Serghiou S, Chu L, Egilman AC, Vasiliou V, Ross JS, Ioannidis JPA. Evaluation of confounding in epidemiologic studies assessing alcohol consumption on the risk of ischemic heart disease. BMC Medical Research Methodology 2020;20:64 https://doi.org/10.1186/s12874-020-0914-6
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 237: Relation of alcohol consumption in the elderly to the chances of reaching 90 years of age — 2 March 2020
An interesting and well-done study from a cohort of aging men in the Netherlands that evaluated how alcohol consumption data collected at 68 – 70 years of age related to the risk that the individual would survive to age 90. The authors report that “The highest probability of reaching 90 was found in those consuming 5–<15g/d alcohol, with RR=1.36 (95% CI, 1.20–1.55) when compared with abstainers.” Further, the authors noted that “Wine intake was positively associated with longevity (notably in women), whereas liquor was positively associated with longevity in men and inversely in women.” They also noted that there was a tendency for a lower chance of living to age 90 for subjects reporting binge drinking.
Forum members were unanimous in considering this to be an excellent study. It adds information on alcohol consumption collected in the elderly (ages 68-70 in this study) and subsequent longevity of life. It tends to counter fears expressed by some that the very elderly must be “protected” from alcohol, as it suggests that there are still health benefits from moderate drinking at all ages. Further, the reduction in risk of cardiovascular diseases is especially important in the elderly. This critique provides references to a multitude of research reports that strengthen the conclusions of the authors that, even among very elderly subjects, moderate drinking is associated with a greater longevity of life.
Reference: van den Brandt PA, Brandts L. Alcohol consumption in later life and reaching longevity: the Netherlands Cohort Study. Age and Ageing 2020;00:1–8 doi:10.1093/ageing/afaa003.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 236. Reasons for apparently diverse results from epidemiologic studies relating alcohol consumption to the risk of breast cancer 19 February 2020
The relation of alcohol consumption to the risk of breast of cancer has been the subject of innumerable epidemiologic studies over many decades, with most showing a slight increase in risk even for light drinking. However, it has been shown that this relation is attenuated when certain potential confounders are adjusted for, including folate levels, frequency of binge drinking, and the use of post-menopausal hormonal therapy. The present paper took the results of a recent large-scale meta-analysis and sought to try and explain why there is a large variability of results when the 97 studies included in that analysis were compared. The authors attempted to judge to what degree differences in exposure definitions, contrast levels, different study populations, different adjustment covariates, and different model approaches affected estimates of the effect of alcohol on cancer risk. The key factor the authors used in their analyses was the ratio between the most harmful and the most protective effects of estimated risk within each study.
All of the contrasts studied (different measures of alcohol consumption, different populations, different analytic approaches, etc.) had some effect on the estimates of effect of alcohol on the risk of cancer. As stated by the authors, “These findings suggest that whereas certain analytical and modelling choices, reflecting different types of alcohol and/or doses, can result in genuine differences, it is possible that many different analytical options, with different results, are pursued and selectively reported. Therefore, individual reported relative risk estimates from observational studies should be interpreted with caution.” Some Forum members disagreed with this conclusion, suggesting that due to marked variation in population, type of alcohol, analytic approaches, adjustment for confounding, etc., considerable error may be built in when combining data from heterogeneous studies. They felt that single large, long-term, well-done individual prospective studies may be preferable for judging the true effect of alcohol on the risk of breast cancer.
Thus, while Forum reviewers appreciated the attempt to explain differences in results of studies to get a more valid estimate of the true relation of alcohol consumption to the risk of breast cancer, and the analyses presented were done appropriately, some considered the approach described as not being a useful or valid one. Finding large differences in effects among sub-groups may not provide a reliable measure. Alternative approaches to scrutinize findings from observational studies, including Mendelian randomization or discussion centered on E-value (which assesses how strong an unmeasured confounder would have be to eliminate observed effect estimates), may be preferable. While such methods are imperfect, their use would be more interesting in informing the public and advancing scientific knowledge.
Reference: Chu L Ioannidis J PA, Egilman AC Vasiliou V, Ross JS, Wallach JD. Vibration of effects in epidemiologic studies of alcohol consumption and breast cancer risk. Inter J Epidemiol 2020;10:1–11. doi: 10.1093/ije/dyz271
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 235: Does type of alcohol or drinking pattern explain greater adverse effects of alcohol consumption among lower socio-economic subjects? 15 January 2020
The authors of this paper aimed to investigate whether and to what extent consumption by beverage type, BMI, smoking and other factors explain inequalities in alcohol-related harm evidenced though wholly attributable alcohol-related hospital admissions (ARHA). They especially evaluated levels of socio-economic status (SES) as determined by geographic and individual levels of deprivation. They based their analyses on data from 11,038 respondents to the Welsh Health Survey who answered questions on their health and lifestyle.
The results of this study support previous research on how factors associated with poor socio-economic status relate to poor health outcomes. It provides added information by providing an expanded definition for deprivation (assessed from geographic area of residence as well as from personal data), and for potential differences by type of beverage consumed. The definition of deprivation included many factors that, together, seem to be the primary reason why poorer, less educated people seem to have more adverse health effects that have been attributed to alcohol consumption.
Specifically, this study shows that the amount of alcohol consumed by people with low SES may be only a minor factor in explaining their increase in adverse effects that are usually classified as being “alcohol-related.” In this study, the frequency of alcohol consumption explained only 4% of the greater number of “wholly attributable alcohol-related hospital admissions.” Co-existing other behaviors and conditions, especially smoking, obesity, living in a deprived environment, poor health status, and mental health, appeared to have much greater effect. Thus, the conclusions of this study suggest that even for what are referred to as “wholly attributable .alcohol-related hospital admissions,” other factors associated with low SES may be more important than alcohol consumption itself as determinants of such adverse health outcomes.
Reference: Gartner A, Trefan L, Moore S, Akbari A, Paranjothy S, Farewell D. Drinking beer, wine or spirits – does it matter for inequalities in alcohol-related hospital admission? A record-linked longitudinal study in Wales. BMC Public Health 2019;19:1651. https://doi.org/10.1186/s12889-019-8015-3
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 234: Effects of red wine consumption on gut microbiota that affect health and disease – 14 November 2019
This brief paper supports earlier research relating wine consumption to gut microbiota, and the relation of the latter to obesity and to cardiovascular and other diseases. The authors report that “Red wine consumption was positively associated in a frequency-dependent manner with ɑ-diversity, but even rare consumption showed an effect. White wine also displayed a lesser but suggestive positive association with ɑ-diversity, while we saw no association with other alcohol categories.” They suggested that these effects of red wine on gut microbiota may play a role in the reduced risk of obesity, cardiovascular disease, and reduced total mortality associated with red wine intake that have been demonstrated in many cohort studies.
An increasing number of studies point to beneficial effects of wine, especially red wine, which may not be present for other types of beverages containing alcohol. However, we agree with the conclusions of the authors: “Red wine consumption should always be studied in the context of the overall dietary habits of individuals to take into account residual confounding and bias. The majority of observational studies fail to do this adequately; and thus, results from large scale clinical trials are needed in order to establish a cause and effect relationship between red wine polyphenols and gut microbiota.”
Forum members consider that the present analyses support a beneficial health effect of regular and moderate red wine, but also agree that much further research will be required to work out the complex relation between the consumption of red wine and gut microbiota and the effects on health.
Reference: Le Roy CI, Wells PM, Si J, Raes J, Bell JT, Spector TD. Red wine consumption associated with increased gut microbiota ɑ-diversity in 3 independent cohorts. Gastroenterology 2019. In press, doi.org/10.1053/j.gastro.2019.08.024
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 233: The relation of alcohol consumption to the development of dementia, with very extensive evaluations of the latter – 7 November 2019
This study was designed to assess the association between alcohol consumption and dementia and the roles of mild cognitive impairment (MCI) and apolipoproteinEε4 (APOEE4) genotype in modifying this association. It was based on data from the Ginkgo Evaluation of Memory Study, conducted from 2000 to 2008 among US community-dwelling participants (which did not demonstrate beneficial effects of ginkgo). The study analyzed 3,021 participants aged 72 years and older who were free of dementia at baseline.
The assessment of alcohol consumption included both the amount and frequency of intake, and the authors had a very broad assessment of potential confounders, including cardiovascular and other diseases, depression, race, ethnicity, educational level, social activity, medication use, and genotype for APOE-E4. There was a very complete and careful attention to the assessment of cognitive function, as subjects underwent numerous and repeated cognitive assessments. For example, if there was any suggestion of cognitive impairment, cerebral magnetic resonance imaging and referral to an expert panel of clinicians, who reviewed and validated presence of dementia, was carried out. No previous studies have had such an extensive assessment of cognition.
The main results include a finding that for the large majority of participants (the 2,548 without mild cognitive impairment at baseline), complete abstention from alcohol was associated with a slightly higher risk of dementia than seen in any of the groups consuming alcohol. For 473 subjects with MCI at baseline, there was no effect on risk of dementia for up to about 10 drinks/week, then a slight but insignificant increase in risk with greater intake. Daily low-quantity drinking was associated with more than 50% lower dementia risk than infrequent higher alcohol consumption. Many of the associations shown had a consistent pattern (a decrease in risk with light drinking) but did not reach statistical significance. The association was similar for all sub-groups, and was not modified by APOEE4 genotype.
The analyses seem well done, and Forum members agreed that, while some of the associations did not reach statistical significance, the data support most previous studies that show a J-shaped or U-shaped association for the relation of alcohol consumption to the risk of dementia. As has been shown in most previous studies, regular (even daily) light drinking was found to be preferable to infrequent higher levels of alcohol consumption in terms of the effect on the risk of dementia.
Reference: Koch M, Fitzpatrick AL, Rapp SR, Nahin RL, Williamson JD, Lopez OL, et al. Alcohol Consumption and Risk of Dementia and Cognitive Decline Among Older Adults With or Without Mild Cognitive Impairment. JAMA Network Open 2019:2(9):e1910319. doi: 10.1001/jamanetworkopen.2019.10319
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 232: Does moderate drinking of alcohol in later life reduce the risk of mortality? 3 September 2019
There are well-known problems inherent in most observational studies of alcohol and health. In addition to having to rely on self-report of intake, these include single-time point consumption assessments, inadequate confounder adjustments, accounting for reverse causation, selection bias, short follow up, residual confounding, and lacking information on chronic health conditions that may mediate the association between alcohol consumption and mortality. Further, there have been a lot of assumptions expounded about the generic fragility of older individuals in terms of alcohol consumption; they are generally without supportive clinical or experimental evidence. For light to moderate intake, the elderly tend to have similar benefits associated with alcohol as younger people, and they are at an age when the risk of mortality is at its peak.
The present study was able to adjust for many of these factors: it describes the risk of total mortality among a large group of older subjects, who were ≥ 56 years of age at the start of a 16 year follow up. They were participants in a nationally representative cohort of men and women in the USA, the Health and Retirement Study. Its strengths, in addition to its large size, is the fact that there were repeated assessments of alcohol so that changes of intake could be evaluated, and the authors were able to judge the potential importance of residual confounding.
The authors conclude that occasional drinking and moderate drinking among older subjects are associated with a lower risk of total mortality. The usual argument that light or moderate drinkers tend to have less severe or fewer common diseases and to enjoy better health and socioeconomic status is addressed in this study, which accounted for time-varying confounders that included smoking, body mass index, income, health/functioning, depression, and chronic diseases. From quantitative bias analysis studies they were able to estimate the effects of residual confounding on their results; the authors conclude that it is very unlikely that residual confounding by unrecorded variables would be the cause of the reduction in mortality associated with moderate drinking. Survival analyses supported notably decreased mortality for moderate drinkers. Forum members considered that this study adds important information about the effects on mortality of moderate drinking in the elderly.
Despite many decades of observational data, animal experiments, and limited clinical trials showing beneficial effects on many diseases and mortality from moderate drinking, it is noted that some researchers appear to be loath to admit to any positive health effects of alcohol. We all appreciate the serious adverse effects of heavy drinking and alcohol use disorders, both on the health of persons and on the community. However, when well-done analyses provide reliable data for light-to-moderate drinkers who do not binge drink, it is disturbing that, even then, some scientists question the observed beneficial results and appear to focus only on warnings about abuse.
There is evidence of a disinclination to admit to any beneficial effects of alcohol in many papers, including this one, which throughout the text seems to accentuate the negative aspects of alcohol. Such statements detract from an otherwise clear report suggesting, as one reviewer stated, that this paper is part research results, part polemic. In the opinion of the Forum, this paper provides strong evidence indicating that elderly people who are light-to-moderate drinkers tend to have a lower risk of mortality.
Reference: Keyes KM, Calvo E, Ornstein KA. Rutherford C. Fox MP, Staudinger UM, Fried LP. Alcohol Consumption in Later Life and Mortality in the United States: Results from 9 Waves of the Health and Retirement Study. Alcoholism: Clin Exper Res 2019;43:1734-1746.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 231: Association of alcohol consumption with obesity: Does moderate drinking increase or decrease the risk of obesity? 20 August 2019
While alcoholic beverages contain calories that are absorbed, the association between alcohol intake and body weight and obesity is unclear. Limited clinical trials have not confirmed a positive association between alcohol intake and weight, and some epidemiologic studies, including prospective cohort studies, show that regular moderate drinkers are less likely to be obese than are abstainers.
The present study uses data from National Health and Nutrition surveys between 2011 and 2016 to evaluate the association between reported amount and frequency of alcohol consumption and weight status. An estimated 78.1 % of males and 70.1% of females (who reported at least one drink in the past year) were classified as “drinkers.” A total of about 36% of US males and 41% of US females were described as “obese” (defined as BMI ≥ 30 kg/m2). The analyses included the level of obesity (Class 1, 2, or 3) as outcomes (with Class II defined as BMI 35-<40 kg/m2 and Class III as BMI ≥ 40 kg/m2) making it possible to judge the effects of alcohol on varying levels of obesity.
The present study reports that male current drinkers versus nondrinkers had 38% lower odds of Class 3 obesity versus subjects with a healthy weight; female current drinkers versus nondrinkers had more than 30% lower odds of Class I, Class II, or Class III obesity In both sexes, more frequent alcohol consumption was associated with less obesity, while heavy alcohol consumption was associated with increased risk of obesity. Females who reported that they were trying to lose weight consumed more than others, but there was not a strong relation between reported attempts to lose weight and outcomes.
Forum reviewers considered this to be a well-done analysis, with adjustments for most common potential confounding variables. It provides some support for previous findings of an inverse association with obesity for light-to-moderate alcohol consumption but an increase in obesity for heavy consumption. The authors state that this is the first study to be able to provide data showing that the magnitude of the inverse association is stronger for higher levels of weight status (Classes 1 to 3).
Forum members noted, however, that this study was based on assessments of different subjects in each wave of the national surveys, rather than on repeated assessments among the same individuals over time. It is clear that repeated recordings of alcohol intake in prospective cohort studies make it possible to obtain a reliable estimate of any changes in alcohol intake that may occur, rather than having to base results on a single measure, such as only a baseline value. Further, members caution that there are many genetic and lifestyle variables associated with the development of obesity, and residual confounding is always a potential problem in such analyses. Thus, while the present paper provides data indicating that more severe obesity may result from higher intake of alcohol, and that light-to-moderate intake may actually lead to a decrease in the risk of obesity, data from cohort studies with repeated assessments of alcohol and body size may provide more precise estimates of effect.
Reference: White GE, Mair C, Richardson GA, Courcoulas AP, King WC. Alcohol Use Among U.S. Adults by Weight Status and Weight Loss Attempt: NHANES, 2011−2016. Am J Prev Med 2019;57:220−230.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 230: An extensive review of the role of dietary constituents (foods, nutrients, and beverages) in the development of diabetes 1 August 2019
Of all lifestyle factors that relate to health and disease, probably the most difficult ones to evaluate are dietary factors, including foods, nutrients, and beverages. The present paper consists of a meta-analysis (an “umbrella” analysis) based on 53 previous meta-analyses from prospective cohort observational studies. This analysis includes 153 adjusted summary hazard ratios on dietary behaviors or diet quality indices, food groups and foods, beverages, alcoholic beverages, macronutrients, and micronutrients related to the incidence of type 2 diabetes. Data from previous meta-analyses on very few foods or nutrients are adequate to clearly determine their effects, but among those that have been identified as reducing the risk of diabetes, high-quality evidence was found only for whole grains, cereal fiber, and alcohol. As for dietary factors that have strong evidence of increasing the risk of diabetes, the authors of this paper identify only red meat, processed meat, bacon, and sugar-sweetened beverages.
Forum members considered this to be a well-done, appropriate analysis in a paper that summarizes well the current scientific literature. Some members were concerned about the number of assumptions that scientists must make when doing a simple meta-analysis, and especially when attempting an umbrella one; they consider it key to also evaluate single, large prospective studies where adjustments for many confounding socio-economic factors are less likely to be important.
Overall, the results of this paper strongly support most of the findings of previous meta-analyses and umbrella analyses and indicate only a few dietary factors for which “high-quality” evidence exists for an association with the risk of developing diabetes. The clearest evidence from the analyses in this paper, which was based only on prospective cohort studies, is that cereal grains and moderate alcohol lower the risk, while meats and sugar-sweetened beverages increase the risk of diabetes.
Given the complexity of evaluating dietary factors for their relation to disease outcomes, it will be useful for future studies to attempt to measure a multitude of foods, beverages, nutrients, and eating patterns, preferably over time, to evaluate further the association with disease. For now, current evidence suggests that cereals, grains, and moderate alcohol (that decrease risk) and meat and sugar-sweetened beverages (that increase risk) have the most consistent data for a relation to subsequent diabetes mellitus.
Reference: Neuenschwander M, Ballon A, Weber KS, Norat T, Aune D, Schwingshackl L, Schlesinger S. Role of diet in type 2 diabetes incidence: umbrella review of meta-analyses of prospective observational studies. BMJ 2019;365:l2368.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 229: A J-shaped curve for the relation of alcohol consumption to the risk of colorectal cancer — 10 July 2019
While heavy alcohol consumption is recognized as a contributor to the development of colorectal cancer (CRC), an increasing number of studies suggest that moderate alcohol consumption may not have an adverse effect on the risk of CRC, or even decrease the risk.
The present paper, a meta-analysis of 16 studies on the relation of alcohol consumption to invasive CRC, was conducted by leading investigators in the field. Forum members consider this to be a well-done study, with a large number of subjects, the ability to use individual level data in their meta-analysis, and the use of appropriate and complete analytic techniques.
The key finding of their study was that there was a J-shaped curve evident in all of their analytic approaches; their results strongly support a J-shaped association for the relation of alcohol intake to CRC: a slightly lower risk of cancer for light to moderate drinkers and an increased risk for subjects reporting an average of 3 or more drinks/day. Further, they found that their results did not vary by age, obesity, smoking, or family history of CRC. Overall, the effects of benefits/harms were somewhat more striking for cancers in the distal colon than in the proximal colon.
Potential mechanisms for heavy alcohol consumption being related to an increase in risk were discussed by the authors. As for moderate drinking decreasing the risk, potential mechanisms are discussed by a Forum member in this critique. He describes active, beverage-specific metabolites other than ethanol that reach the intestine. In particular, our attention goes to the several microbial catabolites which can be formed via our host microbiota in the colon.
The finding of a J-shaped curve between alcohol and CRC is similar to the relation seen for a number of other diseases, including coronary artery disease, ischemic stroke, dementia, and total mortality. While a linear relation between heavy drinking and certain upper aero-digestive tract cancers has been shown, for certain cancers there may be a J-shaped curve of effect, with reductions in risk for light-to-moderate drinkers.
Reference: McNabb S, Harrison TA, Albanes, Berndt S, Brenner H, Caan BJ, et al. Meta-analysis of 16 studies of the association of alcohol with colorectal cancer. Int J Cancer. 2019 Apr 29. doi: 10.1002/ijc.32377. [Epub ahead of print]
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
A Tribute to Elizabeth Barrett-Connor, MD (1935-2019)
It is with great sadness that we have learned of the death on 9 June 2019 of Elizabeth Barrett-Connor, a major contributor to the field of epidemiology for many decades and, especially, to a scientifically balanced and sound appraisal of the relation of alcohol consumption to health. Elizabeth was a member of our International Scientific Forum on Alcohol Research until April 2019, when she retired from the Forum because of ill health.
With degrees from Mount Holyoke College in Massachusetts, Cornell University Medical College, and London School of Hygiene and Tropical Medicine, Elizabeth also had medical training at the University of Texas Southwestern Medical School and the University of Miami in Florida. Joining the faculty at the University of California, San Diego, in 1970, she became a Distinguished Professor of Family Medicine and Public Health.
As described in the UCSD Faculty Profile from her university, “Dr. Barrett-Connor’s research concerned healthy aging with a focus on gender differences and women’s health. Dr. Barrett-Connor was founder and director of the Rancho Bernardo Heart and Chronic Disease Study, begun in 1972, with continuous support (4 MERIT awards) from the NIH. She served as a principal investigator of many multicenter clinical trials, including the Postmenopausal Estrogen/Progestin Interventions trial, the Heart and Estrogen-Progestin Replacement Study, the Raloxifene Use in the Heart study, and the Diabetes Prevention Program Observational Study. She was Past President of the Epidemiology Section of the American Public Health Association (APHA), the Epidemiology Council of the American Heart Association (AHA), the Society for Epidemiologic Research (SER), and the American Epidemiological Society (AES). She was a member of the Institute of Medicine (IOM), and a Master of the American College of Physicians (ACP).”
The author of more than 1,000 scientific publications (starting with articles on shigellosis and sickle cell anemia in the 1960s), during her career Dr. Barrett-Connor made important contributions to many fields, including epidemiology, gerontology, endocrinology, cardiology, gender effects, and lifestyle factors such as physical activity, diet, and alcohol consumption. She was the key individual responsible for maintaining and extracting data from the very long-term follow up of participants in the Rancho Bernardo Study of Healthy Aging. She was honored by the American Heart Association by the establishment of the annual Elizabeth Barrett-Connor Competition for young trainees in epidemiology.
Dr. Barrett-Connor was a highly respected mentor of young trainees and faculty. It is noteworthy that she was an author on at least 22 scientific publications during 2018-2019 that included, just in 2019, titles such as “Hearing impairment and cognitive decline in older, community-dwelling adults,” “Effects of APOE on cognitive aging in community-dwelling older adults,” “Genetic Ancestry Markers and Difference in A1c Between African American and White in the Diabetes Prevention Program,” “Cardiovascular Risk Factors Associated With Venous Thromboembolism,” and “Lifetime physical activity and late-life cognitive function: the Rancho Bernardo study.”
The obituary in the New York Times on 20 June 2019 by Karen Weintraub included a revealing anecdote about Elizabeth’s early days: “According to family lore, she was heading to the train station to take a nursing school entrance exam when she bumped into a friend. ‘You’d make a terrible nurse,’ the friend was said to have told her. ‘You can’t take orders from anybody.’ Acknowledging the truth of her friend’s comment, Dr. Barrett-Connor instead applied to medical school.”
Dr. Barrett-Connor was presented with a large number of awards. For example, all in one year she received awards from The University of Western Australia, the Society for the Advancement of Women’s Health Research, the Society for Epidemiologic Research, the Cleveland Clinic Foundation Department of Cardiology, and Scripps Clinic and Research Foundation.
In 2018, Dr. Barrett-Connor was awarded the Fred Conrad Koch Lifetime Achievement Award by the Endocrine Society with the following comments: “Elizabeth Barrett-Connor, MD, has made paradigm-shifting contributions in endocrine physiology and the role of hormones in disease pathogenesis (focus on gender differences) in cardiovascular disease, diabetes, osteoporosis, and breast cancer. It is hard to imagine the existence of any other individual whose work reflects such staggering impact. The hallmarks of Dr. Barrett-Connor’s enduring success — a driving quest for the truth, rigorous scientific discipline, and a joyful passion — have infused every aspect of her career, whether as investigator, lecturer, teacher, or mentor. She has helped make women more visible in the endocrinology field, not by example of her own shining star, but by her constant recognition of light coming from others.”
In a tribute to Dr. Barrett-Connor in Diabetes Care in April, 2019, former trainee and now Professor at the University of Cambridge in the UK, Kay-Tee Khaw noted: “When asked what her motto or philosophy of life was in an interview for her local newspaper, La Jolla Light, Elizabeth Barrett-Connor’s response was that she did not have any one particular philosophy so much as an attitude: ‘My defining principle is that I am a pathological optimist.’ Boundlessly curious, fearless, challenging, inspiring, and great fun to be with are some of the words her colleagues and mentees might use to describe her.”
In addition to her unbelievable contributions to the scientific literature and as a mentor to countless trainees and faculty, Elizabeth was a close friend to many of us in the Forum, who always enjoyed meeting with her at numerous conferences. She especially appreciated the contributions of good food, wine, and vibrant conversation on such occasions.
Among the number of comments received from Forum members were the following: “Dr. Barrett-Connor enjoyed critical debate, not only of scientific topics but also of politics and cultural issues. At a European conference, Elizabeth was one of the outstanding speakers with a talk on nutritional experiences in the US. When a female colleague from Finland was so moved by a certain theme and started crying Elizabeth commented very politely ‘I don`t like weeping women.’ Elizabeth was a strong woman with a lot of empathy and a lot of humour. She has truly been a wonderful and worldwide ambassador for public health and humanity.”
Stated another member: “Elizabeth argued against some of the best, was a clear, linear thinker, and never wavered in self-confidence. She strongly believed in the scientific method, as stated by Popper: ‘The only reason to have a hypothesis is to try to disprove it. If you couldn’t disprove it, you might be right—not guaranteed to be right, but you might be right.’ It teaches us about humility in science; something we need more of.”
We will sorely miss her
================================================================
Critique 227: A reduced risk of chronic obstructive pulmonary disease (COPD) associated with the intake of some alcoholic beverages – 29 May 2019
Chronic obstructive pulmonary disease (COPD) is a major health problem and cause of death throughout the world. While cigarette smoking is known to be the most important risk factor, there are limited data available on the relation of alcohol consumption to the condition. Given that moderate alcohol intake has been shown to decrease the risk of many inflammatory conditions, it may also affect the risk of COPD, which is associated with marked inflammation of lung tissues.
In the present study, the investigators related total alcohol consumption and intake of specific alcoholic beverages with the risk of COPD, based on data from more than 44,000 Swedish men in a population-based prospective cohort study. A total of 2,177 COPD cases were ascertained during follow up that extended up to 17 years. In their analyses, the authors had data permitting them to evaluate a number of demographic and lifestyle factors as potential confounders (including smoking status and pack-years of smoking, education, physical activity, BMI, and some indices of diet). However, there were very few ex-smokers or current smokers among the non-drinkers, making it somewhat difficult to adequate adjust for cigarette use as a cause of COPD.
Forum members thought that there are a number of deficiencies in this study that somewhat weaken its conclusions; especially important was the lack of ability to consider the pattern of drinking (regular, moderate versus binge drinking). Still, there is a strong consistency between the results of this study (indicating a “J-shaped” or “U-shaped” curve for alcohol intake and COPD) and results from extensive previous epidemiologic and experimental research.
Overall, the cumulative research findings now suggest that pulmonary disease might be included among the “diseases of ageing” that show a reduction in risk among moderate consumers of certain alcoholic beverages. Based on some previous epidemiologic studies and results from numerous experimental studies, data now suggest that, in addition to alcohol, the polyphenols present in wine and some beers may offer protection against COPD. While in the present study red wine consumption was associated with the lowest risk of COPD, Forum members acknowledge residual confounding by other lifestyle factors may still play a role.
Reference: Kaluza J, Harris HR, Linden A, Wolk A. Alcohol Consumption and Risk of Chronic Obstructive Pulmonary Disease: A Prospective Cohort Study of Men. Am J Epidemiol 2019;188:907–991.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 226: Consumption of red wine may lower the risk of lethal prostate cancer —- 16 May 2019
In an analysis from the Health Professionals Follow-up Study, the investigators evaluated the relation of alcohol consumption in their more than 45,000 study participants to the development of lethal prostate cancer. They related alcohol first to the overall risk of prostate cancer among all subjects, and then focused on the 5,182 men who developed non-metastatic prostate cancer to judge their risk of developing lethal prostate cancer or mortality. They judged the alcohol intake both prior to the diagnosis and after a diagnosis of prostate cancer. For reported alcohol consumption among subjects prior to the initial diagnosis of prostate cancer, there was a small (16%) but significant reduction in the risk of lethal prostate cancer among subjects reporting any alcohol consumption, but no significant effects of specific beverages on the risk of lethal prostate cancer. However, total mortality was lower for consumers of total alcohol intake and for most categories of intake for all types of beverage.
When they then related post-diagnosis alcohol intake (after the diagnosis of non-metastatic prostate cancer), the investigators found that red wine consumption was associated with a 50% reduction in the risk of developing lethal prostate cancer or mortality. There were no significant relations between total alcohol consumption or between the intake of other specific beverages and lethal disease.
The authors describe a number of hypotheses by which red wine, with its combination of high levels of polyphenols in addition to alcohol, may have lowered the risk of lethal prostate cancer. And there are numerous basic science experiments that have shown how polyphenols impede the development and growth of cancer cells. Presumably, it was not due to the alcohol in red wine, as similar amounts of alcohol in other beverages did not show a protective effect. While the effects of various polyphenols may play a role, at present the mechanisms of such an effect are not known.
Forum reviewers considered this to be a very well-done study and analysis, with repeated assessments of alcohol intake and essentially complete ascertainment of lethal prostate cancer and mortality. Forum members agree with the conclusions of the authors: “Our results indicate that moderate alcohol intake among men with prostate cancer is not associated with a higher risk of progression to lethal disease or overall mortality. The potential benefit of red wine on prostate cancer progression merits additional research.”
Reference: Downer MK, Kenfield SA, Stampfer MJ, Wilson KM, Dickerman BA, Giovannucci, EL, et al. Alcohol Intake and Risk of Lethal Prostate Cancer in the Health Professionals Follow-Up Study abstract. J Clin Oncology 2019 Pre-publication: : DOI https://doi. org/10.1200/JCO.18. 02462
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 225: Moderate alcohol consumption may lower the risk of chronic kidney disease — 8 April 2019
While numerous studies have found that moderate consumers of alcohol tend to be at a lower risk of developing chronic kidney disease (CKD), potential mechanisms for such an effect are unclear. The present large prospective, population-based, multi-cultural study provides important additional data on the effects of alcohol intake on the initial diagnosis of CKD over many years. It is based on data from the Atherosclerosis Risk in Communities Study and reports the relation of varying levels of alcohol consumption, versus non-drinking, to the incidence of CKD over a 24 year follow-up period.
Among the strengths of the study are the very large number of subjects (n=3,664) who developed CKD during follow up, using advanced methods for diagnosing the disease. Only baseline alcohol intake was used as the exposure and type of beverage or pattern of drinking could not be assessed; however, the authors considered multiple appropriate potentially confounding variables in the analyses, including total energy intake, age, sex, race-center, income, education level, health insurance, smoking, and physical activity. In comparison with the 25% of subjects in their analyses who were life-time abstainers, for subjects reporting all levels of alcohol consumption (≤1 drink per week, 2 to 7 drinks per week, 8 to 14 drinks per week, and ≥15 drinks per week), there was a statistically significant decrease in risk of incident CKD (from a 12% decrease in risk for the lowest category of alcohol intake to a 29% decrease for subjects reporting that they consumed 8-14 drinks/week).
The authors conclude: “Consuming a low or moderate amount of alcohol may lower the risk of developing CKD. Therefore, moderate consumption of alcohol may not likely be harmful to the kidneys.” Forum members agree that this study supports much earlier research showing a protective effect of moderate drinking on the risk of kidney disease. While mechanisms are not clear, effects of alcohol on renal vessels that are similar to those described for coronary and cerebrovascular arteries may play a role.
Reference: Hu EA, Lazo M, Rosenberg SD, Grams ME, Steffen LM, Coresh J, Rebholz CM. Alcohol Consumption and Incident Kidney Disease: Results From the Atherosclerosis Risk in Communities Study. J of Renal Nutrition, 2019, in press. DOI: https://doi.org/10.1053/j.jrn.2019.01.011
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 224: A brief summary of the association between wine/alcohol consumption and health in diabetics 12 March 2019
Diabetes mellitus is an increasingly common condition throughout the world, related closely to increases in obesity and ageing of populations. There are many, serious health conditions associated with diabetes, especially a marked increase in the risk of morbidity and mortality from cardiovascular disease. Scientific data from well-done cohort studies have demonstrated for decades that people who are moderate consumers of alcohol tend to have a considerably lower risk of developing diabetes in the first place, and diabetics who consume moderate amounts of alcohol are, in comparison with abstainers, at much lower risk of developing cardiovascular disease.
The present “mini-review” by scientists who have previously carried out the first large randomized clinical trial of wine and health outcomes among diabetics provides an interesting overview of the association of alcohol, particularly of wine, with health. The authors expand the implications of their research and conclude that “Initiating moderate alcohol consumption among well controlled persons with type 2 diabetes is apparently safe, in regard to changes in heart rate variability and carotid plaque formation.” Their findings have stimulated this critique by our Forum to also consider if available data now suggest that physicians should encourage the modest consumption of wine with food for selected patients with diabetes.
Our critique describes a number of risk factors (lipid levels, glucose, insulin, etc.) and intermediate conditions (such as endothelial function and arterial calcification) that have been shown to relate to the consumption of alcohol. Some Forum members believe that while all of these associations are important, the key information needed is the effect of alcohol consumption on disease outcomes themselves (coronary heart disease, stroke, dementia, etc.) and on mortality. At present, any recommendations regarding alcohol consumption must be based primarily on observational data from long-term cohort studies.
The key question we discuss in this critique is “Should physicians advise their older diabetic patients who are non-drinkers to begin to consume small amounts of an alcoholic beverage?” The consensus of Forum members is that current data suggest that, at a minimum, we should not advise such patients who currently consume alcohol moderately to stop their consumption. On the other hand, most members emphasize that we should discuss alcohol consumption with all patients. If they are at least occasional consumers of alcohol (the large majority of patients in most Western countries), our only advice might relate to the pattern of drinking. At present, the pattern commonly shown to be associated with the lowest risk of the usual diseases of ageing and mortality appears to be small amounts of alcohol, especially wine, with meals on a regular basis. For patients who indicate that they are drinking only in binges, we should emphasize the adverse health effects (for them as well as for society), and encourage a healthier pattern of drinking.
But what about current non-drinkers? For middle-aged or older non-drinkers who avoid alcohol because of religious prohibitions, previous misuse of alcohol, certain medical conditions, or a stated dislike of alcohol, our advice on prevention of disease should focus on not smoking, getting exercise, eating a healthy diet, and trying to avoid obesity. But for patients without such conditions that would indicate that they should avoid alcohol, many Forum members believe that they should at least be told of the current scientific evidence of possible beneficial health effects of regular, moderate intake. However, until considerably more data on its effects are available, we are not encouraging physicians to prescribe alcohol consumption for their diabetic patients.
Reference: Golan R, Gepner Y, Shai I. Wine and Health–New Evidence. Mini Review. European Journal of Clinical Nutrition. https://doi.org/10.1038/s41430-018-0309-5; 2019: in press.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 223: A new major review of the relation of alcohol consumption to the risk of dementia. 17 January 2019
While many studies have shown that excessive alcohol intake is associated with cognitive impairment and increased risk of dementia, most cohort studies have shown that the risks of these outcomes are lower among light-to-moderate drinkers than among abstainers. The authors of this paper conducted a scoping review on this topic, based on a systematic search of systematic reviews published from January 2000 to October 2017. A total of 28 systematic reviews were identified relating alcohol intake at various time periods to incidence of cognitive impairment/dementia, specific brain functions, or induced dementias. The authors report that light to moderate alcohol use in middle to late adulthood was associated with a decreased risk of cognitive impairment and dementia, but heavy alcohol use was associated with changes in brain structures, cognitive impairments, and an increased risk of all types of dementia.
Forum members considered this to be a well-done analysis, but were concerned that the focus was only on the potentially adverse effects of heavy drinking, with little regard or discussion of the findings of protection against such cognitive outcomes among light or moderate drinkers. Forum members point out that there are very many adverse health effects, both for the drinker and for society, resulting from heavy drinking. To them, the most interesting and provocative aspect of this paper was the conclusion of a protective effect against cognitive decline and dementia associated with light-to-moderate alcohol consumption.
Scientific data, including the results of the present systematic analysis, are very consistent in showing that cognitive decline, associated impairments in the functions of daily living, incident dementia, and survival are all associated favorably with light-to-moderate consumption of alcohol in middle age. The reasons and mechanisms that lead to these associations deserve further evaluation. With the increasing ageing of populations throughout the world, cognitive decline and dementia are expected to increase and create serious challenges for health care providers. Insight into ways of preventing or delaying the onset of such cognitive decline (in addition to decreasing the prevalence of heavy alcohol intake, the focus of this paper) could be extremely important in planning for the future.
Reference: Rehm J, Hasan OSM, Black SE, Shield KD, Schwarzinger M. Alcohol use and dementia: a systematic scoping review. Alzheimer’s Research & Therapy 2019; 11: pre-publication. https://doi.org/10.1186/s13195-018-0453-0
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 222. A new analysis relating alcohol intake to coronary heart disease – 20 December 2018
In an attempt to judge the effects of alcohol on the risk of coronary heart disease (CHD), the authors have carried out analyses using a sample of subjects from the National Epidemiologic Survey on Alcohol and Related Conditions III (NESARC-III). They based their exposure to current alcohol use on a single assessment at baseline of self-reported consumption during the past year, when the subjects were an average of 38.9 years of age. In addition they asked subjects if they had consumed larger amounts of alcohol when they were younger.
Their assessment of CHD was based on answers to questions at baseline as to having been told by a doctor that they had chest pain or CHD, apparently within the same 12-month period when they were asked about current alcohol consumption. Nothing in the paper indicates that the authors had data on the subsequent development of CHD during a follow-up period. When relating reported alcohol intake to CHD, they excluded 1,671 who reported “previous CHD,” although for this relatively young group it is questionable how many actually had CHD, as no data on validation of the diagnosis was done. For unclear reasons, for their comparison group they excluded any subjects with conditions that “may increase the risk of CHD (e.g., pneumonia, influenza, tuberculosis, liver disease, neurologic conditions, osteoporosis, arthritis, STD) and can be viewed as comorbid conditions related to alcohol consumption.”
Given that the exposure (alcohol) and outcome (CHD) were apparently from the same time period, there is reason to worry about reverse causation (i.e., subjects may have developed CHD and changed, either decreased or increased, their alcohol consumption during the same period).. As for using the self-reported amount of alcohol consumed at some time in the past as the exposure, there is a large chance of serious misclassification of exposure due to recall bias and bias according to current alcohol intake (as subjects currently reporting greater amounts of alcohol were more likely to report even higher intake in the past).
With only a single assessment of current alcohol intake, an inadequate assessment of long-term alcohol intake, a lack of data during a follow-up period for the main outcome, CHD, and no validation of the outcome, Forum members considered that this was an unusual cohort to use when attempting to judge the relation of changes in alcohol consumption to the development of CHD. The necessary elements for a useful analysis were not available to these investigators using this population sample.
In any case, results from many well-done long-term cohort studies with repeated assessments of alcohol and validated CHD outcomes during follow up have already provided key data on this topic: they almost uniformly demonstrate that light-to-moderate drinkers who do not binge drink have significantly lower risk of developing CHD. The present analysis does not provide data that would question such findings.
Reference: Fan AZ, Ruan WJ, Chou SP. Re-examining the relationship between alcohol consumption and coronary heart disease with a new lens. Pre-publication. Preventive Medicine 2019;118:336=343.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 221: The relation of alcohol intake to stomach cancer – 20 November 2018
There have been conflicting results from studies of the association between alcohol intake and the risk of gastric cancer. Some of the differences among studies have related to mixing subjects from Western countries with those from Asia, where dietary patterns, lifestyle factors, drinking patterns, and types of alcohol consumed differ from those among Western populations. Results usually differ between Asian and Western populations.
The present study is based on almost 500,000 subjects from the USA with follow up for a median of 15.5 years. The investigators identified a total of more than 1,300 cases of gastric cardia cancer (GCA) or gastric noncardia cancer (GNCA ). The authors report: “We found no association between higher alcohol consumption and GCA or GNCA, when examined as total alcoholic beverage intake or individual beverage types of beer, wine and liquor. Furthermore, we observed no association by stratum of sex, ethnic group, educational level or smoking status. We did, however, observe lower risk of GNCA among participants who drank up to one drink per day (HR = 0.81, 95% CI: 0.67–0.97) compared to nondrinkers.” They conclude: “Alcohol consumption was not associated with increased risk of GCA or GNCA in this large U.S. cohort.”
Forum members considered this to be a large, very well-done analysis; subjects were aged 50-71 years at baseline, appropriate for evaluating the risk of gastric cancer. Data on a large number of potential confounders were included in the analysis. Diagnosis of cancer was from state cancer registries, shown to be very accurate. The statistical analyses included restricted spine analysis to test for a dose-response curve (not found), and excluded the first two years after alcohol assessment to lower the risk of reverse causality. Further beverage-specific analyses were carried out, and did not show differences according to whether the consumption was of beer, wine, or spirits.
Weaknesses included only one assessment of alcohol intake, at baseline, and no data on binge drinking or other aspects of the pattern of drinking. Subjects were generally well-educated, white, and consumed alcohol moderately (75% reported one drink or less). Thus, these results may not pertain to other ethnic groups or to heavier consumers of alcohol.
Overall, these results provide further support for the lack of an association between light-to-moderate alcohol intake and the risk of gastric cancer. The significant decrease in risk of gastric non-cardia cancer associated with consumption of up to one drink/day should obviously be replicated, but the authors provide some potential mechanisms that could explain such a phenomenon. The study did not support previous data suggesting that wine consumption might have additional benefits to those of other beverages in terms of cancer risk.
Reference: Wang SM, Freedman ND, Loftfield E, Hua X, Abn CC. Alcohol consumption and risk of gastric cardia adenocarcinoma and gastric noncardia adenocarcinoma: A 16-year prospective analysis from the NIH-AARP diet and health cohort. Int J Cancer 2018; pre-publication.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 220: An unusual analysis relating alcohol intake to mortality – October 16, 2018
The authors of this treatise on alcohol consumption and mortality combined, for an unclear reason, results from two, very different studies: one from the Veterans’ Health Administration, based on outpatient clinical medical records, and the other from a national survey in the USA [The National Health Interview Survey (NHIS)]. Unfortunately, the VA data did not adjust for tobacco use or other important lifestyle habits, and are not useful in judging the effects of alcohol consumption on mortality.
While the NHIS survey included data on potential confounding, both it and the VA study based their analyses on a single estimate of alcohol consumption. The authors then created a variable that they stated was associated with the lowest risk of mortality and compared results from such alcohol intake with data from subjects reporting less or more alcohol. They combined data on all subjects reporting 1 to 2 drinks/week, so did not have the ability to provide a precise estimate of the association between low levels of intake and mortality risk. They did not comment on the effects that under-reporting of alcohol would have on their studies (and most investigators agree that the self-reported level of alcohol consumption is usually an under-estimate of actual consumption). Further, they did not point out the very much higher risk of mortality of non-drinkers, compared with moderate drinkers, demonstrated in their data.
To the extent that people accurately reported their past drinking status (never vs former), this study should put to rest concerns that protective associations of drinking versus non-drinking arise from inclusion of former drinkers into non-drinking groups. Never drinkers had higher risk of mortality than former drinkers in this study.
There are considerable data from many well-done cohort studies that have repeated assessments of alcohol intake over many decades and the subsequent risk of mortality. Such studies provide very clear and consistent results indicating a J-shaped curve: lower risk of mortality for light and moderate drinkers than for non-drinkers (even lifetime abstainers) and some increase in risk for heavy drinkers. These are the studies that can provide reliable information upon which drinking guidelines for different individuals and populations can be based.
Reference: Hartz SM, Oehlert M, Horton AC, Grucza RA, Fisher SL, et al. Daily Drinking Is Associated with Increased Mortality. Alcoholism: Clin & Experimental Research 2018; pre-publication. DOI: 10.1111/acer.13886.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 219: A global overview of alcohol consumption and health – 3 September 2018
Investigators working with data from the Global Burden of Diseases, Injuries, and Risk Factors Study 2016 have combined data from 195 locations around the world, from 1990 to 2016, for both sexes and for 5-year age groups between the ages of 15 years and 95 years and older. Their purpose was to determine how estimates of the prevalence of current drinking, abstention, the distribution of alcohol consumption among current drinkers in standard drinks daily (defined as 10 g of pure ethyl alcohol) relate to alcohol-attributable deaths and disability-adjusted lifeyears (DALYs). The paper does not present estimates of the effects of alcohol on a key outcome, total mortality.
The paper presents a huge number of analyses with data specific for each contributing center. However, the Forum considers that real problems emerge when they attempt to combine data from many divergent cultures to determine a single association between alcohol consumption and health. Many lifestyle and cultural factors strongly modify the relation of a given amount of alcohol to health and diseases. Such modifying factors include especially the socio-economic status of the individual, circumstances such as drinking with or without food, the pattern of drinking (regular moderate versus binge drinking), the type of beverage (e.g., wine versus spirits), the intention of the individual (drinking to get drunk versus drinking to enhance meals), level of physical activity, etc. When such modifying factors are not taken into consideration, the estimated intake of a given amount of alcohol (even if accurate), provides an incomplete assessment of the effects of alcohol on health.
The authors spend much of their paper focusing on their contention that these analyses have large implications for setting alcohol policy around the world. They then expand primarily on ways of decreasing alcohol intake world-wide through changes in guidelines. However, their failure to consider specifics of the culture for which the policy is being formulated, such as evaluating other lifestyle factors, the pattern of drinking, underreporting of alcohol intake, cultural factors, etc., negates their ability to provide useful information that is applicable to any single population: their guidelines end up applying to no one. And, their specific statement that zero consumption would be preferable everywhere is sharply contradicted by consistent reports from very large, well-done cohort studies (where individual data are available) which indicate that non-drinkers have higher risks of cardiovascular disease and total mortality than regular moderate drinkers who do not binge drink.
Setting guidelines for the public regarding alcohol consumption requires information not only on the reported intake but on other health conditions, as well as genetic, lifestyle, and cultural factors that may modify the effects of alcohol. Further, advice differs by age and the key problems within a country that the guidelines are directed toward improving. In the opinion of the Forum, despite the massive amount of work done by the investigators in the preparation of this paper, the overall combined results from such divergent populations have little applicability in setting guidelines that would lead to avoidance of alcohol abuse in any specific group of people around the world — they apply to no specific population.
Reference: GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. www.thelancet.com Published online August 23, 2018 http://dx.doi.org/10.1016/S0140-6736(18)31310-2
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here
================================================================
Critique 218: Long-term study of alcohol intake and the risk of Alzheimer Disease or other types of dementia – 21 August 2018
While there is general agreement that the moderate intake of alcohol is associated with a significantly lower risk of cardiovascular disease, there are less data on the relation of moderate alcohol consumption to dementia. However, the vast majority of well-done prospective studies indicate that, in comparison with non-drinkers, moderate, non-binge-drinking older adults have lower risk of Alzheimer Disease and other types of dementia. The present study provides important information on this association by monitoring for the development of dementia among subjects in a large cohort of British civil servants (the Whitehall Study) over more than two decades; there were repeated assessments of alcohol consumption.
The main results indicate that abstinence in middle life is associated with a significantly higher risk of dementia than the risk among moderate drinkers, while subjects reporting the intake of larger amounts of alcohol or evidence of an alcohol use disorder are at increased risk of dementia. Specifically, the study shows that among the 397 cases of dementia that were recorded over a mean follow up of 23 years, abstinence in midlife was associated with a 47% higher risk of dementia compared with consumption of 1-14 units/week (a British unit is the equivalent of 8 grams of alcohol). There was a 17% increase in risk of dementia for those reporting more than 14 units/week. With repeated assessments of alcohol the authors also calculated trajectories of alcohol consumption from midlife to early old age, with continued abstinence being associated with an increase in dementia of 74% and a decrease in consumption with an increase of 55% in comparison with subjects reporting continued moderate consumption. In several analyses, wine consumption was associated with more favorable effects than those of other beverages.
Forum members thought that this was a well-done analysis, but considered that the data presented do not allow for a firm determination of a cut-point for increased risk of dementia from alcohol intake. While the authors provide estimates of a linear increase in dementia risk for subjects reporting more than 14 units/week or reporting evidence of alcohol abuse, they do not give data that permits an estimate of the level of intake where the risk of dementia exceeds that of non-drinkers.
Overall, the results showing a decreased risk of dementia for moderate drinkers support the findings from most well-done prospective cohort studies. As for implications for policy, the study further shows that, in terms of the risk of dementia as well as cardiovascular disease, middle-aged and older individuals who are consuming alcohol moderately and without binge drinking should not be advised to stop drinking.
Reference: Sabia S, Fayosse A, Dumurgier J, Dugravot A, Akbaraly T, Britton A, Kivimäki M, Singh-Manoux A. Alcohol consumption and risk of dementia: 23 year follow-up of Whitehall II cohort study. BMJ 2018;362:k2927. http://dx.doi.org/10.1136/bmj.k2927
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================
Critique 217: Alcohol, cancer, and mortality: Further affirmation of the J-shaped curve for mortality and increase in incidence of cancer with larger intake of alcohol – 9 July 2018
Scientific studies have shown consistently that that the consumption of small amounts of alcohol on a regular basis is associated with a lower risk of total mortality, while consumption of large amounts is associated with an increased risk of certain cancers and mortality. The present report is from a population-based cohort study of almost 100,000 older subjects who were followed for a median of 8.9 years. There were large numbers of deaths (n=9,599) and incident cancers (n=12,763) diagnosed during follow up, which should lead to more precise estimates of effect.
The authors report that light-to-moderate drinking was associated with lower total mortality, but the risk of incident cancer increased with greater alcohol consumption, especially the intake of beer or spirits. However, the analyses indicate that the slightly increased risk of cancer associated with moderate alcohol consumption was less than the beneficial effect on mortality.
Specifically, in comparison with never drinkers or very light (< 1 drink/week) drinkers, the study shows lower mortality for “light-to-moderate” alcohol consumers (up to 2 drinks/day) but greater mortality among subjects classified as “heavy” (2 to < 3) or “very heavy” (3+ drinks/day) consumers. In beverage-specific analyses, there was a slight increase in total mortality for reported intake of spirits starting at the consumption of about 1 ½ drinks/day and for beer at or above about 2 drinks/day; no significant increase in cancer risk was associated with wine consumption, regardless of the amount. The authors conclude that “there is a J-shaped association between alcohol and mortality in older adults, which remains after adjustment for cancer risk.”
Forum member considered this to be a well-done analysis, and shows, essentially for the first time in a single study, how the beneficial effects of light and moderate drinking on cardiovascular disease and total mortality exceed the slight increase in cancer risk for alcohol consumption at this level. In other words, while even light-to-moderate drinking may be associated with a slight increase in the risk of certain cancers, such drinking still favorably affects the overall risk of mortality.
Reference: Kunzmann AT, Coleman HG, Huang W-Y, Berndt SI. The association of lifetime alcohol use with mortality and cancer risk in older adults: A cohort study. PLoS Med 2018;15:e1002585. https://doi.org/10.1371/journal.pmed.1002585.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================
Critique 216: Strong effects of five lifestyle factors on risk of mortality and longevity of life – 31 May 2018
It has long been known that a number of lifestyle factors – such as not smoking, being physically active, avoiding obesity – decrease the risk of many of the “diseases of ageing,” especially cardiovascular disease and cancer. The present paper from the Nurses’ Health Study and the Health Professionals Follow-up Study is especially important as it demonstrates the joint effects of five healthy factors on disease-specific and total mortality in very large cohorts of subjects. The “healthy lifestyle factors” evaluated were (1) never smoking, (2) body mass index of 18.5 to 24.9 kg/m2, (3) ≥30 min/d of moderate to vigorous physical activity, (4) moderate alcohol intake, and (5) a high diet quality score (upper 40%). The similarity in education and other socio-economic factors of the subjects in these studies tends to reduce potential confounding by such factors.
There were more than 42,000 deaths in their cohorts during follow-up periods extending up to 34 years. The effects of these factors on subsequent risk of mortality were striking: for subjects meeting criteria for all five factors versus none, there was an 84% reduction in all-cause mortality, 65% less cancer mortality, and 82% less cardiovascular disease mortality. The overall effect was associated with 12 to 14 additional years of life after age 50 for subjects meeting criteria for all five factors.
Forum members consider this to be an excellent study, as it was based on data from very large cohorts of well-monitored subjects over many decades, with essentially full ascertainment of mortality. This study strongly suggests that the leading causes of premature death throughout the developed world are, to a large extent, preventable.
Reference: Li Y, Pan A, Wang DD, Liu X, Dhana K, Franco OH, Kaptoge S, Di Angelantonio E, Stampfer M, Willett WC. Hu FB. Impact of Healthy Lifestyle Factors on Life Expectancies in the US Population. Circulation 2018;137:00–00. (Pre-publication). DOI: 10.1161/CIRCULATIONAHA.117.032047.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 215: Long-term effects of smoking and moderate drinking on the quality and longevity of life of elderly women — 9 May 2018
While essentially all epidemiologic studies have shown adverse health effects of cigarette smoking and beneficial effects of moderate alcohol consumption, the present study is important as it follows a cohort of elderly women into very old age. It is a prospective cohort study of 9,704 women at least 65 years of age, who were living independently at baseline and were not heavy drinkers; they had a mean baseline age of 71.7 years (range 65-99) and underwent repeated assessments of lifestyle habits starting in 1986 to 1988. They were followed longitudinally until death, loss to follow-up, or to April, 2016. Outcomes included grip strength, walking speed, prevalence of threshold scores for self-reported health, difficulty with three or more instrumental activities of daily living (IADLs), depression, prevalence of falls, living in a nursing home, and death after 10- or 20-year follow up. The main comparisons evaluated in this study were between women who were smokers and those who consumed alcohol moderately, with each analysis adjusted for the other exposure.
Forum members considered this to be a well-done study that provides some important data relating effects of smoking and moderate drinking on function and mortality in very elderly subjects (an age group where data are lacking). There were criticisms that the study does not report the effects of moderate drinking among smokers; previous studies have shown that the adverse effect of smoking is modified by moderate alcohol intake. Further, given that the reasons why some women quit drinking during follow up are not known, the article does not contribute to clarification of the problem of reverse causation (e.g., healthier women may tend to continue drinking whereas sicker women stop alcohol consumption). Also, the authors did not adjust for some strong confounders, especially those related to socio-economic status (SES).
Nevertheless, the results of this study make a real contribution to our knowledge of the effects of drinking on both quality of life and mortality among women who are 65 years or older. The follow up of subjects continued for a least 20 years, by which time almost 70% of the women had died. Hence, the effects on mortality should be excellent estimates. As expected, women who were smokers had greater risk for almost all adverse outcomes, while drinkers who continued to consume moderate alcohol into old age had the most favorable outcomes. While the authors report that women who reported drinking at baseline but quit later on had mortality risks that were intermediate between non-drinkers and persistent drinkers, the reasons why some women quit drinking were not known. Hence, it is appreciated that continued drinking could be only a marker of better health, and not the cause.
Reference: Nelson HD, Lui L, Ensrud K, Cummings SR, Cauley JA, Hillier TA. Associations of Smoking, Moderate Alcohol Use, and Function: A 20-Year Cohort Study of Older Women. Gerontology & Geriatric Medicine 2018;4:1–9. Pre-publication.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 214: Some methodologic problems in a recent paper urging changes in drinking guidelines – 23 April 2018
Using individual-participant data from a number of large studies, predominantly from the UK and other European countries, the authors of the present paper have estimated the association between the reported level of alcohol intake among drinkers with cardiovascular outcomes and mortality. They conclude that the lowest risk of these outcomes is from the intake of less than 100 g of alcohol per week, and that guidelines for the public should reduce the upper limits for the amount of alcohol that could be safely consumed.
Forum members identified a number of flaws in these analyses, including failure to separate advice for men versus women or for older adults versus young people. Further, the authors do not point out the effects of under-reporting of intake, the marked differences in many health effects according to type of alcoholic beverage (such differences are shown only in their supplement but not mentioned in the abstract); also, there is little discussion of the importance of the pattern of drinking on health results.
Most important, by excluding never-drinkers as a reference group in their main analyses, the authors essentially eliminated the ability to evaluate for any potentially beneficial (or adverse) effects of light-to-moderate drinking as compared with non-drinking. This is problematic, as in essentially all previous large studies, moderate drinkers are those for whom significant and large benefits have been reported for risk of cardiovascular disease and total mortality.
Guidelines for the public regarding alcohol intake relate to many factors, including the net overall physiologic effects on health as well as the particular needs of different countries and cultures. And, as in this study, the inclusion of results from so many different cultures is a problem for determining appropriate guidelines for alcohol intake. Given that culturally specific drinking patterns, type of beverage, and many other lifestyle factors modify the health effects of alcohol, mixing data from markedly different cultures may give results that may not be appropriate for any specific population.
Reference: Wood AM, Kaptoge S, Butterworth AS . . . John Danesh, et al, for the Emerging Risk Factors Collaboration/EPIC-CVD/UK Biobank Alcohol Study Group (120 authors). Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet 2018;391:1513-1523.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 213: A meta-analysis on lifestyle factors, cardiovascular disease, and total mortality for a very large number of middle-aged and elderly women – 27 March 2018
Overall, Forum members considered this to be a well-done paper that provides additional information on alcohol’s effects on CVD and mortality among a very large number of middle-aged or elderly women. Although women markedly increase their risk of CVD following menopause, this is a group of women for whom data are sparse. Weaknesses of the analysis include a lack of information on the pattern of drinking (binge versus regular), type of beverage, and drinking alcohol with or without food. It is of note that in some of the studies included in the meta-analysis, factors such as HDL-cholesterol and fibrinogen were adjusted for in the study; given that these are mechanisms of alcohol’s effects, overall results will surely underestimate the effects. Further, as the authors point out, this study provides little information on the physiologic mechanisms of alcohol’s effects on health.
Forum members praised the authors for this meta-analysis of a very large dataset. It strengthens previous analyses that show that each of the lifestyle factors considered – not smoking, not becoming obese, being physically active, and regularly consuming small to moderate amounts of alcohol – benefit health. The more healthy lifestyle factors a subject has, the greater the benefit.
It will be especially important that future research evaluates what happens if subjects change their lifestyle habits, as such results would help target specific behavioral changes. There are very limited data available on this at present, but such studies that have been done suggest that the onset of moderate drinking among non-drinkers, or a slight increase in alcohol consumption among light drinkers, have beneficial effects on health. Still, it is appreciated that moderate alcohol consumption is only one of a number of factors making up a “healthy lifestyle,” which is clearly associated with less cardiovascular and other diseases and a much lower risk of mortality.
Reference: Colpani V, Baena CP, Jaspers L, van Dijk GM, Farajzadegan Z, Dhana K, Tielemans MJ, Voortman T, Freak-Poli R, Veloso GGV, Chowdhury R, Kavousi M, Muka T. Franco OH. Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: a systematic review and metaanalysis. European Journal of Epidemiology 2018; pre-publication. https://doi.org/10.1007/s10654-018-0374-z
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 212: Is it the alcohol or other substances in wine that lead to beneficial health effects? — 15 March 2018
While epidemiologists have long noted that consumers of wine tend to have better health outcomes than consumers of other alcoholic beverages, it has always been of concern that we were comparing drinkers, and not the drink itself. In recent years, many basic scientists have evaluated the non-alcoholic constituents in wine, and most studies show beneficial health effects from polyphenols and other components in wine as well as beneficial health effects from the alcohol in wine.
The present study provides an excellent review of clinical trials that compared the effects of wine versus no intervention or versus the effects of other alcoholic beverages. The specified outcomes related to effects on lipids, glucose/insulin metabolism, hemostatic mechanisms, and inflammatory/endothelial systems. The authors conclude that “The most repeated result of wine consumption is on lipid metabolism, attributed mainly to ethanol, while wine micro-constituents seem to have an important role mainly in haemostatic and inflammatory/endothelial systems.” Forum members cite several other important effects of wine micro-constituents, including demonstrated effects of such components at the cellular, molecular, and gene levels to sustain increased fibrinolytic activity, which is closely related to the development of cardiovascular disease.
Forum members were unanimous is considering that this was an excellent review of human clinical trials on the topic; the paper does not, however, comment on the mechanisms by which micro-constituents may operate to improve health. Given that since virtually none of the wine micro-constituents circulates in the human biofluids in their native form, it is especially important that the catabolites of wine micro-constituents be better defined and evaluated.
Overall, current data indicate that wine may be especially effective in lowering the risk of cardiovascular disease not only through the alcohol it contains, but also from a number of its key polyphenols. Forum members also point out that, for beneficial health effects of any type of alcoholic beverage, the pattern of drinking is especially important: the consumption of small or moderate amounts on a regular basis, and preferably with food.
Reference: Fragopoulou E, Cholevaa M, Antonopoulou S, Demopoulos CA. Wine and its metabolic effects. A comprehensive review of clinical trials. Metabolism Clinical and Experimental 2018;83:102-119.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 211: Effects of alcohol and aldehydes on DNA and risk of cancer; potential implications from a study in mice — 22 January 2018
The authors of this paper, based on an extensive basic scientific experiment in mice, describe the features and mutational landscape of DNA damage caused by acetaldehyde, an endogenous and alcohol-derived metabolite. This damage results in DNA double-stranded breaks that, despite stimulating recombination repair, also cause chromosome rearrangements. Furthermore, the authors identify how the choice of DNA-repair pathway and a stringent p53 response limit the transmission of aldehyde-induced mutations in stem cells.
Forum members considered this to be a well-done series of experiments that add additional data on the effects of aldehyde on cellular damage, which could potentially lead to an increased risk of cancer. While interesting, these results in mice have limited applicability to the effects of alcohol in humans, as the study conditions do not correspond to that found in real life. For example, the levels of ethanol used to elicit the DNA changes were high and alcohol was directly injected into the animals, whereas in humans alcohol is orally absorbed and undergoes several types of metabolism that reduce maximum blood alcohol concentrations achieved. Further, the animal model was based on mice that had been genetically manipulated in that particular genes had been selectively ‘knocked out’ to make them unable to metabolize aldehyde or to repair DNA damage; while this was necessary to study the effects in a basic scientific experiment, it is in contrast to what would occur under non-manipulated conditions of alcohol consumption in humans
The damages shown in this experiment were to hematologic cells, and epidemiologic studies have generally not found an increase in the risk of hematologic cancers in humans to be associated with alcohol, especially from the moderate intake of alcohol (and many studies show instead a decrease in risk among drinkers). Thus, studies in humans have not provided support for these reported results from mice. Further, Forum members conclude that the polyphenols that are present in wine may play an important role in blocking a carcinogenic effect associated with alcohol intake.
Reference: Garaycoechea JI, Crossan GP, Langevin F, Mulderrig L, Louzada S, Yang F, Guilbaud G, Park N, Roerink S, Nik-Zainal S, Stratton MR, Patel1 KJ. Alcohol and endogenous aldehydes damage chromosomes and mature stem cells. Nature 2017;553:171-177. doi:10.1038/nature25154.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 210: Beer, wine, and spirits consumption and risk of gastric cancer – 8 January 2018
While heavy alcohol intake has been regularly found to increase the risk of upper aero-digestive tract (UADT) cancers (mouth, tongue, pharynx, larynx, etc.), results are less clear for gastric cancer. The present study is notable because it is based on a large number of subjects, uses appropriate analytic methods, and provides dose-dependent results according to type of beverage.
For total alcohol, the dose-response results in this meta-analysis show a curvilinear relation between alcohol intake and gastric cancer, with a minimal (4%) but significant increase per typical drink (12.5 g/alcohol). However, there were varying responses for different beverages. In beverage-specific analyses, for beer, a non-linear relation was found with a significant increase of 7%/drink (CI 1.01, 1.13); for liquor, there was a linear association, with RR=1.03 (CI 0.98, 109); and for wine, the RR was 0.99 (CI 0.93, 1.06).
While the authors show a figure of the dose-response curves for each beverage using a non-linear approach, they do not provide the specific values in a table or in the text; this makes it difficult to clearly determine threshold effects of beverages. The figures suggest that the risk associated with beer consumption shows a slight decrease for 1 to 2 drinks/day, then an increase; for spirits, no decrease with lighter intake is seen; for wine, the curve is continuously downward. The authors do state that “light, moderate, and wine drinking would not increase gastric cancer risk,” so it is presumed that significant increased risk was not noted for moderate drinking for any specific beverage when non-linear effects were evaluated. Thus, overall, it appears that this large meta-analysis shows no significant increases in risk for light to moderate consumption of an alcoholic beverage, but a slight increase in risk associated with greater intake of beer and spirits. For wine, no increase in the risk of gastric cancer was seen for any level of consumption.
In a number of sensitivity analyses, the authors found tendencies for a lower gastric cancer risk associated with alcohol for cohort versus case-control studies, for studies with larger numbers of subjects, for studies judged to be of higher quality, and for studies adjusting for confounding by SES & income; these types of studies would be expected to yield more precise estimates of effect. These results led the authors to state these sensitivity analyses “ . . . indicate that our results may be exaggerated to some degree, but it should be noted that the pooled risk estimates of high-quality studies yielded similar results to the original analysis.”
Overall, Forum members considered this to be a well-done analysis, and the data support an increase in gastric cancer risk for heavier drinking (of beer or spirits) but no significant effects for light or moderate drinking of any alcoholic beverage. Forum members considered that if the lack of increase in cancer risk from wine consumption seen in this analysis proves to be true, it might relate to the polyphenols in wine that block any adverse effects of alcohol on gastric cancer risk.
Reference: Wang P-L, Xiao F-T, Gong B-C, Liu F-N. Alcohol drinking and gastric cancer risk: a meta-analysis of observational studies. Oncotarget 2017;8:99013-99023.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 209: Does alcohol intake increase the risk of obesity? — 13 December 2017
The public, and scientists, have long been concerned about the relation between alcohol consumption and weight gain, as all alcoholic beverages contain calories. However, most epidemiologic studies do not find that light or moderate drinkers weigh more than their abstaining peers, and some even show lower weight among moderate drinkers than among abstainers. The reasons for this apparent effect are unclear.
The present study is important as it describes the effects on weight of changes in alcohol intake over repeated 4-year periods among a large cohort of health professionals, followed for 24 years. They found very slight increases in weight (mostly less than one-half pound over a four-year period) for subjects consuming alcoholic beverages; these were statistically significant for regular beer and liquor, but not for wine or light-beer. Overall, the largest increases in weight (still, only an increase of 0.6 pounds) were seen for subjects increasing their alcohol by an average of 2 or more drinks/day. For subjects decreasing their alcohol intake over the periods, there was a slight decrease in weight, still only about one-half pound or less.
The investigators conclude that any effects of drinking on weight are very minor, and probably of no clinical significance. While effects on weight gain were slightly lower among consumers of wine and light beer than for those consuming regular beer or spirits, the differences were not large. The study does not present data on the mechanisms of such associations.
Forum members considered this to be a very well-done analysis of repeatedly collected exposure and outcome data among health professionals over an extended period of time. Adjustments were made for known potential confounders associated with changes in weight and appropriate sensitivity analyses were done. While the paper indicates that calories from alcohol are metabolized similarly to those from other foods and do affect weight change, the changes associated with moderate alcohol intake appear to be very minor and would be expected to have very little effect on the development of obesity.
Reference: Downer MK, Bertoia ML, Mukamal KJ, Rimm EB, Stampfer MJ. Change in Alcohol Intake in Relation to Weight Change in a Cohort of US Men with 24 Years of Follow-Up. Obesity 2017;25:1988-1996. doi:10.1002/oby.21979
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 208: A statement on alcohol and cancer that ignores the net health effects of moderate drinking, such as increasing longevity of life — 16 November 2017
The present publication is an attempt by the American Society of Clinical Oncology to describe the relation between alcohol consumption and cancer, including the effects on the risk of developing cancer and effects among subjects currently being treated for cancer. It came to the conclusion that there is a need for the public to be warned about the use of alcohol because of its effects on cancer, and describes numerous approaches for decreasing alcohol use in the population.
Forum members considered this paper to markedly distort the associations between alcohol consumption, especially light drinking, and health outcomes. The authors were particularly remiss in not describing the net health effects of light to moderate consumption: longer longevity of life. Their long discussion of policy implications, and ways of decreasing alcohol use in the population, were unrelated to the data they presented, and failed to describe how complex and culturally specific such recommendations are. The authors describe many ways of decreasing alcohol consumption in the population, but do not provide any data about whether or not the measures they propose are successful.
While all Forum members agree that heavy alcohol consumption increases the risk of several cancers (information that oncologists should be aware of), light drinking has generally been associated only with a slight increase in breast cancer, but not with other types of cancer (especially when under-reporting of intake is considered). Further, factors such as dietary folate intake, patterns of drinking such as binge versus regular moderate drinking, and type of beverage generally consumed have been shown to modify even this relation. Also, regular light or moderate drinking has been consistently shown to decrease the risk of cardiovascular disease (the leading cause of death), diabetes, dementia, and even total mortality, associations largely ignored in this paper.
Our Forum considers that this publication from the American Society of Clinical Oncology misses an opportunity to provide, for oncologists and for the public, up-to-date and balanced information of the true relations of alcohol consumption to the risk of cancer and other health outcomes. They have especially ignored the effects of moderate drinking on the risk of total mortality.
Reference: LoConte NK, Brewster AM, Kaur JS, Merrill JK, Alberg AJ. Alcohol and Cancer: A Statement of the American Society of Clinical Oncology. J Clin Oncol 2017;35:pre-publication. DOI: https://doi.org/10.1200/JCO.2017. 76.1155
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 207: Effects on birth weight and risk of preterm birth of light-to-moderate drinking during pregnancy – 2 November 2017
There is no question that high levels of alcohol consumption during pregnancy can lead to severe adverse effects on the fetus, with the most serious condition known as fetal alcohol syndrome (FAS). Many studies have also related alcohol intake during pregnancy with premature birth, low birth weight, and the infant being small for gestational age (SGA). Data are not as clear on the effects just of occasional or light drinking, but most studies have not detected adverse effects.
The present paper, based on a pooled sample of almost 200,000 women from nine European cohorts, provides data indicating that premature birth, an infant being small for gestational age (SGA), or being of low birth weight do not appear to be associated with light-to-moderate intake (up to 6 drinks/week); these results are similar to those from many other recent studies. In this large study, mothers who consumed greater amounts of alcohol tended to have an increased risk of the infant being SGA or with low birth weight, but such a level of drinking had no effect on the risk of premature delivery. This cohort consisted almost exclusively of light drinkers; no data were available on other potentially harmful effects of excessive drinking.
An interesting additional finding was that the reported frequency of any alcohol consumption during pregnancy in the cohorts studied has decreased dramatically in recent decades (from approximately 50% of women studied prior to 2000, to 39% in 2000-2004, to 14% in 2005-2011). This suggests that most women are responding to guidelines recommending that a woman not drink during pregnancy.
Based on currently available information, the Forum considers that a recommendation to “avoid alcohol during pregnancy” is appropriate as part of drinking guidelines for the public. However, scientific data, including the present paper, do not suggest that women who may have an occasional drink or very light alcohol consumption during pregnancy should have undue concern about having a premature birth or a low-birth-weight infant.
Reference: Strandberg-Larsen K, Poulsen G, Bech BH, Chatzi L, Cordier S, et al. Association of light-to-moderate alcohol drinking in pregnancy with preterm birth and birth weight: elucidating bias by pooling data from nine European cohorts. Eur J Epidemiol 2017 pre-publication; DOI 10.1007/s10654-017-0323-2
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 206: Importance of considering cultural factors in determining effects on health of alcohol consumption – 3 October 2017
It has been clearly shown that presumably similar amounts of alcohol tend to have different health effects (both beneficial and adverse) in different cultures. Greater health benefits from moderate alcohol intake have been shown, for example, in southern European countries (where wine with meals is common) than in more northern European countries, where beer and spirits are more likely to be consumed and usually not with food. Some of these differences may relate to the beverage consumed, while others may relate especially to different patterns of consumption. Further, in certain cultures, intoxication after drinking is expected and even tends to not be condemned. In the typical Italian culture, however, it would not be socially acceptable for a guest at a family dinner to become overtly intoxicated, and such would probably be less often reported in an epidemiologic study even if it had occurred. Thus, similar rates of alcohol-use disorders would be ascertained differently in different countries.
We know that the net effect of alcohol consumption relates to the amount of alcohol, the type of beverage, the rapidity of consumption, whether drinking with or without food, and surely a number of genetic factors of the drinker. What we are often unsure about is what the cultural context of drinking is for an individual subject or subjects in a certain population: different cultures seem to help control, or not control, the risk of drinking excessively. As pointed out by the present paper, these factors complicate the comparison of results of epidemiologic studies from different cultures.
In planning and interpreting results of epidemiologic studies, investigators now realize that simply estimating the average alcohol consumption over a period of time, usually a week, is inadequate to quantify alcohol exposure. The pattern of consumption (especially whether with or without food and whether regularly or in binges) is especially important. And, as the present study points out, knowing about the cultural aspects of drinking for a specific population is also key to interpreting the results. How best to do this, so that studies in different countries can be compared, remains difficult.
Reference: Rehm J, Room R. The cultural aspect: How to measure and interpret epidemiological data on alcohol-use disorders across cultures. Nordic Studies on Alcohol and Drugs 2017;34:330–341. DOI: 10.1177/1455072517704795.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 205: A very large population-based study of the association of alcohol consumption with total and disease-specific mortality – 4 September 2017
The usual finding in longitudinal cohort studies has been that light-to-moderate consumers of alcohol tend to be at lower risk for total mortality and show greater longevity of life, even when other lifestyle/demographic factors known to affect longevity are adjusted for in the analysis. The present analysis is important as it presents data on the relation of alcohol intake to total mortality as well as to specific mortality from cardiovascular disease (CVD) and cancer for a very large number of subjects in the USA. It is based on data from more than 300,000 subjects, of whom almost 25,000 died during a follow-up period averaging 8.2 years. There was a very large number of lifetime abstainers which could serve as an appropriate reference group for their analyses. Further, by adjusting for a number of chronic diseases, and carrying out sensitivity analyses with a 2-year lag period for mortality, the investigators improved their ability to avoid having their results affected by “sick quitters.”
The authors conclude that their analysis shows that light and moderate drinkers have a lower risk of total mortality, as well as mortality from CVD, heart disease, and cerebrovascular disease. The protective effects of alcohol for such cardiovascular outcomes were not present for subjects who reported binge drinking or for those reporting what was defined as “heavy” drinking (>7 drinks/week for women and older men, 14 drinks/week for younger men). Interestingly, the mortality risk for light and moderate drinking was also significantly reduced for deaths attributed to cancer; Forum members thought that this may have possibly resulted from subjects with cancer who actually died from CVD having their deaths attributed to cancer. Subjects reporting heavy drinking and those with binge drinking showed increased risk of all-cause and cancer mortality, with no significant effect on CVD outcomes. The key results of the study are that there is a very clear J-shaped curve for the relation of alcohol to mortality, with lower total, cardiovascular, and even cancer mortality rates for light and moderate drinkers who do not binge drink. There was increased total mortality and cancer mortality for those classified as “heavy” drinkers.
Forum Members thought it unfortunate that beverage-specific data were not presented (as in many studies wine, and sometimes beer, drinkers have better outcomes than consumers of spirits), that subjects of all ages (≥ 18 years of age) were included in a single analysis (rather than also presenting results specifically for older subjects, when the outcome events studied usually occur), and especially that women and older men who consumed > 7 drinks/week, and younger men consuming >14 drinks/week were all combined into a “heavy” drinking category. It would have been preferable that the investigators also had a category for those consuming only slightly more than the recommended levels, who may well have had different outcomes than heavier drinkers.
Overall, Forum members considered this to be a well-done study providing additional data supporting a J-shaped curve for the association of alcohol consumption with mortality. Thus, data continue to indicate that light-to-moderate intake of alcoholic beverages without binge drinking reduces total mortality as well as death from CVD or cancer. The cumulative scientific data on this topic are well described in the accompanying Editorial Comment by de Gaetano and Constanzo in the same issue of the journal.
Reference: Xi B, Veeranki SP, Zhao M, Ma C, Yan Y, Mi J. Relationship of Alcohol Consumption to All-Cause, Cardiovascular, and Cancer-Related Mortality in U.S. Adults. J Am Coll Cardiol 2017;70:913–922
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 204: Moderate drinking improves the chances for healthy survival to age 85 – 21 August 2017
A number of studies have shown that the risk of cognitive impairment appears to be reduced among elderly subjects who consume moderate amounts of alcohol; most studies indicate that both light and moderate drinking are associated with a lower risk of dementia, but heavy drinking is often shown to be associated with higher cognitive risk for dementia and cognitive impairment. In some studies, a protective effect of light-to-moderate alcohol intake has been seen primarily among consumers of wine, or sometimes beer/wine. Further, almost all well-done cohort studies have shown that moderate drinkers tend to have longer lifespans.
The present study is based on a group of ageing subjects in California that had been observed closely for several decades; the average follow-up period for these particular analyses were about 14 years. Subjects in this cohort have had multiple assessments of cognitive ability and frailty. The authors conclude that their subjects who reported moderate alcohol consumption in the late 1980s were more likely than non-drinkers during follow up to survive to age 85 years of age, and also to be more likely to survive to age 85 cognitively intact (without evidence of dementia). Also, daily or near-daily drinkers had better health outcomes than those of non-drinkers or less-frequent drinkers.
The Forum considers this to be a well-done study; while it is not based on a large cohort, it provides new data by having extensive evaluation over time in a cohort of community-dwelling elderly subjects. The results support data from most other studies of survival and dementia among moderate drinkers, but adds specific information on survival to age 85 without cognitive impairment.
This study and the review of prior scientific data on this subject led Forum members to also raise a question about the typical guidelines for alcohol consumption for the elderly: generally less or no alcohol consumption is advised. Given that current scientific data show that the risks of the common disease outcomes of older subjects (e.g., coronary artery disease, ischemic stroke, osteoporosis, dementia, mortality) are lower among moderate drinkers than among non-drinkers, it may be time to reevaluate such restrictions that are based on age alone.
Reference: Richard EL, Kritz-Silverstein D, Laughlin GA, Fung TT, Barrett-Connor E, McEvoy LK. Alcohol Intake and Cognitively Healthy Longevity in Community-Dwelling Adults: The Rancho Bernardo Study. J Alzheimer’s Dis 2017;9:803–814. DOI 10.3233/JAD-161153
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 203: Moderate alcohol intake may reduce, not increase, the risk of falls in the elderly – 7 August 2017
Falls are common among the elderly, and markedly increase the subsequent risk of morbidity and mortality. There has been much written about the dangers of even light-to-moderate intake of alcohol among the elderly, with an increase in potential falls being one key reason cited. This may not be in the best interest of many elderly subjects; the demonstrated protection of light-to-moderate alcohol intake against many of the diseases of ageing (especially coronary heart disease, stroke, osteoporosis, dementia) could outweigh any dangers from falls if the latter risk is not great.
The present study examined the association between certain patterns of alcohol consumption, including the Mediterranean drinking pattern (MDP), and the risk of falls in more than 2,000 elderly subjects over 3.3 years; at the end of follow up, 21.4 % of subjects reported at least one fall in the previous year. The study found that up to moderate amounts of alcohol (defined as less than 40 grams of alcohol/day for men and less than 24 grams/day for women) did not increase the risk of falls, but actually resulted in a significant decrease of 20% or more in such risk. The risks for having multiple falls or those requiring medical care were also lower for moderate drinkers. The investigators report further that subjects with higher scores for a Mediterranean-type diet, that includes regular wine consumption, had similar or more impressive reduction in their risk of falls.
The specific reasons for such protection are not fully known, but a number of favorable effects on health of moderate drinking (e.g., less osteoporosis, less cardiovascular disease, less dementia, greater functional capacity, etc.) may play a role. While the investigators of this study were able to adjust for many factors known to be associated with falls, residual confounding is always a possibility to explain these results.
To summarize, while previous studies have often reported an increase in risk of falls for heavy drinkers, the present study supports results of many previous studies indicating that light-to-moderate alcohol intake does not increase the risk, and often is shown to decrease the risk of falls and fractures. In the present study, even with adjustments for most known lifestyle factors affecting risk, moderate drinking was associated with at least a 20% decrease in the risk of falls when compared with abstainers. This is a message that needs to be incorporated into drinking recommendations for the elderly.
Reference: Ortolá R, García-Esquinas E, Galán I, Guallar-Castillón P, López-García E, Banegas JR, Rodríguez-Artalejo F. Patterns of alcohol consumption and risk of falls in older adults: a prospective cohort study. Osteoporosis International 2017, on-line publication. DOI 10.1007/s00198-017-4157-2.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
==================================================================
Critique 202: Importance of folate intake for reducing breast cancer risk from alcohol consumption, especially for women with a positive family history of breast cancer – 17 July 2017
The strongest factor associated with the risk of a woman developing breast cancer appears to be a positive family history of such a diagnosis in a sibling or mother. Among environmental factors, almost all studies have shown that alcohol consumption relates to increased risk; a slight increase is often seen even among women who report only light drinking, e.g., an average of less than one drink per day. The present study evaluates how a positive family history of breast cancer in a first-degree relative and folate intake may modify the association between alcohol intake and breast cancer; the analysis is based on data from a large number of young women, aged 27-44 years at baseline, over a follow-up period of 20 years.
Forum members considered that this was a very well-done analysis from the large Nurses’ Health Study II, which followed young women for two decades. Alcohol consumption in total drinks/week was based on repeated assessments (but the pattern of drinking, binge versus regular drinking, was not evaluated). Repeated dietary questionnaires were used to estimate folate input. More than 2,800 incident invasive breast cancers were detected, essentially all being validated by a review of medical records.
The main results of this study were that without a positive family history of breast cancer, there was no significant increase in cancer risk for any level of alcohol intake. With a positive family history, however, there was a tendency for higher risk with increasing alcohol intake; this increase was not statistically significant for those with high folate, but a significant positive association (HR=1.82, 95% CI 1.06, 3.12; P-trend = 0.08) with cancer was seen for subjects with the highest level of alcohol intake plus low levels of folate.
Forum members conclude that the results from the present study should greatly relieve anxiety about breast cancer for women without a positive family history of breast cancer who choose to consume light-to-moderate amounts of alcohol. For women with a first-degree relative with breast cancer, the data indicate that if they maintain a high level of folate intake, it may attenuate an increase in risk associated with alcohol intake.
Reference: Kim HJ, Jung S, Eliassen AH, Chen WY, Willett WC, Cho E. Alcohol consumption and breast cancer risk by family history of breast cancer and folate intake in younger women. Am J Epidemiol 2017: pre-publication.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
==================================================================
Critique 201: The marked effect of lifestyle on mortality — 26 June 2017
The aim of the present study was to examine differences in the risk of mortality and in survival associated with a healthy lifestyle versus a less healthy lifestyle. The analyses were based on a total of more than 60,000 Swedish men and women who were followed in one of two studies; at baseline, the subjects were aged 45 to 83 years and were free of cancer and cardiovascular disease. The goal was to evaluate the effects of four “healthy” lifestyle factors: (1) nonsmoking; (2) physical activity at least 150 min/week; (3) alcohol consumption of 0–14 drinks/week; and (4) a healthy diet, with the latter defined as a modified Dietary Approaches to Stop Hypertension (DASH) Diet score above the median. Cox proportional hazards regression models and Laplace regression were used to estimate respectively hazard ratios of all-cause mortality and differences in survival time.
The authors report: “Compared with individuals with no or one healthy lifestyle factor, the multivariable hazard ratios of all-cause mortality for individuals with all four health behaviors were 0.47 (95% confidence interval [CI] 0.44-0.51) in men and 0.39 (95% CI 0.35-0.44) in women. This corresponded to a difference in survival time of 4.1 (95% CI 3.6-4.6) years in men and 4.9 (95% CI 4.3-5.6) years in women.”
Forum members considered this to be a well-done study on a large cohort with complete follow-up data on mortality. Notable weaknesses included the fact that never drinkers and consumers of 0 to 14 drinks/week were considered in one group (thus, including lifetime abstainers, ex-drinkers, and current moderate drinkers); these subjects were compared with consumers of >14 drinks/week. Thus potential differences between abstinence versus light/moderate consumption could not be determined. Further, there were incomplete data on the pattern of drinking, and no data on the type of beverage consumed were reported. Nevertheless, the reduction in mortality for subjects following a healthy lifestyle was impressive: a reduction by half, or more, in the risk of mortality and a 4- to 5-year longer lifespan.
Based on a number of previous studies that evaluated similar lifestyle factors and mortality, the results of this study were not unexpected. Still, they strongly support the remarkable effects on mortality and survival of these lifestyle factors. While not smoking was clearly the factor with the strongest effect on reducing mortality, having a healthy diet, exercising, and consuming light to moderate amounts of alcohol all make additional contributions. This is an important message in that even individuals who may be challenged by genetic or socioeconomic predispositions to earlier demise, adopting certain lifestyle habits can help them reach their greatest potential for a longer and healthier lifespan.
Reference: Larsson SC, Kaluza J, Wolk A. Combined impact of healthy lifestyle factors on lifespan: two prospective cohorts. J Int Med 2017. Pre-publication. Doi: 10.1111.joim.12637.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
Critique 200: Does Light Drinking Increase the Risk of Cancer? — 8 June 2017
The association between the consumption of alcohol and the risk of cancer has been of great interest for many decades. There are a number of types of cancer, especially those of the upper aero-digestive tract (such as mouth, tongue, pharynx, etc.) that are clearly increased among heavy drinkers, especially among subjects who are also heavy smokers. Cancer of the liver can be a result of alcoholic liver cirrhosis, related to long-term heavy drinking. Further, an increased risk for many other cancers have been shown for heavy drinkers, but generally not for light or moderate drinkers.
The risk of breast cancer in women, however, is usually found to be slightly higher in even light drinkers than it is among non-drinkers. This has been a common finding, although some studies suggest that the pattern of drinking, the estimated level of underreporting of alcohol intake, use of hormone replacement therapy, and level of folate intake may all affect this association. For colorectal cancer, some studies suggest an increase in risk even among light-to-moderate drinkers. This has led some to proclaim that no alcohol consumption is preferable for the prevention of cancer. Others suggest that it is important to consider not only cancer, but other diseases; for example, coronary heart disease, ischemic stroke, diabetes, and dementia (all of which are important causes of disability and death) occur less frequently among moderate drinkers than among non-drinkers. Further, the risk of total mortality is almost always found to be lower among light to moderate drinkers than among abstainers.
The present analysis was designed to help determine the association of light or moderate drinking with the risk of cancer. It consisted of a meta-analysis based on a total of 60 studies from 135 articles and included only cohort studies of high quality. The analysis focused on the association between very light (≤0.5 drink/day), light (≤1 drink/day), or moderate drinking (1-2 drinks/day) and the risk of cancer incidence and mortality.
The authors found that very-light drinking was not associated with the incidence of most cancers except for female breast cancer and male colorectal cancer, and was associated with a decreased incidence of both female and male lung cancer and both female and male thyroid cancer. Moderate drinking significantly increased the incidence of male colorectal cancer and female breast cancer, whereas it decreased the incidence of both female and male hematologic malignancy.
Forum members considered this to be a well-done meta-analysis, based on a large number of studies. The main weaknesses of the study related to the lack of ability of the authors to evaluate a number of known confounders: underreporting of alcohol intake, the pattern of drinking or the type of beverage consumed, socio-economic status, and folate intake or other dietary factors. Further, the authors did not describe the effects of alcohol consumption on total mortality.
The results of this study, obviously, support most previous epidemiologic evidence on the association between alcohol consumption and cancer. Larger amounts of alcohol are associated with increased risk of a number of cancers, and even light consumption is associated with the risk of breast cancer, and possibly colorectal cancer. However, given the inability to adjust for many confounders in this study, and lack of data on the net effects in terms of total mortality, it remains difficult for scientists to provide scientifically sound and balanced guidelines regarding the health consequences of alcohol consumption that are applicable to everyone in the population.
Reference: Choi Y-J, Myung S-K, Lee J-H. Light Alcohol Drinking and Risk of Cancer: A Meta-analysis of Cohort Studies. Cancer Research and Treatment 2017; pre-publication release.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=======================================================================
Critique 199: Potential mechanisms for the greater risk and fewer health advantages from alcohol consumption for subjects with low socio-economic status – 25 May 2017
The majority of epidemiologic studies have shown that both the positive and negative health effects of alcohol consumption are modified by the socio-economic status (SES) of individuals, with truly moderate drinkers who are from higher SES strata having better health outcomes and fewer adverse effects from alcohol than lower-SES subjects supposedly consuming similar amounts. One potential explanation for this has been that higher SES subjects (those with higher education, income, job status, etc.) are more likely to be regular moderate drinkers, more likely to be wine drinkers, and to drink primarily with meals, while lower SES subjects are more likely to binge drink (mainly beer or spirits), not with food, and may tend to under-report their alcohol intake. However, there are limited scientific data on the specific mechanisms by which such differences occur.
The authors of the present paper have used data on alcohol intake collected in the Scottish Health Surveys from more than 50,000 subjects to investigate whether the harmful effects of alcohol differ by socioeconomic status when accounting for a number of SES factors. They had very good measures of SES based on education, income, social class (professionals, skilled manual labor, unskilled labor, etc.), and a “measure of deprivation” of the geographic area of the subject (based on multiple measures of deprivation from government administrative data). Their health outcome measures were based on public records for deaths, admissions, and prescriptions; their primary outcome was alcohol-attributable admission or death. Their data show that, even without considering alcohol consumption, lower SES subjects were at much greater risk for poor health outcomes. And, while risks associated with increasing amounts of alcohol were present in all SES groups, they were much greater in the lower groups.
Forum members considered this to be a well-done study, but pointed out that there was limited information on the pattern of drinking and no data on the type of alcoholic beverage consumed or whether or not it was consumed with food. There was no dietary information or genetic information available, and little data on access to health care. While the study showed very marked differences in adverse health outcomes according to SES, the authors found that the factors they considered explained little of the health effects seen. They concluded: “Disadvantaged social groups have greater alcohol-attributable harms compared with individuals from advantaged areas for given levels of alcohol consumption, even after accounting for different drinking patterns, obesity, and smoking status at the individual level.”
Forum members agree that there may be many other lifestyle factors associated with poverty that scientists are unaware of, or unable to adequately control for, in their analyses. Differences by SES in the assessment of alcohol intake remains as a potential factor (especially given that higher SES subjects are usually found to consume alcohol regularly and moderately, less in binges, more often consuming wine with food, etc.). The authors of the present paper have evaluated a number of factors (including smoking status and obesity) as potential explanations for the poorer outcomes among lower SES subjects, and still found large differences in health effects despite adjusting for a number of such lifestyle factors. Thus, the specific reasons why lower SES subjects have worse health overall and poorer effects after alcohol consumption remain unclear.
Reference: Katikireddi SV, Whitley E, Lewsey J, Gray L, Leyland AH. Socioeconomic status as an effect modifier of alcohol consumption and harm: analysis of linked cohort data. Lancet Public Health 2017. Online publication May 10, 2017. http://dx.doi.org/10.1016/S2468-2667(17)30078-6
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================
Critique 198: A study of alcohol and cardiovascular disease based on “Big Data,” linked electronic medical records from the population — 24 April 2017
Essentially all observational cohort epidemiologic studies have shown a “J-shaped” curve for the association of moderate alcohol consumption with coronary heart disease and myocardial infarction, in that non-drinkers and heavy drinkers have higher risk than moderate drinkers. The present study presents a new approach for evaluating this relation by using electronic medical records for a very large number of patients (“big data”) in the UK to judge the relation between alcohol consumption and a variety of cardiovascular disease (CVD) outcomes. The study evaluated clinical data recorded by physicians from almost 2 million subjects, with about 115,000 CVD events recorded in public records. The exposures and outcomes came solely from the medical diagnoses given by individual physicians, and such diagnoses are known to often be inaccurate. For individual subjects, the exposure was based on codes for alcohol use or misuse in their medical records, and the cause of death was based on that recorded by the physician (which is not always consistent with diagnoses from autopsies or medical record reviews). Such problems would be expected to decrease the precision of the exposure and of outcome diagnoses.
Forum reviewers of this paper considered that the authors made a valiant effort in attempting to take into account the limiting factors of using big data for epidemiologic research. It is recognized that studies such as these cannot evaluate the pattern of drinking (regular versus binge) and the investigators were unable to evaluate different effects according to the type of beverage consumed (beer, wine, or spirits). It would be expected that both of these factors may have affected their results. Nevertheless, their conclusions strongly support the extensive observational data from cohort studies over many decades that have shown a higher risk among abstainers (versus moderate drinkers) for many CVD outcomes. In the present study, non-drinkers had significantly higher risk for unstable angina, myocardial infarction (MI), unheralded coronary death, heart failure, ischemic stroke, peripheral arterial disease, and abdominal aortic aneurysm. For most of these outcomes, heavy drinkers tended to have an increased risk (a J-shaped curve), but the risk for myocardial infarction and for stable angina remained decreased even for the heavy drinking category. For other manifestations of CVD, especially those related to cerebral artery disease (other than ischemic stroke), there was less of a clear pattern relating alcohol to disease. For their aggregate, overall outcome based on all manifestations of CVD, their analyses add further support for a J-shaped curve between alcohol intake and CVD.
Reference: Bell S, Daskalopoulou M, Rapsomaniki E, George J, Britton A, Bobak M, Casas JP, Dale CE, Denaxas S, Shah AD, Hemingway H. Association between clinically recorded alcohol consumption and initial presentation of 12 cardiovascular diseases: population based cohort study using linked health records. BMJ 2017;356:j909. http://dx.doi.org/10.1136/bmj.j909
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================
Critique 197: Alcohol consumption and the risk of developing dementia – 13 April 2017
A number of epidemiologic studies have found that light-to-moderate alcohol intake is associated with a lower risk of developing dementia and/or cognitive decline, while excessive drinking may increase the risk. The authors of the present paper carried out a meta-analysis of the current scientific literature that was based on data from 11 studies with 4,586 cases of all-cause dementia diagnosed among more than 70,000 subjects and two additional analyses of studies of approximately 50,000 subjects each for evaluating the association of alcohol intake with the diagnosis of Alzheimer’s disease or vascular dementia. Seven studies provided results according to type of alcoholic beverage consumed, while two provided results according to APOE 4 levels.
The conclusions of the authors are that, considering all sources of alcohol, light-to-moderate alcohol consumption was associated with a lower risk of all forms of dementia; the risk was reduced for up to 12.5 g/day (about one typical drink) and increased for consumers of more than 38 g/day (about 3 to 4 typical drinks). However, beverage-specific analyses indicated that the effect was only for wine, and not for consumption of beer or spirits. For moderate consumers of wine, the risk of dementia was reduced by 40% or more in comparison with that of non-drinkers. Little effect was noted among drinkers of spirits, and heavy beer drinkers appeared to have an increased risk of dementia. The presence or absence of APOE 4 did not appear to modify the effects.
Forum reviewers considered this to be a very well-done meta-analysis of the current literature on the topic. It was based only on prospective epidemiologic studies of very good quality, and sub-analyses evaluated the separate effects of each type of alcoholic beverage. While the authors were unable to include the pattern of drinking (binge versus regular moderate) in their analyses, and could not test for previous alcohol consumption among current non-drinkers, Forum members agreed with the primary findings of a J-shaped curve between alcohol consumption and all types of dementia (including vascular dementia and Alzheimer’s disease).
Most of this Forum critique deals with potential mechanisms by which wine consumption may reduce the risk of dementia and/or cognitive decline. In addition to the effects of both alcohol and polyphenols in wine on decreasing atherosclerosis and having beneficial effects on hematological factors (affecting cerebral as well as coronary arteries), there may also be anti-inflammatory effects and direct effects on brain structures that play a role. Given that the beneficial effects were primarily among wine consumers, this suggests that the polyphenols and other non-alcohol substances in wine (perhaps in interaction with alcohol) may be more important than the alcohol itself in reducing the risk of dementia.
The mechanistic studies described in the paper and in this critique provide considerable support for the epidemiologic findings of less dementia and cognitive decline among moderate drinkers. Forum member agree with the authors of this paper that light-to-moderate wine consumption may help lower the risk of dementia, an increasingly important condition in the world’s rapidly ageing populations.
Reference: Xu W, Wang H, Wan Y, Tan C, Li J, Tan L, Yu JT. Alcohol consumption and dementia risk: a dose-response meta-analysis of prospective studies. Eur J Epidemiol 2017;32:31-42. doi: 10.1007/s10654-017-0225-3. Epub 2017.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================
Critique 196: Adverse health effects of binge drinking on cardiovascular disease — 2 February 2017
This review paper on the effects of binge drinking on the risk of cardiovascular disease (CVD) provides considerable information on a topic of importance to public health. It clearly indicates that subjects who binge drink, however defined, tend to be at increased risk for hypertension, myocardial infarction, stroke, and cardiac arrhythmias. These adverse health outcomes are in addition to the well-known effects of binge drinking on drunkenness and many adverse health effects, both acute and chronic, as well as risk from violence and accidents to the drinker and to others.
While the members of the Forum applaud the efforts of the authors to present data on this relation, this paper failed to include many important previous research reports on the topic. Forum member Ian Puddey and others have prepared an extensive summary of many of the key research papers not addressed by the authors of this paper; their remarks are included in the full Forum critique. It describes how many factors, such as not only the amount but the rate at which alcohol is consumed, the type of beverage, whether or not food is being consumed, the prior drinking habits of the subjects, and many other factors can influence the effects of alcoholic beverages on health.
The Forum members conclude that a “comprehensive review” of binge drinking and other drinking patterns of alcohol in relation to the risk of CVD should include all of the available scientific data on the topic to be most useful. Taking into consideration the additional research results described in this critique provides a much better overview of the effects of binge drinking on CVD. The bottom line is that episodic heavy drinking, or binge drinking, has adverse influences on many health outcomes, including the risk of CVD.
Reference: Piano MR, Mazzuco A, Kang M, Phillips SA. Cardiovascular Consequences of Binge Drinking: An Integrative Review with Implications for Advocacy, Policy, and Research. Alcoholism: Clinical and Experimental Research 2017; Pre-publication. doi: 10.1111/acer.13329
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=========================================================================
Critique 195: How much of the “health benefits” of alcohol relate to higher socio-economic status of drinkers? — 19 December 2016
It has long been recognized from epidemiologic studies that both the positive and negative health effects of alcohol consumption are modified by the socio-economic status (SES) of individuals. Higher SES subjects (higher education, income, job status, etc.) are more likely to be regular moderate drinkers, while lower SES subjects are more likely to binge drink and under-report their alcohol intake. Truly moderate drinkers tend to have better health outcomes and fewer adverse effects from alcohol, and consistently show lower total mortality risks than non-drinkers or heavy drinkers.
The present study, from the New Zealand Longitudinal Study of Ageing, used data from the second examination of the cohort to do a cross-sectional analysis judging the relation of alcohol consumption to “health”. When controlling for age, income, and education (the latter two as measures of SES), they found a significant “J-shaped” association between reported alcohol intake and self-reported “physical health”. However, the authors state that they then used another measure of SES, the Living Standard Index-Short Forum (ELSI-SF), and found that the reported alcohol intake of subjects correlated with their measure of physical health almost exactly the same as with the results of the ELSI-SF. They conclude that there are no health benefits of moderate drinking, only that people with higher SES are more likely to drink moderately.
Forum members considered it unfortunate that the assessment of the exposure (alcohol intake) used in this study was based only on self-reported average intake and did not include data on the pattern of drinking (binge versus regular moderate intake, etc.). Further, their outcome was based only on a self-reported questionnaire of “physical health,” and did include any hard data; an overall index based on assessments of functional status, biomarkers of and the occurrence of disease, and mortality would be preferable when judging “health benefits” of alcohol. The Forum considered that the authors used inadequate indices of both the exposure to alcohol and their assessment of “health” (based on a questionnaire) to reach a conclusion that moderate drinking does not have any beneficial effects on health. This was done ignoring the massive amount of not only observational data but results from extensive experimental studies over more than four decades. Such research has found that moderate drinking not only has beneficial effects on assessments of physical health and disease occurrence, but results in significantly lower total mortality when moderate drinkers are compared with abstainers.
Regardless, given that this study, as have almost all epidemiologic studies, has shown the importance of SES on health outcomes, a key challenge to scientists is to seek to determine the mechanisms by which these differences occur. One potentially important factor is that the differing health outcomes relate to errors in judging the exposure, i.e., inadequate assessments of alcohol: not evaluating for binge drinking versus regular intake, consuming alcohol with or without food, type of beverage consumed, under-reporting of intake, etc. Also, much broader definitions of “health” are needed (rather than the results of a single self-administered questionnaire) that include the effects on functional status, disease states, and mortality. And, it is important that other lifestyle factors (smoking, drug use, etc.) that affect health be properly evaluated as determinants of health. Only with such data will we be able to fully judge the overall effects of alcohol consumption on health outcomes.
Reference: Towers A, Philipp M, Dulin P, Allen J. The “Health Benefits” of Moderate Drinking in Older Adults may be Better Explained by Socioeconomic Status. Pre-publication: J Gerontol B Psychol Sci Soc Sci 2016. doi:10.1093/geronb/gbw152
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 194: Long-term alcohol use and mortality among Swedish women – 22 November 2016
In a follow-up analysis of almost 50,000 young women, aged 30-49 at baseline, in the Swedish Women’s Lifestyle and Health cohort, the authors used self-reported information on alcohol consumption on two occasions, 12 years apart, to estimate the effects of alcohol on overall and cause-specific mortality. There were 2,100 deaths during follow up. Effects of alcohol on the two occasions, and changes between the two assessments among 33,000 women with available data, were related to mortality, as assessed from virtually complete national records.
Using “light” drinkers (0.1 – 1.49 grams of alcohol/day) as the referent group, the authors report an inverse association between greater amounts of alcohol consumption and mortality from cardiovascular disease. They report increased risk of cardiovascular and total mortality for abstainers. Despite the large number of total subjects, the authors report results separately for relatively narrow ranges of alcohol intake (none, 0.1-1.49, 1.5-4.9, 5-9.9, 10-14.9, 15+ g/day), which makes the numbers of subjects in many groups quite small. Given that the total mortality risks for most groups of drinkers were similar, it would have been interesting to see the effects of alcohol consumption (versus no consumption) using a broader definition of “moderate” drinking.
Forum members in general thought that this was a well-done study, using an excellent source of national records available in Sweden for determining mortality. They had concerns that the under-reporting of alcohol intake was not addressed; there is a high probability that some of the supposedly “light” drinkers may have actually consumed more alcohol, which would tend to decrease any differences between the referent group and the next groups of drinkers. This could help explain why, despite the strikingly lower risk ratios for cardiovascular disease for all drinkers when compared with the referent group, the inverse relation of alcohol was not statistically significant for any single group considered alone.
The Forum was also concerned that while the investigators had data on binge drinking and whether or not alcohol was usually consumed with meals, they chose not to include these data in their analyses. Given that drinking pattern plays a large role in determining favorable or unfavorable health effects of alcohol, the inclusion of such information may have better delineated the true effects of alcohol. Also, the authors “chose not to separately study the effects of different alcohol beverages;” reporting effects separately for beer, wine, and spirits could have provided key data on the effects of alcohol consumption.
The attempt of the authors to judge the effects of changes in alcohol intake during the study is laudable. Importantly, data on the reason that a woman may decide to increase or decrease her intake is not known; if due to the development of a serious disease, it may be the disease and not the change in alcohol intake that relates to subsequent mortality. However, given the inherent problems in assessing change, the results of this study are consistent with other studies that have suggested an increase in mortality risk for moderate drinkers who stop their alcohol consumption.
Reference: Licaj I, Sandin S, Skeie G, Adami H-O, Roswall N, Weiderpass E. Alcohol consumption over time and mortality in the Swedish Women’s Lifestyle and Health cohort. BMJ Open 2016;6:e012862. doi:10.1136/ bmjopen-2016-012862
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 193: The association of reported alcohol intake with the risk of subarachnoid hemorrhage: A meta-analysis – 1 November 2016
Data from epidemiologic studies are quite consistent for the relation of alcohol consumption with the different types of stroke: for ischemic stroke, an inverse association with moderate drinking and a possible increase with heavy drinking (a “j-shaped curve”); for hemorrhagic stroke, a direct positive association, although some studies suggest that there may be a threshold level for an increase in risk. Data are mixed on a possible association between the most uncommon type of stroke, subarachnoid hemorrhage (SAH). The present paper presents results of a meta-analysis relating reported intake of alcohol with subsequent risk of SAH. It was based on 14 observational studies reporting data on 483,553 individuals and 2,556 patients.
Forum members agree that this study suggests that alcohol intake, especially heavier drinking, increases the risk of SAH, although there was considerable heterogeneity among studies from different parts of the world, there were no countries from the Mediterranean area included, and there was no accounting for pattern of drinking (binge versus moderate regular) or type of beverage, all of which may affect risk.
The authors concluded that there was no relation between light (<15 g/day) or moderate alcohol consumption (15‑30 g/day) compared with abstaining individuals; this was based on statistically insignificant increases in RR of 1.27 (95% CI: 0.95, 1.68) and 1.33 (95% CI: 0.84, 2.09) for these two groups, respectively. However, Forum members suggest that there could be a slight increase in risk even for these two groups. For heavier drinkers (> 30 g/day, about 2 ½ to 3 typical drinks per day), the data indicate an increase in risk: RR=1.78 (95% CI: 1.46, 2.17).
It should be noted that the overall risk of total stroke is decreased from moderate drinking, as the most common type of stroke is ischemic, and moderate drinking has consistently been shown to lower such risk; this is especially related to lowering the risk of atherosclerotic or embolic clots. However, while rare, SAH is often a devastating disease, and the risk may be increased from alcohol consumption through its effects on decreasing coagulation.
Reference: Yao X, Zhang K, Bian J, Chen G. Alcohol consumption and risk of subarachnoid hemorrhage: A meta-analysis of 14 observational studies. Biomedical Reports 2016;5:428-436.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=========================================================================
Critique 192: The association of alcohol consumption with the risk of prostate cancer –- 12 September 2016
Scientific data are mixed on the association of alcohol consumption with the risk of prostate cancer. In the present paper, the authors have used data from 11, 372 subjects in the Older Finnish Twin Cohort who provided data on alcohol intake on two occasions. They were followed for the development of prostate cancer from 1981 to 2012, during which 601 incident cases of prostate cancer and 110 deaths from prostate cancer occurred. The authors relate reported average alcohol intake, and whether or not the subject reported binge drinking, to the risk of prostate cancer and prostate cancer-specific death. They also evaluated the risks of prostate cancer among alcohol-discordant twins. The authors used current abstainers and ex-drinkers as the referent group in their main analyses, but did sensitivity analyses using never drinkers as an alternative referent group.
The type of beverage consumed was not known, so whether or not wine or beer consumption may have a different relation with prostate cancer than spirits intake cannot be determined. However, overall the data indicated a higher risk of prostate cancer from heavy intake and binge drinking, but also a high risk among abstainers. The number of discordant twins (for alcohol consumption) was too small for definitive results in terms of the risk of prostate cancer among subjects with the same or a similar genetic background , but the lowest risk was among light drinkers who did not binge drink. Even among this subset of the population, abstainers had higher risk than light drinkers.
Thus, the results of this well-done study suggest that there may be a J-shaped relation between alcohol consumption and prostate cancer risk. Light drinkers appear to have the most favorable results for both incident prostate cancer and prostate cancer-specific mortality. The risk for subjects reporting heavy drinking and binge drinking was higher for both incidence and mortality than the risk of light drinkers; for unexplained reasons, abstainers also tended to have higher risk of prostate cancer and mortality.
Reference: Dickerman BA, Markt SC, Koskenvuo M, Pukkala E, Muccil LA, Kaprio J. Alcohol intake, drinking patterns, and prostate cancer risk and mortality: a 30-year prospective cohort study of Finnish twins. Cancer Causes Control 2016;27:1049–1058. DOI 10.1007/s10552-016-0778-6
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 191: A new study on the mechanisms of alcohol’s effects on health and disease – 25 August 2016
While observational epidemiologic studies for many decades have consistently shown that moderate drinkers have a lower risk of cardiovascular diseases than do non-drinkers or heavy drinkers, the specific metabolic effects of alcohol have been little studied. In the present analysis, among almost 10,000 young adults from three population-based cohorts in Finland, associations of alcohol intake with 86 metabolic measures were assessed. Circulating lipids, fatty acids and metabolites were quantified by high-throughput nuclear magnetic resonance metabolomics and biochemical assays. The investigators found that alcohol consumption was associated with a complex metabolic signature, including aberrations in multiple biomarkers for reduced as well as elevated cardiometabolic risk; many factors showed different associations according to the estimated amount of alcohol consumed.
Among key associations found for greater alcohol intake were increases in HDL-cholesterol and its subclasses, decreases in LDL size, an increase in monounsaturated fatty acids and a decrease in omega-6 fatty acids, and lower concentrations of glutamine and citrate. For unexplained reasons, the changes in fatty acids from alcohol in this study were similar to those occurring following the administration of canola oil in other research. Some Forum reviewers pointed out that the analyses were not theory driven, and should only be used to generate hypotheses that would need to be tested in future experiments. As stated by one reviewer, the major contribution from this paper could be that it ignites the interest for experimental studies and provides new variables to be evaluated in prospective studies. In any case, the findings of this study provide valuable clues to the biologic effects on health, both favorable and adverse, related to alcohol consumption.
While not discussed by the authors, Forum members considered that the results of this paper might also be useful in providing a new approach for judging the level of alcohol intake of individuals in epidemiologic studies. At present, alcohol intake is judged almost exclusively from self-reports by subjects. Previous attempts designed to identify subjects more likely to be under-reporting their intake have shown that they may sharpen relations between estimated intake and health outcomes. Forum members believe that approaches that identify sources of bias for self-reported data, whether based on genetic, behavioral, physiological, or other information (preferably on all), might allow epidemiologists to have more precise and accurate information on alcohol intake when relating such to disease outcomes. A new approach for providing more accurate and unbiased estimates of alcohol intake is suggested by this excellent analysis.
Reference: Würtz P, Cook S, Wang Q, Tiainen M, Tynkkynen T, Kangas AJ, et al. Metabolic profiling of alcohol consumption in 9778 young adults. Int J Epidemiol 2016; pre-publication: doi: 0.1093/ije/dyw175
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 190: Alcohol intake during middle age and later atherosclerosis – 11 August 2016
Carotid artery disease can be estimated by ultrasound from the thickness of the wall of the arteries (recorded as carotid artery intima/medial thickness, cIMT) and by evidence of atherosclerotic plaques within the carotid arteries. The association between alcohol intake and such lesions is unclear, as some studies show a positive association with cIMT and/or plaques while others show no association. Given that carotid disease relates to the subsequent risk of coronary artery disease, there is increasing use of carotid ultrasound measurements to help determine long-term risk.
The present large study from the UK provides valuable information by reporting the cross-sectional relation between alcohol consumption and cIMT as well as how the drinking pattern over 20 years in middle age may relate to cIMT later in life. While heavy alcohol intake was found to increase later cIMT measures, no clear differences were noted between subjects reporting abstinence and those reporting moderate drinking in middle age.
Forum reviewers considered this to be a well-done study. There were some concerns that only total average alcohol intake was considered, as there were no data on the type of beverage consumed, the pattern of drinking (binge versus regular moderate), whether the alcohol was consumed with food, etc., and there was an absence of data on diet, physical activity, adiposity, and other factors related to atherosclerosis. Further, only the thickness of the carotid artery was evaluated, and not the presence or absence of atherosclerotic plaques on the ultrasound readings.
Overall, current scientific data provide strong evidence that moderate alcohol consumption lowers the risk of most manifestations of cardiovascular disease; it appears to work through a combination of effects on lipids, inflammation, coagulation, fibrinolysis, glucose metabolism, and other paths. Further, heavy drinking is known to increase blood pressure, and is an important factor for developing hypertension (and a strong determinant of cIMT). The failure of the present study to find a significant association between moderate alcohol intake and later carotid thickness supports what has been shown in some, but not all, previous studies.
If indeed chronic alcohol use has little effect on atherosclerosis (using images from the carotids as an index of atherosclerosis in the coronary arteries and elsewhere in the body), it may indicate that the mechanisms for the protective effect of moderate alcohol consumption on cardiovascular disease are not so much related to preventing atherogenesis, but due primarily to the effects on coagulopathy. And it is known that clot formation within the arterial wall is often the precipitating event for an acute myocardial infarction or other cardiovascular event.
Reference: Britton A, Hardy R, Kuhf D, Deanfield J, Charakida M, Bell S. Twenty-year trajectories of alcohol consumption during midlife and atherosclerotic thickening in early old age: findings from two British population cohort studies. BMC Medicine 2016l;14:111. DOI 10.1186/s12916-016-0656-9.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 189: Importance of drinking pattern on the effects of wine on health — 26 July 2016
A review article appearing in Food & Function, a publication of the Royal Society of Chemistry in the United Kingdom, presents a summary of evidence-based scientific data relating the moderate consumption of wine and other alcoholic beverages to health. Forum members considered the paper to be a well-thought-out appraisal of the effects that the pattern of consumption (e.g., the type of beverage, regular versus binge drinking, consumption with meals, etc.) affects its risks and benefits. (It is recognized that some of the authors of this publication work primarily with wine, but the review article covers key behaviors that affect the relation of the consumption of all types of alcohol to health.)
The authors describe how the polyphenols and other non-alcoholic components of wine provide anti-oxidants and decrease post-prandial oxidative stress. These phenols can also scavenge free radicals in the mouth and throughout the gastro-intestinal tract, preventing lipid peroxidation as well as the absorption of cytotoxic lipid peroxidation products. Wine also favorably affects urate levels; thus, the antioxidant activity is apparently influenced by two separate mechanisms: wine-derived phenolic compounds and plasma urate. A further important biological property of wine is its potent antimicrobial activity that tends to decrease adverse effects of food-borne and oral pathogens.
The article summarizes the key differences in health effects when alcohol (especially wine) is consumed moderately, with food, and on a regular basis rather than in binges. These differences emphasize why evaluating only the total amount of alcohol consumed, and not how it is consumed, is inadequate when evaluating its effects on health and disease. Further, the authors emphasize how all medical and scientific information concerning the effects of wine and alcohol consumption on human health should be evidence-based and communicated in a competent, credible and unbiased manner.
Reference: Boban M, Stockley C, Teissedre P-L, Restani P, Fradera U, Stein-Hammer C, Ruf J-C. Drinking pattern of wine and effects on human health: why should we drink moderately and with meals? Food Funct 2016;7:2937–2942. DOI:10.1039/c6fo00218h
Note on potential conflict of interest: While several of the authors of this paper are members of our Forum, they have had no input into the review of the article.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 188: Alcohol-attributable cancer in New Zealand . . . 28 June 2016
Previous scientific research has shown that heavy alcohol consumption is a major risk factor for upper aero-digestive cancers, and even light drinking increases slightly the risk of breast cancer in women. The present study is based on a very small number of cases of cancer in New Zealand, tabulated separately for Māori and non-Māori subjects, and applies estimates of alcohol effects from other population-based studies. Besides having so few cases, the investigators had no individual data (on the pattern of alcohol consumption, type of beverage, smoking or other lifestyle habits, socio-economic status, etc.) on subjects who did, or did not, develop these cancers. It is not even known whether or not the specific subjects who developed these cancers consumed alcohol.
It has repeatedly been emphasized that disease-specific death rates must be interpreted in light of the effects of the exposure (in this case, alcohol consumption) on other causes of death as well, especially on total mortality risk. The large majority of studies have shown that moderate drinking clearly reduces the risk of most cardiovascular diseases, diabetes, and other of the diseases of ageing, as well as the risk of total mortality. However, the estimated effects of alcohol on total mortality are not included in this paper.
The very long Discussion in this paper is primarily a treatise on how the public must be told of the dangers of cancer from any alcohol consumption; it focuses on health policy recommendations and very little on the limitations of the data and the study. The authors end up making very broad recommendations based on very small numbers of subjects. Limitations to this study suggest that it adds little to our current understanding of the relation of alcohol consumption to the risk of cancer and other diseases.
Reference: Connor J, Kydd R, Maclennan B, Shield K, Rehm J. Alcohol-attributable cancer deaths under 80 years of age in New Zealand. Drug and Alcohol Review 2016; pre-publication. DOI: 10.1111/dar.12443
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 187: Alcohol and squamous cell carcinoma of the skin — 14 June 2016
Skin cancers, whether melanoma, basal cell, or squamous cell, are all increased by ultra-violet rays of the sun, and such cancers are much more common in areas of the world with more sun exposure. Further, the risk of such cancers is higher among individuals reporting excessive tanning (either from the sun or from tanning salons). The present study was undertaken to judge the relation between alcohol consumption and the risk of cutaneous squamous cell carcinoma (cSCC), an association that is unclear from earlier research. Determining the relation between alcohol and skin cancer is made difficult by the fact that excessive sun exposure has been shown to be greater among consumers of alcohol than among abstainers, thus the potential for confounding.
In the present analyses, combined data from three cohorts of subjects in the US, who had repeated assessments of alcohol intake over many years, were evaluated tor the relation of alcohol to the development of verified cSCC. Subjects included women in two cohorts of the Nurses’ Health Study and men in the Health Professionals’ Follow-up Study. Among subjects providing a total of more than 4 million person-years of follow up, 2,938 cases of cSCC were identified.
The results varied somewhat among the different cohorts, but in the meta-analysis of the three studies using continuous measures of alcohol, there was an increase in risk of cSCC with alcohol intake. Among women, there was a steep increase in risk of cancer for low levels of intake (up to 5 grams of alcohol/day, slightly less than ½ of a typical drink), then a gradual increase in risk thereafter, whereas among men there was more of a gradual increase in risk with larger reported alcohol intake.
Overall, the authors report an increase in risk per typical drink per day of 22% for invasive cSCC and 14% for in situ cSCC. In beverage-specific analyses, white wine consumption of >/= 5 times/week was associated with an increased risk of cSCC (RR 1.31, 95% confidence interval: 1.09-1.59), but an increased risk of cSCC was not seen for other alcoholic beverages. The population-attributable risk associated with alcohol intake of ≥ 20 grams/day (about 1 ½ typical drinks) was 3% of cSCCs.
Forum members considered that the analyses were well done, and the results of the study are consistent with increases in risk associated with alcohol consumption for other types of skin cancer. Given that sun exposure is by far the primary risk factor for skin cancer, and consumers of alcohol tend to have greater number of sunburns (also shown in this study), it is always difficult to determine if residual confounding by sun exposure is playing a role. The authors of this paper attempted to adjust for sun exposure by including in their analyses the typical exposure values in the area of the world where the subjects resided, by recording the frequency that subjects reported 5 or more severe sunburns, and several other measures. As expected, there were reductions in the estimated RR for invasive cSCC when going from age-adjusted RR (1.34) to multivariable-adjusted estimates (1.22) of risk. However, the magnitude of decrease in risk estimates when only those adjustments for sun-exposure were added to the equation cannot be determined from the data presented.
Forum reviewers consider that these analyses support results from many previous studies and indicate that consumers of alcohol have a greater risk than non-drinkers of all types of skin cancer. Attempts to judge how much of this association may be due to residual confounding related to sun exposure are less than conclusive. Various hypotheses have been raised for possible interactions between sun exposure and alcohol, but currently there are no experimental data to test these theories. While the authors conclude that “physicians may consider counseling their patients about the association between alcohol consumption and risk for cSCC,” it might be more advantageous for physicians to focus more on the much greater protection against this disease that would occur if they were able to limit their patient’s exposure to ultra-violet radiation.
Reference: Siiskonen S, Han J, Li T, Cho E, Nijsten T, Qureshi A, Alcohol intake is associated with increased risk of squamous cell carcinoma of the skin: three US prospective cohort studies. Nutrition and Cancer 2016;68:545-553.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 186: Changes in alcohol and effects on risk of breast cancer and heart disease — 19 May 2016
This large study from Denmark was designed to test the hypothesis that women who increase their alcohol intake over a five year period have a higher risk of breast cancer and a lower risk of coronary heart disease (CHD) compared with women who exhibit a stable alcohol intake. It consisted of more than 20.000 postmenopausal women who had two assessments of alcohol intake, about 5 years apart; changes during that period were related to their subsequent risk of developing breast cancer or CHD, or dying, during the subsequent follow-up period that averaged 8 years.
For the risk of breast cancer, the baseline alcohol consumption reported by the women showed that higher alcohol intake was associated with a greater risk of developing breast cancer during follow up, but a lower risk of developing CHD and for total mortality. For relating changes in alcohol intake in the 5 years between the two alcohol assessments, those who increased their reported alcohol intake showed an increased risk of subsequent breast cancer, while those who decreased their intake also had a tendency for greater breast cancer. In terms of CHD and total mortality, the data were consistent with an increase in consumption lowering risk, while there was a tendency for a decrease in consumption to increase risk. Hence, the directionality for risk from changes in intake reflected the risks associated with baseline risk, and the authors conclude that their results “ . . .support the hypotheses that alcohol intake is associated with increased risk of breast cancer and decreased risk of coronary heart disease.”
Forum reviewers considered this to be a very well-done study. They, and the authors, appreciated the innate difficulty in separating effects on health of usual alcohol intake over time and changes over a limited period of time. Reviewers were also concerned by these problems, suggesting that some of the reported changes in alcohol consumption in this study may have just reflected individuals replying differently to questions regarding their drinking at different points of time. Further, the reason why some women may have actually increased or decreased their intake are not known.
Nevertheless, Forum members applaud the attempt of the authors to judge if changes in alcohol intake relate to cancer, CHD, and total mortality. This is a difficult task given that baseline and life-time alcohol consumption clearly relate to these outcomes. Further, data on the pattern of drinking (regular versus binge), any estimate of underreporting of alcohol, the type of beverage consumed and, as stated by the authors, certain known risk factors of breast cancer, were not available to be included in their analyses. Thus while the results of this study add important information on the relation of alcohol to disease, there remain questions about the specific relevance of changes in intake for such outcomes.
Reference: Dam MK, Hvidtfeldt UA, Tjønneland A, Overvad K, Grønbæk M, Tolstrup JS. Five year change in alcohol intake and risk of breast cancer and coronary heart disease among postmenopausal women: prospective cohort study. BMJ 2016;353:i2314. http://dx.doi.org/10.1136/bmj.i2314
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 185: An innovative assessment of alcohol consumption and the risk of atrial fibrillation – 28 April 2016
A study from Denmark has been carried out to test the hypothesis that alcohol consumption, both observational (self-reported) and estimated by genetic instruments, is associated with the risk of atrial fibrillation (AF) and to determine whether people with high cardiovascular risk are more sensitive towards alcohol than people with low risk. It was based on a large cohort of subjects (more than 88,000) with a mean follow-up period of 6.1 years; there were almost 3,500 cases of AF diagnosed from hospital records during follow up. Unfortunately, the authors did not have data to identify binge drinkers, which tend to show greater adverse cardiovascular events than regular moderate drinkers whose weekly intake may be the same.
The main results of the study were that men consuming more than 14 drinks/week, especially those consuming more than 28 drinks/week, had an increase in risk of AF, but no significant increase in risk was seen for any level of alcohol intake among women. When genotypes affecting alcohol metabolism (AHD1B, ADH1C) were studied in a Mendelian randomization analysis, the authors state that they “found no evidence to support causality of the observational findings.”
Forum reviewers of this article considered it to be a well-done study with appropriate analyses. Its results reflect the findings of most previous prospective studies and meta-analyses of little effect of light drinking on AF, but an increase in risk for heavier drinkers. The study also showed that the effects of alcohol consumption on the risk of AF were not different between subjects who had cardiovascular disease or were at high-risk of cardiovascular disease than for other subjects.
While Mendelian randomization using genetic factors affecting alcohol metabolism has been touted as an unbiased approach for judging causal health effects of alcohol, there are questions about the adequacy of such instruments for judging effects. In the present study, their use did not suggest that the relations shown by the self-report of alcohol by subjects necessarily indicated a causal association of alcohol with AF.
Overall, current data suggest that heavy drinking may increase the risk of AF, but there is little evidence of a meaningful increase in risk from light drinking. Luckily, such levels of alcohol intake (some guidelines suggest no more than 2 drinks/day for men or 1 drink/day for women) have been shown from many previous studies to significantly lower the risk of cardiovascular disease and total mortality.
Reference: Tolstrup JS, Wium-Andersen MK, Ørsted DD, Nordestgaard BG. Alcohol consumption and risk of atrial fibrillation: Observational and genetic estimates of association. European Journal of Preventive Cardiology 2016; pre-publication. DOI: 10.1177/2047487316641804
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 184: A major new meta-analysis on alcohol consumption and the risk of pancreatic cancer — 4 April 2016
The present meta-analysis was based on data from more than four million subjects in prospective cohort studies, among whom 11,846 incident cases of pancreatic cancer were diagnosed. With the lowest intake group (non-drinkers or occasional drinkers) as the referent group, the authors defined “light” consumption as up to 12 grams/day (essentially one typical drink); 12-24 g/day as “moderate”; and ≥24 g/day as “heavy” drinking. The key results of the study were that, overall, neither light drinkers (RR = 0.97) nor moderate drinkers (RR = 0.98) showed an increase in risk of pancreatic cancer, while subjects classified as heavy drinkers had a slight increase (RR= 1.15, 95% CI 1.06 – 1.25). The increase in risk was due to heavy drinkers of liquor, as there was no significant increase in risk even for heavy drinkers of beer (RR = 1.08, CI 0.90 – 1.30) or wine (RR = 1.09, CI 0.79 -1.49).
Forum members considered this to be an excellent paper on the association between alcohol consumption and pancreatic cancer. The authors used appropriate methods and limited subjects to those in prospective cohort studies, which would tend to limit bias. The paper shows that the significant increase in risk occurred only among men, with no significant effect of alcohol being found among women. Among the weaknesses of the study were that there was a mixture of lifetime abstainers and ex-drinkers included in the referent group, and the same cut-points for category of alcohol intake was used for both men and women, whereas drinking guidelines are generally lower for women than for men. Further, data on the pattern of drinking (regular versus binge) were not available.
To summarize, this study showed no significant association with cancer risk for any level of consumption of beer or wine, which could relate to their lower concentration of alcohol per volume of the beverage, to non-alcoholic substances (such as polyphenols, present in wine and beer), or even to different drinking practices among subjects consuming different beverages. Thus, Forum members agree with the conclusions of the authors that heavy alcohol consumption, especially of liquor, increases the risk of pancreatic cancer, but the intake of beer or wine may not be associated with an increased risk.
Reference: Wang Y-T, Gou Y-W, Jin WW, Xiao M, Fang H-Y. Association between alcohol intake and the risk of pancreatic cancer: a dose–response meta-analysis of cohort studies. BMC Cancer 2016;16:212. DOI 10.1186/s12885-016-2241-1
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
==============================================================================
Critique 183: An unusual analysis of the association of alcohol consumption with mortality — 24 March 2016
The stated purpose of this new analysis was to determine whether misclassifying former and occasional drinkers as abstainers and other potentially confounding study characteristics underlie observed positive health outcomes for low volume drinkers in prospective studies of mortality. Unfortunately, the authors include in their analyses a number of old epidemiologic studies and do not acknowledge that when the “errors” that they have commented on in the past (such as including heavy ex-drinkers in the no-alcohol referent group) have been dealt with in the majority of studies over the past decade. The authors still exclude the vast majority of these well-done studies in their new meta-analysis. Results of essentially all studies that adjust for their concerns continue to show a significant and meaningful reduction in the risk of cardiovascular disease (CVD) and total mortality from the moderate intake of wine and alcohol.
Forum members note how very selective the authors are in choosing which papers to include in their new analyses: they identified 2,575 studies on the subject, analyzed 87, but then they found some reason to exclude almost all of these studies to reach a conclusion that “ . . . there was no significant protection for low-volume drinkers (RR = 1.04, 95% CI [0.95, 1.15])” based on what is apparently only 6 remaining studies! The paper ignores the comments by two other scientists (Roerecke & Rehm) who, like these authors, have in the past been very concerned that confounding and errors weaken the purported relation between alcohol and a lower risk of cardiovascular disease, but have more recently concluded: “For drinkers having one to two drinks per drinking day without episodic heavy drinking, there is substantial and consistent evidence from epidemiological and short-term experimental studies for a beneficial association with IHD risk when compared to lifetime abstainers. The alcohol-IHD relationship fulfills all criteria for a causal association proposed by Hill.”
The authors of the present paper also ignore the immense amount of experimental data, not only animal experiments but trials in humans, that have described the mechanisms by which moderate alcohol and wine intake have been shown to decrease essentially all of the risk factors for CVD, including low HDL-cholesterol, elevated LDL-cholesterol, endothelial dysfunction, coagulopathies, inflammation, abnormal glucose metabolism, and many others. The consistent finding of lower CVD risk among moderate drinkers in all well-done cohort studies is strongly supported by experimental evidence of the mechanisms.
In the opinion of Forum members, the present paper markedly distorts the accumulated scientific evidence on alcohol and CVD. As stated by one Forum member, “The biased selection of studies that are included undermines the value of the paper, but more importantly promulgates misinformation in the name of appropriate scientific method. Failure to acknowledge the robust body of knowledge that supports the opposite conclusion, and disqualification of extensive animal and cell culture studies that offer plausible biologic explanation of observed benefits, is unconscionable.”
The Forum concludes that the overwhelming body of observational scientific data, as well as an immense number of experimental studies, support the contention that, for most middle-aged and older men and women who choose to do so, the regular consumption of small amounts of an alcoholic beverage can be considered as one component of a “healthy lifestyle.” Such a habit has been shown to be associated with a lower risk of cardiovascular disease and of total mortality.
Reference: Stockwell T, Zhao J, Panwar S, Roemer A, Naimi T, Chikritzhs T. Do “Moderate” Drinkers Have Reduced Mortality Risk? A Systematic Review and Meta-Analysis of Alcohol Consumption and All-Cause Mortality. J Stud Alcohol Drugs 2016;77:185–198.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 182: A major meta-analysis on the association of alcohol consumption with the risk of diabetes mellitus — 8 March 2016
Most previous studies have shown that consumers of light-to-moderate amounts of alcoholic beverages tend to have a significant reduction in their subsequent risk of developing Type II diabetes mellitus (DM). The purpose of the present study was to explore and summarize the evidence on the strength of the association between alcohol consumption and the subsequent risk of DM by using a dose-response meta-analytic approach. The authors identified 26 prospective cohort studies providing data appropriate for a meta-analysis; their analyses were based on 706,716 individuals (275,711 men and 431,005 women) with 31,621 cases of DM.
This meta-analysis reports that light and moderate drinkers have a significantly reduced risk of developing DM. For “light” drinkers (defined as an average of ≤ 12 g/day of alcohol), in comparison with non-drinkers, the overall risk ratio for DM was 0.83, with 95% CIs of 0.73, 0.95 (P = 0.005). For “moderate” drinkers (>12- <24 g/day), the RR was 0.74, with 95% CIs of 0.67, 0.82 (P = 0.001). Thus, data from this meta-analysis indicate a 17% and 26% reduction in the risk of DM, respectively, for these two drinking categories.
For subjects classified as “heavy” users of alcohol (reported intake averaging ≥ 24 g/day), the RR was 0.98, with 95% CIs of 0.83, 1.09, P = 0.480), interpreted as no effect. In a figure in the paper showing the separate results for each individual study included, the point estimates for the risk of DM were 1.0 or less than 1.0 for light and moderate drinkers in essentially all studies. Thus, data from the individual studies support the overall finding of a decrease in risk of DM for light or moderate drinkers.
Sub-group analyses showed that when subjects were stratified by sex, age, BMI, smoking, physical activity, and family history of DM, the point estimates of the risk ratios associated with light or moderate alcohol consumption were less than 1.0 in all groups, adding further to the robustness of the overall conclusions of a reduction in risk of DM from alcohol intake. Similarly, for all subjects, as well as for men and women separately, there was a clear U-shaped curve for the association. The nadir of the effect was just over 20 grams of alcohol per day (about 2 typical drinks), and even the risk of heavy drinkers did not reach the estimated risk of non-drinkers.
Forum members considered this to be a well-done analysis that confirms most previous results from prospective studies indicating a reduction in the risk of developing DM associated with moderate drinking. Further, an increasing number of randomized clinical trials are supporting such beneficial effects on the development and clinical treatment of DM. The Forum thought it unfortunate that beverage-specific results were not available in this study, as increasingly it is being shown that, beyond alcohol effects, there are polyphenols and other substances in wine and beer that provide additional protection against diabetes. Further, the Forum felt it important to also emphasize the protective effects against cardiovascular disease among subjects who already have DM, who are especially vulnerable to coronary heart disease and other effects of atherosclerosis.
Overall, this meta-analysis based on a large number of subjects indicates that the risk of DM is considerable lower among light and moderate drinkers than among abstainers. This finding supports the contention that, for most middle-aged and older adults (with the exception of individuals with specific prohibitions against alcohol such as former drug or alcohol abuse, certain types of neurological or severe hepatic disease, etc.), moderate alcohol consumption should be considered as a component of a “healthy lifestyle” that reduces the risk of diabetes and most of the chronic diseases of ageing.
Reference: Li X-H, Yu F-F, Zhou Y-H, He J. Association between alcohol consumption and the risk of incident type 2 diabetes: a systematic review and dose-response meta-analysis. Pre-publication: Am J Clin Nutr 2016; doi: 10.3945/ajcn.115.114389.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 181: Support for a causal role of alcohol consumption in improving the lipid profile — 16 February 2016
The present paper is based on data from more than 10,000 Americans of European descent who were participants in the Atherosclerosis Risk in Communities (ARIC) study. Common and rare variants in alcohol dehydrogenase and acetaldehyde dehydrogenase genes were evaluated using Mendelian randomization (MR), and then a genetic score based on 5 SNPs was used in regression analyses for the association of alcohol with lipids. Results reported by the authors state: “Alcohol consumption significantly increased HDL2-c and reduced TG, total cholesterol, LDL-c, sdLDL-c, and apoB levels. For each of these lipids a non-linear trend was observed. Compared to the first quartile of alcohol consumption, the third quartile had a 12.3% lower level of TG (p < 0.001), a 7.71 mg/dL lower level of total cholesterol (p = 0.007), a 10.3% higher level of HDL2-c (p = 0.007), a 6.87 mg/dL lower level of LDL-c (p = 0.012), a 7.4% lower level of sdLDL-c (p = 0.037), and a 3.5% lower level of apoB (p = 0.058, P overall = 0.022).”
The authors thus conclude that “This study supports the causal role of regular low-to-moderate alcohol consumption in increasing HDL2-c, reducing TG, total cholesterol, and LDL-c, and provides evidence for the novel finding that low-to-moderate consumption of alcohol reduces apoB and sdLDL-c levels among European-Americans.”
Forum members considered this to be a well-done and important study, the results of which indicate favorable effects of moderate alcohol consumption on lipid factors. However, they doubt that the inclusion of the genetic score from MR played a large part in the results; the authors state that the genetic score used in this paper explained only approximately 0.1% variance of alcohol consumption, suggesting that it was a weak instrumental variable for the MR. Several Forum members stated that randomized control trials, especially cross-over trials, testing the effects of alcohol intake on risk factors, may provide even better evaluation of alcohol’s effects on lipids. Until large-scale RCTs of alcohol and disease occurrence can be are carried out, such RCTs may provide the most reliable data on mechanisms of alcohol’s effects on the risk of cardiovascular disease.
Overall, the present study provides important data indicating that light-to-moderate alcohol consumption has favorable effects on most lipid values. The effects shown for HDL-cholesterol support much earlier data, and the effects on small dense LDL-cholesterol and ApoB provide key new information. The effects on lipids are surely important factors in the protective effects of moderate drinking against cardiovascular disease that have been seen in almost all well-done cohort studies.
Reference: Vu KN, Ballantyne CM, Hoogeveen RC, Nambi V, Volcik KA, Boerwinkle E, Morrison AC. Causal Role of Alcohol Consumption in an Improved Lipid Profile: The Atherosclerosis Risk in Communities (ARIC) Study. PLoS One 2016;11:e0148765. doi: 10.1371/journal.pone.0148765. eCollection 2016.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 180: The association of alcohol intake with total mortality risk among women — 9 February 2016
The follow up of more than 6,000 women in a population-based cohort in an area of southern Sweden was used to estimate how baseline levels of alcohol consumption, at age 50-59 years, related to total mortality risk over the subsequent 17 years. At baseline, 26% of women reported no alcohol consumption while 13% reported an average of 12 or more grams of alcohol per day. Thus, the large majority (61%) were light drinkers, reporting the equivalent of no more than one drink per day. The authors report that, even when adjusting for education, marital status, smoking, BMI, physical fitness, diabetes and ischemic heart disease before screening, mortality risk during follow up was significantly higher among non-drinkers and heavier drinkers than among women reporting the equivalent no more than one typical drink per day. They state that their analyses thus support a “J-shaped” association between alcohol and total mortality risk, and that “The observed protective effect of light drinking (1–12 grams/day) could thus not be attributed to any of these known confounders.”
Forum members agreed this was a well-done study, but noted that the authors were unable to adjust for the pattern of drinking (regular versus binge), previous drinking among abstainers, or potential changes in drinking during follow up. Also, beverage-specific results are not presented. Further, the data presented in this study are not adequate to judge the specific level of alcohol consumption at which total mortality risk for drinkers reaches or exceeds the risk for non-drinkers; in other words, the “threshold” for adverse effects of alcohol on mortality cannot be determined very well. Nevertheless, the results of these analyses are very consistent with most long-term follow-up studies and support a “J-shaped” association between alcohol and the risk of total mortality.
Reference: Midlöv P, Calling S, Memon AA, Sundquist J, Sundquist K, Johansson S-E. Women’s health in the Lund area (WHILA) – Alcohol consumption and all-cause mortality among women – a 17 year follow-up study. Pre-publication: BMC Public Health 2016;16:22. DOI 10.1186/s12889-016-2700-2.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 179: Response to proposed guidelines regarding alcohol consumption in “Guidelines for a Healthy Diet” from the the Health Council of the Netherlands – 26 January 2016
The Health Council of the Netherlands has published “Guidelines for a Healthy Diet” that include a section related to alcohol consumption. Our Forum has been asked to provide comments on the alcohol guidelines (an English translation of certain sections related to alcohol consumption are attached as an appendix to the full review of these guidelines). The closing guidelines given in the Dutch document are as follows: “Do not drink alcohol, or at least no more than one glass per day. [The guidelines from 2006 recommended limiting one’s alcohol intake to one glass (women) or two glasses (men). The current data suggests that the guideline for men should be adjusted downwards.]”
Forum members were concerned that the guidelines were based on a very restricted number of the many hundreds of excellent epidemiologic and experimental publications in recent years that clearly indicate that moderate alcohol has favorable effects on most of the diseases of ageing, and on total mortality risk. For example, the proposed guidelines focus on adverse effects of alcohol on lung cancer, while current scientific knowledge suggests that it has negligible effect. Much of the discussion in the guidelines focusses on the dangers of alcohol on cancer, whereas data show that almost all of the risk (except for breast cancer) is from heavy drinking, not light-to-moderate drinking. Data strongly support a major role of alcohol abuse for upper aero-digestive cancers, but only minor effect on cancer in general from light-to-moderate drinking, especially when other lifestyle factors and under-reporting of intake are taken into account.
The findings for a benefit of moderate drinking on cardiovascular disease among middle-aged and older adults are very much under-played, despite overwhelming data showing a significant benefit. The “J-shaped” curve (lower risk of many diseases with light-to-moderate alcohol intake with higher risk for heavier drinking) is not presented in the guidelines, a major omission when presenting data on alcohol to the public. The additional protection against disease when moderate alcohol consumption occurs with meals was not mentioned. As one Forum member commented: “When professionals discuss alcohol consumption, what consumers want to know is first ‘how much,’ and then ‘when’ to drink.”
Overall Forum members considered that the proposed guidelines regarding alcohol consumption from the Health Council of the Netherlands in a number of sections do not reflect current scientific knowledge on the association of alcohol to health and disease. Forum members tend to agree with the statement of Boffetta and Hashibe who, in an extensive review of alcohol and cancer, stated that “Drinking, especially heavy drinking, increases cancer risk. However, total avoidance of alcohol, although optimum for cancer control, cannot be recommended in terms of a broad perspective of public health, in particular in countries with high incidence of cardiovascular disease.”
Forum members consider that it is important to describe both the potential harms and benefits for health associated with alcohol consumption, especially for middle-aged and older adults. The “J-shaped” curve should be an important concept in any guidelines on drinking that are presented to the public.
Reference: An English translation provided to the Forum includes parts of Section 8 of the Guidelines for a Healthy Diet, from the Health Council of the Netherlands; this material is included as an Appendix to the full report of this critique.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 178: The association of alcohol intake with health-related quality of life — 12 January 2016
Many studies have shown that moderate alcohol drinkers tend to have higher ratings of their quality of life (QOL) than non-drinkers. The directionality of this association has been difficult to ascertain: does moderate drinking improve someone’s QOL, or do people with higher QOL to begin with tend to drink alcohol moderately? The present study attempts to provide data designed to evaluate the directionality of these associations for both physical aspects of QOL as well as mental aspects.
Forum reviewers considered this to be a very well-done study from the Nurses’ Health Study II, with excellent and repeated measurements of both alcohol consumption and indices of QOL. It deals with the assessment of both physical and mental aspects of quality of life as well as the directionality of such an association: subjects were repeatedly assessed for the effects of alcohol intake on subsequent QOL as well as the effects of a given QOL measure on subsequent alcohol intake.
The key reported findings of this study were a positive association between alcohol and subsequent indices of physical QOL indices, with the poorest outcomes in abstainers and former drinkers; in spline analyses, the favorable effect appears to be up to about 2 drinks/day. Subjects with higher physical QOL also appeared to consume more alcohol in subsequent assessments. Somewhat surprising was the finding of little relation between alcohol and mental aspects of QOL, and even an apparent deleterious effect at the highest category of drinking. Thus, the study reports that physical aspects of QOL are positively associated with alcohol consumption, while mental aspects show little relation.
There was some concern by some Forum members about the methods used by the authors in adjusting, or not adjusting, for previous exposures (both alcohol and indices of QOL). Given that both baseline alcohol intake and QOL measures may tend to remain rather static over the period of the study (this “prevalent” exposures), adjusting for the effects of baseline values could attenuate any effect seen on subsequent outcomes. For example, if alcohol consumption indeed affects QOL and consumption remains roughly the same over the time period of the study, any effect of subsequent alcohol on QOL may be subsumed by the effects shown at baseline. In that situation, the net effect of adjustment for baseline alcohol may attenuate (or remove) the effect of the follow-up exposure on the outcome variable. The authors of this paper were aware of this problem, and attempted to deal with it. However, from the data presented, it is not possible to ascertain the specific analytic procedures used, and the final estimates of effect given for alcohol and QOL may still be biased.
Overall, the Forum considers this to be an important contribution to our understanding of how alcohol consumption may affect quality of life, and how quality of life affects alcohol consumption. As interpreted by the authors, physical aspects of QOL may be positively affected by alcohol consumption, but there is little effect on mental aspects of QOL.
Reference: Schrieks IC, Wei MY, Rimm EB, Okereke OI, Kawachi I, Hendriks HFJ, Mukamal KJ. Bidirectional associations between alcohol consumption and health-related quality of life amongst young and middle-aged women. J Intern Med 2015, pre-publication. doi:10.1111/joim.12453.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 177: A clinical trial testing the effects of alcohol on inflammatory markers — 21 December 2015
While there have been many observational studies of the relation of alcohol consumption to health risks and benefits, the number of clinical trials of alcohol administration for its health effects are limited. The present paper is based on a controlled diet cross-over trial among 53 postmenopausal women. A standard diet was provided for a period of 6 months; two meals each weekday were consumed at the study facility and food was provided for other meals. To the standard meal, during three 8-week interventions, either 0, 15 g, of 30 g of alcohol (ethanol) were added to the daily diet, with the two doses of alcohol the equivalent of a little over one typical drink and 2 ½ typical drinks. Weight remained stable and no adverse effects were reported.
The key results of the trial were that, during periods when alcohol was consumed, there were small but significant decreases in markers of cellular adhesion molecules and components in the hemostatic pathway; these are indices of inflammation and the effects are consistent with a decreased risk of cardiovascular disease (CVD). Specifically, reductions were seen when alcohol was administered for s-ICAM, fibrinogen, and D-dimer, all of which would be expected to lower CVD risk. PAI-1 increased with alcohol, and there were no effects on CRP, Factor VIIc or IL-6.
While there were a number of question about the study, Forum members considered that, overall, this was a very well-done, difficult-to-carry-out study that shows alcohol’s beneficial effects on a number of inflammatory and hemostatic factors. The results are in line with many observational studies, although some previous intervention studies have found such effects only after the administration wine (but not of gin), suggesting a key effect of the polyphenols in wine. This study indicates that ethanol itself may have similar beneficial effects on mechanisms that relate to the development of cardiovascular disease.
Reference: Stote KS, Tracy RP, Taylor PR, Baer DJ. The effect of moderate alcohol consumption on biomarkers of inflammation and hemostatic factors in postmenopausal women. European J Clin Nutrition 2015; advance online publication. doi:10.1038/ejcn.2015.182
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 176: A New Report on Alcohol Consumption and Total Mortality Risk — 14 December 2015
Most observational studies have found that moderate drinkers, in comparison with nondrinkers, tend to have lower risk of all-cause (total) mortality; this is probably related primarily to a reduction in the risk of cardiovascular disease, the leading cause of death among the elderly. This large study has conflicting findings, as the author claims that the present analyses do not demonstrate protection against mortality from light-to-moderate drinking. In this study, what were termed “occasional drinkers,” rather than nondrinkers, were used as the comparison group.
Forum members had two main concerns about this study that warrant an investigation of the author’s conclusions: there was no consideration of under-reporting of alcohol intake when declaring “occasional drinkers” as the referent group, and (2) the inclusion, and adjusting for as “confounders,” several factors that are actually mechanisms by which alcohol has been shown to reduce mortality.
The first concern could have led to many light drinkers being included in the referent group, and thus not evaluated for a potential protective effect of light drinking on mortality. In fact, presented only in the Appendix to the paper are data showing that when nondrinkers make up the referent group, consumers of 1-7 as well as 7-14 drinks per week show significant 20-30% reductions in the risk of mortality; these findings are very similar to those of most previous epidemiologic studies.
The second, and perhaps more important concern, is that some of the mechanisms by which moderate alcohol intake may lead to lower mortality, such as reducing the risk of diabetes and coronary heart disease, were “adjusted” for in the analyses. This would attenuate or even erase any true reduction in risk of mortality from moderate drinking.
Some Forum members also were concerned that some subjects were missing data on alcohol consumption but, rather than excluding them, an estimated value was imputed for them. Further, data on the pattern of drinking (regular moderate versus binge drinking) or on the type of beverage consumed were not included in the evaluation.
Forum members conclude that the results of this study will obviously be considered in conjunction with other scientific data when seeking to judge the relation of alcohol intake to mortality. However, concerns about the analysis raise questions about the conclusion of the author of no protective effect of alcohol on mortality, a finding that conflicts with the results of most previous studies.
Reference: Goulden R. Moderate Alcohol Consumption Is Not Associated with Reduced All-cause Mortality. Am J Med 2015; pre-publication. http://dx.doi.org/10.1016/j.amjmed.2015.10.013.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 175: An update on the association of alcohol consumption with breast cancer: Effects of BMI — 24 November 2015
Most observational epidemiologic studies have shown a slight increase in the risk of breast cancer for women who consume alcohol; the degree of increase is usually small for light-to-moderate drinkers (between 5% and 15% increase for consumers of no more than one drink/day), but the risk may be higher for women consuming greater amounts of alcohol. However, there are a number of factors that affect this relationship, including the type of study (cohort or case-control), the pattern of drinking (regular versus binge), the type of beverage consumed, folate intake, use of hormone replacement therapy, as well as genetic factors. It has also been shown that the risk of breast cancer among obese women tends to be higher than among non-obese women, but there are limited data on how obesity interacts with alcohol in affecting the risk of breast cancer. It is clear that alcohol consumption cannot be evaluated in isolation, without considering other factors that relate to the development of breast cancer.
The present study is based on a large cohort of Swedish women who were examined as part of the Women’s Lifestyle and Health Study in 1991 – 1992, then followed through 2009 for the development of breast cancer: 1,385 cases were ascertained among the more than 45,000 women in the study. Alcohol was assessed at baseline and again at the follow-up examination, and the diagnosis of breast cancer was gleaned through linkage to the nationwide health registries in Sweden. Almost all of the women were pre-menopausal at baseline.
Forum members considered this to be a very well-done study, with almost complete ascertainment of cancer cases. There were some concerns, however, including the fact that the height and weight of subjects was not measured but self-reported, perhaps resulting in less accurate estimates of BMI. Further there may have been residual confounding from other factors related to breast cancer that were not assessed. Finally, the reported levels of alcohol consumption among the women in this study were very low (72% of the cohort drank either zero alcohol or below 5 g per day), but it cannot be determined if these are indeed the levels in this population or whether there may have been under-reporting of consumption.
The key findings as reported by the authors were that, overall, there was “no statistically significant association between alcohol intake and breast cancer risk after adjustment for confounders.” While this is indeed supported by their data, Forum members warned that readers should also note that there was an increase in risk found in less-obese women (BMI ≤ 25 kg/m2), among whom there was a step-wise increase in the risk ratio for cancer from 1.0, to 1.05, to 1.19, to 1.32 with increasing category of alcohol intake. This association was not seen in the more obese women for total cancer or for any of the sub-categories of cancer.
While the overall results did not show an increase in risk from alcohol intake, the results among non-obese women are similar to those seen in many other studies, and suggest a slight increase in the risk of breast cancer associated with alcohol for at least some women. The differences in effect according to BMI reported by the investigators are interesting and add to our understanding of the association of alcohol with breast cancer which, however, remains unclear.
Reference: Shin A, Sandin S, Lof M, Margolis KL, Kim K, Couto E, Adami HO, Weiderpass E. Alcohol consumption, body mass index and breast cancer risk by hormone receptor status: Women’ Lifestyle and Health Study. BMC Cancer 2015;15:881 (DOI 10.1186/s12885-015-1896-3)
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 174: Two-year clinical trial of wine administration in diabetics who were previous abstainers or very-light drinkers — 19 October 2015
Observational epidemiologic studies have consistently found that moderate drinkers are at lower risk of cardiovascular disease (CVD); such alcohol consumption also lowers both the risk of diabetes as well as of CVD among diabetics. However, there have been few clinical trials of the administration of alcohol or wine among diabetics, and most have been for relatively short periods of time. Forum members welcomed the publication of the results of the present study, and consider that it provides valuable information on the relation between wine and cardiometabolic risk.
In this study, among 224 subjects with diabetes aged 40 to 75 years who were abstainers or very light drinkers (previously reported none or < 1 drink/week), the investigators carried out a randomized clinical trial of the effects of wine on cardiometabolic factors. The subjects were randomly assigned to 150 mL of mineral water, white wine, or red wine with dinner for 2 years; all groups followed a Mediterranean diet without caloric restriction. The study was described to subjects as a dietary intervention, and there were group sessions led by clinical dietitians each month for the first three months and then at 3-monthly intervals thereafter. The focus was on the Mediterranean diet, and wine was not discussed at these meetings. There was excellent compliance with the provided beverages (>80%) and excellent continued participation of subjects (94% for one year and 87% for the full two years).
The key results of this study were that the administration of 150 ml of red wine with dinner each evening, in comparison with mineral water, favorably affected many cardiometabolic factors, and especially led to an increase in HDL-cholesterol and apolipoprotein (a). The administration of similar amounts of white wine was also beneficial, and specifically improved measures of glycemic control.
Further, in 203 of the subjects, effects according to the genetic factors determining ADH were evaluated. In the study, 35.6% of subjects were homozygous for the polymorphism for “slow ethanol metabolism,” 21.3% were homozygous for that for “fast ethanol metabolism,” and 43% were heterozygous. Forum members agreed with the summary statement of the authors: “We found that diabetic patients who were slow alcohol metabolizers had improved glycemic control by initiating moderate wine consumption, which suggests that alcohol may play a role in glucose metabolism. In contrast, diabetic patients who were fast ethanol metabolizers benefited the most from the wine-induced BP-lowering effect, which suggests a mediatory role for ethanol metabolites.”
The study has important implications for advice to be given to diabetics. Most, but not all, Forum members agreed with the authors’ conclusion that “Initiating moderate wine intake, especially red wine, among well-controlled diabetics as part of a healthy diet is apparently safe and modestly decreases cardiometabolic risk.”
Reference: Gepner Y, Golan R, Harman-Boehm I, . . . Stampfer MJ, Shai I, et al. Effects of initiating moderate alcohol intake on cardiometabolic risk in adults with type 2 diabetes. A 2-year randomized, controlled trial. Ann Intern Med 2015; pre-publication. doi:10.7326/M14-1650
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 173: A Large Study of the Association of Alcohol with the Risk of Acute Myocardial Infarction — 15 October 2015
This paper presents prospective data from a large population-based cohort from rural Norway, a region with typically light alcohol drinking and many abstainers who were not ex-heavy drinkers. It relates reported alcohol intake, assessed on two occasions, with the risk of developing an acute myocardial infarction (AMI). Its key findings are that, even in this very light-drinking population, drinkers had significantly lower risk (about 20% to 30%) of developing a MI than non-drinkers. As the authors conclude: “Light-to-moderate alcohol consumption was linearly associated with a decreased risk of AMI in a population in which abstaining from alcohol is not socially stigmatized. Our results suggest that frequent alcohol consumption is most cardioprotective and that this association is not driven by misclassification of former drinkers.”
As this was a rather homogeneous rural cohort without huge differences among subjects in socioeconomic status, it allows much better control of confounding. The fact that these results show essentially a continuous inverse association (rather than the usually seen “J-shaped” curve) is not unexpected given the very few heavy drinking subjects in this cohort. In addition to cardiovascular disease, the investigators also reported effects on total mortality, which showed a “J-shaped” curve.
Forum members considered this to be a very well-done study, and supports almost all previous research showing a protective effect of moderate drinking on the risk of coronary heart disease. The authors had good data on alcohol exposure and the occurrence of AMI. A key result from this study is that frequent light drinking, even less than an average of one drink/day, is associated with a significant decrease in the risk of coronary heart disease. Based on this study and most previous research, the clear message to the public remains: if you have no contraindications to alcohol use and decide to consume an alcoholic beverage, the healthiest approach is to drink frequently but in small amounts.
Reference: Gémes K, Janszky I, Laugsand LE, Lászlo KD, Ahnve S, Vatten LJ, Mukamal KJ. Alcohol consumption is associated with a lower incidence of acute myocardial infarction: results from a large prospective population-based study in Norway. J Intern Med 2015; doi: 10.1111/joim.12428.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===========================================================================================================
Critique 172: Alcohol and the risk of developing diabetes — 7 October 2015
Prospective cohort studies for decades have tended to show that the risk of developing Type II diabetes mellitus is reduced among moderate drinkers in comparison with non-drinkers, with previous meta-analyses suggesting that moderate drinkers may have about 30% lower risk than that of abstainers. The present study carried out a multi-language search for studies on alcohol and diabetes and conducted a meta-analysis involving almost two million subjects from a final group of 38 cohort, case-cohort, case-control, or nested case-control studies. The main conclusions of the authors are that only females may show a significant inverse association between alcohol consumption and the risk of diabetes, and that previous studies may have overestimated the reduction in risk from moderate drinking.
Forum members had concerns about the analyses and the conclusions of the authors, as the males in the study were primarily Asian (86%), and there were huge differences between the associations with alcohol for Asian and non-Asian populations. There are always problems when the basic study data have a marked degree of heterogeneity. In general, many of the factors that relate to diabetes (diet, body size and adiposity, type of beverages consumed, etc.) are quite different between Asians and non-Asians; combining such groups when their analyses show opposite effects of alcohol on diabetes risk may not be a reasonable way of trying to develop results that apply globally. Forum members do not believe that the analyses presented in this paper can support the conclusion of the authors that there is “no effect among males.” It could be unwise if the results of this study were used to develop alcohol guidelines for western populations.
The authors could not take the pattern of drinking (regular versus binge) or the type of alcohol into consideration. Clinical trials have suggested that wine and its polyphenols may have effects above and beyond those seen with alcohol alone, and beneficial effects of such polyphenols have been demonstrated both for women and for men. Thus, while the analyses in this paper were all carried out accurately, attempting to use these data to develop guidelines that would apply globally, as was done by the authors, may not be appropriate.
Reference: Knott C, Bell S, Britton A. Alcohol Consumption and the Risk of Type 2 Diabetes: A Systematic Review and Dose-Response Meta-analysis of More Than 1.9 Million Individuals From 38 Observational Studies. Diabetes Care 2015;38:1804–1812 | DOI: 10.2337/dc15-0710
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 171: A global assessment of alcohol and health — 29 September 2015
The present publication is from the very large Prospective Urban Rural Epidemiological (PURE) study that focuses especially on middle-income and lower-income countries, for which previous data on the association of alcohol consumption with health outcomes are sparse. Included in this analysis are data from high-income countries (HICs: Sweden and Canada); upper-middle-income countries (UMICs: Argentina, Brazil, Chile, Poland, South Africa and Turkey); lower-middle-income countries (LMICs: China and Columbia); and low-income countries (LICs: India and Zimbabwe). The large majority of the subjects were from lower income countries.
It has long been recognized that, when evaluating the health effects of drinking, it is especially important to evaluate alcohol intake within a particular population, with its specific genetic, lifestyle, environmental, and cultural factors, and not study alcohol in isolation. While the PURE study is a very well-done study, Forum members were concerned that the authors have attempted to answer overall questions about alcohol and health by combining data from such diverse populations. For example, the issue of very different causes of mortality in different populations would lead to very different approaches to improving longevity. There are too many factors associated with health outcomes to attempt to determine the specific alcohol effects when considered in isolation.
The authors tried to adjust for confounders as far as that was possible, but one cannot exclude further confounding, especially as subjects from lower-income countries contained a much larger proportion of smokers than there were in higher-income countries. The authors also point at differences between countries not fully explained by drinking pattern (or other factors); this suggests that further confounding exists. Further, lumping all types of stroke into one category may be hiding associations, especially as lower-income countries might have a higher frequency of cerebral hemorrhages. Similarly, using a single grouping for all cancers may be inadequate. Other limitations of this study include the short duration of follow-up time (4.3 years) and the low number of cases of each outcome.
The Forum concluded that even though the study includes information from many countries, it is not possible from such data to determine net health effects of alcohol consumption that are applicable to people everywhere. Their analytic results cannot be used, as the authors suggest, to “support global health strategies,” although they may surely be useful for developing “national initiatives to reduce harmful alcohol use,” especially for lower-income countries.
Reference: Smyth A, Teo KK, Rangarajan S, O’Donnell M, Zhang X, Rana P, Leong DP, et al. Alcohol consumption and cardiovascular disease, cancer, injury, admission to hospital, and mortality: a prospective cohort study. Lancet 2015. Pre-publication. http://dx.doi.org/10.1016/ S0140-6736(15)00235-4. Online/Comment http://dx.doi.org/10.1016/ S0140-6736(15)00236-6.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 170: An update on the association of alcohol consumption with the risk of cancer — 1 September 2015
This well-done analysis based on data from two very large cohort studies, the Nurses’ Health Study and the Health Professionals’ Follow-up Study, evaluated the association of alcohol consumption over many years with the risk of cancer. The authors conclude that men reporting an average intake of more than 15 grams of alcohol per day, but not less, have a significant increase in risk of alcohol-related cancers. In women, however, even the consumption of an average of 5.0 – 14.9 grams of alcohol per day (the equivalent of between ½ and 1 ½ typical drinks) was associated with a slight increase in total cancer risk, stated to be primarily from an increase in the risk of breast cancer. For both genders, there seemed to be a dose-response increase in risk of cancer with larger amounts of alcohol. At the same time, smoking was identified as an even more important risk factor than alcohol for these cancers.
Forum members considered this to be an important study presenting data that are of relevance to individuals and agencies providing advice regarding alcohol consumption. There is little question that heavy drinking markedly increases the risk of upper aero-digestive cancers, and no physician or agency advises people to consume in excess of the typical limits of no more than one or two drinks/day. Hence the finding in this study of an increase in some cancers among women (especially breast cancer) even for lighter drinking has implications for alcohol policy.
The Forum was disappointed that all dietary and other lifestyle factors that have been shown to increase the risk of cancer (data that are known to be available to these investigators) were not included in their report. Members were especially concerned that the net effects on health and mortality of light-to-moderate alcohol consumption were not commented upon in the paper. Given that the risk of the most common causes of death, especially cardiovascular diseases, are reduced by moderate drinking, it seems that the authors should have included data, or at least mentioned, the effects of alcohol on cancer mortality and, especially, on total mortality. It has recently been emphasized that cohort studies that report on only one outcome (in this case, cancer) but do not mention other outcomes that are affected by the same exposure, especially total mortality, do not present the full picture, and can lead to biased recommendations. The inclusion of such information from these cohorts could provide even more valuable data upon which to develop appropriate guidelines for alcohol use by individual patients and the public.
Reference: Cao Y, Willett WC, Rimm EB, Stampfer MJ, Giovannucci EL. Light to moderate intake of alcohol, drinking patterns, and risk of cancer: results from two prospective US cohort studies. BMJ 2015;351:h4238; doi: 10.1136/bmj.h4238
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 169: Effects of IQ on risk of morbidity and mortality related to alcohol consumption — 25 August 2015
The present paper is based on a large cohort of subjects in Sweden who had IQ tests as children (when they were 13 years old) and were then followed for more than 30 years. The study reports an inverse association between childhood IQ and hospitalization for alcohol-related diseases or death. The association is strongly dose-dependent, with a marked increase in disease/mortality risk for each decrease in the childhood IQ score.
A key finding in this analysis is that the attained socio-economic status (SES) of the subjects at age 32 played a large role in explaining the association between IQ and alcohol-related disease and appeared to completely explain the association with death from alcohol-related causes. This suggests that much of the effect of IQ during childhood may be through its effect on later education, occupation, and income of the subjects, associations that have been noted in many previous epidemiologic studies to favor better health. It is reassuring that being born into a poor, uneducated family is not as important as a determinant of adverse effects of alcohol later in life as is the attained socio-economic status of the individual in young adulthood.
A possible explanation for the inverse relation of SES in young adulthood with adverse alcohol outcomes could relate to the type of beverage consumed, which was not evaluated in the present analysis. In a previous study from Denmark, it was shown that higher SES in young adults was associated with a strong preference for wine rather than for other types of alcoholic beverage. Wine consumption has been associated with better health in numerous studies, although it is unclear whether this is due primarily to the non-alcoholic constituents in wine or to confounding from associated lifestyle factors of wine drinkers.
Forum members agree with the authors that the underlying causes for an association between IQ (or SES) and adverse alcohol-related disease and death are not clearly defined. It could be that intelligence has effects on health through choices in lifestyle behavior or socioeconomic environment as an adult, or the relationship between intelligence and health is confounded by other factors such as biological or socioeconomic conditions early in life. As for now, we can only describe the association, but not explain it fully.
Reference: Sjölund S, Hemmingsson T, Gustafsson JE, Allebeck P. IQ and alcohol-related morbidity and mortality among Swedish men and women: the importance of socioeconomic position. Journal of Epidemiology and Community Health 2015;69:858-864.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 168: Effects of alcohol on blood pressure in women: A randomized trial — 5 August 2015
The present paper describes the effects among 24 normotensive pre-menopausal women, all of whom were regular drinkers (of an average of 2 to 3 drinks/day), of the administration of two levels of alcohol in the form of red wine in a randomized clinical trial. Subjects were given low amounts of wine and higher amounts of wine during two 4-week intervention periods, with the effects on blood pressure compared with changes when subjects were given similar amounts of dealcoholized red wine. Subjects were divided into a “lower level” usual intake group who previously consumed < 200 g/week of alcohol and a “higher level” group who previously consumed >200 g/week.
Previous “lower level” drinkers were given two levels of alcohol, in the form of 100 ml/day of red wine on 4 days per week (an average of 46 g/week of alcohol, or the equivalent of about ½ typical drink per day) and 200 ml/day of red wine daily (about 146 g/week of alcohol, the equivalent of about 1 ½ to 2 typical drinks/day) for another 4-week period. Subjects who were previous “higher level” drinkers were given 100 ml of red wine daily (about 73 g/d of alcohol per week, the equivalent of about one typical drink/day) for 4 weeks and 300 ml/d of red wine (about 218 g/week of alcohol, the equivalent of about 2 to 3 typical drinks/day) for another 4 weeks.
The main results are a small but significant increase in 24-hour average blood pressure (+2.0 mmHg systolic and +1.3 mmHg diastolic) with higher levels of red wine but no significant effects (+0.4 mmHg systolic, -0.3 mmHg diastolic) from lower levels of red wine administration, when compared with blood pressure levels during periods when dealcoholized red wine was given. The differences were predominantly due to slightly higher awake rather than asleep blood pressures. These findings are similar to results of a limited number of randomized controlled trials of alcohol in men.
Forum members considered this to be a well-conducted clinical trial, with important results. There were, however, some concern that the study focused only on regular drinkers; results may have been different if previous abstainers had also been studied. Further, while the slight increase in blood pressure from higher levels of alcohol support previous research, the finding of no significant findings for lower levels of intake (when subjects were given the equivalent of between ½ and 1 drink/day) may not support what the authors suggest: “Our results provide no support for the concept that regular low-level alcohol intake can lower BP, suggesting that the J-shaped relationship between alcohol and BP in several studies is more likely because of the presence of unmeasured confounders.” Forum members considered their results to be consistent with either a slight increase or a slight decrease in blood pressure among such drinkers and are not necessarily inconsistent with data from some previous cohort studies that showed a “J-shaped” relation between alcohol and blood pressure.
A number of Forum reviewers also raised the question as to whether or not the results of a 4-week intervention study can be extended to the effects of the regular intake of alcohol for many years. Further, the fact that the study group included previous drinkers of up to similar amounts of alcohol as given during the higher intervention (yet were still normotensive) might suggest that their blood pressure was not “sensitive” to alcohol, and could limit the applicability of these results to the general public. Nevertheless, this intervention study provides important trial data on the short-term effects of alcohol on blood pressure.
Reference: Mori TA, Burke V, Beilin LJ, Puddey IB. Randomized Controlled Intervention of the Effects of Alcohol on Blood Pressure in Premenopausal Women. Hypertension 2015;66:00-00. DOI: 10.1161/HYPERTENSIONAHA. 115.05773
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 167: What determines a person’s belief that “alcohol is heart-healthy?” — 22 July 2015
This paper, based on data from more than 5,000 adults participating in an internet-based survey, sought to determine what were the perceptions of subjects on the relation of alcohol to heart disease, and how these perceptions resulted in particular behaviors related to alcohol consumption. Partricipants for the survey were recruited by a variety of methods, including announcements “in the lay press, promotional events, word of mouth, social media, e-mail, and clinic visits.” While the goal of the study is commendable, the results of any such survey obviously depend on many social and cultural factors of the people who respond to the survey; it was not a random sample of the population used in this analysis. This is critical because an interpretation of the data requires an understanding of the population surveyed.
Forum members had other concerns about this paper, including the specific survey questions regarding the perceptions of alcohol effects. For example, the key question asked in the survey was “Do you believe alcohol is good for your heart?” Forum members pointed out that it is obvious to nearly everyone that this cannot be answered without quantifying the amount of alcohol or the pattern of drinking. They consisdered that a more appropriate quesiton might be something such as “Do you believe that the moderate consumption of alcoholic beverages can benefit your heart?”
The authors make statements such as “Participants perceiving alcohol as heart healthy consumed 47% more alcohol.” This may sound alarming until it is revealed that the observed difference was from a baseline of 0-3 to 1-5 glasses of wine/week and from 1-7 to 2-8 total drinks/week. These higher amounts are not ‘alarming’ at all, and in fact fall within usual guidelines for “sensible drinking.”
Forum members were particularly upset that the authors misquote a number of scientific papers to support their claim that even low levels of drinking increase the risk of certain diseases. The authors also use such misrepresentations of data to justify their concerns that current guidelines for alcohol consumption may not be appropriate. Forum reviewers found it especially disturbing that the peer review process by the journal failed to uncover such misrepresentations of data.
The authors repeatedly give the impression that they are against any amount of alcohol consumption. They do not comment on the consistent findings in almost all well-done prospective studies indicating that moderate drinkers live longer than abstainers. Further, statements by the authors that suggest that people who think that alcohol is heart healthy are misinformed does not stand up to scientific data, which indicate that moderate and responsible drinking is associated wtith better health and longevity.
It is interesting that the report indicates that older, higher-income, and more highly educated subjects are more likely to consider alcohol to be heart healthy than younger and less-educated subjects. While a question was asked by the investigators as to whether or not the responder’s perception of the health effects of alcohol influences their decision to drink or to not drink, the specific responses to this question are not presented in the paper. It remains unclear to what extent beliefs about alcohol’s potential health effects relate to alcohol use or, more importantly, to alcohol abuse.
Overall, Forum members thought that the idea behind this study was of interest, but emphasized that it is important to collect data based on a random and well described sample of the population if one is to provide significant and understandable results. Further, the report is compromised by what appears to be a deliberate misrepresentation of the prior scientific literature to support the authors’ contention that alcohol is not healthy; there are a number of obvious errors that should have been detected during the review process by the journal. In the opinion of the Forum, the most reliable result from these analyses relates to where people obtain their information regarding alcohol and health: it does not come from physicians or scientific publications, but primarily from the lay press.
Reference: Whitman IR, Pletcher MJ, Vittinghoff E, Imburgia KE, Maguire C, Bettencourt L, Sinha T, Parsnick T, Tison GH, Mulvanny CG, Olgin JE, Marcus GM. Perceptions, Information Sources, and Behavior Regarding Alcohol and Heart Health. Am J Cardiol 2015; pre-publication. http:// dx.doi.org./10-1016/j.amjcard/2015.05-029.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 166: The association between alcohol consumption and suicidal ideation and suicidal attempt — 1 July 2015
The present study evaluates the relation of alcohol consumption and the pattern of drinking with self-reports of suicidal ideation and suicidal attempts among more than 43,000 men and women in Korea, using data from a 2007-2011 survey. Overall, 11.3% of males and 21.2% of females reported that they had experienced suicidal ideation, and 0.8% of males and 1.1% of females had attempted suicide. High scores on the Alcohol Use Disorders Identification Test (AUDIT) and a history of alcoholic blackouts were associated with suicidal ideation among both men and women and, for males, with suicidal attempts.
There is little known about the epidemiology of suicidal tendencies, or the specific causes of suicide. It is generally agreed that depression is the most important risk factor for suicide, and depression can lead to alcohol abuse; however, alcohol abuse can also lead to depression. Unfortunately, with cross-sectional data, analyses such as those in this paper cannot sort out the confounding issues nor, more importantly, address the causality of alcohol consumption with suicidal tendencies. The egg and hen question has never been solved – whether the depression or the heavy drinking came first. Thus, whether alcohol abuse increases the risk of depression (that may lead to suicide) or whether depressed people turn to alcohol seeking relief, cannot be determined from analyses such as these. However, it is also noted that this study suggests that drinking alcohol according to the usual guidelines for “sensible drinking” (generally, advising no more than 1 to 2 drinks/day) is not associated with the risk of suicidal ideation or attempt.
Forum members also commented on the large differences between populations in suicidal tendencies, being much higher in Korea and Japan than in most of Europe and North America. This could limit the applicability of the conclusions of this study to western populations.
Reference: Bae H-C, Hong S, Jang S-I, Lee K-S, Park F-C. Patterns of Alcohol Consumption and Suicidal Behavior: Findings From the Fourth and Fifth Korea National Health and Nutritional Examination Survey (2007–2011). J Prev Med Public Health 2015;48:142-150 • http://dx.doi.org/10.3961/jpmph.14.027
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 165: Fiber intake may modify the association of alcohol consumption with certain hormone-dependent cancers — 4 June 2015
The positive association between alcohol intake and certain hormone-dependent cancers (especially breast cancer) noted in many studies has been attributed to an effect of alcohol through an increase in levels of estrogen and other hormones. The present study had extensive dietary data on more than 5,000 men and women in France, among whom comparisons were made between the sex-specific tertile of alcohol intake and the risk of hormone-related cancers (breast, prostate, ovarian, endometrial, and testicular).
The study found that, overall, the risk of some cancers (e.g., breast) but not others (e.g., prostate) were positively related to reported alcohol intake. The key results reported by the authors are that when the risks of cancer were related to alcohol while adjusting for fiber intake, subjects whose fiber intake was below the median value showed higher risks of cancer related to alcohol, but not subjects with higher fiber intake. For example, when the risk of breast cancer in women was related to the tertile of their alcohol intake, the 2nd tertile showed a HR of 1.55 (1.01 – 2.38) and the 3rd tertile (HR 1.70, CI 1.11 – 2.61), when compared with women in the lowest tertile.
For prostate cancer in men, however, the 2nd tertile showed a HR of 1.28 (CI 0.82 – 2.00) and the 3rd tertile a HR of 0.89 (CI 0.55 – 1.45). The interaction terms between alcohol intake and cancer were not significant for all hormone-dependent cancers or for breast cancer. Only the interaction term for prostate cancer reached statistical significance, but here the relationship between tertile of alcohol intake even among subjects with low dietary fiber did not show a clear dose-response relation.
Forum members had concerns about the large number of potential confounders in these analyses (e.g., different effects for different types of fiber, the intake of fiber being just a marker for folate intake or for other dietary or lifestyle factors), that made it difficult for the authors to reach firm conclusions. Unfortunately, the numbers of tumors for each of the sub-groups were often too small to give meaningful results. And there was no data on alcohol drinking pattern (regular moderate versus binge drinking) or type of beverage consumed. Thus, while this study indicates that alcohol intake may relate to certain hormone-dependent cancers, the analyses do not present a clear demonstration as to whether it is fiber intake or some other related factor that may modify the association.
Reference: Chhim A-S, Fassier P, Latino-Martel P, Druesne-Pecollo N, Zelek L, Duverger L, Hercberg S, Galan P, Deschasaux M, Touvier M. Prospective association between alcohol intake and hormone dependent cancer risk: modulation by dietary fiber intake. Amer J Clin Nutr 2015; pre-publication. Doi: 10.3945/ajcn.114.098418.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 164: Why are the harmful effects of alcohol consumption greater among people with low education and income? — 14 May 2015
Epidemiologists have noted for many years that one of the key factors that modifies the relation between alcohol intake and many diseases is the education, income, or other index of socio-economic status (SES) of subjects. While differences in drinking practices (regular moderate versus binge drinking), other more moderate lifestyle factors, better access to health care, etc., have been suggested as potential mechanisms, there has been little research directed at this relation.
The present study is a systematic review of published reports to investigate the relationship between SES and risk of mortality or morbidity for each alcohol-attributable condition and, where feasible, to explore alcohol consumption as a mediating or interacting variable in this relationship. It summarized data from 31 case-control or cohort studies, relating an overall measure of the effects of low SES (variously defined) to the risk of cancers related to alcohol, as well as to liver disease, hypertension, stroke, epilepsy, cardiac arrhythmias, and pancreatitis.
The key findings of the study demonstrate a tendency for greater risk for low-SES subjects than for high-SES subjects to develop a number of diseases that are associated with alcohol consumption. Specifically, the authors report higher and statistically significant increases in risk of head and neck cancer and of stroke associated with alcohol consumption among lower-SES subjects than among higher-SES subjects. There was a tendency for lower risk of breast cancer among lower-SES women, but differences were not significant when adjusted for known confounders. The authors suggest that some of the effects shown may relate to greater total amounts of alcohol consumption by lower-SES subjects, or due to their higher levels of smoking.
Forum members thought this was a valiant attempt of the authors to unravel what has been a mystery: why do people at lower levels of SES seem to have more adverse effects of alcohol consumption than subjects at higher levels of SES. Unfortunately, as the authors admit, current scientific data do not allow firm answers. Suggested theories for reasons why low-SES subjects may have more adverse effects from alcohol include (1) different drinking patterns, with more binge drinking, (2) clustering of poor lifestyle factors, and (3) less access to health care. In some studies, even though the reported total alcohol intake of low- and high-SES subjects may be similar, the latter seem more likely to drink moderate amounts of alcohol on a regular basis, while lower-SES subjects are more likely to binge drink on fewer days per week. However, other studies do not support such a finding. Further, there may be differences according to the type of alcoholic beverage consumed, which was not considered in this study.
Forum members pointed out that differences in factors other than drinking patterns probably contribute to the greater adverse effects among subjects with lower SES. One member suggested that lower SES affects susceptibility to many diseases, most likely due to effect modification of hitherto unrecognized factors. The Forum concluded that there are too many confounders to make a conclusion about this topic, and much more research will be needed to understand how socio-economic factors affect the risk of disease and may modify the relation between alcohol consumption and disease.
Reference: Jones L, Bates G, McCoy E, Bellis MA. Relationship between alcohol-attributable diseaseand socioeconomic status, and the role of alcohol consumption in this relationship: a systematic review and meta-analysis. BMC Public Health 2015;15:400. DOI 10.1186/s12889-015-1720-7.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 163: The association of alcohol consumption with the risk of developing heart failure — 5 May 2015
Two new papers have provided data on the association of alcohol consumption with the risk of developing heart failure (HF). The first is a meta-analysis by Larsson et al that is based on eight prospective studies, with more than 200,000 subjects and 6,211 cases of HF. Meta-analyses provide important information because they are usually based on very large numbers of subjects and cases, and can detect smaller increases in risk than seen in individual studies. However, single large prospective cohort studies tend to provide more detailed information on, and allow better adjustment for, potential confounders. The second paper discussed in this critique by Dorans et al, is based on 33,760 men who were followed for 14 years, with almost 3,000 cases of fatal or non-fatal HF.
There was a high degree of consistency between these two studies: both concluded that moderate alcohol consumption, in comparison with non-drinking, is associated with a lower risk of developing HF. The meta-analysis (Larsson et al) concluded that there was a dose-response association between alcohol and HF; for example, a reduced risks of HF for consumers of 3 and 10 drinks/week (a 10% and 17% decreased risk, respectively), but not for those reporting the consumption of 21 drinks/week (a RR of 1.07; 95% CI 0.77 – 1.48). In the report from the single large Swedish prospective study (Dorans et al), the risk of HF for most categories of drinkers tended to be lower than that of never drinkers, with the lowest risk among consumers of 7 – 14 drinks/week (HR=0.81, 95% CI 0.69 – 0.96).
Forum members considered both of these studies to have been very well done, and the similar results not unexpected. HF has many causes, but in developed countries the most common is coronary artery disease (CAD), and moderate drinking has long been known to be associated with a lower risk of developing CAD. In their critique, Forum members discuss other conditions that relate to the development of HF, including conditions (such as respiratory infection, excessive salt intake, non-compliance with prescribed medication, etc.) that may trigger an attack of symptomatic HF.
To summarize, based on previous research and these two excellent papers, current data suggest that the moderate intake of an alcoholic beverage lowers the risk of the development of symptomatic HF. This undoubtedly relates, as least to some extent, to the demonstrated protection of alcoholic beverages against CAD. As for giving advice regarding the consumption of alcohol, Forum members agree with the conclusions stated by Klatsky in his editorial accompanying one of the papers: “All persons should avoid heavy drinking and many persons should avoid all alcohol. However, it is the author’s opinion that many middle-aged and older persons at risk of CAD or HF should be told that he or she is better off as a light to moderate drinker. Dispassionate objectivity plus common sense should dictate advice about drinking.”
References:
- Larsson SC, Orsini N, Wolk A. Alcohol consumption and risk of heart failure: a dose–response meta-analysis of prospective studies. European Journal of Heart Failure 2015;17:367–373. doi:10.1002/ejhf.228
- Dorans KS, Mostofsky E, Levitan EB, Håkansson N, Wolk A, Mittleman MA. Alcohol and Incident Heart Failure Among Middle-Aged and Elderly Men: The Cohort of Swedish Men. Circulation Heart Failure 2015; pre-publication. DOI:10.1161/CIRCHEARTFAILURE.114.001787.
For the full critique of these papers, and general comments on the association of alcohol with heart failure, by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 162: What is the association between alcohol consumption and cancer? 13 April 2015
Three major papers on the association of alcohol consumption and cancer have recently been published. Forum members considered that all were well-done, and presented valuable new information on the topic. While the key findings in each study are similar, each brings specific information on how alcohol relates to the risk of developing cancer. In this critique, we present the authors’ abstracts of each paper, our comments on the paper, and then an overall discussion of the topic.
Problems can occur when combing case-control studies with prospective cohort studies, as was done in one of the papers reviewed, as risk estimates are usually higher in the former type of study and potential confounding may be less complete. Further, it is especially important to consider the interaction between alcohol consumption and smoking for upper aero-digestive tract cancer, as was not always done. And none of the studies covered in this critique emphasized the net effects of alcohol that, because of protective effects against cardiovascular disease, is almost always associated with lower total mortality among moderate drinkers than among abstainers.
In summary, the Forum considers that the three papers reviewed provide important data on one of very few lifestyle factors that have been shown to relate to the risk of cancer. And cumulative research data clearly show that heavy alcohol intake increases the risk of upper aero-digestive tract cancers and some other cancers. Further, in these and many previous reports, even light alcohol consumption was associated with an increase in risk of breast cancer in women. Unfortunately, the threshold level of drinking associated with an increase in risk is not clearly defined for most cancers.
Forum members agree with the conclusions of Klatsky et al, who stated: “At present, a possible increased cancer risk at moderate intake should enter into individual estimation of the overall risk-benefit equation for alcohol drinking, especially for young persons. For most persons older than age 50 years, the overall benefits of lighter drinking, especially the reduced risk of atherothrombotic disease, outweigh possible cancer risk.”
References:
-
-
-
- Klatsky AL, Li Y, Tran HN, Baer D, Udaltsova N, Armstrong MA, Friedman GD. Alcohol Intake, Beverage Choice, and Cancer: A Cohort Study in a Large Kaiser Permanente Population. Perm J 2015;19:March 1, 2015. http//dx.doi.org/10.7812/TPP/14-189
- Bagnardi V, Rota M, Botteri E, et al. Alcohol consumption and site-specific cancer risk: a comprehensive dose–response meta-analysis. British Journal of Cancer 2015;112:580–593. doi: 10.1038/bjc.2014.579
- Wienecke A, Barnes B, Neuhauser H, Kraywinkel K. Incident cancers attributable to alcohol consumption in Germany, 2010. Cancer Causes Control 2015;[Epub ahead of print].
-
-
For the full critique of these papers, and general comments on alcohol and cancer, by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 161: The effects of alcohol consumption on the risk of hip fracture — 31 March 2015
Among elderly people, falls leading to hip fracture are a major health problem, leading to severe morbidity and mortality. Underlying factors that increase the risk of hip and other fractures include osteoporosis and low bone mineral density, as well as an unsteady gait making falls more common. The role that alcohol consumption among the elderly may relate to hip fracture has been a topic of concern for many decades, but data from a number of prospective studies now suggest that light-to-moderate drinking may actually decrease the risk of such fractures, while heavy drinking may increase the risk.
The present meta-analysis is based on prospective studies that have yielded more than 26,000 incidences of hip fracture. It concludes that there is a “J-shaped” association between alcohol consumption, especially of wine, and the risk of hip fractures, with lower risk for a reported consumption of about 1 drink/day, no effect from drinking between 1 and 4 to 5 drinks, and an increased risk from heavier drinking. Part of the “protection” from light drinking is apparently from the effects of alcohol on increasing bone mineral density.
Forum reviewers considered this to be a very well-done meta-analysis that provides balanced information on the risk of this common public health problem. Noting that the major differences seen in this study were between light drinkers and heavy drinkers, it was commented that there are many differences between people who are moderate in their habits, including moderate drinking, and people who usually consume more than 4 or 5 drinks/day; thus, there is still the possibility of other lifestyle factors confounding this association. Also, it was noted that most of the subjects in this analysis were North American or European, so applicability to other racial/ethnic groups may be limited.
In summary, this large and very well-done meta-analysis supports a protective effect of light alcohol consumption on the risk of hip fracture, with an increase in bone density from alcohol being a probable important factor. Data suggest that wine consumption may have the most favorable effect, perhaps indicating that polyphenols and other compounds may also play a role. The study shows that heavy drinking (an average of 4 to 5 or more drinks/day) is associated with an increase in the risk of hip fracture.
Reference: Zhang X, Yu Z, Yu M, Qu X. Alcohol consumption and hip fracture risk. Osteoporos Int 2015;26:531–542. DOI 10.1007/s00198-014-2879-y
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 160: Do the calories in alcoholic beverages lead to increased obesity? — 23 March 2015
Among people who consume alcohol, it would be assumed that the excess calories provided by the alcohol would add to their risk of obesity; however, current data suggest that the association may be more complex. It is unclear to what extent people who consume alcohol may modify other aspects of their diets, either decreasing or increasing other sources of calories. Further, alcohol is metabolized differently from other foods, which suggests that its calories may not be as readily available as those from fat, carbohydrate, and protein to increase obesity. The present paper provides an update on scientific data on the association between alcohol consumption and obesity. The overall conclusions of the authors are that light-to-moderate drinking does not increase the risk of obesity, while heavier drinking (or even moderate drinking among obese subjects) may lead to weight gain.
Forum reviewers appreciated the excellent summary of scientific reports on this topic, and thought that the authors gave a sound and balanced update on the topic. However, mechanisms why numerous prospective epidemiologic studies show that moderate drinking does not increase the risk of obesity are unclear. Given that alcohol contains calories, and if drinking alcohol does not displace the intake of other foods, it would be assumed that such calories would increase the risk of obesity unless there are particular metabolic differences between alcohol calories and those from protein, fat, and carbohydrate.
Potential mechanisms suggested have included a decreased utilization of calories from alcohol due to what is known as ‘Non-exercise Activity Thermogenesis’ (NEAT), in which the metabolism of alcohol may create more heat than fat. Also, the Forum discussion included comments that alcohol could bring into play effects on insulin, glucose, and fat mobilization (however, in the laboratory, such mechanisms tend to increase, rather than decrease, body fat). Also, a reasonable interpretation of the fat tissue decrease related to ‘moderate’ ethanol intake seen in many studies could be an associated decrease in the intake of carbohydrates. One glass of wine substituting for approximately 50 g of glucose could be a reasonable mechanism for shifting the metabolism from lipogenesis to oxidation of lipids. Genetic factors undoubtedly play a role in the effects among individuals.
In summary, this update on the association of alcohol consumption and obesity concludes that most well-done prospective studies show that moderate drinkers do not have an increase in obesity, and in some studies there is even a slight decrease in weight. One possibility is that, especially for wine with meals, satiety may occur earlier and result in less intake of food. However, precise mechanisms for a lack of increase in weight are not known, and the effect could still result from drinkers compensating for their drinks by taking in fewer calories from other sources and perhaps also by being a little more physically active.
Reference: Traversy G, Chaput JP. Alcohol Consumption and Obesity: An Update. Curr Obes Rep 2015;4:122–130. DOI 10.1007/s13679-014-0129-4
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 159: Alcohol as a component of the Mediterranean-type diet; effects on the risk of mortality among diabetics — 17 March 2015
Many scientists have reported on health benefits associated with the traditional diet of much of the Mediterranean area: the primary basis of the diet is on plant-based foods (whole grains, vegetables, fruits), olive oil, moderate wine consumption, and limited intake of meat or dairy products. In 2003, Antonia Trichopoulou and her associates created a scoring system based on the number of components of the Mediterranean Diet (Med-Diet) consumed by subjects, giving a total score to judge the degree that individuals were following a Med-Diet pattern. The score is based on the intake of 7 items (cereal intake, ratio of monounsaturated to saturated fats, vegetables, fruits, nuts, fish, and moderate alcohol), considered to have positive effects, and 2 items (dairy products, meat and meat products) considered to have negative effects. Many groups have found that greater adherence to such a diet (a higher score) is associated with a lower risk of many diseases, and lower mortality. There are limited data on the relative merits of each component of the Med-Diet. In the present paper, the authors attempt to judge the proportion of the protection against mortality that can be attributed to each component of the score.
The authors’ calculations estimated that, in descending order of importance, moderate alcohol consumption (associated with a reduction of 14.7% in the protection against mortality when it was removed from the total score), cereal intake (12.2% reduction), ratio of monounsaturated to saturated fats (5.8%), and consumption of vegetables (5.8%), fruits and nuts (5.2%) and fish (5.0%) lowered mortality risk. Lower intakes of dairy products (reduction of 13.4%) and meat and meat products (3.4%) were also associated with lower mortality. Alcohol has long been known to relate to a lower risk of developing diabetes, and the present study indicates that it is an important factor in reducing the risk of mortality among subjects who have already developed diabetes, as has been shown in previous studies. This study indicates further that the full Med-Diet has very favorable effects on mortality among diabetics.
Forum members considered this to be a well-done attempt to tease apart the relative importance of each component of the Med-Diet as it relates to health outcomes among diabetics. They felt that these researchers from the MOLI-SANI study have published a convincing paper extending the known benefits of the Mediterranean diet to a cohort of type 2 diabetics, a group of subjects at high risk for cardiovascular and all-cause mortality.
There were some questions raised about the precision of the Med-Diet Score, as published and used in this study, in judging the relative contributions of the different dietary constituents, especially because of known complexities in judging the effects of avoiding one particular food when its absence may affect the intake of other foods. And for alcohol, the score used did not permit an evaluation of the role of the pattern of drinking or even the type of beverage consumed, which are known to affect the net effects of drinking on health.
Nevertheless, the results of this study add to an accumulating base of knowledge of the importance of the Mediterranean-type diet in reducing the risk of many health outcomes, including mortality among diabetics.
Reference: Bonaccio M, Di Castelnuovo A, Costanzo S, Persichillo M, De Curtis A, Donati MB, de Gaetano G, Iacoviello L, on behalf of the MOLI-SANI StudyInvestigators.
Adherence to the traditional Mediterranean diet and mortality in subjects with diabetes. Prospective results from the MOLI-SANI study. European Journal of Preventive Cardiology 2015. Pre-publication. DOI: 10.1177/2047487315569409.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 158: Comments on Alcohol Recommendations included in the Scientific Report of the 2015 Dietary Guidelines Advisory Committee – 4 March 2015
Note: The 2015 Dietary Guidelines Advisory Committee (Committee) submitted the Scientific Report of the 2015 Dietary Guidelines Advisory Committee (Advisory Report) to the Secretaries of the U.S. Department of Health and Human Services (HHS) and the U.S. Department of Agriculture (USDA) in February 2015. The purpose of the Advisory Report is to inform the Federal government of current scientific evidence on topics related to diet, nutrition, and health. It provides the Federal government with a foundation for developing national nutrition policy. However, the Advisory Report is not the Dietary Guidelines for Americans policy or a draft of the policy. The Federal government will determine how it will use the information in the Advisory Report as the government develops the 2015 version of the Dietary Guidelines for Americans. HHS and USDA will jointly release the Dietary Guidelines for Americans, 2015 later this year.
Sections of the Advisory Committee report related to alcohol are copied in the full Forum critique, which is available at www.bu.edu/alcohol-forum/critique-158. The full Advisory Committee report can be assessed at the following address: http://www.health.gov/dietaryguidelines/2015-scientific-report/PDFs/Scientific-Report-of-the-2015-Dietary-Guidelines-Advisory-Committee.pdf.
Forum Comments
Members of the International Scientific Forum on Alcohol Research (the Forum) have reviewed the sections of the Advisory Committee’s report that relate to the consumption of alcohol. They consider the report to be well written and a very clear statement on alcohol and health, one that generally reflects current scientific data.
Some Forum members thought that for dietary guidelines, there should have been more emphasis on the inclusion of moderate alcohol consumption as part of a Mediterranean-type diet, which is described in the report as being associated with very favorable health outcomes. The Forum found it interesting that the health problems associated with alcohol receive extensive detailed notice, but substantial favorable effects are barely mentioned. For example, while the comments on the increase in the risk of breast cancer are warranted, there is no mention that moderate alcohol consumption provides substantial protection against ischemic cardiovascular events, despite consistent and extensive data showing that the latter issue has a major public health benefit. Also, lacking any explanatory statements, the public and health professionals may be confused as to the basis for the recommendation that alcohol is “an important component of a healthy lifestyle.” So we recommend that some explanations for the statement, based on the relevant scientific literature, should be included. (Further, the report does not describe the favorable effects of moderate drinking on sociability, stress reduction, and relaxation, which are key reasons why most people consume alcohol in the first place.)
Despite our concerns, given that this is a statement that must get approval by a large number of governmental agencies and a variety of interested parties, it is consistent with current epidemiological data as well as mechanistic studies. The Forum strongly agrees that current scientific evidence indicates that, for mature adults without contraindications to alcohol use, moderate alcohol consumption can be included as a component of a balanced and healthy lifestyle.
For the full critique of the report by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 157: A mistaken interpretation of data relating alcohol to mortality – 20 February 2015
The authors of this paper have carried out a regression analysis to examine the association of reported alcohol consumption with all-cause mortality, dividing their sample into different age groups. They used data from Health Survey for England 1998-2008, linked to national mortality registration data. Their published results show lower risk of mortality (hazard ratios < 1.0 for mortality in comparison with recent non-drinkers and with never drinkers) for subjects in essentially all categories of moderate drinking. However, the authors have interpreted their analyses as indicating that moderate drinking is not associated with all-cause mortality for the vast majority of the population.
Forum members, and many other scientists, have been surprised by the conclusions of the authors, who apparently did not consider basic statistical principles (such as dealing with type-2 errors) in judging their results. The investigators appear to have looked only at p-values and ignored the estimates of effect in their own data, coming to the conclusion of no association between moderate alcohol and total mortality for most age groups. Focusing only on significance testing for estimating effects has been strongly condemned by epidemiologists and statisticians and can lead to inaccurate results.
The paper reflects a gross misinterpretation of the data, not what would be expected in a publication in a leading journal. In other words, the authors’ conclusions are not backed up by their data. A more appropriate headline based on this paper would be “Study supports a moderate protective effect of alcohol against all-cause mortality.” Given the wide media coverage of this article, with striking headlines indicating that moderate drinking does not affect mortality, one Forum reviewer wondered “How can more than 30 years of research in this field be undone by one misguided paper in the BMJ? Once in a while I reflect on how some doctors and journalists interpret scientific papers; they seem to rely more on abstracts and press releases.”
The Forum considers that the conclusions of the authors of this paper are simply not supported by the data provided. Rather, their findings are in accordance with those from previous prospective studies showing that, for all age groups, moderate alcohol consumption is associated with a decrease in all-cause mortality risk.
Reference: Knott CS, Coombs N, Stamatakis E, Biddulph JP. All cause mortality and the case for age specific alcohol consumption guidelines: pooled analyses of up to 10 population based cohorts. BMJ 2015;350:h384 doi: 10.1136/bmj.h384.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 156: The pattern of alcohol consumption and risk of cirrhosis — 10 February 2015
This paper, from a group of experienced investigators in Denmark using data from a large population-based cohort, attempted to judge how drinking pattern affects the risk of a subject developing alcoholic cirrhosis. From a cohort study of 55,917 participants (aged 50–64 years), the authors calculated hazard ratios (HRs) for alcoholic cirrhosis in relation to drinking frequency, lifetime alcohol amount, and beverage type. A total of 342 subjects developed alcoholic cirrhosis. The authors concluded that, in men, daily drinking was associated with an increased risk of alcoholic cirrhosis as compared with less frequent consumption; they also concluded that wine consumption might be associated with a lower risk of alcoholic cirrhosis that associated with the consumption of beer or liquor.
The major concern of Forum reviewers regarding this paper was the use of a diagnosis of “alcoholic cirrhosis” to judge the effects of alcohol on the disease; this was considered a type of circular reasoning. A diagnosis of alcoholic cirrhosis generally requires a history of alcoholism or heavy drinking, and subjects given that diagnosis would essentially be limited to those who were heavy drinkers. Thus, it would be no surprise to find a history of heavy drinking when evaluating alcohol as an exposure.
There was also concern about the implications of the author regarding frequency of drinking. The authors’ described in detail the relation of drinking pattern to liver cirrhosis, differentiating, in particular, effects associated with drinking daily versus drinking on 4-5, or 6 days a week. However, Forum members were concerned that as the overall average amount of alcohol for the daily drinkers exceeded that of those drinking less frequently, it was difficult to know if it was primarily the frequency of drinking (as concluded by the authors) or the total amount of alcohol consumed by subjects. The authors stated that they wanted to “execute evidence-based counselling,” which of course is praiseworthy, but Forum members had difficulty understanding why the effect of drinking 5-6 days/week should differ much from 7 days/week, especially if the usual amount was moderate. Indeed, the investigators state: “The mean alcohol amounts for daily drinkers were somewhat higher compared to those drinking less frequently in each category of alcohol amount, making it difficult to detangle the effect of drinking frequency and alcohol amount.” Forum members noted that the authors conclude that “daily drinking” was associated with increased cirrhosis, but they do not state daily drinking of how many drinks, which would be especially important. The study did not provide reliable data that would support alcohol-free days during the week.
The referent group in this study was made up of subjects reporting < 0 to 14 drinks/week, which would consist of light-to-moderate drinkers, those considered to be “sensible drinkers” in most cultures. Hence, it is no surprise that as subjects reported greater amounts of alcohol in the study, the risk of alcoholic cirrhosis increased. No one advises people to drink more than sensible limits. Further, there was a much higher risk of of cirrhosis among “current abstainers” than in the referent group, undoubtedly indicating that the current abstainers group included many former heavy drinkers.
Overall, the Forum thought that this paper raises, but does not answer, a number of questions about the relation of alcohol to the risk of cirrhosis: (1) Is wine really less liver-toxic than beer or liquor? (2) Should we really tell everyone to have one day each week without wine being included with their meal, or on which to avoid any alcohol? (3) Why is daily drinking, rather than 5 or 6 days per week dangerous for men but tends to be even slightly protective in women regarding liver disease? Because of concerns due to problems with bias from the diagnostic approach, the probability of under-reporting of alcohol consumption, and the lack of biological plausibility, we will need further scientific data to answer these important questions.
Reference: Askgaard G, Grønbæk M, Kjær MS, Tjønneland A, Tolstrup JS. Alcohol drinking pattern and risk of alcoholic liver cirrhosis: A prospective cohort study. Pre-publication. J Hepatol (2015) http://dx.doi.org/10.1016/j.jhep.2014.12.005.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 155: The effects of alcohol consumption on the risk of developing heart failure — 27 January 2015
An analysis of data from the large Atherosclerosis Risk in Communities (ARIC) study evaluated the effects of alcohol consumption at baseline, and the cumulative average intake based on several later assessments during a 24 year follow-up period, on the risk of the development of heart failure (HF). The authors conclude: “In this community, alcohol consumption of up to 7 drinks/week at early-middle age is associated with lower risk for future HF, with a similar but less definite association in women than in men. These findings suggest that despite the dangers of heavy drinking, modest alcohol consumption in early-middle age may be associated with a lower risk for HF.” The authors reported further that the risk of total mortality was higher than that of abstainers for former drinkers and for the heaviest drinkers, but did not demonstrate a “J-shaped” curve for total mortality (i.e., a lower risk for moderate drinkers in comparison with abstainers).
Forum members considered this to be a well-done analysis, with findings for a lower risk of HF among light-to-moderate drinkers consistent with many earlier reports. They noted that these findings may be somewhat affected by the inability of the investigators to include data on the pattern of alcohol consumption (regular moderate intake versus periodic binge drinking of similar total amounts) to disease. It would be expected that the relations between alcohol intake and HF (as well as with total mortality) would be stronger for regular moderate drinkers than for those who consumed their alcohol in binges (even if the total weekly average intake was the same). This could be one reason why a “J-shaped” curve was not seen for the relation of alcohol intake to total mortality in this study.
While coronary artery disease (CAD) is known to be a major precursor of HF, it is not clear from the data presented if the alcohol-HF relation may have differed between subjects with and those without CAD. For the effects of current heavy drinking, the implications from this study are limited because of the small number of such drinkers in this cohort; this was especially the case for women. The authors do not discuss the potential effects on their results of under-reporting of alcohol intake among their subjects; other studies have suggested means for identifying such subjects and ways of adjusting for such.
This study adds support to other large studies, including one just released as a pre-publication (see Addendum), that suggest that moderate alcohol consumption may reduce the risk of the development of heart failure. Some of this putative protective effect surely relates to a decrease in the risk of coronary artery disease among moderate drinkers. Heavy alcohol intake, especially among alcoholics, may increase the risk of both heart disease and heart failure.
Reference: Gonḉalves A, Claggett B, Jhund PS, Rosamond W, Deswal A, Aguilar D, Shah AM, Cheng S, Solomon SD. Alcohol consumption and risk of heart failure: the Atherosclerosis Risk in Communities Study. European Heart Journal, 2015, pre-publication; doi:10.1093/eurheartj/ehu514.
Addendum
Following the preparation of this critique, the pre-publication version of another paper has appeared: Larsson SC, Orsini N, Wolk A. Alcohol consumption and risk of heart failure: a dose–response meta‐analysis of prospective studies. European Journal of Heart Failure 2015; January, 2015. 10.1002/ejhf.228. According to its abstract, this paper is based on “a meta-analysis that included eight prospective studies, with a total of 202,378 participants and 6,211 cases of HF.”
While the Forum has not yet had an opportunity for a careful review of this new paper, the authors’ conclusions appear to provide strong support for the paper by Gonḉalves et al. The authors of the Larsson et al paper conclude their abstract by stating that when carrying out a dose-response meta-analysis, they “observed a non-linear relationship between alcohol consumption and risk of HF. Compared with non-drinkers, the RRs (95% CI) across levels of alcohol consumption were 0.90 (0.84–0.96) for 3 drinks/week, 0.83 (0.73–0.95) for 7 drinks/week, 0.84 (0.72–0.98) for 10 drinks/week, 0.90 (0.73–1.10) for 14 drinks/week, and 1.07 (0.77–1.48) for 21 drinks/week. Alcohol consumption in moderation is associated with a reduced risk of HF.”
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 154: Effects of changes in alcohol consumption on risk of dementia among elderly women — 12 January 2015
A number of prospective studies have shown that moderate drinkers are at lower risk of developing dementia or cognitive impairment than abstainers or heavy drinkers; possible mechanisms of a putative beneficial effect could relate to a reduction in the risk of cerebral atherosclerosis, a direct effect on cognition through the release of acetylcholine in the hippocampus, the antioxidant effects of alcohol and polyphenols, or from the down-regulation of inducible nitric synthase and up-regulation of endothelial nitric oxide synthase.
The present study is based on 1,309 women who were aged 65 years or greater at the beginning of a 20-year follow up, during which they had at least two assessments of cognitive function. At baseline, 42.1% of the women reported that they were “light” drinkers (>0 – < 3 drinks/week, 13.8% reported “moderate” consumption (3-7 drinks/week), and 3.6% reported “heavy” consumption (> 7 drinks/week). By the 20th year of follow up, 17.5% of the previously normal women had developed dementia (by several standard tests, a previous diagnosis of dementia, or nursing home residence), and 22.7% had developed mild cognitive impairment (MCI). Thus, a total of 40.2% of the women had developed some degree of cognitive impairment.
In this paper, there was no suggestion that the small percentage of women (5%) who increased their intake changed their risk of cognitive impairment (fully adjusted OR=1.04, 95% CI 0.56, 1.95), when compared with women who did not change their intake or decreased it only slightly. However, for women who decreased their intake by > 0.5 drinks/week, the authors suggest that there was an increase in risk of cognitive impairment, with unadjusted results showing an OR of 1.34, 95% CI: 1.05-1.70. However, with full adjustment for confounders, the effect was attenuated: OR = 1.26, 95% CI 0.98, 1.61; p = 0.07.
Forum members noted that the reasons that some women changed their drinking habits could not be ascertained (as is usually the case in observational studies). Alzheimer’s dementia has a long prodromal period and latent pathology could precede/contribute to a decrease in drinking. They were also concerned about the lack of cognitive characterization of the cohort at baseline. Thus, Forum members had some difficulty in knowing how to interpret the finding of a lack of association of baseline drinking with risk of cognitive impairment 20 years later given that we are not told whether the groups defined on baseline drinking differed from each other in age or other health risk factors. For those who changed their intake, decreasing drinking by > 0.5 glasses/week may be very different for someone drinking > 7 drinks/week than in someone drinking < 1 drink/week. It would have been better if the authors somehow took baseline drinking into account when assessing effects of change in drinking.
There was also the concern that any observational study that relates the effects of changes in alcohol intake on the risk of a disease without somehow taking earlier drinking into account may give paradoxical results. (An example is the relation of obesity to cardiovascular disease; overall, there is an increase in risk for obese individuals but when changes in intake among older people are evaluated, the result is often no effect or even a protective effect: the “obesity paradox.”) The same has been shown for the relation of usual alcohol intake and changes in intake to other diseases.
Thus, while the analyses were done appropriately, Forum members had concerns about whether the findings presented in this paper justify the wisdom of the authors in stating in their conclusion that “Women in their ninth and tenth decade of life who decrease alcohol use may be at risk of cognitive impairment.” As one reviewer stated: “Knowing from other studies that light to moderate alcohol consumption is good for the heart and the head, I would not advise elderly people to stop drinking. However, the conclusions of the authors that this paper shows that decreasing alcohol consumption increases the risk of cognitive impairment in elderly women may be true, but are not justified because the design, analysis, and results of the study do not permit such a statement.”
Reference: Hoang TD, Byers AL, Barnes DE, Yaffe K. Alcohol Consumption Patterns and Cognitive Impairment in Older Women. Am J Geriatr Psychiatry 2014; 22:1663-1667.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 153: Moderate alcohol intake may lower the risk of developing diabetes among obese subjects — 11 December 2014
This case-control study compared the risk of having a high level of hemoglobin A1c, a measure of hyperglycemia, and of the waist/height ratio, a measure of obesity, according to reported alcohol consumption. Overall, subjects reporting an average alcohol intake between 22 and 44 g/day (the equivalent of between about 2 and 4 typical drinks) had lower levels of hemoglobin A1c and lower weight/height values. The author concludes: “The associations between obesity and hyperglycemia were weaker in light-to-moderate drinkers than in nondrinkers. Thus, light-to-moderate drinking may reduce the impact of obesity on the risk for diabetes.”
While Forum reviewers had some concerns about the first analytic approach given in the paper, they agreed that the second approach, in which specific levels of A1c were reported according to alcohol intake and measures of obesity, had merit. These latter data clearly indicate that hyperglycemia is affected both by obesity (which increases the risk) and alcohol intake (which decreases the risk); hyperglycemia is the leading factor associated with the development of diabetes mellitus.
A therapeutic implication of this study may be that obese subjects who are moderate drinkers should not be advised to stop their alcohol consumption. The results, along with a large amount of other research currently available, also suggest that obese subjects who do not drink and have no contraindications to alcohol consumption should be informed that consuming moderate amounts of alcohol may be associated with a reduction in their risk of developing diabetes.
Reference: Wakabayashi U. Light-to-Moderate Alcohol Drinking Reduces the Impact of Obesity on the Risk of Diabetes Mellitus. J Stud Alcohol Drugs 2014;75:1032–1038.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 152: Specific genetic factors modify the reduction in heart disease risk from alcohol consumption — 27 November 2014
It has long been known that genetic and other environmental factors modify the association between alcohol consumption and a variety of diseases, especially coronary heart disease (CHD). Foremost among these modifying factors are genes that affect alcohol metabolism, age (effects seen only in older individuals), and drinking patterns (regular moderate versus binge drinking). Also, certain cholesteryl ester transfer protein (CETP TaqIB) polymorphisms, that relate to HDL-cholesterol activity, may interact with alcohol consumption for their effects on the risk of CHD. In the present study, the investigators have carried out a population-based case-control study among subjects in southwest Sweden to determine if there was an interaction between CETP genotypes and alcohol consumption for its effects on the risk of CHD. The authors conclude that a significant reduction in the risk of CHD from moderate drinking was seen only among the 18.6% of their subjects who had a particular CETP polymorphism.
Forum members considered this to be an interesting paper, but had some questions about the selection of cases, as they included not only new cases of CHD but subjects “who had an exacerbation of previously diagnosed coronary heart disease;” this makes it somewhat difficult to compare their results with other papers. Further, despite a large number of potential “control” subjects from their base population, the controls chosen were considerably younger than the cases and had different medical histories. While they adjusted for some of these factors in their analysis, residual confounding remains possible.
The major concern of Forum members was the broad conclusion of the authors (that only a small proportion of the population will show any cardio-protective effects of moderate drinking) based on such a small number of subjects. For example, among their “intermediate” category of drinkers with the supposedly “protective” CETP polymorphism, there were only 13 cases of CHD. Further, a number of previous large studies have had quite conflicting results regarding the effects of CETP polymorphisms on the alcohol-CHD association. While this paper adds information on one (of many) factors that affect the association between alcohol consumption and CHD, larger studies in different populations will be needed to determine the overall importance of this particular genetic polymorphism.
Reference: Mehlig K, Strandhagen E, Svensson P-A, Rosengren A, Torén K, Thelle DS, Lissner L. CETP TaqIB genotype modifies the association between alcohol and coronary heart disease: The INTERGENE case-control study. Alcohol 2014;48:695e700.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 151: “Fetal alcohol syndromes” result from multiple maternal factors during pregnancy — 20 November 2014
Excessive maternal alcohol consumption during pregnancy (especially among women with alcohol dependency) is known to markedly increase the risk of the fetus showing a group of developmental disorders defined as fetal alcohol spectrum syndrome (FASD), with the most serious form being fetal alcohol syndrome (FAS). The present paper attempts to identify maternal risk factors for FASD and FAS, but the authors report that there were not enough data to carry out a formal meta-analysis. They do, however, describe important maternal risk factors that have been reported in the literature to relate to these syndromes. The more frequent maternal conditions related to the risk of FASD or FAS include older age of mother, lower educational level, family relatives who abuse alcohol, little prenatal care, and a more severe pattern of alcohol consumption in general and particularly during pregnancy. They emphasize that “FAS is a multifactorial condition, and it is potentiated by complex relationships among several factors, social and biological.”
Forum reviewers considered this to be a well-done analysis presenting important and balanced information on these syndromes. Forum members agreed that many genetic and environmental factors, in addition to heavy alcohol consumption, may contribute to the development of these syndromes (e.g., certain genetic polymorphisms, inadequate pre-natal care, poverty, low education, familial alcoholism, use of illicit drugs, etc.).
Given the permanent nature of many of the defects found in FASD and FAS, and limited therapeutic options, it is important that the focus should be on the prevention of these syndromes. If they are to be prevented, it will be necessary to intervene among high-risk women, either prior to or early during pregnancy. Better knowledge of all the factors involved will help facilitate interventions that may help prevent these serious conditions.
Reference: Esper LH, Furtado EF. Identifying maternal risk factors associated with Fetal Alcohol Spectrum Disorders: a systematic review. Eur Child Adolesc Psychiatry (2014) 23:877–889; DOI 10.1007/s00787-014-0603-2.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 150: A new meta-analysis on the relation of alcohol consumption to the risk of ischemic heart disease — 6 November 2014
This meta-analysis is from authors who in the past have tended to argue that the demonstrated inverse association between moderate alcohol consumption and ischemic heart disease (IHD) shown in most studies is due to confounding by other lifestyle factors. However, in this paper, they come to the conclusion (in their words): “Results from our quantitative meta-analysis showed that drinkers with average intake of < 30 g/day and no episodic heavy drinking had the lowest IHD risk (relative risk = 0.64, 95% confidence interval 0.53 to 0.71). Drinkers with episodic heavy drinking occasions had a risk similar to lifetime abstainers (relative risk = 1.12, 95% confidence interval 0.91 to 1.37).”
The conclusions of the authors thus not only support a “J-shaped” curve for alcohol consumption and IHD but provide additional support suggesting that the effect may be causal, i.e., related to the alcohol consumption and not to other associated lifestyle factors. They state: “For drinkers having one to two drinks per drinking day without episodic heavy drinking, there is substantial and consistent evidence from epidemiological and short-term experimental studies for a beneficial association with IHD risk when compared to lifetime abstainers. The alcohol-IHD relationship fulfills all criteria for a causal association proposed by Hill.”
It is clear from epidemiologic studies that moderate drinkers may exhibit moderation in other lifestyle factors (such as not smoking, eating a healthy diet, etc.). Indeed, there is aggregation of healthy lifestyle factors that must be considered when judging how a single factor (such as moderate drinking) relates to disease outcomes. This meta-analysis suggests that other lifestyle factors do not explain the lower risk of IHD found to occur among moderate drinkers. In fact, increasingly, moderate drinking is found to be an independent (and rather important) lifestyle factor that lowers the risk of cardiovascular disease, regardless of other factors. Such protection is not seen when drinking is more than moderate, defined in this paper as an average of 30 grams or more of alcohol per day, the equivalent of about 2 ½ to 3 typical drinks.
Reference: Roerecke M, Rehm J. Alcohol consumption, drinking patterns, and ischemic heart disease: a narrative review of meta-analyses and a systematic review and meta-analysis of the impact of heavy drinking occasions on risk for moderate drinkers. BMC Medicine 2014;12:182.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 149: The association of alcohol consumption with the risk of death from colorectal cancer — 28 October 2014
Data from prospective cohort studies on the association between alcohol consumption and the occurrence of colorectal cancer (CRC) are conflicting, with some suggesting an increase in risk while others failing to show such an effect. There are little data on the effects of alcohol consumption on the risk of mortality from CRC. The present study is based on a meta-analysis of data from nine cohort studies (with a total of more than two million subjects) to judge how the level of alcohol intake relates to CRC mortality. A total of almost 4,000 deaths from CRC were recorded. The conclusions of the authors are that the consumption of ≥ 50 grams of alcohol (about 4 typical drinks or more) per day increases the risk of death from CRC modestly [RR 1.21 (95% CI 1.01, 1.46)], but “light” drinking (≤ 12.5 g/day) or “moderate” drinking (12.6-49.9 g/day) do not increase the risk of CRC death. In fact, they state that their data support a “J-shaped” relation between alcohol intake and CRC mortality (i.e., a slight decrease in mortality associated with light drinking but an increased risk with heavier drinking).
Forum members considered this to be a well-done analysis. They noted the inability of the authors to evaluate differences in effect according to type of beverage consumed, the pattern of drinking, or the underlying folate levels of subject, all of which probably modify such a relation. The results are in line with earlier reports on alcohol and breast cancer, where alcohol appears to increase the incidence of the disease but does not increase mortality. For most diseases, including colorectal cancer, there may a J-shaped effect on mortality: a reduction in risk for light-to-moderate drinking but an increase with heavier drinking.
Overall, the present meta-analysis supports a finding of increased risk of death from colorectal cancer from heavy drinking. However, it shows rather convincingly that light to moderate amounts of alcohol do not increase the risk of death from this disease, probably because of the protective effects of moderate drinking on cardiovascular disease, a more common cause of mortality.
Reference: Cai S, Li Y, Ding Y, Chen K, Jin M. Alcohol drinking and the risk of colorectal cancer death: a meta-analysis. European Journal of Cancer Prevention 2014;23:532–539.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 148: Alcohol and liver cancer — 24 September 2014
Hepatic cirrhosis frequently precedes the development of liver cancer, and excessive alcohol consumption is known to be one cause of cirrhosis. The investigators in the present study carried out a meta-analysis to evaluate the association of alcohol consumption with liver cancer. They used data from 19 prospectively studied cohorts with a large total number of cases: 4,445 incident cases and 5,550 deaths from liver cancer.
The analysis from this large study indicates that liver cancer is related to heavier alcohol intake, but not to light-to-moderate drinking (with the latter defined in this study as < 3 typical drinks per day). The authors conclude: “This systematic review suggests a moderate detrimental role of consumption of 3 or more alcoholic drinks per day on liver cancer, and a lack of association with moderate drinking.”
Forum reviewers considered this to be a well-done analysis with appropriate statistical methodology. While the authors were unable to test the potential effects of pattern of drinking (regular moderate versus binge drinking), the type of beverage (wine or other beverages), or potential effects of obesity (with the latter being a key factor associated with the most common type of liver disease in the US, non-alcoholic fatty liver disease), the results of this study support most other research indicating that more than moderate drinking increases the risk of cirrhosis and liver cancer. However, the findings of no effect from what the authors considered “moderate” drinking (< 3 drinks/day, which exceeds the guidelines for most countries), also fits with another recent meta-analysis showing no increase in risk of liver cancer to be associated with light drinking.
There are many adverse health effects of heavy alcohol consumption. Liver cirrhosis, which frequently precedes the development of liver cancer, is one such potential outcome. On the other hand, this study suggests that moderate alcohol intake does not increase the risk of liver cancer.
Reference: F. Turati, C. Galeone, M. Rota, C. Pelucchi, E. Negri, V. Bagnardi, G. Corrao, P. Boffetta, C. La Vecchia. Alcohol and liver cancer: a systematic review and meta-analysis of prospective studies. Annals of Oncology 2014; advance publication; doi:10.1093/annonc/mdu020
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 147: Association of alcohol intake with different types of breast cancer — 11 September 2014
The present study was based on a large number of women participating in a clinical trial (enhanced screening for certain cancers versus routine care) focusing on prostate, lung, colorectal, and ovarian cancer. During a follow-up period averaging about 9 years, a total of 1,905 women were diagnosed with invasive breast cancer. The analyses showed that an increase in cancer risk was associated with alcohol intake for estrogen and progestin positive (ER+/PR+) tumors, but not for other histologic types of breast cancer. The increased risk was predominantly seen among PR+ cancers, as there was no evidence of an increase in risk from alcohol for women with ER+/PR- tumors. An association with the highest category of alcohol intake was noted for ductal (the most prominent type), lobular, and mixed ductal/lobular tumors, but a clear dose-response curve was not present. The authors conclude that alcohol consumption is not associated with all breast cancer subtypes, and that future research should include precise definition of subtypes of cancer.
Forum reviewers considered this to be a well-done analysis. There were some questions about the characteristics of the participants in the study that could affect generalizability of the results. For example, the cohort of women in this study were more highly educated, more likely to have a positive family history of breast cancer, to be smokers, and perhaps more obese that the general population. Of more concern, however, was the lack of ability to evaluate a number of other potential risk factors for breast cancer: folate levels and other dietary factors, the pattern of drinking (regular versus binge), potential changes in drinking after the baseline measurement, type of beverage, or the HER2 status of tumors. The finding in the paper of an increase in breast cancer risk, in comparison with non-drinkers, even for women reporting less than ½ drink per week (RR 1.15, CI 0.97, 1.39) and 0.5 – < 1 drink per week (RR 1.25, CI 1.03, 1.53), suggests that residual confounding must also be considered; it is unlikely that such small amounts of alcohol would have a physiological effect.
Overall, the present study shows a significant increase in the risk of breast cancer among women in a cancer prevention trial who, at baseline, indicated that they were consuming even less than 1 drink/week. The increase was exclusively in ER+/PR+ tumors, but not in ER+/PR- or ER-/PR- tumors.
In future research on this association, information on folate levels and drinking pattern, and especially on type of beverage consumed and on evidence of under-reporting of alcohol intake, will be important in better defining how alcohol consumption relates to the risk of breast cancer. While the results of this study are important in studying the etiology of breast cancer (as alcohol appears to relate only to hormone receptor positive tumors), the findings may not necessarily help individual women know how their alcohol consumption by itself may relate to their overall risk of the disease.
Reference: Falk RT, Maas P, Schairer C, Chatterjee N, Mabie JE, Cunningham C, Buys SS, Isaacs C, Ziegler RG. Alcohol and Risk of Breast Cancer in Postmenopausal Women: An Analysis of Etiological Heterogeneity by Multiple Tumor Characteristics. Am J Epidemiol 2014; advance access; DOI: 10.1093/aje/kwu189.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 146: Alcohol and the risk of abdominal aortic aneurysm — 4 September 2014
The large majority of prospective epidemiologic studies on the effects of alcohol consumption and the risk of coronary heart disease and stroke have shown a significant reduction in risk for moderate drinkers. There have been few studies relating alcohol intake to the development of abdominal aortic aneurysm (AAA), and results have been inconsistent. The present study is based on two very large population-based cohorts in Sweden that were followed prospectively for the clinical development of AAA (identified by radiography, surgical repair, or death resulting from rupture). There were more than 1,200 cases identified during a 14-year follow-up period. The results of this study suggest that moderate drinking is associated with a lower risk of AAA, with the beneficial effects primarily among consumers of beer or wine.
Forum reviewers were unanimous in considering this to be a well-done analysis, with unbiased estimates of effect of alcohol on the risk of aneurysm. The reduced risk of AAA among moderate drinkers was similar to that seen for common manifestations of atherosclerosis, especially coronary heart disease and ischemic stroke. Reviewers were uncertain why only consumers of wine and beer showed a beneficial effect, but not consumers of spirits: this could be explained by the polyphenols present in wine and beer that have been shown to be anti-inflammatory, anti-oxidant, and anti-platelet aggregation (all mechanisms that may relate to the development of AAA). However, residual confounding could also play a role.
It was noted that the percentage of the population with hypertension, probably the most important risk factor for AAA, was much lower than is common in most industrialized countries, but the degree to which this affected the results cannot be known. While alcohol is known to increase blood pressure, some large studies suggest that an increase occurs only with more than light-to-moderate drinking. Further, there were few very heavy drinkers (the highest category of alcohol was an average consumption of ≥1 drink/day among women and ≥2 drinks/day among men), so this study could not assess whether or not large amounts of alcohol might increase risk of AAA.
There have been a very limited number of studies on alcohol intake and aortic aneurysm. While this study suggests a slight decrease in occurrence of AAA with moderate wine and beer intake, it will be important for other large studies to evaluate this association. Additional studies on polyphenol intake and occurrence of AAA will also be useful.
Reference: Stackelberg O, Björck M, Larsson SC, Orsini N, Wolk A. Alcohol Consumption, Specific Alcoholic Beverages, and Abdominal Aortic Aneurysm. Circulation 2014;130:646-652.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 145: Alcohol consumption and brain structure on MRI scans — 25 August 2014
While numerous prospective epidemiologic studies have provided evidence that light-to-moderate amounts of alcohol reduce the risk of dementia and heavy drinking increases the risk, there are few studies on the effects of alcohol on brain structure assessed by magnetic resonance imaging (MRI). The present study is a cross-sectional evaluation between reported alcohol intake and MRI-assessed brain structure among 589 multi-ethnic community residents of New York. Total brain volume (TBV), white matter hyperintensity volume (WMHV), and presence of infarcts were derived from MRI scans when subjects were, on average, 80 years of age..
A key finding of this analysis is that, in comparison with non-drinkers, light-to-moderate alcohol intake (up to an average of 1 drink/day for women or 2 drinks/day for men, which was reported in 31% of their subjects) was associated with larger TBV (i.e., less brain atrophy). The effect was primarily among consumers of wine rather than of beer or liquor. Significant associations were not found for alcohol or for specific beverages for other measures of brain structure (WMHV or presence of infarcts).
Forum reviewers considered this to be an appropriate analysis that was able to consider many of the potential confounders of such an association. On the other hand, it was not a large study and was based on a cross-sectional analysis; thus it cannot be used to judge causation (e.g., it is possible that people with larger brains to begin with were more likely to consume wine or total alcohol, rather than their alcohol intake increasing their brain size).
Data from many previous studies have shown that moderate alcohol intake lowers the risk of developing clinical signs of cognitive decline and of dementia. Such a finding has led Forum members to be of the opinion that instructing the elderly to refrain from light-to-moderate amounts of alcohol may not be wise. Although prospective studies may show that the decrease in the risk ratio for dementia (comparing drinking with abstainers) tends to be less among the elderly than among middle-aged subjects, the absolute risk of dementia increases markedly with age. Thus, any intervention that lowers the risk of cognitive impairment will have a much greater impact in older people as compared with younger people.
Given the inconsistences in previous reports on the effects of alcohol on brain structure, we must conclude that while this study suggests that there might be a beneficial association between alcohol (especially wine intake) and brain size, such a relation is not definitive. An inverse relation between moderate drinking and clinical evidence of dementia, however, has received support from a large number of prospective epidemiologic studies; it may be a better association for us to use when advising the elderly regarding alcohol consumption.
Overall, scientific data indicate that, for elderly subjects without contraindications to alcohol, small amounts of wine or other alcoholic beverage consumed regularly may reduce the risk of dementia and other diseases of ageing. As stated by Michel de Montaigne many centuries ago: “ . . . drinking is the almost last pleasure that the years steal from us.”
Reference: Gu Y, Scarmeas N, Eaton Short E, Luchsinger JA, DeCarli C, Stern Y, Manly JJ, Schupf N, Mayeux R, Brickman AM. Alcohol intake and brain structure in a multiethnic elderly cohort. Clinical Nutrition 2014;33:662e667.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 144: Alcohol consumption and risk of endometrial cancer — 18 August 2014
Most epidemiologic studies have shown that moderate alcohol consumption does not increase the risk of uterine cancer, and some have suggested an inverse or J-shaped relation. In a new analysis from the Nurses’ Health Study, with 68,067 female participants aged 34–59 years in 1980, investigators have related repeatedly assessed long-term alcohol intake, and related the cumulative average intake over time to the risk of invasive uterine cancer. A total of 794 cases of invasive endometrial adenocarcinoma were identified over a 30 year follow-up period.
The authors report an inverse association among alcohol drinkers (multivariable RR=0.81; 95% CI: 0.68–0.96) compared with nondrinkers. Women with an intake of <5 g per day (an average of approximately one-half drink per day) had a 22% lower risk of endometrial cancer (multivariable RR=0.78; 95% CI: 0.66–0.94), with no further decrease evident from larger amounts of alcohol. In comparison with non-drinkers, the relative risk was similarly reduced for consumers of more than 30 grams of alcohol per day, but the number of subjects in this category was small, and a potential increase in risk from heavy drinking could not be adequately assessed in this study.
Forum members considered this to be a very well-done prospective study, with clear and biologically plausible results. By having repeated assessments of alcohol, an estimate of long-term average consumption was possible. The approximately 20% lower risk of uterine cancer among subjects with light alcohol intake remained statistically significant after multivariate adjustments for known potential confounders. Reviewers agreed with the authors that a potential mechanism for the association could be a reduction in insulin concentrations and improved insulin sensitivity that have been shown to occur with moderate alcohol consumption. Further, the frequently demonstrated inverse relation for alcohol with obesity may also play a mechanistic role. Overall, this study adds to accumulating scientific data showing that moderate drinking does not increase the risk of uterine cancer, and probably is associated with a reduction in risk
Reference: Je Y, DeVivo I, Giovannucci E. Long-term alcohol intake and risk of endometrial cancer in the Nurses’ Health Study, 1980–2010. British Journal of Cancer 2014;111:186–194; doi: 10.1038/bjc.2014.257.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 143: A Mendelian randomization assessment of alcohol and cardiovascular disease — 20 July 2014
Using a very large dataset from subjects of European descent, the authors have carried out a Mendelian randomization analysis to estimate the effects of alcohol consumption on cardiovascular disease (CVD), using as the instrumental variable an uncommon allele affecting alcohol metabolism, the ADH1B rs1229984 variant. People with this variant are unusually sensitive to alcohol (developing flushing and other uncomfortable symptoms from alcohol) and it has been well demonstrated that they are less likely than people without this variant to consume alcohol, and are unlikely to be heavy drinkers. The authors conclude that since the 7% of their subjects with the uncommon allele had less cardiovascular disease, this indicates that alcohol consumption is unrelated to CVD.
Forum members agree that the analyses were done correctly, but strongly disagree with the premise of the study and the conclusions of the authors, and consider the genetic factor chosen as inappropriate to use as the instrumental variable in Mendelian randomization. The gene studied explains only a fraction of alcohol consumption in the population (not stated in the paper) and it may have effects on CVD beyond those explained by alcohol consumption. Thus, this ADH1b allele violates the assumptions required for a variable for Mendelian randomization and would be inappropriate for judging the effects of alcohol on CVD. Further, in the present study, the authors report little relation of their estimate of alcohol consumption with HDL-cholesterol, while essentially all observational studies, clinical trials, and experimental studies have shown that alcohol is an important determinant of HDL. This further suggests that the use of the ADH1B allele provides an inadequate estimate of alcohol consumption.
Even without the weakness of the allele chosen to reflect alcohol effects, conclusions derived from Mendelian randomization in general are heavily dependent on the assumption that the instrumental chosen is appropriate, of which you can rarely be confident. Forum reviewers consider this method to be a very blunt instrument and subject to considerable bias for variables that are weakly correlated with exposure and not true instruments.
Some reviewers were concerned by the conclusion of the authors that this Mendelian randomization paper shows that all persons should drink less; this does not necessarily mean for people to completely avoid drinking. The protection of moderate drinking against CVD that is generally observed shows a non-linear gradient: it is better manifested at a low alcohol consumption, while it is less strong as the consumption levels rise above optimum and finally disappears and is transformed into harm with heavy alcohol consumption. This would be in agreement with the conclusions of most prospective studies and meta-analyses that drinking alcohol at low doses offers the best protection against CVD, as there is a J-shaped curve.
Reference: Holmes MV, Dale CE, Zuccolo L, et al (a total of 155 authors). Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. BMJ 2014;349:g4164 doi: 10.1136/bmj.g4164.
For the full critique of this study by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 142: A large study of alcohol consumption and mortality — 14 July 2014
The large European Prospective Investigation into Cancer and Nutrition Study (EPIC) has released a new analysis of the relation of alcohol consumption to mortality. The study concluded that alcohol use was positively associated with overall mortality, alcohol-related cancers, and violent death and injuries, but marginally to cardiovascular disease, and that absolute risks of death observed in EPIC suggest that alcohol is an important determinant of total mortality.
There is no question that heavy alcohol consumption, especially when associated with smoking, increases the risk of a number of upper aero-digestive cancers that are commonly referred to as “alcohol-related cancers.” In the present study, the authors have also included in this group a number of other cancers that may be related less directly to the effects of alcohol; these include colorectal cancer and female breast cancer which, because they are so much more common, make up the large majority of cancers “related to alcohol.” Forum members consider the EPIC study to be an important source of data on cancer, but had a number of questions about the analysis and especially about the conclusions of the authors.
Major weaknesses of the study are that an assessment of alcohol intake was obtained only at a baseline visit, with no further assessments during a follow-up period averaging 12 years, and especially, no information was available on the pattern of drinking of subjects (e.g., regular moderate versus binge drinking). Further, Forum members noted that there was no discussion of the effects of under-reporting of alcohol, which has been shown to markedly affect health effects of alcohol intake in epidemiologic studies. In fact, recent large studies show that most of the cases of cancer that appear to relate to “light-to-moderate drinking” actually relate to underreporting of consumption by subjects who are found, from other collected medical data, to be heavy users or abusers of alcohol.
The authors focus on “extreme drinkers,” which consist of women who consume (≥30 g/day) or men who consume ≥60 g/day. They do not point out that only 2.4% of the women in this study consumed at this level, and little attention is given to the fact that almost all of the women were non-drinkers or light-moderate drinkers. From the data presented in the paper, there is a clear U-shaped curve among women: the highest risks for total mortality were in the abstainers (a 26% increase over the referent group of light drinkers) and the very small number of women in the highest drinking category (a 27% increase).
For men, 8.2% were in the highest drinking category, reporting an average consumption of ≥ 60 g/d (5 – 6 typical drinks). For men, there was generally a U-shaped curve, with lower death rates for light to moderate drinkers. However, the heaviest drinkers had the highest risk of death for overall mortality and for deaths from cancers and other causes of death. For both men and women, at every level of drinking, smokers had an increased risk of death in comparison with non-smokers.
Some reviewers were also concerned about the unusual categorization of alcohol intake used in the study. Referring to subjects reporting 0.1 – 4.9 g/day as “moderate drinkers” is a strange designation for an alcohol intake that in most other studies would be named as light or very modest, and may lead to confusion in interpreting results. (Most studies would define 5 – 14.9 g/day as light to moderate drinkers, and this group is not given a name in this study).
Overall, this study tends to show a U-shaped relation between alcohol consumption and mortality. The data presented focus primarily on the highest categories of drinking, levels that are well known to relate to many diseases and mortality. For truly light-to-moderate consumption, however, there is overwhelming epidemiologic data that such drinking relates to lower mortality risks, and the present study does not contradict such an association.
Reference: Ferrari P, Licaj I, Muller DC, et al (36 other authors). Lifetime alcohol use and overall and cause-specific mortality in the European Prospective Investigation into Cancer and nutrition (EPIC) study. Pre-publication; BMJ Open 2014;4:e005245. doi:10.1136/bmjopen-2014-005245
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 141: A world-wide study of alcohol consumption and the risk of myocardial infarction — 3 July 2014
The authors report on data collected in the INTERHEART Study, a large international collaborative project of individuals with a first myocardial infarction (MI) and age- and sex-matched controls from 52 countries in Asia, Europe, the Middle East, Africa, Australia, North and South America. Included were nations with very divergent lifestyles, religions, degrees of development, and drinking habits. The authors attempted to provide a “world-wide” overview of the relation of alcohol consumption to the risk of myocardial infarction (MI). However, they were forced to use a case-control design, a type of study with many opportunities for bias and one that prevents determination of a causal relation. Further, the lack of detailed data on the amount of alcohol consumed by individuals weakens their results.
While the authors state that their study shows that low levels of alcohol use are associated with a moderate reduction in the risk of MI, they point out differences in results in different countries. Forum members considered that these large differences severely limit their ability to use such a dataset to provide overall conclusions on alcohol and MI. For example, only 1% of the non-drinkers in this study came from W. Europe and 1% from North America, while more than 70% of the non-drinkers came from the Middle East or Asia. With such diversity (e.g., almost all the abstainers were from one area), it is not possible to adequately “adjust” for such regional differences in analysis.
The authors also studied how alcohol consumption shortly prior to (in the 24 hours before) the occurrence of a MI relate to the short-term risk of MI. While their results show an increased risk for heavy drinking immediately prior to an MI (a result that differs from that of some previous studies), they admit analytic problems, stating: “Thus there remains uncertainty over the risk of MI in the period immediately following alcohol intake.”
Previous large prospective cohort studies (a type of epidemiologic study that decreases the risk of recall bias regarding alcohol intake and certain types of confounding) have clearly shown an inverse relation between moderate alcohol consumption and MI. Most of the previous studies have provided much more detailed data on alcohol exposure than did the present study. The authors realized many of these problems, and warn against using their results to make overall conclusions about the association between alcohol and MI from their paper. They state: “The associations observed between alcohol use and MI may be accounted for by unmeasured confounders such as genetic differences between populations, variation in alcohol type or preparation, and heterogeneity of social context. The present analysis should therefore prompt further research to clarify the nature of the association between alcohol use and MI.” Unfortunately, the conclusions presented in the abstract and in the do not mention such problems.
Some Forum members worried that many readers of the paper will be left with a very misleading impression of the relation of alcohol consumption to myocardial infarction, and will not be aware that the conclusions trumpeted in the abstract are compromised by weak data. Overall, members considered that the present paper adds little to our knowledge about the risks and benefits of alcohol in relation to cardiovascular disease.
Reference: Leong DP, Smyth A. Teo KK, McKee M, Rangarajan S, Pais P, Liu L, Yusuf S, on behalf of the INTERHEART investigators. Patterns of Alcohol Consumption and Myocardial Infarction Risk: Observations from 52 Countries in the INTERHEART Case-Control Study. Circulation 2014 (pre-publication) DOI: 10.1161/CIRCULATIONAHA.113.007627.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 140: A meta-analysis shows that light alcohol consumption is associated with a reduced risk of stroke, while heavier drinking may increase risk — 5 June 2014
Most epidemiologic studies have shown a reduction in the risk of ischemic stroke (and total stroke, as ischemic stroke is by far the most common type in western countries) to be associated with light to moderate alcohol consumption. The present study, a meta-analysis, was based on 27 prospective studies; the authors categorized a reported intake of <15 g/day as light consumption, and 15-30 g/day as moderate consumption. The authors point out differences (greater smoking, larger amounts of alcohol) between Chinese subjects and those from other countries, which may explain some of the differences shown between alcohol’s effects in the different countries. They also point out that they had no data on the pattern of drinking (regular, moderate intake versus binge-drinking) or on the type of alcoholic beverage consumed.
The key results of the study are a significant 15% reduction in total stroke for low alcohol intake, no effect for moderate, and a 20% increased risk for heavy alcohol consumption (RR 1.20, 95% CI 1.01, 1.43). Analyses were also done according to type of stroke: for ischemic stroke and stroke mortality there were decreases for low alcohol intake, but no significant effects of either moderate or heavy intake. For hemorrhagic stroke, the RR for subjects reporting heavy alcohol intake was higher than that of abstainers, but none of the differences between drinkers and non-drinkers was statistically significant.
This meta-analysis supports previous findings of a decrease in the risk of most strokes with light drinking and possibly an increase in the risk for heavy drinking. Forum members generally agreed with the conclusions of the authors: “Low alcohol intake is associated with a reduced risk of stroke morbidity and mortality, whereas heavy alcohol intake is associated with an increased risk of total stroke. The association between alcohol intake and stroke morbidity and mortality is J-shaped. An alcohol intake of 0-20 grams/day is associated with decreased rates of stroke morbidity and mortality.”
Reference: Zhang C, Qin Y-Y,Chen Q, Jiang H, Chen X-Z, Xu C-L, Mao P-J, He J, Zhou Y-H. Alcohol intake and risk of stroke: A dose–response meta-analysis of prospective studies. Int J Cardiol 2014; pre-publication; http://dx.doi.org/10.1016/j.ijcard.2014.04.225.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 139: Does adjustment for stress levels explain the protective effect of moderate drinking on the risk of mortality? — 18 May 2014
An inverse association between moderate alcohol consumption and total mortality has been reported in most prospective epidemiologic studies, even after adjustments for all known potential confounders. The present analysis was carried out specifically to focus on the effects of psychosocial stressors on the association, using a large population-based German cohort from the WHO MONICA study. No alcohol intake was reported by 15.3% of males and 41.8% of females; “moderate drinking” was defined as an average intake of 0.1-39.9 g/day for men (making up 51.1% of the cohort) and 0.1 – 19.9 g/day for women (38.8% of the cohort). Although data are not presented, there were apparently few women in the higher drinking categories.
The authors related the effects of including, or not including, in their equations a large number of psychosocial stressors, including educational level, occupational status, several indices of social support, job strain symptoms, depressive symptoms, somatic symptoms, and self-perceived health status, in the estimation of the effects of alcohol consumption on risk of total mortality over an average follow-up period of 12 years. In their analyses, there was little effect on risk estimates for mortality when these factors were added to the multi-variable analysis. The authors conclude: “The observed protective effect of moderate drinking could not be attributed to misclassification or confounding by psychosocial stressors.”
The authors have demonstrated among men a “U-shaped” curve, with the risk for moderate drinkers being 25-30% lower than that of both non-drinkers and heavier drinkers. For women, there was a lower estimated mortality risk ratio for all drinkers than for non-drinkers, although the confidence intervals included 1.0 in all categories (perhaps, as the authors state, there were few women in their higher categories of alcohol intake).
Forum reviewers thought that this was a well-done analysis of a large population-based population. It did not support the hypothesis that social support, job strain, depressive symptoms, and other such psychosocial factors have a strong influence on the demonstrated inverse relation between moderate alcohol consumption and total mortality. Thus, this study provides additional evidence that the observed reduction in total mortality seen among moderate drinkers is not due to confounding by other lifestyle factors, including psychosocial stressors.
Reference: Ruf E, Baumert J, Meisinger C, Döring A, Ladwig K-H, and for the MONICA/KORA Investigators. Are psychosocial stressors associated with the relationship of alcohol consumption and all-cause mortality? BMC Public Health 2014, 14:312. http://www.biomedcentral.com/1471-2458/14/312.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 138: Underreporting of alcohol intake affects the relation of alcohol to the risk of cancer — 23 April 2014
Epidemiologists are often faced with reported adverse health effects of alcohol among subjects reporting very low levels of consumption, levels that physiologically should not cause diseases such as cancer. It is often assumed that at least some of the subjects reporting low levels of intake may be underreporting their actual intake, but heretofore it has been difficult to judge this.
In the present study, the authors used each subject’s computer-based data on conditions and diseases (including laboratory and social factors), related to alcohol misuse, collected over many years to identify subjects reporting “light-to-moderate” alcohol intake who were likely, or unlikely, to be underreporting their intake at a baseline examination. Overall, 18.4% of subjects were suspected of being underreporters while 46.5% had adequate data that suggested that they were not underreporters. (The remaining 35.1% of subjects had inadequate data stored in the computer to be classified.)
Among their cohort of more than 100,000 subjects, 14,880 developed cancer during an average follow-up period of 18 years. There were 23,363 subjects who reported that they were light (up to 1 drink/day) or moderate (1 to 2 drinks/day) drinkers. In all comparisons, subjects suspected of being underreporters of their alcohol intake had a higher risk of cancer than those not categorized as being underreporters. For example, among subjects reporting 1 to 2 drinks/day, in comparison with non-drinkers, the risk ratio of any type of cancer among those considered to not be underreporters was 0.98 (95% CI 0.87-1.09); in other words, no effect on cancer risk from alcohol. For those categorized underreporters, however, the relative risk of any cancer was 1.33 (95% CI 1.21–1.45). Similar results were seen for alcohol-related cancers as for any cancer. Also, the risk of breast cancer among women was less than one-half as high among moderate drinkers who were unlikely to be underreporters of their alcohol intake as among those considered likely to be underreporting their drinking.
Adjusting for confounding in prospective studies is an ever-present challenge for epidemiologists. One factor that has often been considered probable, but difficult to adjust for, is the underreporting of actual alcohol intake by subjects. Being able to adjust for such unerreporting would greatly improve studies relating alcohol consumption to the risk of cancer (and other chronic diseases). For epidemiologic studies that have extensive longitudinal data on all medical conditions (such as the Kaiser-Permanente Study, the basis for these analyses), the approach described in this paper could be an extremely valuable way of seeking the true relation between light-to-moderate alcohol intake and cancer as well as with a variety of other health outcomes. Based on the present study, an increase in the risk of cancer among light-to-moderate drinkers may occur primarily among those who underreport their alcohol intake.
Reference: Klatsky AL, Udaltsova N, Li Y, Baer D, Tran HN, Friedman GD. Moderate alcohol intake and cancer: the role of underreporting. Cancer Causes Control 2014; on-line publication; DOI 10.1007/s10552-014-0372-8 2014.
Potential Conflict of Interest: The first author of this paper, Dr. Klatsky, is a member of the International Scientific Forum on Alcohol Research. While he has not contributed to this critique, readers may wish to take this fact into account when interpreting the conclusions of the review.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 137: Alcohol intake prior to and during pregnancy and birth outcomes — 28 March 2014
The present analysis was carried out among 1,264 women from Leeds, UK, whose alcohol intake was estimated prior to and during pregnancy. The outcomes were birth weight of the infant and whether or not it was small for gestational age (SGA). In comparison with most previous research on this topic, this study is notable for being of a relatively small size. Further, it had a high percentage of women who consumed alcohol both prior to and during the first trimester, had a very low participation rate of eligible women (only 30%), failed to present estimated effects by ethnicity, and had some questions related to residual confounding. It is unclear how the results of this study increase our knowledge of maternal alcohol consumption and birth outcomes.
Forum members do not believe that the consumption of alcohol should be recommended for pregnant women. A certain percentage of newborns will be small for gestational age, have certain deformities, and have later emotional and behavioral abnormalities. If a woman has consumed any alcohol during the pregnancy, she (and perhaps even her doctor) may blame the abnormality on alcohol consumption, whether or not it had anything to do with it. Hence, the majority of Forum members agree that women should not be encouraged to consume alcohol during pregnancy.
Further, scientific data are very consistent on the potential risks of serious adverse health outcomes of the infant from heavy maternal drinking, especially among women who are alcoholics. Heavy-drinking women who become pregnant should be strongly urged to stop their drinking.
On the other hand, sound data indicating harmful effects on the fetus of light or occasional drinking by a pregnant woman are difficult to come by. Because of the epidemiologic concerns of the present paper, described in our Forum critique, we do not believe that this study adds materially to our understanding of the topic. The serious anxiety occurring among some women who may have ingested some alcohol prior to learning that they were pregnant seems, based on numerous studies, to generally be unnecessary; the need to abort a fetus because of previous light drinking by the mother cannot be justified.
There is a serious problem in interpreting all studies of prenatal alcohol exposure and the outcomes of pregnancy because of potential confounding, especially by ethnicity, education, smoking, coexisting use of illegal drugs, etc. Further, alcohol use by pregnant women has become an especially emotional and even a moral issue, and the entangled confounders make rational analysis most difficult. This means that there is a difficult challenge for epidemiologists and statisticians, as well as for public health officials and the general public, about how to interpret results of individual research projects. The literature can support varying views, from no alcohol at all for those who might soon be expectant mothers to being able to drink moderately throughout pregnancy.
Also, it should be pointed out that the potential health benefits of moderate alcohol consumption relate primarily to middle-aged and older people, so there is no reason for pregnant women to consume alcohol for its “health effects.” Thus, it is very reasonable that the majority of women choose to avoid alcohol during pregnancy. Further, heavy drinking during pregnancy has known potentially serious consequences, and should never be encouraged. Finally, there is insufficient scientific evidence that an occasional drink of alcohol during pregnancy leads to harm to the fetus, and should not cause undue alarm in a pregnant woman who may have consumed some alcohol before she realized she was pregnant.
Reference: Nykjaer C, Alwan NA, Greenwood DC, Simpson NAB, Hay AWM, White KLM, Cade JE. Maternal alcohol intake prior to and during pregnancy and risk of adverse birth outcomes: evidence from a British cohort. J Epidemiol Community Health 2014, pre-publication. doi:10.1136/jech-2013-202934
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 136: Alcohol’s effects on cardiovascular risk among subjects with diabetes mellitus — 18 March 2014
A U- or J-shaped curve for the relation of alcohol consumption to cardiovascular disease (CVD) among diabetics has been shown in most prospective epidemiologic studies for many years, and CVD is the leading cause of death among diabetics. A variety of potential mechanisms of protection against CVD have been described, including beneficial effects of moderate drinking on lipids, inflammatory markers, and insulin resistance. The current paper assesses the effects of alcohol use among participants in the Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified-Release Controlled Evaluation (ADVANCE) trial. It was based on more than 11,000 subjects with diabetes from 20 countries, including those in Eastern Europe, Asia, and established market economies in Western Europe, North America, and the Pacific region. The outcomes over 5 years of follow up were CVD events (death from CVD, non-fatal myocardial infarction, non-fatal stroke), microvascular disease (renal disease, diabetic eye disease), and all-cause mortality.
Key results of the analyses showed that during follow up, more than 1,000 subjects (about 10%) had a major CVD, with similar percentages experiencing a microvascular complication or dying. The authors report that “Compared with abstainers, any alcohol use was associated with a 17% lower risk of cardiovascular events, a 15% lower risk of microvascular complications, and a 13% lower risk of all-cause mortality.” While there were few heavy drinkers (<4% of subjects), their data indicated that there was no significant lowering of risk of the outcomes among such subjects. Subjects who consumed wine had lower estimates of cardiovascular disease outcomes and mortality than consumers of other beverages.
Forum reviewers considered this to be a well-done analysis based on a large cohort of subjects with diabetes mellitus, with an adequate number of non-drinkers to serve as a referent group. The results strongly support previous studies that have shown a lower risk of cardiovascular events and total mortality among diabetic subjects who consume moderate alcohol. The study also showed that the risks of microvascular complications (diabetic kidney disease, diabetic eye disease) were lower among moderate drinkers.
The Forum considers this to be an important message (to physicians and the public), as the vascular ravages of diabetes are very serious, and diabetes is such a common disease that is increasing throughout the world. Diabetic patients without contraindications to alcohol sorely need to know of the potential cardiovascular protection of moderate alcohol consumption.
Reference: Blomster JI, Zoungas S, Chalmers J, Li Q, Chow CK, Woodward M, Mancia G, Poulter N, Williams B, Harrap S, Neal B, Patel A, Hillis GS. The relationship between alcohol consumption and vascular complications and mortality in individuals with type 2 diabetes mellitus. Diabetes Care 2014; pre-publication: DOI: 10.2337/dc13-2727
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here
===============================================================================
Critique 135: Binge drinking greatly increases mortality risk among moderate drinkers — 11 March 2014
This study was based on a sample of “late-middle-aged” (55-65 years old at baseline) community residents who were recruited from the western part of the United States to participate in a study of late-life alcohol consumption and drinking problems. The present analyses evaluated association between episodic heavy drinking and total mortality among 446 adults who were considered to be “moderate” drinkers. The authors report that the 74 moderate drinkers who engaged in episodic heavy drinking (“binge drinking”) had more than two times higher odds of 20-year mortality than moderate drinkers who did not binge drink.
An association between binge drinking and health outcomes has been demonstrated in epidemiologic studies for decades. Many (but not all) studies have shown an approximately two-fold increase in the risk of adverse outcomes for binge drinkers, in comparison with moderate drinkers who do not binge drink. In reviewing the present study, Forum members commented on the small number of subjects (only 74 binge drinkers in the analysis), and some other analytic weaknesses (e.g., no data on potential changes in drinking habits over 20 years, inadequate control of some potential confounders, results not applicable to the general population as some subjects were recruited because of previous alcohol misuse). Nevertheless, the results of the study support adverse effects on mortality of such a drinking pattern.
There are now considerable scientific data indicating harmful health effects of episodic excessive drinking in terms of coronary heart disease, other diseases of ageing, and mortality. Simply knowing the average intake of subjects over a period of time is inadequate for classifying their alcohol consumption. For middle-aged and older subjects the drinking pattern that has been shown to be associated with the most favorable health outcomes (including greater longevity of life) is regular, light-to-moderate intake, especially when the alcoholic beverage is consumed with food.
Reference: Holahan CJ, Schutte KK, Brennan PL, Holahan CK, Moos RH. Episodic heavy drinking and 20-year total mortality among late-life moderate drinkers. Alcohol Clin Exp Res 2014; pre-publication; DOI: 10.1111/acer.12381.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 134: Comments on “Section 2.3, Alcohol Consumption,” from the “World Cancer Report 2014” issued by the World Health Organization – 11 February 2014
A recently released report by IARC (International Agency for Research on Cancer) of the World Health Organization, entitled “World Cancer Report 2014,” includes a section on alcohol consumption as a factor in the etiology of cancer. From reading this report, it is clear that the conclusion of the authors is that all alcohol consumption is harmful, regardless of the amount consumed, the type of beverage, or the pattern of drinking. The members of the International Scientific Forum on Alcohol Research (the Forum) have real concerns about the WHO report.
It appears that the authors have been very selective in choosing the data upon which they base their conclusions, often citing their own work and ignoring thousands of scientific articles relating alcohol consumption to cancer rates and mortality. The report fails to discuss potential lower risks of cancer associated with polyphenols in wine and some other beverages. It ignores the consistent finding in almost all prospective epidemiologic studies over many decades that total mortality rates are lower among light-to-moderate alcohol consumers (and recent evidence suggests that this may even be true among people with cancer).
Members of the Forum strongly agree that heavy alcohol consumption and “binge” drinking are associated with many adverse effects (and would never be advised by responsible agencies). However, the WHO report seriously undermines its credibility by publishing a report that seems to deliberately ignore overwhelming scientific evidence showing that light-to-moderate consumption of alcohol not only reduces overall mortality but is usually not associated with an increased risk of cancer.
Excessive and binge drinking in young people is a growing scourge in many parts of the world, and alcohol consumption (especially in conjunction with smoking) clearly increases the risk of upper aero-digestive cancers; further, even moderate consumption is associated with a slight increase in the risk of breast cancer in women. However, the scare tactics condemning all alcohol consumption in the WHO report tend to obscure those important messages.
It is the opinion of our Forum that WHO, in the alcohol section of its new publication World Cancer Report 2014, has not provided an objective statement on alcohol and cancer based on current scientific data. By doing so, WHO has lost credibility and, more importantly, has missed a key opportunity to convey important focused messages about alcohol and cancer that would be more likelty to improve the health of the public.
Reference: Rehm J, Shield K. Section 2.3, Alcohol Consumption, from World Cancer Report 2014, pp. 97-106, released 3 February 2014 by IARC (International Agency for Research on Cancer), of the World Health Organization.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 133: Alcohol intake may lower the risk of developing multiple sclerosis — 4 February 2014
Previous research has shown that alcohol consumption may be associated with a reduced risk of rheumatoid arthritis, lupus erythematosus, and other autoimmune diseases. There have also been reports that alcohol may lower the risk of multiple sclerosis (MS). The authors of the present paper have used data from two large Swedish case-control studies of MS to evaluate the relation of alcohol consumption to MS. Key results showed that in both of the case-control analyses, there was a dose-response inverse relation between alcohol consumption and the risk of developing MS. In comparison with subjects reporting no alcohol intake in the 5- or 10-year period during which the diagnosis of MS was first made, subjects in the highest alcohol consumption group (> 112 g/week, about 9 drinks per week for women; >168 g/week, about 14 drinks per week for men) had 30% to 50% lower risk of developing MS. A variety of potential confounders were included in the analysis, including smoking, education, and SES.
Forum members who reviewed this paper all thought that it reflected a well-done analysis. The main concerns were that, as are most studies of uncommon diseases, these were case-control comparisons (which may be associated with recall bias, reverse causation, and other potential confounding variables), and that the investigators could not determine if the “non-drinkers,” their referent group, were lifetime abstainers or former drinkers. Also, while earlier research has shown that the polyphenols in wine may provide protection beyond that of alcohol in combating inflammation, there were no data on beverage-specific results.
In general, however, Forum members welcomed this contribution to our knowledge on the subject, and thought that the authors did a good job in discussing the strengths and weaknesses of their study. There was a brief discussion of potential mechanisms by which alcoholic beverages could lower the risk of MS, but no discussion of the potential added effects related to polyphenolic substances. Forum members also thought that serum uric acid (which may increase with alcohol consumption) could play a role in an autoimmune disease, but this was not discussed by the authors.
Based on previous research and the results of this paper, it is probable that moderate alcohol intake, especially of wine, may lower the risk of developing MS, a neurological disease for which no cure is currently available. While MS is too uncommon a condition to use these findings to recommend alcohol consumption for the prevention of the disease, it would be useful if future research could help determine if, for subjects who already have MS, moderate drinking may affect the progression of their disease.
Reference: Hedström AK, Hillert J, Olsson T, Alfredsson L. Alcohol as a modifiable lifestyle factor affecting multiple sclerosis risk. JAMA Neurology 2014; doi:10.1001/jamaneurol.2013.5858; published online January 6, 2014.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 132: Pattern of alcohol consumption and cause of death in a large European prospective study — 21 January 2014
A large group of investigators participating in the European Prospective Investigation into Cancer and Nutrition (EPIC) study have reported on the association of alcohol consumption with disease-specific mortality over a 12-year period among a very large number of men and women. Alcohol intake over the past year (as well as estimates of earlier intake) was reported at baseline. A variety of approaches were used to identify deaths in the participating cohorts, but validation of the cause of death was not possible. No data were reported on certain key aspects of drinking pattern (frequency of alcohol intake, binge drinking, with meals, etc.) and beverage-specific effects were not reported.
The authors report that the risk of death from cardiovascular diseases was lower, and from cancer and certain other causes of death were higher, among drinkers than among their referent group of “lifetime light users” (men reporting ≤1 drink/week and women reporting ≤ 0.5 drinks/week). However, their graphs of alcohol intake and risk of total mortality (not included in the paper but in supplementary data they provide on the internet) show strong J-shaped curves for increasing alcohol intake for both men and women. For men, the risk among alcohol consumers of up to about 48 gr/day (the equivalent of approximately four “typical drinks”) was lower than that of the lifetime light users that made up the referent group; at higher intake, the risk increased above that of light drinkers. For women, the risk of total mortality for drinkers remained lower than that of the referent group at all reported levels of intake. Despite these findings, the entire paper focuses only on the increased risk of death from alcohol for certain diseases, and almost completely ignores the net, overall effects on total mortality.
Forum reviewers considered that while the analyses were done correctly, there were major weaknesses in the estimation of “lifetime alcohol intake,” no data on the pattern of intake, no validation of coexisting diseases and, especially, no validation of the specific cause of death, even though this was the primary outcome of the study. All of these factors weaken the strong assertions made by the authors in their conclusions.
Forum members were concerned that the authors seemed to obscure the total effects of light-to-moderate drinking (lower risk of all-cause mortality), and emphasize only the harmful effects. Some reviewers considered that the presentation appeared to be based more on ideology than on an unbiased assessment of the data, and one suggested that the paper appears to have been written starting from pre-conceived conclusions, then finding data to support them.
It is interesting that two Commentaries published with this article came to divergent views. One by Stockwell and Chikritzhs emphasized potential bias and confounding that cause concern when relating alcohol to mortality in observational studies. While they then pointed out how well the present authors adjusted for many of these factors, they nevertheless concluded their commentary repeating how such factors are difficult to control and stating that “ . . . a healthy dose of skepticism is warranted for the hypothesis that light/moderate alcohol consumption is beneficial to health.” (They do not mention that data on alcohol and mortality are far more robust that data supporting generally accepted beliefs of the beneficial effects of physical exercise, eating a healthy diet, maintaining a lean body mass, etc.)
On the other hand, the commentary on the present paper by Banks considered the data presented quite sound, and concluded: “If taken as causal, these findings are consistent with most public health advice about alcohol, except that most advice recommends an upper limit to alcohol consumption, but does not actually encourage drinking. In fact, the evidence goes further than this and indicates that, in later life, on average and bearing in mind the priorities and risks of specific individuals, drinking at least some alcohol, but not too much, is likely to minimize the overall risk of death.”
Reference: Bergmann MM, Rehm J, Klipstein-Grobusch K, et al (38 authors). The association of pattern of lifetime alcohol use and cause of death in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Int J Epidemiol 2013;42:1772-1790
Attached Commentaries:
Banks E. Commentary: Lifetime alcohol consumption and mortality: have some, but not too much. Int J Epidemiol 2013;42:1790–1792; doi:10.1093/ije/dyt218
Stockwell T, Chikritzhs T. Commentary: Another serious challenge to the hypothesis that moderate drinking is good for health? Int J Epidemiol 2013;42:1792–1794; doi:10.1093/ije/dyt217
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 131: Effects of alcohol consumption on the risk of gout — 23 December 2013
A new meta-analysis has been conducted to assess the effects of alcohol consumption on the risk of gout. A total of 12 articles with 17 studies involving 42,924 cases met the inclusion criteria. The authors report that the pooled RRs for light (≤1 drink/day), moderate (>1 to <3 drinks/day), and heavy drinking (≥3 drinks/day) vs. non/occasional alcohol drinking were 1.16 (95 % CI, 1.07–1.25), 1.58 (95 % CI, 1.50–1.66), and 2.64 (95 % CI, 2.26–3.09), respectively. The results suggested that alcohol consumption might be associated with increased risk of gout.
Forum reviewers agreed that the analytic methodology in this paper was appropriate. Considerable research has shown that alcohol intake, especially heavier drinking, increases serum uric acid levels and the risk of gout. There remain some questions about the relation of wine consumption with gout, and the present study did not have data to test beverage-specific responses.
Overall, data suggest that alcohol intake, especially heavier drinking, raises serum uric acid levels and may trigger an acute attack in persons with gout, especially those who are not controlling their disease with appropriate medication. A number of studies, including the present one, suggest that even light alcohol intake may increase the risk of developing gout. In any case, the risk appears to be rather low with light drinking, a level of alcohol intake that should reduce the risk of cardiovascular disease. Also, some studies suggest that the risk is lower for the consumption of wine than for the consumption of other beverages containing alcohol.
Reference: Wang M, Jiang X, Wu W, Zhang D. A meta-analysis of alcohol consumption and the risk of gout. Clin Rheumatol 2013;32:1641–1648.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 130: How alcohol consumption may interact with genetic factors that relate to health and disease — 10December 2013
Despite extensive research over the past few decades, our knowledge about the genes that underlie most chronic diseases remains incomplete. For example, even for alcohol-related diseases, it is not possible at present to determine how an individual person will respond over a lifetime to varying amounts of alcohol intake: not all heavy drinkers develop cirrhosis; not all moderate drinkers lower their risk of cardiovascular disease. While the underlying genetic pattern of a person undoubtedly plays a role in his/her health outcomes, environmental factors, including alcohol consumption, may modify the effects of genes. The modification of the effects of genes by environmental factors, such as alcohol intake, can be referred to as “epigenetics.”
A new paper on epigenetics, by a leading scientist who has worked at the National Institute of Alcohol Abuse and Alcoholism (NIAAA) for many years, provides important new insight into mechanisms by which alcohol intake, especially heavy consumption, may modify the activity of genes affecting health. Dr. Zakhari describes specific effects that heavy alcohol intake can have on the activities of enzymes involved in epigenetic modifications. In some cases, alcohol enhances genetically determined effects, in others it suppresses such activity. As stated by the author, “Metabolites, including those generated during ethanol metabolism, can impact disease states by binding to transcription factors and/or modifying chromatin structure, thereby altering gene expression patterns.”
Forum members consider this to be a very well-thought-out and well-done presentation of important new data. They agree with the author that these observations could help researchers to design model medications to treat or at least ameliorate alcohol-related organ damage, such as cirrhosis of the liver and alcohol-related cancers. While reviewers consider that these observations are important in our understanding of how alcohol affects health, they point out that they must be tested in further research, especially epidemiologic studies, to evaluate the extent that such interations between alcohol and genes actually affect health outcomes. Key problems that limit our ability to determine causality of disease from epidemiologic studies include not knowing the underlying genetic susceptibility of individual subjects and, as pointed out in the present paper, not accounting for environmental factors that may modify such genetic effects.
Reference: Zakhari S. Alcohol metabolism and epigenetics changes. Alcohol Research: Current Reviews 2013;35:9-16.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 129: Association of alcohol consumption with skin cancer; A report from the Women’s Health Initiative — 20 November 2013
A report from more than 59,000 women in the Women’s Health Initiative related reported alcohol consumption to the risk of melanoma (MM) and non-melanoma skin cancer (NMSC). This was a fairly large study, with 532 cases of melanoma and 9,593 cases of NMSC occurring over approximately 10 years of follow up. The key reported results were for a higher hazard of MM (HR 1.64) and NMSC (OR 1.23) for drinkers of 7 or more drinks/week, compared with non-drinkers. Lifetime alcohol consumption was also positively associated with hazard of MM and risk of NMSC, with the only significant increases for MM according to type of beverage being seen for women with a preference for white wine or liquor. As shown in many previous studies, the risk of these skin cancers was lower among smokers than among non-smokers.
Forum reviewers thought that this was a very well-done analysis. They did note that there were large decreases in the estimates of HRs related to alcohol consumption when adjustments were made for sun exposure and other known confounders. For example, the HR for MM decreased for total wine from 1.30 to 1.06 when adjusted; for red wine:1.71 to 1.34; for white wine: 1.93 to 1.52; for liquor: 1.87 to 1.65; for beer: 1.34 to 1.18. The magnitude of these changes, as well as the very different baseline characteristics of the women according to their drinking habits, raises the possibility that there may be residual confounding affecting the results. In addition, reviewer Zhang points out that by including subjects with these skin cancers prior to baseline in their main analyses, there could be a problems with bias in their results.
Forum member Klatsky has recently reported on this topic using several decades of follow-up data from the Kaiser-Permanente study, with more than 300,000 subjects and more than 1,000 cases of MM. In that study, he and his colleagues found that among persons preferring wine, the HR for MM at 3+ drinks per day was 1.7 (95% CI 1.2-2.5), while it was 1.2, 1.3, and 1.1 in persons with preference for liquor, beer, and no beverage type. However, at 1-2 drinks per day, wine drinkers had a HR of 0.9. Klatsky states “So maybe too much should not be made of the beverage type data in these analyses. However, the association with alcohol seems statistically solid.”
A previous study by Mukamal, with data from 300,000 subjects participating in a risk factor surveillance survey reports: “Approximately 33.5% of respondents reported a sunburn within the past year. Heavier average alcohol use and binge drinking were both positively associated with prevalence and number of sunburns within the past year. The adjusted odds ratios for prevalence and number of sunburns among binge drinkers were 1.39 (1.31-1.48) and 1.29 (1.20-1.38), respectively.” Klatsky wonders whether “possible confounding by sun is not only an artifact of SES and tropical vacations, but whether heavy imbibers at the beach may fall asleep when exposed or simply do not notice their sunburn until it is severe.” Other Forum reviewers also worry that there may be residual confounding in the present study from sun and ultraviolet exposure.
Klatsky adds: “However, even if the alcohol-melanoma association is due to confounding by sun exposure, the same explanation seems less plausible for the inverse association between smoking and melanoma. While there is obviously no public health utility in any ‘protective’ effects of smoking, that association is scientifically interesting and could be a clue to mechanisms.”
The bottom line is that there are considerable observational epidemiologic data suggesting that alcohol consumption may relate to an increase in the risk of MM and NMSCs. As mechanisms are not known, there is still concern that much of this relation may relate to residual confounding by ultraviolet sun exposure, the most important environmental factor for these diseases.
Rerference: Kubo JT, Henderson MT, Desai M, Wactawski-Wende J, Stefanick ML, Tang JY. Alcohol consumption and risk of melanoma and non-melanoma skin cancer in the Women’s Health Initiative. Cancer Causes Control 2013 (pre-publication) DOI 10.1007/s10552-013-0280-3
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 128: Little effect of alcohol consumption on breast cancer risk found among African-American women — 14 November 2013
Alcohol is known to be a risk factor for breast cancer in Caucasian women, but the evidence in African-American (AA) women is limited and results from previous studies are inconclusive. The present case-control study, based on 803 cases of breast cancer among African American women in the northeastern part of the USA, evaluated associations between recent and lifetime drinking and breast cancer risk. The authors report that there was no association between recent drinking and breast cancer risk, even when stratified by menopausal status or by hormone receptor status. Further, their analyses suggested a slight decrease in cancer risk with alcohol consumption among women who drank when under 20 years of age (OR = 0.65; 95% CI: 0.47–0.89), regardless of menopausal or hormone receptor status.
Forum reviewers point out that this was a case-control study of breast cancer, which always presents an opportunity for recall bias, and the number of cases was not large. Further, AA women generally drink very little, so it may be difficult to determine if larger amounts of alcohol may increase breast cancer risk.
On the other hand, the results were based on a very well-done and complete analysis, with appropriate control for known risk factors, similar results were obtained when recent (in last year) alcohol intake and long-term alcohol consumption were considered, and their finding of increased risk of breast cancer among subjects with a family history of breast cancer, a personal history of benign breast disease, and HRT use strengthen the results.
The results of this study are consistent with those from many previous studies showing little effect of alcohol consumption on breast cancer risk among AA women. However, given that few AA women in the USA drink alcohol, and those that do typically consume only small amounts, the study cannot estimate the potential effect on breast cancer among heavier drinkers. Further, Forum members believed that the decrease in the risk of breast cancer found in this study for drinking early in life (before age 20 years) may be due to residual confounding by socio-economic factors.
Overall, the present study supports previous research suggesting that the light alcohol consumption typically seen among AA women in the USA is not an important factor in their risk of breast cancer. On the other hand, this paper reports similar null results between alcohol and cancer risk among Caucasian women in their study. Current data do not necessarily indicate that there are ethnic differences in alcohol metabolism that may lead to differences between Caucasian and AA women in the association of alcohol consumption with breast cancer, and this study alone cannot be used to support such a premise.
Reference: Chandran U, Zirpoli G, Ciupak G, McCann SE, Gong Z, Pawlish K, Lin Y, Demissie K, Ambrosone CB, Bandera EV. Does alcohol increase breast cancer risk in African-American women? Findings from a case–control study. British J Cancer 2013;109:1945–1953 | doi: 10.1038/bjc.2013.513.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 127: Estimation of alcohol-attributable and alcohol-preventable mortality in Denmark — 6 November 2013
In an attempt to judge the harmful and beneficial health effects related to alcohol consumption, Danish scientists have carried out analyses comparing alcohol-attributable and alcohol-preventable mortality in Denmark. They have used estimates of the potentially harmful effects of alcohol use on more than 20 diseases, giving 100% values to “alcohol use disorders,” although the specific causes of death are not known for this category. Most of the other attributions for harm are realistic, but the alcohol preventable attributions for diabetes and ischemic heart disease appear to be low. The authors conclude that 5.0% of deaths among women and 9.5% of deaths among men were attributable to alcohol in Denmark in 2010, with the majority of all alcohol-attributable deaths caused by high consumption. They attribute only between 2 and 3% of deaths to be preventable by alcohol.
Previous estimates of alcohol-attributable and alcohol-preventable effects have varied widely, emphasizing the importance of the assumptions made by the investigators in any set of analyses. For example, an analysis of deaths in Germany by Konnopka et al (Konnopka A, Hans-Helmut König H-H. The health and economic consequences of moderate alcohol consumption in Germany 2002. Value in Health 2009;12:253-261) concluded that there were more alcohol-preventable deaths than alcohol-attributable deaths and a report from the UK also estimated much lower rates for alcohol-attributable deaths (White IR, Altmann DR, Nanchahal K. Mortality in England and Wales attributable to any drinking, drinking above sensible limits and drinking above lowest-risk level. Addiction 2004;99:749–756). Further, a previous report that included data for Denmark gave very different results for net alcohol effects, estimating that less than 1% of deaths were attributable to alcohol (Britton A, Nolte E, White IR, Gronbaek M, Powles J, Cavallo F, McPherson K. A comparison of the alcohol-attributable mortality in four European countries. Eur J Epidemiol. 2003;18:643–51). It is probable that different underlying assumptions of alcohol effects on various diseases are the prime reason for such differences.
There is no question that heavy alcohol consumption contributes to a large number of disease conditions, and the findings of this study emphasize the magnitude of the problem. On the other hand, if the potentially beneficial effects of moderate alcohol consumption on many common diseases are underestimated, a net unfavorable result, as in the present study, is unavoidable. It will be interesting to see what assumptions are made in other studies such as this, and how such assumptions affect the outcome of analyses.
Reference: Eliasen M, Becker U, Grønbæk M, Juel K, Tolstrup JS. Alcohol-attributable and alcohol-preventable mortality in Denmark: an analysis of which intake levels contribute most to alcohol’s harmful and beneficial effects. Eur J Epidemiol 2013; DOI 10.1007/s10654-013-9855-2
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 126: Moderate alcohol intake may lower the risk of rheumatoid arthritis — 11 October 2013
Moderate alcohol intake, compared with abstinence, has been related to lower inflammatory markers and a reduced risk of many auto-immune diseases, including rheumatoid arthritis (RA), systemic lupus erythematosus, autoimmure diabetes, and Graves hyperthyroidism. The present large meta-analysis relating alcohol to RA includes data from 5 prospective cohort studies and 3 nested case-control studies. Their analyses are based on prospective data from a total of almost 200,000 subjects, among whom 1,878 developed RA.
This meta-analysis concludes that low to moderate alcohol consumption is inversely associated with the development of RA. It suggests a “J-shaped” curve, with a lowered risk for an average intake of up to 15 g of alcohol (about 1 to 1 ½ typical drinks), in comparison with non-drinkers, and an increased risk for heavier drinking. While the immediate effects were greater for women in this study, for long-term effects the authors noted that “Regardless of sex, a consistent low to moderate alcohol consumption for a period of at least 10 years was found to have a 17% reduction in RA risk.”
Beneficial effects of alcohol on indices of inflammation have been shown repeatedly. The probable mechanism of alcohol’s effect on the risk of RA is down regulation of the immune response and a decrease in pro-inflammatory cytokines.
Reference: Jin Z, Xiang C, Cai Q, Wei X, He J. Alcohol consumption as a preventive factor for developing rheumatoid arthritis: a dose-response meta-analysis of prospective studies. Ann Rheum 2013. doi: 10.1136/annrheumdis-2013-203323
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 125: Effects of alcohol consumption on risk of colorectal cancer; potential modification by folate intake — 25 September 2013
Many epidemiologic studies have shown a small increase in the risk of breast cancer and colorectal cancer to be associated with alcohol consumption. Some have found that higher intakes of folic acid may attenuate such an increase in risk. The present study was designed to evaluate the influence of alcohol consumption on the risk of colorectal cancer according to folic acid fortification period in the United States. The relation of alcohol intake to colorectal cancer in two prospective studies (the Nurses’ Health Study and the Health Professionals Follow-up Study) was compared for a prefortification period (before 1998) with such risk estimates during the postfortification period, which began in 1998. A total of 2,793 cases of invasive colorectal cancer were documented.
The authors concluded that their data support an increase in colorectal cancer with high alcohol intake, and suggest that the risk may be lower in the postfortification period due to a higher folate intake in the US population. Forum reviewers had some concerns about these conclusions, as they point out that no dose-response relation between alcohol and colorectal cancer was shown in either period, and in data since 1998 no significant relation is seen between alcohol and such cancers. In fact, the authors of the present study state: “We also examined drinking pattern in relation to colorectal cancer risk; neither frequency of drinking nor quantity of drinking was associated with the risk of colorectal cancer;” they do not report their data upon which that statement is based.
Overall, the present paper does not answer the question as to the extent to which alcohol may relate to the risk of colorectal cancer, or if folate intake may modify any relation that may exist. Given that colorectal cancer (and breast cancer in women) are so common, it is important to evaluate how dietary folate and other nutrients may relate to such cancers. Further research on the relation of alcohol to these cancers, and potentially modifying factors, is greatly needed.
Reference: Nan H, Lee JE, Rimm EB, Fuchs CS, Giovannucci EL, Cho E. Prospective study of alcohol consumption and the risk of colorectal cancer before and after folic acid fortification in the United States. Annals of Epidemiology 2013;23:558-563.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 124: The J-shaped curve for the relation of alcohol consumption to mortality — 17 September 2013
An analysis based on data from more than 110,000 subjects in the USA, of whom 3,364 died during a follow-up period of up to 9 years, was used to evaluate the relation of “heavy drinking” and “nonheavy drinking” to the risk of all-cause mortality. The authors defined heavy drinking as 5 or more drinks/occasion, and recorded the frequency in which subjects consumed such amounts. Subjects consuming < 5 drinks/occasion were classified as nonheavy drinkers.
The key findings of the analyses were that there was a positive and linear increase in risk of mortality for subjects consuming heavy amounts of alcohol, with the risk increasing as drinking at this level was more frequent. For nonheavy drinkers, there was a J-shaped relation with mortality. The point at which the nonheavy drinkers’ risk of mortality exceeded that of abstainers was between 4 and 5 drinking occasions/week.
Forum reviewers thought that this was a well-done analysis that emphasizes the importance of the pattern of drinking, and not just the average weekly intake. Although the upper limits of drinks/occasion exceeded that usually considered as “moderate,” a J-shaped curve between alcohol and mortality for these drinkers was demonstrated. This is the pattern usually seen in prospective epidemiologic studies when “moderate” is defined at somewhat lower levels of alcohol intake.
Forum reviewers agreed with the conclusions of the authors regarding the importance of considering the pattern of drinking when evaluating the health effects of alcohol. The authors concluded: “Promoting less harmful drinking patterns by reducing heavy drinking frequency is an appropriate harm reduction strategy, and assessing drinking pattern by determining the frequency of heavy and nonheavy drinking is a simple and fast way to determine risk and promote less risky drinking behavior.”
Reference: Plunk AD, Syed-Mohammed H, Cavazos-Rehg P, Bierut LJ, Grucza RA. Alcohol consumption, heavy drinking, and mortality: Rethinking the J-shaped curve. Alcohol Clin Exp Res 2013;pre-publication: DOI: 10.1111/acer.12250
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 123: Alcohol consumption and lymphoid and myeloid neoplasms — 5 September 2013
Many prospective studies have shown that moderate drinkers are at lower risk of certain types of lymphoid cancer. For example, a report in 2009 from the Million Women’s Study in the UK found that alcohol consumption showed a significant inverse association with the occurrence of non-Hodgkin lymphoma (NHL). Further, a 2012 paper from that study based on 9,162 incident cases of haematological malignancy, including 7,047 lymphoid and 2,072 myeloid cancers, concluded: “Among predominantly moderate alcohol drinkers, higher intake was associated with lower risk of lymphoid malignancies.” Those investigators did not find a significant effect of alcohol on the risk of myeloid tumors, such as acute myeloid leukemia. Another 2012 paper based on almost 2,000 cases of Non-Hodgkin Lymphoma concluded: “In summary, findings from the prospective study presented here support the hypothesis that alcohol intake might be associated with a reduced risk of NHL.”
The authors of the present paper from the Netherlands, based on 17.3 years of follow up with 1,375 cases of lymphoid and 245 cases of myeloid neoplasms, did not find a statistically significant reduction in the risk of lymphoid cancers, and the authors suggest: “If any association between alcohol consumption and lymphoid neoplasms exists, our study suggests an increased risk rather than a decreased risk.”
While reasons for this difference in results of this study when compared with other recent studies may be used to better understand the association between alcohol and such cancers, Forum reviewers were concerned about a number of aspects of this study. For example, the authors had data on alcohol consumption only at baseline for this very long (17+ year) follow up, so changes (either increases or decreases in intake) were not known. Further, the key relations reported were not adjusted for a large number of potentially confounding variables, such as a positive family history of hematological cancer. (The authors state that they carried out such multivariable analyses but do not present the data.) Of even more concern was the apparent inverse effect of alcohol on cancer risk for a number of types of tumors when dose-response relations were shown.
Given the rather consistent findings in other very large studies of hematological malignancies that the risk of many types of lymphoid cancer may be reduced by alcohol, and inconsistencies in the results of the present analyses, it is difficult to conclude that the present paper should change our current interpretation of the association between alcohol and these types of cancer.
Forum members look forward to reports from other prospective studies on this topic. For the present, however, the overwhelming scientific evidence suggests that moderate alcohol consumption is associated with a decrease in the risk of many types of lymphoid malignancies, but has little effect on myeloid cancers.
Reference: Heinen MM, Verhage BAJ, Schouten LJ, Goldbohm RA, Schouten HC, van den Brandt PA. Alcohol consumption and risk of lymphoid and myeloid neoplasms: Results of the Netherlands cohort study. Int J Cancer 2013l133:1701–1713.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 122: Does moderate wine consumption lower the risk of developing depression? — 3 September 2013
There is a large literature relating heavy alcohol consumption to depression: most studies show that heavy drinkers tend to be depressed, and depressed people may self-medicate with large amounts of alcohol. This large prospective study of subjects at high risk of cardiovascular disease has shown that “moderate” drinkers, especially wine drinkers (the majority of their subjects), were at lower risk of developing depression during 7 years of follow up than were non-drinkers. An important aspect of this study is indeed that the analyses were based on moderate drinkers, as people exceeding certain amounts of alcohol or testing positive on the CAGE questionnaire (a measure of alcohol misuse) were excluded.
Strengths of the study include it being a large prospective study, with more than 5,000 subjects, aged 55-80 years at baseline, who were followed for up to 7 years for the initial development of clinical depression (which was diagnosed in 443 instances). Especially important was the ability of the investigators to have repeated assessments of alcohol consumption, every two years. A rather complete list of potentially confounding variables was available. The key findings of the study were that subjects reporting >5-15 grams/day of total alcohol intake, and wine drinkers of 2-7 drinks/week, were at a lower risk of developing depression than were non drinkers.
Some Forum members remained concerned that there may have been residual confounding by other lifestyle habits, and that the results may apply primarily to subjects who are also following a Mediterranean-type diet and lifestyle. Also, data were not available to evaluate the relation of heavy drinking or alcoholism to depression. However, the authors provide good scientific support for their conclusions that subjects reporting >5-15 grams/day of total alcohol intake (from about ½ to 1 ½ of a typical drink), and wine drinkers of 2-7 drinks/week, are at approximately 30% lower risk of developing depression than are abstainers of alcohol.
Reference: Gea A, Beunza JJ, Estruch R, et al (17 authors). Alcohol intake, wine consumption and the development of depression: the PREDIMED study. BMC Medicine 2013. Advanced publication, released 29 August 2013.
For the full critique of this paper by members of the International scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 121: Differences between wine and other alcoholic beverages in terms of adverse consequences of alcohol consumption – 22 August 2013
Questionnaire-based data on alcohol consumption were collected from more than 5,000 military recruits in Switzerland, who had a mean age of just over 19 years. There were very few drinkers who averaged more than 21 drinks/week, so the emphasis was on the effects of what is usually referred to as “binge drinking,” defined in this study as the consumption of 6 or more typical drinks (a drink containing 10-12 g of alcohol) on a single occasion. The “preference” of one particular type of beverage was based on the subject indicating that it made up more than two-thirds of his total alcohol consumption. The specific type of beverage preferred — beer, wine, or “other beverages” (the latter including apertifs, “pops,” chillers, and coolers) — was related to the pattern of drinking (frequency of binge drinking) and to the reported occurrence of adverse alcohol-related consequences (e.g., blackouts, driving after heavy drinking, missing work due to drinking, accidents, unprotected sex, encounters with police).
The authors report: “Preference for beer was associated with risky drinking patterns and, comparable with a preference for strong alcohol, with the use of illicit substances (cannabis and other illicit drugs). In contrast, a preference for wine was associated with low-risk alcohol consumption and a reduced likelihood of experiencing at least four negative alcohol-related consequences or of daily cigarette smoking.” More frequent binge drinking of any beverage was strongly associated with an increase in adverse alcohol-related consequences.
Forum reviewers thought that the adverse outcomes, especially those related to heavy beer intake, tend to characterize a particular subculture that demonstrates problematic substance use due to personal characteristics of the subjects. The unhealthy outcomes may be a feature more of the cultural habits of the subjects rather than just due to the type of beverage they consume most frequently.
The authors conclude that strategies for preventing problems with alcohol abuse should attempt to reduce excessive drinking of all types of beverages. However, they add: “to lessen the additional negative effects of beer and strong alcohol, which are particularly cheap in Switzerland, targeted strategies such as minimum pricing policies for these beverage types should be considered.” Forum members think that the extent to which such beverage-specific price restructuring would decrease unhealthy drinking practices among young people remains unclear.
Reference: Dey M, Gmel G, Studer J, Dermota P, Mohler-Kuo M. Beverage preferences and associated drinking patterns, consequences and other substance use behaviours. European Journal of Public Health 2013; advance access; doi:10.1093/eurpub/ckt109
For the full critique of this critique by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 120: Binge drinking impairs endothelial function in young people — 20 August 2013
The function of the vascular endothelium is a key process in the development of atherosclerosis and coronary heart disease, and extensive studies among middle-aged and elderly adults generally show beneficial effects of moderate drinking on vascular function. Whether or not alcohol consumption among young people has any lasting biological effects on cardiovascular risk is unclear: risk factors tend to track from childhood into adulthood, but specific long-lasting effects related only to drinking in young people are not known. Hence, data are currently not available to answer the question as to when during life people might consider beginning the moderate consumption of alcohol for the potential lowering of cardiovascular risk later in life.
The present study does not answer that question, as it only compares abstaining young people with binge drinkers, with the latter being defined as subjects reporting that they consumed ≥ 5 drinks in 2 hours for males, and ≥ 4 drinks in 2 hours for females. (The average number of binge-drinking episodes for these subjects was 6 ± 1 within the past month.) It does not compare abstainers with moderate drinkers. However, the paper does show that binge drinking among 18 – 25 year olds has adverse effects on endothelial function.
Forum reviewers were pleased to see this study, but point out that it is a cross-sectional analysis, and only compares binge drinkers with non-drinking young people. Further, inadequate data are presented to know the degree to which the results of the study may suffer from residual confounding from other factors.
The authors conclude that their study showed adverse effects on both microvascular and macrovascular function to be associated with frequent binge drinking in young people. It is hoped that these investigators, or others, will in the future provide data on the effects on vascular function of regular, moderate alcohol consumption among young people. It would also be interesting to learn if effects are different for high-polyphenol wine than for other beverages. Further, it will be important to determine how long beneficial or adverse effects on vascular function may persist, with or without continued alcohol intake.
Reference: Goslawski M, Piano MR, Bian J-T, Church EC, Szczurek M, Phillips SA. Binge drinking impairs vascular function in young adults. J Am Coll Cardiol 2013;62:201–207.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 119: A consensus statement on the association of moderate alcohol consumption and health — 13 August 2013
A group of Italian scientists has prepared a consensus paper to review the available evidence on the association between moderate alcohol use and health and disease. The report resulted from extensive discussions among 36 prominent Italian scientists, and provides a working document for the scientific and health professional communities. The report has been signed by 19 separate societies or federations in Italy, including societies in nutrition, cardiology, and general medicine, as well as organizations of scientists dealing with diabetes, hypertension, and obesity.
The consensus report ends with four conclusions:
“(1) In healthy adults and in the elderly, spontaneous consumption of alcoholic beverages within 30 g ethanol/d for men and 15 g/d for women is to be considered acceptable and do not deserve intervention by the primary care physician or the health professional in charge. In fact, there is no evidence to suggest complete abstention from alcohol drinking by moderate users.
(2) Patients with increased risk for specific diseases, for example women with familiar history of breast cancer, or subjects with familiar history of early CVD or cardiovascular patients should discuss their drinking habits with their physician.
(3) No abstainer should be advised to drink for health reasons.
(4) Alcohol use must be discouraged in specific physiological or personal situations or in selected age classes (children and adolescents, pregnant and lactating women and recovering alcoholics). Moreover, the possible interactions between alcohol and acute or chronic drug use must be discussed with the primary care physician.”
Forum reviewers considered this to be a well-done and generally well-balanced appraisal of the current literature on alcohol and health; it could help inform physicians and the general public about our current knowledge on this topic. However, Forum reviewers were concerned by several aspects of the report where it appeared that the conclusions were more “political” than “scientific” (perhaps necessary to gain the support of all of the societies endorsing the report).
The authors of the report provided good data to support their first two conclusions, and recent publications that were not available to the authors at the time they prepared their report strongly support these conclusions. However, Forum members found little data provided in the paper to support the third statement in their summary; in fact, the information the authors presented in the text would tend to support the opposite conclusion. Further, while it may be correct, their fourth conclusion was not supported by scientific data in the paper.
Forum members agreed that the importance of the effects of alcohol consumption on total mortality must always be considered, and agreed with the statement of the authors that “Low levels of alcohol intake (1-2 drinks per day for women and 2-4 drinks per day for men) are inversely associated with total mortality in both men and women.”
Key areas that the Forum believed could have been given more emphasis related to the association between alcohol and diabetes mellitus, where data strongly support an approximately 30% lower risk for moderate drinkers, in comparison with non-drinkers. And the risk of cardiovascular disease is considerably reduced among diabetics who consume alcohol moderately. And the potential effects of moderate drinking on reducing the risk of congestive heart failure, a rapidly increasing health problem related to ageing of the population, were not discussed. Forum members also wished that more emphasis had been given in the consensus report to the pattern of drinking: current data indicate that regular moderate drinking, rather than binge drinking, is the pattern associated with the most favorable health outcomes.
Overall, this consensus report is an important and useful addition to the scientific literature on the relation of moderate alcohol consumption to a variety of health outcomes. It could be of great values to physicians and policy makers when providing advice to the public regarding the effects of alcohol on health.
Reference: Poli A, Marangoni F, Avogaro A . . . de Gaetano G . . . et al (total of 36 authors). Moderate alcohol use and health: A consensus document. Nutrition, Metabolism, & Cardiovasular Disease 2013;23:487-504.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 118: Clustering of alcohol consumption with socioeconomic and biologic risk factors for cancer — 30 July 2013
It has been shown in most previous studies that moderate drinkers, especially those who generally consume wine, tend to have other “moderate” lifestyle factors. For example, they tend to be better educated, of higher socio-economic status, and generally are more active and eat a healthier diet than non-drinkers. An exception is cigarette smoking, which tends to be more common in drinkers than in abstainers. Epidemiologists studying alcohol and health are always striving to adjust appropriately for other lifestyle factors, attempting to assure that the difference in health outcomes among subjects relates to their drinking, and not to associated lifestyle factors.
In the present study, the investigators related alcohol consumption to a large number of socio-demographic and lifestyle factors that relate to the risk of cancer. They report that several factors were associated with alcohol consumption ≥10g/d in both genders: older age, smoking, higher socio-demographic category, higher income, and less healthy dietary intakes. Other factors were associated with alcohol consumption differently for men and women. The authors then report that the total number of such factors was higher among consumers of ≥10g/d of alcohol than among abstainers or lighter drinkers. They conclude: “The multiplicity of deleterious lifestyle behaviours combined with alcohol drinking must be taken into account in cancer prevention efforts. Gender-specific medical advice for people with personal or family history of alcohol-related diseases, including cancer, should be strengthened.”
While Forum reviewers found the data presented in this paper to be of interest, they did not believe that simply adding up all adverse risk factors provided useful information for the prevention of cancer. It is well known that smoking is a major risk factor for certain cancers, and in almost all studies alcohol consumers are more likely to be smokers; hence, drinkers should certainly be advised about the dangers of smoking. On the other hand, by simply summing the number of factors into a total score, the authors included a number of risk factors for which there is less of a scientific basis for their effect on cancer risk (e.g, the intake of supplements). Such factors should not be given the same weight as smoking as risk factors for cancer. Further, this study was carried out among computer-literate volunteers, so it may have limited relevance for the general population.
There have been extensive data showing that “healthy” and “unhealthy” lifestyle factors tend to cluster: for example, light-to-moderate drinkers tend to be leaner and eat a healthier diet than non-drinkers or heavy drinkers, as shown in this study. However, the prevention of chronic diseases relates to a large number of behaviors, and alcohol consumption cannot be considered as an isolated factor. Current epidemiologic data suggest that the combination of not smoking, being physically active, eating a healthy diet, avoiding obesity, and, unless contraindicated, regularly consuming small amounts of an alcoholic beverage, together make up what can be defined as a “healthy lifestyle.”
Reference: Touvier M, Druesne-Pecollo N, Kesse-Guyot E, Andreeva VA, Galan P, Hercberg S, Latino-Martel P. Demographic, socioeconomic, disease history, dietary and lifestyle cancer risk factors associated with alcohol consumption. Int J Cancer 2013;in press
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 117: Changes in alcohol intake modify levels of fibrinogen, an important risk factor for coronary heart disease — 18 July 2013
A prospective analysis of data from 2,520 subjects in the Coronary Artery Risk Development in Young Adults Study (CARDIA) cohort related reported alcohol intake at two examinations, 13 years apart, to levels of fibrinogen on the two occasions. Fibrinogen is a strong determinant of thrombosis, and is an important risk factor for coronary heart disease. The authors report that, in comparison with participants who never drank, those who became/stayed drinkers had smaller increases in fibrinogen, while those who quit drinking had the highest increase in fibrinogen over 13 years of follow-up. They conclude that lower levels of fibrinogen may be a key mechanism for the established protective effect of moderate alcohol intake on cardiovascular disease outcomes.
Forum reviewers considered this to be a potentially important paper, as the finding of higher fibrinogen among never drinkers and those who quit drinking may relate to the higher risk of coronary disease commonly reported from such subjects in prospective studies. However, the reviewers point out that the reasons that subjects quit drinking are not known (although the authors did adjust for conditions related to quitting drinking). Further, blood clotting factors other than fibrinogen may be affected by changes in alcohol consumption, and they were not reported in this paper. More research will be needed to determine if changes in fibrinogen levels are key elements in alcohol’s effects on cardiovascular disease.
Reference: Okwuosa TM, Klein O, Chan C, Schreiner P, Liu K, Green D. Long-term change in alcohol-consumption status and variations in fibrinogen levels: the coronary artery risk development in young adults (CARDIA) study. BMJ Open 2013;3:e002944. doi:10.1136/bmjopen-2013-002944
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 116: Effects of genetic factors on the metabolism of alcohol — 10 July 2013
A summary paper on genetically determined mechanisms related to the metabolism of alcohol and acetaldehyde describes numerous ways that the metabolism, especially of acetaldehyde, may be modified, both in the periphery of the body and in the brain. Individuals with a mutation of the aldehyde dehydrogenase gene (the ALDH2*2 allele), and certain other genetically determined enzymes, do not tolerate alcohol and are much less likely to become alcohol abusers. The authors state that their studies suggest possible therapeutic avenues in the treatment of alcoholism.
Reference: Israel Y, Rivera-Meza M, Karahanian E, Quintanilla ME, Tampier L, Morales P, Herrera-Marschitz M. Gene specific modifications unravel ethanol and acetaldehyde actions. Front Behav Neurosci 2013;7:80.doi:10.3389/fnbeh.2013.00080
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 115: Potential association of alcohol consumption with diverticulosis — 25 June 2013
The etiology of diverticulosis of the colon is poorly understood. Many, but not all, studies suggest that low fiber intake and obesity increase the risk; few studies have evaluated the relation of alcohol consumption and diverticulosis, with inconclusive results. This paper tests the cross-sectional association of alcohol consumption with diverticulosis among 746 asymptomatic consecutive subjects undergoing screening colonoscopies in Lebanon.
One-half of the subjects in this study were abstainers. Most of the “drinkers” stated that they consumed alcohol occasionally or < 1 drink/day; only about 10% reported 1 or more drinks/day, and no data on type of beverage or pattern of drinking were available. Nevertheless, from their analyses the authors conclude that alcohol consumption raises the risk of diverticulosis.
Forum members considered that this cross-sectional analysis provides little support for a causative effect of alcohol on the risk of diverticulosis. Most larger observational studies have not shown such an effect. In the present study, about 90% of subjects were either abstainers or consumed alcohol only occasionally or averaged < 1 drink/day. Further, the investigators did not evaluate the pattern of drinking (including binge drinking) and the results do not support an increase in risk with greater drinking (lack of a dose-response relation). Mechanisms for such an effect are largely unknown. Thus, few of the Hill criteria for “causality” are met.
The authors’ use of an inter-country comparison of per-capita alcohol intake and reported diverticulosis has no relevance: there are large cultural differences between nations with high and those with low per-capita alcohol intake, and alcohol use may well have been just a marker for a western-type culture. While the present study could be used to generate an hypothesis of a relation of alcohol intake to diverticulosis, attempts to validate such an association will require much additional research.
Reference: Sharara AI, El-Halabi MM, Mansour NM, Malli A, Ghaith OA, Hashash JG, Maasri K, Soweid A, Barada K, Mourad FH, El Zahabi L. Alcohol consumption is a risk factor for colonic diverticulosis. J Clin Gastroenterol 2013;47:420–425.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 113: Metabolic and biochemical mechanisms by which alcohol consumption affects health — 11 June 2013
A large study from Australia, that included a high percentage of current or former alcohol abusers, related alcohol consumption with a variety of metabolic and biologic parameters that relate to health. Included were markers of lipid function, inflammation, glucose metabolism, and liver function. As expected, there was a linear increase in HDL-cholesterol with increasing alcohol intake; somewhat surprisingly, there was a linear decrease in insulin levels with increasing alcohol consumption (which may relate to the typical finding of a significantly lower risk of diabetes mellitus among moderate drinkers). Essentially all of the other factors showed a “J-shaped” or “U-shaped” relation with alcohol: a decrease with small to moderate amounts of alcohol and an increase with larger intake.
In their association with alcohol, the lowest (most favorable) values of parameters varied by the measure: lowest triglycerides at about 1 to 2 drinks per day, lowest CRP at about 1 drink/day, lowest blood sugar and lowest alkaline phosphatase values at 1 to 3 drinks/day. Adverse effects on liver enzymes, blood glucose, and inflammatory markers showed a threshold level of intake that varied somewhat by marker. For example, reported non-drinkers had higher values of CRP, triglycerides, and alkaline phosphatase; among drinkers, significant increases were seen only in consumers of 40 or more drinks/week. Unfortunately, the investigators did not report on the pattern of drinking, which usually shows preferable results from regular, moderate intake of alcohol with no binge drinking.
The key findings of the study can be summarized as favorable effects of moderate alcohol intake on HDL-cholesterol and insulin levels, and for most other factors (including liver enzymes, triglycerides, blood glucose, and the inflammatory marker CRP), a “J-shaped” relation: lower values with light drinking and higher values with larger amounts of alcohol. For most of these, there was either no effect or a favorable effect until alcohol intake exceeded a “threshold value,” at which heavier drinking began to show adverse effects.
Forum reviewers agreed with the conclusion of the authors: “The pattern of potentially beneficial effects of alcohol on HDL-C and insulin increasing progressively as consumption increases, whereas the negative effects show thresholds, is consistent with net U- or J-shaped effects of alcohol on health.” While actual health outcomes were not evaluated in this study, overall it provides strong support for the results of most prospective epidemiologic studies that show lower rates of cardiovascular and other diseases among light-to-moderate drinkers than among abstainers or heavy drinkers.
Reference: Whitfield JB, Heath AC, Madden PAF, Pergadia ML, Montgomery GW, Martin NG. Metabolic and biochemical effects of low-to-moderate alcohol consumption. Alcohol Clin Exp Res 2013;37:575–586.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 112: Relation of alcohol intake to risk of dying from cancer — 23 May 2013
This paper presents a meta-analysis that related alcohol consumption to all-cancer mortality; it was based on almost 50,000 deaths reported in the literature from prospective cohort studies. Forum reviewers had some concerns about the conclusions of the paper, based on some discrepancies in the text, the lack of data on drinking pattern, no beverage-specific results, etc. Nevertheless, as expected, the reported average consumption of 50 or more grams of alcohol per day (equivalent to 4 or more typical drinks each day) was associated with an estimated 32% increased risk of dying from cancer.
However, there was no increase in the estimated risk of cancer death for subjects classified as “moderate” drinkers (defined by the authors using a wide range of intake: 12.6 to 49.9 grams/day, the equivalent of up to approximately 4 or more typical drinks). Further, Forum members were surprised that a slight but statistically significant decrease in cancer mortality risk was seen for “light” drinkers (those reporting an average of ≤ 12.5 grams/day, or about one typical drink). Forum members appreciated that misclassification of cause of death or residual confounding could have contributed to this latter result.
It is especially important that the only significant increase in risk in cancer mortality among the almost 50,000 cancer deaths reported in this meta-analysis was for consumers of 50 grams or more of alcohol. This suggests strongly that the overall risk of cancer mortality related to alcohol consumption is primarily (perhaps almost exclusively) from heavier drinking. Certainly, the findings from this study do not support the premise that “any amount of alcohol increases the overall risk of dying from cancer.”
Reference: Jin M, Cai S, Guo J, Zhu Y, Li M, Yu Y, Zhang S, Chen K. Alcohol drinking and all cancer mortality: a meta-analysis. Ann Oncol 2013;24:807-816. doi: 10.1093/annonc/mds508.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 111: Association of alcohol consumption with a measure of osteoporosis in elderly women — 7 May 2013
The density of bones, measured as bone mineral density (BMD), is strongly related to osteoporosis. Elderly women with osteoporosis, in particular, are at increased risk of fractures of the hip, arm, and spine; such fractures often relate to severe disability. With data on alcohol collected as part of a clinical trial on the prevention of osteoporosis, investigators in Finland have related alcohol consumption to changes over three years in BMD. After those excluded due to incomplete data, data on 300 women were available for analysis. The majority of women were abstainers or consumed little alcohol. Nevertheless, the results support much earlier research: regular, moderate drinking is associated with higher levels of BMD (i.e., lower risk of osteoporotic fractures) than is abstinence.
Forum reviewers, as did the authors, noted a number of limitations of the study: a rather small cohort with a very low intake of alcohol, a short duration of follow up, and rather small differences according to whether the women consumed alcohol or not.
Data from European surveys have shown that women in Finland tend to have high levels of osteoporosis and to drink very little; hence the increase in BMD associated with alcohol intake, even though slight, could be important in this population. Over the past three decades, there has been an increase in alcohol consumption in Finland, especially a marked increase in the consumption of wine. Hence, some Forum reviewers thought that the improvement in BMD among drinkers in this study may have been primarily from wine (which may have additional components, other than alcohol, that relate to BMD). However, the number of subjects was not large enough to test this hypothesis in the present study. Overall, this study supports the premise that moderate alcohol intake, along with an adequate calcium intake and vitamin D and exercise, may have a favorable influence on the risk of developing osteoporosis
Reference: Sommer I, Erkkilä AT, Järvinen R, Mursu J, Sirola J, Jurvelin JS, Kröger H, Tuppurainen M. Alcohol consumption and bone mineral density in elderly women. Public Health Nutr 2013;16:704-712. doi: 10.1017/S136898001200331X.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 110: Divergent effects of regular moderate and binge drinking – 30 April 2013
The present study relates alcohol consumption measured in young to middle-aged adults to mortality over a follow-up period of 20 years. The analyses are based on data from a large population in a region of Norway where the alcohol drinking pattern most commonly reported was binge drinking on infrequent occasions. Previous research has demonstrated that a very different drinking pattern – the frequent consumption of small amounts of alcohol – is generally considered to be the pattern associated with most health benefits.
In the present study, both men and women who reported consuming alcohol up to twice a month had about 20% lower mortality than did abstainers. All groups reporting binge drinking had higher mortality than non-binge drinkers (which was statistically significant for men and had a similar estimated effect among women). Cardiovascular and ischemic heart disease mortality had similar patterns as total mortality, being lower among drinkers but higher among those who reported binge drinking.
The key finding of this study is that there are divergent effects on mortality of the frequency of drinking and the amount of alcohol consumed per occasion. While the results for this study may reflect a certain Northern European pattern of drinking (not frequent but heavy on each occasion), they may not apply to other European or North American populations, where drinking is more frequent but binge drinking less common. Nevertheless, the results of this study support results typically found in more moderately drinking populations: more frequent drinking, but smaller amounts per occasion, is the pattern of alcohol consumption associated with the lowest risk of mortality. Both aspects of drinking must be considered when studying the relation of alcohol to mortality.
Reference: Graff-Iversen S, Jansen MD, Hoff DA, Høiseth G, Knudsen GP, Magnus P, Mørland J, Normann PT, Næss ØE, Tambs K. Divergent associations of drinking frequency and binge consumption of alcohol with mortality within the same cohort. J Epidemiol Community Health 2013;67:350-357. doi:10.1136/jech-2012-201564.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 109: In women developing breast cancer, moderate alcohol consumption before or after diagnosis does not increase breast cancer mortality and decreases total mortality — 16 April 2013
Most previous research has shown a slight increase in the risk of breast cancer (BrCa) among women who consume alcohol (versus nondrinkers), even among those whose average is only one drink/day. The association with death due to breast cancer is less clear, although overall total mortality among moderate drinkers is almost always lower than among non-drinkers; this reduction is generally attributed to a lower risk of cardiovascular disease.
The present study related alcohol consumption, both prior to the diagnosis of BrCa and after the diagnosis, with survival; deaths from BrCa and from cardiovascular disease, as well as total mortality, were related to alcohol intake. Specifically, in this study the authors assessed alcohol intake in a cohort of 22,890 women with incident invasive breast cancer (BrCa) who were residents of one of four US states and diagnosed at ages 20 to 79 years. During a median follow-up period of 11.3 years after diagnosis of BrCa, 7,780 deaths occurred, including 3,484 attributed to breast cancer.
Based on a quadratic analysis, moderate alcohol consumption before diagnosis showed a tendency towards lower risk of death from BrCa, and a significantly greater reduction in the risk of cardiovascular disease mortality and total mortality. Alcohol consumption after diagnosis was not associated with disease-specific survival, but was associated with a lower risk of total mortality. For women consuming alcohol prior to the diagnosis of BrCa, those who decreased their intake showed little effect on mortality, while those who increased their intake showed further lowering of their risk of cardiovascular and total mortality.
Forum reviewers considered this to be an excellent paper providing important new data on the association of alcohol consumption with survival after a diagnosis of invasive breast cancer. They thought that the statements of the authors accurately reflected their data, as they concluded: “Overall alcohol consumption before diagnosis was not associated with disease-specific survival, but we found a suggestion favoring moderate consumption. There was no evidence for an association with postdiagnosis alcohol intake and breast cancer survival. This study, however, does provide support for a benefit of limited alcohol intake for cardiovascular and overall survival in women with breast cancer.”
An accompanying editorial* agreed with the conclusions of the authors. The editorial stated, “Based on the best available evidence, including [the present report], it appears that modest alcohol consumption after breast cancer diagnosis, up to approximately one drink per day on average, may be associated with optimal overall survival, without compromising breast cancer-specific survival.”
*Demark-Wahnefried W. To your health: How does the latest research on alcohol and breast cancer inform clinical practice? jco.ascopubs.org/cgi/doi/10.1200/JCO.2013.490466),
Reference: Newcomb PA, Kampman E, Trentham-Dietz A, Egan KM, Titus LJ, Baron JA, Hampton JM, Passarelli MN, Willett WC. Alcohol consumption before and after breast cancer diagnosis: Associations with survival from breast cancer, cardiovascular disease, and other causes. J Clin Oncol 2013; pre-publication. Available at jco.ascopubs.org/cgi/doi/10.1200/JCO.2012.46.5765
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 108: An unusual paper relating alcohol consumption to the risk of stroke
Numerous well-done prospective epidemiologic studies have shown that while heavy drinking may increase the risk of stroke, light-to-moderate alcohol consumption is usually associated with a significant decrease in the risk of the most common type of stroke, ischemic stroke.
This paper from investigators in Finland states that it was designed to relate alcohol consumption and obesity to the risk of ischemic stroke. Unfortunately, even though it has clearly been shown that the amount and pattern of alcohol consumption strongly modify the effect on the risk of stroke, for some unknown reason the authors have grouped all consumers of alcohol into a single group. Specifically, there are no data given that describe the relation of light-to-moderate alcohol consumption with stroke. Hence, the conclusion of the authors that “alcohol increases the risk of stroke” is not supported by the data presented. In the opinion of members of the Forum, without reporting the effects according to the amount of alcohol consumed or the pattern of drinking, this is an unsupported and potentially dangerous statement to present in a scientific journal.
Reference: Rantakömi SH, Laukkanen JA, Sivenius J, Kauhanen J, Kurl S. Alcohol consumption and the risk of stroke among hypertensive and overweight men. J Neurol 2013;260:534–539. DOI 10.1007/s00415-012-6672-6
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 107: Little effect on child’s mental functioning associated with mother’s light, occasional drinking in early pregnancy – 25 March 2013
A new report from the prospective, population-based Avon Longitudinal Study of Parents and Children (ALSPAC) in the UK is based on investigation of the association between light drinking in pregnancy (<1 glass per week in the first trimester) and child mental health. Mental health was assessed in more than 6,000 children using both parent- and teacher-rated Strengths and Difficulties Questionnaires (SDQs) at age 11 years. Academic outcomes based on Key Stage 2 examination results were measured in more than 10,000 children.
Approximately 40% of women consumed some alcohol but less than 1 glass/week, while 16% reported consuming ≥1 glass per week during the first trimester. The authors report that after adjustment, relative to abstainers, there was no effect of light drinking on teacher-rated scores or examination results. In girls, although there was a suggestion of worse outcomes on the parent-rated total score in those exposed to light drinking compared to abstainers, no dose–response relationship was evident. The authors conclude: “Light drinking in pregnancy does not appear to be associated with clinically important adverse effects for mental health and academic outcomes at the age of 11 years.”
Forum reviewers considered this to be a well-done study, with a balanced assessment of results by the authors. Reviewers were surprised at the somewhat arbitrary separation of alcohol consumption: <1 drink per week versus ≥1 drink per week. Current guidance about alcohol consumption in pregnancy from the Department of Health in England (2009) allows for pregnant women to drink up to 1–2 units of alcohol once or twice a week, and it would have been preferable to have data presented for drinkers at this level.
Forum Co-Director Conibear considered that “The most important aspect of this study relates to the fact that 25% of babies in the UK are unplanned, and 17% of mothers do not know they are pregnant until eight weeks or more. Therefore balanced advice concerning the effect of alcohol use in early pregnancy is crucial to prevent unnecessary concern amongst this group of mothers to be. Although the best advice is to avoid alcohol if you are pregnant, the present research can reassure mothers who drank occasionally without realising that they were pregnant that they have not done long-term harm to their baby.”
Forum reviewer Stockley added: “I think that another important message is that if a woman decides to consume a small amount of alcohol during pregnancy, she should never binge drink or get drunk. This we know can have adverse effects on the developing fetus, especially in the first trimester, but interestingly, also in the third trimester of pregnancy.”
Reference: Sayal K, Draper ES, Fraser R, Barrow M, Davey Smith G, Gray R. Light drinking in pregnancy and mid-childhood mental health and learning outcomes. Arch Dis Child 2013;98:107–111. doi:10.1136/archdischild-2012-302436.
For the full critique of this publication by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 106: A clinical trial shows that glucose metabolism is improved more by red wine than by gin — 14 March 2013
To compare the effects of moderate consumption of red wine, dealcoholized red wine, and gin on glucose metabolism and the lipid profile, a group of Spanish investigators carried out a randomized control trial among 67 men at high cardiovascular risk. All received each of red wine (30 g alcohol/d), the equivalent amount of dealcoholized red wine, and gin (30 g alcohol/d) for 4 week periods, in a randomized order. While fasting glucose levels were not affected, mean adjusted plasma insulin and HOMA-IR decreased after red wine and dealcoholized red wine, but not after gin. HDL cholesterol, Apolipoprotein A-I and A-II increased after red wine and gin. Lipoprotein(a) decreased after the red wine intervention. The authors conclude that their results support a beneficial effect of the non-alcoholic fraction of red wine (mainly polyphenols) on insulin resistance, thus greater protective effects on cardiovascular disease from red wine than from other alcoholic beverages.
Forum members were unanimous in considering this to be a very well-done and important trial. It supports a huge amount of observational data from epidemiologic cohort studies that have shown that subjects who consume moderate amounts of alcohol tend to have much lower risk of developing diabetes. Further, patients with diabetes who drink moderately have much lower risk of subsequent cardiovascular disease and lower mortality. Studies such as this one help scientists understand the mechanisms by which moderate drinking, especially of wine, can reduce the risk of metabolic and vascular diseases.
Reference: Chiva-Blanch G, Urpi-Sarda M, Ros E, Valderas-Martinez P, Casas R, Arranz S, Guillén M, Lamuela-Raventós RM, Llorach R, Andres-Lacueva C, Estruch R. Effects of red wine polyphenols and alcohol on glucose metabolism and the lipid profile: A randomized clinical trial. Clinical Nutrition 2013. Pre-publication. dx.doi.org/10.1016/j.clnu.2012.08.022.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 105: For preventing cardiovascular disease, an unrestricted-calorie Mediterranean-type diet provides 30% more benefit than a low-fat diet: Results of a large population-based clinical trial — 6 March 2013
A large well-done clinical trial in Spain was carried out among 7,447 subjects at high-risk of cardiovascular disease (on the basis of diabetes, hypertension, dyslipidemia, and other risk factors). The trial compared the effects of two versions of an energy-unrestricted Mediterranean-type diet, one with large amounts of extra-virgin olive oil (EVOO) and one with a supplement of mixed nuts, with results among subjects in a “control group,” made up of subjects who were advised to follow a low-fat, low-cholesterol diet (that has typically been recommended for reducing the risk of cardiovascular disease).
Both of the groups advised to consume a Med-Diet showed an increase in total fat, from an average of 39.3 % of total calories to an average of more than 41%; the group advised to decrease their total fat lowered their intake from 39 to 37 % of calories. All three groups showed slight decreases in saturated fat and slight decreases in dietary cholesterol intake (but blood cholesterol levels were not reported). Only the Med-Diet + nuts group showed an increase in alpha-linolenic acid (ALA), the fatty acid related to the lowest risk of cardiovascular disease in the Cretan cohort of the Seven-Countries Study and in the Lyon Diet-Heart Study.
The large majority of subjects in all groups consumed wine at baseline, and about one-third of the Med-Diet groups and one-quarter of the control group reported consuming ≥ 7 glasses of wine/week during the trial. However, alcohol consumption was not evaluated specifically for its effects in the present study.
The study was ended early by its data and safety monitoring board due to marked advantages being shown in terms of the occurrence of the primary end-point (the occurrence of myocardial infarction, stroke, or death from cardiovascular causes) in both Med-Diet groups in comparison with the control group. The multivariable-adjusted hazard ratios were 0.70 and 0.72 for the Med-Diet with olive oil and the Med-Diet with added nuts, hence an approximately 30% decrease in risk among subjects assigned to a Med-Diet compared with those in the control group.
Forum members (as did the authors) had difficulty in determining which specific components of the Med-Diet may have been the primary reasons for its more favorable results, as significant dietary changes during the trial were mainly related to the supplementary olive oil or nuts given to subjects in the two Med-Diet groups. Among potential factors were increased mono-unsaturated fat and higher antioxidants from the added EVOO and an increase in ALA from the supplemental nuts. Forum members noted that the Med-Diet interventions apparently did not provide an increase in the intake of ALA, which could have led to even more protection against cardiovascular disease.
In any case, the striking reduction in risk shown in the study from the Med-Diet provide further evidence of the effectiveness of such a diet in reducing cardiovascular disease. It has been shown repeatedly that people advised to consume a Mediterranean-type diet tend to comply much better with such advice than do people advised mainly to decrease their intake of all fats and cholesterol. A very large amount of scientific data now support advice to follow a Mediterranean-type diet, one that does not restrict calories but encourages the intake of selected fats (which may include extra-virgin olive oil or canola oil), as well as more fruits, vegetables, grains, nuts, and wine; it may be the most effective dietary approach for reducing cardiovascular disease.
Reviewer Keil points out that many good prospective cohort studies have shown that an increase in adherence to components of a Mediterranean-type diet decreases the risk of many diseases and mortality. He adds: “The great thing about the present study is that when the skeptics raise their voice and argue that the proponents of the Mediterranean diet have only observational data available, we can now respond that we not only have RCT data on secondary prevention (Lyon Diet-Heart study) but also the present study on primary prevention of cardiovascular disease.”
Reference: Estruch R, Ros E, Salas-Salvadó J, Covas M-I, Corella D, Arós F, et al, for the PREDIMED Study Investigators. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 2013. DOI: 10.1056/NEJMoa1200303
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please clickhere.
===============================================================================
Critique 104: Moderate alcohol consumption is associated with a lower risk of diabetes — 26 February 2013
A population-based longitudinal study in Norway showed a lower risk of developing type II diabetes, and a tendency for less auto-immune diabetes, among subjects reporting moderate alcohol consumption. The lowest risk was among subjects reporting that they consumed alcohol 5-10 times during the previous two weeks or reporting a daily consumption of 10-15 grams of alcohol per day (slightly less than one to a little over one drink per day, using 12 g of alcohol per day as a “typical drink”).
The overall results from this study support most previous research showing a rather large (approximately 30% or more) reduction in the risk of Type II diabetes mellitus to be associated with moderate drinking. In this study, the strongest protective effect related to the consumption of wine, rather than beer or spirits. Unlike some previous research, the present study did not show an increased risk of diabetes among binge drinkers, heavier drinkers, those reporting episodes of intoxication, or those giving positive responses on a CAGE questionnaire (a measure of an alcohol use disorder). As it is likely that alcoholics were under-represented in the cohort, the ability to show the effects of very heavy drinking may have been limited.
While the numbers of subjects with auto-immune diabetes were small, there was a tendency seen for a similar reduction in risk with moderate drinking as with the much more common Type II diabetes. Overall, this study strongly supports much previous research showing that moderate alcohol consumption is associated with a lower risk of developing diabetes.
Reference: Rasouli B, Ahlbom A, Andersson T, Grill V, Midthjell K, Olsson L, Carlsson S. Alcohol consumption is associated with reduced risk of Type 2 diabetes and autoimmune diabetes in adults: results from the Nord-Trøndelag health study. Diabet Med 2013;30:56–64.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 103: Alcohol intake just prior to bed-time may affect your sleep patterns — 18 February 2013
A paper from experts in the science of sleep provides an excellent review of intervention studies since the 1980s on the effects of alcohol consumption on sleep. The study finds that the time required to fall asleep, and sleep patterns in the first part of the night, tend to be improved by alcohol. The authors conclude that “The onset of the first REM sleep period is significantly delayed at all doses and appears to be the most recognizable effect of alcohol on REM sleep, followed by the reduction in total night REM sleep.” Slow-wave sleep is more common and REM sleep less common after alcohol.
The studies reviewed in this report were intervention studies among mainly young normal subjects, not people with sleep disorders. Other studies have demonstrated that small amounts of alcohol given in the evening to the elderly may improve sleep, and reduce the need for sleep-inducing medications. Overall, the data reviewed in this paper suggest that small amounts of alcohol in the evening have few adverse effects on sleep, and relate to earlier onset of sleep and less awakening in the first part of the night. Larger amounts of alcohol tend to make the onset of sleep faster, but may have some adverse overall effects on sleep patterns, with a shorter duration of REM sleep throughout the night.
Reference: Ebrahim IO, Shapiro CM, Williams AJ, Fenwick PB. Alcohol and sleep I: Effects on normal sleep. Alcohol Clin Exp Res 2013;doi: 10.1111/acer.12006. [Epub ahead of print]
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Requested comments on paper by Nelson et al
by R. Curtis Ellison, MD, Professor of Medicine & Public Health,
Boston University School of Medicine
NOTE: These comments do not necessarily reflect the views of the members of the International Scientific Forum on Alcohol Research
Nelson DE, et al. Alcohol-attributable cancer deaths and years of potential life lost in the United States. Am J Pub Health, released February 14, 2013
We always welcome new scientific publications that help elucidate factors related to the development of cancer. The new paper by Nelson et al focuses on the role that alcohol consumption may play in the risk of a number of cancers.
Background: It has long been appreciated that there are a number of upper aero-digestive cancers, such as cancer of the mouth, throat, and esophagus, that occur much more frequently in heavy drinkers, especially alcoholics, than in abstainers. Physiologic studies suggest that these are not diseases of light to moderate drinkers, as a certain amount of alcohol is required to produce these diseases. Similarly, among people consuming enough alcohol to lead to liver cirrhosis, the risk of liver cancer is also markedly increased.
These “alcohol-related cancers” should be discussed separately from other more common cancers – especially colon cancer and female breast cancer – for which the risk may be only slightly increased by alcohol. In the case of breast cancer, there may be a slight increase in risk among some women consuming an average of only one drink/day (in some studies, such an increase in risk occurs primarily among women who binge drink, have an inadequate intake of folate, and/or are also on hormone replacement therapy.)
For these types of cancer, it is especially important to consider the net health effects of alcohol consumption. For example, it is estimated that if a woman at average risk of breast cancer (i.e., does not have such a cancer in a first-degree relative) decides to avoid drinking completely in hopes of reducing her risk of breast cancer, her risk of breast cancer would be expected to be slightly decreased, on average, by perhaps 5-10%; however, her risk would be increased of dying from much more common diseases such as heart attack, stroke, or other conditions for which small amounts of alcohol have been shown to reduce risk. And, importantly, her risk of dying of any cause (total mortality) would actually be increased by her avoiding light alcohol consumption.
The pattern of drinking has often been shown to be even more important than the average amount of alcohol consumed. A stronger association with beneficial effects is seen with the regular (up to daily) intake of small amounts of an alcoholic beverage; drinking larger amounts on fewer days (including binge drinking) is almost always associated with adverse health effects. For example, a man having up to 2 drinks each day would have an average of 14 drinks per week, generally considered to be within recommended guidelines. However, a man consuming 7 drinks on each of only two days each week, despite the same weekly average consumption, would not be considered to be a moderate drinker.
Comments on the present paper: There are a number of concerns about the analyses and conclusions of the authors of the present paper. These include the following:
(1) The authors have “corrected” the reported data on alcohol consumption to make up for presumed under-reporting, using a method not generally accepted by statisticians and other researchers. This means that even many “light” drinkers are listed as reporting greater amounts of alcohol.
(2) The authors do not clearly separate the effects of truly moderate drinking from heavier drinking in their conclusions. They use up to 20 grams of alcohol per day as their lowest drinking category; this is higher than the 14 g/day that is the current definition of responsible drinking for women in the US Guidelines. Further, as stated, if reported intakes are increased artificially, many more light drinkers would be bumped up into higher categories of drinking. The result of this mis-categorization is that bona fide moderate drinking, which has been shown by others to have no association with most types of cancer, is improperly associated in this study with increased cancer.
(3) The authors’ implications that even regular, moderate drinking increases the risk of many cancers is not consistent with most previous research. Further, by not having data on the pattern of drinking, the authors include binge drinkers in the same category as regular drinkers, further exaggerating the association of cancer with moderate drinking. Others have clearly shown that there are large differences in effect between these two patterns. (It is troubling also that in the paper, the estimated percentage of alcohol-attributable cancer risk among subjects reporting > 0 to 20 grams of alcohol per day is much higher than that of subjects reporting > 20 to 40 grams/day; while this partly relates to the large number of persons who drink only small amounts, such an association makes no sense biologically. It is difficult to understand who the subjects are in the lowest drinking group, but it may include a large percentage of ex-alcoholics or heavier drinkers underreporting their intake. However, this makes any conclusions in this paper regarding the risk of cancer among moderate drinkers highly suspect.)
(4) The authors do not point out the demonstrated effects of alcohol on total mortality; regular, light-to-moderate drinkers live longer. By focusing only on cancer risks, the authors fail to mention the effects on the risk of much more common conditions, such as coronary heart disease, stroke, dementia, other important health problems of ageing, and on total mortality. The study of the health benefits and problems of drinking is a very mature field — authors generally discuss their observations in the context of total mortality or other major diseases that would be affected by their experimental design. In nearly all cases, light drinking is shown to be beneficial; these studies are ignored here.
(5) Overall, a criticism of this paper relates to the failure of the authors to put their results into perspective. Statements such as “There is no safe threshold for alcohol and cancer risk” is more of a “scare” statement than a balanced discussion of their results. Given that almost all prospective studies show that regular moderate drinkers have better health as they age and live longer than lifetime abstainers, even papers focused on the effects of alcohol on any particular disease should present a balanced view on its net effects on health and disease.
(6) Finally, the authors of this paper have taken the results of their analyses (some of which are based on questionable assumptions) as “truth,” then expounding at length about the public health implications. There should always be a certain amount of doubt when presenting the results of an individual study, as no one analysis can possibly reveal everything about an association. (As stated by Voltaire: “Doubt is not a pleasant condition, but certainty is absurd!)
As the authors acknowledge, observational epidemiologic data can never reveal the full “truth” about the causation of disease from exposures, and each new study’s results must be interpreted taking into consideration previous research. However, the overall implications presented by the authors of this paper suggest that their goal may have been to support a presumed conclusion to discourage alcohol consumption, not to carefully interpret the available data to best advance the public health.
Key points of these comments
- There are a number of assumptions taken by the authors in their analyses that raise questions about their results. The authors present only “adjusted” data for reported alcohol intake (based on national sales, not on individual intake), making the relation of alcohol intake to the occurrence of cancer in individuals unclear.
- There is poor differentiation between regular moderate drinking and periodic heavy drinking (binge drinking) or alcoholism, although there are marked differences in health effects between these groups. Regular, moderate drinking is associated with net health benefits, whereas binge drinking and alcoholism have almost exclusively adverse effects (including increases in many types of cancer).
- There has been a huge amount of previous research in this field, but the authors do not put their own results into perspective or discuss the overall health effects of alcohol consumption. Previous data have clearly shown that regular moderate drinkers tend to have lower risk of cardiovascular disease, stroke, diabetes, and many other diseases, and have a lower overall risk of all-cause mortality.
Submitted by
- Curtis Ellison, MD, Professor of Medicine & Public Health; Director, Institute on Lifestyle & Health;l Boston University School of Medicine
Co-Director, International Scientific Forum on Alcohol Research
===============================================================================
Critique 102: Possible prevention of myocardial infarction from alcohol’s effects on periodontal disease: An hypothesis — 6 February 2013
A cross-sectional analysis among more than 5,000 Norwegian men was designed to determine if the frequency of alcohol consumption related to the risk of myocardial infarction associated with infectious periodontal disease. The authors hypothesized that because it is bactericidal, frequent alcohol consumption would decrease periodontal infection and lower the risk of tooth extraction related to periodontal infection. The authors state that their main finding was that frequent drinking lowers the risk of MI associated with periodontal disease.
Forum reviewers had real concern about the paper and the conclusions of the authors. Some stressed that the per cent of alcohol in most “drinks” is too low to be really bactericidal, that the key exposures (alcohol and oral infections) were based exclusively on self report and did not have information on type of beverage or pattern of drinking, that many confounders (especially related to socio-economic status) were not adequately taken into consideration, and that the authors did not really test the results of their study with appropriate statistical testing.
Current scientific data show an increase in the risk of cardiovascular disease to be associated with periodontitis. Further, data consistently show a decrease in the risk of cardiovascular disease from moderate drinking, and a very large number of mechanisms have been identified. However, the present study does not confirm that alcohol consumption plays an important role in preventing heart disease through its effect on periodontitis.
Reference: Håheim LL, Olsen I, Rønningen KS. Oral infection, regular alcohol drinking pattern, and myocardial infarction. Medical Hypotheses 2012;79:725–730.
For the full critique of this article by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 101: A review of the association of alcohol consumption with the risk of developing hypertension — 22 January 2013
A meta-analysis from investigators at Columbia University in New York evaluated the risk of developing hypertension according to the level of alcohol consumption previously recorded. The analyses were based on data from 16 prospective studies. The paper’s main results are that among men, there is little effect of alcohol consumption up to 30 grams of alcohol per day (the equivalent of about 2 ½ “typical drinks” by US standards or more than 3 drinks by UK standards), but evidence of an increased risk of hypertension for the intake of greater amounts of alcohol. For women, light drinking appears to be associated with a slightly lower risk of hypertension, but more than 20 grams/day of alcohol may increase the risk.
While Forum members thought that the analyses were done well, they had some concerns about the conclusions of the authors, some of which appear to not be in line with the data they presented. For example, their statement that “heavier alcohol consumption >20 g⁄d is associated with the risk of development of hypertension in both women and men” is not consistent with their findings of a significant increased risk of hypertension only with an intake of 31 – 40 grams of alcohol per day.
Similarly, the authors conclude: “Even for light drinkers, vigilant blood pressure monitoring is necessary,” which may not be appropriate given that their data show that intake below 30 grams per day has no significant association with hypertension in men and may actually reduce the risk of hypertension in women.
Overall, the results of this study, in line with findings from most previous research, indicate that people who consume alcohol according to most current drinking guidelines (no more than 2 typical drinks/day for men or 1/day for women) do not show an increase in their risk of hypertension, but heavier drinking appears to increase the risk. Not discussed in this paper, but especially important in terms of health, is that light drinking is associated with a significant and rather large decrease in the risk of the most serious sequelae of hypertension: coronary heart disease and ischemic stroke.
Reference: Briasoulis A, Agarwal V, Messerli FH. Alcohol consumption and the risk of hypertension in men and women: A systematic review and meta-analysis. J Clin Hypertens 2012;14:792-798.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 100: The effects of moderate drinking on cognitive function and dementia: An update — 15 January 2013
A paper from a group of Italian scientists provides an extensive review of the available research relating alcohol consumption to cognitive function. It presents brief summaries of results from most key epidemiologic studies dealing with this topic between 1987 and 2011. The large majority of these studies, and recent meta-analyses, support a finding of a lower risk of cognitive impairment from ageing and of dementia to be associated with moderate drinking.
Reviewers praised the authors for pointing out difficulties caused by having to develop guidelines for alcohol consumption based only on observational data, and not having large clinical trials for judging effect. A further problem faced in judging the numerous studies on this topic is that many lack data on beverage type and most lack detailed information on the pattern of drinking, which may be especially important in judging the effects of drinking.
Some reviewers stated that the paper does not present anything new, as previous meta-analyses have clearly shown a potentially protective effect of moderate alcohol consumption on the risk of cognitive decline and dementia. Given that recent large meta-analyses have shown that moderate drinking, is comparison with abstention, is usually associated with 20-35% lower risk of cognitive decline and dementia, Forum reviewers thought that the conclusions of the authors of this review paper were unnecessarily cautious. Overall, current scientific data support a conclusion that moderate consumption of alcoholic beverages, especially of wine, is neuroprotective.
Reference: Panza F, Frisardi V, Seripa D, Logroscino G, Santamato A, Imbimbo BP, Scafato E, Pilotto A, Solfrizzi V. Alcohol consumption in mild cognitive impairment and dementia: harmful or neuroprotective? Int J Geriatr Psychiatry 2012;27:1218-1238.
For the full review of this critique by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 099: Alcohol and survival after postmenopausal diagnosis of breast cancer — 20 December 2012
This paper assessed the association of pre-diagnostic alcohol consumption with disease recurrence and survival in a prospective cohort study in Germany based on 2,522 postmenopausal breast cancer patients, aged 50–74 years. The authors report that alcohol consumption was non-linearly associated with increased breast cancer-specific mortality, but not with breast cancer recurrence. Results were independent of estrogen receptor status. The authors also report a non-significantly decreased risk of mortality due to other causes.
Forum reviewers considered this to be a well-done analysis that was limited, however, by the lack of data on drinking patterns prior to breast cancer diagnosis and because no data were available on drinking after the diagnosis (the latter limits the applicability of its results to women who have already developed breast cancer). The comparisons were primarily between non-drinkers/light drinkers and women in the highest alcohol category; the authors state that when ex-drinkers were removed from the referent category, their results regarding breast cancer-specific mortality were no longer statistically significant. The authors do not describe the potential effects on their main results that could result from what is known as “index event bias,” which may occur when an exposure (e.g., alcohol) relates to the development of a disease, breast cancer in this study, and may also relate to sequelae (e.g., recurrence or death) from the same disease.
Forum reviewers conclude that current scientific data show that alcohol consumption may increase the risk of developing breast cancer. However, they believe that the effects on subsequent survival after such a diagnosis remain unclear.
Reference: Vrieling A, Buck K, Heinz J, Obi N, Benner A, Flesch-Janys D, Chang-Claude J. Pre-diagnostic alcohol consumption and postmenopausal breast cancer survival: a prospective patient cohort study. Breast Cancer Res Treat 2012;136:195–207. DOI 10.1007/s10549-012-2230-2
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 098: Moderate alcohol consumption may lower the risk of developing depression — 13 December 2012
Analyses from a prospective study of more than 13,000 adults in Spain related baseline alcohol intake (mainly wine) with the development of depression, with the outcome based on a physician’s diagnosis or on the habitual use of anti-depressant drugs for four or more years. Reported depression was much higher among women than men. Among women, the estimated hazard ratios for groups reporting an average alcohol intake of < 5 g/day of alcohol, 5-15 g/day, and > 15 g/day were 0.97, 0.62, and 0.84 (in comparison with subjects reporting no alcohol). The difference was statistically significant (CI = 0.43-0.89) for the group reporting 5-15 g/day.
Few men reported a diagnosis of depression; among moderately drinking men, the estimated risks of depression were similar to those of women, but none of the differences were statistically different from those of non-drinkers. The investigators found no differences according to the type of alcoholic beverage consumed.
The merits of this study include that the data were collected prospectively, that there were repeated questionnaires seeking data on depression, and that there were a large number of subjects, all of whom were college graduates. There were few men reporting depression, and few heavy drinkers, so results apply only to moderately drinking women. Among these women (those consuming between about ½ drink/day to about 1 or 1 ½ drinks per day) there was evidence of a lower risk of depression during a follow-up period extending up to 10 years.
Forum reviewers thought that this was a well-done analysis, and the use of cut-points for drinking groups according to spline analyses was appropriate. Some reviewers cautioned that moderate drinkers, especially regular wine drinkers, tend to have a large number of other healthy lifestyle habits that could relate to the risk of depression. While many of the recognized potential confounders were included in the Cox regression analysis in this paper, it will be important to determine if future studies support the conclusions of the authors.
Reference: Gea A, Martinez-Gonzalez MA, Toledo E, Sanchez-Villegas A, Bes-Rastrollo M, Nuñez-Cordoba JM, Sayon-Orea C, Beunza JJ. A longitudinal assessment of alcohol intake and incident depression: the SUN Project. BMC Public Health 2012, 12:954 doi:10.1186/1471-2458-12-954
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 097: Per-capita alcohol intake and all-cause mortality in Australia — 4 December 2012
An ecologic analysis from a group in Australia has related trends in the per-capita consumption of alcohol in Australia with rates of all-cause mortality. Unfortunately, the authors do not have data on individual consumption of alcohol (and no way of knowing if the people who drink or do not drink are those who die) and do not have data on many key factors that relate to both alcohol consumption and mortality (e.g., education, income, diet, occupation, etc.). Especially, they have no data on the patterns of consumption of members of the population (regular moderate intake or binge drinking). They “adjust” for death rates in women but do not report sex-specific mortality rates.
This paper illustrates many of the dangers of the so-called “ecologic fallacy,” in which comparisons are made between aggregate population data and biologic outcomes. It has been shown that such comparisons may be of interest in generating hypotheses, but not for answering questions of causation, for which different types of studies are required. As stated in a leading textbook of epidemiology: “Ecologic analysis poses major problems of interpretation when making ecologic inferences and especially when making biologic inferences. In contemporary epidemiology, the ‘ecologic fallacy’ reflects the failure of the investigator to recognize the need for biologic inference and thus for individual-level data. This need arises even when the primary exposure of interest is an ecologic measure and the outcome of interest is the health status of entire populations.”
With such serious limitations from the use of ecologic comparisons, this paper does not provide data upon which alcohol policy can be based. The authors of this paper appear to have ignored previous research providing very different interpretations of an inverse association between per-capita alcohol intake and mortality. A plethora of studies based on alcohol intake among individuals, and especially patterns of consumption, provide data needed for such policy decisions.
Reference: Livingston M, Wilkinson C. Per-capita alcohol consumption and all-cause male mortality in Australia, 1911–2006. Alcohol and Alcoholism 2012. Pre-publication: doi: 10.1093/alcalc/ags123
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 096: Frequency of alcohol consumption and cardiovascular risk factors: implications for drinking guidelines — 20 November 2012
As stated by the authors, “many observational studies suggest that increased drinking frequency is associated with reduced mortality among those with low-dose alcohol consumption. The purpose of this paper was to examine whether frequent drinkers consume lower-risk amounts during drinking days or have favorable risk factor profiles compared with those who drink less frequently, and discuss implications for the larger debate about the limitations of non-randomized studies about ‘moderate’ drinking and the development of low-risk drinking guidelines.” Indeed, previous epidemiologic research has clearly shown that the healthiest outcomes occur among regular, moderate drinkers who do not binge drink. Further, almost all studies have adjusted for a large number of socio-economic factors that are known to be potentially confounding factors for evaluating the association of alcohol consumption with health outcomes.
As expected, the present study shows that regular drinkers tend to consume less alcohol per occasion, and are less likely to binge drink. Further, such individuals tend to have better socio-economic status and lower levels of most cardiovascular risk factors. Most previous researchers have interpreted the better educational status and economic levels of moderate drinkers to be important causes of their more moderate lifestyle factors (including avoiding abusive drinking). Further, most previous research, including many basic science interventions and limited trials in humans, have shown that the administration (intake) of moderate amounts of an alcoholic beverage leads to more favorable cardiovascular risk factors, and numerous mechanisms have been identified (higher HDL-cholesterol, improved vascular reactivity, improved platelet and other coagulation factors, etc.).
The authors of this paper take an unusual turn when it comes to discussing the implications of their results. They tend to down-play any potential health benefits that may be caused by alcohol or the pattern of drinking and infer instead that the favorable risk factors themselves may lead to the drinking pattern. Forum members disagreed with the implications of the authors on a number of factors: (1) the lack of randomized trials of low-dose alcohol consumption; (2) levels of evidence; (3) drinking frequency and alcohol intake; (4) clustering of lifestyle behaviors; (5) alcohol consumption and CVD-related biomarkers; (6) alcohol intake, cancer and total mortality. Further, Forum reviewers cite a large body of scientific research that refutes some of the conclusions of the authors, e.g., that regular moderate alcohol intake does not relate to improved cardiovascular risk factors.
Forum reviewers agree with a concluding statement of the authors about using caution before recommending drinking to the general public. However, they believe that the arguments presented in this paper are not based on a balanced appraisal of available scientific data, and should not be used to support changes in guidelines for the public.
Reference: Naimi TS, Xuan Z, Brown DW, Saitz R. Confounding and studies of ‘moderate’ alcohol consumption: the case of drinking frequency and implications for low-risk drinking guidelines. Addiction 2012; pre-publication. doi:10.1111/j.1360-0443.2012.04074.x.
For the complete critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
A Tribute to Francesco Orlandi
(1927 – 2012)
It is with sadness that we have learned of the death on 12 November 2012 in Ancona, Italy, of Francesco Orlandi, MD. Francesco was a founding member of our International Scientific Forum on Alcohol Research, and a frequent and valuable contributor to our critiques. He will be sorely missed, both as a friend and as a respected scientist. Besides his strong passion for science, he was an extraordinarily cultivated man, rich in his sense of humor, and a sincere friend of many members of our Forum.
Francesco Orlandi was Professor of Gastroenterology at the University of Ancona from 1975 to 1999 and Direttore, Dottorato di ricerca Alimenti e Salute, 1997-99. He also served as Professor on wine and health at the Corso di Laurea Specialistica in Scienze Viticole ed Enologiche at the University of Turin.
Francesco was counselor and coordinator of the “wine and health” group of the Accademia Italiana della Vite e del Vino, and an OIV expert at the Italian Ministry of Agricultural, Food and Forestry Policies in Rome. In addition, he served as Visiting Professor in the Department of Medicine, Albert Einstein College of Medicine, New York, in 1977-8.
Francesco was always interested in the study of the health risks and benefits of alcohol consumption. In the 1990’s, he performed a number of experimental studies in rats on the mechanisms of early ethanol-induced liver damage, with particular attention to apoptosis and cell proliferation.
More recently Francesco became increasingly interested in the beneficial effects of moderate alcohol consumption on human health. He became convinced that only by working in a multi-disciplinary context could young investigators contribute to a new renaissance of alcohol and wine research in Italy. This is why in June, 2011, he organized the first seminar on responsible drinking in the context of the Mediterranean Diet, which was held in the ancient Pontignano Abbey, near Siena. There he brought together all young Italian scientists involved in this field of research; the abstracts of this meeting have been published (Eur J Nutr 2011;50:489–498).
As stated by a Forum member, Francesco was much more than a great doctor and an outstanding scientist. He was an old style gentleman, able to use the right words in every social context. He was an extremely educated person, cultivating interests from art, music, and sailing to science with the emotional motivation, intellectual freedom, and motivated curiosity that usually only young talents can have. Francesco will remain forever a young enthusiastic scientist for all of us who had the fortunate chance of interacting with him.
These comments provided by members of the International Scientific Forum on Alcohol Research (www.bu.edu/alcohol-forum)
15 November 2012
===============================================================================
Critique 095: Effects of alcohol on lymphoma, leukemia, and other types of hematological cancers —- 13 November 2012
Many observational epidemiologic studies have found an inverse association between alcohol consumption and hematological cancers (such as lymphoma and leukemia). This study, based on the Million Women’s Study in the UK, is large enough to permit an evaluation of associations with various types of such cancers. Further, it takes into account newer coding systems for morphology so that diseases associated with the lymphatic system can be separated from those of the myeloid system.
The key findings are that alcohol consumption appears to lower the risk of several types of lymphoma and plasma cell neoplasms, but has little effect on the risk of myeloid tumors such as acute myeloid leukemia. Smoking is associated with an increase in risk for most such cancers.
Forum reviewers considered this to be a very well-done analysis, and the ability of the authors to separate the effects on lymphoid and myeloid cancers is important. Forum members emphasize the strong differences in effect of smoking (an increase) and alcohol consumption (a decrease) on the risk of these cancers. They support future research to discover the mechanisms by which moderate drinking may lower such risk.
Reference: Kroll ME, Murphy F, Pirie K, Reeves GK, Green J, Beral V, for the Million Women Study Collaborators. Alcohol drinking, tobacco smoking and subtypes of haematological malignancy in the UK Million Women Study. British Journal of Cancer 2012;107:879–887.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
A Tribute to Serge Renaud
(1927 – 2012)
It is with sorrow that we have learned of the death in France on 28 October 2012 of Professor Serge Renaud at 84 years of age. In addition to being a colleague and close friend of many of us, he was celebrated as a pioneer in scientific research on the prevention of cardiovascular and other diseases. His innovative mind opened up new fields of inquiry that have greatly broadened research into the role of wine, alcohol, fatty acids, and other nutrients in preserving health and preventing disease. For his many contributions to science, on July 14, 2005, Serge received France’s highest distinction, the Legion d’Honneur.
Over many decades, Professor Renaud was the scientist who initiated much of the work relating the consumption of wine and other types of alcohol to cardiovascular disease and other of the diseases associated with ageing. He was the scientist most associated with the role of red wine in protecting the French from coronary artery disease (the “French Paradox”), and a leading figure in studying how other dietary factors relate to health. His innovative concepts have sometimes taken many years to be appreciated by other scientists. He made a major contribution with his research demonstrating how alpha-linolenic acid, monounsaturated fats, and other components of the “Cretan-type Mediterranean Diet,” play key roles in promoting health.
Serge Renaud was born in Cartelègue, Haute Gironde, France, and after starting his medical training in France moved to Montreal, Canada, and later to Boston, Massachusetts, USA. He returned to France in 1973 and became director of the INSERM unit in Lyon, France, where much of his research was carried out.
In an excellent tribute to Renaud in the Lancet in 2000, Bruno Simini pointed out his major contributions investigating the association between wine, diet, and thrombosis. Simini quotes Serge as saying: “If I hadn’t lived with my grandparents and great-grandparents on a vineyard near Bordeaux, perhaps this idea wouldn’t have occurred to me. When you see people reach the age of 80 or 90 years, who have been drinking small amounts of wine every day, you don’t believe wine in low doses is harmful.”1
In 1991, Serge Renaud appeared on the popular US television program, “60 Minutes,” in a segment entitled the “French Paradox.” When asked by Morley Safer, the host, what was the real reason that the French have rates of coronary artery disease so much lower than those in other developed nations, Renaud replied: “I think it is the alcohol.” And when Morley Safer closed the segment holding a glass of red wine and saying, “The protection of the French from heart disease may rest in this inviting glass,” the response in the US was remarkable – nothing such as this had ever been stated in the country that earlier in the century had made any alcohol consumption illegal through nation-wide prohibition. Following the television program, sales of red wine rose immediately by 40 per cent!
In addition to his studies on wine and alcohol, Professor Renaud, noting the very low rates of heart disease among participants from Crete in the “Seven Countries Study,” initiated the Lyon Diet Heart Study in 1985 to determine the effects of a diet based on that of Crete on the course of disease among patients who already had coronary disease. There were very dramatic reductions in subsequent coronary problems and in total mortality among subjects given the “Cretan-type diet,” which contained increased levels of an omega-3 fatty acid (alpha-linolenic acid) to replace some of the fats from meat and dairy products.
As quoted in the Lancet tribute by Simini, Professor Renaud said the results of these studies on heart disease and cardiac arrhythmias made him “wonder about the origins of civilisations. It is intriguing that ancient Asian and Mediterranean civilisations used natural oils in cooking—colza and olive—with similar fatty acid compositions.” [Colza oil is closely related to the widely used rapeseed oil and canola oil.] And because of his belief in ancient wisdom when it comes to diet and health, Renaud ends his book Le régime santé2 with a warning: “Don’t look for a pill that replaces [the Cretan diet]. There is no such thing.”
People around the world have profited, and will continue to profit, from the lifelong scientific work of Serge Renaud. For those of us who knew and worked with him, we cherish our memories of Serge the person, and of Serge the consummate scientist. As stated so well by a Forum member, “We are all in debt to Serge for the lesson he gave to our scientific community: curiosity as the sole reason to investigate, diligence in observing the facts, unbiased stringency in interpreting results, and, definitely not least, the modesty that only a great man can have. We shall keep him in our memory as an example and a mentor of the meaning of being a scientist.”
References
- Simini B. Serge Renaud: From French Paradox to Cretan miracle. The Lancet 2000;335:48. doi:10.1016/S0140-6736(05)71990-5.
- Renaud S. Le régime santé. Odile Jacob, Paris, 1998.
These comments provided by members of the International Scientific Forum on Alcohol Research (www.bu.edu/alcohol-forum)
31 October 2012
===============================================================================
Critique 094: The complex association between moderate alcohol consumption and breast cancer — 23 October 2012
An excellent review article from two scientists at the National Institue on Alcohol Abuse and Alcoholism describes the epidemiologic and basic scientific evidence linking alcohol consumption to the risk of breast cancer. The authors point out deficiencies in the epidemiologic data, especially that the pattern of drinking (regular moderate versus binge drinking) has generally not been taken into consideration (and the latter pattern can be associated with much higher blood alcohol concentrations). Further, epidemiologic studies usually provide data for only a short period of time, while the development of cancer may relate to exposures over many decades. The authors also comment upon the effect that under-reporting of alcohol by study participants could exaggerate effects on cancer risk from light drinking. They discuss two hypotheses that could relate alcohol to breast cancer risk: alcohol as a breast tumor promoter, and alcohol as a weak cumulative breast carcinogen, and present evidence from epidemiology and basic science that would relate to each hypothesis.
Overall, Forum reviewers were enthusiastic about this review paper, considering that it clearly outlined some of the difficulties scientists have in determining the causes of cancer. They agreed with the authors’ statements regarding the necessity to consider the overall net effects of moderate drinking, including reductions in the risk of cardiovascular disease and total mortality. They also agreed that future epidemiologic studies should focus on the pattern of drinking (and not just the average weekly amount of alcohol), and with their suggestions for future animal studies. One Forum reviewer cautioned that our understanding of the causes of breast cancer is still very incomplete, limiting our ability to provide well-founded recommendations to the public regarding moderate drinking as it relates to breast cancer risk.
Reference: Brooks PJ, Zakhari S. Moderate alcohol consumption and breast cancer in women: From epidemiology to mechanisms and interventions. Alcohol Clin Exp Res 2012; pre-publication: DOI: 10.1111/j.1530-0277.2012.01888.x.
For the full critique of this article by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 093: Is moderate alcohol consumption associated with an increased risk of atrial fibrillation among patients with cardiovascular disease? — 8 October 2012
An analysis of the association of alcohol consumption with the development of atrial fibrillation (AF) among subjects with coronary heart disease, stroke, diabetes, or other manifestations of cardiovascular disease (CVD) was based on subjects in two large antihypertensive drug treatment trials. Previous research in the general population has suggested an increase in the risk of the development of AF for heavy drinkers, and the present study shows such an association among subjects who already have CVD.
Among subjects in this study (all of whom had previous CVD), the authors also report that even “moderate” drinkers had a higher risk of AF than low-alcohol consumers, although the risk of death during follow up of moderate drinkers (9.9%) was lower than that of subjects reporting low-levels of drinking(12.5%). Excluding binge drinkers, the estimated risk of AF was about 13% higher in moderate drinkers than among subjects classified as low-alcohol consumers.
While the multiple analyses in this paper were done appropriately, Forum reviewers were concerned about two aspects of this study. First, there was concern about the wide range the authors chose for the category of “moderate” drinkers, which included subjects reporting from 1 drink per week up through those reporting 21 drinks per week for men and 14 drinks per week for women. It would have been useful to present results also for subjects who met more common definitions for moderate drinking: no more than 14 drinks/week for men and 7 drinks/week for women, the values used to define moderate drinking in the United States, Australia, and many other countries. Unfortunately, there is a conspicuous absence of data in this paper of the effects on the risk of AF of subjects consuming alcohol “moderately” by these standards.
Another major concern about these analyses relates to potential bias in the estimates from what is known as index event bias or collider bias. Given that alcohol intake prior to enrollment in this study may well have related to subjects’ development of cardiovascular disease, it is problematic to judge the effects of alcohol after a cardiovascular event on the subsequent risk of AF, a condition frequently associated with CVD.
All subjects in these analyses had already developed CVD (the prerequisite for being in the present study). Thus, the study included those who consumed alcohol prior to the diagnosis of CVD or diabetes and those who did not drink prior to these diagnoses. Given that moderate alcohol consumption has been shown to reduce substantially the risk of both CVD and diabetes, it can be assumed that subjects in this study who developed CVD despite being drinkers had other risk factors contributing to the disease that overcame any “protection” afforded by alcohol consumption. Unless adjusted for, these other risk factors could well affect the subsequent course of subjects following the onset of CVD, including the development of AF. A similar phenomenon has been seen for obesity (the “obesity paradox”), aspirin use (the “aspirin paradox”), and other exposures, where the associations with CVD seen prior to the initial development of the disease differ from those seen after the development of CVD.
It is clear from many previous studies in the general population that heavy alcohol intake and binge drinking increase the risk of developing atrial fibrillation. This cardiac arrhythmia is a common component of the “holiday heart” syndrome that may occur after very heavy bouts of drinking. As for the effects on the risk of atrial fibrillation from moderate drinking, as studied in this paper, there were a number of concerns from Forum reviewers about the analyses and results. They raise questions about the conclusions of the authors that even “moderate” drinking results in an increased risk of atrial fibrillation after the development of cardiovascular disease. Especially when defined as no more than 14 drinks per week for men or 7 drinks per week for women, the association between “moderate” alcohol consumption and atrial fibrillation remains unclear.
Reference: Liang Y, Mente A, Yusuf S, Gao P, Sleight P, Zhu J, Fagard R, Lonn E, Teo KK; for the ONTARGET and TRANSCEND Investigators. Alcohol consumption and the risk of incident atrial fibrillation among people with cardiovascular disease. CMAJ 2012. DOI:10.1503/cmaj.120412.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 092: The association of alcohol and tobacco with age at diagnosis among subjects with pancreatic cancer — 2 October 2012
This analysis from a group of distinguished scientists supports previous research showing that smoking is associated with an earlier onset of pancreatic adenocarcinoma. Other research has shown that smoking may also be a causative factor in the development of this type of cancer. For alcohol, this study shows that heavy drinking also appears to be associated with earlier diagnosis; previous research from some epidemiologic studies has suggested further that heavy intake of alcohol may be associated with the development of pancreatic cancer.
Forum reviewers were concerned, however, about potential bias in regards to the time of diagnosis of such cancer, and about many other limitations of the study. For example, the inability to separate drinkers by the pattern of drinking (binge drinking versus regular, moderate intake), by the socioeconomic status of subjects, and by a lack of information on chronic pancreatitis, a known risk factor, weaken the implications of this paper. Forum members do not think that the results of this study will have a large impact on clinical practice, or on measures for the prevention of pancreatic cancer.
Reference: Anderson MA; Zolotarevsky E; Cooper KL; Sherman S; Shats O; Whitcomb DC; Lynch HT; et al. Alcohol and tobacco lower the age of presentation in sporadic pancreatic cancer in a dose-dependent manner: A multicenter study. Am J Gastroenterol 2012; advance online publication, doi: 10.1038/ajg.2012.288
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 091: Light drinking may relate to increase in risk for certain cancers — 18 September 2012
A meta-analysis by a distinguished group of scientists was designed to determine if “light drinking” (defined as an average of up to 1 drink per day) was associated with the risk of certain cancers that have been shown in previous studies to be associated with the risk of cancer. The authors concluded that while the risk of these cancers was only slightly increased from such drinking, there were detectable increases in cancers of the oral cavity and pharynx, esophagus and female breast. They report no increase in the risk of cancers of the colorectum, liver, and larynx to be associated with such drinking.
Forum reviewers were concerned about a number of aspects of this study. While the statistical methodology was correct and done appropriately, the fact that the investigators (1) included both ex-drinkers and never drinkers in the reference group; (2) could not separate the effects of regular light drinking from binge drinking; (3) had no data on the duration of alcohol consumption at different levels; (4) did not adjust their analyses according to geographic region or type of study (both of which had large estimated effects on cancer risk); and (5) did not adjust their estimates of effect by other lifestyle habits, including smoking. All of these factors tend to weaken the implications of their results.
Forum reviewers were also concerned that despite the acknowledged limitations of their data, the authors present conclusions indicating that even light drinking increases the risk of certain cancers without commenting on the net health effects. They present only the effects on cancer (which was the topic of the meta-analysis) but do not comment on the overall or net health effects of light drinking: a marked reduction in the risk of much more common diseases, especially cardiovascular diseases, and a longer lifespan. Further, the lack of data on genetic patterns, folate intake, and other lifestyle factors makes it difficult to apply their findings to individual subjects. The Forum considers that while their analyses may be helpful in understanding associations between alcohol and cancer, the many limitations of this study indicate that it can provide only incomplete information on light alcohol consumption to be used as a basis for making recommendations to the public.
Reference: Bagnardi V, Rota M, Botteri E, Tramacere I, Islami F, Fedirko V, Scotti L, Jenab M, Turati F, Pasquali E, Pelucchi C, Bellocco R, Negri E, Corrao G, Rehm J, Boffetta P, La Vecchia C. Light alcohol drinking and cancer: a meta-analysis. Pre-publication: Annals of Oncology 2012; doi:10.1093/annonc/mds337
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 090: Effects of stopping alcohol consumption on subsequent risk of esophageal cancer — 13 September 2012
This paper provides an evaluation of the time following cessation of alcohol consumption that the risk of esophageal cancer returns to that of non-drinkers; it is based on 17 studies providing such information, 9 of which provided data for a meta-analysis. The authors conclude that an alcohol-related increased risk of esophageal cancer is reversible following drinking cessation, most likely requiring up to 16 years. The authors estimate that about one-half of the reduction in risk of cancer may occur within in a much shorter time, perhaps within about 4 or 5 years.
Forum reviewers considered this to be a well-done analysis. Forum members emphasized, as did the authors, a number of limitations of the study. Adjustments for smoking may not have been adequate: most upper aero-digestive cancers show a strong interaction between smoking and alcohol consumption in relation to cancer risk. (For many “alcohol-related” cancers, there is little effect of alcohol consumption among non-smokers.)
Further, large differences in the alcohol-cancer association were shown in this study for different geographical regions (some associations being much higher in Asia than in Europe or North America), but such differences were not adjusted for in the main analyses. The fact that the authors of this paper did not have data permitting the separation of ex-drinkers and never drinkers (both groups being included in the “non-drinker” category), and their inability to judge the effects of the baseline pattern of drinking (regular versus binge drinking), may also be limitations to the interpretation of their results. Adjustment for such factors may have influenced the effects of stopping drinking on subsequent cancer risk, and markedly changed the calculated effects on the numbers of cancers prevented worldwide.
In any case, the fact that cessation of drinking may reduce the risk of esophageal cancer is of importance. Other studies suggest further that just reducing the amount of alcohol consumed, rather than the complete cessation of drinking, may be associated with lowering of cancer risk, and low-level alcohol intake has been shown to have beneficial health effects on cardiovascular disease, diabetes, and other medical conditions.
Reference: Jarl J, Gerdtham Ulf-G. Time pattern of reduction in risk of oesophageal cancer following alcohol cessation — a meta-analysis. Addiction, 107, 1234–1243. doi:10.1111/j.1360-0443.2011.03772.x
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 089: Combination of hormone treatments and alcohol consumption influences the risk of breast cancer in women — 29 August 2012
An analysis among more than 40,000 postmenopausal women who were in the California Teachers Study was carried out to determine if there were differences in risk of breast cancer among women consuming alcohol according to their previous or current use of hormone therapy (HT). In the cohort, 660 women were diagnosed with invasive breast cancer during follow up.
Results from multivariate Cox proportional hazards regression models showed an increase in risk of breast cancer among alcohol consumers of more than 20 grams of alcohol per day (about 1 ½ to 2 typical drinks) who were current users of HT but not among those who were ex-users of HT. The authors conclude: “Following the cessation of HT use, alcohol consumption is not significantly associated with breast cancer risk, although a non-significant increased risk was observed among women who never used HT. Our findings confirm that concurrent exposure to HT and alcohol has a substantial adverse impact on breast cancer risk. However, after HT cessation, this risk is reduced.”
Forum reviewers considered this to be a very well-done analysis on a large group of post-menopausal women with repeated assessments of alcohol consumption and HT use. However, results from even very large studies on the relation between alcohol, HT, and breast cancer risk have often been conflicting. Even with numerous studies on this topic, we still have very poor predictors of which women will develop breast cancer. There is some increase in risk for women with a family history of such cancers and those who are obese. However, the percentage increases in risk associated with HT, alcohol consumption, and other environmental factors are generally small (unlike the many-fold increase in the risk of lung cancer among smokers in comparison with never smokers). This may explain why the results of individual studies may reach apparently conflicting conclusions. While the present study suggests that women who consume alcohol may have a decrease in their risk of breast cancer if they stop taking hormone replacement therapy, our current understanding of factors affecting breast cancer risk remains quite inadequate.
Reference: Horn-Ross PL, Canchola AJ, Bernstein L, Clarke CA, Lacey JV, Neuhausen SL, Reynolds P, Ursin G. Alcohol consumption and breast cancer risk among postmenopausal women following the cessation of hormone therapy use: the California Teachers Study. Cancer Epidemiol Biomarkers Prev 2012. [Epub ahead of print]
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 088: Higher levels of alcohol intake may slightly increase risk of age-related macular degeneration, with no effect from moderate drinking 22 August 2012
An analysis based on the follow up of more than 20,000 participants recruited in 1990-1994 for the Melbourne Collaborative Cohort Study in Australia related alcohol consumption at baseline to the subsequent development of age-related macular degeneration (AMD), a common cause of blindness in the elderly. At a follow-up examination between 2003 and 2007, digital macula photographs of both eyes were taken and evaluated for early and late AMD signs; there were 2,663 cases of early AMD and 121 cases of late AMD identified.
The authors report: “Drinking more than 20 g of alcohol per day was associated with an approximate 20% increase in the odds of early AMD (odds ratio = 1.21, 95% confidence interval: 1.06, 1.38; P = 0.004) when compared with those who reported no alcohol intake at baseline.” (An average of 20 grams/day of alcohol is the equivalent of about 2 daily drinks by British standards or 1 ½ drinks by US standards.) The analyses show that the increased risk was almost exclusively among smokers, with no significant effect among non-smokers who consumed any amount of alcohol.
Forum reviewers had some concern that approximately one-half of this “population-based” study did not have measurements for AMD; these included those who had died during the follow-up period (and deaths were more common among non-drinkers than among drinkers). Further, the authors focus only on the slight increase in risk of AMD seen for heavier drinkers, but do not emphasize that among never smokers there was no increase in risk for consumers of any amount of alcohol. Their results suggest a possible interaction between smoking and alcohol consumption in the etiology of this disease.
The findings of no effect (either positive or negative) from drinking < 20 g/day of alcohol in this study does not support some earlier reports of reduced risk of AMD among moderate wine drinkers. In the present study, there were no detectable differences in effect between the consumption of wine or of beer. A key point of this study may be that never-smokers do not show increased risk of AMD with alcohol consumption.
Reference: Adams MKM, Chong EW, Williamson E, Aung KZ, Makeyeva GA, Giles GG, English DR, Hopper J, Guymer RH, Baird PN, Robman LD, Simpson JA. 20/20—Alcohol and age-related macular degeneration: The Melbourne Collaborative Cohort Study. Am J Epidemiol 2012;176:289-298.
For the full critique of this article by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 087: Smoking increases, while alcohol consumption may decrease, the risk of amyotrophic lateral sclerosis (ALS) — 8 August 2012
Reference: de Jong SW, Huisman MHB, Sutedja NA, van der Kooi, AJ, de Visser M, Schelhaas HJ, Fischer K, Veldink JH, van den Berg LH. Smoking, alcohol consumption, and the risk of amyotrophic lateral sclerosis:A population-based study. Am J Epidemiol 2012;176:233–239
A population-based case-control study of the rare but devastating neurological disease amyotrophic lateral sclerosis (ALS) has shown that the risk of such disease is increased among smokers, as has been shown previously. However, surprisingly, the risk of ALS was found to be markedly lower among consumers of alcohol than among abstainers.
Forum reviewers thought that this was a well-done and important paper, as it is a population-based analysis, with almost 500 cases of ALS, a very large number of cases for this rare disease. They were especially struck by the magnitude of the difference in risk of ALS between alcohol consumers and never drinkers: the risk among drinkers was about one half that of non-drinkers. Said one reviewer: “The results in this study are astonishing in this mysterious disease. One should expect that alcohol, as a toxic agent, rather should contribute to the development of ALS than to prevent it. The lower risk among drinkers compared with non-drinkers is remarkable”
Forum reviewers cautioned that the results of this paper should not be used to prompt people to consume alcohol just to prevent ALS, as it is such a rare disease. However, this paper presents important data that could help scientists understand the etiology of ALS and perhaps other more common diseases.
For the full critique of this paper by members of the International Scientientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 086: Mechanisms for a beneficial effect of moderate alcohol consumption on osteoporosis in women — 1 August 2012
Women after menopause tend to develop weaker bones from what is known as osteoporosis, which may lead to fractures (especially hip fractures) from falling. The weakness of the bones results from an imbalance between the normal resorption (a type of dissolving of old bone) and the laying down of new bone, an ongoing process for both men and women referred to as “bone turnover.” For poorly understood reasons, after menopause the resorption of old bone in women continues but new bone is laid down less well, leading to a decrease in the density of bone. A variety of substances (calcium, vitamin D, various medications) have been used in an attempt to prevent the development of osteoporosis; in epidemiologic studies, moderate drinking of alcohol has been shown to lower this risk.
An intervention trial evaluating the association of alcohol intake with indices of bone metabolism shows beneficial effects of moderate alcohol intake on factors that relate to osteoporosis in post-menopausal women. The authors state that excessive bone turnover, combined with an imbalance whereby bone resorption exceeds bone formation, is the principal cause of post-menopausal bone loss. This study among 40 healthy post-menopausal women investigated the hypothesis that moderate alcohol intake (an average of 19 grams per day, or approximately 1 and ½ typical drinks per day in this study) attenuates bone turnover after menopause. Measurements were carried out while the women were consuming alcohol, after they had stopped drinking as part of the trial, and following resumption of alcohol. The study showed that abstinence from alcohol resulted in increased markers of bone turnover (hence, higher risk of developing osteoporosis), whereas resumption of alcohol reduced bone turnover markers.
Forum reviewers considered this to be an innovative and well-done study. The key questions raised were how alcohol may affect bone metabolism in a longer period of time than was tested in this study. Reviewers realized that such long-term intervention trials are very difficult and expensive to carry out. On the other hand, many prospective epidemiologic studies in the elderly have shown greater bone mineral density and a lower risk of fractures among regular moderate drinkers than among abstainers. The most important aspect of this study may be that it has helped identify cellular mechanisms for the increased bone density observed in post-menopausal women who are moderate alcohol consumers.
Reference: Marrone JA, Maddalozzo GF, Branscum AJ, Hardin K, Cialdella-Kam L, Philbrick KA, Breggia AC, Rosen CJ, Turner RT, Iwaniec UT. Moderate alcohol intake lowers biochemical markers of bone turnover in postmenopausal women. Menopause 2012;19: DOI: 10.1097/gme.0b013e31824ac071
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research and other invited scientists, please click here.
(Note: an ADDENDUM to the original Forum critique has been added on 15 August 2012.)
===============================================================================
Critique 085: Moderate alcohol intake is associated with a lower risk of kidney cancer — 19 July 2012
A majority of previous epidemiologic studies have shown that moderate drinking is associated with a lower risk of kidney cancer, which may affect about 1% of the general population. In published prospective cohort studies, the risk for such cancer among moderate drinkers is usually about 25% less than the risk seen among non-drinkers.
This well-done meta-analysis supports these findings: for the more-reliable prospective cohort studies (rather than case-control studies) the current study finds a 29% lower risk for subjects in the highest category of alcohol consumption in comparison with subjects in the lowest alcohol category. The findings suggest similar effects among men and women, and for all types of alcohol beverages. The effects are seen at a level of about one drink/day, with little further reduction in risk for greater alcohol consumption.
Reference: Song DY, Song S, Song Y, Lee JE. Alcohol intake and renal cell cancer risk: a meta-analysis. British Journal of Cancer 2012;106:1881–1890.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 084: Moderate drinking lowers risk of developing rheumatoid arthritis in women — 17 July 2012
A follow-up study of more than 34,000 women in Sweden has shown that moderate drinkers, in comparison with abstainers, were at significantly lower risk of developing rheumatoid arthritis (RA), an often serious and disabling type of arthritis. RA is known to relate to inflammation, and it is postulated that this is blocked to some degree by the consumption of alcohol. In this study, women who consumed at least 4 drinks per week (with a drink being defined as containing 15 grams of alcohol) had 37% lower risk of developing RA than subjects reporting never drinking or consuming less than 1 drink/week.
This large study is important as few prospective studies are of adequate size to have sufficient cases of RA to evaluate factors related to its development. The study supports previous research showing a lower risk of developing RA, or milder severity of the disease, among moderate drinkers than among abstainers.
Reference: Di Giuseppe D, Alfredsson L, Bottai M, Askling J, Wolk A. Long term alcohol intake and risk of rheumatoid arthritis in women: a population based cohort study. BMJ 2012;345:e4230 doi: 10.1136/bmj.e4230 (Published 10 July 2012)
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 083: Higher indices of quality of life are seen among persistent moderate drinkers than among abstainers — 20 June 2012
Data from a nationally representative sample of 5,404 community-dwelling Canadians ages 50 and older at baseline (1994/1995) was used to estimate the effects of alcohol drinking patterns on indices of quality of life, at baseline (when subjects were aged ≥50 years) and after a follow-up period. Health-related quality of life was assessed with the Health Utilities Index Mark 3 (HUI3). The authors report that most participants showed stable alcohol-consumption patterns over 6 years. Persistent regular moderate drinkers had the highest indices of quality of life at baseline, but subsequent changes in HUI3 were similar in all groups except those reporting decreasing alcohol consumption. The investigators conclude that persistent moderate drinkers had higher initial levels of health-related quality of life than persistent nonusers and those in other groups. However, rates of decline over time were similar for all groups except those decreasing their consumption, which had a greater decline in their level of health-related quality of life than persistent moderate users. While Forum reviewers admired the intent of this study, there were concerns about some of the statistical and epidemiologic aspects. The reasons that some people stopped drinking or decreased their intake were not known; while the authors state that subjects decreasing their alcohol consumption had a more rapid decline in quality of life measures, it is not known what percentage of such subjects decreased alcohol intake due to the development of serious iseases. If this were the case, such diseases may have been more important in their subsequent adverse health than the change in their drinking habits.
Further, the “baseline” quality of life measures in this study were obtained when subjects were aged 50 or older; this baseline value of quality of life was higher in moderate drinkers. However, there are statistical problems if adjustments are made for this when quality of life is assessed subsequently and related to drinking pattern. Peto has described this problem as a “horse-racing effect.” He states that in prospective studies, the correlation between exposures (e.g., drinking pattern) and outcomes (e.g., quality of life) assessments during follow up are likely to be the same as the outcome at the end of follow up. As an analogy he uses a race between ‘slow’ and ‘fast’ horses; it is likely that the fast horses will be ahead at the mid-point of the race as well as at the end. Environmental effects on quality of life begin early in life, and if one adjusts for the mid-life value (as done and referred to as “baseline” in the present study), you may end up disregarding much of the effect of subsequent alcohol intake.
Overall, this study shows a positive relation between moderate alcohol intake and quality of life in middle-aged adults. The effects on the subsequent quality of life as one ages of continued alccohol consumption, or of decreasing intake, remain unclear.
Reference: Kaplan MS, Huguet N, Feeny D, McFarland BH, Caetano R, Bernier J, Giesbrecht N, Oliver L, Ross N. Alcohol Use Patterns and Trajectories of Health-Related Quality of Life in Middle-Aged and Older Adults: A 14-Year Population-Based Study. J. Stud Alcohol Drugs 2012;73:581–590.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 082: A statistical model attempting to estimate the level of alcohol consumption that is “optimal” for health — 6 June 2012
Scientists from Australia and Oxford University have carried out a complex analysis in an attempt to determine the “optimal” level of alcohol consumption that is associated with the lowest rates of chronic disease in the UK. They conclude that the intake of about one-half of a typical drink per day would result in the healthiest outcomes, and the authors conclude that the recommended alcohol intake for the UK should be reduced from the current advised level of drinking.
There were a number of concerns by Forum members about the paper. It is based on an extremely complex statistical model that requires many assumptions, most of which cannot be validated. The parameters chosen to use in such a model determine the results, and a number of instances were identified where the values used in this analysis do not reflect current scientific knowledge. Further, the conclusions of the authors are based exclusively on the lowest point of the “J-shaped” curve for alcohol and disease, and disregard the findings that the risk of death, in comparison with non-drinkers, remains lower for drinkers of alcohol of up to several drinks per day.
There were other aspects of the paper that were of particular concern: (1) focusing only on the average amount of alcohol consumed, while the pattern of drinking (regular moderate versus binge drinking) has the greatest effect on health outcomes; (2) giving a single recommended level of alcohol intake irrespective of age; the greatest risks and lowest expected benefits of alcohol intake are among the young, whereas most of the putative health benefits relate to the diseases of ageing; (3) giving a single value for both men and women, since women are known to react (both adversely and beneficially) to lower levels of alcohol than do men; (4) the use of their estimated value alone for making recommendations for the population; guidelines should be based on a large number of social and behavioral factors, not just on the results of one scientific study.
The level of alcohol that is most likely to be associated with the lowest risk of adverse health outcomes and the most likely health benefits varies markedly among individuals. Middle-aged men and post-menopausal women are most likely to demonstrate enhanced health (e.g., lower risk of cardiovascular diseases, diabetes, dementia) from moderate drinking. For all ages, binge drinking is associated with predominantly adverse outcomes. In general, women should drink less than men. While the analyses presented in this paper are of scientific interest, they alone do not support changes in the current population recommendations for alcohol consumption.
Reference: Nichols M, Scarborough P, Allender S, Rayner M. What is the optimal level of population alcohol consumption for chronic disease prevention in England? Modelling the impact of changes in average consumption levels. BMJ Open 2012;2:e000957. doi:10.1136/bmjopen-2012-000957.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 081: Alcohol intake in the elderly affects risk of cognitive decline and dementia — 22 May 2012
A well-done review paper on the association between alcohol consumption and cognition in the elderly provides an excellent summary of potential mechanisms by which alcohol may affect cognitive function and the risk of dementia, both adversely and favorably. Current scientific data indicate that heavy drinking is associated with an increased risk of neurological disease and dysfunction, while regular light-to-moderate alcohol intake seems to be associated with a reduced risk of such dysfunction, including a lower risk of developing Alzheimer’s disease.
At present, the mechanisms by which the moderate intake of wine and other alcoholic beverages reduces the risk of cardiovascular diseases are much better defined than they are for cognition. Forum members agree with the authors that further research is needed to evaluate a potential role that wine and other alcoholic beverages may play in reducing the risk of dementia. Forum members also agree that, at present, the specific mechanisms of such putative protection are not well defined, and it would be premature to recommend light-to-moderate drinking for reducing the risk of dementia. On the other hand, current epidemiologic and biomedical data suggest that most elderly subjects who are responsible and moderate drinkers would not benefit from being advised to stop their alcohol consumption.
Reference: Kim JW, Lee DY, Lee BC, Jung MH, Kim H, Choi YS, Choi I-G. Alcohol and Cognition in the Elderly: A Review. Psychiatry Investig 2012;9:8-16; On-line: http://dx.doi.org/10.4306/pi.2012.9.1.8
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 080: Modest alcohol intake is associated with less inflammation among patients with the most common type of liver disease, non-alcoholic fatty liver disease (NAFLD) — 15 May 2012
NAFLD (non-alcoholic fatty liver disease) is the most common type of liver disease in the developed world, affecting up to one-third of the US population. NAFLD is often associated with obesity and other parameters of the so-called “metabolic syndrome,” which is a major risk factor for the development of cardiovascular disease. In a well-done study among subjects with NAFLD, the investigators have demonstrated that modest alcohol consumption (an average of up to 20 grams of alcohol per day and no binge drinking) is associated with less evidence of inflammation of the liver (steatohepatitis), a condition known to markedly increase the risk of progression of liver disease to cirrhosis.
Given that NAFLD and other conditions associated with the metabolic syndrome are so common, and are major risk factors for developing cardiovascular disease, the results of the present study are important. They show that modest drinking is associated with decreased, not increased, inflammation of the liver. Further, even among subjects with NAFLD, cardiovascular disease is a much more common cause of death than liver disease. The authors suggest that intervention studies should be done to support their findings; if confirmed, subjects with NAFLD should not be advised to avoid all alcohol, which is the current advice usually given to such patients.
Reference: Dunn W, Sanyal AJ, Brunt EM, Unalp-Arida A, Donohue M, McCullough AJ, Schwimmer JB. Modest alcohol consumption is associated with decreased prevalence of steatohepatitis in patients with non-alcoholic fatty liver disease (NAFLD). Journal of Hepatology 2012 (pre-publication release)
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
A Tribute to Federico Leighton Puga, MD — 8 May 2012
Frederico Leighton Puga, MD, Professor and Director of the Center for Molecular Nutrition and Chronic Diseases of the Catholic University of Chile in Santiago, died on 27 April 2012 at the age of 74 years. Dr. Leighton was a valued member of the International Scientific Forum on Alcohol Research, and was noted for his seminal work in nutrition, antioxidants, the health aspects of moderate wine consumption, and public health approaches for the prevention of chronic diseases.
Many Forum members knew and had worked with Dr. Leighton through many decades. All feel a deep loss, of a great scientist, a loyal and good friend, and someone very concerned with the health of people everywhere. As stated by one Forum member, “Federico was a great scientist motivated by curiosity and the desire to be useful for his country. His culture and education and intellectual rigor were well integrated into his humanity and the sweetness of his character.” Said another: “Federico had in abundance that indefinable quality known as ‘class.’” The world has lost an honest and honorable scientist.
For the full tribute to Dr. Leighton by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 079: Moderate alcohol consumption both prior to, and following, a myocardial infarction is associated with lower risk of mortality — 17 April 2012
In a very well-done analysis based on the follow up of more than 50,000 subjects from The Health Professionals Follow-up Study (HPFS), 1,818 men were confirmed with incident non-fatal myocardial infarction (MI). Among MI survivors, 468 deaths were documented during up to 20 years of follow up. Repeated reports were obtained on alcohol consumption throughout follow up. Average alcohol consumption was calculated prior to and then following the MI.
The overall results show that, in comparison with no alcohol consumption, the pre-MI and the post-MI intakes of light (0.1-9.9 g/day) and moderate (10.0-29.9 g/d) amounts of alcohol were both associated with lower risk of all-cause mortality and cardiovascular morality among these men. The significant reductions in all-cause mortality risk (22% lower for 0.1-9.9 g/day and 34% lower for 10.0 – 29.9 g/day, in comparison with non-drinkers) were no longer present for consumers of ≥ 30 g/day; for this highest consumer group, the adjusted hazard ratio was 0.87 with 95% CI of 0.61-1.25.
There are a number of other informative and interesting results described from this study. First, there was little change in reported alcohol prior to and following the MI: drinkers tended to remain drinkers of similar amounts. Few non-drinkers began to drink after their MI; among heavier drinkers, there was a tendency to decrease the amount somewhat (but very few stopped drinking completely). Further there were no significant differences in outcome according to type of beverage consumed although, interestingly, lower hazard ratios were seen for consumers of beer and liquor than of wine. While the authors state that the effects of alcohol were stronger for the association with non-anterior MIs, the HRs for all-cause mortality were little different: among the moderately drinking men the HRs were 0.58 for anterior MI and 0.51 for other types of MI.
Even though exposures (such as alcohol) for cardiovascular events (such as MI and cardiovascular mortality) may be different after a person has an event than it was before the event, in this study the reductions in risk were almost the same. For example, both for alcohol intake reported prior to a MI, and that after a non-fatal MI, the risk of mortality was about 30% lower for moderate drinkers than it was for abstainers. This suggests that, in terms of reducing cardiovascular disease, alcohol may have relatively short-term effects. Frequent consumption (of moderate amounts) may result in the best health outcomes.
Reference: Pai JK, Mukamal KJ, Rimm EB. Long-term alcohol consumption in relation to all-cause and cardiovascular mortality among survivors of myocardial infarction: the Health Professionals Follow-up Study. European Heart Journal 2012;doi:10.1093/eurheartj/ehs047
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 078: An update on the association of alcohol consumption with risk of breast cancer — 10 April 2012
An excellent review paper on the relation of alcohol consumption to the risk of breast cancer concludes that, overall, there is a positive dose-response relation between alcohol drinking and the risk of breast cancer. The analysis shows that an increase in risk is seen even among women reporting an average of only about one drink/day. Given the high prevalence of such light drinking in most female populations, the authors estimate that up to 1 to 2% of breast cancers in Europe and North America may be attributable to light drinking alone. Thus, while alcohol appears to be a risk factor for breast cancer, it does not explain a very high percentage of cases.
Forum members considered this to be a well-done analysis, with a good review not only of epidemiologic studies but of potential mechanisms of effect of alcohol on breast cancer risk. An increase in estrogen levels from alcohol seems to be the physiologic mechanism most commonly suggested for the increase in risk.
The meta-analysis is noteworthy in presenting risks specifically for women who consume up to one drink/day, which is the common pattern for a high proportion of women in western cultures. On the other hand, the authors herefailed to discuss the potential modification of alcohol effects on cancer risk from folate in the diet; in many studies, high folate levels tend to diminish or eliminate an increase in risk from alcohol. Further, the paper does not provide a discussion of the net effects of moderate drinking on mortality. In older women, the decrease in the risk of cardiovascular disease (a much more common cause of death than breast cancer), greatly exceeds the potential increase in risk of death from breast cancer.
Reference: Seitz HK, Pelucchi C, Bagnardi V, La Vecchia C. Epidemiology and Pathophysiology of Alcohol and Breast Cancer: Update 2012. Alcohol and Alcoholism 2012; doi: 10.1093/alcalc/ags011
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 077: Swedish study supports a “U-shaped” association of alcohol consumption with risk of pre-diabetes and diabetes mellitus — 29 March 2012
Subjects in a cohort in Sweden, some of whom had been exposed to a community intervention program to prevent diabetes, were evaluated 8-10 years after baseline for the presence of diabetes mellitus or impaired glucose metabolism (“pre-diabetes”) in relation to a baseline report of alcohol consumption. Approximately 2,000 men and 3,000 women had a normal glucose tolerance test at baseline; of these 105 men and 57 women developed type II diabetes. Of subjects with pre-diabetes at baseline, 175 men and 98 women progressed to diabetes. The authors report that total alcohol consumption and binge drinking increased the risk of pre-diabetes and diabetes in men, while low consumption decreased diabetes risk in women. However, the authors did not discuss the fact that in essentially all comparisons, the highest risk of diabetes or pre-diabetes was among abstainers.
Forum reviewers had some concerns about the study. For example, the study included some subjects who had been exposed to an intervention trial to prevent diabetes, yet no information is given on potential effects of the intervention. It was not a population-based group. Also, the sample was “enriched” with subjects who had a positive family history of diabetes, which may make it more difficult to judge the effects of environmental factors. Ex-drinkers and never drinkers were included in the abstainer group.
It appears that the authors focused only on the “statistically significant” results rather than commenting on the overall pattern of association (lower risk of developing diabetes for moderate drinkers than for abstainers and heavier drinkers). Further, the number of subjects in many of the sub-groups was very small, making it difficult to define specific cut-points for effects of alcohol on risk.
Nevertheless, reviewers considered that, overall, these analyses support the usual findings from previous research of a “U-shaped curve” for alcohol and diabetes for both men and women. There appears to be a reduction in risk with moderate alcohol intake and possibly an increased risk for heavier drinking.
Reference: Cullmann M, Hilding A, Östenson CG. Alcohol consumption and risk of pre-diabetes and type 2 diabetes development in a Swedish population. Diabet Med 2012;29:441–452. DOI: 10.1111/j.1464-5491.2011.03450.x
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 076: Evaluating the association of alcohol intake with cognitive functioning using a Mendelian randomization study design — 22 March 2012
Many observational cohort studies have shown that moderate alcohol use is associated with better cognitive function. However, since such studies are vulnerable to residual confounding by other lifestyle and physiologic factors, the authors conducted a Mendelian randomization study, using aldehyde dehydrogenase 2 (ALDH2) genotype (AA, GA, or GG) as an instrumental variable in 2-stage least squares analysis. Cognitive function was assessed from delayed 10-word recall score (n = 4,707) and Mini-Mental State Examination (MMSE) score (n = 2,284) among men from the Guangzhou Biobank Cohort Study (2003–2008). The authors had previously reported an association between reported alcohol intake and cognitive function from a larger group of subjects from the same study finding that women reporting occasional alcohol intake and men reporting occasional or moderate intake had better scores related to cognitive function than did abstainers.1
In the present Mendelian study, the authors found no significant association between groups defined by the ALDH2 genotype (as an “unbiased” estimate of alcohol consumption) and the two measures of cognitive functioning. A problem with the present analysis is that ALDH2 genotypes explained only 3% of the variance in reported alcohol intake, which weakens the conclusions of the authors. Further, differences in the predominant type of beverage consumed (rice wine), and probably marked differences in drinking patterns between these subjects and Europeans and Americans, make it difficult to know what the implications of this study are for western industrialized societies.
We agree with the authors that “Causality should be thoroughly verified in a variety of settings using different kinds of evidence, including experimental or genetic studies, rather than relying on simple observations in a particular setting.” We strongly support future attempts at using Mendelian randomization studies, hopefully using better instruments for estimating alcohol intake. On the other hand, as stated by recent evaluations of various study designs for determining causality,3 we appreciate that Mendelian randomization sounds good, but it is not the “Holy Grail.”
Reference: Au Yeung SL, Jiang CQ, Cheng KK, Liu B, Zhang WS, Lam TH, Leung GM, Schooling CM. Evaluation of moderate alcohol use and cognitive function among men using a Mendelian randomization design in the Guangzhou Biobank Cohort Study. Am J Epidemiol 2012; pre-publication release. DOI: 10.1093/aje/kwr462
Please click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 075: Moderate drinking associated with lower risk of stroke in women — 15 March 2012
A well-done analysis from the Nurses’ Health Study shows that the risk of total stroke is slightly lower among light-to-moderate consumers of alcohol than among subjects reporting no alcohol intake. In comparison with non-drinkers, the estimated risk is 17-21% lower for women averaging up to 15 grams of alcohol per day (a little over one drink/day by US definitions of approximately 12 grams of alcohol for a typical “drink.”). For consumers of larger amounts of alcohol, the risk of stroke has a tendency to be slightly increased, but not statistically significantly so.
Data on the pattern of drinking (regularly, binge, etc.) were not reported. Among these predominantly light drinkers, there were no differences between effects on the risk of the most common type of stroke, ischemic stroke (due to atherosclerotic obstruction of a artery or an embolic clot) or the less-common hemorrhagic stroke (bleeding into the brain).
The results, with full adjustment for other factors that may affect risk, suggest a “J-shaped” curve for total stroke, with reductions in risk for light-to-moderate drinking and possibly an increase with greater amounts. In this study, the point at which the risk of drinkers exceeds that of non-drinkers was about 38 grams of alcohol per day (the equivalent of about 3 typical “drinks”), with a 95% confidence interval of 28 to 57 grams/day.
The study supports many previous reports from observational epidemiologic studies that have shown a slight reduction in risk of the ischemic type of stroke from moderate alcohol intake. Some, but not all previous studies, show an increase in hemorrhagic stroke for any amounts of alcohol, but that was not seen in this study, possibly because there were few heavy drinkers in this group of nurses.
Reference: Jimenez M, Chiuve SE, Glynn RJ, Stampfer MJ, Camargo Jr CA, Willett WC, Manson JE, Rexrode KM. Alcohol Consumption and Risk of Stroke in Women. Stroke 2012, pre-publication. http://stroke.ahajournals.org. DOI: 10.1161/STROKEAHA.111.639435
Please click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 074: Does moderate wine consumption improve lung function? — 8 March 2012
An analysis based on a prospective study in the Netherlands assessed the impact of wine and resveratrol intake on lung function. It also studied genetic factors (affecting sirtuin) that have been found to be mechanisms by which resveratrol relates to metabolism and longevity of life. The authors report that resveratrol intake was associated with higher lung volumes and that white wine intake (but not red wine intake) was associated with lower risk of airway obstruction. They report that the genetic factors studied did not relate to the associations found.
While several previous studies (as does this one) have reported that wine intake improves lung function, Forum reviewers were concerned about several aspects of the paper, and especially with the conclusions of the authors that resveratrol was the key factor in improved lung function. A reviewer stated: “Resveratrol may well be just the bystander of something else present in wine.” The beneficial effects on lung function are probably related to many compounds present in wine, and not just resveratrol.
Based on a number of scientific studies, moderate wine intake appears to have a favorable effect on lung function. The doses of resveratrol seen in these epidemiologic studies are in the physiological range that could be expected from moderate wine consumption, unlike the huge doses of resveratrol being evaluated as a potential life-extending drug in pharmaceutical studies.
Reference: Siedlinski M, Boer JMA, Smit HA, Postma DS, Boezen HM. Dietary factors and lung function in the general population: wine and resveratrol intake. Eur Respir J 2012; 39: 385–391; DOI: 10.1183/09031936.00184110
Please click here for the full critique by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 073: The association of alcohol consumption with osteoporosis — 5 March 2012
Osteoporosis is a key underlying factor in fractures among the elderly, which are increasingly a major health problem. A review paper from France on the association between alcohol consumption and bone metabolism states that heavy alcohol intake may adversely affect bone mineral density and increase the risk of osteoporosis. It states that lighter drinking may actually improve bone density, but presents very limited data to support this statement. Forum members were disappointed that the paper did not carry out a meta-analysis or other synthesis of the data; further, data from a number of key epidemiologic studies on the subject were not discussed in the paper.
The paper provides important information on the mechanisms by which alcohol may affect bone metabolism. The authors describe effects of alcoholic beverages on bone density, bone microarchitecture, bone remodeling, and other mechanisms, which help explain how alcohol and polyphenols and other constituents of beer and wine may relate to the risk of fractures in the elderly.
Unfortunately, despite what the authors’ conclude, the paper does not provide a summation of the scientific data upon which public health policy can be based. Overall, current scientific data suggest that bone mineral density and the risk of fractures are favorably affected by light-to-moderate drinking, but adversely affected by heavy drinking and alcoholism.
Reference: Maurel DB, Boisseau N, Benhamou CL, Jaffre C. Alcohol and bone: review of dose effects and mechanisms. Osteoporos Int (2012) 23:1–16; DOI 10.1007/s00198-011-1787-7.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 072: Obesity may modify the association between alcohol consumption and the risk of colorectal cancer. 23 February 2012
A case-control study from Newfound/Labrador has reported that greater alcohol intake may increase the risk of colorectal cancer among obese subjects, but not among non-obese subjects. This is not a particularly large study, and only 45-60% of subjects who were recruited by telephone ended up providing data. Further, it is a case-control comparison, rather than a cohort analysis, making bias in the results more likely.
In this study, there was no relation of alcohol with the risk of CRC when considering the entire population. However, when subjects were stratified by BMI (<30 versus ≥ 30), the data indicate an increase in CRC risk for obese subjects who were “drinkers” (OR=2.2, 95% CI 1.2-4.0), especially among subjects reporting 5 or more drinks/daily (OR=3.7, CI 1.5-9.0). On the other hand, even among obese subjects there was not a clear dose-response effect noted, i.e., there was not a step-wise increase in CRC risk with greater number of drinks/day For example, the odds ratio (OR) was 2.3 times that of non-drinkers for obese subjects reporting 1-2 drinks/daily and 1.3 for those reporting 3-4 drinks/daily.
It will be interesting to determine if other studies show that there is modification of the association between alcohol intake and colorectal cancer by obesity. If such is the case, it could help understand some of the mechanisms for the development of cancer and provide better guidelines for screening for CRC.
Reference: Zhao J, Zhu Y, Wang PP, et al. Interaction between alcohol drinking and obesity in relation to colorectal cancer risk: a case-control study in Newfoundland and Labrador, Canada. BMC Public Health2012, 12:94 doi:10.1186/1471-2458-12-94
Please click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 071: Forum Comments on proposed new dietary guidelines for Australia — 16 February 2012
Members of the International Scientific Forum on Alcohol Research have provided comments on the chapter related to alcohol intake that has been included in “A review of the evidence to address targeted questions to inform the revision of the Australian Dietary Guidelines,” by the Australian Government Department of Health and Ageing and National Health and Medical Research Council (NHMRC), November 2011, ISBN Online 1864965304.
Forum members considered that the authors of the report should be commended on their work. Criticisms are primarily about the restriction in the time frame of the review, and minimal consideration of key nuances, such as quantity of alcohol consumed and its relation to risk or benefit, patterns of drinking, the balance between risks and benefits, and making statements at all when the evidence is too weak. More details (e.g. considering cardiovascular mechanisms to widen the search) would have added weight to the conclusions.
For the full comments of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 070: Potentially important new mechanisms found for the anti-aging effects of resveratrol, a phenolic compound found in red wine — 9 February 2012
A well-conducted experimental study in mice has provided potentially important new insights into the association of the intake of resveratrol and like compounds with health benefits. Resveratrol is a constituent of red wine and other vegetable products, and is being evaluated in high-doses as a pharmaceutical. The biologic mechanisms demonstrated in this study could provide key new approaches for the prevention or treatment of a number of chronic diseases in humans, especially those related to vascular and metabolic diseases and to the risk of mortality.
More than two decades ago, particularly through publicity related to the so-called “French Paradox,” the public became aware of the potential reduction in the risk of coronary heart disease from the moderate consumption of red wine, and the media focused on a single constituent in red wine, resveratrol, as being the “key” factor. We now know that resveratrol is only one of hundreds of phenolic compounds in wine, many of which have been shown to have beneficial effects on vascular function, and that alcohol itself (present in wine, beer or spirits) also provides considerable protection against heart disease. Still, there has remained considerable attention paid to resveratrol, and extensive scientific research on resveratrol and related substances have shown that, in high doses, they may increase longevity of life and reduce metabolic diseases of aging.
In general, Forum reviewers thought that this was a very well-done study. Their concerns related to the dose used in these experiments; while the levels of resveratrol and like compounds might be accessible with pharmaceutical doses, the suggestion that similar levels could be connected with wine consumption is misleading. Further, in humans, resveratrol in the diet will interact with many other chemicals to achieve an effect, as whole plant extracts consist of many active and inactive micronutrients that may play a role in health and disease. To ascribe a specific effect on health from one chemical found in wine or other plant products could be misleading.”
Still, the reviewers believed that this paper was an important contribution to our knowledge about the mechanisms by which resveratrol and other chemicals may play a role in cardiovascular and other diseases. Such knowledge could help develop approaches for the prevention and treatment of human disease and for increasing the longevity of a healthy life.
Reference: Park S-J, Ahmad F, Philp A, Baar K, Williams T, Luo H, Ke H, Rehmann H, Taussig R, Brown AL, Kim MK, Beaven MA, Burgin AB, Manganiello V, Chung JH. Resveratrol ameliorates aging-related metabolic phenotypes by inhibiting cAMP phosphodiesterases. Cell 2012;148:421-433. DOI 10.1016/j.cell.2012.01.017.
Click here for the full critique of this paper by the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 069: Little effect of binge drinking on heart disease or mortality among moderate drinkers in Denmark — 2 February 2012
In a well-done, population-based analysis from Denmark, it was found that subjects who were overall “light-to-moderate” drinkers but reported an episode of “binge drinking” (consumption >5 drinks on an occasion) did not show differences in risk of ischemic heart disease (coronary disease) or total mortality than did other moderate drinkers who did not report such an episode. These results are somewhat different from results of many other epidemiologic studies that have shown increased risk of health problems (even higher risk of coronary disease) to be associated with what was referred to as “binge drinking.”
Why there were no adverse effects of such drinking in the present study has provoked considerable discussion among members of the Forum. The general consensus of opinion has to do with inconsistencies in the definition of “binge drinking.” The rapid consumption of more than 5 drinks on an empty stomach surely has different effects than the consumption of alcohol over several hours with food, such as during a prolonged dinner. The rate of consumption strongly affects the consequences of alcohol; in fact, some have suggested that the consumption of more than 2 or 3 drinks in less than two hours may constitute a better definition of binge that the total number of drinks.
The Forum continues to suggest that “binge drinking,” however defined, is not a healthy pattern of alcohol consumption. But the circumstances of consumption (rate of consumption, with or without food, etc.) may also be important in its definition and in judging its effects on health.
Reference: Skov-Ettrup LS, Eliasen M, Ekholm O, Grønbaek M, Tolstrup JS. Binge drinking, drinking frequency, and risk of ischaemic heart disease: A population-based cohort study. Scandinavian Journal of Public Health 2011;39:880–887.
Click here for the full critique of this study by the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 068. Heavier alcohol consumption may increase risk of colon cancer in people with a family history of such cancer — 30 January 2012
An analysis based on a large number of subjects being followed in the Nurses’ Health Study and the Health Professionals Follow-up Study, relates alcohol consumption to the risk of colon cancer according to whether or not the subjects had a positive family history of colon cancer. Their results indicate that subjects with a family history whose average alcohol intake was 30 or more grams per day (about 2 ½ typical drinks by US standards) have an increase in their risk of colon cancer; there was not a significant association between alcohol and colon cancer among subjects without a positive family history.
Forum reviewers were somewhat concerned that the pattern of drinking (regularly or binge drinking) was not assessed, and that there was not a clear dose-response curve between the level of alcohol consumption and the risk of cancer (i.e., there was not a consistent increase in risk of cancer with greater alcohol intake). Further, folate intake was found to modify the association, with the highest risk for subjects with a positive family history of colon cancer, low levels of folate, and in the highest category of alcohol consumption.
The present study provides some support for an association between higher levels of alcohol intake and the risk of colon cancer among subjects with a positive family history of such cancer. However, there have been changes in the guidelines for screening for cancer (by endoscopy, with removal of pre-malignant tumors) and other preventive measures for people with a positive family history of colon cancer. Such measures could modify the effects of all risk factors for colon cancer in future analyses.
Reference: Cho E, Lee JE, Rimm EB, Fuchs CS, Giovannucci EL. Alcohol consumption and the risk of colon cancer by family history of colorectal cancer. Am J Clin Nutr 2012;95:413–419.
Click here for the full critique of this paper by the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 067: Comparison of effects of red wine versus white wine on hormones related to breast cancer risk 19 January 2012
Aromatase inhibitors (AIs) prevent the conversion of androgens to estrogens, and could play a role in the development of breast cancer. This study of 36 pre-menopausal women consisted of a cross-over intervention trial to determine if there were differences between red wine and white wine in their effects on AIs. Subjects sequentially consumed eight ounces of red wine, followed by white wine (or vice versa), each beverage for a one-month period. The investigators concluded that red wine, but not white wine, was associated with significant effects on some indices of estrogen metabolism; free testosterone and luteinizing hormone were increased, but no significant differences were noted in estrogen levels.
Forum reviewers considered the results interesting and that they contribute to our understanding of the relation of wine to hormonal levels. On the other hand, they were concerned about methodological problems, including a lack of baseline data and variations in the timing during the menstrual period of blood sampling (which could affect estrogen levels). Also, no significant effect of the interventions was seen on blood levels of estradiol.
Further, the Forum thought that it should be pointed out that data are inconsistent on the relation of red wine consumption to the risk of breast cancer; many studies do not show beverage-specific effects on risk. More research will be needed to determine if the polyphenols in red wine can play a role in lowering the risk of breast cancer.
Reference: Shufelt C, Bairey Merz CN, Yang YC, Kirschner J, Polk D, Stanczyk F, Paul-Labrador M, Braunstein GD. Red versus white wine as a nutritional aromatase inhibitor in premenopausal women. J Women’s Health, 2011;DOI: 10.1089/jwh.2011.3001
Click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 066: Is it the alcohol or the polyphenols in red wine (or both) that decrease cardiovascular disease in wine drinkers? 16 January 2012
Human randomized intervention trials of wine and alcohol are not common. This randomized, cross-over study was based on 67 male volunteers in Spain who were considered to be at “high-risk” of cardiovascular disease. The subjects agreed to not consume any alcohol for a baseline period, then for three one-month periods consumed 30 g/day of alcohol as red wine or as gin, or an equivalent amount of phenolics from dealcoholized red wine. The effects of each intervention on a large number of adhesion molecules and chemokines that affect inflammation and relate to the development of vascular disease were evaluated.
The key results of the study were that both ethanol and nonalcoholic compounds in red wine have potentially protective effects that may reduce the risk of vascular disease. Specifically, the authors conclude that “the phenolic content of red wine may modulate leukocyte adhesion molecules, whereas both ethanol and polyphenols of red wine may modulate soluble inflammatory mediators in patients at high risk of cardiovascular disease.” Thus, this study provides important new mechanistic evidence that the reduced risk of cardiovascular disease among red wine drinkers observed in most epidemiologic studies may result from a combination of both the alcohol and the polyphenols in the wine.
Reference: Chiva-Blanch G, Urpi-Sarda M, Llorach R, Rotches-Ribalta M, Guillèn M, Casas R, Arranz S, Valderas-Martinez P, Portoles O, Corella D, Tinahones F, Lamuela-Raventos RM, Andres-Lacueva C, Estruch R. Differential effects of polyphenols and alcohol of red wine on the expression of adhesion molecules and inflammatory cytokines related to atherosclerosis: a randomized clinical trial. Am J Clin Nutr 2012. doi: 10.3945/ajcn.111.022889.
Click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 065: Are there differences in mortality between people consuming wine and those consuming other types of alcoholic beverages? 20 December 2011
Wine consumers, especially in comparison with spirits drinkers, have been shown to have higher levels of education and income, to consume a healthier diet, be more physically active, and have other characteristics that are associated with better health outcomes. However, epidemiologic studies have been inconsistent in showing that, after adjustment for all associated lifestyle factors, consumers of wine have lower risk of cardiovascular disease and mortality than do consumers of other beverages.
A study based on the long-term follow up of a group of older Americans concluded that the associated lifestyle habits and environmental factors of wine consumers largely explained their better health outcomes. Forum reviewers were concerned about some of the methodological approaches used, and believed that the data presented in the paper were inadequate to support such a conclusion. This was a small study, had only a single estimate of alcohol intake (at baseline but not throughout 20 years of follow up), and the authors may have over-adjusted for large differences in lifestyle factors between what they termed as “low-wine” and “high-wine” consumers. The study did confirm a lower mortality risk for alcohol consumers than for non-drinkers.
Experimental studies have clearly indicated that the polyphenols and other constituents that are present in wine and some beers have independent protective effects against most cardiovascular risk factors. Whether or not such advantages are seen among moderate drinkers of wine (or beer) in epidemiologic studies is difficult to determine, as comparisons are not being made between wine, beer, and spirits but between humans who consume one or other such beverage. In almost all populations, drinkers of a specific beverage differ in many ways other than just the type of beverage they consume.
Reference: Holahan CJ, Schutte KK, Brennan PL, North RJ, Holahah CK, Moos BS, Moos RH. Wine consumption and 20-year mortality among late-life moderate drinkers. J Stud Alcohol Drug 2012; 73: 80–88.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 064: Association of lifestyle and environmental factors with the risk of cancer — 13 December 2111
It has been well established that certain lifestyle habits relate to the risk of certain cancers (e.g., smoking and lung cancer). In a well-done analysis, the authors estimate the proportion of cancer in the population associated with a variety of lifestyle and environmental factors. They find that smoking has, by far, the largest effect on the risk of cancer, with 19.4% of cancer cases in the UK attributable to tobacco use. A poor diet (less intake of fruits and vegetables and fiber and greater intake of meat and salt), obesity, and alcohol are the next most important factors that relate to cancer, with alcohol being calculated to relate to 4.0% of cancer cases in the UK.
Forum reviewers considered this to be a well-done paper that used epidemiologic methods that are preferable to those used in some previous such analyses. Generally, they disagreed with the authors that no alcohol consumption was the theoretical “optimum exposure level,” as the risk of certain cancers seems to increase primarily from heavy drinking. Further, they found reason to believe that the purported effects related to diet may have been over-estimated.
Nevertheless, this paper provides considerable new information on lifestyle and environmental factors that may relate to the risk of cancer. It puts into perspective the importance of targeting certain behaviors for the potential reduction in the risk of cancer.
Reference: Parkin DM, Boyd L, Walker LC. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. Summary and conclusions. British Journal of Cancer 2011;105:S77 – S81.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 063: Genes modify the risk of liver disease among alcoholics — 5 December 2011
It has been widely observed that only a small percentage of alcoholics develop cirrhosis of the liver, the most advanced form of alcoholic liver disease (ALD); the reason why all alcoholics do not develop such disease is not known. The present study from Spain, that includes original work and a meta-analysis, evaluates whether genetic polymorphisms that determine levels of glutathione-S-transferases (GST) relate to the risk of developing ALD among alcoholics. Alcoholics with certain genetic GST polymorphisms were found to be at significant excess risk for such liver disease in comparison with alcoholics without these polymorphisms.
As stated by the authors, the theory that these enzymes may affect risk is based on the ability of certain GST alleles to detoxify harmful ethanol metabolites in the liver by conjugating acetaldehyde and ROS to reduced glutathione. The specific polymorphisms that they found to be associated with increased liver disease are among those that would be expected to lower the activity of the corresponding GST enzymes; this would permit higher levels of toxic metabolites of alcohol and oxidative stress to be present for longer periods of time after excessive alcohol consumption.
Some Forum reviewers thought that while the study was well done, the authors were unclear as to how these data could directly lead to “potential therapeutic targets” for liver disease in alcoholics. Nevertheless, the original study and meta-analysis provide important data on how specific genetic factors relate to the development of liver disease among alcoholics and could theoretically lead to better strategies for the prevention and treatment of alcoholic liver disease.
Reference: Marcos M, Pastor I, Chamorro A-J, Ciria-Abad S, González-Sarmiento R, Laso F-J. Meta-analysis: glutathione-S-transferase allelic variants are associated with alcoholic liver disease. Aliment Pharmacol Ther 2011;34:1159–1172.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 062: Similar effects of beer and wine on the risk of cardiovascular disease and of total mortality — 22 November 2011
The authors carried out an updated meta-analysis on the relationship between wine, beer or spirit consumption and cardiovascular outcomes, using state-of-the-art statistical techniques. Their meta-analysis provides evidence of J-shaped relationships between both wine and beer intake and vascular risk, with maximal protection of about 33% at a level of 25 g/day of alcohol (approximately 2 drinks/day by US standards). A statistically significant association between spirits intake and vascular disease was not found.
The key result of this meta-analysis is the finding of a very similar inverse association between the consumption of beer and the consumption of wine in relation to cardiovascular outcomes. While a similar associationwas not seen for spirits consumption, the data presented do not permit the conclusion that the key effects on cardiovascular disease are primarily due to the polyphenols in beer and wine. Similarly, the results do not permit the conclusion that the effect on cardiovascular disease is due primarily to the alcohol in these beverages. The lack of a similar J-shaped association for spirits may have been due to different drinking patterns (e.g., more binge drinking among consumers of spirits), as the pattern of drinking was not included as a confounder in the analyses.
Reference: Costanzo S, Di Castelnuovo A, Donati MB, Iacoviello L, de Gaetano G. Wine, beer or spirit drinking in relation to fatal and non-fatal cardiovascular events: a meta-analysis. Eur J Epidemiol 2011;DOI 10.1007/s10654-011-9631-0
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
A response from the Alcohol Policy Coalition of Australia to the Forum Critique #058: “A misguided statement on alcohol and health from a coalition in Australia,” which was published on the Forum web-site on 28 September 2011.
The Alcohol Policy Coalition of Australia has provided a response to Forum critique #058, “A misguided statement on alcohol and health from a coalition in Australia,” that was published on the Forum web-site on 28 September 2011.
The original Forum critique is available under Recent Reviews, #058 (click Critique o58). A description of the Forum, its members, the goals of the Forum, a disclosure statement, etc., are available from the home page of the web-site.
The response from the Alcohol Policy Coalition is now published in full on our web-site, dated 18 November 2011. To read the response to our critique # 058 provided by the Alcohol Policy Coalition, please click here.
===============================================================================
Critique 061: The reduction in risk of coronary heart disease from alcohol consumption may involve mechanisms other than an increase in HDL-cholesterol. 10 November 2011
In a prospective, observational study of approximately 150,000 Norwegians, the investigators found that alcohol consumption was associated with a large decrease in the risk of death from coronary artery disease. For men, the fully adjusted hazard ratio for cardiac death was 0.52 (95% CI 0.39 – 0.69) when comparing subjects reporting more than one drink/week in comparison with those reporting never or rarely drinking; for women, it was 0.62 (0.32–1.23). There was little change in the hazard ratio when HDL-cholesterol (HDL) was added to the model, suggesting that very little of the lower risk of heart disease was due to an increase in HDL from alcohol consumption.
Forum members considered this a well-done analysis. They were surprised at the very low amounts of alcohol intake reported by the subjects, with only 16% of males and about 8% of females reporting more than one drink/week. It is possible that the low levels of drinking, or perhaps over-adjustment in the multivariable analysis, led to the lack of effect of HDL. Most other studies have shown a much larger proportion of the effect of alcohol on heart disease risk to be associated with an increase in HDL.
Reference: Magnus P, Bakke E, Hoff DA, Høiseth G, Graff-Iversen S, Knudsen GP, Myhre R, Normann PT, Næss Ø, Tambs K, Thelle DS, Mørland J. Controlling for High-Density Lipoprotein Cholesterol Does Not Affect the Magnitude of the Relationship Between Alcohol and Coronary Heart Disease. Circulation 2011;124: DOI: 10.1161/CIRCULATIONAHA.111.036491
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 060: A new analysis from the Nurses’ Health Study on the association of alcohol with risk of breast cancer 3 November 2011
In a well-done analysis using prospectively collected data from the Nurses’ Health Study, the risk of breast cancer was found to be modestly increased among consumers of alcohol, even those whose total alcohol consumption was reported to be in the range of 3 to 6 drinks/week. Similar small increases in the risk of breast cancer have been found from alcohol consumption in the majority of previous studies observational studies. A strength of this study was the very large number of subjects, permitting the investigators to attempt to determine if both the amount of alcohol and the frequency of consumption were important in this association; strong effects were not found for either. A weakness is the failure to report the effects of folate intake on the association between alcohol and cancer; the same investigators have previously shown that folate is a potential moderator of the effects of alcohol on breast cancer risk.
The authors describe well the dilemma that women face regarding alcohol intake, which may increase slightly the risk of breast cancer but markedly decrease the risk of other more common diseases, especially cardiovascular conditions. For example, the authors state that regarding breast cancer, “We did find an increased risk at low levels of use, but the risk was quite small.” Forum members agree with the statement of the authors that “An individual will need to weigh the modest risks of light to moderate alcohol use on breast cancer development against the beneficial effects on cardiovascular disease to make the best personal choice regarding alcohol consumption.”
Reference: Chen WY, Rosner B, Hankinson SE, Colditz GA, Willett WC. Moderate alcohol consumption during adult life, drinking patterns, and breast cancer risk. JAMA 2011;306:1884-1890.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 059: Association of quantity of alcohol and frequency of consumption with cancer mortality
20 October 2011
A paper from the National Institutes of Health in the United States attempts to evaluate the separate and combined effects of the frequency of alcohol consumption and the average quantity of alcohol per occasion as they relate to the risk of mortality from all cancers, as well as cancer-specific mortality. It is based on repeated administrations of the National Health Interview Survey in the United States, with a total of more than 300,000 subjects and over 8,000 deaths from cancer, and reports on total cancer deaths and deaths from lung, colorectal, prostate, and breast cancers.
For total alcohol consumption (frequency x quantity), the data indicate a significant reduction in the risk of all-site cancers (RR=0.87, CI 0.80-0.94) which, interestingly, is not emphasized by the authors and is not included in their abstract. Moderate drinking consistently shows no effect, and only heavier drinking is associated with an increase in all-site cancer risk. For site-specific cancers, an increase in risk of lung cancer was seen only for heavier drinkers, with a tendency for less cancer among light drinkers. There was no evidence of an effect of total alcohol consumption on colorectal, prostate, or breast cancer.
The authors excluded non-drinkers in a second analysis in which they used categories of usual daily quantity and of frequency of consumption in an attempt to investigate their separate effects. For all-site cancer and for lung cancer, these results again show an increase in risk only for drinkers reporting greater amounts of alcohol. The data also show an increase in cancer risk from more frequent drinking among women but not among men. For colorectal, prostate, and breast cancer, there is no clear pattern of an increase in risk from quantity of alcohol consumed. For frequency of drinking, again there is a suggestion of an increase in risk with more frequent drinking, although the trends are not statistically significant.
The overall message of this analysis is that light to moderate alcohol intake does not appear to increase the risk of all-site cancer (and light drinking was shown in this study to be associated with a significant decrease in risk). Similarly, light to moderate consumption was not associated with site-specific cancers of the lung, colorectum, breast, or prostate. Heavier drinking is known to be associated with a large number of adverse health effects, including certain cancers, as was shown in this study.
When considering cancer, alcohol consumption should not be considered in isolation, but in conjunction with, other lifestyle behaviors (especially smoking). We agree with the authors that both quantity and frequency of consumption need to be considered when evaluating the relation of alcohol to cancer; further, beverage-specific effects need to be further evaluated.
Reference: Rosalind A. Breslow RA, Chen CM, Graubard BI, Mukamal KJ. Prospective study of alcohol consumption quantity and frequency and cancer-specific mortality in the US population. Am J Epidemiol 2011; DOI: 10.1093/aje/kwr210.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 058: A misguided statement on alcohol and health from a coalition in Australia. 28 September 2011
A group known as the Alcohol Policy Coalition in Australia has released a document entitled Cancer, Cardiovascular Disease and Alcohol Consumption. Forum members agree that excessive alcohol use has many adverse effects on the individual and on society, and efforts to reduce such use are important. On the other hand, they were disturbed that the coalition statement was limited almost exclusively to the effects of abusive drinking, was based primarily on extremely limited sources of information (mainly position statements by other organizations, and not publications based on sound research), and indicated a strong bias against alcohol.
Forum members contend that the Australian report misrepresents the extensive scientific data available on alcohol and health. The report specifically ignores scientific data indicating that in all developed countries, moderate consumers of alcohol are at much lower risk of essentially all of the diseases of ageing: coronary heart disease, ischemic stroke, diabetes, and dementia. And conspicuously absent from the Australian report is a description of the lower total mortality among middle-aged and elderly people associated with moderate alcohol consumption, a finding that has been found consistently throughout the world. Further, there is no mention in the report of the key relevance of the pattern of drinking, although regular moderate drinking (versus binge drinking only on week-ends, even when the total volume of alcohol is the same) has been shown to be a strong determinant of beneficial effects of alcohol consumption.
Scientific data over many decades have shown that while excessive or irresponsible alcohol use has severe adverse health and societal effects, regular moderate drinking is associated with beneficial effects on health. And a very large number of experimental studies, including results from human trials, have described biological mechanisms for the protective effects of both alcohol and the polyphenolic components of wine.
There have been a number of comprehensive meta-analyses published that Forum members believe can provide much more accurate, up to date, and scientifically balanced views of the current status of the health effects of alcohol consumption. Such documents are better sources of data upon which policy decisions should be based.
Reference: Alcohol Policy Coalition Position Statement. “Cancer, Cardiovascular Disease and Alcohol Consumption.” Released in Australia, September 2011.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 057: Differences in effects on atherosclerosis of regular moderate drinking and binge drinking. An experimental study in mice. 20 September 2011
An excellent study among experimental animals has reported very dramatic differences between the effects of alcohol administered in moderation on a daily basis and the same total weekly amount of alcohol administered on only two days of the week: binge drinking. The mice used in the study that were given regular moderate amounts of alcohol showed no weight gain, improved lipid values, and much less development of atherosclerosis than did control animals. However, those given alcohol in a binge-drinking pattern showed worse outcomes than control animals, and much worse outcomes than those given regular moderate alcohol.
This experimental study provides strong support for the frequent finding among humans in epidemiologic studies: benefits from regular moderate drinking, adverse effects from binge drinking. It is especially important since, being an experimental study, the potential confounding effects of other lifestyle habits are not an issue, as is always the case for observational studies among humans.
Reference: Liu W, Redmond EM, Morrow D, Cullen JP. Differential effects of daily-moderate versus weekend-binge alcohol consumption on atherosclerotic plaque development in mice. Atherosclerosis 2010, doi:10.1016/j.atherosclerosis.2011.08.034
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 056: Relation of alcohol consumption to colorectal cancer 13 September 2011
A meta-analysis of case-control and cohort studies on the association of alcohol consumption with colorectal cancer was carried out, based on 22 studies from Asia, 2 from Australia, 13 from Western Europe, and 24 from North America. The paper provides evidence that alcohol, at least at higher levels of consumption, is associated with an increase in the risk of colorectal cancer. Overall, there was no increase in the risk for consumers reporting an average intake of up to 1 drink per day, but a modest increase (of 21%) for what the authors defined as “moderate drinking” (averaging up to 49.9 g of alcohol, or about 4 typical drinks, per day). The increase in risk was greater (52%) for consumers of 50 or more grams of alcohol per day.
Forum reviewers thought that this was, in general, a very well-done study that used appropriate statistical techniques for meta-analysis. There were some key concerns, however, including the following: (1) the authors’ definition of “moderate drinking” extended well above the usual recommended limits for sensible drinking; effects of consumption in categories of 1 to 2 drinks/day, 2 to 3 drinks/day, etc., were not given; (2) no results were provided according to type of beverage even though many previous studies have shown differences between health effects for consumers of wine, or wine/beer, and other beverages; and (3) no data were available on the pattern of drinking. Many studies have shown that regular, moderate drinking on most days of the week has very different health outcomes than drinking only on week-ends or binge drinking.
Despite these concerns, Forum members agreed that current data indicate that alcohol intake, especially heavier drinking, is associated with an increase in the risk of colorectal cancers. Future studies are needed to help determine if there is a threshold level of alcohol that increases the risk, if there are differences by type of beverage, and if the pattern of drinking (regular versus binge drinking) affects the risk.
Reference: FedirkoV, Tramacere I, Bagnardi V, Rota M, Scotti L, Islami F, et al. Alcohol drinking and colorectal cancer risk: an overall and dose–response meta-analysis of published studies. Annals of Oncology 22: 1958–1972, 2011, doi:10.1093/annonc/mdq653
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 055. Alcohol intake and “successful ageing” 8 September 2111
Among 13,894 women in the Nurses’ Health Study, investigators prospectively examined alcohol use assessed at midlife in relation to “successful ageing,” which was defined as survival to age 70 years, not having a major chronic disease (such as coronary disease, cancer, stroke, diabetes), and having no major cognitive impairment, physical impairment, or mental health problems. Only 11% of the women met these criteria.
The results indicate that moderate drinkers, especially those consuming wine and drinking regularly, were more likely to exhibit successful ageing. For average amount consumed, the largest benefit (an increase of 28%) was among women who reported 15.1 – 30 g of alcohol per day (an average of just over 1 to 2 ½ drinks per day), when compared with non-drinkers. The frequency of drinking was especially important: in comparison with nondrinkers, women who drank only on 1 to 2 days per week had little increase in their risk of successful ageing, but those drinking on at least 5 days per week had almost a 50% greater chance of successful ageing.
Forum reviewers had some questions about the definition of “successful ageing” used in this study. It is believed that a much greater percentage of people who may not meet these criteria make huge contributions to society and should be considered “successful.”
In summary, these results support the findings of earlier studies showing that many aspects of successful ageing, in addition to just survival, are favorably affected by regular, moderate consumption of alcohol.
Reference: Sun Q, Townsend MK, Okereke OI, Rimm EB, Hu FB, Stampfer MJ, Grodstein F. Alcohol consumption at midlife and successful ageing in women: A prospective cohort analysis in the Nurses’ Health Study. PLoS Med 8(9): e1001090. doi:10.1371/journal.pmed.1001090
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 054. Role of alcohol intake and smoking on upper aerodigestive cancers – 6 September 2011
This paper provies an extensive analysis of the proportion of the risk of upper aero-digestive tract (UADT) cancers in the population (the population attributable risk) may be due to alcohol consumption and/or smoking. The analyses provide strong evidence that smoking is the most important factor in the risk of these cancers, and the risk is enhanced among those who also consume 2 or more drinks per day. Alcohol alone (i.e., among non-smokers) has little effect on the risk.
The authors state that their observations “are consistent with the hypothesis that alcohol acts as a carcinogen primarily because of its promoting effect on tobacco smoke.” In terms of the population-attributable risk, the authors conclude that “Our findings confirm that tobacco and alcohol together explain 73% of total UADT cancer burden in Europe.” Overall, tobacco use alone explained 28.7%, the combination of smoking and drinking 43.9%, and alcohol use alone only 0.4% of the population attributable risk. Among women, the risk of these cancers was higher among smokers than among those who both smoked and consumed alcohol; this perhaps suggests that the moderate intake of wine, the most common beverage among European women, may play a role in reducing the risk associated with smoking.
Forum reviewers thought that this was a very good paper, but hoped that in the future we would have more studies that evaluated the effects on risk of varying levels of alcohol consumption, differential effects of various beverages, and even differential effects according to subjects’ genetically determined differences in alcohol metabolizing enzymes.
Reference: Anantharaman D, Marron M, Lagiou P, Samoli E, Ahrens W, Pohlabeln H, et al. Population attributable risk of tobacco and alcohol for upper aerodigestive tract cancer. Oral Oncology 2011;47:725–731.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 053: An extensive review of the effects of alcohol consumption on the risk of cognitive impairment and dementia 25 August 2011
The authors of this paper have carried out an excellent review of the relation of alcohol consumption to the risk of cognitive impairment and dementia. They reviewed a total of 143 previous publications on the topic. There were 74 studies, based on a total of more than 250,000 subjects, that provided risk estimates for varying levels of alcohol consumption which allowed the investigators to include them in a comprehensive meta-analysis. These papers were published mainly after 1998, were predominantly among older subjects (92% were ≥ 55 years of age and 70% ≥ 65 years of age), and almost all employed mental status examinations to define cognitive impairment/dementia.
As stated by the authors, “These studies overwhelmingly found that moderate drinking either reduced or had no effect on the risk of dementia or cognitive impairment.” Overall, in the new meta-analysis based on these studies, the average ratio of risk for cognitive risk associated with moderate drinking of alcohol was 0.77, with nondrinkers as the reference group. This estimate is close to the estimates of reduction in the risk of cognitive dysfunction (RR of 0.73 and 0.74) seen in other recent selective meta-analyses. The present study found that both light and moderate drinking provided a similar benefit, but heavy drinking was associated with non-significantly higher cognitive risk for dementia and cognitive impairment.
Forum reviewers of this paper were particularly pleased that the authors attempted to answer a number of specific questions on this topic that have been raised from previous research. Their results included finding no appreciable differences whether or not “sick quitters” were included in the reference group, little effect from adjustments for other lifestyle factors, and no significant differences between alcohol’s effects on dementia, Alzheimer’s dementia, or vascular dementia (but, based on a small number of studies, no significant reduction in risk of cognitive decline over time). The investigators concluded that there were no differences between results in men and women. Their analyses also led to the conclusion that wine is associated with more beneficial effects on cognition than beer or spirits, but the authors caution that these results are based on a limited number of reports, and that many studies show no significant differences according to type of beverage.
Forum reviewers agreed with the conclusions of the authors that “Overall, light to moderate drinking does not appear to impair cognition in younger subjects and actually seems to reduce the risk of dementia and cognitive decline in older subjects.”
Reference: Neafsey EJ, Collins MA. Moderate alcohol consumption and cognitive risk. Neuropsychiatric Disease and Treatment 2011:7:465–484.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 052: Does moderate alcohol consumption increase body weight? 16 August 2011
A paper from Spain provides an extensive review of the association between alcohol consumption and body weight. It includes descriptions of cross-sectional and prospective studies (and a few small intervention studies) among subjects who varied in age (adolescence to old age), culture (from Americans and Europeans to Asians), and principal type of beverage consumed and pattern of drinking. The authors state that many of the studies they reviewed appear to be contradictory in their results. However, based on their review, they conclude that “as positive associations between alcohol and weight gain were mainly found in studies with data on higher levels of drinking, it is possible that an effect on weight gain or abdominal adiposity may only be experienced by heavy drinkers.” A second conclusion of the authors is that “the type of alcoholic beverage might play an important role in modifying the effect of alcohol consumption on weight gain,” with more favorable effects generally seen among consumers of wine. A formal meta-analysis is not provided. Forum members were uncertain whether the higher risk seen for spirits drinkers in this study was due to the beverage they chose or to their consumption of larger amounts of alcohol.
The overall conclusions of the authors is that it is currently unclear whether alcohol consumption a risk factor for weight gain, but if so it appears to occur mainly among heavier drinkers. They also state that “light-to-moderate alcohol intake, especially of wine, may be more likely to protect against, rather than promote, weight gain.”
Forum reviewers agreed with most of the conclusions of the authors, especially that current data do not clearly indicate if moderate drinking increases weight; further, the biologic mechanisms relating alcohol to changes in body weight are not well understood. The Forum review comments on the strong protective effects of moderate drinking on the risk of metabolic syndrome and diabetes, both of which relate to increasing obesity. And some studies suggest that even very obese people may be at lower risk of diabetes if they are moderate drinkers. Forum members also reviewed some of the distinctive mechanisms by which alcohol is metabolized in the body (it provides calories that are rapidly absorbed and are not stored in fat) that could explain differences in the effects of calories from alcohol and from other foods.
Forum members agree with the authors of this paper that future research efforts should be directed towards assessing the specific roles of different types of alcoholic beverages, taking into account drinking patterns, and perhaps including in the analysis the propensity of individual subjects to gain weight in the past. For now, there is little evidence that someone consuming small to moderate amounts of alcohol on a regular basis is increasing his or her risk of becoming obese.
Reference: Sayon-Orea C, Martinez-Gonzalez MA, Bes-Rastrollo M. Alcohol consumption and body weight: a systematic review. Nutrition Reviews 2011;69:419-431.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 051: Types of alcohol in relation to acute pancreatitis 11 August 2011
A very well-done analysis from scientists in Sweden has related the type of alcoholic beverage, and the amount consumed per occasion, to the risk of acute pancreatitis. The study suggests that a greater number of drinks per occasion (“binge drinking”) of spirits increases the risk of acute pancreatitis, but no such relation was seen for the consumption of beer or wine. Forum reviewers suggested that a faster rate of drinking, with a greater rise in BAC, for spirits drinkers may be an important factor in the observed higher risk of pancreatitis; the increased risk may not necessarily be due to lower levels of antioxidants or to the presence of other toxic substances in spirits.
In any case, the average total alcohol consumption did not affect the risk of pancreatitis; instead, it was the number of drinks consumed per occasion (of spirits, in this study) that was associated with an increase in risk. Residual confounding by the pattern of drinking, diet, or by other lifestyle factors could still be operating, and it will require replication of these results in other studies to support the conclusions of the authors.
Reference: Azodi OS, Orsini N, Andrén-Sandberg Å, Wolk A. Effect of type of alcoholic beverage in causing acute pancreatitis. Brit J Surgery 2011;DOI: 10.1002/bjs.7632.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 050: Multiple maternal risk factors for fetal alcohol disorders 7 August 2011
An extremely well researched and written review on the relation of maternal drinking during pregnancy to adverse fetal outcomes has been published by scientists from the University of New Mexico Center on Alcoholism, Substance Abuse, and Addictions. It covers many factors (host, agent exposure, and environment) that have been found to relate to the occurrence of fetal alcohol spectrum disorders (FASD). Such factors modify the risk associated with alcohol consumption during pregnancy, although the risk of abnormalities is clearly increased with frequent consumption of large amounts of alcohol, and is greater among women who are alcoholics. While current data do not show that light or occasional alcohol consumption during pregnancy increases the risk of FASD, Forum members do not believe that pregnant women should be encouraged to drink.
Forum members agree with the authors that “More research is needed to more clearly define what type of individual behavioral, physical, and genetic factors are most likely to lead to having children with FASD.” Evaluating these multidimensional factors should help identify women at particular risk for having a child with FASD and lead to interventions to prevent such fetal abnormalities.
Reference: May PA, Gossage JP. Maternal risk factors for fetal alcohol spectrum disorders. Not as simple as it might seem. Alcohol Research & Health 2011;34:15-26.
For the full critique of this article by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 049: Effects of smoking and alcohol use on risk of upper aero-digestive cancers 1 August 2011
A case-control analysis from subjects living in areas of South America with high rates of upper aero-digestive tract cancers showed that both alcohol consumption and smoking tended to increase the risk of such cancers. However, the predominant cause of these cancers was the combination of smoking and alcohol consumption, with much higher risk than either exposure alone. The effects on risk were greater for smoking than for alcohol: for non-smokers, there was little effect of alcohol on risk. For non-drinkers, the risk of cancer associated with smoking was still increased, but was lower than it was for current drinkers.
An especially important finding in this study was that, among ex-drinkers and former smokers, the increased risks associated with alcohol and tobacco use decreased steadily as the time since quitting increased. As stated by the authors, most of these cancers “could be prevented by quitting the use of either of these two agents.”
Reference: Szymańska K, Hung RJ, Wűnsch-Filho V, Eluf-Neto J, Curado MP, Koifman S, Matos E, Menezes A, Fernandez L, Daudt AW, Boffetta P, Brennan P. Alcohol and tobacco, and the risk of cancers of the upper aerodigestive tract in Latin America: a case–control study. Cancer Causes Control (2011) 22:1037–1046. DOI 10.1007/s10552-011-9779-7
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 048: A new report on drinking guidelines and the association of alcohol with risk of cancer. 18 July 2011
The Canadian Medical Association Journal has published a commentary by some French scientists relating drinking guidelines to the association between alcohol and cancer. They conclude that the current guidelines for sensible drinking for the general population are not adequate for the prevention of cancer, and revisions and eventual exclusion of such guidelines are needed.
Forum reviewers agree that alcohol consumption, especially heavy intake, increases the risk of certain types of cancer. However, they consider that the opinions of the authors in the paper (labeled as an “Analysis” rather than an editorial or comments) do not reflect current sound scientific data, that the report is highly selective in citing a small number of papers that support their opinions, and that the authors have ignored a huge amount of recent data from more scientifically sound research that have largely discredited such studies. Further, the report provides no mention of the consistent finding from studies around the world that moderate drinkers tend to have lower all-cause mortality risk than do abstainers.
Scientific data over many decades have shown that excessive or irresponsible alcohol use has severe adverse health effects, including an increase in the risk of certain cancers. On the other hand, moderate drinking is associated with lower risk of cardiovascular disease and many other diseases of ageing and with all-cause mortality. A very large number of experimental studies, including results from human trials, have described biological mechanisms for the protective effects of alcoholic beverages against such diseases. A number of comprehensive meta-analyses provide much more accurate, up to date, and scientifically balanced views than does the current paper; such documents may be better sources of data upon which guidelines to the public regarding alcohol consumption should be based.
Reference: Latino-Martel P, Arwidson P, Ancellin R, Druesne-Pecollo N, Hercberg S, Le Quellec-Nathan M, Le-Luong T, Maraninchi D. Alcohol consumption and cancer risk: revisiting guidelines for sensible drinking. CMAJ 2011. DOI:10.1503. /cmaj.110363
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 047: Overall health effects of alcohol consumption. Comments on a WHO report 10 July 2011
The World Health Organization (WHO) has released its global status report on alcohol and health for 2011. Forum members largely agreed with the discussion in the report of the serious health and societal problems associated with the misuse of alcohol, which contributes to accidents, many diseases, and premature deaths. On the other hand, Forum members were disturbed that the report was limited almost exclusively to abusive drinking, was based primarily on out-dated information, and minimized the beneficial health effects associated with moderate drinking. The report ignored a massive amount of scientific data indicating that in all developed countries, moderate consumers of alcohol are at much lower risk of essentially all of the diseases of ageing: coronary heart disease, ischemic stroke, diabetes, dementia, and osteoporosis. And conspicuously absent from the WHO report is a description of the decrease in total mortality among middle-aged and elderly people associated with moderate alcohol consumption, a finding that has been found consistently throughout the world.
Epidemiologic studies over many decades have shown that while excessive or irresponsible alcohol use has severe adverse health and societal effects, moderate drinking is associated with lower risk of cardiovascular disease and other diseases of ageing. And a very large number of experimental studies, including results from human trials, have described biological mechanisms for the protective effects of both alcohol and the polyphenolic components of wine. A number of comprehensive meta-analyses are cited by Forum reviewers which they consider to provide much more accurate, up to date, and scientifically balanced views of the current “status” of the health effects of alcohol consumption. Such documents are better sources of data upon which policy decisions should be based.
Reference: Global status report on alcohol and health. World Health Organization 2011. ISBN 978 92 4 156415 1 (NLM classification: WM 274)
For the full critique of this publication by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 046: All-cause mortality rates are lower among moderate drinkers than among abstainers. 4 July 2011
The author of this paper set out to determine the extent to which potential “errors” in many early epidemiologic studies led to erroneous conclusions about an inverse association between moderate drinking and coronary heart disease (CHD). His analysis is based on prospective data for more than 124,000 persons interviewed in the U.S. National Health Interview Surveys of 1997 through 2000 and avoids the pitfalls of some earlier studies. He concludes that the so-called “errors” have not led to erroneous results, and that there is a strong protective effect of moderate drinking on CHD and all-cause mortality.
The results of this analysis support the vast majority of recent well-done prospective studies. In the present paper, non-drinkers had much higher risk of death than did almost all categories of subjects consuming alcohol. The author contends that these results lend credence to the argument that the relationship between alcohol and mortality is causal.
While some Forum reviewers felt that this analysis only replicates what has been shown in many other papers, it appears that erroneous information continues to be used by some policy groups. Thus, most reviewers believe that this new analysis provides important information on potential health effects of moderate drinking.
Reference: Fuller TD. Moderate alcohol consumption and the risk of mortality. Demography 2011. DOI 10.1007/s13524-011-0035-2
For the full review of this publication by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 045: Alcohol drinking in the elderly: Risks and benefits. 26 June 2011
The Royal College of Psychiatrists of London has published a report related primarily to problems of unrecognized alcohol misuse among the elderly. The report provides guidelines for psychiatrists and family physicians on how to find and how to treat elderly people with misuse of alcohol and drugs. The report also mentions lower “sensible limits” for older people in comparison with younger people. The Forum reviewers point out, however, inherent difficulties in providing guidelines for a very non-homogenous group of individuals whose only criterion for inclusion is being above the age of 65 years. Such a group includes individuals varying from marathon runners to very sick, frail people. Forum reviewers thought that advice to lower limits of drinking for everyone in this age group is not based on reliable research, and would certainly not apply to all in this age group.
The Forum reviewers were also struck by the absence in the Royal College report of any discussion of the strong positive effects of moderate drinking on most of the diseases of ageing, especially cardiovascular diseases, diabetes, and dementia, which are leading causes of morbidity and mortality in this age group. For healthy moderate and responsible drinkers, advice to reduce or stop all alcoholic beverage intake would not be in the best health interests of such individuals.
Reference: Royal College of Psychiatrists, London. Our invisible addicts. First Report of the Older Persons’ Substance Misuse Working Group of the Royal College of Psychiatrists, College Report CR165. June 2011
For the full review of this publication by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 044: The association of alcohol drinking with migraine headache 12 June 2011
An excellent paper from a headache center in Italy summarizes the scientific data relating alcohol ingestion to migraine headaches. The factors that trigger an attack of migraine, or of other headaches as well, are poorly understood. While retrospective studies tend to include alcohol as a trigger for an attack, the authors describe that in a recent prospective study (in which information on the factors that could potentially trigger an attack were collected prior to the migraine attack), menstruation, stress, and fatigue were found most commonly to relate to a subsequent attack, but not alcohol consumption (in fact, beer consumption on the previous day reduced the risk of a migraine attack). In the present paper, the authors reviewed the role and mechanism of action of alcohol or other components of alcoholic drinks in relation to alcohol-induced headache. They conclude from their review that reports overestimate the role of alcohol, as well as other foods, in the triggering of migraine.
Forum members thought that this was a very balanced review of the subject, and that it provided straightforward and sensible advice. Although some individuals surely have the onset of a migraine or other type of headache after the consumption of wine or alcohol, the findings are not consistent. Forum members suggest that given that subjects reporting migraine headaches have been found to be at increased risk of cardiovascular disease, it would not be appropriate to advise all such sufferers to avoid alcohol. As suggested by the authors of this paper, it may be reasonable for those subjects who had a desire to consume alcohol to drink small amounts of specific beverages to see if each beverage was tolerated or not. After seeing the effects, and factoring in symptoms versus potential benefits from moderate drinking, a reasonable discussion can be carried out with respect to continued alcohol use by subjects with migraine.
Reference: Panconesi A, Bartolozzi ML, Guidi L. Alcohol and migraine: What should we tell patients? Curr Pain Headache Rep 2011;15:177–184. DOI 10.1007/s11916-011-0184-4.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 043: Frequent moderate drinking of alcohol is associated with a lower risk of fatty liver disease. 23 May 2011
In a large study of men in Japan, the presence of fatty liver disease by ultrasonography showed an inverse association with the frequency of alcohol consumption; there was some suggestion of an increase in fatty liver disease with higher volume of alcohol consumed per day. Moderate drinkers had lower levels of obesity than did non-drinkers, and both obesity and metabolic abnormalities were positively associated with fatty liver disease.
These findings support the results of a number of other recent studies showing that moderate drinking does not increase the risk of this common type of liver disease; instead, it is associated with a lower risk of its occurrence. We agree with the implications of these studies as stated by the authors: “These results suggest that lifestyle modifications aimed at fighting central obesity and metabolic abnormalities should be the most important recommendations for the management of fatty liver. In addition, it seems unlikely that the risk of fatty liver can be reduced by the discontinuation and/or reduction of alcohol consumption alone.”
Reference: Hiramine Y, Imamura Y, Uto H, Koriyama C, Horiuchi M, Oketani M, Hosoyamada K, Kusano K, Ido A, Tsubouchi H. Alcohol drinking patterns and the risk of fatty liver in Japanese men. J Gastroenterol 2011 46:519–528. DOI 10.1007/s00535-010-0336-z.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 042: An increase in risk of certain types of gastric cancer from heavy drinking, but no increase from moderate alcohol consumption 17 May 2011
A very well-done meta-analysis supports other data generated on the risk of alcohol consumption and gastric cancer – that is – that the risk may be real for heavy alcohol consumption but not for moderate intake. The type of gastric cancer relating to heavier alcohol intake in this study tended to be tumors involving the noncardia, but differences between the association with tumors of the gastric cardia were not significant.
There was no increased risk of gastric cancer from alcohol among Asians; this may be due to lower alcohol intake; there is a greater prevalence among Asians of the inactive ALDH2 genotype that is associated with flushing and other adverse effects of alcohol, and such subjects tend to drink less alcohol. However, a number of studies have shown higher risk for upper aero-digestive cancers for subjects with this ALDH2 genotype, so the overall reason for the lower risk among Asians in this study remains unclear. The main outcome of the study is that there is no increase in the risk of gastric cancer associated with the moderate intake of alcohol.
Reference: Tramacere I, Negri E, Pelucchi C, Bagnardi V, Rota M, Scotti L, Islami F, Corrao G, La Vecchia C, Boffetta P. A meta-analysis on alcohol drinking and gastric cancer risk. Ann Oncology 2011;doi:10.1093/annonc/mdr135
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 041: Estimated health effects of changes in advice for alcohol consumption between the 2005 and 2010 Dietary Guidelines for Americans 6 May 2011
This paper from the National Institute on Alcohol Abuse and Alcoholism in the US suggests that the changes in wording of the alcohol recommendations in the Dietary Guidelines for Americans between 2005 and 2010 indicate that some at-risk drinkers could be classified as moderate drinkers. The authors carried out an analysis using data from a large, nationally representative sample of U.S. adults to estimate differences between subjects following the 2005 recommendations and a “gray zone” of subjects who exceed the 2005 recommendations but fall within the moderate guidelines according to the 2010 recommendations. The differences between these two groups were minimal; other than the gray zone subjects having an increased risk of alcohol dependence (which is unlikely to relate to their slight differences in consumption), the only other differences between the two groups related to alcohol-related interpersonal relations and job loss. And, as the authors state, “There were no associations with medical conditions or mental disorders.”
More importantly, the authors state that “Moreover, of the gray area drinkers who experienced incident alcohol dependence and interpersonal problems, 89% of the former and 94% of the latter had moved out of the gray area and into the highest-risk consumption group over the course of the follow-up interval.” Problems were thus very rare in those who remained in the gray zone of drinking during follow up.
Obviously, drinking 3 or 4 drinks/day (other than doing so only occasionally) should not be considered a healthy way to consume alcohol. But if, as the authors state, almost all of the estimated effects on health are due to subjects who increase their drinking above this “gray zone,” there is little support for their argument that the changes in guidelines make a difference.
Reference: Dawson DA, Grant BF. The “Gray Area” of consumption between moderate and risk drinking. J Stud Alcohol Drugs 2011;72:453–458.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 040: Lower risk of coronary heart disease from alcohol, even with heavy drinking 27 April 2011
Using data from The 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions study (the NESARC study, n = 43,093), the authors of this paper conclude that alcohol may have cardioprotective effects not only in moderate drinkers, but also in individuals with patterns of use traditionally considered as “hazardous.” While such a finding has been shown in some population studies, there were questions by Forum reviewers as to the adequacy of the method for diagnosing coronary artery disease: self-report, with most subjects listing angina pectoris, a “soft” criterion for coronary disease.
In addition, the categories of drinking used in this study were very broad: rare or only occasional drinkers were combined with regular drinkers up to 7 or 14 drinks per week in the “moderate” category; the “hazardous” category included a broad range of drinkers, from a minimal increase over the recommended limits to very heavy drinkers. The pattern of drinking (especially the number of days per week that alcohol was consumed) was not reported, making it difficult to separate regular from heavy week-end drinkers. The effects of heavier drinking on other conditions (such as alcohol-related liver disease, mortality, etc.) were not included in this analysis.
It is physiologically possible that even hazardous use of alcohol, like moderate use, may well lead to cleaner arteries and therefore lower rates of coronary artery disease. If this is the case, an explanation for the increases in cardiovascular mortality reported for heavy drinkers in many studies may relate not directly to coronary artery disease, but to conditions such as cardiomyopathy or cardiac arrhythmias. However, the rates of accidents, suicide and other morbidity associated with hazardous alcohol use may well overcome any protective effects on coronary disease.
Reference: Le Strat Y, Gorwood P. Hazardous drinking is associated with a lower risk of coronary heart disease: Results from a national representative sample. Am J Addict 2011;20:257–263.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 039: The role that alcohol drinking may play in the risk of cancer 17 April 2011
A large group of distinguished scientists have published a very detailed and rather complex paper describing the association between alcohol consumption and cancer. It is based on data from the EPIC study in Europe, with a mean follow up of 8.8 years for more than 300,000 subjects. The authors describe an increase in risk of many cancers from alcohol intake, but do not give data permitting the detection of a threshold of intake for an adverse effect on cancer risk. The investigators conclude that “In western Europe, an important proportion of cases of cancer can be attributable to alcohol consumption, especially consumption higher than the recommended upper limits.”
Members of the Forum were concerned that the authors did not separate moderate consumption from heavy consumption for their main analyses, ignored the demonstrated benefits of moderate drinking on total mortality, and did not point out other environmental influences (such as smoking, diet, obesity, etc.) that often have much larger effects on the risk of many cancers than does alcohol consumption. The authors make statements such as alcohol has negative effects on total mortality that are not supported by the data presented in their paper, and are contradicted by most large-scale population-based studies. Overall, while this paper supports the well-known association between heavy drinking and an increased risk of upper aero-digestive and certain other cancers, it adds little information useful for the prevention of most types of cancer.
Reference: Schűtze M, Boeing H, Pischon T, et al, Alcohol attributable burden of incidence of cancer in eight European countries based on results from prospective cohort study. BMJ 2011; 342:d1584 doi: 10.1136/bmj.d1584 (Published 7 April 2011)
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 038: Effects of a large reduction in alcohol prices on mortality in Finland 7 April 2011
Time series intervention analysis modeling was applied to the monthly aggregations of deaths in Finland for the period 1996–2006 to assess the impact of a reduction in alcohol prices in 2004. The authors report that alcohol-related deaths increased in men aged 40–49 years, and in men and women aged 50–69 years: the mean rate of alcohol-related mortality increased by 17%, 14%, and 40%, respectively, which implies 2.5, 2.9 and 1.6 additional monthly deaths per 100,000 person-years following the price reduction. In contrast to alcohol-related mortality, CVD and all-cause mortality decreased among men and women in the highest age category. The changes were consistent with 19 and 25 fewer monthly deaths per 100,000 person-years for CVD and 42 and 69 fewer monthly deaths for all-cause mortality.
Forum members agreed that both potentially harmful and beneficial effects resulting from changes in alcohol intake should be considered when estimating population effects. They were unsure whether all of the reported effects in the elderly should be attributed to changes in alcohol intake, as decreases in CVD and all-cause mortality rates were occurring prior to the change in alcohol intake.
Reference: Herttua K, Mäkelä P, Martikainen P. An evaluation of the impact of a large reduction in alcohol prices on alcohol-related and all-cause mortality: time series analysis of a population-based natural experiment. Int J Epidemiol 2011;40:441-454; doi:10.1093/ije/dyp336.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 037: Genes found to relate to level of alcohol consumption among Asians 27 March 2011
In a study of 1,721 Korean male drinkers aged 40–69 y in an urban population–based cohort, and another sample of 1,113 male drinkers from an independent rural cohort, information on average daily alcohol consumption was collected and DNA samples were collected for genotyping. In a genome-wide association (GWA) study, 12 single-nucleotide polymorphisms (SNPs) on chromosome 12q24 had genome-wide significant associations with alcohol consumption. These polymorphisms were closely related to genes that determine levels of ALDH, low levels of which relate to flushing after even small amounts of alcohol. Such enzymes are much more common among Asians than among westerners. Further, associations were tested only with the weekly amount of alcohol consumed, not the pattern of drinking; hence, these findings are not direct measures of alcoholism.
The editorial by Freedman et al states “epidemiologic literature suggests that those who begin drinking at an early age may be at greater risk for a maladaptive and more genetically pronounced form of alcohol consumption, and other environmental milieus affect the risk of alcoholism.” It will be important to investigate the interplay of genes and environmental factors when seeking the determinants of alcohol abuse. Despite the findings of this study, our understanding of factors associated with alcoholism remains very limited.
Reference: Baik I, Cho NH, Kim SH, Han B-G, Shin C. Genome-wide association studies identify genetic loci related to alcohol consumption in Korean men. Am J Clin Nutr 2011;93:809–816.
Accompanying Editorial: Agrawal A, Freedman ND, Bierut LJ. Genome-wide association studies of alcohol intake—a promising cocktail? Am J Clin Nutr 2011;93:681–683.
For the full critique of this article by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 036: Alcohol consumption after age 75 associated with lower risk of developing dementia
7 March 2011
A population-based study of elderly Germans, aged 75 and older, evaluated the association between alcohol consumption and incident overall dementia and Alzheimer dementia over 3 years. There was good ascertainment of the development of dementia, even among subjects who died during follow up.
Of 3,202 subjects free of dementia at baseline, 217 subjects met criteria of dementia during follow up. Subjects consuming alcohol had approximately 30% less overall dementia and 40% less Alzheimer dementia than did non-drinking subjects. Unlike many previous studies showing greater effects of wine on reducing risk of dementia, no significant differences were seen according to the type of alcoholic beverage consumed. Overall, these results are similar to several previous studies in the very elderly and suggest that moderate drinking is associated with less dementia, even among individuals aged 75 years and older.
Reference: Weyerer S, Schaufele M, Wiese B, Maier W, Tebarth F, van den Bussche H, Pentzek M, Bickel H, Luppa M, Riedel-Heller SG, for the German AgeCoDe Study Group (German Study on Ageing, Cognition and Dementia in Primary Care Patients). Current alcohol consumption and its relationship to incident dementia: results from a 3-year follow-up study among primary care attenders aged 75 years and older. Age and Ageing 2011; 0: 1–7; doi: 10.1093/ageing/afr007.
For the full critique of this article by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 035: A review of the association of alcohol consumption with cardiovascular disease outcomes 5 March 2011
In an excellent summary, the authors of this paper have synthesized results from longitudinal cohort studies comparing alcohol drinkers with non-drinkers for the outcomes of overall mortality and mortality from cardiovascular disease (CVD), incident coronary heart disease (CHD), mortality from CHD, incident stroke, and mortality from stroke. They conclude that light to moderate alcohol consumption is associated with a reduced risk of multiple cardiovascular outcomes. Further, they suggest that current scientific data satisfy Hill criteria indicating causality, that alcohol intake is the cause of the lower risk of cardiovascular disease among moderate drinkers.
Forum members thought that this was a very well-done, comprehensive summary of a large number of studies on alcohol and cardiovascular disease. Some believed that two topics were not adequately discussed: (1) greater benefits from wine than from other beverages, a result seen in many studies, and (2) the importance of the pattern of drinking on the health effects of alcohol. However, Forum members welcomed the discussion in the paper as to causality and regarding future directions in research, with more emphasis into how physicians and individual patients might respond to encouragement to consume alcohol for its potentially beneficial effects on cardiovascular disease. Most believe that there is no substitute for balanced judgment by a knowledgeable, objective health professional when discussing alcohol intake, and this requires is a synthesis of common sense and the best available scientific facts as they apply to the individual.
Reference: Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 2011;342:d671; doi:10.1136/bmj.d671
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 034: A review of interventional studies in humans showing effects of alcohol on risk factors for cardiovascular disease 5 March 2011
A summary paper on the effects of alcohol consumption on biologic mechanisms associated with coronary heart disease provides an excellent review of a large number of intervention studies in humans. Appropriate analyses were done and the results are presented in a very clear fashion, although there was little discussion of the separate, independent effects of alcohol and polyphenols on risk factors.
The trials the authors reviewed have demonstrated that the moderate intake of alcoholic beverages leads to increases in HDL-cholesterol, apolipoprotein A1, and adiponectin and decreases in fibrinogen, all factors associated with a lower risk of heart disease. The findings described in this paper strengthen the case for a causal link between alcohol intake and a reduced risk of coronary heart disease, suggesting that the lower risk of heart disease observed among moderate drinkers is caused by the alcoholic beverage itself, and not by other associated lifestyle factors.
Reference: Brien SE, Ronksley PE,Turner BJ, Mukamal KJ, Ghali WA. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ 2011;342:d636; doi:10.1136/bmj.d636.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 033: Moderate-to-heavy alcohol intake may increase risk of atrial fibrillation 12 February 2011
A number of well-done studies have shown an increase in the risk of atrial fibrillation to be associated with heavy alcohol intake or with alcoholism. Most previous studies suggest little if any increase in risk from light-to-moderate drinking. The present study was a meta-analysis based on 14 studies from Europe or North America. It showed an increase in risk with alcohol, but there were limited dose-response data to determine if there was a threshold above which the risk was increased.
Overall, the scientific evidence from many studies suggests that at least heavy drinking may increase the risk of atrial fibrillation, although whether light-to-moderate intake increases the risk seems unlikely. Previous basic scientific data of mechanisms of atrial fibrillation have suggested that alcohol has little effect on this arrhythmia.
Reference: Kodama S, Saito K, Tanaka S, Horikawa C, Saito A, Heianza Y, Anasako Y, Nishigaki Y, Yachi Y, Iida KT, Ohashi Y, Yamada N, Sone H. Alcohol consumption and risk of atrial fibrillation. A meta-analysis. J Am Coll Cardiol 2011;57:427–436.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 032: Comments on alcohol in newly released Dietary Guidelines for Americans, 2010 9 February 2011
The United States has released new Dietary Guidelines for Amercans, 2010. While the Key Recommendations regarding alcohol remain similar to those of earlier guidelines, there were some changes in the text that reflect increasing scientific data indicating potential health benefits of moderate drinking. The key recommendation is as follows:
“If alcohol is consumed, it should be consumed in moderation—up to one drink per day for women and two drinks per day for men—and only by adults of legal drinking age.”
Within the main body of the guidelines, comments on alcohol include the following:
“The consumption of alcohol can have beneficial or harmful effects, depending on the amount consumed, age, and other characteristics of the person consuming the alcohol. Alcohol consumption may have beneficial effects when consumed in moderation. Strong evidence from observational studies has shown that moderate alcohol consumption is associated with a lower risk of cardiovascular disease. Moderate alcohol consumption also is associated with reduced risk of all-cause mortality among middle-aged and older adults and may help to keep cognitive function intact with age. However, it is not recommended that anyone begin drinking or drink more frequently on the basis of potential health benefits because moderate alcohol intake also is associated with increased risk of breast cancer, violence, drowning, and injuries from falls and motor vehicle crashes.”
Reference: www.cnpp.usda.gov/Publications/DietaryGuidelines/2010/PolicyDoc/Chapter3.pdf
To see a copy of the section on alcohol from the new Dietary Guidelines, click here.
===============================================================================
Critique 031: Wine polyphenols have a variety of beneficial effects on health 30 January 2011
Much of the protection against cardiovascular disease attributed to wine intake may relate not only to the alcohol in wine, but to its polyphenolic constituents. This review article summarizes research into the chemistry, bioavailability, metabolism and excretion of polyphenols as well as mechanisms of their action. As stated by the authors, “These protective effects could be due to one or many components of the complex mixture of bioavailable and bioactive compounds present in red wine including ethanol, resveratrol, flavonols, flavan-3-ols, anthocyanins, phenolic acids as well as their metabolites formed either in the tissues or in the colon by the microflora.” The authors describe their cardioprotective effects, effects on vascular function and atherosclerosis, anti-platelet effects, effects on myocardial ischemia, and anti cancer and anti-diabetic effects.
The authors conclude that “Polyphenols are the most abundant antioxidants in the diet and are widespread constituents of wine, fruits and vegetables.” Their review provides an extensive scientific literature on polyphenols in wine; it suggests multiple mechanisms by which such substances may have beneficial effects on health.
Reference: Rodrigo R, Miranda A, Vergara L. Modulation of endogenous antioxidant system by wine polyphenols in human disease. Clin Chim Acta 2011;412:410-424
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research please click here.
===============================================================================
Critique 030: Young rats given red wine polyphenols show less deterioration in endothelial function with ageing. 30 January 2011
The gradual decrease in endothelial function over time is a key factor in the development of diseases associated with ageing, especially cardiovascular disease (CVD). Many epidemiologic studies suggest greater protection against CVD from wine than from other beverages containing alcohol, with at least one factor being the polyphenols in red wine (RWPs).
The present study in rats found that the administration of red wine polyphenols protected against ageing-induced endothelial dysfunction. As stated by the authors: “The present findings indicate that regular intake of RWPs in the drinking water starting at young age (16 week-old) prevented the aging-related endothelial dysfunction most likely by reducing the excessive oxidative stress in the arterial wall.” They further suggest an important role of NADPH oxidase and possibly also the angiotensin system in the abnormal vascular response in aging. Their study showed that, “RWPs intake had also a physiological beneficial effect since it improved the physical exercise capacity of old rats.”
Forum members thought that this was an excellent paper, as it begins to delve into mechanisms by which polyphenols improve health. A mechanism is addressed and results are consistent with the working hypothesis of a specific interaction between polyphenols and peculiar enzymes. There is a satisfying agreement between basic mechanisms and pathophysiology.
Some scientists believe that interventions to improve endothelial function (such as the consumption of red wine or other sources of polyphenols) should begin earlier in life to slow down the endothelial dysfunction that occurs with ageing. This study in rats tends to support such a belief.
Reference: Dal-Ros S, Zoll J, Lang AL, Auger C, Keller N, Bronner C, Geny B, Schini-Kerth VB. Chronic intake of red wine polyphenols by young rats prevents aging-induced endothelial dysfunction and decline in physical performance: Role of NADPH oxidase. Biochem Biophys Res Commun 2011;404:743-749
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 029: Differing opinions on the message to the public regarding alcohol consumption 16 January 2011
A Letter to the Editor entitled “What should we advise about alcohol consumption?” was recently published by Maurizio Ponz de Leon in Intern Emerg Med.1 Dr. de Leon argues that the message of health benefits of moderate drinking “seems to me hazardous and extremely dangerous to diffuse in the general population.” His reasons included (1) many people may be unable to distinguish between low–moderate and high consumption of wine, beer or spirits, and alcohol metabolism may differ remarkably from one subject to another; (2) alcohol remains a frequent cause of car crash, and governments (in almost all western countries) try to convince or force people to abstain from drinking before driving; and (3) to consider alcohol as a medication whose consumption may contribute to improved health is another source of concern. Dr. de Leon asks: “Are we truly at the point of prescribing alcohol consumption in order to reduce the risk of stroke and coronary damage?” He concluded that “more studies are needed before we can give sensible recommendations on alcohol consumption to the general population.”
The de Leon editorial has prompted considerable response from other scientists, including further Letters to the Editor of the journal by Di Castelnuovo, Costanzo, Donati, Iacoviello, and de Gaetano,2 and by Estruch and Lamuela-Raventos.3 In addition, the original editorial has stimulated considerable debate among members of the International Scientific Forum on Alcohol Research. Among key arguments presented by the Forum members, all experts in scientific research on alcohol, are that messages to the public should not be “paternalistic” (we will tell you what is best for you since you are not smart enough to understand the facts), and that guidelines must always be based on sound, balanced scientific data rather than on uninformed opinion. Forum members emphasized that there are certain people who should not drink at all (including former abusers of drugs or alcohol, people with certain medical conditions, children and adolescents, and people with religious or moral proscriptions against alcohol), and there can never be a general recommendation for everybody to consume alcohol. On the other hand, physicians should not withhold from their patients and the public scientifically sound and balanced data on alcohol and health. And the data are extremely strong supporting a role for moderate alcohol intake, for appropriate adults, for the reduction in risk of coronary artery disease and other diseases of ageing.
Several Forum members pointed out that it was unfortunate that the journal had chosen to publish the original letter that castigates alcohol from an author with good scientific credentials, but little to no apparent research expertise in the subject of alcohol and health. Many Forum members disagreed with the statement of de Leon that “Many people may be unable to distinguish between low–moderate and high consumption of wine, beer or spirits.” A leading scientist dealing with this subject for decades, Dr. Arthur Klatsky, has written: “Most people know very well what the difference is between light to moderate drinking and binge or excessive drinking. While some patients may rationalize their heavy drinking because of its purported health effects, I have yet to find someone who had developed alcohol abuse because of messages about the health effects of moderate drinking.” Medical practitioners, in his view, “have a ‘solemn duty’ to tell the truth about alcohol consumption, as they understand it, to all of their patients.” While pointing out that certain individuals will not benefit from the consumption of alcohol, several Forum members believed that it would be unethical for physicians to withhold from middle-aged or elderly subjects at risk of cardiovascular disease information on the potential benefits of light-to-moderate drinking
References:
- Maurizio Ponz de Leon. What should we advise about alcohol consumption? Intern Emerg Med, DOI 10.1007/s11739-010-0487-1.
- Augusto Di Castelnuovo, Simona Costanzo, Maria Benedetta Donati, Licia Iacoviello, Giovanni de Gaetano. What should we advise about alcohol consumption? Reply letter by A. Di Castelnuovo. Intern Emerg Med, DOI 10.1007/s11739-010-0502-6.
- Ramon Estruch • Rosa Ma Lamuela-Raventos. What should we advise about alcohol consumption: reply letter by R. Estruch. Intern Emerg Med; DOI 10.1007/s11739-010-0503-5.
For the full critique of these publications by members of the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 028: Changes over time in relation of social class to mortality from cirrhosis 9 January 2011
To explore the nature of the social class gradient of cirrhosis mortality in England and Wales across the 20th century, data on male cirrhosis mortality by social class were obtained from the Registrar General’s Decennial Supplements for the years 1921–1991. This paper describes a dramatic change during the 20th century in the association between social class and mortality from liver cirrhosis. While deaths from cirrhosis were more common among higher social classes in the early part of the century, the pattern changed so that deaths from cirrhosis were much more common among the lower social classes by the end of the century.
Suggested reasons for the lower current rates among subjects at higher social class include different patterns of alcohol consumption, with regular moderate consumption (especially of wine with meals) becoming more common with higher social class subjects while binge drinking (especially of beer and spirits) remaining more common in lower social classes. However, a number of other factors may relate to the class differences in rates of hepatic cirrhosis, including a less healthy diet and greater rates of obesity (associated with hepatic fatty liver and cirrhosis) among lower social class subjects and social class differences in hepatitis rates. Further, certain medications, coffee consumption, and many other lifestyle factors are associated with hepatic cirrhosis. The actual reasons for the changes over time reported in this paper remain unclear.
Reference: Crombie IK, Precious E. Changes in the social class gradient of cirrhosis mortality in England and Wales across the 20th century. Alcohol and Alcoholism 2011;46:80–82.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 027: Effects of resveratrol and quercetin on inflammation and insulin resistance – 20 December 2010
A study was carried out to examine the extent to which quercetin and trans-resveratrol (RSV) prevented inflammation or insulin resistance in primary cultures of human adipocytes treated with tumor necrosis factor-a (TNF-a)—an inflammatory cytokine elevated in the plasma and adipose tissue of obese, diabetic individuals. Cultures of human adipocytes were pretreated with quercetin and trans-RSV followed by treatment with TNF-a. Subsequently, gene and protein markers of inflammation and insulin resistance were measured. The authors report that quercetin, and to a lesser extent trans-RSV, attenuated the TNF-a–induced expression of inflammatory genes such as interleukin (IL)-6, IL-1b, IL-8, and monocyte chemoattractant protein-1 (MCP-1) and the secretion of IL-6, IL-8, and MCP-1.
Forum members were concerned about certain aspects of the study, especially the extrapolation of in vitro results to in vivo situations. The in vitro conditions the authors describe are minimally representative of an in vivo condition. In vivo, after consumption of quercetin or resveratrol, these compounds undergo extensive metabolism, leading to glucuronidated, sulphated or methylated compounds. In a previous study, quercetin 3-glucoside was transformed to 3,4-dihydroxyphenylacetic acid, acetate and butyrate in cells from human gut; only 3′-methylquercetin has been detected in human plasma, present at a concentration of 0.1 to 0.2 µM after 3 h. The authors of the current paper are using concentrations up to 60 µM, concentrations which have not been found in vivo.
There were also concerns with the work on cell uptake of quercetin and resveratrol. Primary adipocytes were incubated with the polyphenols, but it is not clear whether or not the concentrations used were subtoxic. Our current knowledge is limited about local concentration of the molecules we are studying in subcellular compartments, their interaction with alternative targets, and eventually their transformation into products that could be more or less active on a given specific pathway. The real difficult and important issue is the identification of a reasonable convergence — if not agreement — between data originating from extremely distant approaches. In this case, the notion that metabolic diseases are related to a homeostatic imbalance in adipose tissue, linked to a different redox status, linked to activation of specific pathways, and that different redox sensitive polyphenols do have a protective effect, encompasses the evidence produced by extremely distant approaches.
From a clinical point of view, the role of phytochemicals acting as antioxidants and anti-inflammatory agents could be extremely important in inflammation-associated chronic conditions such as cardiovascular disease, diabetes, and cancer. Quercetin and resveratrol may indeed play an important role in this regard, and need to be investigated further to establish the clinical importance of natural dietary compounds in the prevention of chronic degenerative conditions.
Reference: Chuang C-C, Martinez K, Xie G, Kennedy A, Bumrungpert A, Overman A, Jia W, McIntosh MK. Quercetin is equally or more effective than resveratrol in attenuating tumor necrosis factor-a–mediated inflammation and insulin resistance in primary human adipocytes. Am J Clin Nutr 2010;92:1511–1521.
For the full critique of this paper by the International Scientific Forum on Alcohol Research please click here.
===============================================================================
Critique 026: Chinese study suggests that alcohol increases angiographically significant coronary artery disease 8 December 2010
Among a large number of Chinese men presenting with chest pain or EKG changes, sequential subjects undergoing cardiac angiography were evaluated for obstructive coronary artery disease (CAD) lesions according to their reported recent alcohol intake. The study population consisted of 1,476 consecutive men 36 to 84 years of age; participants were categorized as nondrinkers, light drinkers, moderate drinkers, or heavy drinkers.
Adjusted odds ratios for angiographically proved CAD for light, moderate, and heavy drinking were 1.16 (95% confidence interval 0.68 to 1.94), 1.78 (1.35 to 2.27), and 2.18 (1.46 to 3.25). Compared to non-drinking, adjusted odds ratios were 1.03 (0.54 to 1.87) for drinking 0 to 15 years, 1.61 (1.28 to 2.14) for 16 to 30 years, and 1.98 (1.23 to 3.05) for >30 years. The authors concluded that moderate-to-heavy alcohol consumption increased the risk of CAD in Chinese men. CAD risk tended to increase with an increase in frequency and duration of drinking.
This was a very select group of patients (those presenting with chest pain or EKG changes), and not typical of the Chinese population. No information was available on drinking patterns or on previous alcohol intake. Further, a recent large population-based study from mainland China showed that consumers of alcohol were less likely to develop coronary disease, results similar to those in most Western populations. It is not possible from the present study to say that the association of alcohol intake with CAD is different between Chinese and Western populations, as the present study gives results only for a very select group of patients.
The most important outcome regarding CAD is the occurrence of clinical events (myocardial infarction, cardiac death, etc.). The detection of such events requires long-term follow-up studies to be able to judge the overall effects of alcohol drinking on CAD.
Reference: Zhou X, Li C, Xu W, Hong X, Chen J. Relation of alcohol consumption to angiographically proved coronary artery disease in Chinese men. Am J Cardiol 2010;106:1101–1103.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 025: Pattern of drinking and type of beverage affect the relation of alcohol intake to coronary heart disease 1 December 2010
Using cohort data from Belfast and France, investigators related weekly alcohol consumption, incidence of binge drinking (alcohol >50 g on at least one day a week), incidence of regular drinking (at least one day a week, and alcohol <50 g if on only one occasion), volume of alcohol intake, frequency of consumption, and types of beverage consumed to risk of coronary heart disease (CHD) events over a 10 year follow-up period. Overall, 60.5% of subjects from N. Ireland and 90.6% of French reported drinking alcohol at least once a week. Among drinkers, 12% of men in Belfast drank alcohol every day compared with 75% of men in France. Mean alcohol consumption was 22.1 g/ day in Belfast and 32.8 g/day in France. Binge drinkers comprised 9.4% and 0.5% of the Belfast and France samples, respectively.
Results showed that, after multivariate adjustment, the hazard ratio for hard coronary events compared with regular drinkers was 1.97 (95% CI 1.21 – 3.22) for binge drinkers, 2.03 (95% CI 1.41 – 2.94) for never drinkers, and 1.57 (95% CI 1.11 – 2.21) for former drinkers. The hazard ratio for hard coronary events in Belfast compared with in France was 1.76 (95% CI 1.37 to 2.67) before adjustment, and 1.09 (95% CI 0.79 to 1.50) after adjustment for alcohol patterns and wine drinking. Only wine drinking was associated with a lower risk of hard coronary events, irrespective of the country.
The authors conclude that regular and moderate alcohol intake throughout the week, the typical pattern in middle-aged men in France, is associated with a low risk of ischemic heart disease, whereas the binge drinking pattern more prevalent in Belfast confers a higher risk.
While a strong inverse association between moderate alcohol consumption and cardiovascular disease has been demonstrated for decades, more recent research has emphasized the importance of the pattern of drinking (regular moderate versus episodic or binge drinking). Further, there continues to be debate about the potential greater effect of wine versus other beverages containing alcohol. This study shows that regular moderate drinking (especially of wine) is associated with lower risk of MI, but episodic or binge drinking (especially of beer or whiskey) increases the risk. Lifetime abstinence has a similar adverse relation to CHD as does episodic or binge drinking.
Reference: Ruidavets J-B, Ducimetièere P, Evans A, Montaye M, Haas B, Bingham A, Yarnell J, Amouyel P, Arveiler D, Kee F, Bongard V, Ferrières J. Patterns of alcohol consumption and ischaemic heart disease in culturally divergent countries: the Prospective Epidemiological Study of Myocardial Infarction (PRIME). BMJ 2010;341:c6077 doi:10.1136/bmj.c6077.
For the detailed critique of this study by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 024: Moderate alcohol consumption lowers risk of metabolic diseases in a population with high mean alcohol intake. 28 November 2010
A cross-sectional analysis of data from subjects in Switzerland related varying levels of alcohol intake to the presence of diabetes mellitus, the “metabolic syndrome,” and an index of insulin resistance (HOMA-IR). The strengths of this paper include being population-based and having a large number of subjects who reported that they consumed 14 or more drinks/week. Also, there was a good percentage (27%) of subjects reporting no alcohol intake during the one week of assessment used for classifying subjects. Another strength is the careful confirmation of drinking status with state-of-the-art laboratory tests. In multivariate analysis, the prevalence of the metabolic syndrome, diabetes and mean HOMA-IR decreased with low-risk drinking and increased with high-risk drinking. No differences were noted according to the type of beverage consumed.
This is a cross-sectional analysis, so a causative relation between alcohol intake and the metabolic outcomes cannot be assessed. Still, the data support much that has been shown in prospective studies. Several Forum members commented on potential problems when considering a number of physiologic conditions as the “metabolic syndrome” and focusing therapy on the syndrome; they believed that each metabolic factor should be evaluated and treated singly.
Reference: Clerc O, Nanchen D, Cornuz J, Marques-Vidal P, Gmel G, Daeppen J-B, Paccaud F, Mooser V, Waeber G, Vollenweider P, Rodondi N. Alcohol drinking, the metabolic syndrome and diabetes in a population with high mean alcohol consumption. Diabet Med 2010;27:1241–1249.
For the detailed critique of this study by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 023: Evidence that PPAR-gamma is a mechanism for the effects of wine polyphenolics on cardiovascular risk. 27 November 2010
It is important that biological mechanisms are identified for the observed inverse relation between the moderate consumption of wine and cardiovascular disease shown in most epidemiologic studies. A paper by Zoechling et al is an elegant example of the needed effort to provide a biochemical mechanism for the biological effects of wine. Data on binding of different wine component were produced and this result is interpreted in light of epidemiological evidence.
It would have been appropriate to provide evidence also for the actual shift of gene expression primed by the same wine component in a cell or animal model. In this respect, results must be rated appropriate but still as preliminary; a ligand could have different effects. Further, biological evidence is not provided to support the contention that these polyphenols act through the PPAR-gamma receptor. The sort of evidence that should have been provided is a comparison with rosiglitazone in a cell population known to respond to PPAR-gamma agonists (e.g. adipocytes).
Further, the analytical data does not describe the amounts of any of the “active” substances. So while there is a lot of discussion of the active components, it is not possible to compare any wine’s “activity” with the amount of the key substances. Lacking such a comparison, it is very hard to conclude that these substances are in fact the responsible factors in the observed activity.
Nevertheless, this paper provides important data on potential mechanisms by which the constituents of wine and certain other beverages may act to reduce the risk of cardiovascular disease.
Reference: Zoechling A, Liebner F, Jungbauer A. Red wine: A source of potent ligands for peroxisome proliferator-activated receptor γ. Food & Function, Journal of the Royal Society of Chemistry, in press. DOI: 10.1039/c0fo00086h.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 022: Alcohol consumption decreases with the development of disease — 21 November 2010
In a cross-sectional study from the 2004 and 2007 Australian National Drug Strategy Household (NDSH) surveys, respondents were questioned about their current and past drinking, the presence of formal diagnosis for specific diseases (heart disease, type 2 diabetes, hypertension, cancer, anxiety, depression) and self-perceived general health status. The sample sizes for the 2004 and 2007 NDSH surveys were 24,109 and 23,356, respectively.
The authors report that respondents with a diagnosis of diabetes, hypertension, or anxiety were more likely to have reduced or stopped alcohol consumption in the past 12 months. The likelihood of having reduced or ceased alcohol consumption in the past 12 months increased as perceived general health status declined from excellent to poor (although the authors do not point out that lifetime abstainers were more likely than moderate drinkers to report less than excellent health status).
The authors conclude that the experience of ill health is associated with subsequent reduction or cessation of alcohol consumption (“sick quitters), which is consistent with most prospective epidemiologic studies. The authors also conclude that this may at least partly underlie the observed ‘J-shaped’ function relating alcohol consumption to premature mortality. On the other hand, most modern epidemiologic studies are careful not to include “sick quitters” within the non-drinking category, and relate health effects of drinkers with those of lifetime abstainers. Further, prospective studies in which alcohol intake is assessed at different times (rather than having “changes” based only on recall at one point in time, as was done in this study) usually indicate that subjects who decrease their intake are more likely to subsequently develop adverse health outcomes, especially related to cardiovascular disease, than those who continue moderate drinking.
Reference: Liang W, Chikritzhs T. Reduction in alcohol consumption and health status. Addiction 2010; in press (doi:10.1111/j.1360-0443.2010.03164.x).
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 021: Alcohol consumption affects risk of cataracts 25 October 2010
A population-based prospective study from Australia utilized repeated lens photographs over a period of 5 to 10 years to diagnose cataracts among more than 2,500 subjects. The investigators related the risk of their development, and the risk of cataract surgery, to the reported alcohol intake of subjects. Previous research has provided some biological mechanisms that make an association between alcohol and cataracts plausible.
Overall, the present study showed few statistically significant relations between alcohol and cataracts, although adjusted results suggested a “U-shaped” association between total alcohol intake and development of cataracts (a lower risk for moderate drinkers, higher risk for both abstainers and heavier drinkers). The U-shaped association with alcohol consumption was stronger for the risk of cataract surgery. These results are consistent with previous cohort studies. On inspection of the data presented, the potential reduction in risk of cataract was primarily for wine and beer. While some types of cataract may be reduced by moderate drinking, larger intake of alcohol may be associated with increased risk.
Reference: Kanthan GL, Mitchell P, Burlutsky G, Wang JJ. Alcohol Consumption and the Long-Term Incidence of Cataract and Cataract Surgery: The Blue Mountains Study. Am J Ophthalmol 2010;150:434–440.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 20: New data on effects of alcohol during pregnancy 12 October 2010
A very large population-based observational study from the UK found that at the age of 5 years, the children of women who reported light (no more than 1-2 units of alcohol per week or per occasion) drinking did not show any evidence of impairment on testing for behavioral and emotional problems or cognitive ability. There was a tendency for the male children of women reporting “heavy/binge” drinking during pregnancy (7 or more units per week or 6 or more units per occasion) to have poorer behavioral scores, but the effects were less clear among female offspring.
Scientific data continue to indicate that higher intake of alcohol during pregnancy may adversely affect the fetus, and could lead to very severe developmental or other problems in the child. However, most recent publications (as does this one) show little or no effects of occasional or light drinking by the mother during pregnancy. They also demonstrate how socio-economic, education, and other lifestyle factors of the mother may have large effects on the health of the fetus and child; these must be considered when evaluating the potential effects of alcohol during pregnancy.
Overall, current scientific data indicate that while drinking during pregnancy should not be encouraged, there is little evidence to suggest that an occasional drink or light drinking by the mother is associated with harm. Heavy drinking, however, may be associated with serious developmental defects in the fetus.
Reference: Kelly YJ, Sacker A, Gray R, Kelly J, Wolke D, Head J, Quigley MA. Light drinking during pregnancy: still no increased risk for socioemotional difficulties or cognitive deficits at 5 years of age? J Epidemiol Community Health 2010; doi:10.1136/jech.2009.103002
Addendum: After the above critique was prepared, a new paper has been published on the topic by O’Leary et al (O’Leary CM, Nassar N, Kurinczuk JJ, de Klerk N, Geelhoed E, Elliott EJ, Bower C. Prenatal Alcohol Exposure and Risk of Birth Defects Pediatrics 2010;126;e843-e850; DOI: 10.1542/peds.2010-0256). Overall, the results of that study are similar to those of the study by Kelly et al, with no increase in risk of birth defects in children born of women reporting low or moderate drinking during pregnancy but with an increased risk of defects among children of women reporting heavy drinking.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 019: Both alcohol and caffeinated coffee intake are associated with lower risk of diabetes in African-American women. 27 September 2010
In a very large cohort of African-American women in the US, the association between the consumption of alcohol, tea, and coffee was related to the development of type 2 diabetes mellitus over a follow-up period averaging 12 years. Tea and decaffeinated coffee showed no relation with diabetes, but the intake of both caffeinated coffee and alcohol showed a significant inverse association.
This paper is particularly important because some previous studies have not shown a strong association between alcohol and the risk of cardiovascular disease among African-Americans. African-Americans, especially women, tend to drink little alcohol, yet are at markedly increased risk of diabetes. In the present study, the approximately 30% lower risk for moderate alcohol drinkers was about the same in these African-American women as has been found in many previous studies of whites.
Reference
Boggs DA, Rosenberg L, Ruiz-Narvaez EA, Palmer JR. Coffee, tea, and alcohol intake in relation to risk of type 2 diabetes in African American women. Am J Clin Nutr 2010;92:960–966.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 018: Alcohol consumption following diagnosis of early-stage breast cancer may increase risk of recurrence of cancer but not total mortality risk 14 September 2010
In the Life After Cancer Epidemiology (LACE) study, 1,897 participants diagnosed with early-stage breast cancer between 1997 and 2000 and recruited on average 2 years post-breast cancer diagnosis were evaluated for the association between alcohol intake and breast cancer recurrence and death. The women, who were generally light drinkers, were followed for an average of 7.4 years. The study reported an increase in risk of breast cancer recurrence and breast cancer death, but no effect on total mortality, to be associated with consumption of 3 to 4 or more drinks per week when compared with women not drinking following their cancer diagnosis.
Previous research has been mixed on this topic. Almost all large studies have shown no increase in all-cause mortality for women who drink moderately following a diagnosis of breast cancer (as does this study). As for recurrence of breast cancer, most have shown no increase in risk, although one previous study of women with estrogen-receptor + tumors found an increased risk of a primary cancer developing in the contralateral breast to be associated with alcohol intake of more than 7 drinks per week.
Because of conflicting results among studies on this topic, further research will be needed to determine the extent to which alcohol following a diagnosis of breast cancer may relate to subsequent disease and death.
Reference: Kwan ML, Kushi LH, Weltzien E, Tam EK, Castillo A, Sweeney C, Caan BJ. Alcohol Consumption and Breast Cancer Recurrence and Survival Among Women With Early-Stage Breast Cancer:The Life After Cancer Epidemiology Study. J Clin Oncol 2010;28 (published ahead of print, 10.1200/JCO.2010.29.2730)
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 017: Moderate alcohol intake is associated with a lower risk of total mortality than are either abstinence or heavy drinking 5 September 2010
In a study based on data from 1,824 predominantly Caucasian Americans from the Western part of the United States, alcohol consumption at baseline was related to mortality risk during a 20-year follow-up period. Subjects were recruited into a longitudinal project that has examined late-life patterns of alcohol consumption and drinking problems. Lifetime abstainers were not included in the study, which focused on stress and coping processes among problem drinkers and non-problem drinkers. The sample at baseline included only subjects aged 55 to 65 years who had had outpatient contact with a health care facility in the previous 3 years.
The database at baseline included information on daily alcohol consumption, sociodemographic factors, former problem drinking status, health factors, and social-behavioral factors. Subjects who were not lifetime abstainers but did not report drinking at the time of the baseline examination were classified as “abstainers.” Data on potential changes in alcohol consumption during the course of the study were not collected. Death during follow up was confirmed primarily by death certificate.
The key results of the paper are that even when adjusting for sociodemographic factors, former problem drinking status, health factors, and social-behavioral factors, moderate drinking was associated with considerably lower risk of all-cause mortality. In comparison with “moderate drinkers” (subjects reporting up to 3 drinks/day), abstainers had 51 % higher mortality risk and heavy drinkers had 45% higher risk. The study supports most previous scientific studies showing that moderate drinking, in comparison with both abstinence and heavy drinking, is associated with lower risk of total mortality.
Reference: Holahan CJ, Schutte KK, Brennan PL, Holahan CK, Moos BS, Moos RH. Late-Life Alcohol Consumption and 20-Year Mortality. Alcoholism: Clinical and Experimental Research 2010;34:in press, November 2010
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 016: Association of alcohol with breast cancer risk varies according to subtype of tumor
29 August 2010
Most studies show a slight increase in the risk of breast cancer for women who consume alcohol. The association is thought to relate to alcohol’s effects on hormones, and alcohol use tends to be more strongly associated with hormonally sensitive breast cancers than tumors not sensitive to hormones. Few studies have evaluated how alcohol-related risk varies by breast cancer subtype. In the present study, follow-up data from 87,724 women in the Women’s Health Initiative Observational Study prospective cohort were evaluated for the relation of baseline alcohol consumption with subsequent breast cancer.
A total of 2,944 invasive breast cancer patients were diagnosed during follow up. In multivariable-adjusted analyses alcohol consumption was associated with an increase in the risk of lobular carcinoma (which makes up approximately 15-20% of breast cancers), but there was not a statistically significant association with the more-common ductal type of carcinoma. Hormone + cancers showed an association with alcohol intake, but not hormone – cancers. The findings support the importance of hormonal mechanisms in mediating the relation between alcohol use and breast cancer risk.
Reference Li CI, Chlebowski RT, Freiberg M, Johnson KC, Kuller L, Lane D, Lessin L, O’Sullivan MJ, Wactawski-Wende J, Yasmeen S, Prentice R. Alcohol consumption and risk of postmenopausal breast cancer by subtype: the Women’s Health Initiative Observational Study. J Natl Cancer Inst 2010 Aug 23. [Epub ahead of print]
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here : Critique 016.
===============================================================================
Critique 015: Moderate drinking does not appear to increase risk of breast cancer among women with a BRCA gene mutation 22 August 2010
A large study was carried out to assess the effects of alcohol consumption on breast cancer risk among women with a BRCA1 or a BRCA2 gene mutation, both of which markedly increase the risk of breast cancer. Comparisons were made between women with a gene mutation who had developed invasive breast cancer matched with women with the same gene mutation who had not developed breast cancer. After a number of appropriate exclusions, there were 1,480 matched pairs with BRCA1 mutations and 445 pairs with BRCA2 mutations.
Data from the study support an earlier report suggesting no increase in breast cancer risk from alcohol intake for women with either gene mutation. In the previous study on this topic, a slight lowering of breast cancer risk was noted with light drinking among women with the BRCA2 mutation but not among those with the BRCA1 mutation. In the present study, a possible reduction in risk of breast cancer was seen for moderately drinking women with the BRCA1 mutation, but not the BRCA2 mutation. Further, in the present study, the reduction is risk of breast cancer was seen only for wine consumers. While one should not over-interpret epidemiologic data in the absence of identified biologic mechanisms, there have been a very large number of experimental studies showing that certain polyphenols present in wine actively impede the initiation and growth of cancer cells.
Overall, current scientific data suggest that alcohol in moderation does not increase the risk of breast cancer among women with a BRCA mutation, and wine may be somewhat protective. If this is indeed the case and given the high risk associated with these genetic mutations, it would be important to inform women with such a mutation that moderate alcohol does not appear to increase their risk of breast cancer.
Reference: Dennis J, Ghadirian P, Little J, et al: The Hereditary Breast Cancer Clinical Study Group. Alcohol consumption and the risk of breast cancer among BRCA1 and BRCA2 mutation carriers. The Breast 2010; e-pub.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here.
=========================================================================
Critique 014: Moderate drinking, especially of wine, is associated with better cognitive function 13 August 2010
A large prospective study of men and women in northern Norway reported that moderate wine consumption was independently associated with better performance on cognitive tests after 7 years of follow up. There was no consistent association between consumption of beer or spirits and cognitive test results. The authors also reported that abstinence was associated with significantly lower cognitive performance in women. As noted by the authors, in any observational study there is the possibility of residual confounding by other lifestyle habits affecting cognitive function, and the present study was not able to adjust for certain ones (e.g., diet, income, or profession) but did adjust for age, education, body mass index, depression, and cardiovascular disease and its major risk factors.
The results of this study support findings from a number of observational, prospective studies that have shown that the moderate consumption of alcohol, especially of wine, may have favorable effects on cognitive function. Such effects could relate to the presence in wine of a number of polyphenols and other substances that reduce the risk of cognitive decline with ageing. Mechanisms that have been suggested for such protection against cognitive dysfunction include effects on atherosclerosis, coagulation, inflammation, as well as direct neuroprotective effects.
Reference: Arntzen KA, Schirmer H, Wilsgaard T, Mathiesen EB. Moderate wine consumption is associated with better cognitive test results: a 7 year follow up of 5033 subjects in the Tromsø Study. Acta Neurol Scandd 2010; Suppl 190:23-29.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 013: Greater than moderate alcohol intake increases the risk of liver cirrhosis 27 July 2010
A new meta-analysis shows that alcohol consumption is a strong factor in the development of cirrhosis of the liver. The study also supports the theory that there is a threshold of drinking above which the risk is increased, as some of their analyses suggest that the risk increases only with intake of more than 24 grams/day of alcohol for women (about 2 typical drinks by US standards) and 36 grams/day of alcohol for men (about 3 typical US drinks).
Despite some concerns about the approach used, our Forum agrees that the present meta-analysis supports previous studies indicating a strong role of heavy alcohol drinking in the development of cirrhosis. The differences found by the investigators between the effects of moderate alcohol intake on cirrhosis morbidity and on cirrhosis mortality are difficult to explain, but may relate to misclassification of alcohol intake (heavy drinkers reporting less alcohol), always a problem in observational studies of the effects of alcohol.
The results related to morbidity suggest that small amounts of alcohol are not associated with an increased risk of cirrhosis, and may be associated with lower risk of disease. Thus, the data provide evidence for a “threshold effect” of alcohol intake for the development of cirrhosis. Limited previous data are available suggesting that wine consumption may be associated with lower risk of cirrhosis than the intake of other beverages, but essentially all studies show heavy drinking of any type of beverage increases the risk.
Reference: Rehm J, Taylor B, Patra SM, Irving H, Baliunas D, Patra J, Roerecke M. Alcohol as a risk factor for liver cirrhosis: A systematic review and meta-analysis. Drug and Alcohol Review 2010,29,437–445. DOI: 10.1111/j.1465-3362.2009.00153.x
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 012: Moderate drinking in the elderly is associated with lower total mortality 23 July 2010
The effects of alcohol consumption in the elderly may be modified by a decreased ability to metabolize alcohol, an altered volume of distribution due to reduced lean body mass and total body water, and an increased prevalence of co-morbid conditions. These factors make this study of the net effects of drinking among a large number of community-dwelling elderly men and women especially important.
In large prospective studies from Australia of men aged 60-79 and women aged 70-75 years of age, men consuming up to 4 drinks/day and women up to 2 drinks/day had considerably lower risk of dying (total mortality) than did non-drinkers. For subjects reporting 1-2 drinks/day, their total mortality risk was about 20-30% lower than that of abstainers.
While the authors concluded that not consuming alcohol on 1 or 2 days per week was associated with better outcomes, this conclusion is not in accordance with their own data. The benefit of one or two “alcohol-free” days per week has never been substantiated with solid evidence from any large epidemiological study.
Our Forum review concludes that in terms of total mortality risk, recommendations for very low levels of drinking among the elderly may be overly restrictive, as this study showed lower total mortality for up to 4 drinks/day for elderly men and 2 drinks/day for elderly women. Further, this study does not provide support for the conclusion that mortality is lower for people who have 1 or 2 “alcohol-free” days per week.
Reference: McCaul KA, Almeida OP, Hankey GJ, Jamrozik K, Byles JE, Flicker L. Alcohol use and mortality in older men and women. Addiction 2010. On-line prior to publication: doi:10.1111/j.1360-0443.2010.02972.x
For the full critique of this paper by the International Scientific Forum on Alcohol Research, click here
===============================================================================
Critique 011: A Review of the Proposed New US Dietary Guidelines 14 July 2010
Members of our International Scientific Forum on Alcohol Research have submitted a detailed review of the draft recently circulated by the United States Department of Agriculture for proposed new US Dietary Guidelines for 2010. In general, Forum members were very pleased with the alcohol recommendations in the proposal, finding them interesting, balanced, and accurate. Many commented that, rather than just focusing on warnings against heavy drinking, the new Guidelines appear to take into account the large amount of recent epidemiologic and experimental data that support many potential beneficial health effects of moderate drinking.
Among specific recommendations from the Forum were the following:
■ A stronger statement is needed of the effects of light-to-moderate drinking on total mortality, in that recent prospective studies show a considerably lower of risk of death for moderate drinkers.
■ Additional emphasis is needed on the reduced risk of developing diabetes for moderate drinkers, and the much lower risk of cardiovascular disease among diabetics who consume some alcohol.
■ Further information should be presented on the consistent scientific data showing that women who drink moderately are at reduced, not increased, risk of weight gain in adult life.
There were a number of topics not discussed in the draft Guidelines that members of the Forum thought deserved consideration for inclusion.
■ Recent reports have consistently shown that among people who have already had a myocardial infarction or other cardiovascular event, moderate drinking is associated with a reduced risk of further cardiovascular events and death.
■ More emphasis in the Guidelines should be put on the pattern of drinking (regular moderate rather than occasional binge drinking) and also on the much lower blood alcohol levels after drinking when the beverage is consumed with food, rather than on an empty stomach.
■ It was also suggested to the Guidelines Committee that the beneficial effects on cardiovascular risk of polyphenols and other substances in wine and certain beers, in addition to alcohol, be discussed more adequately.
There were also some suggestions from ISFAR regarding future research needs in the field.
■ The Forum strongly supports the need for further research on the risks and benefits of light-to-moderate alcohol consumption, rather than focusing research only on alcohol abuse.
■ The Forum proposed emphasis on future research dealing with targeting recommendations for groups of people according to age, gender, other behaviors, etc., although there was some disagreement among Forum members as to whether or not moderate drinking has strong health effects in the young and not just in middle-aged and older adults.
■ ISFAR considers moderate drinking, unless contraindicated by certain conditions (e.g, former abuse, some types of severe liver disease), to be an important aspect of a healthy lifestyle. It should be a complement, not an alternative, to other lifestyle factors such as not smoking, getting exercise, eating a healthy diet, and avoiding obesity.
The draft of the proposed new Dietary Guidelines is available at http://www.cnpp.usda.gov/DGAs2010-DGACReport.htm.
For the full ISFAR critique of the proposed new Guidelines, click here
===============================================================================
Summary Critique 010 30 June 2010
Should moderate alcohol consumption be advised following a heart attack?
There has been considerable recent interest in the effects of alcohol consumption following an acute myocardial infarction (AMI). In an observational study among 325 subjects who were moderate drinkers prior to an AMI, 84% continued to drink and 16% quit. While most of the outcome measures showed no statistically significant effects between the two groups of patients, all outcomes showed a tendency towards better physical and mental health outcomes for persistent drinkers in comparison with those who quit drinking.
A key problem with this analysis, and with all observational epidemiologic studies on this topic, is that the reason that some subjects stopped drinking after having an AMI, while others continued to drink, is not known. Even though adjustments were made for many known related factors, there is always the possibility that subjects who stopped drinking were “sicker” in many ways than those who persisted in their alcohol consumption.
It may well require a randomized trial, in which some subjects having an AMI are randomly advised to continue to drink and others advised to stop drinking, to be able to determine reliably the effects on the clinical course of the persistence of alcohol intake following an AMI.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: Critique 010
===============================================================================
Summary: Critique 009 25 June 2010
Should moderate alcohol consumption be advised for its health effects?
A report from a conference that took place at the Medicine Grand Rounds at Beth Israel Deaconess Medical Center, Boston, Massachusetts, on January 15, 2009 has recently been published in the Journal of the American Medical Association, JAMA. It provides a discussion by an epidemiologist with a broad knowledge in the field in response to a theoretical question, as from a middle-aged patient, as to the advisability of consuming some alcohol “for his health.”
The paper provides an excellent discussion of a theoretical question about drinking and health. It focuses on the potential risks and benefits associated with moderate drinking for a middle-aged male patient. Most members of the International Scientific Forum on Alcohol Research (ISFAR) were pleased with the discussion of the topic. It was noted how uncommon it is that such knowledgeable, detailed, and mostly objective data appear in the mainstream medical literature. It was thought to be “readable, informative and thoughtful.”
The ISFAR critique points out a number of topics that were covered incompletely in the paper, including inadequate information on the importance of the pattern of drinking: moderate regular consumption versus binge drinking. Further, there was a notable lack of information on the beneficial effects on many pathophysiologic processes of polyphenols and other non-alcohol substances present in wine and certain other foods and beverages.
Overall, it was believed that the paper provided important information for physicians who may be discussing alcohol consumption with their patients.
Reference
Clinical Crossroads: Conferences with patients and doctors. A 42-year-old man considering whether to drink alcohol for his health. Kenneth J. Mukamal, MD, MPH, Discussant. JAMA 2010;303:2065-2073. (doi:10.1001/jama.2010.550)
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: Critique 009.
===============================================================================
Summary: Critique 008: 13 June 2010
Further evidence that moderate alcohol consumption may play a role in the prevention of Alzheimer’s Disease
In a case-control study from Spain on the effects of smoking and alcohol use on the risk of Alzheimer’s Disease (AD), the authors found that the risk of AD was unaffected by any measure of tobacco consumption. On the other hand, alcohol consumers showed a 47% lower risk of developing AD than did never consumers, with effects mainly among women and among never smokers. No differences were noted by type of alcoholic beverage consumed. The authors conclude that mean daily total consumption of alcohol showed increasingly protective dose-response relationships in women.
The numbers in this analysis were rather small, and there is always the possibility of confounding by other lifestyle factors. Still, the study supports a number of previous epidemiologic studies showing a lower risk of developing AD for moderate consumers of alcohol.
Reference
García AM, Ramón-Bou N, Porta M. Isolated and joint effects of tobacco and alcohol consumption on risk of Alzheimer’s Disease. Journal of Alzheimer’s Disease 2010;20:577–586. (DOI 10.3233/JAD-2010-1399).
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: Critique 08.
===============================================================================
Summary: Critique 007 9 June 2010
People may change to a “healthier” pattern of drinking as they age
In a prospective longitudinal study of a cohort of Americans in the “Baby Boomer” generation, subjects’ drinking habits were assessed at two points, when they were approximately 53 years of age and again when they were approximately 64 years of age. As the subjects got older, they began to consume fewer drinks per occasion but to consume alcohol more frequently; the net effect was little change in total alcohol intake for women but a slight increase for men.
In most epidemiologic studies, regular moderate drinking is the pattern associated with lower risk of many chronic diseases; hence, the described change in drinking pattern in this study (smaller amounts on more frequent occasions) can be considered a “healthy” change. Most long-term observational studies show a decrease in total alcohol intake with ageing, although reasons for such are poorly understood.
This paper emphasizes the importance of knowing the pattern of drinking, and not just the total number of drinks consumed over a week, when evaluating the impact of alcohol consumption on health and disease.
Reference
Molander RC, Yonker JA, Krahn DD. Age-related changes in drinking patterns from mid- to older age: results from the Wisconsin Longitudinal Study. Alcoholism: Clinical and Experimental Research 2010;34 (Published early online 7 May 2010).
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: Critique 07.
===============================================================================
Summary: Critique 006 2 June 2010
For patients who already have cardiovascular disease, continued moderate alcohol consumption may reduce their risk of death
This review paper in Circuation summarizes data from 8 epidemiologic studies of subjects with cardiovascular disease (CVD) as to their subsequent mortality (both CV and total-mortality) according to their alcohol consumption. Most studies showed significantly lower risk of both CV and total mortality for patients with CVD who were consumers of alcohol.
Despite these clear-cut findings, the authors were very cautious in their conclusions, focusing on the dangers of excessive drinking and not encouraging cardiovascular patients who do not drink to start regular drinking. They state that moderate consumers of alcohol who have CV disease should not be advised to stop drinking, but should be advised to not consume alcohol more heavily.
It is interesting that these authors published the meta-analysis upon which this review is largely based in the Journal of the American College of Cardiology earlier in 2010. In that paper, their conclusions were less restrained: “Cardiologists should be aware that regular, moderate alcohol consumption, in the context of a healthy lifestyle (increased physical activity, no smoking), dietary habits (decreased dietary fat intake, high consumption of fruit and vegetables), and adequate drug therapy, would put their patients at a level of cardiovascular or mortality risk substantially lower than either abstainers or heavy or binge drinkers.”
Reference
Costanzo S, Di Castelnuovo A, Donati MB, Iacoviello L, de Gaetano G. Contemporary Reviews in Cardiovascular Medicine. Cardiovascular and overall mortality risk in relation to alcohol consumption in patients with cardiovascular disease. Circulation 2010;121;1951-1959.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 006.
===============================================================================
Summary: Critique 005 27 May 2010
Alcohol in young women may increase their risk of benign breast disease
Among more than 6,000 young women being followed in a longitudinal study, 67 confirmed cases of benign breast disease (BBD) were diagnosed. Alcohol consumption was reported on 57 women who developed BBD when they were 16 – 23 years of age, with all but 8 subjects being 18 or older when they reported alcohol intake, and no data were presented on potential exposures earlier following menarche. A significant increase in the risk of BBD was associated with alcohol intake, although many key factors that have been shown to relate to BBD were not reported in the paper. Hence, while the number of cases is small, and a number of potential risk factors are not included, this study suggests that BBD may be increased by alcohol consumption in young women.
Reference
Berkey CS; Willett WC; Lindsay Frazier A; Rosner B; Colditz GA; Rockett RH; Helaine RM. Prospective study of adolescent alcohol consumption and risk of benign breast disease in young women. Pediatrics 2010;125:e1081-e1087.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 005.
===============================================================================
Summary: Critique 004 24 May 2010
Moderate alcohol consumption is associated with other healthy lifestyle factors
An analysis based on a very large number of subjects in France demonstrates, as have most other studies, that moderate consumers of alcohol have many associated healthy lifestyle habits: lower levels of body mass index, blood glucose, heart rate, stress and depression scores; higher subjective health status, HDL-cholesterol values, levels of physical activity and social status. The authors suggest that alcohol is not related causally to any of these factors, and that the other lifestyle factors, not alcohol consumption, are the reason that moderate drinkers have less cardiovascular disease. They chose a very narrow group of citations from the literature to support this contention.
The authors ignore a large number of well-conducted prospective epidemiologic studies showing that moderate drinkers are at lower risk over time of developing certain risk factors. Further, the authors of this paper ignore an immense basic science literature that suggests that alcohol is an important factor in the development of biological risk factors, atherosclerosis, and cardiovascular disease. Further, they do not describe a number of studies that have shown specifically that moderate drinking is associated with less cardiovascular disease and diabetes among subjects who are otherwise very healthy (non-smokers, not obese, physically active, and on a healthy diet).
There is no doubt that confounding by associated lifestyle factors can play a role in the lower risk of chronic diseases among moderate drinkers, who tend to also have other healthy behaviors. However, there is now a large body of scientific evidence that indicates that alcohol is an important factor in the lower rates of such diseases; current scientific data do not support the conclusions of the authors of this paper.
Reference
Hansel B, Thomas F, Pannier B, Bean K, Kontush A, Chapman MJ, Guize L, Bruckert E. Relationship between alcohol intake, health and social status and cardiovascular risk factors in the urban Paris-Ile-De-France Cohort: is the cardioprotective action of alcohol a myth? European J Clin Nutrition, advance online publication, doi:10:1038/ejcn.2010.61.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 004.
===================================================================================
Summary: Critique 003 17 May 2010
Moderate alcohol consumption markedly reduces the risk of diabetes mellitus, even among subjects with otherwise very healthy lifestyles
In a very well-done analysis from a large Dutch population, it was shown that moderate drinking considerably lowers the risk of developing type 2 diabetes even among subjects who are otherwise following a healthy lifestyle (not obese, non-smokers, physically active, eating a healthy diet). Thus, it indicates that the effect of moderate drinking on lowering the risk of diabetes cannot be explained by other healthy lifestyle habits of such drinkers. Moderate drinking should be considered as a complement, and not as an alternative, to other healthy lifestyle habits that lower the risk of chronic diseases such as diabetes and coronary heart disease.
Reference
Joosten MM, Grobbee DE, van der A DL, Verschuren WWM, Hendriks HFJ, Beulens JWJ. Combined effect of alcohol consumption and lifestyle behaviors on risk of type 2 diabetes. Am J Clin Nutr 2010;91: 1777-1783.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 003.
===============================================================================
Summary: Critique 002 26 April 2010
Red wine, but not other types of alcohol, improve endothelial function in a randomized trial
The healthy state of cells that form the lining of arteries, assessed by indices of endothelial function, is a key factor associated with preventing the development and progression of atherosclerosis and coronary heart disease. In a randomized trial among healthy young adults, the daily consumption of about 3 ounces of red wine for three weeks led to significant improvement in endothelial function. Such improvements were not seen with the consumption of water, or of beer or vodka containing similar amounts of alcohol.
Further, in a series of in-vitro studies, the authors showed very similar effects from red wine and from a high concentration of resveratrol (but not from beer or ethanol) on factors associated with improved endothelial function. The study supports many epidemiologic and animal experiments suggesting that certain non-alcoholic constituents of red wine have additional beneficial effects on cardiovascular risk over those of just the alcohol itself.
Reference
Huang PH, Chen YH, Tsai HY, Chen JS, Wu TC, Lin FY, Sata M, Chen JW, Lin SJ. Intake of red wine increases the number and functional capacity of circulating endothelial progenitor cells by enhancing nitric oxide bioavailability. Arteriosclerosis Thrombosis and Vascular Biology 2010;30:869-877.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 002.
===============================================================================
Summary: Critique 001 24 April 2010
Genetic effects on alcohol metabolism modify the relation of alcohol to breast cancer
A study from Germany compared the association between alcohol and breast cancer risk according to genetic variations affecting levels of alcohol dehydrogenase, an enzyme that clears alcohol from the blood stream. The authors conclude that genetic factors associated with the slow clearance of alcohol are associated with increased risk of breast cancer for drinkers; an increase in cancer risk was not seen for drinkers with genetic factors leading to fast clearance of alcohol. Such a finding would suggest that alcohol itself is the cause of an increase in breast cancer risk among drinkers.
Unfortunately, some previous studies have shown the opposite, that an increase in breast cancer risk occurs only among women who have genes associated with fast, rather than slow, alcohol metabolism. Overall, current scientific data indicate that breast cancer’s relation to drinking is not resolved, remaining murky and conflicted, and perhaps overemphasized. This facet of that murkiness is itself also conflicted. As of now, it is unclear the degree to which genes affecting alcohol dehydrogenase modify the association between alcohol and the risk of breast cancer and other diseases.
Reference
Larsen SB, Vogel U, Christensen J, Hansen RD, Wallin H, Overvad K, Tjønneland A, Tolstrup I. Interaction between ADH1C Arg272Gln and alcohol intake in relation to breast cancer risk suggests that ethanol is the causal factor in alcohol related breast cancer. Cancer Letters, 2010, in press.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 001.
=====================================================
Critique 256: Alcohol consumption and health outcomes among 70 year olds in Sweden –22 August 2022
In a population-based cohort of 70-year-old men and women recruited in Gothenburg, Sweden, in 2014-2016, the authors of this paper have presented a detailed listing of many social, environmental, and biological factors that relate to non-drinking, former drinking, or current drinking of varying amounts of alcohol. Our Forum critique raises some questions about the traditional belief that the elderly should consume markedly less alcohol than younger subjects, and that the limitations placed on subjects related sorely to their age may often not be appropriate.
The paper emphasizes how a very large number of factors may modify the association between the amount of alcohol consumed and measures of health and disease. Many of these, such as indices of socio-economic state, are usually adjusted for in epidemiologic studies. Data on other factors that relate to alcohol consumption (such as self-related health, having a partner, grip strength, having others worried about their drinking, religiosity, gait speed, life satisfaction, etc.) represent data usually not collected in epidemiologic studies.
Forum members thought that these analyses show that subjects whose reported alcohol intake is only slightly above the recommended “safe” levels for subjects of this age should not be classified as “at-risk” drinkers. Most of their features match those of subjects reporting intake within current recommendations; certainly, they do not match the characteristics of heavier drinkers.
Forum members also pointed out that in addition to improved mortality associated with truly moderate drinking, as seen in essentially all epidemiologic studies, these analyses demonstrate that many other components of “successful ageing” are also associated with regular, moderate consumption of alcohol.
Reference: Ahlner F, Erhag HF, Johansson L, Fässberg MM, Sterner TR, Samuelsson J. Zettergren A, Waern M, Skoog I. Patterns of Alcohol Consumption and Associated Factors in a Population-Based Sample of 70-Year-Olds: Data from the Gothenburg H70 Birth Cohort Study 2014–16.
Int J Environ Res Public Health 2022;19:8248; https://doi.org/10.3390/ijerph1914824
Comments on this critique by the International Scientific Forum on Alcohol Research have been provided by the following members:
Giovanni de Gaetano, MD, PhD, Department of Epidemiology and Prevention, IRCCS Istituto Neurologico Mediterraneo NEUROMED, Pozzilli, Italy
Curtis Ellison, MD, Professor of Medicine, Emeritus; Section of Preventive Medicine & Epidemiology, Boston University School of Medicine, Boston, MA, US
Harvey Finkel, MD, Hematology/Oncology, Retired (Formerly, Clinical Professor of Medicine, Boston University Medical Center, Boston, MA, USA)
Tedd Goldfinger, DO, FACC, Desert Cardiology of Tucson Heart Center, University of Arizona School of Medicine, Tucson, AZ, USA
Dominique Lanzmann-Petithory, MD, PhD, Nutrition Geriatrics, Hôpital Emile Roux, APHP Paris, Limeil-Brévannes, France
Linda McEvoy, PhD, Department of Radiology, University of California at San Diego (UCSD), La Jolla, CA, USA
Erik Skovenborg, MD, specialized in family medicine, member of the Scandinavian Medical Alcohol Board, Aarhus, Denmark
Creina Stockley, PhD, MSc Clinical Pharmacology, MBA; Principal, Stockley Health and Regulatory Solutions; Adjunct Senior Lecturer, The University of Adelaide, Adelaide, Australia
Arne Svilaas, MD, PhD, general practice and lipidology, Oslo University Hospital, Oslo, Norway
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please type in www.alcoholresearchforum.org/critique-256.
=====================================================
Critique 255: Wine consumption and the risk of cognitive decline in the elderly – 29 June 2022
The results of this systematic review and meta-analysis of longitudinal studies showed that, in almost every study, both wine consumption within the usual guidelines (no more than 2 drinks/day for men or 1 drink/day for women), as well as consumption in excess of these limits, were similarly associated with a lower risk of cognitive decline. For studies providing data on the amount of alcohol consumed, the risk of cognitive decline was reduced by 41% for both wine consumers drinking within the recommended guidelines as well as those reporting wine consumption in excess of the guidelines, when compared with abstainers. In studies where the amount of wine consumption was not reported, the estimate was an 18% reduction in the risk of cognitive decline for wine consumers versus abstainers.
Forum members noted that many potential confounders of the relation of alcoholic beverage consumption and cognition may modify the effects of alcohol on cognition, and were not evaluated very well in this study. Especially important may be the pattern of drinking (regularly or irregularly, with or without food, with associated binge drinking, etc), Forum members agreed that the calculations of the authors support a protective effect of wine consumption against cognitive decline, but their conclusions may be limited because of residual confounding by the pattern of drinking and other key factors not included in their analyses.
Forum members also noted another recent paper relating brain MRI markers to alcohol intake. However, changes in cognitive function were not assessed in the latter paper, and a direct comparison between the two papers cannot be done. However, we conclude that there remain questions regarding the effects of wine and other beverages containing alcohol on cognition. Other studies have shown divergent effects on the risk of dementia associated with wine consumption and the intake of spirits, so there may indeed be different effects on cognition with wine intake, the factor studied in the present paper. And, when compared with non-drinking or drinking of other beverages, extensive research supports health and mortality advantages when wine is consumed moderately, and especially with meals.
Reference:Lucerón-Lucas-Torres M, Cavero-Redondo I, Martínez-Vizcaíno V, Saz-Lara A, Pascual-Morena C, Álvarez-Bueno C. Association Between Wine Consumption and Cognitive Decline in Older People: A Systematic Review and Meta-Analysis of Longitudinal Studies. Frontiers in Nutrition 2022;9:863059
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
=====================================================
Critique 254: Adjusting for underreporting of alcohol intake in epidemiologic studies – 13 April 2022
It has been demonstrated repeatedly that the total population alcohol consumption based on self-reports by subjects in surveys and epidemiologic studies is lower than the amount of alcohol sold or taxed (disappearance data) within the population. This is assumed to relate to marked underreporting of individuals of their consumption, sometimes by one half or more. A key problem in attempting to adjust the self-reported values to more closely match the total alcohol disappearance data is that everyone does not underreport their intake, or may do so by different degrees.
The present study was based on data from US adults who responded to the 2011-2015 Behavioral Risk Factor Surveillance System (BRFSS; N = 2,198,089). The authors tested six methods for adjusting the self-reported data to provide what they hoped to be a more accurate value; some methods included adjustments based on differences in consumption by age and sex subgroups. From an unadjusted value of self-reported consumption of only 31.3% of that indicated by disappearance data, the various methods provided adjusted values ranging from 36.1% to 73%. The authors then used higher values to estimate the effect on alcohol-attributable deaths, using a population-attributable fraction approach.
While applauding the authors for attempting to obtain better estimates of alcohol consumption, Forum members were surprised that the authors did not even mention the method for identifying underreporting of individual subjects described by Klatsky and colleagues in the Kaiser Permanente Studies. The results of their method have been demonstrated to relate closely to alcohol’s effects on the risk of cancer, hypertension, and total mortality. Their method includes, in addition to self-reported data on alcohol consumption, adjustments for a variety of health conditions known to relate to excessive alcohol exposure, including alcoholic liver disease, hospitalizations for intoxication, mental problems associated with heavy drinking, etc. The presence of these conditions not only suggested that such subjects markedly underreported their intake (the exposure), but they also had much higher risk of adverse health effects (the outcome). When these conditions were not present at any of the study visits of subjects (allowing such subjects to be classified as being unlikely to be underreporting their alcohol consumption), adverse effects of low to moderate alcohol intake were generally not seen or their occurrences were markedly less frequent. This adjustment approach seems to be the only one previously described that gives reasonable results for individuals, and is clearly associated with the future health outcomes of subjects (and we realize that the occurrence of certain diseases or death happens for individual subjects, not for the population).
The Forum also raised questions about using “alcohol-attributable risk”. The authors base their calculations of population attributable risk on the hypothetic assumption of a rather low degree of underreporting in the population studies that are used as foundation of relative risk associations between alcohol intake and disease. Thus, risk is based mainly on self-reports of intake, even though their present paper indicates that adjustment for underreporting is so important. Further, throughout the paper, it appears that the authors tend to focus only on the adverse effects of alcohol without taking into regard the beneficial effects of light-to-moderate drinking, especially the regular consumption of wine with meals, which is found almost universally to be associated with lower risk of cardiovascular disease, diabetes, and total mortality.
While appropriate adjustment for underreporting could greatly improve the results of epidemiologic studies on alcohol and health, the goal would be to develop methods of determining the risk of individual subjects by including data on their own pattern of drinking and not assuming that the same adjustment formula applies to everyone in a population. By being able to identify subjects who underreport their intake, it would lead to some people changing categories of intake, and should result in estimates of either a lower risk, or greater risk, of adverse health effects of alcohol for that category of drinking. Further, more accurate and updated assessments of future health conditions that may be adversely (or beneficially) related to alcohol consumption should improve results and provide better data for setting drinking guidelines.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 253 – The relation of alcohol consumption to the risk of glioma tumors of the brain – 5 January 2022
There appears to be an increase in the risk of glioma tumors of the brain, yet very few lifestyle or genetic factors shown to be true “risk factors” for the disease have been identified. The authors of this paper present the association between reported alcohol consumption from multiple assessments over decades and the diagnosis of such tumors, combining data from subjects in large cohort studies of nurses and male health care providers. Among the important strengths of this paper is the fact that the data were collected as part of a prospective study, difficult to do in cancer epidemiology except with very large cohorts. A total of 554 cases of glioma tumors were identified in these cohorts from a total sample of more than 200,000 subjects.
Forum reviewers agree with the conclusions of the authors that light-to-moderate alcohol consumption does not increase the risk of glioma; in fact, total alcohol consumption over many decades was found to reduce the risk. For example, a cumulative average consumption of total alcohol of >8 to 15 g/d (approximately 0.5 to 1.0 drink/day) was associated with a 25% lower risk of glioma when compared with the lowest category of intake (0 to 0.5 g/day) for both men and women. For consumers of > 15 g/d (just over 1 typical drink/day) versus the referent group, the risk for women was further significantly reduced to HR = 0.61; for men, the HR estimate was 0.79, but not statistically significant. (Some previous cohort studies have suggested an increase in risk for heavy drinkers.) There were no differences according to type of alcoholic beverage. For the subgroup of subjects with glioblastomas, findings were similar but less precise, due to smaller case counts.
The Forum concludes that light-to-moderate alcohol consumption, versus no alcohol intake or very occasional drinking, does not increase the risk; in this very well-done study, such consumption showed a significant reduction in the risk of glioma tumors of the brain.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 252: Dealing with previous alcohol exposure among “current non-drinkers” in epidemiologic studies testing the J-shaped curve – 3 December 2021
Most cohort studies have demonstrated a reduced risk of cardiovascular diseases, diabetes, and even dementia among light-to-moderate consumers of alcohol when compared with lifetime abstainers. This is often described as a “J-shaped curve,” a reduction in disease risk for light drinkers (compared with abstainers) but an increase in risk for heavy drinkers. Many criticisms of the J-shaped curve have been based on claims that many studies include “sick quitters” in their referent group. Such criticisms ignore most recent cohort studies in which only lifetime abstainers make up the referent group. Epidemiologists have known for decades that including ex-drinkers in the referent group for evaluating health effects of alcohol is an error; such a group cannot be used for comparisons with moderate drinkers.
While the present study from a large cohort in Germany clearly shows how previous alcohol excess and other unhealthy lifestyle factors and socio-economic factors influence the risk of many diseases, it creates a referent group made up of mixing lifetime abstainers and some ex-drinkers, and that their analyses show that this group does not have a higher risk of mortality than light drinkers (thus, the protection of light drinking leading to a decrease in risk of disease is erroneous). The authors of this paper apparently did this because they had such a small group of lifetime abstainers (only 42 subjects out of a cohort of 4,000!), a number grossly inadequate for comparisons with drinkers.
Forum members agreed that it was a serious error for the investigators; instead of admitting that their numbers were too low in this group for reliable comparisons, it appears that the authors augmented the comparison group with a group of ex-drinkers (that they considered to not be heavy drinkers) and reported that their analyses do not support a reduced risk among light drinkers. Thus, their claim that the lower risk of cardiovascular disease demonstrated in most studies among moderate drinkers is unrelated to alcohol consumption. However, this claim is based on an improper referent group used in their analyses. Forum members considered this to be a deeply flawed analysis, and of no merit for use in setting drinking guidelines.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 251: Does moderate drinking increase, or decrease, the risk of falls in middle-age to elderly adults? 1 November 2021
To judge the relation of reported alcohol consumption to the risk of subsequent falls requiring hospitalization, the authors of this paper used data from the EPIC-Norfolk study, a prospective population-based cohort study in Norfolk, UK. In that study, there were a total of 25,637 community-dwelling adults, aged 40–79 years when recruited. The main outcome was the first hospital admission due to a fall over a follow-up period of about 11.5 years.
The key results of the study were that 19.2 % of non-drinkers were hospitalized for a fall during follow up, compared with 13.7% of low drinkers, 10.9 % of moderate drinkers, and 12.3% of heavy drinkers. In addition, the cumulative incident rates for falls at 121-180 months of follow up were 11.08% for teetotalers, 7.53% for low drinkers, 5.91% for moderate drinkers, and 8.20 % for heavy drinkers.
Forum members considered this to be a well-done study, with the analysis adjusting for a large number of factors that were potential confounders of the relation of alcohol intake to the risk of falls. We agree with the conclusions of the authors: “Moderate alcohol consumption appears to be associated with a reduced risk of falls hospitalization, and intake above the recommended limit is associated with an increased risk,” although we note that the increase in risk for heavier drinkers only appeared after essentially all covariates were added to the analysis. Obviously, residual confounding is always a possibility, but the present analyses indicating some protection against falls among light-to-moderate drinkers are supported by some well-done previous research.
The results of this study do not support the claim that any alcohol increases the risk of falls in older adults. It appears that this is not a concern for light-to-moderate drinkers who, in this study, had a lower risk of falls requiring hospitalization than did non-drinkers.
Reference: Tan GJ, Tan MP, Luben RN, Wareham NJ, Khaw K-T, Myint PK. The relationship between alcohol intake and falls hospitalization: Results from the EPIC-Norfolk. Geriatr Gerontol Int 2021;21:657-663.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 250: Importance of a favorable pattern of drinking (regularly, and with food) on risk of mortality – 28 July 2021
This is an analysis based on a very large data base of alcohol consumers (subjects reporting > 0 g of alcohol/week) from the UK Biobank (analyses based on 316,627 subjects with a median follow up of 8.9 years). The authors constructed categories of Drinking Habit Scores (DHS) for subjects; a “favorable” DHS was used for those subjects reporting a drinking frequency of 3 or more days/week and consuming alcohol with meals. The investigators then related the DHS categories to subsequent all-cause and cause-specific mortality, with adjustments for essentially all of the common known confounders/modifiers of alcohol effect.
Overall, Forum reviewers agreed with the main outcomes of the study, which indicate that subjects with a favorable DHS (in comparison with other drinkers) had significantly lower all-cause mortality (HR=0.82), CVD mortality (HR=0.84); cancer mortality (HR=0.82), and death from other causes (HR=0.77). In relation to the number of drinks consumed, the authors report that for all-cause, CVD, and other cause mortality, subjects with a favorable DHS showed a U-shaped or L-shaped curve (in that even for the heaviest drinkers, the mortality risk remained the same or lower than that of abstainers). Only for cancer mortality was there an increase in risk for subjects in the highest category of alcohol intake, leading to a J-shaped curve.
While the authors did not report specifically on the types of beverage being consumed in their favorable drinking pattern, it is the typical pattern generally found in southern Europe, and typically it is wine with meals. In these societies, wine is considered part of the meal, and is not consumed as “shots” that are usually being taken primarily as a way of getting drunk. As described in this paper, it is important to separate the health effects of these opposite approaches for consuming a beverage containing alcohol; putting all subjects into groups based only on the grams of alcohol consumed over a period, usually a week, does not take into account the important differences associated with the pattern of drinking.
We are finally appreciating that we are much further along in our research on alcohol and health than the innumerable studies that have focused just the amount of alcohol consumed, or on the J-shaped curve. We now realize the importance of the pattern of drinking. This constitutes not only the type of beverage and frequency of drinking, but also the consumption of alcohol with food and the absence of binge drinking. The pattern of drinking appears to be as important as, or even more important than, the quantity of alcohol consumed.
Reference: Ma H, Li X, Zhou T, Sun D, Shai I, Heianza Y, Rimm EB, Manson JE, Qi L. Alcohol Consumption Levels as Compared With Drinking Habits in Predicting All-Cause Mortality and Cause-Specific Mortality in Current Drinkers. Mayo Clin Proc 2021;96:1758-1769.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
========================================================
Critique 249: Does light-to-moderate drinking increase the risk of atrial fibrillation? — 23 June 2021
While many epidemiologic studies have demonstrated an increase in the risk of AF for consumers of alcoholic beverages, there remains a question as to whether or not there is a threshold amount that would increase the risk. The present study concludes that “less than two alcohol units/day significantly increased the risk of incident AF, however, in men only. Reduction of even a moderate alcohol intake may thus reduce the risk of AF at the population level.”
While this may be the case, Forum members had a number of concerns about using the results of the present study to determine whether or not there is a threshold amount of alcohol necessary to increase the risk of AF. The methods used to judge alcohol consumption did not report the type of beverage or have a good estimate of the pattern of drinking, both of which factors are known to modify the health effects of alcohol. Further, the authors stated that there was evidence of considerable under-reporting of alcohol in their cohort, as the level of HDL noted in their “light” drinkers was above the level expected. This suggested to them that subjects in their lowest category of alcohol may actually have consumed more than they reported (probably about twice the reported amount of alcohol). This makes it difficult to determine if truly “light” drinking is associated with an increased risk of AF.
Overall, scientific data continue to show that light-to-moderate alcohol intake, especially when the pattern of drinking is found to be regular moderate consumption with food and without binge drinking, is associated with a lower risk of ischemic stroke and death. For the effects of alcohol intake on the risk of AF, the situation remains unclear. Unfortunately, the present study cannot answer the question as to whether there is, or is not, a clear threshold effect of alcohol intake on the risk of developing AF.
Reference: Ariansen I, Degerud E, Gjesdal K, Tell GS, Næss O. Examining the lower range of the association between alcohol intake and risk of incident hospitalization with atrial fibrillation. IJC Heart & Vasculature 2020;31:100679.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 248: Association of Alcohol Consumption with Cataract Surgery — 19 April 2021
This was a well-done analysis of a very large number of cases of cataract surgery in the UK; there were reasonable measures of the exposure (alcohol consumption), including the amount and type of beverage consumed, and appropriate potentially confounding factors were taken into consideration. However, data on the consumption of alcohol with or without food were not available. The use of national registries of cataract surgery provide an appropriate approach for estimating the main outcome of the analyses, and the results probably reflect the incidence of clinically significant cataract occurrence in these populations.
The key results were that there was a small but highly significant lower risk of cataract surgery among moderate drinkers. Red and white wine consumers showed more consistent and significantly lower risks of cataract surgery than consumers of other beverages. (In one of the two studies included in the analysis, small amounts of beer and spirits also showed a lower risk than that of non-drinkers.) There were too few heavy drinkers in these studies to determine the extent to which such drinking might affect risk. We appreciate that residual confounding, especially by factors that relate to subjects choosing to have surgical treatment of their cataracts, could still be present in these results.
Forum reviewers conclude that, in agreement with the investigators of this study, the data indicate a small but statistically and clinically significant decrease in the risk of cataract surgery for low-to-moderate drinkers, versus non-drinkers. A lowering of risk was especially clear for wine drinkers, in comparison with consumers of beer and spirits. There is an extensive literature regarding potential mechanisms by which constituents of the diet, especially those present in wine, may influence the development of cataracts. Among these are antioxidants or ROS scavengers, aldose reductase inhibitors, antiglycating agents, and inhibitors of lens epithelial cell apoptosis. However, the ultimate reason for the lower risk of cataract surgery associated with wine consumption found in this study has not been clearly delineated.
Reference: Chua SYL, Luben RN, Hayat S, Broadway DC, Khaw K-T, Warwick A, et al, on behalf of The UK Biobank Eye and Vision Consortium. Alcohol Consumption and Incident Cataract Surgery in Two Large UK Cohorts. Ophthalmology 2021, pre-publication.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 247: Effects of alcohol consumption on risk of stroke and systemic embolism among subjects with atrial fibrillation – 15 March 2021
The main aim of the current study was to investigate the associations of regular alcohol intake with incident stroke or systemic embolism in patients with established atrial fibrillation (AF), most of whom (84%) were on anti-coagulant therapy. The authors used combined data from two prospective studies of subjects with AF, followed for an average of 3 years. While they excluded subjects with “only short, potentially reversible AF episodes (e.g., as after cardiac surgery or sepsis)” about one half of subjects in the study were diagnosed as having paroxysmal AF. Reported alcohol at baseline and at subsequent examinations was classified as none, > 0 to < 1 drink/day, 1 to < 2 drinks/day, and ≥ 2 drinks/day.
The primary outcome was a composite of stroke and systemic embolism. Secondary outcomes were all-cause mortality, myocardial infarction, hospital admission for acute heart failure, and a composite of major and clinically relevant nonmajor bleeding. In their analyses, they adjusted for age, sex, education, hypertension, history of heart failure, history of diabetes, BMI, smoking status, physical activity, history of stroke, history of coronary heart disease, oral anticoagulation, history of renal failure, AF type, and health perception. With annual assessments, the investigators updated all covariates over time, if appropriate.
The main results indicated no significant effect of alcohol consumption on the risk of the major outcomes (stroke or systemic embolism). However, there were significant decreases in risk for several secondary outcomes. For hospital admissions for heart failure, in comparison with non-drinkers the HR for moderate drinkers was 0.60 (CI 0.41-0.87); further, among moderate drinkers the HR for myocardial infarction was 0.39 (CI 0.20 – 0.78), and for all-cause mortality the HR was 0.49 (CI 0.35-0.69).
Forum members had two major concerns with the paper. First, the authors failed to report specifically how alcohol consumption was associated with increased or decreased presence of AF during follow up, even though approximately one-half of subjects had only paroxysmal AF at baseline. Determining if alcohol consumption affected subsequent AF would be information of importance to practitioners who are advising their patients with AF regarding alcohol consumption.
Secondly, it was pointed out by Forum members that the results may have been affected by what is known as collider bias: as moderate drinking shows an inverse association with coronary heart disease (which is strongly related to the presence of AF), subjects who consumed alcohol prior to the baseline diagnosis of AF were probably different from those who had no prior alcohol exposure, and the results of combining these two groups (as was done in these analyses) may have been biased. Such bias usually tends to result in estimates of effect going toward the null.
While the reported results of no real effect of alcohol consumption on the risk of stroke or systemic embolism among patients with AF is encouraging, to decrease the risk of bias in future studies it will be important that such research attempts to separate subjects according to their prior use of alcohol before baseline measurements are assessed. The marked reduction in the risk of other major cardiovascular outcomes and total mortality, found in this study to be associated with light to moderate drinking, matches the results seen in most previous studies.
Reference: Reddiess P, Aeschbacher S, Meyre P, Coslovsky M, Kühne M, Rodondi N, et al, for the BEAT-AF and Swiss-AF investigators. Alcohol consumption and risk of cardiovascular outcomes and bleeding in patients with established atrial fibrillation. CMAJ 2020;193:E117-E123. doi: 10.1503/cmaj.200778
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 246: Light to moderate alcohol intake and the risk of cancer — 8 February 2021
The present paper attempts to use alcohol-attributable data, based on combining average alcohol intake from diverse European populations, to judge the effects of moderate alcohol consumption on the risk of cancer for all populations. It is based on earlier calculations of risk, extensively covered in previous publications by the senior author. The investigators conclude that the risk of a number of types of cancer are increased even among subjects reporting no more than 20 grams of alcohol per day (up to about 2 typical drinks), an amount they state to be within recommended levels of consumption (but exceed current US Drinking Guidelines for women of no more than 1 drink/day). The largest contribution to their calculated effects of alcohol was from breast cancer in women (which made up “68.7% of all alcohol attributable cancer for both sexes”). Breast cancer is a condition for which many factors other than just average alcohol intake are important: factors such as pattern of drinking, type of beverage, folate intake, smoking, obesity, physical activity, etc., all of which tend to confound the association.
Forum members had real concerns about their methodology of using an estimate of “alcohol-attributable cancer” based on reported average intake from 28 separate countries, including the large countries in western Europe (e.g., Germany, France, UK, Italy, Spain, Sweden), East-European countries (such as Poland and Hungary), and many smaller countries (e.g., Malta, Cyprus, Luxembourg, Latvia). Given the marked variation in culture and drinking patterns among these countries, it was considered that there are a large number of confounders and modifiers of alcohol effects that vary by country, and make it impossible to simply take the average alcohol intake from such diverse cultures to estimate causality of alcohol and cancer for everyone. By lumping data from all of these countries, the analyses end up with values that relate to a non-existent hypothetical population; different countries have different risk relationships, so the estimates of effect described in the paper apply to no single country.
Further, the investigators do not report rates of other outcomes, especially total mortality, associated with drinking. Taking only one outcome condition, without at least noting that moderate drinking has almost uniformly been found to decrease all-cause mortality, limits the usefulness of their results for setting alcohol guidelines. Heavy alcohol use is recognized by all as a serious impediment to the health of individuals, and to society at large. However, recommending lowering the intake of alcohol for everyone does not take into consideration that light drinkers might be more likely than heavy drinkers to follow such advice and might decrease their consumption to zero. Because of moderate drinking’s almost uniformly demonstrated beneficial effect on cardiovascular disease, if many light drinkers stopped drinking completely it would be expected to increase, rather than decrease, total mortality rates and the health of the population.
In their conclusions, the authors only mention the results of their actual analyses briefly, then start the usual chant of the need for extensive public health measures (warning labels, public information campaigns, increasing alcohol taxes, etc.) which tend to emphasize the dangers of any alcohol consumption. However, the analyses in this paper do not provide the data that are needed if one is to set appropriate drinking guidelines, which should be age-specific, sex-specific, and population-specific. Such factors would include not only the alcohol-disease relation but the particular characteristics of the population, the objective of guidelines (to influence and change behavior among target populations), the behavior that is thought to be in need of change, the culture and mindset of the target population, and the kind of message that is likely to be effective. Forum members realize that there are tensions between advice intended only to reduce the prevalence of misuse versus advice that takes into account the well demonstrated beneficial health effects of light-to-moderate consumption. When setting guidelines, it is important to take into account the prevailing drinking culture of a country or population, because only in that way is it possible to produce a public health message that is likely to be respected and regarded.
Reference: Rovira P, Rehm J. Estimation of cancers caused by light to moderate alcohol consumption in the European Union. European Journal of Public Health 2021; pre-publication. doi:10.1093/eurpub/ckaa236.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================
Critique 245: Effects of different patterns of alcohol consumption on risk of mortality, major cardiovascular events, cirrhosis, and cancer — 25 January 2021
This study was designed to determine factors that affect the pattern of alcohol consumption (including the frequency of consumption, type of beverage, with or without food, etc.), rather than just the reported average amount of alcohol, related to all-cause mortality, major cardiovascular events-MACE (MI/stroke/cardiovascular death), accidents/injuries, liver cirrhosis, all-cause and alcohol-related cancer incidence. It was based on a large prospective cohort study of UK Biobank (UKB) participants and included more than 300,000 subjects; outcomes were ascertained over a 9-year median follow-up period. Non-drinkers and only occasional drinkers were excluded from the analyses, so this paper does not judge the effects of light or moderate drinking versus not drinking, but only the effects of the pattern of reported alcohol consumption among regular drinkers.
The study showed that in comparison with subjects who consumed red wine more than 50% of the time (the reference group) there were lower risks of many adverse outcomes than among consumers of more than 50% of the time of spirits; the latter had 25% greater risk of all-cause mortality, 31% greater risk of MACE, and 48% higher risk of liver cirrhosis after controlling for total weekly alcohol consumption and relevant confounders. In comparison with red-wine drinkers, consumers of beer/cider showed an 18% higher risk for all-cause mortality, 16% higher risk of MACE, and 36% higher risk of liver cirrhosis. There were no statistically significant differences in outcomes between white wine drinkers and red wine drinkers.
Consumption of alcohol with food, versus not with food, showed a 10% (CI 2%-17%) lower risk of all-cause mortality. While consumers reporting alcohol consumption 3-4 days/week had lower risk of some adverse outcomes than subjects reporting intake on only 1-2 days/week, for some reasons subjects reporting daily or near-daily intake had an increased risk of liver cirrhosis, probably related to under-reporting by some heavy drinkers.
Forum members agree with the conclusions of this study as reported in the Authors’ Abstract: “Red wine drinking, consumption with food and spreading alcohol intake over 3–4 days were associated with lower risk of mortality and vascular events among regular alcohol drinkers, after adjusting for the effects of average amount consumed.” The results of this well-done study emphasize how inappropriate it is to use just the total average alcohol intake when relating the consumption of alcoholic beverages to the risk of adverse health outcomes.
Reference: Jani BD, McQueenie R, Nicholl BI, Field R, Hanlon P, Gallacher KI, Mair FS, Lewsey J. Association between patterns of alcohol consumption (beverage type, frequency and consumption with food) and risk of adverse health outcomes: a prospective cohort study. BMC Medicine 2021;19:8. https://doi.org/10.1186/s12916-020-01878-2.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 244: Is “ideal cardiovascular health” more common among consumers of wine than among drinkers of other beverages? — 18 December 2020
While a beneficial effect on cardiovascular disease of moderate drinking has been shown repeatedly in epidemiologic studies, the specific effects of different types of alcohol have not been well established. The authors examined the relation between alcohol type and an index of ideal cardiovascular health (CVH) as measured by the American Heart Association’s seven CVH metrics. Data from more than six thousand men and women, participants in the Multi-Ethnic Study of Atherosclerosis, were used to relate the association of the consumption of wine, beer, and liquor to the CVH score.
The authors report that participants who consumed 1-2 drinks/day of wine had higher odds of optimal CVH scores compared to those who never drank wine [adjusted prevalence odds ratio (POR) 1.64 (1.12-2.40)]. However, in comparison with participants who never drank beer or liquor, the odds of optimal CVH scores were lower for consumers of these beverages.
Forum members had some questions about the methodology for judging intake of the different beverages, as well as the statistical approach used in these analyses. However, they consider that the results (more favorable associations with wine consumption than from that of other beverages on indices of cardiovascular health) are in line with most previous studies.
It is important to realize that this study did not measure effects on the risk of disease occurrence or mortality, but just on the CVH index, a measure of overall cardiovascular health. Thus, we cannot tell specifically from this study whether the higher health indices among moderate wine drinkers was the result of the wine that they drink (even though this might be expected to some extent since, for example, moderate wine intake is known to favorably affect BMI, blood lipids, and blood glucose) or that their results relate to the fact that people with more moderate lifestyles and higher education, income, etc., tend to prefer moderate wine consumption and are less likely to be binge or heavy drinkers. It may be that wine drinkers make better decisions on all lifestyle behaviors than consumers of other beverages.
Reference: Ogunmoroti O, Osibogun O, McClelland RL, Lazo M, Mathews L, Okunrintemi V, Oni ET, Burke GL, Michos ED. Alcohol type and ideal cardiovascular health among adults of the Multi-Ethnic Study of Atherosclerosis. Drug and Alcohol Dependence 2020: Pre-publication release
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 243: Does the “quality” of the diet modify the relation of alcohol intake to the risk of hypertension? – 19 October 2020
The authors of this paper test the hypothesis that overall diet quality influences associations between alcohol consumption and the risk of hypertension, based on data from a study in the USA (NHANES) and two studies in China. In general, their designation of a “high-quality” diet for Chinese was one with greater amounts of fruit, vegetables, and beans, while for Caucasians and Hispanics it was one with more whole grains, fruit, vegetables and nuts; “low-quality” diets were mainly those with higher intakes of red meat products. For comparisons with abstainers, subjects reporting < 7 drinks/week for total alcohol were categorized as light and those reporting 7-21 drinks/week categorized as moderate drinkers, with those reporting more referred to as heavy drinkers.
The paper concludes that light alcohol consumption among subjects with a high-quality diet was significantly associated with a decreased risk of hypertension in Caucasians, and the risk of hypertension was not significantly increased with increasing alcohol consumption in Caucasians, Chinese, and Hispanics. On the contrary, in context of a diet calculated to be low quality the risk of hypertension was significantly increased in a linear fashion with increasing alcohol consumption in all groups except African Americans.
Forum reviewers considered this to be a generally well-done and interesting study, but had concern that the authors may not have adjusted adequately for a factor strongly related to diet quality: socio-economic status. The authors included in their analyses whether or not subjects had a high school diploma, but no adjustments were made for occupation, income, or other important indices of deprivation, which may be important since lower SES subjects have consistently been shown to have poorer diets. Thus, we are unsure whether or not it is the diet solely that is the reason that alcohol consumption was found to be associated with lower, higher, or no effect depending on the type of diet. Further, no results are shown indicating whether or not there were differences if the beverage consumed was beer, wine, or spirits, and there was insufficient data on the pattern of drinking. The authors begin their abstract saying that ‘Alcohol is commonly consumed around mealtimes,’ but apparently do not have any data on whether the beverage was consumed with or without food for the present analyses.” All of these factors may modify how alcohol affects the risk of developing hypertension.
Finally, some Forum members were uneasy with the term “quality of diet”, based on the inclusion or exclusion of certain foods, which may be very important to taste. Said one member, we trust that diets recommended as being of “high quality” are not those whose savor has been removed.
Reference: Jiang W, Meng X, Hou W, Wu X, Wang W, Wang M, Chu X, Wang P, Sun C, Han T, Li Y. Impact of overall diet quality on association between alcohol consumption and risk of hypertension: evidence from two national surveys with multiple ethnics. Eur J Clin Nutr 2020; doi.org/10.1038/s41430-020-00708-1.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
=========================================================================
Critique 242: The relation of light alcohol consumption to the risk of common cancers – 1 October 2020
In an attempt to assess the relation between light alcohol consumption (<12.5g per day) and the risk of a number of types of cancer, the authors carried out a review of meta-analyses published within the past 15 years. Using as keywords “light alcohol drinking,” “light alcohol consumption” and “cancer”, they found 29 meta-analyses on the subject. They report their results as indicating that “Light alcohol drinking was not associated with an increased risk of cancer occurrence, with the exception of breast and prostate cancer and melanoma. Furthermore, a possible protective role of light alcohol consumption on the development of bladder, kidney and ovarian cancer and Non Hodgkin Lymphoma was observed.”
Forum reviewers found a number of weaknesses in the paper. While their title focuses on “light alcohol drinking,” most of their reports of results and their discussion deal with harmful effects of heavier drinking; however, by not including papers on ‘heavy drinking’ in their original search, they may have left out many relevant papers. Further, the very brief reviews of each common cancer that they comment upon are sometimes based on only one or two meta-analyses, leaving out a huge amount of key data, especially that from single, well-done, long-term cohort studies with important information on the relation of alcohol to cancer; potential confounding by many factors could not be taken into consideration.
In the analyses in the present paper, the reported average level of alcohol consumed is used, but there is insufficient evaluation of possibly more important indices of alcohol exposure: the pattern of drinking (e.g., type of beverage consumed, in binges or on a regular basis, consumption with or without food, etc.). Further, there is probably inadequate control for important confounders or consideration of the effects of under-reporting, which may have been seen in single studies but not apparent in meta-analyses. In addition, a number of errors are present within the report, such as conflicting statements that may misrepresent the numeric data given. These problems make these results of limited use to professionals in health policy who are developing guidelines for alcohol use in the general public.
Reference: Caprio GG, Picascia D, Dallio M, Vitiello PP, Giunta EF, De Falco V, et al. Light Alcohol Drinking and the Risk of Cancer Development: A Controversial Relationship. Reviews on Recent Clinical Trials 2020;15:164-177
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 241: A Mendelian randomization study of alcohol consumption and the risk of breast cancer and ovarian cancer reveals no significant associations — 22 July 2020
The authors of this ambitious study used a Mendelian Randomization (MR) approach in an attempt to determine if alcohol consumption is causally associated with the risk of female hormone-dependent cancers. They used summary level genetic data from the hitherto largest genome-wide association study (GWAS) conducted on alcohol consumption (N = ~1.5 million individuals), breast cancer (N cases = 122,977) and ovarian cancer (N cases = 25,509). They examined three different alcohol intake exposures: drinks per week, alcohol use disorder (AUD) and age-adjusted alcohol use disorder identification test (AUDIT-C), to reflect general and harmful drinking behavior. For instrumental variables (IVs), they constructed updated and stronger genetic instruments using 99 SNPs related to drinks/week, 9 SNPs related to AUD, and 13 AUDIT-C-related SNPs, and estimated the causal relationship applying several two-sample MR methods.
The key result of these analyses was that the investigators did not find any evidence that alcohol intake increased the risk of breast cancer. For ovarian cancer, an initial inverse association with alcohol intake became null when adjustments were made for confounders. While members of our Forum agreed with the overall conclusions of the authors, who stated that they did not find “any compelling evidence in support for a causal relationship between genetically predicted alcohol consumption and risk of breast or ovarian cancer, consistent across three different alcohol-related exposures,” Forum members identified a number of weaknesses of the analyses. For example, there were very limited data on the pattern of drinking or the type of beverage consumed, and no data on smoking and other lifestyle habits, diet, and many other environmental factors that relate to the effects of alcohol consumption. Further, much of the data utilized to generate the IVs of alcohol exposure were from men, rather than women, although the two conditions being studied are present only in women.
Forum members agreed with the authors about the need to combine data from MR analyses with data from observational and experimental studies before making conclusions about the relation of alcohol consumption to health and disease. Given the rapid expansion of genetic studies, it is likely that MR analyses will be increasingly important in our research efforts, but we agree that the consideration of a combination of data from observational studies, clinical trials, animal experiments, and MR analyses will be needed as we seek to improve our knowledge on the relation of alcohol intake to health and disease; it is, and will remain, a continuing challenge.
Reference: Zhu J, Jiang X, Niu Z. Alcohol consumption and risk of breast and ovarian cancer: A Mendelian randomization study. Cancer Genetics 2020;245:35–41
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 240: Are there health risks from amounts of alcohol referred to as being within “low-risk drinking” guidelines? — 8 July 2020
The authors of this paper use very questionable data to suggest that drinking guidelines for all countries should be lowered to no more than 1 drink/day. In their analyses, they make a very large number of assumptions, including adding 80% to reported amounts of alcohol for all subjects to make up for alcohol disappearance data, and do not modify this according to their individual likelihood of being an under-reporter of intake. Further, they are not able to adjust for the pattern of drinking or type of beverage consumed, and it is considered bizarre that they grouped ex-drinkers (many of whom were apparently heavy drinkers) with current drinkers who report consuming within the guidelines to state that such subjects have a high risk of adverse effects. From the numbers presented in the tables in this paper, the risk of alcohol-attributable death for consumers of alcohol within-guidelines was fifty times lower than for those consuming above the guidelines. Such deficiencies in methodology, and especially possibly deliberate combinations of groups to support their premise, make it impossible to utilize their conclusions for setting guidelines for “low-risk” drinking.
Further, their conclusions do not reflect what the vast majority of well-done epidemiologic studies have shown for decades that light-to-moderate alcohol consumption (when defined as up to 1 drink/day for women and up to 2 drinks/day for men and not consumed in binges) is associated with a significant decrease in the risk of cardiovascular mortality as well as total mortality. The results of the current paper are not sufficient to warrant changing drinking guidelines.
Reference: Sherk A, Thomas G, Churchill S, Stockwell T. Does Drinking Within Low-Risk Guidelines Prevent Harm? Implications for High-Income Countries Using the International Model of Alcohol Harms and Policies. J Stud Alcohol Drugs 2020;81:352–361.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 239: Does the source of funding of epidemiologic studies on alcohol and health affect their results? – 28 May 2020
Funding of research by industry can lead to sponsorship bias. The aim of the current study was to evaluate for sponsorship bias in observational alcohol research by focusing on a spectrum of health outcomes related to moderate alcohol consumption. The authors utilized data from seven recent meta-analyses that included information from 386 observational studies of the relation of moderate alcohol consumption to a large number of health outcomes, including cardiovascular diseases, cancer, and mortality.
The authors report that only 5.4% of studies had some support from the alcohol industry, while 80.1% were funded by governments or other sources (non-industry-funded). Further, the results of moderate drinking on almost all health outcomes (including cardiovascular diseases and cancer) were essentially the same whether the study was funded by the beverage industry or not. Where there were slight differences, the results from non-alcohol-industry sources tended to have more favorable health results from moderate drinking than did those sponsored by the industry. The authors end their discussion stating: “In conclusion, only a small proportion of observational studies in meta-analyses, referred to by several international alcohol guidelines, are funded by the alcohol industry. Based on this selection of observational studies the association between moderate alcohol consumption and different health outcomes does not seem to be related to funding source.”
Forum members considered that the analyses were very complete, and detailed data were given in the very exhaustive supplementary material provided (exceeding 90 pages). (This makes it possible for a reevaluation of their results by others.) While Forum members noted that this analysis was apparently supported by the Dutch Beer Institute, the extensive data presented provide no evidence that there was bias in any of the analyses, upon which most international drinking guidelines have been based. The Forum concludes that the major studies that have shown that moderate drinking can have health benefits, especially for coronary heart disease and type 2 diabetes, are not based on bias because of support from the alcohol beverage industry.
Reference: Vos M, van Soest APM, Wingerden T, Janse ML, Dijk RM, Brouwer RJ, deKoning I, Feskens EJM, Sierksma A. Exploring the Influence of Alcohol Industry Funding in Observational Studies on Moderate Alcohol Consumption and Health. Adv Nutr 2020: pre-publication.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 238: Differences in evaluating confounding in epidemiologic studies when judging the effects of alcohol consumption on the risk of cardiovascular disease – 7 April 2020
The authors of the present paper compared studies included in a recent meta-analysis on alcohol consumption and the risk of coronary heart disease (CHD) for the number of potential confounding variables included in the analysis for each paper. While they found that most studies included adjustments for smoking, age, BMI, height and weight, physical activity, and education, many studies included adjustments for a multitude of other factors. They reach the conclusion that the large variation between studies in adjusting for confounding makes it impossible to accept the finding of a J-shaped curve between alcohol consumption and CHD (despite the consistency of such results).
Forum members agree that evaluating confounders in epidemiologic studies is extremely important. However, standardizing environmental confounders is not possible as there are so many, and so many yet undefined, and these confounders would be expected to vary in their influence among different populations. The authors did not focus on the key factor: the potential impact of each potential confounder. Limited research suggests that any “unknown confounder” would need to be extremely powerful to negate the reported protective effect of light-to-moderate consumption of alcohol, especially of wine, on the risk of CHD.
In addition, the authors were perturbed that many individual studies did not state specifically in their discussion that “residual confounding may be present in our results” or that “results of individual studies must be interpreted with caution.” Forum members assume that most readers of scientific reports realize that there should always be caution in making conclusions from a single study, especially observational studies, without the authors pointing in out in their paper. It may be analogous to stating that “further research is needed,” which should be assumed for any scientific paper.
Members of the Forum acknowledge that confounding makes it a difficult process to judge causality from observational studies, but point out that potential confounders in one study may be insignificant in another. It is not possible to generate a list of potential confounders that would apply to all epidemiologic studies. However, the consistency of the J-shaped curve between alcohol intake and risk of CHD in almost all epidemiologic studies, with support from a multitude of experimental studies, strongly supports the validity of such a relation.
Reference: Wallach JD, Serghiou S, Chu L, Egilman AC, Vasiliou V, Ross JS, Ioannidis JPA. Evaluation of confounding in epidemiologic studies assessing alcohol consumption on the risk of ischemic heart disease. BMC Medical Research Methodology 2020;20:64 https://doi.org/10.1186/s12874-020-0914-6
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 237: Relation of alcohol consumption in the elderly to the chances of reaching 90 years of age — 2 March 2020
An interesting and well-done study from a cohort of aging men in the Netherlands that evaluated how alcohol consumption data collected at 68 – 70 years of age related to the risk that the individual would survive to age 90. The authors report that “The highest probability of reaching 90 was found in those consuming 5–<15g/d alcohol, with RR=1.36 (95% CI, 1.20–1.55) when compared with abstainers.” Further, the authors noted that “Wine intake was positively associated with longevity (notably in women), whereas liquor was positively associated with longevity in men and inversely in women.” They also noted that there was a tendency for a lower chance of living to age 90 for subjects reporting binge drinking.
Forum members were unanimous in considering this to be an excellent study. It adds information on alcohol consumption collected in the elderly (ages 68-70 in this study) and subsequent longevity of life. It tends to counter fears expressed by some that the very elderly must be “protected” from alcohol, as it suggests that there are still health benefits from moderate drinking at all ages. Further, the reduction in risk of cardiovascular diseases is especially important in the elderly. This critique provides references to a multitude of research reports that strengthen the conclusions of the authors that, even among very elderly subjects, moderate drinking is associated with a greater longevity of life.
Reference: van den Brandt PA, Brandts L. Alcohol consumption in later life and reaching longevity: the Netherlands Cohort Study. Age and Ageing 2020;00:1–8 doi:10.1093/ageing/afaa003.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 236. Reasons for apparently diverse results from epidemiologic studies relating alcohol consumption to the risk of breast cancer 19 February 2020
The relation of alcohol consumption to the risk of breast of cancer has been the subject of innumerable epidemiologic studies over many decades, with most showing a slight increase in risk even for light drinking. However, it has been shown that this relation is attenuated when certain potential confounders are adjusted for, including folate levels, frequency of binge drinking, and the use of post-menopausal hormonal therapy. The present paper took the results of a recent large-scale meta-analysis and sought to try and explain why there is a large variability of results when the 97 studies included in that analysis were compared. The authors attempted to judge to what degree differences in exposure definitions, contrast levels, different study populations, different adjustment covariates, and different model approaches affected estimates of the effect of alcohol on cancer risk. The key factor the authors used in their analyses was the ratio between the most harmful and the most protective effects of estimated risk within each study.
All of the contrasts studied (different measures of alcohol consumption, different populations, different analytic approaches, etc.) had some effect on the estimates of effect of alcohol on the risk of cancer. As stated by the authors, “These findings suggest that whereas certain analytical and modelling choices, reflecting different types of alcohol and/or doses, can result in genuine differences, it is possible that many different analytical options, with different results, are pursued and selectively reported. Therefore, individual reported relative risk estimates from observational studies should be interpreted with caution.” Some Forum members disagreed with this conclusion, suggesting that due to marked variation in population, type of alcohol, analytic approaches, adjustment for confounding, etc., considerable error may be built in when combining data from heterogeneous studies. They felt that single large, long-term, well-done individual prospective studies may be preferable for judging the true effect of alcohol on the risk of breast cancer.
Thus, while Forum reviewers appreciated the attempt to explain differences in results of studies to get a more valid estimate of the true relation of alcohol consumption to the risk of breast cancer, and the analyses presented were done appropriately, some considered the approach described as not being a useful or valid one. Finding large differences in effects among sub-groups may not provide a reliable measure. Alternative approaches to scrutinize findings from observational studies, including Mendelian randomization or discussion centered on E-value (which assesses how strong an unmeasured confounder would have be to eliminate observed effect estimates), may be preferable. While such methods are imperfect, their use would be more interesting in informing the public and advancing scientific knowledge.
Reference: Chu L Ioannidis J PA, Egilman AC Vasiliou V, Ross JS, Wallach JD. Vibration of effects in epidemiologic studies of alcohol consumption and breast cancer risk. Inter J Epidemiol 2020;10:1–11. doi: 10.1093/ije/dyz271
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 235: Does type of alcohol or drinking pattern explain greater adverse effects of alcohol consumption among lower socio-economic subjects? 15 January 2020
The authors of this paper aimed to investigate whether and to what extent consumption by beverage type, BMI, smoking and other factors explain inequalities in alcohol-related harm evidenced though wholly attributable alcohol-related hospital admissions (ARHA). They especially evaluated levels of socio-economic status (SES) as determined by geographic and individual levels of deprivation. They based their analyses on data from 11,038 respondents to the Welsh Health Survey who answered questions on their health and lifestyle.
The results of this study support previous research on how factors associated with poor socio-economic status relate to poor health outcomes. It provides added information by providing an expanded definition for deprivation (assessed from geographic area of residence as well as from personal data), and for potential differences by type of beverage consumed. The definition of deprivation included many factors that, together, seem to be the primary reason why poorer, less educated people seem to have more adverse health effects that have been attributed to alcohol consumption.
Specifically, this study shows that the amount of alcohol consumed by people with low SES may be only a minor factor in explaining their increase in adverse effects that are usually classified as being “alcohol-related.” In this study, the frequency of alcohol consumption explained only 4% of the greater number of “wholly attributable alcohol-related hospital admissions.” Co-existing other behaviors and conditions, especially smoking, obesity, living in a deprived environment, poor health status, and mental health, appeared to have much greater effect. Thus, the conclusions of this study suggest that even for what are referred to as “wholly attributable .alcohol-related hospital admissions,” other factors associated with low SES may be more important than alcohol consumption itself as determinants of such adverse health outcomes.
Reference: Gartner A, Trefan L, Moore S, Akbari A, Paranjothy S, Farewell D. Drinking beer, wine or spirits – does it matter for inequalities in alcohol-related hospital admission? A record-linked longitudinal study in Wales. BMC Public Health 2019;19:1651. https://doi.org/10.1186/s12889-019-8015-3
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 234: Effects of red wine consumption on gut microbiota that affect health and disease – 14 November 2019
This brief paper supports earlier research relating wine consumption to gut microbiota, and the relation of the latter to obesity and to cardiovascular and other diseases. The authors report that “Red wine consumption was positively associated in a frequency-dependent manner with ɑ-diversity, but even rare consumption showed an effect. White wine also displayed a lesser but suggestive positive association with ɑ-diversity, while we saw no association with other alcohol categories.” They suggested that these effects of red wine on gut microbiota may play a role in the reduced risk of obesity, cardiovascular disease, and reduced total mortality associated with red wine intake that have been demonstrated in many cohort studies.
An increasing number of studies point to beneficial effects of wine, especially red wine, which may not be present for other types of beverages containing alcohol. However, we agree with the conclusions of the authors: “Red wine consumption should always be studied in the context of the overall dietary habits of individuals to take into account residual confounding and bias. The majority of observational studies fail to do this adequately; and thus, results from large scale clinical trials are needed in order to establish a cause and effect relationship between red wine polyphenols and gut microbiota.”
Forum members consider that the present analyses support a beneficial health effect of regular and moderate red wine, but also agree that much further research will be required to work out the complex relation between the consumption of red wine and gut microbiota and the effects on health.
Reference: Le Roy CI, Wells PM, Si J, Raes J, Bell JT, Spector TD. Red wine consumption associated with increased gut microbiota ɑ-diversity in 3 independent cohorts. Gastroenterology 2019. In press, doi.org/10.1053/j.gastro.2019.08.024
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 233: The relation of alcohol consumption to the development of dementia, with very extensive evaluations of the latter – 7 November 2019
This study was designed to assess the association between alcohol consumption and dementia and the roles of mild cognitive impairment (MCI) and apolipoproteinEε4 (APOEE4) genotype in modifying this association. It was based on data from the Ginkgo Evaluation of Memory Study, conducted from 2000 to 2008 among US community-dwelling participants (which did not demonstrate beneficial effects of ginkgo). The study analyzed 3,021 participants aged 72 years and older who were free of dementia at baseline.
The assessment of alcohol consumption included both the amount and frequency of intake, and the authors had a very broad assessment of potential confounders, including cardiovascular and other diseases, depression, race, ethnicity, educational level, social activity, medication use, and genotype for APOE-E4. There was a very complete and careful attention to the assessment of cognitive function, as subjects underwent numerous and repeated cognitive assessments. For example, if there was any suggestion of cognitive impairment, cerebral magnetic resonance imaging and referral to an expert panel of clinicians, who reviewed and validated presence of dementia, was carried out. No previous studies have had such an extensive assessment of cognition.
The main results include a finding that for the large majority of participants (the 2,548 without mild cognitive impairment at baseline), complete abstention from alcohol was associated with a slightly higher risk of dementia than seen in any of the groups consuming alcohol. For 473 subjects with MCI at baseline, there was no effect on risk of dementia for up to about 10 drinks/week, then a slight but insignificant increase in risk with greater intake. Daily low-quantity drinking was associated with more than 50% lower dementia risk than infrequent higher alcohol consumption. Many of the associations shown had a consistent pattern (a decrease in risk with light drinking) but did not reach statistical significance. The association was similar for all sub-groups, and was not modified by APOEE4 genotype.
The analyses seem well done, and Forum members agreed that, while some of the associations did not reach statistical significance, the data support most previous studies that show a J-shaped or U-shaped association for the relation of alcohol consumption to the risk of dementia. As has been shown in most previous studies, regular (even daily) light drinking was found to be preferable to infrequent higher levels of alcohol consumption in terms of the effect on the risk of dementia.
Reference: Koch M, Fitzpatrick AL, Rapp SR, Nahin RL, Williamson JD, Lopez OL, et al. Alcohol Consumption and Risk of Dementia and Cognitive Decline Among Older Adults With or Without Mild Cognitive Impairment. JAMA Network Open 2019:2(9):e1910319. doi: 10.1001/jamanetworkopen.2019.10319
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 232: Does moderate drinking of alcohol in later life reduce the risk of mortality? 3 September 2019
There are well-known problems inherent in most observational studies of alcohol and health. In addition to having to rely on self-report of intake, these include single-time point consumption assessments, inadequate confounder adjustments, accounting for reverse causation, selection bias, short follow up, residual confounding, and lacking information on chronic health conditions that may mediate the association between alcohol consumption and mortality. Further, there have been a lot of assumptions expounded about the generic fragility of older individuals in terms of alcohol consumption; they are generally without supportive clinical or experimental evidence. For light to moderate intake, the elderly tend to have similar benefits associated with alcohol as younger people, and they are at an age when the risk of mortality is at its peak.
The present study was able to adjust for many of these factors: it describes the risk of total mortality among a large group of older subjects, who were ≥ 56 years of age at the start of a 16 year follow up. They were participants in a nationally representative cohort of men and women in the USA, the Health and Retirement Study. Its strengths, in addition to its large size, is the fact that there were repeated assessments of alcohol so that changes of intake could be evaluated, and the authors were able to judge the potential importance of residual confounding.
The authors conclude that occasional drinking and moderate drinking among older subjects are associated with a lower risk of total mortality. The usual argument that light or moderate drinkers tend to have less severe or fewer common diseases and to enjoy better health and socioeconomic status is addressed in this study, which accounted for time-varying confounders that included smoking, body mass index, income, health/functioning, depression, and chronic diseases. From quantitative bias analysis studies they were able to estimate the effects of residual confounding on their results; the authors conclude that it is very unlikely that residual confounding by unrecorded variables would be the cause of the reduction in mortality associated with moderate drinking. Survival analyses supported notably decreased mortality for moderate drinkers. Forum members considered that this study adds important information about the effects on mortality of moderate drinking in the elderly.
Despite many decades of observational data, animal experiments, and limited clinical trials showing beneficial effects on many diseases and mortality from moderate drinking, it is noted that some researchers appear to be loath to admit to any positive health effects of alcohol. We all appreciate the serious adverse effects of heavy drinking and alcohol use disorders, both on the health of persons and on the community. However, when well-done analyses provide reliable data for light-to-moderate drinkers who do not binge drink, it is disturbing that, even then, some scientists question the observed beneficial results and appear to focus only on warnings about abuse.
There is evidence of a disinclination to admit to any beneficial effects of alcohol in many papers, including this one, which throughout the text seems to accentuate the negative aspects of alcohol. Such statements detract from an otherwise clear report suggesting, as one reviewer stated, that this paper is part research results, part polemic. In the opinion of the Forum, this paper provides strong evidence indicating that elderly people who are light-to-moderate drinkers tend to have a lower risk of mortality.
Reference: Keyes KM, Calvo E, Ornstein KA. Rutherford C. Fox MP, Staudinger UM, Fried LP. Alcohol Consumption in Later Life and Mortality in the United States: Results from 9 Waves of the Health and Retirement Study. Alcoholism: Clin Exper Res 2019;43:1734-1746.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 231: Association of alcohol consumption with obesity: Does moderate drinking increase or decrease the risk of obesity? 20 August 2019
While alcoholic beverages contain calories that are absorbed, the association between alcohol intake and body weight and obesity is unclear. Limited clinical trials have not confirmed a positive association between alcohol intake and weight, and some epidemiologic studies, including prospective cohort studies, show that regular moderate drinkers are less likely to be obese than are abstainers.
The present study uses data from National Health and Nutrition surveys between 2011 and 2016 to evaluate the association between reported amount and frequency of alcohol consumption and weight status. An estimated 78.1 % of males and 70.1% of females (who reported at least one drink in the past year) were classified as “drinkers.” A total of about 36% of US males and 41% of US females were described as “obese” (defined as BMI ≥ 30 kg/m2). The analyses included the level of obesity (Class 1, 2, or 3) as outcomes (with Class II defined as BMI 35-<40 kg/m2 and Class III as BMI ≥ 40 kg/m2) making it possible to judge the effects of alcohol on varying levels of obesity.
The present study reports that male current drinkers versus nondrinkers had 38% lower odds of Class 3 obesity versus subjects with a healthy weight; female current drinkers versus nondrinkers had more than 30% lower odds of Class I, Class II, or Class III obesity In both sexes, more frequent alcohol consumption was associated with less obesity, while heavy alcohol consumption was associated with increased risk of obesity. Females who reported that they were trying to lose weight consumed more than others, but there was not a strong relation between reported attempts to lose weight and outcomes.
Forum reviewers considered this to be a well-done analysis, with adjustments for most common potential confounding variables. It provides some support for previous findings of an inverse association with obesity for light-to-moderate alcohol consumption but an increase in obesity for heavy consumption. The authors state that this is the first study to be able to provide data showing that the magnitude of the inverse association is stronger for higher levels of weight status (Classes 1 to 3).
Forum members noted, however, that this study was based on assessments of different subjects in each wave of the national surveys, rather than on repeated assessments among the same individuals over time. It is clear that repeated recordings of alcohol intake in prospective cohort studies make it possible to obtain a reliable estimate of any changes in alcohol intake that may occur, rather than having to base results on a single measure, such as only a baseline value. Further, members caution that there are many genetic and lifestyle variables associated with the development of obesity, and residual confounding is always a potential problem in such analyses. Thus, while the present paper provides data indicating that more severe obesity may result from higher intake of alcohol, and that light-to-moderate intake may actually lead to a decrease in the risk of obesity, data from cohort studies with repeated assessments of alcohol and body size may provide more precise estimates of effect.
Reference: White GE, Mair C, Richardson GA, Courcoulas AP, King WC. Alcohol Use Among U.S. Adults by Weight Status and Weight Loss Attempt: NHANES, 2011−2016. Am J Prev Med 2019;57:220−230.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 230: An extensive review of the role of dietary constituents (foods, nutrients, and beverages) in the development of diabetes 1 August 2019
Of all lifestyle factors that relate to health and disease, probably the most difficult ones to evaluate are dietary factors, including foods, nutrients, and beverages. The present paper consists of a meta-analysis (an “umbrella” analysis) based on 53 previous meta-analyses from prospective cohort observational studies. This analysis includes 153 adjusted summary hazard ratios on dietary behaviors or diet quality indices, food groups and foods, beverages, alcoholic beverages, macronutrients, and micronutrients related to the incidence of type 2 diabetes. Data from previous meta-analyses on very few foods or nutrients are adequate to clearly determine their effects, but among those that have been identified as reducing the risk of diabetes, high-quality evidence was found only for whole grains, cereal fiber, and alcohol. As for dietary factors that have strong evidence of increasing the risk of diabetes, the authors of this paper identify only red meat, processed meat, bacon, and sugar-sweetened beverages.
Forum members considered this to be a well-done, appropriate analysis in a paper that summarizes well the current scientific literature. Some members were concerned about the number of assumptions that scientists must make when doing a simple meta-analysis, and especially when attempting an umbrella one; they consider it key to also evaluate single, large prospective studies where adjustments for many confounding socio-economic factors are less likely to be important.
Overall, the results of this paper strongly support most of the findings of previous meta-analyses and umbrella analyses and indicate only a few dietary factors for which “high-quality” evidence exists for an association with the risk of developing diabetes. The clearest evidence from the analyses in this paper, which was based only on prospective cohort studies, is that cereal grains and moderate alcohol lower the risk, while meats and sugar-sweetened beverages increase the risk of diabetes.
Given the complexity of evaluating dietary factors for their relation to disease outcomes, it will be useful for future studies to attempt to measure a multitude of foods, beverages, nutrients, and eating patterns, preferably over time, to evaluate further the association with disease. For now, current evidence suggests that cereals, grains, and moderate alcohol (that decrease risk) and meat and sugar-sweetened beverages (that increase risk) have the most consistent data for a relation to subsequent diabetes mellitus.
Reference: Neuenschwander M, Ballon A, Weber KS, Norat T, Aune D, Schwingshackl L, Schlesinger S. Role of diet in type 2 diabetes incidence: umbrella review of meta-analyses of prospective observational studies. BMJ 2019;365:l2368.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 229: A J-shaped curve for the relation of alcohol consumption to the risk of colorectal cancer — 10 July 2019
While heavy alcohol consumption is recognized as a contributor to the development of colorectal cancer (CRC), an increasing number of studies suggest that moderate alcohol consumption may not have an adverse effect on the risk of CRC, or even decrease the risk.
The present paper, a meta-analysis of 16 studies on the relation of alcohol consumption to invasive CRC, was conducted by leading investigators in the field. Forum members consider this to be a well-done study, with a large number of subjects, the ability to use individual level data in their meta-analysis, and the use of appropriate and complete analytic techniques.
The key finding of their study was that there was a J-shaped curve evident in all of their analytic approaches; their results strongly support a J-shaped association for the relation of alcohol intake to CRC: a slightly lower risk of cancer for light to moderate drinkers and an increased risk for subjects reporting an average of 3 or more drinks/day. Further, they found that their results did not vary by age, obesity, smoking, or family history of CRC. Overall, the effects of benefits/harms were somewhat more striking for cancers in the distal colon than in the proximal colon.
Potential mechanisms for heavy alcohol consumption being related to an increase in risk were discussed by the authors. As for moderate drinking decreasing the risk, potential mechanisms are discussed by a Forum member in this critique. He describes active, beverage-specific metabolites other than ethanol that reach the intestine. In particular, our attention goes to the several microbial catabolites which can be formed via our host microbiota in the colon.
The finding of a J-shaped curve between alcohol and CRC is similar to the relation seen for a number of other diseases, including coronary artery disease, ischemic stroke, dementia, and total mortality. While a linear relation between heavy drinking and certain upper aero-digestive tract cancers has been shown, for certain cancers there may be a J-shaped curve of effect, with reductions in risk for light-to-moderate drinkers.
Reference: McNabb S, Harrison TA, Albanes, Berndt S, Brenner H, Caan BJ, et al. Meta-analysis of 16 studies of the association of alcohol with colorectal cancer. Int J Cancer. 2019 Apr 29. doi: 10.1002/ijc.32377. [Epub ahead of print]
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
A Tribute to Elizabeth Barrett-Connor, MD (1935-2019)
It is with great sadness that we have learned of the death on 9 June 2019 of Elizabeth Barrett-Connor, a major contributor to the field of epidemiology for many decades and, especially, to a scientifically balanced and sound appraisal of the relation of alcohol consumption to health. Elizabeth was a member of our International Scientific Forum on Alcohol Research until April 2019, when she retired from the Forum because of ill health.
With degrees from Mount Holyoke College in Massachusetts, Cornell University Medical College, and London School of Hygiene and Tropical Medicine, Elizabeth also had medical training at the University of Texas Southwestern Medical School and the University of Miami in Florida. Joining the faculty at the University of California, San Diego, in 1970, she became a Distinguished Professor of Family Medicine and Public Health.
As described in the UCSD Faculty Profile from her university, “Dr. Barrett-Connor’s research concerned healthy aging with a focus on gender differences and women’s health. Dr. Barrett-Connor was founder and director of the Rancho Bernardo Heart and Chronic Disease Study, begun in 1972, with continuous support (4 MERIT awards) from the NIH. She served as a principal investigator of many multicenter clinical trials, including the Postmenopausal Estrogen/Progestin Interventions trial, the Heart and Estrogen-Progestin Replacement Study, the Raloxifene Use in the Heart study, and the Diabetes Prevention Program Observational Study. She was Past President of the Epidemiology Section of the American Public Health Association (APHA), the Epidemiology Council of the American Heart Association (AHA), the Society for Epidemiologic Research (SER), and the American Epidemiological Society (AES). She was a member of the Institute of Medicine (IOM), and a Master of the American College of Physicians (ACP).”
The author of more than 1,000 scientific publications (starting with articles on shigellosis and sickle cell anemia in the 1960s), during her career Dr. Barrett-Connor made important contributions to many fields, including epidemiology, gerontology, endocrinology, cardiology, gender effects, and lifestyle factors such as physical activity, diet, and alcohol consumption. She was the key individual responsible for maintaining and extracting data from the very long-term follow up of participants in the Rancho Bernardo Study of Healthy Aging. She was honored by the American Heart Association by the establishment of the annual Elizabeth Barrett-Connor Competition for young trainees in epidemiology.
Dr. Barrett-Connor was a highly respected mentor of young trainees and faculty. It is noteworthy that she was an author on at least 22 scientific publications during 2018-2019 that included, just in 2019, titles such as “Hearing impairment and cognitive decline in older, community-dwelling adults,” “Effects of APOE on cognitive aging in community-dwelling older adults,” “Genetic Ancestry Markers and Difference in A1c Between African American and White in the Diabetes Prevention Program,” “Cardiovascular Risk Factors Associated With Venous Thromboembolism,” and “Lifetime physical activity and late-life cognitive function: the Rancho Bernardo study.”
The obituary in the New York Times on 20 June 2019 by Karen Weintraub included a revealing anecdote about Elizabeth’s early days: “According to family lore, she was heading to the train station to take a nursing school entrance exam when she bumped into a friend. ‘You’d make a terrible nurse,’ the friend was said to have told her. ‘You can’t take orders from anybody.’ Acknowledging the truth of her friend’s comment, Dr. Barrett-Connor instead applied to medical school.”
Dr. Barrett-Connor was presented with a large number of awards. For example, all in one year she received awards from The University of Western Australia, the Society for the Advancement of Women’s Health Research, the Society for Epidemiologic Research, the Cleveland Clinic Foundation Department of Cardiology, and Scripps Clinic and Research Foundation.
In 2018, Dr. Barrett-Connor was awarded the Fred Conrad Koch Lifetime Achievement Award by the Endocrine Society with the following comments: “Elizabeth Barrett-Connor, MD, has made paradigm-shifting contributions in endocrine physiology and the role of hormones in disease pathogenesis (focus on gender differences) in cardiovascular disease, diabetes, osteoporosis, and breast cancer. It is hard to imagine the existence of any other individual whose work reflects such staggering impact. The hallmarks of Dr. Barrett-Connor’s enduring success — a driving quest for the truth, rigorous scientific discipline, and a joyful passion — have infused every aspect of her career, whether as investigator, lecturer, teacher, or mentor. She has helped make women more visible in the endocrinology field, not by example of her own shining star, but by her constant recognition of light coming from others.”
In a tribute to Dr. Barrett-Connor in Diabetes Care in April, 2019, former trainee and now Professor at the University of Cambridge in the UK, Kay-Tee Khaw noted: “When asked what her motto or philosophy of life was in an interview for her local newspaper, La Jolla Light, Elizabeth Barrett-Connor’s response was that she did not have any one particular philosophy so much as an attitude: ‘My defining principle is that I am a pathological optimist.’ Boundlessly curious, fearless, challenging, inspiring, and great fun to be with are some of the words her colleagues and mentees might use to describe her.”
In addition to her unbelievable contributions to the scientific literature and as a mentor to countless trainees and faculty, Elizabeth was a close friend to many of us in the Forum, who always enjoyed meeting with her at numerous conferences. She especially appreciated the contributions of good food, wine, and vibrant conversation on such occasions.
Among the number of comments received from Forum members were the following: “Dr. Barrett-Connor enjoyed critical debate, not only of scientific topics but also of politics and cultural issues. At a European conference, Elizabeth was one of the outstanding speakers with a talk on nutritional experiences in the US. When a female colleague from Finland was so moved by a certain theme and started crying Elizabeth commented very politely ‘I don`t like weeping women.’ Elizabeth was a strong woman with a lot of empathy and a lot of humour. She has truly been a wonderful and worldwide ambassador for public health and humanity.”
Stated another member: “Elizabeth argued against some of the best, was a clear, linear thinker, and never wavered in self-confidence. She strongly believed in the scientific method, as stated by Popper: ‘The only reason to have a hypothesis is to try to disprove it. If you couldn’t disprove it, you might be right—not guaranteed to be right, but you might be right.’ It teaches us about humility in science; something we need more of.”
We will sorely miss her
================================================================
Critique 227: A reduced risk of chronic obstructive pulmonary disease (COPD) associated with the intake of some alcoholic beverages – 29 May 2019
Chronic obstructive pulmonary disease (COPD) is a major health problem and cause of death throughout the world. While cigarette smoking is known to be the most important risk factor, there are limited data available on the relation of alcohol consumption to the condition. Given that moderate alcohol intake has been shown to decrease the risk of many inflammatory conditions, it may also affect the risk of COPD, which is associated with marked inflammation of lung tissues.
In the present study, the investigators related total alcohol consumption and intake of specific alcoholic beverages with the risk of COPD, based on data from more than 44,000 Swedish men in a population-based prospective cohort study. A total of 2,177 COPD cases were ascertained during follow up that extended up to 17 years. In their analyses, the authors had data permitting them to evaluate a number of demographic and lifestyle factors as potential confounders (including smoking status and pack-years of smoking, education, physical activity, BMI, and some indices of diet). However, there were very few ex-smokers or current smokers among the non-drinkers, making it somewhat difficult to adequate adjust for cigarette use as a cause of COPD.
Forum members thought that there are a number of deficiencies in this study that somewhat weaken its conclusions; especially important was the lack of ability to consider the pattern of drinking (regular, moderate versus binge drinking). Still, there is a strong consistency between the results of this study (indicating a “J-shaped” or “U-shaped” curve for alcohol intake and COPD) and results from extensive previous epidemiologic and experimental research.
Overall, the cumulative research findings now suggest that pulmonary disease might be included among the “diseases of ageing” that show a reduction in risk among moderate consumers of certain alcoholic beverages. Based on some previous epidemiologic studies and results from numerous experimental studies, data now suggest that, in addition to alcohol, the polyphenols present in wine and some beers may offer protection against COPD. While in the present study red wine consumption was associated with the lowest risk of COPD, Forum members acknowledge residual confounding by other lifestyle factors may still play a role.
Reference: Kaluza J, Harris HR, Linden A, Wolk A. Alcohol Consumption and Risk of Chronic Obstructive Pulmonary Disease: A Prospective Cohort Study of Men. Am J Epidemiol 2019;188:907–991.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 226: Consumption of red wine may lower the risk of lethal prostate cancer —- 16 May 2019
In an analysis from the Health Professionals Follow-up Study, the investigators evaluated the relation of alcohol consumption in their more than 45,000 study participants to the development of lethal prostate cancer. They related alcohol first to the overall risk of prostate cancer among all subjects, and then focused on the 5,182 men who developed non-metastatic prostate cancer to judge their risk of developing lethal prostate cancer or mortality. They judged the alcohol intake both prior to the diagnosis and after a diagnosis of prostate cancer. For reported alcohol consumption among subjects prior to the initial diagnosis of prostate cancer, there was a small (16%) but significant reduction in the risk of lethal prostate cancer among subjects reporting any alcohol consumption, but no significant effects of specific beverages on the risk of lethal prostate cancer. However, total mortality was lower for consumers of total alcohol intake and for most categories of intake for all types of beverage.
When they then related post-diagnosis alcohol intake (after the diagnosis of non-metastatic prostate cancer), the investigators found that red wine consumption was associated with a 50% reduction in the risk of developing lethal prostate cancer or mortality. There were no significant relations between total alcohol consumption or between the intake of other specific beverages and lethal disease.
The authors describe a number of hypotheses by which red wine, with its combination of high levels of polyphenols in addition to alcohol, may have lowered the risk of lethal prostate cancer. And there are numerous basic science experiments that have shown how polyphenols impede the development and growth of cancer cells. Presumably, it was not due to the alcohol in red wine, as similar amounts of alcohol in other beverages did not show a protective effect. While the effects of various polyphenols may play a role, at present the mechanisms of such an effect are not known.
Forum reviewers considered this to be a very well-done study and analysis, with repeated assessments of alcohol intake and essentially complete ascertainment of lethal prostate cancer and mortality. Forum members agree with the conclusions of the authors: “Our results indicate that moderate alcohol intake among men with prostate cancer is not associated with a higher risk of progression to lethal disease or overall mortality. The potential benefit of red wine on prostate cancer progression merits additional research.”
Reference: Downer MK, Kenfield SA, Stampfer MJ, Wilson KM, Dickerman BA, Giovannucci, EL, et al. Alcohol Intake and Risk of Lethal Prostate Cancer in the Health Professionals Follow-Up Study abstract. J Clin Oncology 2019 Pre-publication: : DOI https://doi. org/10.1200/JCO.18. 02462
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 225: Moderate alcohol consumption may lower the risk of chronic kidney disease — 8 April 2019
While numerous studies have found that moderate consumers of alcohol tend to be at a lower risk of developing chronic kidney disease (CKD), potential mechanisms for such an effect are unclear. The present large prospective, population-based, multi-cultural study provides important additional data on the effects of alcohol intake on the initial diagnosis of CKD over many years. It is based on data from the Atherosclerosis Risk in Communities Study and reports the relation of varying levels of alcohol consumption, versus non-drinking, to the incidence of CKD over a 24 year follow-up period.
Among the strengths of the study are the very large number of subjects (n=3,664) who developed CKD during follow up, using advanced methods for diagnosing the disease. Only baseline alcohol intake was used as the exposure and type of beverage or pattern of drinking could not be assessed; however, the authors considered multiple appropriate potentially confounding variables in the analyses, including total energy intake, age, sex, race-center, income, education level, health insurance, smoking, and physical activity. In comparison with the 25% of subjects in their analyses who were life-time abstainers, for subjects reporting all levels of alcohol consumption (≤1 drink per week, 2 to 7 drinks per week, 8 to 14 drinks per week, and ≥15 drinks per week), there was a statistically significant decrease in risk of incident CKD (from a 12% decrease in risk for the lowest category of alcohol intake to a 29% decrease for subjects reporting that they consumed 8-14 drinks/week).
The authors conclude: “Consuming a low or moderate amount of alcohol may lower the risk of developing CKD. Therefore, moderate consumption of alcohol may not likely be harmful to the kidneys.” Forum members agree that this study supports much earlier research showing a protective effect of moderate drinking on the risk of kidney disease. While mechanisms are not clear, effects of alcohol on renal vessels that are similar to those described for coronary and cerebrovascular arteries may play a role.
Reference: Hu EA, Lazo M, Rosenberg SD, Grams ME, Steffen LM, Coresh J, Rebholz CM. Alcohol Consumption and Incident Kidney Disease: Results From the Atherosclerosis Risk in Communities Study. J of Renal Nutrition, 2019, in press. DOI: https://doi.org/10.1053/j.jrn.2019.01.011
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 224: A brief summary of the association between wine/alcohol consumption and health in diabetics 12 March 2019
Diabetes mellitus is an increasingly common condition throughout the world, related closely to increases in obesity and ageing of populations. There are many, serious health conditions associated with diabetes, especially a marked increase in the risk of morbidity and mortality from cardiovascular disease. Scientific data from well-done cohort studies have demonstrated for decades that people who are moderate consumers of alcohol tend to have a considerably lower risk of developing diabetes in the first place, and diabetics who consume moderate amounts of alcohol are, in comparison with abstainers, at much lower risk of developing cardiovascular disease.
The present “mini-review” by scientists who have previously carried out the first large randomized clinical trial of wine and health outcomes among diabetics provides an interesting overview of the association of alcohol, particularly of wine, with health. The authors expand the implications of their research and conclude that “Initiating moderate alcohol consumption among well controlled persons with type 2 diabetes is apparently safe, in regard to changes in heart rate variability and carotid plaque formation.” Their findings have stimulated this critique by our Forum to also consider if available data now suggest that physicians should encourage the modest consumption of wine with food for selected patients with diabetes.
Our critique describes a number of risk factors (lipid levels, glucose, insulin, etc.) and intermediate conditions (such as endothelial function and arterial calcification) that have been shown to relate to the consumption of alcohol. Some Forum members believe that while all of these associations are important, the key information needed is the effect of alcohol consumption on disease outcomes themselves (coronary heart disease, stroke, dementia, etc.) and on mortality. At present, any recommendations regarding alcohol consumption must be based primarily on observational data from long-term cohort studies.
The key question we discuss in this critique is “Should physicians advise their older diabetic patients who are non-drinkers to begin to consume small amounts of an alcoholic beverage?” The consensus of Forum members is that current data suggest that, at a minimum, we should not advise such patients who currently consume alcohol moderately to stop their consumption. On the other hand, most members emphasize that we should discuss alcohol consumption with all patients. If they are at least occasional consumers of alcohol (the large majority of patients in most Western countries), our only advice might relate to the pattern of drinking. At present, the pattern commonly shown to be associated with the lowest risk of the usual diseases of ageing and mortality appears to be small amounts of alcohol, especially wine, with meals on a regular basis. For patients who indicate that they are drinking only in binges, we should emphasize the adverse health effects (for them as well as for society), and encourage a healthier pattern of drinking.
But what about current non-drinkers? For middle-aged or older non-drinkers who avoid alcohol because of religious prohibitions, previous misuse of alcohol, certain medical conditions, or a stated dislike of alcohol, our advice on prevention of disease should focus on not smoking, getting exercise, eating a healthy diet, and trying to avoid obesity. But for patients without such conditions that would indicate that they should avoid alcohol, many Forum members believe that they should at least be told of the current scientific evidence of possible beneficial health effects of regular, moderate intake. However, until considerably more data on its effects are available, we are not encouraging physicians to prescribe alcohol consumption for their diabetic patients.
Reference: Golan R, Gepner Y, Shai I. Wine and Health–New Evidence. Mini Review. European Journal of Clinical Nutrition. https://doi.org/10.1038/s41430-018-0309-5; 2019: in press.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 223: A new major review of the relation of alcohol consumption to the risk of dementia. 17 January 2019
While many studies have shown that excessive alcohol intake is associated with cognitive impairment and increased risk of dementia, most cohort studies have shown that the risks of these outcomes are lower among light-to-moderate drinkers than among abstainers. The authors of this paper conducted a scoping review on this topic, based on a systematic search of systematic reviews published from January 2000 to October 2017. A total of 28 systematic reviews were identified relating alcohol intake at various time periods to incidence of cognitive impairment/dementia, specific brain functions, or induced dementias. The authors report that light to moderate alcohol use in middle to late adulthood was associated with a decreased risk of cognitive impairment and dementia, but heavy alcohol use was associated with changes in brain structures, cognitive impairments, and an increased risk of all types of dementia.
Forum members considered this to be a well-done analysis, but were concerned that the focus was only on the potentially adverse effects of heavy drinking, with little regard or discussion of the findings of protection against such cognitive outcomes among light or moderate drinkers. Forum members point out that there are very many adverse health effects, both for the drinker and for society, resulting from heavy drinking. To them, the most interesting and provocative aspect of this paper was the conclusion of a protective effect against cognitive decline and dementia associated with light-to-moderate alcohol consumption.
Scientific data, including the results of the present systematic analysis, are very consistent in showing that cognitive decline, associated impairments in the functions of daily living, incident dementia, and survival are all associated favorably with light-to-moderate consumption of alcohol in middle age. The reasons and mechanisms that lead to these associations deserve further evaluation. With the increasing ageing of populations throughout the world, cognitive decline and dementia are expected to increase and create serious challenges for health care providers. Insight into ways of preventing or delaying the onset of such cognitive decline (in addition to decreasing the prevalence of heavy alcohol intake, the focus of this paper) could be extremely important in planning for the future.
Reference: Rehm J, Hasan OSM, Black SE, Shield KD, Schwarzinger M. Alcohol use and dementia: a systematic scoping review. Alzheimer’s Research & Therapy 2019; 11: pre-publication. https://doi.org/10.1186/s13195-018-0453-0
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 222. A new analysis relating alcohol intake to coronary heart disease – 20 December 2018
In an attempt to judge the effects of alcohol on the risk of coronary heart disease (CHD), the authors have carried out analyses using a sample of subjects from the National Epidemiologic Survey on Alcohol and Related Conditions III (NESARC-III). They based their exposure to current alcohol use on a single assessment at baseline of self-reported consumption during the past year, when the subjects were an average of 38.9 years of age. In addition they asked subjects if they had consumed larger amounts of alcohol when they were younger.
Their assessment of CHD was based on answers to questions at baseline as to having been told by a doctor that they had chest pain or CHD, apparently within the same 12-month period when they were asked about current alcohol consumption. Nothing in the paper indicates that the authors had data on the subsequent development of CHD during a follow-up period. When relating reported alcohol intake to CHD, they excluded 1,671 who reported “previous CHD,” although for this relatively young group it is questionable how many actually had CHD, as no data on validation of the diagnosis was done. For unclear reasons, for their comparison group they excluded any subjects with conditions that “may increase the risk of CHD (e.g., pneumonia, influenza, tuberculosis, liver disease, neurologic conditions, osteoporosis, arthritis, STD) and can be viewed as comorbid conditions related to alcohol consumption.”
Given that the exposure (alcohol) and outcome (CHD) were apparently from the same time period, there is reason to worry about reverse causation (i.e., subjects may have developed CHD and changed, either decreased or increased, their alcohol consumption during the same period).. As for using the self-reported amount of alcohol consumed at some time in the past as the exposure, there is a large chance of serious misclassification of exposure due to recall bias and bias according to current alcohol intake (as subjects currently reporting greater amounts of alcohol were more likely to report even higher intake in the past).
With only a single assessment of current alcohol intake, an inadequate assessment of long-term alcohol intake, a lack of data during a follow-up period for the main outcome, CHD, and no validation of the outcome, Forum members considered that this was an unusual cohort to use when attempting to judge the relation of changes in alcohol consumption to the development of CHD. The necessary elements for a useful analysis were not available to these investigators using this population sample.
In any case, results from many well-done long-term cohort studies with repeated assessments of alcohol and validated CHD outcomes during follow up have already provided key data on this topic: they almost uniformly demonstrate that light-to-moderate drinkers who do not binge drink have significantly lower risk of developing CHD. The present analysis does not provide data that would question such findings.
Reference: Fan AZ, Ruan WJ, Chou SP. Re-examining the relationship between alcohol consumption and coronary heart disease with a new lens. Pre-publication. Preventive Medicine 2019;118:336=343.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 221: The relation of alcohol intake to stomach cancer – 20 November 2018
There have been conflicting results from studies of the association between alcohol intake and the risk of gastric cancer. Some of the differences among studies have related to mixing subjects from Western countries with those from Asia, where dietary patterns, lifestyle factors, drinking patterns, and types of alcohol consumed differ from those among Western populations. Results usually differ between Asian and Western populations.
The present study is based on almost 500,000 subjects from the USA with follow up for a median of 15.5 years. The investigators identified a total of more than 1,300 cases of gastric cardia cancer (GCA) or gastric noncardia cancer (GNCA ). The authors report: “We found no association between higher alcohol consumption and GCA or GNCA, when examined as total alcoholic beverage intake or individual beverage types of beer, wine and liquor. Furthermore, we observed no association by stratum of sex, ethnic group, educational level or smoking status. We did, however, observe lower risk of GNCA among participants who drank up to one drink per day (HR = 0.81, 95% CI: 0.67–0.97) compared to nondrinkers.” They conclude: “Alcohol consumption was not associated with increased risk of GCA or GNCA in this large U.S. cohort.”
Forum members considered this to be a large, very well-done analysis; subjects were aged 50-71 years at baseline, appropriate for evaluating the risk of gastric cancer. Data on a large number of potential confounders were included in the analysis. Diagnosis of cancer was from state cancer registries, shown to be very accurate. The statistical analyses included restricted spine analysis to test for a dose-response curve (not found), and excluded the first two years after alcohol assessment to lower the risk of reverse causality. Further beverage-specific analyses were carried out, and did not show differences according to whether the consumption was of beer, wine, or spirits.
Weaknesses included only one assessment of alcohol intake, at baseline, and no data on binge drinking or other aspects of the pattern of drinking. Subjects were generally well-educated, white, and consumed alcohol moderately (75% reported one drink or less). Thus, these results may not pertain to other ethnic groups or to heavier consumers of alcohol.
Overall, these results provide further support for the lack of an association between light-to-moderate alcohol intake and the risk of gastric cancer. The significant decrease in risk of gastric non-cardia cancer associated with consumption of up to one drink/day should obviously be replicated, but the authors provide some potential mechanisms that could explain such a phenomenon. The study did not support previous data suggesting that wine consumption might have additional benefits to those of other beverages in terms of cancer risk.
Reference: Wang SM, Freedman ND, Loftfield E, Hua X, Abn CC. Alcohol consumption and risk of gastric cardia adenocarcinoma and gastric noncardia adenocarcinoma: A 16-year prospective analysis from the NIH-AARP diet and health cohort. Int J Cancer 2018; pre-publication.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 220: An unusual analysis relating alcohol intake to mortality – October 16, 2018
The authors of this treatise on alcohol consumption and mortality combined, for an unclear reason, results from two, very different studies: one from the Veterans’ Health Administration, based on outpatient clinical medical records, and the other from a national survey in the USA [The National Health Interview Survey (NHIS)]. Unfortunately, the VA data did not adjust for tobacco use or other important lifestyle habits, and are not useful in judging the effects of alcohol consumption on mortality.
While the NHIS survey included data on potential confounding, both it and the VA study based their analyses on a single estimate of alcohol consumption. The authors then created a variable that they stated was associated with the lowest risk of mortality and compared results from such alcohol intake with data from subjects reporting less or more alcohol. They combined data on all subjects reporting 1 to 2 drinks/week, so did not have the ability to provide a precise estimate of the association between low levels of intake and mortality risk. They did not comment on the effects that under-reporting of alcohol would have on their studies (and most investigators agree that the self-reported level of alcohol consumption is usually an under-estimate of actual consumption). Further, they did not point out the very much higher risk of mortality of non-drinkers, compared with moderate drinkers, demonstrated in their data.
To the extent that people accurately reported their past drinking status (never vs former), this study should put to rest concerns that protective associations of drinking versus non-drinking arise from inclusion of former drinkers into non-drinking groups. Never drinkers had higher risk of mortality than former drinkers in this study.
There are considerable data from many well-done cohort studies that have repeated assessments of alcohol intake over many decades and the subsequent risk of mortality. Such studies provide very clear and consistent results indicating a J-shaped curve: lower risk of mortality for light and moderate drinkers than for non-drinkers (even lifetime abstainers) and some increase in risk for heavy drinkers. These are the studies that can provide reliable information upon which drinking guidelines for different individuals and populations can be based.
Reference: Hartz SM, Oehlert M, Horton AC, Grucza RA, Fisher SL, et al. Daily Drinking Is Associated with Increased Mortality. Alcoholism: Clin & Experimental Research 2018; pre-publication. DOI: 10.1111/acer.13886.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
================================================================
Critique 219: A global overview of alcohol consumption and health – 3 September 2018
Investigators working with data from the Global Burden of Diseases, Injuries, and Risk Factors Study 2016 have combined data from 195 locations around the world, from 1990 to 2016, for both sexes and for 5-year age groups between the ages of 15 years and 95 years and older. Their purpose was to determine how estimates of the prevalence of current drinking, abstention, the distribution of alcohol consumption among current drinkers in standard drinks daily (defined as 10 g of pure ethyl alcohol) relate to alcohol-attributable deaths and disability-adjusted lifeyears (DALYs). The paper does not present estimates of the effects of alcohol on a key outcome, total mortality.
The paper presents a huge number of analyses with data specific for each contributing center. However, the Forum considers that real problems emerge when they attempt to combine data from many divergent cultures to determine a single association between alcohol consumption and health. Many lifestyle and cultural factors strongly modify the relation of a given amount of alcohol to health and diseases. Such modifying factors include especially the socio-economic status of the individual, circumstances such as drinking with or without food, the pattern of drinking (regular moderate versus binge drinking), the type of beverage (e.g., wine versus spirits), the intention of the individual (drinking to get drunk versus drinking to enhance meals), level of physical activity, etc. When such modifying factors are not taken into consideration, the estimated intake of a given amount of alcohol (even if accurate), provides an incomplete assessment of the effects of alcohol on health.
The authors spend much of their paper focusing on their contention that these analyses have large implications for setting alcohol policy around the world. They then expand primarily on ways of decreasing alcohol intake world-wide through changes in guidelines. However, their failure to consider specifics of the culture for which the policy is being formulated, such as evaluating other lifestyle factors, the pattern of drinking, underreporting of alcohol intake, cultural factors, etc., negates their ability to provide useful information that is applicable to any single population: their guidelines end up applying to no one. And, their specific statement that zero consumption would be preferable everywhere is sharply contradicted by consistent reports from very large, well-done cohort studies (where individual data are available) which indicate that non-drinkers have higher risks of cardiovascular disease and total mortality than regular moderate drinkers who do not binge drink.
Setting guidelines for the public regarding alcohol consumption requires information not only on the reported intake but on other health conditions, as well as genetic, lifestyle, and cultural factors that may modify the effects of alcohol. Further, advice differs by age and the key problems within a country that the guidelines are directed toward improving. In the opinion of the Forum, despite the massive amount of work done by the investigators in the preparation of this paper, the overall combined results from such divergent populations have little applicability in setting guidelines that would lead to avoidance of alcohol abuse in any specific group of people around the world — they apply to no specific population.
Reference: GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. www.thelancet.com Published online August 23, 2018 http://dx.doi.org/10.1016/S0140-6736(18)31310-2
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here
================================================================
Critique 218: Long-term study of alcohol intake and the risk of Alzheimer Disease or other types of dementia – 21 August 2018
While there is general agreement that the moderate intake of alcohol is associated with a significantly lower risk of cardiovascular disease, there are less data on the relation of moderate alcohol consumption to dementia. However, the vast majority of well-done prospective studies indicate that, in comparison with non-drinkers, moderate, non-binge-drinking older adults have lower risk of Alzheimer Disease and other types of dementia. The present study provides important information on this association by monitoring for the development of dementia among subjects in a large cohort of British civil servants (the Whitehall Study) over more than two decades; there were repeated assessments of alcohol consumption.
The main results indicate that abstinence in middle life is associated with a significantly higher risk of dementia than the risk among moderate drinkers, while subjects reporting the intake of larger amounts of alcohol or evidence of an alcohol use disorder are at increased risk of dementia. Specifically, the study shows that among the 397 cases of dementia that were recorded over a mean follow up of 23 years, abstinence in midlife was associated with a 47% higher risk of dementia compared with consumption of 1-14 units/week (a British unit is the equivalent of 8 grams of alcohol). There was a 17% increase in risk of dementia for those reporting more than 14 units/week. With repeated assessments of alcohol the authors also calculated trajectories of alcohol consumption from midlife to early old age, with continued abstinence being associated with an increase in dementia of 74% and a decrease in consumption with an increase of 55% in comparison with subjects reporting continued moderate consumption. In several analyses, wine consumption was associated with more favorable effects than those of other beverages.
Forum members thought that this was a well-done analysis, but considered that the data presented do not allow for a firm determination of a cut-point for increased risk of dementia from alcohol intake. While the authors provide estimates of a linear increase in dementia risk for subjects reporting more than 14 units/week or reporting evidence of alcohol abuse, they do not give data that permits an estimate of the level of intake where the risk of dementia exceeds that of non-drinkers.
Overall, the results showing a decreased risk of dementia for moderate drinkers support the findings from most well-done prospective cohort studies. As for implications for policy, the study further shows that, in terms of the risk of dementia as well as cardiovascular disease, middle-aged and older individuals who are consuming alcohol moderately and without binge drinking should not be advised to stop drinking.
Reference: Sabia S, Fayosse A, Dumurgier J, Dugravot A, Akbaraly T, Britton A, Kivimäki M, Singh-Manoux A. Alcohol consumption and risk of dementia: 23 year follow-up of Whitehall II cohort study. BMJ 2018;362:k2927. http://dx.doi.org/10.1136/bmj.k2927
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================
Critique 217: Alcohol, cancer, and mortality: Further affirmation of the J-shaped curve for mortality and increase in incidence of cancer with larger intake of alcohol – 9 July 2018
Scientific studies have shown consistently that that the consumption of small amounts of alcohol on a regular basis is associated with a lower risk of total mortality, while consumption of large amounts is associated with an increased risk of certain cancers and mortality. The present report is from a population-based cohort study of almost 100,000 older subjects who were followed for a median of 8.9 years. There were large numbers of deaths (n=9,599) and incident cancers (n=12,763) diagnosed during follow up, which should lead to more precise estimates of effect.
The authors report that light-to-moderate drinking was associated with lower total mortality, but the risk of incident cancer increased with greater alcohol consumption, especially the intake of beer or spirits. However, the analyses indicate that the slightly increased risk of cancer associated with moderate alcohol consumption was less than the beneficial effect on mortality.
Specifically, in comparison with never drinkers or very light (< 1 drink/week) drinkers, the study shows lower mortality for “light-to-moderate” alcohol consumers (up to 2 drinks/day) but greater mortality among subjects classified as “heavy” (2 to < 3) or “very heavy” (3+ drinks/day) consumers. In beverage-specific analyses, there was a slight increase in total mortality for reported intake of spirits starting at the consumption of about 1 ½ drinks/day and for beer at or above about 2 drinks/day; no significant increase in cancer risk was associated with wine consumption, regardless of the amount. The authors conclude that “there is a J-shaped association between alcohol and mortality in older adults, which remains after adjustment for cancer risk.”
Forum member considered this to be a well-done analysis, and shows, essentially for the first time in a single study, how the beneficial effects of light and moderate drinking on cardiovascular disease and total mortality exceed the slight increase in cancer risk for alcohol consumption at this level. In other words, while even light-to-moderate drinking may be associated with a slight increase in the risk of certain cancers, such drinking still favorably affects the overall risk of mortality.
Reference: Kunzmann AT, Coleman HG, Huang W-Y, Berndt SI. The association of lifetime alcohol use with mortality and cancer risk in older adults: A cohort study. PLoS Med 2018;15:e1002585. https://doi.org/10.1371/journal.pmed.1002585.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================
Critique 216: Strong effects of five lifestyle factors on risk of mortality and longevity of life – 31 May 2018
It has long been known that a number of lifestyle factors – such as not smoking, being physically active, avoiding obesity – decrease the risk of many of the “diseases of ageing,” especially cardiovascular disease and cancer. The present paper from the Nurses’ Health Study and the Health Professionals Follow-up Study is especially important as it demonstrates the joint effects of five healthy factors on disease-specific and total mortality in very large cohorts of subjects. The “healthy lifestyle factors” evaluated were (1) never smoking, (2) body mass index of 18.5 to 24.9 kg/m2, (3) ≥30 min/d of moderate to vigorous physical activity, (4) moderate alcohol intake, and (5) a high diet quality score (upper 40%). The similarity in education and other socio-economic factors of the subjects in these studies tends to reduce potential confounding by such factors.
There were more than 42,000 deaths in their cohorts during follow-up periods extending up to 34 years. The effects of these factors on subsequent risk of mortality were striking: for subjects meeting criteria for all five factors versus none, there was an 84% reduction in all-cause mortality, 65% less cancer mortality, and 82% less cardiovascular disease mortality. The overall effect was associated with 12 to 14 additional years of life after age 50 for subjects meeting criteria for all five factors.
Forum members consider this to be an excellent study, as it was based on data from very large cohorts of well-monitored subjects over many decades, with essentially full ascertainment of mortality. This study strongly suggests that the leading causes of premature death throughout the developed world are, to a large extent, preventable.
Reference: Li Y, Pan A, Wang DD, Liu X, Dhana K, Franco OH, Kaptoge S, Di Angelantonio E, Stampfer M, Willett WC. Hu FB. Impact of Healthy Lifestyle Factors on Life Expectancies in the US Population. Circulation 2018;137:00–00. (Pre-publication). DOI: 10.1161/CIRCULATIONAHA.117.032047.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 215: Long-term effects of smoking and moderate drinking on the quality and longevity of life of elderly women — 9 May 2018
While essentially all epidemiologic studies have shown adverse health effects of cigarette smoking and beneficial effects of moderate alcohol consumption, the present study is important as it follows a cohort of elderly women into very old age. It is a prospective cohort study of 9,704 women at least 65 years of age, who were living independently at baseline and were not heavy drinkers; they had a mean baseline age of 71.7 years (range 65-99) and underwent repeated assessments of lifestyle habits starting in 1986 to 1988. They were followed longitudinally until death, loss to follow-up, or to April, 2016. Outcomes included grip strength, walking speed, prevalence of threshold scores for self-reported health, difficulty with three or more instrumental activities of daily living (IADLs), depression, prevalence of falls, living in a nursing home, and death after 10- or 20-year follow up. The main comparisons evaluated in this study were between women who were smokers and those who consumed alcohol moderately, with each analysis adjusted for the other exposure.
Forum members considered this to be a well-done study that provides some important data relating effects of smoking and moderate drinking on function and mortality in very elderly subjects (an age group where data are lacking). There were criticisms that the study does not report the effects of moderate drinking among smokers; previous studies have shown that the adverse effect of smoking is modified by moderate alcohol intake. Further, given that the reasons why some women quit drinking during follow up are not known, the article does not contribute to clarification of the problem of reverse causation (e.g., healthier women may tend to continue drinking whereas sicker women stop alcohol consumption). Also, the authors did not adjust for some strong confounders, especially those related to socio-economic status (SES).
Nevertheless, the results of this study make a real contribution to our knowledge of the effects of drinking on both quality of life and mortality among women who are 65 years or older. The follow up of subjects continued for a least 20 years, by which time almost 70% of the women had died. Hence, the effects on mortality should be excellent estimates. As expected, women who were smokers had greater risk for almost all adverse outcomes, while drinkers who continued to consume moderate alcohol into old age had the most favorable outcomes. While the authors report that women who reported drinking at baseline but quit later on had mortality risks that were intermediate between non-drinkers and persistent drinkers, the reasons why some women quit drinking were not known. Hence, it is appreciated that continued drinking could be only a marker of better health, and not the cause.
Reference: Nelson HD, Lui L, Ensrud K, Cummings SR, Cauley JA, Hillier TA. Associations of Smoking, Moderate Alcohol Use, and Function: A 20-Year Cohort Study of Older Women. Gerontology & Geriatric Medicine 2018;4:1–9. Pre-publication.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 214: Some methodologic problems in a recent paper urging changes in drinking guidelines – 23 April 2018
Using individual-participant data from a number of large studies, predominantly from the UK and other European countries, the authors of the present paper have estimated the association between the reported level of alcohol intake among drinkers with cardiovascular outcomes and mortality. They conclude that the lowest risk of these outcomes is from the intake of less than 100 g of alcohol per week, and that guidelines for the public should reduce the upper limits for the amount of alcohol that could be safely consumed.
Forum members identified a number of flaws in these analyses, including failure to separate advice for men versus women or for older adults versus young people. Further, the authors do not point out the effects of under-reporting of intake, the marked differences in many health effects according to type of alcoholic beverage (such differences are shown only in their supplement but not mentioned in the abstract); also, there is little discussion of the importance of the pattern of drinking on health results.
Most important, by excluding never-drinkers as a reference group in their main analyses, the authors essentially eliminated the ability to evaluate for any potentially beneficial (or adverse) effects of light-to-moderate drinking as compared with non-drinking. This is problematic, as in essentially all previous large studies, moderate drinkers are those for whom significant and large benefits have been reported for risk of cardiovascular disease and total mortality.
Guidelines for the public regarding alcohol intake relate to many factors, including the net overall physiologic effects on health as well as the particular needs of different countries and cultures. And, as in this study, the inclusion of results from so many different cultures is a problem for determining appropriate guidelines for alcohol intake. Given that culturally specific drinking patterns, type of beverage, and many other lifestyle factors modify the health effects of alcohol, mixing data from markedly different cultures may give results that may not be appropriate for any specific population.
Reference: Wood AM, Kaptoge S, Butterworth AS . . . John Danesh, et al, for the Emerging Risk Factors Collaboration/EPIC-CVD/UK Biobank Alcohol Study Group (120 authors). Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet 2018;391:1513-1523.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 213: A meta-analysis on lifestyle factors, cardiovascular disease, and total mortality for a very large number of middle-aged and elderly women – 27 March 2018
Overall, Forum members considered this to be a well-done paper that provides additional information on alcohol’s effects on CVD and mortality among a very large number of middle-aged or elderly women. Although women markedly increase their risk of CVD following menopause, this is a group of women for whom data are sparse. Weaknesses of the analysis include a lack of information on the pattern of drinking (binge versus regular), type of beverage, and drinking alcohol with or without food. It is of note that in some of the studies included in the meta-analysis, factors such as HDL-cholesterol and fibrinogen were adjusted for in the study; given that these are mechanisms of alcohol’s effects, overall results will surely underestimate the effects. Further, as the authors point out, this study provides little information on the physiologic mechanisms of alcohol’s effects on health.
Forum members praised the authors for this meta-analysis of a very large dataset. It strengthens previous analyses that show that each of the lifestyle factors considered – not smoking, not becoming obese, being physically active, and regularly consuming small to moderate amounts of alcohol – benefit health. The more healthy lifestyle factors a subject has, the greater the benefit.
It will be especially important that future research evaluates what happens if subjects change their lifestyle habits, as such results would help target specific behavioral changes. There are very limited data available on this at present, but such studies that have been done suggest that the onset of moderate drinking among non-drinkers, or a slight increase in alcohol consumption among light drinkers, have beneficial effects on health. Still, it is appreciated that moderate alcohol consumption is only one of a number of factors making up a “healthy lifestyle,” which is clearly associated with less cardiovascular and other diseases and a much lower risk of mortality.
Reference: Colpani V, Baena CP, Jaspers L, van Dijk GM, Farajzadegan Z, Dhana K, Tielemans MJ, Voortman T, Freak-Poli R, Veloso GGV, Chowdhury R, Kavousi M, Muka T. Franco OH. Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: a systematic review and metaanalysis. European Journal of Epidemiology 2018; pre-publication. https://doi.org/10.1007/s10654-018-0374-z
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 212: Is it the alcohol or other substances in wine that lead to beneficial health effects? — 15 March 2018
While epidemiologists have long noted that consumers of wine tend to have better health outcomes than consumers of other alcoholic beverages, it has always been of concern that we were comparing drinkers, and not the drink itself. In recent years, many basic scientists have evaluated the non-alcoholic constituents in wine, and most studies show beneficial health effects from polyphenols and other components in wine as well as beneficial health effects from the alcohol in wine.
The present study provides an excellent review of clinical trials that compared the effects of wine versus no intervention or versus the effects of other alcoholic beverages. The specified outcomes related to effects on lipids, glucose/insulin metabolism, hemostatic mechanisms, and inflammatory/endothelial systems. The authors conclude that “The most repeated result of wine consumption is on lipid metabolism, attributed mainly to ethanol, while wine micro-constituents seem to have an important role mainly in haemostatic and inflammatory/endothelial systems.” Forum members cite several other important effects of wine micro-constituents, including demonstrated effects of such components at the cellular, molecular, and gene levels to sustain increased fibrinolytic activity, which is closely related to the development of cardiovascular disease.
Forum members were unanimous is considering that this was an excellent review of human clinical trials on the topic; the paper does not, however, comment on the mechanisms by which micro-constituents may operate to improve health. Given that since virtually none of the wine micro-constituents circulates in the human biofluids in their native form, it is especially important that the catabolites of wine micro-constituents be better defined and evaluated.
Overall, current data indicate that wine may be especially effective in lowering the risk of cardiovascular disease not only through the alcohol it contains, but also from a number of its key polyphenols. Forum members also point out that, for beneficial health effects of any type of alcoholic beverage, the pattern of drinking is especially important: the consumption of small or moderate amounts on a regular basis, and preferably with food.
Reference: Fragopoulou E, Cholevaa M, Antonopoulou S, Demopoulos CA. Wine and its metabolic effects. A comprehensive review of clinical trials. Metabolism Clinical and Experimental 2018;83:102-119.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 211: Effects of alcohol and aldehydes on DNA and risk of cancer; potential implications from a study in mice — 22 January 2018
The authors of this paper, based on an extensive basic scientific experiment in mice, describe the features and mutational landscape of DNA damage caused by acetaldehyde, an endogenous and alcohol-derived metabolite. This damage results in DNA double-stranded breaks that, despite stimulating recombination repair, also cause chromosome rearrangements. Furthermore, the authors identify how the choice of DNA-repair pathway and a stringent p53 response limit the transmission of aldehyde-induced mutations in stem cells.
Forum members considered this to be a well-done series of experiments that add additional data on the effects of aldehyde on cellular damage, which could potentially lead to an increased risk of cancer. While interesting, these results in mice have limited applicability to the effects of alcohol in humans, as the study conditions do not correspond to that found in real life. For example, the levels of ethanol used to elicit the DNA changes were high and alcohol was directly injected into the animals, whereas in humans alcohol is orally absorbed and undergoes several types of metabolism that reduce maximum blood alcohol concentrations achieved. Further, the animal model was based on mice that had been genetically manipulated in that particular genes had been selectively ‘knocked out’ to make them unable to metabolize aldehyde or to repair DNA damage; while this was necessary to study the effects in a basic scientific experiment, it is in contrast to what would occur under non-manipulated conditions of alcohol consumption in humans
The damages shown in this experiment were to hematologic cells, and epidemiologic studies have generally not found an increase in the risk of hematologic cancers in humans to be associated with alcohol, especially from the moderate intake of alcohol (and many studies show instead a decrease in risk among drinkers). Thus, studies in humans have not provided support for these reported results from mice. Further, Forum members conclude that the polyphenols that are present in wine may play an important role in blocking a carcinogenic effect associated with alcohol intake.
Reference: Garaycoechea JI, Crossan GP, Langevin F, Mulderrig L, Louzada S, Yang F, Guilbaud G, Park N, Roerink S, Nik-Zainal S, Stratton MR, Patel1 KJ. Alcohol and endogenous aldehydes damage chromosomes and mature stem cells. Nature 2017;553:171-177. doi:10.1038/nature25154.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 210: Beer, wine, and spirits consumption and risk of gastric cancer – 8 January 2018
While heavy alcohol intake has been regularly found to increase the risk of upper aero-digestive tract (UADT) cancers (mouth, tongue, pharynx, larynx, etc.), results are less clear for gastric cancer. The present study is notable because it is based on a large number of subjects, uses appropriate analytic methods, and provides dose-dependent results according to type of beverage.
For total alcohol, the dose-response results in this meta-analysis show a curvilinear relation between alcohol intake and gastric cancer, with a minimal (4%) but significant increase per typical drink (12.5 g/alcohol). However, there were varying responses for different beverages. In beverage-specific analyses, for beer, a non-linear relation was found with a significant increase of 7%/drink (CI 1.01, 1.13); for liquor, there was a linear association, with RR=1.03 (CI 0.98, 109); and for wine, the RR was 0.99 (CI 0.93, 1.06).
While the authors show a figure of the dose-response curves for each beverage using a non-linear approach, they do not provide the specific values in a table or in the text; this makes it difficult to clearly determine threshold effects of beverages. The figures suggest that the risk associated with beer consumption shows a slight decrease for 1 to 2 drinks/day, then an increase; for spirits, no decrease with lighter intake is seen; for wine, the curve is continuously downward. The authors do state that “light, moderate, and wine drinking would not increase gastric cancer risk,” so it is presumed that significant increased risk was not noted for moderate drinking for any specific beverage when non-linear effects were evaluated. Thus, overall, it appears that this large meta-analysis shows no significant increases in risk for light to moderate consumption of an alcoholic beverage, but a slight increase in risk associated with greater intake of beer and spirits. For wine, no increase in the risk of gastric cancer was seen for any level of consumption.
In a number of sensitivity analyses, the authors found tendencies for a lower gastric cancer risk associated with alcohol for cohort versus case-control studies, for studies with larger numbers of subjects, for studies judged to be of higher quality, and for studies adjusting for confounding by SES & income; these types of studies would be expected to yield more precise estimates of effect. These results led the authors to state these sensitivity analyses “ . . . indicate that our results may be exaggerated to some degree, but it should be noted that the pooled risk estimates of high-quality studies yielded similar results to the original analysis.”
Overall, Forum members considered this to be a well-done analysis, and the data support an increase in gastric cancer risk for heavier drinking (of beer or spirits) but no significant effects for light or moderate drinking of any alcoholic beverage. Forum members considered that if the lack of increase in cancer risk from wine consumption seen in this analysis proves to be true, it might relate to the polyphenols in wine that block any adverse effects of alcohol on gastric cancer risk.
Reference: Wang P-L, Xiao F-T, Gong B-C, Liu F-N. Alcohol drinking and gastric cancer risk: a meta-analysis of observational studies. Oncotarget 2017;8:99013-99023.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 209: Does alcohol intake increase the risk of obesity? — 13 December 2017
The public, and scientists, have long been concerned about the relation between alcohol consumption and weight gain, as all alcoholic beverages contain calories. However, most epidemiologic studies do not find that light or moderate drinkers weigh more than their abstaining peers, and some even show lower weight among moderate drinkers than among abstainers. The reasons for this apparent effect are unclear.
The present study is important as it describes the effects on weight of changes in alcohol intake over repeated 4-year periods among a large cohort of health professionals, followed for 24 years. They found very slight increases in weight (mostly less than one-half pound over a four-year period) for subjects consuming alcoholic beverages; these were statistically significant for regular beer and liquor, but not for wine or light-beer. Overall, the largest increases in weight (still, only an increase of 0.6 pounds) were seen for subjects increasing their alcohol by an average of 2 or more drinks/day. For subjects decreasing their alcohol intake over the periods, there was a slight decrease in weight, still only about one-half pound or less.
The investigators conclude that any effects of drinking on weight are very minor, and probably of no clinical significance. While effects on weight gain were slightly lower among consumers of wine and light beer than for those consuming regular beer or spirits, the differences were not large. The study does not present data on the mechanisms of such associations.
Forum members considered this to be a very well-done analysis of repeatedly collected exposure and outcome data among health professionals over an extended period of time. Adjustments were made for known potential confounders associated with changes in weight and appropriate sensitivity analyses were done. While the paper indicates that calories from alcohol are metabolized similarly to those from other foods and do affect weight change, the changes associated with moderate alcohol intake appear to be very minor and would be expected to have very little effect on the development of obesity.
Reference: Downer MK, Bertoia ML, Mukamal KJ, Rimm EB, Stampfer MJ. Change in Alcohol Intake in Relation to Weight Change in a Cohort of US Men with 24 Years of Follow-Up. Obesity 2017;25:1988-1996. doi:10.1002/oby.21979
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 208: A statement on alcohol and cancer that ignores the net health effects of moderate drinking, such as increasing longevity of life — 16 November 2017
The present publication is an attempt by the American Society of Clinical Oncology to describe the relation between alcohol consumption and cancer, including the effects on the risk of developing cancer and effects among subjects currently being treated for cancer. It came to the conclusion that there is a need for the public to be warned about the use of alcohol because of its effects on cancer, and describes numerous approaches for decreasing alcohol use in the population.
Forum members considered this paper to markedly distort the associations between alcohol consumption, especially light drinking, and health outcomes. The authors were particularly remiss in not describing the net health effects of light to moderate consumption: longer longevity of life. Their long discussion of policy implications, and ways of decreasing alcohol use in the population, were unrelated to the data they presented, and failed to describe how complex and culturally specific such recommendations are. The authors describe many ways of decreasing alcohol consumption in the population, but do not provide any data about whether or not the measures they propose are successful.
While all Forum members agree that heavy alcohol consumption increases the risk of several cancers (information that oncologists should be aware of), light drinking has generally been associated only with a slight increase in breast cancer, but not with other types of cancer (especially when under-reporting of intake is considered). Further, factors such as dietary folate intake, patterns of drinking such as binge versus regular moderate drinking, and type of beverage generally consumed have been shown to modify even this relation. Also, regular light or moderate drinking has been consistently shown to decrease the risk of cardiovascular disease (the leading cause of death), diabetes, dementia, and even total mortality, associations largely ignored in this paper.
Our Forum considers that this publication from the American Society of Clinical Oncology misses an opportunity to provide, for oncologists and for the public, up-to-date and balanced information of the true relations of alcohol consumption to the risk of cancer and other health outcomes. They have especially ignored the effects of moderate drinking on the risk of total mortality.
Reference: LoConte NK, Brewster AM, Kaur JS, Merrill JK, Alberg AJ. Alcohol and Cancer: A Statement of the American Society of Clinical Oncology. J Clin Oncol 2017;35:pre-publication. DOI: https://doi.org/10.1200/JCO.2017. 76.1155
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 207: Effects on birth weight and risk of preterm birth of light-to-moderate drinking during pregnancy – 2 November 2017
There is no question that high levels of alcohol consumption during pregnancy can lead to severe adverse effects on the fetus, with the most serious condition known as fetal alcohol syndrome (FAS). Many studies have also related alcohol intake during pregnancy with premature birth, low birth weight, and the infant being small for gestational age (SGA). Data are not as clear on the effects just of occasional or light drinking, but most studies have not detected adverse effects.
The present paper, based on a pooled sample of almost 200,000 women from nine European cohorts, provides data indicating that premature birth, an infant being small for gestational age (SGA), or being of low birth weight do not appear to be associated with light-to-moderate intake (up to 6 drinks/week); these results are similar to those from many other recent studies. In this large study, mothers who consumed greater amounts of alcohol tended to have an increased risk of the infant being SGA or with low birth weight, but such a level of drinking had no effect on the risk of premature delivery. This cohort consisted almost exclusively of light drinkers; no data were available on other potentially harmful effects of excessive drinking.
An interesting additional finding was that the reported frequency of any alcohol consumption during pregnancy in the cohorts studied has decreased dramatically in recent decades (from approximately 50% of women studied prior to 2000, to 39% in 2000-2004, to 14% in 2005-2011). This suggests that most women are responding to guidelines recommending that a woman not drink during pregnancy.
Based on currently available information, the Forum considers that a recommendation to “avoid alcohol during pregnancy” is appropriate as part of drinking guidelines for the public. However, scientific data, including the present paper, do not suggest that women who may have an occasional drink or very light alcohol consumption during pregnancy should have undue concern about having a premature birth or a low-birth-weight infant.
Reference: Strandberg-Larsen K, Poulsen G, Bech BH, Chatzi L, Cordier S, et al. Association of light-to-moderate alcohol drinking in pregnancy with preterm birth and birth weight: elucidating bias by pooling data from nine European cohorts. Eur J Epidemiol 2017 pre-publication; DOI 10.1007/s10654-017-0323-2
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 206: Importance of considering cultural factors in determining effects on health of alcohol consumption – 3 October 2017
It has been clearly shown that presumably similar amounts of alcohol tend to have different health effects (both beneficial and adverse) in different cultures. Greater health benefits from moderate alcohol intake have been shown, for example, in southern European countries (where wine with meals is common) than in more northern European countries, where beer and spirits are more likely to be consumed and usually not with food. Some of these differences may relate to the beverage consumed, while others may relate especially to different patterns of consumption. Further, in certain cultures, intoxication after drinking is expected and even tends to not be condemned. In the typical Italian culture, however, it would not be socially acceptable for a guest at a family dinner to become overtly intoxicated, and such would probably be less often reported in an epidemiologic study even if it had occurred. Thus, similar rates of alcohol-use disorders would be ascertained differently in different countries.
We know that the net effect of alcohol consumption relates to the amount of alcohol, the type of beverage, the rapidity of consumption, whether drinking with or without food, and surely a number of genetic factors of the drinker. What we are often unsure about is what the cultural context of drinking is for an individual subject or subjects in a certain population: different cultures seem to help control, or not control, the risk of drinking excessively. As pointed out by the present paper, these factors complicate the comparison of results of epidemiologic studies from different cultures.
In planning and interpreting results of epidemiologic studies, investigators now realize that simply estimating the average alcohol consumption over a period of time, usually a week, is inadequate to quantify alcohol exposure. The pattern of consumption (especially whether with or without food and whether regularly or in binges) is especially important. And, as the present study points out, knowing about the cultural aspects of drinking for a specific population is also key to interpreting the results. How best to do this, so that studies in different countries can be compared, remains difficult.
Reference: Rehm J, Room R. The cultural aspect: How to measure and interpret epidemiological data on alcohol-use disorders across cultures. Nordic Studies on Alcohol and Drugs 2017;34:330–341. DOI: 10.1177/1455072517704795.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 205: A very large population-based study of the association of alcohol consumption with total and disease-specific mortality – 4 September 2017
The usual finding in longitudinal cohort studies has been that light-to-moderate consumers of alcohol tend to be at lower risk for total mortality and show greater longevity of life, even when other lifestyle/demographic factors known to affect longevity are adjusted for in the analysis. The present analysis is important as it presents data on the relation of alcohol intake to total mortality as well as to specific mortality from cardiovascular disease (CVD) and cancer for a very large number of subjects in the USA. It is based on data from more than 300,000 subjects, of whom almost 25,000 died during a follow-up period averaging 8.2 years. There was a very large number of lifetime abstainers which could serve as an appropriate reference group for their analyses. Further, by adjusting for a number of chronic diseases, and carrying out sensitivity analyses with a 2-year lag period for mortality, the investigators improved their ability to avoid having their results affected by “sick quitters.”
The authors conclude that their analysis shows that light and moderate drinkers have a lower risk of total mortality, as well as mortality from CVD, heart disease, and cerebrovascular disease. The protective effects of alcohol for such cardiovascular outcomes were not present for subjects who reported binge drinking or for those reporting what was defined as “heavy” drinking (>7 drinks/week for women and older men, 14 drinks/week for younger men). Interestingly, the mortality risk for light and moderate drinking was also significantly reduced for deaths attributed to cancer; Forum members thought that this may have possibly resulted from subjects with cancer who actually died from CVD having their deaths attributed to cancer. Subjects reporting heavy drinking and those with binge drinking showed increased risk of all-cause and cancer mortality, with no significant effect on CVD outcomes. The key results of the study are that there is a very clear J-shaped curve for the relation of alcohol to mortality, with lower total, cardiovascular, and even cancer mortality rates for light and moderate drinkers who do not binge drink. There was increased total mortality and cancer mortality for those classified as “heavy” drinkers.
Forum Members thought it unfortunate that beverage-specific data were not presented (as in many studies wine, and sometimes beer, drinkers have better outcomes than consumers of spirits), that subjects of all ages (≥ 18 years of age) were included in a single analysis (rather than also presenting results specifically for older subjects, when the outcome events studied usually occur), and especially that women and older men who consumed > 7 drinks/week, and younger men consuming >14 drinks/week were all combined into a “heavy” drinking category. It would have been preferable that the investigators also had a category for those consuming only slightly more than the recommended levels, who may well have had different outcomes than heavier drinkers.
Overall, Forum members considered this to be a well-done study providing additional data supporting a J-shaped curve for the association of alcohol consumption with mortality. Thus, data continue to indicate that light-to-moderate intake of alcoholic beverages without binge drinking reduces total mortality as well as death from CVD or cancer. The cumulative scientific data on this topic are well described in the accompanying Editorial Comment by de Gaetano and Constanzo in the same issue of the journal.
Reference: Xi B, Veeranki SP, Zhao M, Ma C, Yan Y, Mi J. Relationship of Alcohol Consumption to All-Cause, Cardiovascular, and Cancer-Related Mortality in U.S. Adults. J Am Coll Cardiol 2017;70:913–922
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 204: Moderate drinking improves the chances for healthy survival to age 85 – 21 August 2017
A number of studies have shown that the risk of cognitive impairment appears to be reduced among elderly subjects who consume moderate amounts of alcohol; most studies indicate that both light and moderate drinking are associated with a lower risk of dementia, but heavy drinking is often shown to be associated with higher cognitive risk for dementia and cognitive impairment. In some studies, a protective effect of light-to-moderate alcohol intake has been seen primarily among consumers of wine, or sometimes beer/wine. Further, almost all well-done cohort studies have shown that moderate drinkers tend to have longer lifespans.
The present study is based on a group of ageing subjects in California that had been observed closely for several decades; the average follow-up period for these particular analyses were about 14 years. Subjects in this cohort have had multiple assessments of cognitive ability and frailty. The authors conclude that their subjects who reported moderate alcohol consumption in the late 1980s were more likely than non-drinkers during follow up to survive to age 85 years of age, and also to be more likely to survive to age 85 cognitively intact (without evidence of dementia). Also, daily or near-daily drinkers had better health outcomes than those of non-drinkers or less-frequent drinkers.
The Forum considers this to be a well-done study; while it is not based on a large cohort, it provides new data by having extensive evaluation over time in a cohort of community-dwelling elderly subjects. The results support data from most other studies of survival and dementia among moderate drinkers, but adds specific information on survival to age 85 without cognitive impairment.
This study and the review of prior scientific data on this subject led Forum members to also raise a question about the typical guidelines for alcohol consumption for the elderly: generally less or no alcohol consumption is advised. Given that current scientific data show that the risks of the common disease outcomes of older subjects (e.g., coronary artery disease, ischemic stroke, osteoporosis, dementia, mortality) are lower among moderate drinkers than among non-drinkers, it may be time to reevaluate such restrictions that are based on age alone.
Reference: Richard EL, Kritz-Silverstein D, Laughlin GA, Fung TT, Barrett-Connor E, McEvoy LK. Alcohol Intake and Cognitively Healthy Longevity in Community-Dwelling Adults: The Rancho Bernardo Study. J Alzheimer’s Dis 2017;9:803–814. DOI 10.3233/JAD-161153
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=================================================================
Critique 203: Moderate alcohol intake may reduce, not increase, the risk of falls in the elderly – 7 August 2017
Falls are common among the elderly, and markedly increase the subsequent risk of morbidity and mortality. There has been much written about the dangers of even light-to-moderate intake of alcohol among the elderly, with an increase in potential falls being one key reason cited. This may not be in the best interest of many elderly subjects; the demonstrated protection of light-to-moderate alcohol intake against many of the diseases of ageing (especially coronary heart disease, stroke, osteoporosis, dementia) could outweigh any dangers from falls if the latter risk is not great.
The present study examined the association between certain patterns of alcohol consumption, including the Mediterranean drinking pattern (MDP), and the risk of falls in more than 2,000 elderly subjects over 3.3 years; at the end of follow up, 21.4 % of subjects reported at least one fall in the previous year. The study found that up to moderate amounts of alcohol (defined as less than 40 grams of alcohol/day for men and less than 24 grams/day for women) did not increase the risk of falls, but actually resulted in a significant decrease of 20% or more in such risk. The risks for having multiple falls or those requiring medical care were also lower for moderate drinkers. The investigators report further that subjects with higher scores for a Mediterranean-type diet, that includes regular wine consumption, had similar or more impressive reduction in their risk of falls.
The specific reasons for such protection are not fully known, but a number of favorable effects on health of moderate drinking (e.g., less osteoporosis, less cardiovascular disease, less dementia, greater functional capacity, etc.) may play a role. While the investigators of this study were able to adjust for many factors known to be associated with falls, residual confounding is always a possibility to explain these results.
To summarize, while previous studies have often reported an increase in risk of falls for heavy drinkers, the present study supports results of many previous studies indicating that light-to-moderate alcohol intake does not increase the risk, and often is shown to decrease the risk of falls and fractures. In the present study, even with adjustments for most known lifestyle factors affecting risk, moderate drinking was associated with at least a 20% decrease in the risk of falls when compared with abstainers. This is a message that needs to be incorporated into drinking recommendations for the elderly.
Reference: Ortolá R, García-Esquinas E, Galán I, Guallar-Castillón P, López-García E, Banegas JR, Rodríguez-Artalejo F. Patterns of alcohol consumption and risk of falls in older adults: a prospective cohort study. Osteoporosis International 2017, on-line publication. DOI 10.1007/s00198-017-4157-2.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
==================================================================
Critique 202: Importance of folate intake for reducing breast cancer risk from alcohol consumption, especially for women with a positive family history of breast cancer – 17 July 2017
The strongest factor associated with the risk of a woman developing breast cancer appears to be a positive family history of such a diagnosis in a sibling or mother. Among environmental factors, almost all studies have shown that alcohol consumption relates to increased risk; a slight increase is often seen even among women who report only light drinking, e.g., an average of less than one drink per day. The present study evaluates how a positive family history of breast cancer in a first-degree relative and folate intake may modify the association between alcohol intake and breast cancer; the analysis is based on data from a large number of young women, aged 27-44 years at baseline, over a follow-up period of 20 years.
Forum members considered that this was a very well-done analysis from the large Nurses’ Health Study II, which followed young women for two decades. Alcohol consumption in total drinks/week was based on repeated assessments (but the pattern of drinking, binge versus regular drinking, was not evaluated). Repeated dietary questionnaires were used to estimate folate input. More than 2,800 incident invasive breast cancers were detected, essentially all being validated by a review of medical records.
The main results of this study were that without a positive family history of breast cancer, there was no significant increase in cancer risk for any level of alcohol intake. With a positive family history, however, there was a tendency for higher risk with increasing alcohol intake; this increase was not statistically significant for those with high folate, but a significant positive association (HR=1.82, 95% CI 1.06, 3.12; P-trend = 0.08) with cancer was seen for subjects with the highest level of alcohol intake plus low levels of folate.
Forum members conclude that the results from the present study should greatly relieve anxiety about breast cancer for women without a positive family history of breast cancer who choose to consume light-to-moderate amounts of alcohol. For women with a first-degree relative with breast cancer, the data indicate that if they maintain a high level of folate intake, it may attenuate an increase in risk associated with alcohol intake.
Reference: Kim HJ, Jung S, Eliassen AH, Chen WY, Willett WC, Cho E. Alcohol consumption and breast cancer risk by family history of breast cancer and folate intake in younger women. Am J Epidemiol 2017: pre-publication.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
==================================================================
Critique 201: The marked effect of lifestyle on mortality — 26 June 2017
The aim of the present study was to examine differences in the risk of mortality and in survival associated with a healthy lifestyle versus a less healthy lifestyle. The analyses were based on a total of more than 60,000 Swedish men and women who were followed in one of two studies; at baseline, the subjects were aged 45 to 83 years and were free of cancer and cardiovascular disease. The goal was to evaluate the effects of four “healthy” lifestyle factors: (1) nonsmoking; (2) physical activity at least 150 min/week; (3) alcohol consumption of 0–14 drinks/week; and (4) a healthy diet, with the latter defined as a modified Dietary Approaches to Stop Hypertension (DASH) Diet score above the median. Cox proportional hazards regression models and Laplace regression were used to estimate respectively hazard ratios of all-cause mortality and differences in survival time.
The authors report: “Compared with individuals with no or one healthy lifestyle factor, the multivariable hazard ratios of all-cause mortality for individuals with all four health behaviors were 0.47 (95% confidence interval [CI] 0.44-0.51) in men and 0.39 (95% CI 0.35-0.44) in women. This corresponded to a difference in survival time of 4.1 (95% CI 3.6-4.6) years in men and 4.9 (95% CI 4.3-5.6) years in women.”
Forum members considered this to be a well-done study on a large cohort with complete follow-up data on mortality. Notable weaknesses included the fact that never drinkers and consumers of 0 to 14 drinks/week were considered in one group (thus, including lifetime abstainers, ex-drinkers, and current moderate drinkers); these subjects were compared with consumers of >14 drinks/week. Thus potential differences between abstinence versus light/moderate consumption could not be determined. Further, there were incomplete data on the pattern of drinking, and no data on the type of beverage consumed were reported. Nevertheless, the reduction in mortality for subjects following a healthy lifestyle was impressive: a reduction by half, or more, in the risk of mortality and a 4- to 5-year longer lifespan.
Based on a number of previous studies that evaluated similar lifestyle factors and mortality, the results of this study were not unexpected. Still, they strongly support the remarkable effects on mortality and survival of these lifestyle factors. While not smoking was clearly the factor with the strongest effect on reducing mortality, having a healthy diet, exercising, and consuming light to moderate amounts of alcohol all make additional contributions. This is an important message in that even individuals who may be challenged by genetic or socioeconomic predispositions to earlier demise, adopting certain lifestyle habits can help them reach their greatest potential for a longer and healthier lifespan.
Reference: Larsson SC, Kaluza J, Wolk A. Combined impact of healthy lifestyle factors on lifespan: two prospective cohorts. J Int Med 2017. Pre-publication. Doi: 10.1111.joim.12637.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
Critique 200: Does Light Drinking Increase the Risk of Cancer? — 8 June 2017
The association between the consumption of alcohol and the risk of cancer has been of great interest for many decades. There are a number of types of cancer, especially those of the upper aero-digestive tract (such as mouth, tongue, pharynx, etc.) that are clearly increased among heavy drinkers, especially among subjects who are also heavy smokers. Cancer of the liver can be a result of alcoholic liver cirrhosis, related to long-term heavy drinking. Further, an increased risk for many other cancers have been shown for heavy drinkers, but generally not for light or moderate drinkers.
The risk of breast cancer in women, however, is usually found to be slightly higher in even light drinkers than it is among non-drinkers. This has been a common finding, although some studies suggest that the pattern of drinking, the estimated level of underreporting of alcohol intake, use of hormone replacement therapy, and level of folate intake may all affect this association. For colorectal cancer, some studies suggest an increase in risk even among light-to-moderate drinkers. This has led some to proclaim that no alcohol consumption is preferable for the prevention of cancer. Others suggest that it is important to consider not only cancer, but other diseases; for example, coronary heart disease, ischemic stroke, diabetes, and dementia (all of which are important causes of disability and death) occur less frequently among moderate drinkers than among non-drinkers. Further, the risk of total mortality is almost always found to be lower among light to moderate drinkers than among abstainers.
The present analysis was designed to help determine the association of light or moderate drinking with the risk of cancer. It consisted of a meta-analysis based on a total of 60 studies from 135 articles and included only cohort studies of high quality. The analysis focused on the association between very light (≤0.5 drink/day), light (≤1 drink/day), or moderate drinking (1-2 drinks/day) and the risk of cancer incidence and mortality.
The authors found that very-light drinking was not associated with the incidence of most cancers except for female breast cancer and male colorectal cancer, and was associated with a decreased incidence of both female and male lung cancer and both female and male thyroid cancer. Moderate drinking significantly increased the incidence of male colorectal cancer and female breast cancer, whereas it decreased the incidence of both female and male hematologic malignancy.
Forum members considered this to be a well-done meta-analysis, based on a large number of studies. The main weaknesses of the study related to the lack of ability of the authors to evaluate a number of known confounders: underreporting of alcohol intake, the pattern of drinking or the type of beverage consumed, socio-economic status, and folate intake or other dietary factors. Further, the authors did not describe the effects of alcohol consumption on total mortality.
The results of this study, obviously, support most previous epidemiologic evidence on the association between alcohol consumption and cancer. Larger amounts of alcohol are associated with increased risk of a number of cancers, and even light consumption is associated with the risk of breast cancer, and possibly colorectal cancer. However, given the inability to adjust for many confounders in this study, and lack of data on the net effects in terms of total mortality, it remains difficult for scientists to provide scientifically sound and balanced guidelines regarding the health consequences of alcohol consumption that are applicable to everyone in the population.
Reference: Choi Y-J, Myung S-K, Lee J-H. Light Alcohol Drinking and Risk of Cancer: A Meta-analysis of Cohort Studies. Cancer Research and Treatment 2017; pre-publication release.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=======================================================================
Critique 199: Potential mechanisms for the greater risk and fewer health advantages from alcohol consumption for subjects with low socio-economic status – 25 May 2017
The majority of epidemiologic studies have shown that both the positive and negative health effects of alcohol consumption are modified by the socio-economic status (SES) of individuals, with truly moderate drinkers who are from higher SES strata having better health outcomes and fewer adverse effects from alcohol than lower-SES subjects supposedly consuming similar amounts. One potential explanation for this has been that higher SES subjects (those with higher education, income, job status, etc.) are more likely to be regular moderate drinkers, more likely to be wine drinkers, and to drink primarily with meals, while lower SES subjects are more likely to binge drink (mainly beer or spirits), not with food, and may tend to under-report their alcohol intake. However, there are limited scientific data on the specific mechanisms by which such differences occur.
The authors of the present paper have used data on alcohol intake collected in the Scottish Health Surveys from more than 50,000 subjects to investigate whether the harmful effects of alcohol differ by socioeconomic status when accounting for a number of SES factors. They had very good measures of SES based on education, income, social class (professionals, skilled manual labor, unskilled labor, etc.), and a “measure of deprivation” of the geographic area of the subject (based on multiple measures of deprivation from government administrative data). Their health outcome measures were based on public records for deaths, admissions, and prescriptions; their primary outcome was alcohol-attributable admission or death. Their data show that, even without considering alcohol consumption, lower SES subjects were at much greater risk for poor health outcomes. And, while risks associated with increasing amounts of alcohol were present in all SES groups, they were much greater in the lower groups.
Forum members considered this to be a well-done study, but pointed out that there was limited information on the pattern of drinking and no data on the type of alcoholic beverage consumed or whether or not it was consumed with food. There was no dietary information or genetic information available, and little data on access to health care. While the study showed very marked differences in adverse health outcomes according to SES, the authors found that the factors they considered explained little of the health effects seen. They concluded: “Disadvantaged social groups have greater alcohol-attributable harms compared with individuals from advantaged areas for given levels of alcohol consumption, even after accounting for different drinking patterns, obesity, and smoking status at the individual level.”
Forum members agree that there may be many other lifestyle factors associated with poverty that scientists are unaware of, or unable to adequately control for, in their analyses. Differences by SES in the assessment of alcohol intake remains as a potential factor (especially given that higher SES subjects are usually found to consume alcohol regularly and moderately, less in binges, more often consuming wine with food, etc.). The authors of the present paper have evaluated a number of factors (including smoking status and obesity) as potential explanations for the poorer outcomes among lower SES subjects, and still found large differences in health effects despite adjusting for a number of such lifestyle factors. Thus, the specific reasons why lower SES subjects have worse health overall and poorer effects after alcohol consumption remain unclear.
Reference: Katikireddi SV, Whitley E, Lewsey J, Gray L, Leyland AH. Socioeconomic status as an effect modifier of alcohol consumption and harm: analysis of linked cohort data. Lancet Public Health 2017. Online publication May 10, 2017. http://dx.doi.org/10.1016/S2468-2667(17)30078-6
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================
Critique 198: A study of alcohol and cardiovascular disease based on “Big Data,” linked electronic medical records from the population — 24 April 2017
Essentially all observational cohort epidemiologic studies have shown a “J-shaped” curve for the association of moderate alcohol consumption with coronary heart disease and myocardial infarction, in that non-drinkers and heavy drinkers have higher risk than moderate drinkers. The present study presents a new approach for evaluating this relation by using electronic medical records for a very large number of patients (“big data”) in the UK to judge the relation between alcohol consumption and a variety of cardiovascular disease (CVD) outcomes. The study evaluated clinical data recorded by physicians from almost 2 million subjects, with about 115,000 CVD events recorded in public records. The exposures and outcomes came solely from the medical diagnoses given by individual physicians, and such diagnoses are known to often be inaccurate. For individual subjects, the exposure was based on codes for alcohol use or misuse in their medical records, and the cause of death was based on that recorded by the physician (which is not always consistent with diagnoses from autopsies or medical record reviews). Such problems would be expected to decrease the precision of the exposure and of outcome diagnoses.
Forum reviewers of this paper considered that the authors made a valiant effort in attempting to take into account the limiting factors of using big data for epidemiologic research. It is recognized that studies such as these cannot evaluate the pattern of drinking (regular versus binge) and the investigators were unable to evaluate different effects according to the type of beverage consumed (beer, wine, or spirits). It would be expected that both of these factors may have affected their results. Nevertheless, their conclusions strongly support the extensive observational data from cohort studies over many decades that have shown a higher risk among abstainers (versus moderate drinkers) for many CVD outcomes. In the present study, non-drinkers had significantly higher risk for unstable angina, myocardial infarction (MI), unheralded coronary death, heart failure, ischemic stroke, peripheral arterial disease, and abdominal aortic aneurysm. For most of these outcomes, heavy drinkers tended to have an increased risk (a J-shaped curve), but the risk for myocardial infarction and for stable angina remained decreased even for the heavy drinking category. For other manifestations of CVD, especially those related to cerebral artery disease (other than ischemic stroke), there was less of a clear pattern relating alcohol to disease. For their aggregate, overall outcome based on all manifestations of CVD, their analyses add further support for a J-shaped curve between alcohol intake and CVD.
Reference: Bell S, Daskalopoulou M, Rapsomaniki E, George J, Britton A, Bobak M, Casas JP, Dale CE, Denaxas S, Shah AD, Hemingway H. Association between clinically recorded alcohol consumption and initial presentation of 12 cardiovascular diseases: population based cohort study using linked health records. BMJ 2017;356:j909. http://dx.doi.org/10.1136/bmj.j909
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================
Critique 197: Alcohol consumption and the risk of developing dementia – 13 April 2017
A number of epidemiologic studies have found that light-to-moderate alcohol intake is associated with a lower risk of developing dementia and/or cognitive decline, while excessive drinking may increase the risk. The authors of the present paper carried out a meta-analysis of the current scientific literature that was based on data from 11 studies with 4,586 cases of all-cause dementia diagnosed among more than 70,000 subjects and two additional analyses of studies of approximately 50,000 subjects each for evaluating the association of alcohol intake with the diagnosis of Alzheimer’s disease or vascular dementia. Seven studies provided results according to type of alcoholic beverage consumed, while two provided results according to APOE 4 levels.
The conclusions of the authors are that, considering all sources of alcohol, light-to-moderate alcohol consumption was associated with a lower risk of all forms of dementia; the risk was reduced for up to 12.5 g/day (about one typical drink) and increased for consumers of more than 38 g/day (about 3 to 4 typical drinks). However, beverage-specific analyses indicated that the effect was only for wine, and not for consumption of beer or spirits. For moderate consumers of wine, the risk of dementia was reduced by 40% or more in comparison with that of non-drinkers. Little effect was noted among drinkers of spirits, and heavy beer drinkers appeared to have an increased risk of dementia. The presence or absence of APOE 4 did not appear to modify the effects.
Forum reviewers considered this to be a very well-done meta-analysis of the current literature on the topic. It was based only on prospective epidemiologic studies of very good quality, and sub-analyses evaluated the separate effects of each type of alcoholic beverage. While the authors were unable to include the pattern of drinking (binge versus regular moderate) in their analyses, and could not test for previous alcohol consumption among current non-drinkers, Forum members agreed with the primary findings of a J-shaped curve between alcohol consumption and all types of dementia (including vascular dementia and Alzheimer’s disease).
Most of this Forum critique deals with potential mechanisms by which wine consumption may reduce the risk of dementia and/or cognitive decline. In addition to the effects of both alcohol and polyphenols in wine on decreasing atherosclerosis and having beneficial effects on hematological factors (affecting cerebral as well as coronary arteries), there may also be anti-inflammatory effects and direct effects on brain structures that play a role. Given that the beneficial effects were primarily among wine consumers, this suggests that the polyphenols and other non-alcohol substances in wine (perhaps in interaction with alcohol) may be more important than the alcohol itself in reducing the risk of dementia.
The mechanistic studies described in the paper and in this critique provide considerable support for the epidemiologic findings of less dementia and cognitive decline among moderate drinkers. Forum member agree with the authors of this paper that light-to-moderate wine consumption may help lower the risk of dementia, an increasingly important condition in the world’s rapidly ageing populations.
Reference: Xu W, Wang H, Wan Y, Tan C, Li J, Tan L, Yu JT. Alcohol consumption and dementia risk: a dose-response meta-analysis of prospective studies. Eur J Epidemiol 2017;32:31-42. doi: 10.1007/s10654-017-0225-3. Epub 2017.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================
Critique 196: Adverse health effects of binge drinking on cardiovascular disease — 2 February 2017
This review paper on the effects of binge drinking on the risk of cardiovascular disease (CVD) provides considerable information on a topic of importance to public health. It clearly indicates that subjects who binge drink, however defined, tend to be at increased risk for hypertension, myocardial infarction, stroke, and cardiac arrhythmias. These adverse health outcomes are in addition to the well-known effects of binge drinking on drunkenness and many adverse health effects, both acute and chronic, as well as risk from violence and accidents to the drinker and to others.
While the members of the Forum applaud the efforts of the authors to present data on this relation, this paper failed to include many important previous research reports on the topic. Forum member Ian Puddey and others have prepared an extensive summary of many of the key research papers not addressed by the authors of this paper; their remarks are included in the full Forum critique. It describes how many factors, such as not only the amount but the rate at which alcohol is consumed, the type of beverage, whether or not food is being consumed, the prior drinking habits of the subjects, and many other factors can influence the effects of alcoholic beverages on health.
The Forum members conclude that a “comprehensive review” of binge drinking and other drinking patterns of alcohol in relation to the risk of CVD should include all of the available scientific data on the topic to be most useful. Taking into consideration the additional research results described in this critique provides a much better overview of the effects of binge drinking on CVD. The bottom line is that episodic heavy drinking, or binge drinking, has adverse influences on many health outcomes, including the risk of CVD.
Reference: Piano MR, Mazzuco A, Kang M, Phillips SA. Cardiovascular Consequences of Binge Drinking: An Integrative Review with Implications for Advocacy, Policy, and Research. Alcoholism: Clinical and Experimental Research 2017; Pre-publication. doi: 10.1111/acer.13329
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=========================================================================
Critique 195: How much of the “health benefits” of alcohol relate to higher socio-economic status of drinkers? — 19 December 2016
It has long been recognized from epidemiologic studies that both the positive and negative health effects of alcohol consumption are modified by the socio-economic status (SES) of individuals. Higher SES subjects (higher education, income, job status, etc.) are more likely to be regular moderate drinkers, while lower SES subjects are more likely to binge drink and under-report their alcohol intake. Truly moderate drinkers tend to have better health outcomes and fewer adverse effects from alcohol, and consistently show lower total mortality risks than non-drinkers or heavy drinkers.
The present study, from the New Zealand Longitudinal Study of Ageing, used data from the second examination of the cohort to do a cross-sectional analysis judging the relation of alcohol consumption to “health”. When controlling for age, income, and education (the latter two as measures of SES), they found a significant “J-shaped” association between reported alcohol intake and self-reported “physical health”. However, the authors state that they then used another measure of SES, the Living Standard Index-Short Forum (ELSI-SF), and found that the reported alcohol intake of subjects correlated with their measure of physical health almost exactly the same as with the results of the ELSI-SF. They conclude that there are no health benefits of moderate drinking, only that people with higher SES are more likely to drink moderately.
Forum members considered it unfortunate that the assessment of the exposure (alcohol intake) used in this study was based only on self-reported average intake and did not include data on the pattern of drinking (binge versus regular moderate intake, etc.). Further, their outcome was based only on a self-reported questionnaire of “physical health,” and did include any hard data; an overall index based on assessments of functional status, biomarkers of and the occurrence of disease, and mortality would be preferable when judging “health benefits” of alcohol. The Forum considered that the authors used inadequate indices of both the exposure to alcohol and their assessment of “health” (based on a questionnaire) to reach a conclusion that moderate drinking does not have any beneficial effects on health. This was done ignoring the massive amount of not only observational data but results from extensive experimental studies over more than four decades. Such research has found that moderate drinking not only has beneficial effects on assessments of physical health and disease occurrence, but results in significantly lower total mortality when moderate drinkers are compared with abstainers.
Regardless, given that this study, as have almost all epidemiologic studies, has shown the importance of SES on health outcomes, a key challenge to scientists is to seek to determine the mechanisms by which these differences occur. One potentially important factor is that the differing health outcomes relate to errors in judging the exposure, i.e., inadequate assessments of alcohol: not evaluating for binge drinking versus regular intake, consuming alcohol with or without food, type of beverage consumed, under-reporting of intake, etc. Also, much broader definitions of “health” are needed (rather than the results of a single self-administered questionnaire) that include the effects on functional status, disease states, and mortality. And, it is important that other lifestyle factors (smoking, drug use, etc.) that affect health be properly evaluated as determinants of health. Only with such data will we be able to fully judge the overall effects of alcohol consumption on health outcomes.
Reference: Towers A, Philipp M, Dulin P, Allen J. The “Health Benefits” of Moderate Drinking in Older Adults may be Better Explained by Socioeconomic Status. Pre-publication: J Gerontol B Psychol Sci Soc Sci 2016. doi:10.1093/geronb/gbw152
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 194: Long-term alcohol use and mortality among Swedish women – 22 November 2016
In a follow-up analysis of almost 50,000 young women, aged 30-49 at baseline, in the Swedish Women’s Lifestyle and Health cohort, the authors used self-reported information on alcohol consumption on two occasions, 12 years apart, to estimate the effects of alcohol on overall and cause-specific mortality. There were 2,100 deaths during follow up. Effects of alcohol on the two occasions, and changes between the two assessments among 33,000 women with available data, were related to mortality, as assessed from virtually complete national records.
Using “light” drinkers (0.1 – 1.49 grams of alcohol/day) as the referent group, the authors report an inverse association between greater amounts of alcohol consumption and mortality from cardiovascular disease. They report increased risk of cardiovascular and total mortality for abstainers. Despite the large number of total subjects, the authors report results separately for relatively narrow ranges of alcohol intake (none, 0.1-1.49, 1.5-4.9, 5-9.9, 10-14.9, 15+ g/day), which makes the numbers of subjects in many groups quite small. Given that the total mortality risks for most groups of drinkers were similar, it would have been interesting to see the effects of alcohol consumption (versus no consumption) using a broader definition of “moderate” drinking.
Forum members in general thought that this was a well-done study, using an excellent source of national records available in Sweden for determining mortality. They had concerns that the under-reporting of alcohol intake was not addressed; there is a high probability that some of the supposedly “light” drinkers may have actually consumed more alcohol, which would tend to decrease any differences between the referent group and the next groups of drinkers. This could help explain why, despite the strikingly lower risk ratios for cardiovascular disease for all drinkers when compared with the referent group, the inverse relation of alcohol was not statistically significant for any single group considered alone.
The Forum was also concerned that while the investigators had data on binge drinking and whether or not alcohol was usually consumed with meals, they chose not to include these data in their analyses. Given that drinking pattern plays a large role in determining favorable or unfavorable health effects of alcohol, the inclusion of such information may have better delineated the true effects of alcohol. Also, the authors “chose not to separately study the effects of different alcohol beverages;” reporting effects separately for beer, wine, and spirits could have provided key data on the effects of alcohol consumption.
The attempt of the authors to judge the effects of changes in alcohol intake during the study is laudable. Importantly, data on the reason that a woman may decide to increase or decrease her intake is not known; if due to the development of a serious disease, it may be the disease and not the change in alcohol intake that relates to subsequent mortality. However, given the inherent problems in assessing change, the results of this study are consistent with other studies that have suggested an increase in mortality risk for moderate drinkers who stop their alcohol consumption.
Reference: Licaj I, Sandin S, Skeie G, Adami H-O, Roswall N, Weiderpass E. Alcohol consumption over time and mortality in the Swedish Women’s Lifestyle and Health cohort. BMJ Open 2016;6:e012862. doi:10.1136/ bmjopen-2016-012862
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 193: The association of reported alcohol intake with the risk of subarachnoid hemorrhage: A meta-analysis – 1 November 2016
Data from epidemiologic studies are quite consistent for the relation of alcohol consumption with the different types of stroke: for ischemic stroke, an inverse association with moderate drinking and a possible increase with heavy drinking (a “j-shaped curve”); for hemorrhagic stroke, a direct positive association, although some studies suggest that there may be a threshold level for an increase in risk. Data are mixed on a possible association between the most uncommon type of stroke, subarachnoid hemorrhage (SAH). The present paper presents results of a meta-analysis relating reported intake of alcohol with subsequent risk of SAH. It was based on 14 observational studies reporting data on 483,553 individuals and 2,556 patients.
Forum members agree that this study suggests that alcohol intake, especially heavier drinking, increases the risk of SAH, although there was considerable heterogeneity among studies from different parts of the world, there were no countries from the Mediterranean area included, and there was no accounting for pattern of drinking (binge versus moderate regular) or type of beverage, all of which may affect risk.
The authors concluded that there was no relation between light (<15 g/day) or moderate alcohol consumption (15‑30 g/day) compared with abstaining individuals; this was based on statistically insignificant increases in RR of 1.27 (95% CI: 0.95, 1.68) and 1.33 (95% CI: 0.84, 2.09) for these two groups, respectively. However, Forum members suggest that there could be a slight increase in risk even for these two groups. For heavier drinkers (> 30 g/day, about 2 ½ to 3 typical drinks per day), the data indicate an increase in risk: RR=1.78 (95% CI: 1.46, 2.17).
It should be noted that the overall risk of total stroke is decreased from moderate drinking, as the most common type of stroke is ischemic, and moderate drinking has consistently been shown to lower such risk; this is especially related to lowering the risk of atherosclerotic or embolic clots. However, while rare, SAH is often a devastating disease, and the risk may be increased from alcohol consumption through its effects on decreasing coagulation.
Reference: Yao X, Zhang K, Bian J, Chen G. Alcohol consumption and risk of subarachnoid hemorrhage: A meta-analysis of 14 observational studies. Biomedical Reports 2016;5:428-436.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
=========================================================================
Critique 192: The association of alcohol consumption with the risk of prostate cancer –- 12 September 2016
Scientific data are mixed on the association of alcohol consumption with the risk of prostate cancer. In the present paper, the authors have used data from 11, 372 subjects in the Older Finnish Twin Cohort who provided data on alcohol intake on two occasions. They were followed for the development of prostate cancer from 1981 to 2012, during which 601 incident cases of prostate cancer and 110 deaths from prostate cancer occurred. The authors relate reported average alcohol intake, and whether or not the subject reported binge drinking, to the risk of prostate cancer and prostate cancer-specific death. They also evaluated the risks of prostate cancer among alcohol-discordant twins. The authors used current abstainers and ex-drinkers as the referent group in their main analyses, but did sensitivity analyses using never drinkers as an alternative referent group.
The type of beverage consumed was not known, so whether or not wine or beer consumption may have a different relation with prostate cancer than spirits intake cannot be determined. However, overall the data indicated a higher risk of prostate cancer from heavy intake and binge drinking, but also a high risk among abstainers. The number of discordant twins (for alcohol consumption) was too small for definitive results in terms of the risk of prostate cancer among subjects with the same or a similar genetic background , but the lowest risk was among light drinkers who did not binge drink. Even among this subset of the population, abstainers had higher risk than light drinkers.
Thus, the results of this well-done study suggest that there may be a J-shaped relation between alcohol consumption and prostate cancer risk. Light drinkers appear to have the most favorable results for both incident prostate cancer and prostate cancer-specific mortality. The risk for subjects reporting heavy drinking and binge drinking was higher for both incidence and mortality than the risk of light drinkers; for unexplained reasons, abstainers also tended to have higher risk of prostate cancer and mortality.
Reference: Dickerman BA, Markt SC, Koskenvuo M, Pukkala E, Muccil LA, Kaprio J. Alcohol intake, drinking patterns, and prostate cancer risk and mortality: a 30-year prospective cohort study of Finnish twins. Cancer Causes Control 2016;27:1049–1058. DOI 10.1007/s10552-016-0778-6
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 191: A new study on the mechanisms of alcohol’s effects on health and disease – 25 August 2016
While observational epidemiologic studies for many decades have consistently shown that moderate drinkers have a lower risk of cardiovascular diseases than do non-drinkers or heavy drinkers, the specific metabolic effects of alcohol have been little studied. In the present analysis, among almost 10,000 young adults from three population-based cohorts in Finland, associations of alcohol intake with 86 metabolic measures were assessed. Circulating lipids, fatty acids and metabolites were quantified by high-throughput nuclear magnetic resonance metabolomics and biochemical assays. The investigators found that alcohol consumption was associated with a complex metabolic signature, including aberrations in multiple biomarkers for reduced as well as elevated cardiometabolic risk; many factors showed different associations according to the estimated amount of alcohol consumed.
Among key associations found for greater alcohol intake were increases in HDL-cholesterol and its subclasses, decreases in LDL size, an increase in monounsaturated fatty acids and a decrease in omega-6 fatty acids, and lower concentrations of glutamine and citrate. For unexplained reasons, the changes in fatty acids from alcohol in this study were similar to those occurring following the administration of canola oil in other research. Some Forum reviewers pointed out that the analyses were not theory driven, and should only be used to generate hypotheses that would need to be tested in future experiments. As stated by one reviewer, the major contribution from this paper could be that it ignites the interest for experimental studies and provides new variables to be evaluated in prospective studies. In any case, the findings of this study provide valuable clues to the biologic effects on health, both favorable and adverse, related to alcohol consumption.
While not discussed by the authors, Forum members considered that the results of this paper might also be useful in providing a new approach for judging the level of alcohol intake of individuals in epidemiologic studies. At present, alcohol intake is judged almost exclusively from self-reports by subjects. Previous attempts designed to identify subjects more likely to be under-reporting their intake have shown that they may sharpen relations between estimated intake and health outcomes. Forum members believe that approaches that identify sources of bias for self-reported data, whether based on genetic, behavioral, physiological, or other information (preferably on all), might allow epidemiologists to have more precise and accurate information on alcohol intake when relating such to disease outcomes. A new approach for providing more accurate and unbiased estimates of alcohol intake is suggested by this excellent analysis.
Reference: Würtz P, Cook S, Wang Q, Tiainen M, Tynkkynen T, Kangas AJ, et al. Metabolic profiling of alcohol consumption in 9778 young adults. Int J Epidemiol 2016; pre-publication: doi: 0.1093/ije/dyw175
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 190: Alcohol intake during middle age and later atherosclerosis – 11 August 2016
Carotid artery disease can be estimated by ultrasound from the thickness of the wall of the arteries (recorded as carotid artery intima/medial thickness, cIMT) and by evidence of atherosclerotic plaques within the carotid arteries. The association between alcohol intake and such lesions is unclear, as some studies show a positive association with cIMT and/or plaques while others show no association. Given that carotid disease relates to the subsequent risk of coronary artery disease, there is increasing use of carotid ultrasound measurements to help determine long-term risk.
The present large study from the UK provides valuable information by reporting the cross-sectional relation between alcohol consumption and cIMT as well as how the drinking pattern over 20 years in middle age may relate to cIMT later in life. While heavy alcohol intake was found to increase later cIMT measures, no clear differences were noted between subjects reporting abstinence and those reporting moderate drinking in middle age.
Forum reviewers considered this to be a well-done study. There were some concerns that only total average alcohol intake was considered, as there were no data on the type of beverage consumed, the pattern of drinking (binge versus regular moderate), whether the alcohol was consumed with food, etc., and there was an absence of data on diet, physical activity, adiposity, and other factors related to atherosclerosis. Further, only the thickness of the carotid artery was evaluated, and not the presence or absence of atherosclerotic plaques on the ultrasound readings.
Overall, current scientific data provide strong evidence that moderate alcohol consumption lowers the risk of most manifestations of cardiovascular disease; it appears to work through a combination of effects on lipids, inflammation, coagulation, fibrinolysis, glucose metabolism, and other paths. Further, heavy drinking is known to increase blood pressure, and is an important factor for developing hypertension (and a strong determinant of cIMT). The failure of the present study to find a significant association between moderate alcohol intake and later carotid thickness supports what has been shown in some, but not all, previous studies.
If indeed chronic alcohol use has little effect on atherosclerosis (using images from the carotids as an index of atherosclerosis in the coronary arteries and elsewhere in the body), it may indicate that the mechanisms for the protective effect of moderate alcohol consumption on cardiovascular disease are not so much related to preventing atherogenesis, but due primarily to the effects on coagulopathy. And it is known that clot formation within the arterial wall is often the precipitating event for an acute myocardial infarction or other cardiovascular event.
Reference: Britton A, Hardy R, Kuhf D, Deanfield J, Charakida M, Bell S. Twenty-year trajectories of alcohol consumption during midlife and atherosclerotic thickening in early old age: findings from two British population cohort studies. BMC Medicine 2016l;14:111. DOI 10.1186/s12916-016-0656-9.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 189: Importance of drinking pattern on the effects of wine on health — 26 July 2016
A review article appearing in Food & Function, a publication of the Royal Society of Chemistry in the United Kingdom, presents a summary of evidence-based scientific data relating the moderate consumption of wine and other alcoholic beverages to health. Forum members considered the paper to be a well-thought-out appraisal of the effects that the pattern of consumption (e.g., the type of beverage, regular versus binge drinking, consumption with meals, etc.) affects its risks and benefits. (It is recognized that some of the authors of this publication work primarily with wine, but the review article covers key behaviors that affect the relation of the consumption of all types of alcohol to health.)
The authors describe how the polyphenols and other non-alcoholic components of wine provide anti-oxidants and decrease post-prandial oxidative stress. These phenols can also scavenge free radicals in the mouth and throughout the gastro-intestinal tract, preventing lipid peroxidation as well as the absorption of cytotoxic lipid peroxidation products. Wine also favorably affects urate levels; thus, the antioxidant activity is apparently influenced by two separate mechanisms: wine-derived phenolic compounds and plasma urate. A further important biological property of wine is its potent antimicrobial activity that tends to decrease adverse effects of food-borne and oral pathogens.
The article summarizes the key differences in health effects when alcohol (especially wine) is consumed moderately, with food, and on a regular basis rather than in binges. These differences emphasize why evaluating only the total amount of alcohol consumed, and not how it is consumed, is inadequate when evaluating its effects on health and disease. Further, the authors emphasize how all medical and scientific information concerning the effects of wine and alcohol consumption on human health should be evidence-based and communicated in a competent, credible and unbiased manner.
Reference: Boban M, Stockley C, Teissedre P-L, Restani P, Fradera U, Stein-Hammer C, Ruf J-C. Drinking pattern of wine and effects on human health: why should we drink moderately and with meals? Food Funct 2016;7:2937–2942. DOI:10.1039/c6fo00218h
Note on potential conflict of interest: While several of the authors of this paper are members of our Forum, they have had no input into the review of the article.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 188: Alcohol-attributable cancer in New Zealand . . . 28 June 2016
Previous scientific research has shown that heavy alcohol consumption is a major risk factor for upper aero-digestive cancers, and even light drinking increases slightly the risk of breast cancer in women. The present study is based on a very small number of cases of cancer in New Zealand, tabulated separately for Māori and non-Māori subjects, and applies estimates of alcohol effects from other population-based studies. Besides having so few cases, the investigators had no individual data (on the pattern of alcohol consumption, type of beverage, smoking or other lifestyle habits, socio-economic status, etc.) on subjects who did, or did not, develop these cancers. It is not even known whether or not the specific subjects who developed these cancers consumed alcohol.
It has repeatedly been emphasized that disease-specific death rates must be interpreted in light of the effects of the exposure (in this case, alcohol consumption) on other causes of death as well, especially on total mortality risk. The large majority of studies have shown that moderate drinking clearly reduces the risk of most cardiovascular diseases, diabetes, and other of the diseases of ageing, as well as the risk of total mortality. However, the estimated effects of alcohol on total mortality are not included in this paper.
The very long Discussion in this paper is primarily a treatise on how the public must be told of the dangers of cancer from any alcohol consumption; it focuses on health policy recommendations and very little on the limitations of the data and the study. The authors end up making very broad recommendations based on very small numbers of subjects. Limitations to this study suggest that it adds little to our current understanding of the relation of alcohol consumption to the risk of cancer and other diseases.
Reference: Connor J, Kydd R, Maclennan B, Shield K, Rehm J. Alcohol-attributable cancer deaths under 80 years of age in New Zealand. Drug and Alcohol Review 2016; pre-publication. DOI: 10.1111/dar.12443
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 187: Alcohol and squamous cell carcinoma of the skin — 14 June 2016
Skin cancers, whether melanoma, basal cell, or squamous cell, are all increased by ultra-violet rays of the sun, and such cancers are much more common in areas of the world with more sun exposure. Further, the risk of such cancers is higher among individuals reporting excessive tanning (either from the sun or from tanning salons). The present study was undertaken to judge the relation between alcohol consumption and the risk of cutaneous squamous cell carcinoma (cSCC), an association that is unclear from earlier research. Determining the relation between alcohol and skin cancer is made difficult by the fact that excessive sun exposure has been shown to be greater among consumers of alcohol than among abstainers, thus the potential for confounding.
In the present analyses, combined data from three cohorts of subjects in the US, who had repeated assessments of alcohol intake over many years, were evaluated tor the relation of alcohol to the development of verified cSCC. Subjects included women in two cohorts of the Nurses’ Health Study and men in the Health Professionals’ Follow-up Study. Among subjects providing a total of more than 4 million person-years of follow up, 2,938 cases of cSCC were identified.
The results varied somewhat among the different cohorts, but in the meta-analysis of the three studies using continuous measures of alcohol, there was an increase in risk of cSCC with alcohol intake. Among women, there was a steep increase in risk of cancer for low levels of intake (up to 5 grams of alcohol/day, slightly less than ½ of a typical drink), then a gradual increase in risk thereafter, whereas among men there was more of a gradual increase in risk with larger reported alcohol intake.
Overall, the authors report an increase in risk per typical drink per day of 22% for invasive cSCC and 14% for in situ cSCC. In beverage-specific analyses, white wine consumption of >/= 5 times/week was associated with an increased risk of cSCC (RR 1.31, 95% confidence interval: 1.09-1.59), but an increased risk of cSCC was not seen for other alcoholic beverages. The population-attributable risk associated with alcohol intake of ≥ 20 grams/day (about 1 ½ typical drinks) was 3% of cSCCs.
Forum members considered that the analyses were well done, and the results of the study are consistent with increases in risk associated with alcohol consumption for other types of skin cancer. Given that sun exposure is by far the primary risk factor for skin cancer, and consumers of alcohol tend to have greater number of sunburns (also shown in this study), it is always difficult to determine if residual confounding by sun exposure is playing a role. The authors of this paper attempted to adjust for sun exposure by including in their analyses the typical exposure values in the area of the world where the subjects resided, by recording the frequency that subjects reported 5 or more severe sunburns, and several other measures. As expected, there were reductions in the estimated RR for invasive cSCC when going from age-adjusted RR (1.34) to multivariable-adjusted estimates (1.22) of risk. However, the magnitude of decrease in risk estimates when only those adjustments for sun-exposure were added to the equation cannot be determined from the data presented.
Forum reviewers consider that these analyses support results from many previous studies and indicate that consumers of alcohol have a greater risk than non-drinkers of all types of skin cancer. Attempts to judge how much of this association may be due to residual confounding related to sun exposure are less than conclusive. Various hypotheses have been raised for possible interactions between sun exposure and alcohol, but currently there are no experimental data to test these theories. While the authors conclude that “physicians may consider counseling their patients about the association between alcohol consumption and risk for cSCC,” it might be more advantageous for physicians to focus more on the much greater protection against this disease that would occur if they were able to limit their patient’s exposure to ultra-violet radiation.
Reference: Siiskonen S, Han J, Li T, Cho E, Nijsten T, Qureshi A, Alcohol intake is associated with increased risk of squamous cell carcinoma of the skin: three US prospective cohort studies. Nutrition and Cancer 2016;68:545-553.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 186: Changes in alcohol and effects on risk of breast cancer and heart disease — 19 May 2016
This large study from Denmark was designed to test the hypothesis that women who increase their alcohol intake over a five year period have a higher risk of breast cancer and a lower risk of coronary heart disease (CHD) compared with women who exhibit a stable alcohol intake. It consisted of more than 20.000 postmenopausal women who had two assessments of alcohol intake, about 5 years apart; changes during that period were related to their subsequent risk of developing breast cancer or CHD, or dying, during the subsequent follow-up period that averaged 8 years.
For the risk of breast cancer, the baseline alcohol consumption reported by the women showed that higher alcohol intake was associated with a greater risk of developing breast cancer during follow up, but a lower risk of developing CHD and for total mortality. For relating changes in alcohol intake in the 5 years between the two alcohol assessments, those who increased their reported alcohol intake showed an increased risk of subsequent breast cancer, while those who decreased their intake also had a tendency for greater breast cancer. In terms of CHD and total mortality, the data were consistent with an increase in consumption lowering risk, while there was a tendency for a decrease in consumption to increase risk. Hence, the directionality for risk from changes in intake reflected the risks associated with baseline risk, and the authors conclude that their results “ . . .support the hypotheses that alcohol intake is associated with increased risk of breast cancer and decreased risk of coronary heart disease.”
Forum reviewers considered this to be a very well-done study. They, and the authors, appreciated the innate difficulty in separating effects on health of usual alcohol intake over time and changes over a limited period of time. Reviewers were also concerned by these problems, suggesting that some of the reported changes in alcohol consumption in this study may have just reflected individuals replying differently to questions regarding their drinking at different points of time. Further, the reason why some women may have actually increased or decreased their intake are not known.
Nevertheless, Forum members applaud the attempt of the authors to judge if changes in alcohol intake relate to cancer, CHD, and total mortality. This is a difficult task given that baseline and life-time alcohol consumption clearly relate to these outcomes. Further, data on the pattern of drinking (regular versus binge), any estimate of underreporting of alcohol, the type of beverage consumed and, as stated by the authors, certain known risk factors of breast cancer, were not available to be included in their analyses. Thus while the results of this study add important information on the relation of alcohol to disease, there remain questions about the specific relevance of changes in intake for such outcomes.
Reference: Dam MK, Hvidtfeldt UA, Tjønneland A, Overvad K, Grønbæk M, Tolstrup JS. Five year change in alcohol intake and risk of breast cancer and coronary heart disease among postmenopausal women: prospective cohort study. BMJ 2016;353:i2314. http://dx.doi.org/10.1136/bmj.i2314
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 185: An innovative assessment of alcohol consumption and the risk of atrial fibrillation – 28 April 2016
A study from Denmark has been carried out to test the hypothesis that alcohol consumption, both observational (self-reported) and estimated by genetic instruments, is associated with the risk of atrial fibrillation (AF) and to determine whether people with high cardiovascular risk are more sensitive towards alcohol than people with low risk. It was based on a large cohort of subjects (more than 88,000) with a mean follow-up period of 6.1 years; there were almost 3,500 cases of AF diagnosed from hospital records during follow up. Unfortunately, the authors did not have data to identify binge drinkers, which tend to show greater adverse cardiovascular events than regular moderate drinkers whose weekly intake may be the same.
The main results of the study were that men consuming more than 14 drinks/week, especially those consuming more than 28 drinks/week, had an increase in risk of AF, but no significant increase in risk was seen for any level of alcohol intake among women. When genotypes affecting alcohol metabolism (AHD1B, ADH1C) were studied in a Mendelian randomization analysis, the authors state that they “found no evidence to support causality of the observational findings.”
Forum reviewers of this article considered it to be a well-done study with appropriate analyses. Its results reflect the findings of most previous prospective studies and meta-analyses of little effect of light drinking on AF, but an increase in risk for heavier drinkers. The study also showed that the effects of alcohol consumption on the risk of AF were not different between subjects who had cardiovascular disease or were at high-risk of cardiovascular disease than for other subjects.
While Mendelian randomization using genetic factors affecting alcohol metabolism has been touted as an unbiased approach for judging causal health effects of alcohol, there are questions about the adequacy of such instruments for judging effects. In the present study, their use did not suggest that the relations shown by the self-report of alcohol by subjects necessarily indicated a causal association of alcohol with AF.
Overall, current data suggest that heavy drinking may increase the risk of AF, but there is little evidence of a meaningful increase in risk from light drinking. Luckily, such levels of alcohol intake (some guidelines suggest no more than 2 drinks/day for men or 1 drink/day for women) have been shown from many previous studies to significantly lower the risk of cardiovascular disease and total mortality.
Reference: Tolstrup JS, Wium-Andersen MK, Ørsted DD, Nordestgaard BG. Alcohol consumption and risk of atrial fibrillation: Observational and genetic estimates of association. European Journal of Preventive Cardiology 2016; pre-publication. DOI: 10.1177/2047487316641804
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 184: A major new meta-analysis on alcohol consumption and the risk of pancreatic cancer — 4 April 2016
The present meta-analysis was based on data from more than four million subjects in prospective cohort studies, among whom 11,846 incident cases of pancreatic cancer were diagnosed. With the lowest intake group (non-drinkers or occasional drinkers) as the referent group, the authors defined “light” consumption as up to 12 grams/day (essentially one typical drink); 12-24 g/day as “moderate”; and ≥24 g/day as “heavy” drinking. The key results of the study were that, overall, neither light drinkers (RR = 0.97) nor moderate drinkers (RR = 0.98) showed an increase in risk of pancreatic cancer, while subjects classified as heavy drinkers had a slight increase (RR= 1.15, 95% CI 1.06 – 1.25). The increase in risk was due to heavy drinkers of liquor, as there was no significant increase in risk even for heavy drinkers of beer (RR = 1.08, CI 0.90 – 1.30) or wine (RR = 1.09, CI 0.79 -1.49).
Forum members considered this to be an excellent paper on the association between alcohol consumption and pancreatic cancer. The authors used appropriate methods and limited subjects to those in prospective cohort studies, which would tend to limit bias. The paper shows that the significant increase in risk occurred only among men, with no significant effect of alcohol being found among women. Among the weaknesses of the study were that there was a mixture of lifetime abstainers and ex-drinkers included in the referent group, and the same cut-points for category of alcohol intake was used for both men and women, whereas drinking guidelines are generally lower for women than for men. Further, data on the pattern of drinking (regular versus binge) were not available.
To summarize, this study showed no significant association with cancer risk for any level of consumption of beer or wine, which could relate to their lower concentration of alcohol per volume of the beverage, to non-alcoholic substances (such as polyphenols, present in wine and beer), or even to different drinking practices among subjects consuming different beverages. Thus, Forum members agree with the conclusions of the authors that heavy alcohol consumption, especially of liquor, increases the risk of pancreatic cancer, but the intake of beer or wine may not be associated with an increased risk.
Reference: Wang Y-T, Gou Y-W, Jin WW, Xiao M, Fang H-Y. Association between alcohol intake and the risk of pancreatic cancer: a dose–response meta-analysis of cohort studies. BMC Cancer 2016;16:212. DOI 10.1186/s12885-016-2241-1
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
==============================================================================
Critique 183: An unusual analysis of the association of alcohol consumption with mortality — 24 March 2016
The stated purpose of this new analysis was to determine whether misclassifying former and occasional drinkers as abstainers and other potentially confounding study characteristics underlie observed positive health outcomes for low volume drinkers in prospective studies of mortality. Unfortunately, the authors include in their analyses a number of old epidemiologic studies and do not acknowledge that when the “errors” that they have commented on in the past (such as including heavy ex-drinkers in the no-alcohol referent group) have been dealt with in the majority of studies over the past decade. The authors still exclude the vast majority of these well-done studies in their new meta-analysis. Results of essentially all studies that adjust for their concerns continue to show a significant and meaningful reduction in the risk of cardiovascular disease (CVD) and total mortality from the moderate intake of wine and alcohol.
Forum members note how very selective the authors are in choosing which papers to include in their new analyses: they identified 2,575 studies on the subject, analyzed 87, but then they found some reason to exclude almost all of these studies to reach a conclusion that “ . . . there was no significant protection for low-volume drinkers (RR = 1.04, 95% CI [0.95, 1.15])” based on what is apparently only 6 remaining studies! The paper ignores the comments by two other scientists (Roerecke & Rehm) who, like these authors, have in the past been very concerned that confounding and errors weaken the purported relation between alcohol and a lower risk of cardiovascular disease, but have more recently concluded: “For drinkers having one to two drinks per drinking day without episodic heavy drinking, there is substantial and consistent evidence from epidemiological and short-term experimental studies for a beneficial association with IHD risk when compared to lifetime abstainers. The alcohol-IHD relationship fulfills all criteria for a causal association proposed by Hill.”
The authors of the present paper also ignore the immense amount of experimental data, not only animal experiments but trials in humans, that have described the mechanisms by which moderate alcohol and wine intake have been shown to decrease essentially all of the risk factors for CVD, including low HDL-cholesterol, elevated LDL-cholesterol, endothelial dysfunction, coagulopathies, inflammation, abnormal glucose metabolism, and many others. The consistent finding of lower CVD risk among moderate drinkers in all well-done cohort studies is strongly supported by experimental evidence of the mechanisms.
In the opinion of Forum members, the present paper markedly distorts the accumulated scientific evidence on alcohol and CVD. As stated by one Forum member, “The biased selection of studies that are included undermines the value of the paper, but more importantly promulgates misinformation in the name of appropriate scientific method. Failure to acknowledge the robust body of knowledge that supports the opposite conclusion, and disqualification of extensive animal and cell culture studies that offer plausible biologic explanation of observed benefits, is unconscionable.”
The Forum concludes that the overwhelming body of observational scientific data, as well as an immense number of experimental studies, support the contention that, for most middle-aged and older men and women who choose to do so, the regular consumption of small amounts of an alcoholic beverage can be considered as one component of a “healthy lifestyle.” Such a habit has been shown to be associated with a lower risk of cardiovascular disease and of total mortality.
Reference: Stockwell T, Zhao J, Panwar S, Roemer A, Naimi T, Chikritzhs T. Do “Moderate” Drinkers Have Reduced Mortality Risk? A Systematic Review and Meta-Analysis of Alcohol Consumption and All-Cause Mortality. J Stud Alcohol Drugs 2016;77:185–198.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 182: A major meta-analysis on the association of alcohol consumption with the risk of diabetes mellitus — 8 March 2016
Most previous studies have shown that consumers of light-to-moderate amounts of alcoholic beverages tend to have a significant reduction in their subsequent risk of developing Type II diabetes mellitus (DM). The purpose of the present study was to explore and summarize the evidence on the strength of the association between alcohol consumption and the subsequent risk of DM by using a dose-response meta-analytic approach. The authors identified 26 prospective cohort studies providing data appropriate for a meta-analysis; their analyses were based on 706,716 individuals (275,711 men and 431,005 women) with 31,621 cases of DM.
This meta-analysis reports that light and moderate drinkers have a significantly reduced risk of developing DM. For “light” drinkers (defined as an average of ≤ 12 g/day of alcohol), in comparison with non-drinkers, the overall risk ratio for DM was 0.83, with 95% CIs of 0.73, 0.95 (P = 0.005). For “moderate” drinkers (>12- <24 g/day), the RR was 0.74, with 95% CIs of 0.67, 0.82 (P = 0.001). Thus, data from this meta-analysis indicate a 17% and 26% reduction in the risk of DM, respectively, for these two drinking categories.
For subjects classified as “heavy” users of alcohol (reported intake averaging ≥ 24 g/day), the RR was 0.98, with 95% CIs of 0.83, 1.09, P = 0.480), interpreted as no effect. In a figure in the paper showing the separate results for each individual study included, the point estimates for the risk of DM were 1.0 or less than 1.0 for light and moderate drinkers in essentially all studies. Thus, data from the individual studies support the overall finding of a decrease in risk of DM for light or moderate drinkers.
Sub-group analyses showed that when subjects were stratified by sex, age, BMI, smoking, physical activity, and family history of DM, the point estimates of the risk ratios associated with light or moderate alcohol consumption were less than 1.0 in all groups, adding further to the robustness of the overall conclusions of a reduction in risk of DM from alcohol intake. Similarly, for all subjects, as well as for men and women separately, there was a clear U-shaped curve for the association. The nadir of the effect was just over 20 grams of alcohol per day (about 2 typical drinks), and even the risk of heavy drinkers did not reach the estimated risk of non-drinkers.
Forum members considered this to be a well-done analysis that confirms most previous results from prospective studies indicating a reduction in the risk of developing DM associated with moderate drinking. Further, an increasing number of randomized clinical trials are supporting such beneficial effects on the development and clinical treatment of DM. The Forum thought it unfortunate that beverage-specific results were not available in this study, as increasingly it is being shown that, beyond alcohol effects, there are polyphenols and other substances in wine and beer that provide additional protection against diabetes. Further, the Forum felt it important to also emphasize the protective effects against cardiovascular disease among subjects who already have DM, who are especially vulnerable to coronary heart disease and other effects of atherosclerosis.
Overall, this meta-analysis based on a large number of subjects indicates that the risk of DM is considerable lower among light and moderate drinkers than among abstainers. This finding supports the contention that, for most middle-aged and older adults (with the exception of individuals with specific prohibitions against alcohol such as former drug or alcohol abuse, certain types of neurological or severe hepatic disease, etc.), moderate alcohol consumption should be considered as a component of a “healthy lifestyle” that reduces the risk of diabetes and most of the chronic diseases of ageing.
Reference: Li X-H, Yu F-F, Zhou Y-H, He J. Association between alcohol consumption and the risk of incident type 2 diabetes: a systematic review and dose-response meta-analysis. Pre-publication: Am J Clin Nutr 2016; doi: 10.3945/ajcn.115.114389.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 181: Support for a causal role of alcohol consumption in improving the lipid profile — 16 February 2016
The present paper is based on data from more than 10,000 Americans of European descent who were participants in the Atherosclerosis Risk in Communities (ARIC) study. Common and rare variants in alcohol dehydrogenase and acetaldehyde dehydrogenase genes were evaluated using Mendelian randomization (MR), and then a genetic score based on 5 SNPs was used in regression analyses for the association of alcohol with lipids. Results reported by the authors state: “Alcohol consumption significantly increased HDL2-c and reduced TG, total cholesterol, LDL-c, sdLDL-c, and apoB levels. For each of these lipids a non-linear trend was observed. Compared to the first quartile of alcohol consumption, the third quartile had a 12.3% lower level of TG (p < 0.001), a 7.71 mg/dL lower level of total cholesterol (p = 0.007), a 10.3% higher level of HDL2-c (p = 0.007), a 6.87 mg/dL lower level of LDL-c (p = 0.012), a 7.4% lower level of sdLDL-c (p = 0.037), and a 3.5% lower level of apoB (p = 0.058, P overall = 0.022).”
The authors thus conclude that “This study supports the causal role of regular low-to-moderate alcohol consumption in increasing HDL2-c, reducing TG, total cholesterol, and LDL-c, and provides evidence for the novel finding that low-to-moderate consumption of alcohol reduces apoB and sdLDL-c levels among European-Americans.”
Forum members considered this to be a well-done and important study, the results of which indicate favorable effects of moderate alcohol consumption on lipid factors. However, they doubt that the inclusion of the genetic score from MR played a large part in the results; the authors state that the genetic score used in this paper explained only approximately 0.1% variance of alcohol consumption, suggesting that it was a weak instrumental variable for the MR. Several Forum members stated that randomized control trials, especially cross-over trials, testing the effects of alcohol intake on risk factors, may provide even better evaluation of alcohol’s effects on lipids. Until large-scale RCTs of alcohol and disease occurrence can be are carried out, such RCTs may provide the most reliable data on mechanisms of alcohol’s effects on the risk of cardiovascular disease.
Overall, the present study provides important data indicating that light-to-moderate alcohol consumption has favorable effects on most lipid values. The effects shown for HDL-cholesterol support much earlier data, and the effects on small dense LDL-cholesterol and ApoB provide key new information. The effects on lipids are surely important factors in the protective effects of moderate drinking against cardiovascular disease that have been seen in almost all well-done cohort studies.
Reference: Vu KN, Ballantyne CM, Hoogeveen RC, Nambi V, Volcik KA, Boerwinkle E, Morrison AC. Causal Role of Alcohol Consumption in an Improved Lipid Profile: The Atherosclerosis Risk in Communities (ARIC) Study. PLoS One 2016;11:e0148765. doi: 10.1371/journal.pone.0148765. eCollection 2016.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 180: The association of alcohol intake with total mortality risk among women — 9 February 2016
The follow up of more than 6,000 women in a population-based cohort in an area of southern Sweden was used to estimate how baseline levels of alcohol consumption, at age 50-59 years, related to total mortality risk over the subsequent 17 years. At baseline, 26% of women reported no alcohol consumption while 13% reported an average of 12 or more grams of alcohol per day. Thus, the large majority (61%) were light drinkers, reporting the equivalent of no more than one drink per day. The authors report that, even when adjusting for education, marital status, smoking, BMI, physical fitness, diabetes and ischemic heart disease before screening, mortality risk during follow up was significantly higher among non-drinkers and heavier drinkers than among women reporting the equivalent no more than one typical drink per day. They state that their analyses thus support a “J-shaped” association between alcohol and total mortality risk, and that “The observed protective effect of light drinking (1–12 grams/day) could thus not be attributed to any of these known confounders.”
Forum members agreed this was a well-done study, but noted that the authors were unable to adjust for the pattern of drinking (regular versus binge), previous drinking among abstainers, or potential changes in drinking during follow up. Also, beverage-specific results are not presented. Further, the data presented in this study are not adequate to judge the specific level of alcohol consumption at which total mortality risk for drinkers reaches or exceeds the risk for non-drinkers; in other words, the “threshold” for adverse effects of alcohol on mortality cannot be determined very well. Nevertheless, the results of these analyses are very consistent with most long-term follow-up studies and support a “J-shaped” association between alcohol and the risk of total mortality.
Reference: Midlöv P, Calling S, Memon AA, Sundquist J, Sundquist K, Johansson S-E. Women’s health in the Lund area (WHILA) – Alcohol consumption and all-cause mortality among women – a 17 year follow-up study. Pre-publication: BMC Public Health 2016;16:22. DOI 10.1186/s12889-016-2700-2.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 179: Response to proposed guidelines regarding alcohol consumption in “Guidelines for a Healthy Diet” from the the Health Council of the Netherlands – 26 January 2016
The Health Council of the Netherlands has published “Guidelines for a Healthy Diet” that include a section related to alcohol consumption. Our Forum has been asked to provide comments on the alcohol guidelines (an English translation of certain sections related to alcohol consumption are attached as an appendix to the full review of these guidelines). The closing guidelines given in the Dutch document are as follows: “Do not drink alcohol, or at least no more than one glass per day. [The guidelines from 2006 recommended limiting one’s alcohol intake to one glass (women) or two glasses (men). The current data suggests that the guideline for men should be adjusted downwards.]”
Forum members were concerned that the guidelines were based on a very restricted number of the many hundreds of excellent epidemiologic and experimental publications in recent years that clearly indicate that moderate alcohol has favorable effects on most of the diseases of ageing, and on total mortality risk. For example, the proposed guidelines focus on adverse effects of alcohol on lung cancer, while current scientific knowledge suggests that it has negligible effect. Much of the discussion in the guidelines focusses on the dangers of alcohol on cancer, whereas data show that almost all of the risk (except for breast cancer) is from heavy drinking, not light-to-moderate drinking. Data strongly support a major role of alcohol abuse for upper aero-digestive cancers, but only minor effect on cancer in general from light-to-moderate drinking, especially when other lifestyle factors and under-reporting of intake are taken into account.
The findings for a benefit of moderate drinking on cardiovascular disease among middle-aged and older adults are very much under-played, despite overwhelming data showing a significant benefit. The “J-shaped” curve (lower risk of many diseases with light-to-moderate alcohol intake with higher risk for heavier drinking) is not presented in the guidelines, a major omission when presenting data on alcohol to the public. The additional protection against disease when moderate alcohol consumption occurs with meals was not mentioned. As one Forum member commented: “When professionals discuss alcohol consumption, what consumers want to know is first ‘how much,’ and then ‘when’ to drink.”
Overall Forum members considered that the proposed guidelines regarding alcohol consumption from the Health Council of the Netherlands in a number of sections do not reflect current scientific knowledge on the association of alcohol to health and disease. Forum members tend to agree with the statement of Boffetta and Hashibe who, in an extensive review of alcohol and cancer, stated that “Drinking, especially heavy drinking, increases cancer risk. However, total avoidance of alcohol, although optimum for cancer control, cannot be recommended in terms of a broad perspective of public health, in particular in countries with high incidence of cardiovascular disease.”
Forum members consider that it is important to describe both the potential harms and benefits for health associated with alcohol consumption, especially for middle-aged and older adults. The “J-shaped” curve should be an important concept in any guidelines on drinking that are presented to the public.
Reference: An English translation provided to the Forum includes parts of Section 8 of the Guidelines for a Healthy Diet, from the Health Council of the Netherlands; this material is included as an Appendix to the full report of this critique.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 178: The association of alcohol intake with health-related quality of life — 12 January 2016
Many studies have shown that moderate alcohol drinkers tend to have higher ratings of their quality of life (QOL) than non-drinkers. The directionality of this association has been difficult to ascertain: does moderate drinking improve someone’s QOL, or do people with higher QOL to begin with tend to drink alcohol moderately? The present study attempts to provide data designed to evaluate the directionality of these associations for both physical aspects of QOL as well as mental aspects.
Forum reviewers considered this to be a very well-done study from the Nurses’ Health Study II, with excellent and repeated measurements of both alcohol consumption and indices of QOL. It deals with the assessment of both physical and mental aspects of quality of life as well as the directionality of such an association: subjects were repeatedly assessed for the effects of alcohol intake on subsequent QOL as well as the effects of a given QOL measure on subsequent alcohol intake.
The key reported findings of this study were a positive association between alcohol and subsequent indices of physical QOL indices, with the poorest outcomes in abstainers and former drinkers; in spline analyses, the favorable effect appears to be up to about 2 drinks/day. Subjects with higher physical QOL also appeared to consume more alcohol in subsequent assessments. Somewhat surprising was the finding of little relation between alcohol and mental aspects of QOL, and even an apparent deleterious effect at the highest category of drinking. Thus, the study reports that physical aspects of QOL are positively associated with alcohol consumption, while mental aspects show little relation.
There was some concern by some Forum members about the methods used by the authors in adjusting, or not adjusting, for previous exposures (both alcohol and indices of QOL). Given that both baseline alcohol intake and QOL measures may tend to remain rather static over the period of the study (this “prevalent” exposures), adjusting for the effects of baseline values could attenuate any effect seen on subsequent outcomes. For example, if alcohol consumption indeed affects QOL and consumption remains roughly the same over the time period of the study, any effect of subsequent alcohol on QOL may be subsumed by the effects shown at baseline. In that situation, the net effect of adjustment for baseline alcohol may attenuate (or remove) the effect of the follow-up exposure on the outcome variable. The authors of this paper were aware of this problem, and attempted to deal with it. However, from the data presented, it is not possible to ascertain the specific analytic procedures used, and the final estimates of effect given for alcohol and QOL may still be biased.
Overall, the Forum considers this to be an important contribution to our understanding of how alcohol consumption may affect quality of life, and how quality of life affects alcohol consumption. As interpreted by the authors, physical aspects of QOL may be positively affected by alcohol consumption, but there is little effect on mental aspects of QOL.
Reference: Schrieks IC, Wei MY, Rimm EB, Okereke OI, Kawachi I, Hendriks HFJ, Mukamal KJ. Bidirectional associations between alcohol consumption and health-related quality of life amongst young and middle-aged women. J Intern Med 2015, pre-publication. doi:10.1111/joim.12453.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 177: A clinical trial testing the effects of alcohol on inflammatory markers — 21 December 2015
While there have been many observational studies of the relation of alcohol consumption to health risks and benefits, the number of clinical trials of alcohol administration for its health effects are limited. The present paper is based on a controlled diet cross-over trial among 53 postmenopausal women. A standard diet was provided for a period of 6 months; two meals each weekday were consumed at the study facility and food was provided for other meals. To the standard meal, during three 8-week interventions, either 0, 15 g, of 30 g of alcohol (ethanol) were added to the daily diet, with the two doses of alcohol the equivalent of a little over one typical drink and 2 ½ typical drinks. Weight remained stable and no adverse effects were reported.
The key results of the trial were that, during periods when alcohol was consumed, there were small but significant decreases in markers of cellular adhesion molecules and components in the hemostatic pathway; these are indices of inflammation and the effects are consistent with a decreased risk of cardiovascular disease (CVD). Specifically, reductions were seen when alcohol was administered for s-ICAM, fibrinogen, and D-dimer, all of which would be expected to lower CVD risk. PAI-1 increased with alcohol, and there were no effects on CRP, Factor VIIc or IL-6.
While there were a number of question about the study, Forum members considered that, overall, this was a very well-done, difficult-to-carry-out study that shows alcohol’s beneficial effects on a number of inflammatory and hemostatic factors. The results are in line with many observational studies, although some previous intervention studies have found such effects only after the administration wine (but not of gin), suggesting a key effect of the polyphenols in wine. This study indicates that ethanol itself may have similar beneficial effects on mechanisms that relate to the development of cardiovascular disease.
Reference: Stote KS, Tracy RP, Taylor PR, Baer DJ. The effect of moderate alcohol consumption on biomarkers of inflammation and hemostatic factors in postmenopausal women. European J Clin Nutrition 2015; advance online publication. doi:10.1038/ejcn.2015.182
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 176: A New Report on Alcohol Consumption and Total Mortality Risk — 14 December 2015
Most observational studies have found that moderate drinkers, in comparison with nondrinkers, tend to have lower risk of all-cause (total) mortality; this is probably related primarily to a reduction in the risk of cardiovascular disease, the leading cause of death among the elderly. This large study has conflicting findings, as the author claims that the present analyses do not demonstrate protection against mortality from light-to-moderate drinking. In this study, what were termed “occasional drinkers,” rather than nondrinkers, were used as the comparison group.
Forum members had two main concerns about this study that warrant an investigation of the author’s conclusions: there was no consideration of under-reporting of alcohol intake when declaring “occasional drinkers” as the referent group, and (2) the inclusion, and adjusting for as “confounders,” several factors that are actually mechanisms by which alcohol has been shown to reduce mortality.
The first concern could have led to many light drinkers being included in the referent group, and thus not evaluated for a potential protective effect of light drinking on mortality. In fact, presented only in the Appendix to the paper are data showing that when nondrinkers make up the referent group, consumers of 1-7 as well as 7-14 drinks per week show significant 20-30% reductions in the risk of mortality; these findings are very similar to those of most previous epidemiologic studies.
The second, and perhaps more important concern, is that some of the mechanisms by which moderate alcohol intake may lead to lower mortality, such as reducing the risk of diabetes and coronary heart disease, were “adjusted” for in the analyses. This would attenuate or even erase any true reduction in risk of mortality from moderate drinking.
Some Forum members also were concerned that some subjects were missing data on alcohol consumption but, rather than excluding them, an estimated value was imputed for them. Further, data on the pattern of drinking (regular moderate versus binge drinking) or on the type of beverage consumed were not included in the evaluation.
Forum members conclude that the results of this study will obviously be considered in conjunction with other scientific data when seeking to judge the relation of alcohol intake to mortality. However, concerns about the analysis raise questions about the conclusion of the author of no protective effect of alcohol on mortality, a finding that conflicts with the results of most previous studies.
Reference: Goulden R. Moderate Alcohol Consumption Is Not Associated with Reduced All-cause Mortality. Am J Med 2015; pre-publication. http://dx.doi.org/10.1016/j.amjmed.2015.10.013.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 175: An update on the association of alcohol consumption with breast cancer: Effects of BMI — 24 November 2015
Most observational epidemiologic studies have shown a slight increase in the risk of breast cancer for women who consume alcohol; the degree of increase is usually small for light-to-moderate drinkers (between 5% and 15% increase for consumers of no more than one drink/day), but the risk may be higher for women consuming greater amounts of alcohol. However, there are a number of factors that affect this relationship, including the type of study (cohort or case-control), the pattern of drinking (regular versus binge), the type of beverage consumed, folate intake, use of hormone replacement therapy, as well as genetic factors. It has also been shown that the risk of breast cancer among obese women tends to be higher than among non-obese women, but there are limited data on how obesity interacts with alcohol in affecting the risk of breast cancer. It is clear that alcohol consumption cannot be evaluated in isolation, without considering other factors that relate to the development of breast cancer.
The present study is based on a large cohort of Swedish women who were examined as part of the Women’s Lifestyle and Health Study in 1991 – 1992, then followed through 2009 for the development of breast cancer: 1,385 cases were ascertained among the more than 45,000 women in the study. Alcohol was assessed at baseline and again at the follow-up examination, and the diagnosis of breast cancer was gleaned through linkage to the nationwide health registries in Sweden. Almost all of the women were pre-menopausal at baseline.
Forum members considered this to be a very well-done study, with almost complete ascertainment of cancer cases. There were some concerns, however, including the fact that the height and weight of subjects was not measured but self-reported, perhaps resulting in less accurate estimates of BMI. Further there may have been residual confounding from other factors related to breast cancer that were not assessed. Finally, the reported levels of alcohol consumption among the women in this study were very low (72% of the cohort drank either zero alcohol or below 5 g per day), but it cannot be determined if these are indeed the levels in this population or whether there may have been under-reporting of consumption.
The key findings as reported by the authors were that, overall, there was “no statistically significant association between alcohol intake and breast cancer risk after adjustment for confounders.” While this is indeed supported by their data, Forum members warned that readers should also note that there was an increase in risk found in less-obese women (BMI ≤ 25 kg/m2), among whom there was a step-wise increase in the risk ratio for cancer from 1.0, to 1.05, to 1.19, to 1.32 with increasing category of alcohol intake. This association was not seen in the more obese women for total cancer or for any of the sub-categories of cancer.
While the overall results did not show an increase in risk from alcohol intake, the results among non-obese women are similar to those seen in many other studies, and suggest a slight increase in the risk of breast cancer associated with alcohol for at least some women. The differences in effect according to BMI reported by the investigators are interesting and add to our understanding of the association of alcohol with breast cancer which, however, remains unclear.
Reference: Shin A, Sandin S, Lof M, Margolis KL, Kim K, Couto E, Adami HO, Weiderpass E. Alcohol consumption, body mass index and breast cancer risk by hormone receptor status: Women’ Lifestyle and Health Study. BMC Cancer 2015;15:881 (DOI 10.1186/s12885-015-1896-3)
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 174: Two-year clinical trial of wine administration in diabetics who were previous abstainers or very-light drinkers — 19 October 2015
Observational epidemiologic studies have consistently found that moderate drinkers are at lower risk of cardiovascular disease (CVD); such alcohol consumption also lowers both the risk of diabetes as well as of CVD among diabetics. However, there have been few clinical trials of the administration of alcohol or wine among diabetics, and most have been for relatively short periods of time. Forum members welcomed the publication of the results of the present study, and consider that it provides valuable information on the relation between wine and cardiometabolic risk.
In this study, among 224 subjects with diabetes aged 40 to 75 years who were abstainers or very light drinkers (previously reported none or < 1 drink/week), the investigators carried out a randomized clinical trial of the effects of wine on cardiometabolic factors. The subjects were randomly assigned to 150 mL of mineral water, white wine, or red wine with dinner for 2 years; all groups followed a Mediterranean diet without caloric restriction. The study was described to subjects as a dietary intervention, and there were group sessions led by clinical dietitians each month for the first three months and then at 3-monthly intervals thereafter. The focus was on the Mediterranean diet, and wine was not discussed at these meetings. There was excellent compliance with the provided beverages (>80%) and excellent continued participation of subjects (94% for one year and 87% for the full two years).
The key results of this study were that the administration of 150 ml of red wine with dinner each evening, in comparison with mineral water, favorably affected many cardiometabolic factors, and especially led to an increase in HDL-cholesterol and apolipoprotein (a). The administration of similar amounts of white wine was also beneficial, and specifically improved measures of glycemic control.
Further, in 203 of the subjects, effects according to the genetic factors determining ADH were evaluated. In the study, 35.6% of subjects were homozygous for the polymorphism for “slow ethanol metabolism,” 21.3% were homozygous for that for “fast ethanol metabolism,” and 43% were heterozygous. Forum members agreed with the summary statement of the authors: “We found that diabetic patients who were slow alcohol metabolizers had improved glycemic control by initiating moderate wine consumption, which suggests that alcohol may play a role in glucose metabolism. In contrast, diabetic patients who were fast ethanol metabolizers benefited the most from the wine-induced BP-lowering effect, which suggests a mediatory role for ethanol metabolites.”
The study has important implications for advice to be given to diabetics. Most, but not all, Forum members agreed with the authors’ conclusion that “Initiating moderate wine intake, especially red wine, among well-controlled diabetics as part of a healthy diet is apparently safe and modestly decreases cardiometabolic risk.”
Reference: Gepner Y, Golan R, Harman-Boehm I, . . . Stampfer MJ, Shai I, et al. Effects of initiating moderate alcohol intake on cardiometabolic risk in adults with type 2 diabetes. A 2-year randomized, controlled trial. Ann Intern Med 2015; pre-publication. doi:10.7326/M14-1650
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 173: A Large Study of the Association of Alcohol with the Risk of Acute Myocardial Infarction — 15 October 2015
This paper presents prospective data from a large population-based cohort from rural Norway, a region with typically light alcohol drinking and many abstainers who were not ex-heavy drinkers. It relates reported alcohol intake, assessed on two occasions, with the risk of developing an acute myocardial infarction (AMI). Its key findings are that, even in this very light-drinking population, drinkers had significantly lower risk (about 20% to 30%) of developing a MI than non-drinkers. As the authors conclude: “Light-to-moderate alcohol consumption was linearly associated with a decreased risk of AMI in a population in which abstaining from alcohol is not socially stigmatized. Our results suggest that frequent alcohol consumption is most cardioprotective and that this association is not driven by misclassification of former drinkers.”
As this was a rather homogeneous rural cohort without huge differences among subjects in socioeconomic status, it allows much better control of confounding. The fact that these results show essentially a continuous inverse association (rather than the usually seen “J-shaped” curve) is not unexpected given the very few heavy drinking subjects in this cohort. In addition to cardiovascular disease, the investigators also reported effects on total mortality, which showed a “J-shaped” curve.
Forum members considered this to be a very well-done study, and supports almost all previous research showing a protective effect of moderate drinking on the risk of coronary heart disease. The authors had good data on alcohol exposure and the occurrence of AMI. A key result from this study is that frequent light drinking, even less than an average of one drink/day, is associated with a significant decrease in the risk of coronary heart disease. Based on this study and most previous research, the clear message to the public remains: if you have no contraindications to alcohol use and decide to consume an alcoholic beverage, the healthiest approach is to drink frequently but in small amounts.
Reference: Gémes K, Janszky I, Laugsand LE, Lászlo KD, Ahnve S, Vatten LJ, Mukamal KJ. Alcohol consumption is associated with a lower incidence of acute myocardial infarction: results from a large prospective population-based study in Norway. J Intern Med 2015; doi: 10.1111/joim.12428.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===========================================================================================================
Critique 172: Alcohol and the risk of developing diabetes — 7 October 2015
Prospective cohort studies for decades have tended to show that the risk of developing Type II diabetes mellitus is reduced among moderate drinkers in comparison with non-drinkers, with previous meta-analyses suggesting that moderate drinkers may have about 30% lower risk than that of abstainers. The present study carried out a multi-language search for studies on alcohol and diabetes and conducted a meta-analysis involving almost two million subjects from a final group of 38 cohort, case-cohort, case-control, or nested case-control studies. The main conclusions of the authors are that only females may show a significant inverse association between alcohol consumption and the risk of diabetes, and that previous studies may have overestimated the reduction in risk from moderate drinking.
Forum members had concerns about the analyses and the conclusions of the authors, as the males in the study were primarily Asian (86%), and there were huge differences between the associations with alcohol for Asian and non-Asian populations. There are always problems when the basic study data have a marked degree of heterogeneity. In general, many of the factors that relate to diabetes (diet, body size and adiposity, type of beverages consumed, etc.) are quite different between Asians and non-Asians; combining such groups when their analyses show opposite effects of alcohol on diabetes risk may not be a reasonable way of trying to develop results that apply globally. Forum members do not believe that the analyses presented in this paper can support the conclusion of the authors that there is “no effect among males.” It could be unwise if the results of this study were used to develop alcohol guidelines for western populations.
The authors could not take the pattern of drinking (regular versus binge) or the type of alcohol into consideration. Clinical trials have suggested that wine and its polyphenols may have effects above and beyond those seen with alcohol alone, and beneficial effects of such polyphenols have been demonstrated both for women and for men. Thus, while the analyses in this paper were all carried out accurately, attempting to use these data to develop guidelines that would apply globally, as was done by the authors, may not be appropriate.
Reference: Knott C, Bell S, Britton A. Alcohol Consumption and the Risk of Type 2 Diabetes: A Systematic Review and Dose-Response Meta-analysis of More Than 1.9 Million Individuals From 38 Observational Studies. Diabetes Care 2015;38:1804–1812 | DOI: 10.2337/dc15-0710
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 171: A global assessment of alcohol and health — 29 September 2015
The present publication is from the very large Prospective Urban Rural Epidemiological (PURE) study that focuses especially on middle-income and lower-income countries, for which previous data on the association of alcohol consumption with health outcomes are sparse. Included in this analysis are data from high-income countries (HICs: Sweden and Canada); upper-middle-income countries (UMICs: Argentina, Brazil, Chile, Poland, South Africa and Turkey); lower-middle-income countries (LMICs: China and Columbia); and low-income countries (LICs: India and Zimbabwe). The large majority of the subjects were from lower income countries.
It has long been recognized that, when evaluating the health effects of drinking, it is especially important to evaluate alcohol intake within a particular population, with its specific genetic, lifestyle, environmental, and cultural factors, and not study alcohol in isolation. While the PURE study is a very well-done study, Forum members were concerned that the authors have attempted to answer overall questions about alcohol and health by combining data from such diverse populations. For example, the issue of very different causes of mortality in different populations would lead to very different approaches to improving longevity. There are too many factors associated with health outcomes to attempt to determine the specific alcohol effects when considered in isolation.
The authors tried to adjust for confounders as far as that was possible, but one cannot exclude further confounding, especially as subjects from lower-income countries contained a much larger proportion of smokers than there were in higher-income countries. The authors also point at differences between countries not fully explained by drinking pattern (or other factors); this suggests that further confounding exists. Further, lumping all types of stroke into one category may be hiding associations, especially as lower-income countries might have a higher frequency of cerebral hemorrhages. Similarly, using a single grouping for all cancers may be inadequate. Other limitations of this study include the short duration of follow-up time (4.3 years) and the low number of cases of each outcome.
The Forum concluded that even though the study includes information from many countries, it is not possible from such data to determine net health effects of alcohol consumption that are applicable to people everywhere. Their analytic results cannot be used, as the authors suggest, to “support global health strategies,” although they may surely be useful for developing “national initiatives to reduce harmful alcohol use,” especially for lower-income countries.
Reference: Smyth A, Teo KK, Rangarajan S, O’Donnell M, Zhang X, Rana P, Leong DP, et al. Alcohol consumption and cardiovascular disease, cancer, injury, admission to hospital, and mortality: a prospective cohort study. Lancet 2015. Pre-publication. http://dx.doi.org/10.1016/ S0140-6736(15)00235-4. Online/Comment http://dx.doi.org/10.1016/ S0140-6736(15)00236-6.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 170: An update on the association of alcohol consumption with the risk of cancer — 1 September 2015
This well-done analysis based on data from two very large cohort studies, the Nurses’ Health Study and the Health Professionals’ Follow-up Study, evaluated the association of alcohol consumption over many years with the risk of cancer. The authors conclude that men reporting an average intake of more than 15 grams of alcohol per day, but not less, have a significant increase in risk of alcohol-related cancers. In women, however, even the consumption of an average of 5.0 – 14.9 grams of alcohol per day (the equivalent of between ½ and 1 ½ typical drinks) was associated with a slight increase in total cancer risk, stated to be primarily from an increase in the risk of breast cancer. For both genders, there seemed to be a dose-response increase in risk of cancer with larger amounts of alcohol. At the same time, smoking was identified as an even more important risk factor than alcohol for these cancers.
Forum members considered this to be an important study presenting data that are of relevance to individuals and agencies providing advice regarding alcohol consumption. There is little question that heavy drinking markedly increases the risk of upper aero-digestive cancers, and no physician or agency advises people to consume in excess of the typical limits of no more than one or two drinks/day. Hence the finding in this study of an increase in some cancers among women (especially breast cancer) even for lighter drinking has implications for alcohol policy.
The Forum was disappointed that all dietary and other lifestyle factors that have been shown to increase the risk of cancer (data that are known to be available to these investigators) were not included in their report. Members were especially concerned that the net effects on health and mortality of light-to-moderate alcohol consumption were not commented upon in the paper. Given that the risk of the most common causes of death, especially cardiovascular diseases, are reduced by moderate drinking, it seems that the authors should have included data, or at least mentioned, the effects of alcohol on cancer mortality and, especially, on total mortality. It has recently been emphasized that cohort studies that report on only one outcome (in this case, cancer) but do not mention other outcomes that are affected by the same exposure, especially total mortality, do not present the full picture, and can lead to biased recommendations. The inclusion of such information from these cohorts could provide even more valuable data upon which to develop appropriate guidelines for alcohol use by individual patients and the public.
Reference: Cao Y, Willett WC, Rimm EB, Stampfer MJ, Giovannucci EL. Light to moderate intake of alcohol, drinking patterns, and risk of cancer: results from two prospective US cohort studies. BMJ 2015;351:h4238; doi: 10.1136/bmj.h4238
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 169: Effects of IQ on risk of morbidity and mortality related to alcohol consumption — 25 August 2015
The present paper is based on a large cohort of subjects in Sweden who had IQ tests as children (when they were 13 years old) and were then followed for more than 30 years. The study reports an inverse association between childhood IQ and hospitalization for alcohol-related diseases or death. The association is strongly dose-dependent, with a marked increase in disease/mortality risk for each decrease in the childhood IQ score.
A key finding in this analysis is that the attained socio-economic status (SES) of the subjects at age 32 played a large role in explaining the association between IQ and alcohol-related disease and appeared to completely explain the association with death from alcohol-related causes. This suggests that much of the effect of IQ during childhood may be through its effect on later education, occupation, and income of the subjects, associations that have been noted in many previous epidemiologic studies to favor better health. It is reassuring that being born into a poor, uneducated family is not as important as a determinant of adverse effects of alcohol later in life as is the attained socio-economic status of the individual in young adulthood.
A possible explanation for the inverse relation of SES in young adulthood with adverse alcohol outcomes could relate to the type of beverage consumed, which was not evaluated in the present analysis. In a previous study from Denmark, it was shown that higher SES in young adults was associated with a strong preference for wine rather than for other types of alcoholic beverage. Wine consumption has been associated with better health in numerous studies, although it is unclear whether this is due primarily to the non-alcoholic constituents in wine or to confounding from associated lifestyle factors of wine drinkers.
Forum members agree with the authors that the underlying causes for an association between IQ (or SES) and adverse alcohol-related disease and death are not clearly defined. It could be that intelligence has effects on health through choices in lifestyle behavior or socioeconomic environment as an adult, or the relationship between intelligence and health is confounded by other factors such as biological or socioeconomic conditions early in life. As for now, we can only describe the association, but not explain it fully.
Reference: Sjölund S, Hemmingsson T, Gustafsson JE, Allebeck P. IQ and alcohol-related morbidity and mortality among Swedish men and women: the importance of socioeconomic position. Journal of Epidemiology and Community Health 2015;69:858-864.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 168: Effects of alcohol on blood pressure in women: A randomized trial — 5 August 2015
The present paper describes the effects among 24 normotensive pre-menopausal women, all of whom were regular drinkers (of an average of 2 to 3 drinks/day), of the administration of two levels of alcohol in the form of red wine in a randomized clinical trial. Subjects were given low amounts of wine and higher amounts of wine during two 4-week intervention periods, with the effects on blood pressure compared with changes when subjects were given similar amounts of dealcoholized red wine. Subjects were divided into a “lower level” usual intake group who previously consumed < 200 g/week of alcohol and a “higher level” group who previously consumed >200 g/week.
Previous “lower level” drinkers were given two levels of alcohol, in the form of 100 ml/day of red wine on 4 days per week (an average of 46 g/week of alcohol, or the equivalent of about ½ typical drink per day) and 200 ml/day of red wine daily (about 146 g/week of alcohol, the equivalent of about 1 ½ to 2 typical drinks/day) for another 4-week period. Subjects who were previous “higher level” drinkers were given 100 ml of red wine daily (about 73 g/d of alcohol per week, the equivalent of about one typical drink/day) for 4 weeks and 300 ml/d of red wine (about 218 g/week of alcohol, the equivalent of about 2 to 3 typical drinks/day) for another 4 weeks.
The main results are a small but significant increase in 24-hour average blood pressure (+2.0 mmHg systolic and +1.3 mmHg diastolic) with higher levels of red wine but no significant effects (+0.4 mmHg systolic, -0.3 mmHg diastolic) from lower levels of red wine administration, when compared with blood pressure levels during periods when dealcoholized red wine was given. The differences were predominantly due to slightly higher awake rather than asleep blood pressures. These findings are similar to results of a limited number of randomized controlled trials of alcohol in men.
Forum members considered this to be a well-conducted clinical trial, with important results. There were, however, some concern that the study focused only on regular drinkers; results may have been different if previous abstainers had also been studied. Further, while the slight increase in blood pressure from higher levels of alcohol support previous research, the finding of no significant findings for lower levels of intake (when subjects were given the equivalent of between ½ and 1 drink/day) may not support what the authors suggest: “Our results provide no support for the concept that regular low-level alcohol intake can lower BP, suggesting that the J-shaped relationship between alcohol and BP in several studies is more likely because of the presence of unmeasured confounders.” Forum members considered their results to be consistent with either a slight increase or a slight decrease in blood pressure among such drinkers and are not necessarily inconsistent with data from some previous cohort studies that showed a “J-shaped” relation between alcohol and blood pressure.
A number of Forum reviewers also raised the question as to whether or not the results of a 4-week intervention study can be extended to the effects of the regular intake of alcohol for many years. Further, the fact that the study group included previous drinkers of up to similar amounts of alcohol as given during the higher intervention (yet were still normotensive) might suggest that their blood pressure was not “sensitive” to alcohol, and could limit the applicability of these results to the general public. Nevertheless, this intervention study provides important trial data on the short-term effects of alcohol on blood pressure.
Reference: Mori TA, Burke V, Beilin LJ, Puddey IB. Randomized Controlled Intervention of the Effects of Alcohol on Blood Pressure in Premenopausal Women. Hypertension 2015;66:00-00. DOI: 10.1161/HYPERTENSIONAHA. 115.05773
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 167: What determines a person’s belief that “alcohol is heart-healthy?” — 22 July 2015
This paper, based on data from more than 5,000 adults participating in an internet-based survey, sought to determine what were the perceptions of subjects on the relation of alcohol to heart disease, and how these perceptions resulted in particular behaviors related to alcohol consumption. Partricipants for the survey were recruited by a variety of methods, including announcements “in the lay press, promotional events, word of mouth, social media, e-mail, and clinic visits.” While the goal of the study is commendable, the results of any such survey obviously depend on many social and cultural factors of the people who respond to the survey; it was not a random sample of the population used in this analysis. This is critical because an interpretation of the data requires an understanding of the population surveyed.
Forum members had other concerns about this paper, including the specific survey questions regarding the perceptions of alcohol effects. For example, the key question asked in the survey was “Do you believe alcohol is good for your heart?” Forum members pointed out that it is obvious to nearly everyone that this cannot be answered without quantifying the amount of alcohol or the pattern of drinking. They consisdered that a more appropriate quesiton might be something such as “Do you believe that the moderate consumption of alcoholic beverages can benefit your heart?”
The authors make statements such as “Participants perceiving alcohol as heart healthy consumed 47% more alcohol.” This may sound alarming until it is revealed that the observed difference was from a baseline of 0-3 to 1-5 glasses of wine/week and from 1-7 to 2-8 total drinks/week. These higher amounts are not ‘alarming’ at all, and in fact fall within usual guidelines for “sensible drinking.”
Forum members were particularly upset that the authors misquote a number of scientific papers to support their claim that even low levels of drinking increase the risk of certain diseases. The authors also use such misrepresentations of data to justify their concerns that current guidelines for alcohol consumption may not be appropriate. Forum reviewers found it especially disturbing that the peer review process by the journal failed to uncover such misrepresentations of data.
The authors repeatedly give the impression that they are against any amount of alcohol consumption. They do not comment on the consistent findings in almost all well-done prospective studies indicating that moderate drinkers live longer than abstainers. Further, statements by the authors that suggest that people who think that alcohol is heart healthy are misinformed does not stand up to scientific data, which indicate that moderate and responsible drinking is associated wtith better health and longevity.
It is interesting that the report indicates that older, higher-income, and more highly educated subjects are more likely to consider alcohol to be heart healthy than younger and less-educated subjects. While a question was asked by the investigators as to whether or not the responder’s perception of the health effects of alcohol influences their decision to drink or to not drink, the specific responses to this question are not presented in the paper. It remains unclear to what extent beliefs about alcohol’s potential health effects relate to alcohol use or, more importantly, to alcohol abuse.
Overall, Forum members thought that the idea behind this study was of interest, but emphasized that it is important to collect data based on a random and well described sample of the population if one is to provide significant and understandable results. Further, the report is compromised by what appears to be a deliberate misrepresentation of the prior scientific literature to support the authors’ contention that alcohol is not healthy; there are a number of obvious errors that should have been detected during the review process by the journal. In the opinion of the Forum, the most reliable result from these analyses relates to where people obtain their information regarding alcohol and health: it does not come from physicians or scientific publications, but primarily from the lay press.
Reference: Whitman IR, Pletcher MJ, Vittinghoff E, Imburgia KE, Maguire C, Bettencourt L, Sinha T, Parsnick T, Tison GH, Mulvanny CG, Olgin JE, Marcus GM. Perceptions, Information Sources, and Behavior Regarding Alcohol and Heart Health. Am J Cardiol 2015; pre-publication. http:// dx.doi.org./10-1016/j.amjcard/2015.05-029.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 166: The association between alcohol consumption and suicidal ideation and suicidal attempt — 1 July 2015
The present study evaluates the relation of alcohol consumption and the pattern of drinking with self-reports of suicidal ideation and suicidal attempts among more than 43,000 men and women in Korea, using data from a 2007-2011 survey. Overall, 11.3% of males and 21.2% of females reported that they had experienced suicidal ideation, and 0.8% of males and 1.1% of females had attempted suicide. High scores on the Alcohol Use Disorders Identification Test (AUDIT) and a history of alcoholic blackouts were associated with suicidal ideation among both men and women and, for males, with suicidal attempts.
There is little known about the epidemiology of suicidal tendencies, or the specific causes of suicide. It is generally agreed that depression is the most important risk factor for suicide, and depression can lead to alcohol abuse; however, alcohol abuse can also lead to depression. Unfortunately, with cross-sectional data, analyses such as those in this paper cannot sort out the confounding issues nor, more importantly, address the causality of alcohol consumption with suicidal tendencies. The egg and hen question has never been solved – whether the depression or the heavy drinking came first. Thus, whether alcohol abuse increases the risk of depression (that may lead to suicide) or whether depressed people turn to alcohol seeking relief, cannot be determined from analyses such as these. However, it is also noted that this study suggests that drinking alcohol according to the usual guidelines for “sensible drinking” (generally, advising no more than 1 to 2 drinks/day) is not associated with the risk of suicidal ideation or attempt.
Forum members also commented on the large differences between populations in suicidal tendencies, being much higher in Korea and Japan than in most of Europe and North America. This could limit the applicability of the conclusions of this study to western populations.
Reference: Bae H-C, Hong S, Jang S-I, Lee K-S, Park F-C. Patterns of Alcohol Consumption and Suicidal Behavior: Findings From the Fourth and Fifth Korea National Health and Nutritional Examination Survey (2007–2011). J Prev Med Public Health 2015;48:142-150 • http://dx.doi.org/10.3961/jpmph.14.027
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 165: Fiber intake may modify the association of alcohol consumption with certain hormone-dependent cancers — 4 June 2015
The positive association between alcohol intake and certain hormone-dependent cancers (especially breast cancer) noted in many studies has been attributed to an effect of alcohol through an increase in levels of estrogen and other hormones. The present study had extensive dietary data on more than 5,000 men and women in France, among whom comparisons were made between the sex-specific tertile of alcohol intake and the risk of hormone-related cancers (breast, prostate, ovarian, endometrial, and testicular).
The study found that, overall, the risk of some cancers (e.g., breast) but not others (e.g., prostate) were positively related to reported alcohol intake. The key results reported by the authors are that when the risks of cancer were related to alcohol while adjusting for fiber intake, subjects whose fiber intake was below the median value showed higher risks of cancer related to alcohol, but not subjects with higher fiber intake. For example, when the risk of breast cancer in women was related to the tertile of their alcohol intake, the 2nd tertile showed a HR of 1.55 (1.01 – 2.38) and the 3rd tertile (HR 1.70, CI 1.11 – 2.61), when compared with women in the lowest tertile.
For prostate cancer in men, however, the 2nd tertile showed a HR of 1.28 (CI 0.82 – 2.00) and the 3rd tertile a HR of 0.89 (CI 0.55 – 1.45). The interaction terms between alcohol intake and cancer were not significant for all hormone-dependent cancers or for breast cancer. Only the interaction term for prostate cancer reached statistical significance, but here the relationship between tertile of alcohol intake even among subjects with low dietary fiber did not show a clear dose-response relation.
Forum members had concerns about the large number of potential confounders in these analyses (e.g., different effects for different types of fiber, the intake of fiber being just a marker for folate intake or for other dietary or lifestyle factors), that made it difficult for the authors to reach firm conclusions. Unfortunately, the numbers of tumors for each of the sub-groups were often too small to give meaningful results. And there was no data on alcohol drinking pattern (regular moderate versus binge drinking) or type of beverage consumed. Thus, while this study indicates that alcohol intake may relate to certain hormone-dependent cancers, the analyses do not present a clear demonstration as to whether it is fiber intake or some other related factor that may modify the association.
Reference: Chhim A-S, Fassier P, Latino-Martel P, Druesne-Pecollo N, Zelek L, Duverger L, Hercberg S, Galan P, Deschasaux M, Touvier M. Prospective association between alcohol intake and hormone dependent cancer risk: modulation by dietary fiber intake. Amer J Clin Nutr 2015; pre-publication. Doi: 10.3945/ajcn.114.098418.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 164: Why are the harmful effects of alcohol consumption greater among people with low education and income? — 14 May 2015
Epidemiologists have noted for many years that one of the key factors that modifies the relation between alcohol intake and many diseases is the education, income, or other index of socio-economic status (SES) of subjects. While differences in drinking practices (regular moderate versus binge drinking), other more moderate lifestyle factors, better access to health care, etc., have been suggested as potential mechanisms, there has been little research directed at this relation.
The present study is a systematic review of published reports to investigate the relationship between SES and risk of mortality or morbidity for each alcohol-attributable condition and, where feasible, to explore alcohol consumption as a mediating or interacting variable in this relationship. It summarized data from 31 case-control or cohort studies, relating an overall measure of the effects of low SES (variously defined) to the risk of cancers related to alcohol, as well as to liver disease, hypertension, stroke, epilepsy, cardiac arrhythmias, and pancreatitis.
The key findings of the study demonstrate a tendency for greater risk for low-SES subjects than for high-SES subjects to develop a number of diseases that are associated with alcohol consumption. Specifically, the authors report higher and statistically significant increases in risk of head and neck cancer and of stroke associated with alcohol consumption among lower-SES subjects than among higher-SES subjects. There was a tendency for lower risk of breast cancer among lower-SES women, but differences were not significant when adjusted for known confounders. The authors suggest that some of the effects shown may relate to greater total amounts of alcohol consumption by lower-SES subjects, or due to their higher levels of smoking.
Forum members thought this was a valiant attempt of the authors to unravel what has been a mystery: why do people at lower levels of SES seem to have more adverse effects of alcohol consumption than subjects at higher levels of SES. Unfortunately, as the authors admit, current scientific data do not allow firm answers. Suggested theories for reasons why low-SES subjects may have more adverse effects from alcohol include (1) different drinking patterns, with more binge drinking, (2) clustering of poor lifestyle factors, and (3) less access to health care. In some studies, even though the reported total alcohol intake of low- and high-SES subjects may be similar, the latter seem more likely to drink moderate amounts of alcohol on a regular basis, while lower-SES subjects are more likely to binge drink on fewer days per week. However, other studies do not support such a finding. Further, there may be differences according to the type of alcoholic beverage consumed, which was not considered in this study.
Forum members pointed out that differences in factors other than drinking patterns probably contribute to the greater adverse effects among subjects with lower SES. One member suggested that lower SES affects susceptibility to many diseases, most likely due to effect modification of hitherto unrecognized factors. The Forum concluded that there are too many confounders to make a conclusion about this topic, and much more research will be needed to understand how socio-economic factors affect the risk of disease and may modify the relation between alcohol consumption and disease.
Reference: Jones L, Bates G, McCoy E, Bellis MA. Relationship between alcohol-attributable diseaseand socioeconomic status, and the role of alcohol consumption in this relationship: a systematic review and meta-analysis. BMC Public Health 2015;15:400. DOI 10.1186/s12889-015-1720-7.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 163: The association of alcohol consumption with the risk of developing heart failure — 5 May 2015
Two new papers have provided data on the association of alcohol consumption with the risk of developing heart failure (HF). The first is a meta-analysis by Larsson et al that is based on eight prospective studies, with more than 200,000 subjects and 6,211 cases of HF. Meta-analyses provide important information because they are usually based on very large numbers of subjects and cases, and can detect smaller increases in risk than seen in individual studies. However, single large prospective cohort studies tend to provide more detailed information on, and allow better adjustment for, potential confounders. The second paper discussed in this critique by Dorans et al, is based on 33,760 men who were followed for 14 years, with almost 3,000 cases of fatal or non-fatal HF.
There was a high degree of consistency between these two studies: both concluded that moderate alcohol consumption, in comparison with non-drinking, is associated with a lower risk of developing HF. The meta-analysis (Larsson et al) concluded that there was a dose-response association between alcohol and HF; for example, a reduced risks of HF for consumers of 3 and 10 drinks/week (a 10% and 17% decreased risk, respectively), but not for those reporting the consumption of 21 drinks/week (a RR of 1.07; 95% CI 0.77 – 1.48). In the report from the single large Swedish prospective study (Dorans et al), the risk of HF for most categories of drinkers tended to be lower than that of never drinkers, with the lowest risk among consumers of 7 – 14 drinks/week (HR=0.81, 95% CI 0.69 – 0.96).
Forum members considered both of these studies to have been very well done, and the similar results not unexpected. HF has many causes, but in developed countries the most common is coronary artery disease (CAD), and moderate drinking has long been known to be associated with a lower risk of developing CAD. In their critique, Forum members discuss other conditions that relate to the development of HF, including conditions (such as respiratory infection, excessive salt intake, non-compliance with prescribed medication, etc.) that may trigger an attack of symptomatic HF.
To summarize, based on previous research and these two excellent papers, current data suggest that the moderate intake of an alcoholic beverage lowers the risk of the development of symptomatic HF. This undoubtedly relates, as least to some extent, to the demonstrated protection of alcoholic beverages against CAD. As for giving advice regarding the consumption of alcohol, Forum members agree with the conclusions stated by Klatsky in his editorial accompanying one of the papers: “All persons should avoid heavy drinking and many persons should avoid all alcohol. However, it is the author’s opinion that many middle-aged and older persons at risk of CAD or HF should be told that he or she is better off as a light to moderate drinker. Dispassionate objectivity plus common sense should dictate advice about drinking.”
References:
- Larsson SC, Orsini N, Wolk A. Alcohol consumption and risk of heart failure: a dose–response meta-analysis of prospective studies. European Journal of Heart Failure 2015;17:367–373. doi:10.1002/ejhf.228
- Dorans KS, Mostofsky E, Levitan EB, Håkansson N, Wolk A, Mittleman MA. Alcohol and Incident Heart Failure Among Middle-Aged and Elderly Men: The Cohort of Swedish Men. Circulation Heart Failure 2015; pre-publication. DOI:10.1161/CIRCHEARTFAILURE.114.001787.
For the full critique of these papers, and general comments on the association of alcohol with heart failure, by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 162: What is the association between alcohol consumption and cancer? 13 April 2015
Three major papers on the association of alcohol consumption and cancer have recently been published. Forum members considered that all were well-done, and presented valuable new information on the topic. While the key findings in each study are similar, each brings specific information on how alcohol relates to the risk of developing cancer. In this critique, we present the authors’ abstracts of each paper, our comments on the paper, and then an overall discussion of the topic.
Problems can occur when combing case-control studies with prospective cohort studies, as was done in one of the papers reviewed, as risk estimates are usually higher in the former type of study and potential confounding may be less complete. Further, it is especially important to consider the interaction between alcohol consumption and smoking for upper aero-digestive tract cancer, as was not always done. And none of the studies covered in this critique emphasized the net effects of alcohol that, because of protective effects against cardiovascular disease, is almost always associated with lower total mortality among moderate drinkers than among abstainers.
In summary, the Forum considers that the three papers reviewed provide important data on one of very few lifestyle factors that have been shown to relate to the risk of cancer. And cumulative research data clearly show that heavy alcohol intake increases the risk of upper aero-digestive tract cancers and some other cancers. Further, in these and many previous reports, even light alcohol consumption was associated with an increase in risk of breast cancer in women. Unfortunately, the threshold level of drinking associated with an increase in risk is not clearly defined for most cancers.
Forum members agree with the conclusions of Klatsky et al, who stated: “At present, a possible increased cancer risk at moderate intake should enter into individual estimation of the overall risk-benefit equation for alcohol drinking, especially for young persons. For most persons older than age 50 years, the overall benefits of lighter drinking, especially the reduced risk of atherothrombotic disease, outweigh possible cancer risk.”
References:
-
-
-
- Klatsky AL, Li Y, Tran HN, Baer D, Udaltsova N, Armstrong MA, Friedman GD. Alcohol Intake, Beverage Choice, and Cancer: A Cohort Study in a Large Kaiser Permanente Population. Perm J 2015;19:March 1, 2015. http//dx.doi.org/10.7812/TPP/14-189
- Bagnardi V, Rota M, Botteri E, et al. Alcohol consumption and site-specific cancer risk: a comprehensive dose–response meta-analysis. British Journal of Cancer 2015;112:580–593. doi: 10.1038/bjc.2014.579
- Wienecke A, Barnes B, Neuhauser H, Kraywinkel K. Incident cancers attributable to alcohol consumption in Germany, 2010. Cancer Causes Control 2015;[Epub ahead of print].
-
-
For the full critique of these papers, and general comments on alcohol and cancer, by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 161: The effects of alcohol consumption on the risk of hip fracture — 31 March 2015
Among elderly people, falls leading to hip fracture are a major health problem, leading to severe morbidity and mortality. Underlying factors that increase the risk of hip and other fractures include osteoporosis and low bone mineral density, as well as an unsteady gait making falls more common. The role that alcohol consumption among the elderly may relate to hip fracture has been a topic of concern for many decades, but data from a number of prospective studies now suggest that light-to-moderate drinking may actually decrease the risk of such fractures, while heavy drinking may increase the risk.
The present meta-analysis is based on prospective studies that have yielded more than 26,000 incidences of hip fracture. It concludes that there is a “J-shaped” association between alcohol consumption, especially of wine, and the risk of hip fractures, with lower risk for a reported consumption of about 1 drink/day, no effect from drinking between 1 and 4 to 5 drinks, and an increased risk from heavier drinking. Part of the “protection” from light drinking is apparently from the effects of alcohol on increasing bone mineral density.
Forum reviewers considered this to be a very well-done meta-analysis that provides balanced information on the risk of this common public health problem. Noting that the major differences seen in this study were between light drinkers and heavy drinkers, it was commented that there are many differences between people who are moderate in their habits, including moderate drinking, and people who usually consume more than 4 or 5 drinks/day; thus, there is still the possibility of other lifestyle factors confounding this association. Also, it was noted that most of the subjects in this analysis were North American or European, so applicability to other racial/ethnic groups may be limited.
In summary, this large and very well-done meta-analysis supports a protective effect of light alcohol consumption on the risk of hip fracture, with an increase in bone density from alcohol being a probable important factor. Data suggest that wine consumption may have the most favorable effect, perhaps indicating that polyphenols and other compounds may also play a role. The study shows that heavy drinking (an average of 4 to 5 or more drinks/day) is associated with an increase in the risk of hip fracture.
Reference: Zhang X, Yu Z, Yu M, Qu X. Alcohol consumption and hip fracture risk. Osteoporos Int 2015;26:531–542. DOI 10.1007/s00198-014-2879-y
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 160: Do the calories in alcoholic beverages lead to increased obesity? — 23 March 2015
Among people who consume alcohol, it would be assumed that the excess calories provided by the alcohol would add to their risk of obesity; however, current data suggest that the association may be more complex. It is unclear to what extent people who consume alcohol may modify other aspects of their diets, either decreasing or increasing other sources of calories. Further, alcohol is metabolized differently from other foods, which suggests that its calories may not be as readily available as those from fat, carbohydrate, and protein to increase obesity. The present paper provides an update on scientific data on the association between alcohol consumption and obesity. The overall conclusions of the authors are that light-to-moderate drinking does not increase the risk of obesity, while heavier drinking (or even moderate drinking among obese subjects) may lead to weight gain.
Forum reviewers appreciated the excellent summary of scientific reports on this topic, and thought that the authors gave a sound and balanced update on the topic. However, mechanisms why numerous prospective epidemiologic studies show that moderate drinking does not increase the risk of obesity are unclear. Given that alcohol contains calories, and if drinking alcohol does not displace the intake of other foods, it would be assumed that such calories would increase the risk of obesity unless there are particular metabolic differences between alcohol calories and those from protein, fat, and carbohydrate.
Potential mechanisms suggested have included a decreased utilization of calories from alcohol due to what is known as ‘Non-exercise Activity Thermogenesis’ (NEAT), in which the metabolism of alcohol may create more heat than fat. Also, the Forum discussion included comments that alcohol could bring into play effects on insulin, glucose, and fat mobilization (however, in the laboratory, such mechanisms tend to increase, rather than decrease, body fat). Also, a reasonable interpretation of the fat tissue decrease related to ‘moderate’ ethanol intake seen in many studies could be an associated decrease in the intake of carbohydrates. One glass of wine substituting for approximately 50 g of glucose could be a reasonable mechanism for shifting the metabolism from lipogenesis to oxidation of lipids. Genetic factors undoubtedly play a role in the effects among individuals.
In summary, this update on the association of alcohol consumption and obesity concludes that most well-done prospective studies show that moderate drinkers do not have an increase in obesity, and in some studies there is even a slight decrease in weight. One possibility is that, especially for wine with meals, satiety may occur earlier and result in less intake of food. However, precise mechanisms for a lack of increase in weight are not known, and the effect could still result from drinkers compensating for their drinks by taking in fewer calories from other sources and perhaps also by being a little more physically active.
Reference: Traversy G, Chaput JP. Alcohol Consumption and Obesity: An Update. Curr Obes Rep 2015;4:122–130. DOI 10.1007/s13679-014-0129-4
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
========================================================================
Critique 159: Alcohol as a component of the Mediterranean-type diet; effects on the risk of mortality among diabetics — 17 March 2015
Many scientists have reported on health benefits associated with the traditional diet of much of the Mediterranean area: the primary basis of the diet is on plant-based foods (whole grains, vegetables, fruits), olive oil, moderate wine consumption, and limited intake of meat or dairy products. In 2003, Antonia Trichopoulou and her associates created a scoring system based on the number of components of the Mediterranean Diet (Med-Diet) consumed by subjects, giving a total score to judge the degree that individuals were following a Med-Diet pattern. The score is based on the intake of 7 items (cereal intake, ratio of monounsaturated to saturated fats, vegetables, fruits, nuts, fish, and moderate alcohol), considered to have positive effects, and 2 items (dairy products, meat and meat products) considered to have negative effects. Many groups have found that greater adherence to such a diet (a higher score) is associated with a lower risk of many diseases, and lower mortality. There are limited data on the relative merits of each component of the Med-Diet. In the present paper, the authors attempt to judge the proportion of the protection against mortality that can be attributed to each component of the score.
The authors’ calculations estimated that, in descending order of importance, moderate alcohol consumption (associated with a reduction of 14.7% in the protection against mortality when it was removed from the total score), cereal intake (12.2% reduction), ratio of monounsaturated to saturated fats (5.8%), and consumption of vegetables (5.8%), fruits and nuts (5.2%) and fish (5.0%) lowered mortality risk. Lower intakes of dairy products (reduction of 13.4%) and meat and meat products (3.4%) were also associated with lower mortality. Alcohol has long been known to relate to a lower risk of developing diabetes, and the present study indicates that it is an important factor in reducing the risk of mortality among subjects who have already developed diabetes, as has been shown in previous studies. This study indicates further that the full Med-Diet has very favorable effects on mortality among diabetics.
Forum members considered this to be a well-done attempt to tease apart the relative importance of each component of the Med-Diet as it relates to health outcomes among diabetics. They felt that these researchers from the MOLI-SANI study have published a convincing paper extending the known benefits of the Mediterranean diet to a cohort of type 2 diabetics, a group of subjects at high risk for cardiovascular and all-cause mortality.
There were some questions raised about the precision of the Med-Diet Score, as published and used in this study, in judging the relative contributions of the different dietary constituents, especially because of known complexities in judging the effects of avoiding one particular food when its absence may affect the intake of other foods. And for alcohol, the score used did not permit an evaluation of the role of the pattern of drinking or even the type of beverage consumed, which are known to affect the net effects of drinking on health.
Nevertheless, the results of this study add to an accumulating base of knowledge of the importance of the Mediterranean-type diet in reducing the risk of many health outcomes, including mortality among diabetics.
Reference: Bonaccio M, Di Castelnuovo A, Costanzo S, Persichillo M, De Curtis A, Donati MB, de Gaetano G, Iacoviello L, on behalf of the MOLI-SANI StudyInvestigators.
Adherence to the traditional Mediterranean diet and mortality in subjects with diabetes. Prospective results from the MOLI-SANI study. European Journal of Preventive Cardiology 2015. Pre-publication. DOI: 10.1177/2047487315569409.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 158: Comments on Alcohol Recommendations included in the Scientific Report of the 2015 Dietary Guidelines Advisory Committee – 4 March 2015
Note: The 2015 Dietary Guidelines Advisory Committee (Committee) submitted the Scientific Report of the 2015 Dietary Guidelines Advisory Committee (Advisory Report) to the Secretaries of the U.S. Department of Health and Human Services (HHS) and the U.S. Department of Agriculture (USDA) in February 2015. The purpose of the Advisory Report is to inform the Federal government of current scientific evidence on topics related to diet, nutrition, and health. It provides the Federal government with a foundation for developing national nutrition policy. However, the Advisory Report is not the Dietary Guidelines for Americans policy or a draft of the policy. The Federal government will determine how it will use the information in the Advisory Report as the government develops the 2015 version of the Dietary Guidelines for Americans. HHS and USDA will jointly release the Dietary Guidelines for Americans, 2015 later this year.
Sections of the Advisory Committee report related to alcohol are copied in the full Forum critique, which is available at www.bu.edu/alcohol-forum/critique-158. The full Advisory Committee report can be assessed at the following address: http://www.health.gov/dietaryguidelines/2015-scientific-report/PDFs/Scientific-Report-of-the-2015-Dietary-Guidelines-Advisory-Committee.pdf.
Forum Comments
Members of the International Scientific Forum on Alcohol Research (the Forum) have reviewed the sections of the Advisory Committee’s report that relate to the consumption of alcohol. They consider the report to be well written and a very clear statement on alcohol and health, one that generally reflects current scientific data.
Some Forum members thought that for dietary guidelines, there should have been more emphasis on the inclusion of moderate alcohol consumption as part of a Mediterranean-type diet, which is described in the report as being associated with very favorable health outcomes. The Forum found it interesting that the health problems associated with alcohol receive extensive detailed notice, but substantial favorable effects are barely mentioned. For example, while the comments on the increase in the risk of breast cancer are warranted, there is no mention that moderate alcohol consumption provides substantial protection against ischemic cardiovascular events, despite consistent and extensive data showing that the latter issue has a major public health benefit. Also, lacking any explanatory statements, the public and health professionals may be confused as to the basis for the recommendation that alcohol is “an important component of a healthy lifestyle.” So we recommend that some explanations for the statement, based on the relevant scientific literature, should be included. (Further, the report does not describe the favorable effects of moderate drinking on sociability, stress reduction, and relaxation, which are key reasons why most people consume alcohol in the first place.)
Despite our concerns, given that this is a statement that must get approval by a large number of governmental agencies and a variety of interested parties, it is consistent with current epidemiological data as well as mechanistic studies. The Forum strongly agrees that current scientific evidence indicates that, for mature adults without contraindications to alcohol use, moderate alcohol consumption can be included as a component of a balanced and healthy lifestyle.
For the full critique of the report by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 157: A mistaken interpretation of data relating alcohol to mortality – 20 February 2015
The authors of this paper have carried out a regression analysis to examine the association of reported alcohol consumption with all-cause mortality, dividing their sample into different age groups. They used data from Health Survey for England 1998-2008, linked to national mortality registration data. Their published results show lower risk of mortality (hazard ratios < 1.0 for mortality in comparison with recent non-drinkers and with never drinkers) for subjects in essentially all categories of moderate drinking. However, the authors have interpreted their analyses as indicating that moderate drinking is not associated with all-cause mortality for the vast majority of the population.
Forum members, and many other scientists, have been surprised by the conclusions of the authors, who apparently did not consider basic statistical principles (such as dealing with type-2 errors) in judging their results. The investigators appear to have looked only at p-values and ignored the estimates of effect in their own data, coming to the conclusion of no association between moderate alcohol and total mortality for most age groups. Focusing only on significance testing for estimating effects has been strongly condemned by epidemiologists and statisticians and can lead to inaccurate results.
The paper reflects a gross misinterpretation of the data, not what would be expected in a publication in a leading journal. In other words, the authors’ conclusions are not backed up by their data. A more appropriate headline based on this paper would be “Study supports a moderate protective effect of alcohol against all-cause mortality.” Given the wide media coverage of this article, with striking headlines indicating that moderate drinking does not affect mortality, one Forum reviewer wondered “How can more than 30 years of research in this field be undone by one misguided paper in the BMJ? Once in a while I reflect on how some doctors and journalists interpret scientific papers; they seem to rely more on abstracts and press releases.”
The Forum considers that the conclusions of the authors of this paper are simply not supported by the data provided. Rather, their findings are in accordance with those from previous prospective studies showing that, for all age groups, moderate alcohol consumption is associated with a decrease in all-cause mortality risk.
Reference: Knott CS, Coombs N, Stamatakis E, Biddulph JP. All cause mortality and the case for age specific alcohol consumption guidelines: pooled analyses of up to 10 population based cohorts. BMJ 2015;350:h384 doi: 10.1136/bmj.h384.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 156: The pattern of alcohol consumption and risk of cirrhosis — 10 February 2015
This paper, from a group of experienced investigators in Denmark using data from a large population-based cohort, attempted to judge how drinking pattern affects the risk of a subject developing alcoholic cirrhosis. From a cohort study of 55,917 participants (aged 50–64 years), the authors calculated hazard ratios (HRs) for alcoholic cirrhosis in relation to drinking frequency, lifetime alcohol amount, and beverage type. A total of 342 subjects developed alcoholic cirrhosis. The authors concluded that, in men, daily drinking was associated with an increased risk of alcoholic cirrhosis as compared with less frequent consumption; they also concluded that wine consumption might be associated with a lower risk of alcoholic cirrhosis that associated with the consumption of beer or liquor.
The major concern of Forum reviewers regarding this paper was the use of a diagnosis of “alcoholic cirrhosis” to judge the effects of alcohol on the disease; this was considered a type of circular reasoning. A diagnosis of alcoholic cirrhosis generally requires a history of alcoholism or heavy drinking, and subjects given that diagnosis would essentially be limited to those who were heavy drinkers. Thus, it would be no surprise to find a history of heavy drinking when evaluating alcohol as an exposure.
There was also concern about the implications of the author regarding frequency of drinking. The authors’ described in detail the relation of drinking pattern to liver cirrhosis, differentiating, in particular, effects associated with drinking daily versus drinking on 4-5, or 6 days a week. However, Forum members were concerned that as the overall average amount of alcohol for the daily drinkers exceeded that of those drinking less frequently, it was difficult to know if it was primarily the frequency of drinking (as concluded by the authors) or the total amount of alcohol consumed by subjects. The authors stated that they wanted to “execute evidence-based counselling,” which of course is praiseworthy, but Forum members had difficulty understanding why the effect of drinking 5-6 days/week should differ much from 7 days/week, especially if the usual amount was moderate. Indeed, the investigators state: “The mean alcohol amounts for daily drinkers were somewhat higher compared to those drinking less frequently in each category of alcohol amount, making it difficult to detangle the effect of drinking frequency and alcohol amount.” Forum members noted that the authors conclude that “daily drinking” was associated with increased cirrhosis, but they do not state daily drinking of how many drinks, which would be especially important. The study did not provide reliable data that would support alcohol-free days during the week.
The referent group in this study was made up of subjects reporting < 0 to 14 drinks/week, which would consist of light-to-moderate drinkers, those considered to be “sensible drinkers” in most cultures. Hence, it is no surprise that as subjects reported greater amounts of alcohol in the study, the risk of alcoholic cirrhosis increased. No one advises people to drink more than sensible limits. Further, there was a much higher risk of of cirrhosis among “current abstainers” than in the referent group, undoubtedly indicating that the current abstainers group included many former heavy drinkers.
Overall, the Forum thought that this paper raises, but does not answer, a number of questions about the relation of alcohol to the risk of cirrhosis: (1) Is wine really less liver-toxic than beer or liquor? (2) Should we really tell everyone to have one day each week without wine being included with their meal, or on which to avoid any alcohol? (3) Why is daily drinking, rather than 5 or 6 days per week dangerous for men but tends to be even slightly protective in women regarding liver disease? Because of concerns due to problems with bias from the diagnostic approach, the probability of under-reporting of alcohol consumption, and the lack of biological plausibility, we will need further scientific data to answer these important questions.
Reference: Askgaard G, Grønbæk M, Kjær MS, Tjønneland A, Tolstrup JS. Alcohol drinking pattern and risk of alcoholic liver cirrhosis: A prospective cohort study. Pre-publication. J Hepatol (2015) http://dx.doi.org/10.1016/j.jhep.2014.12.005.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 155: The effects of alcohol consumption on the risk of developing heart failure — 27 January 2015
An analysis of data from the large Atherosclerosis Risk in Communities (ARIC) study evaluated the effects of alcohol consumption at baseline, and the cumulative average intake based on several later assessments during a 24 year follow-up period, on the risk of the development of heart failure (HF). The authors conclude: “In this community, alcohol consumption of up to 7 drinks/week at early-middle age is associated with lower risk for future HF, with a similar but less definite association in women than in men. These findings suggest that despite the dangers of heavy drinking, modest alcohol consumption in early-middle age may be associated with a lower risk for HF.” The authors reported further that the risk of total mortality was higher than that of abstainers for former drinkers and for the heaviest drinkers, but did not demonstrate a “J-shaped” curve for total mortality (i.e., a lower risk for moderate drinkers in comparison with abstainers).
Forum members considered this to be a well-done analysis, with findings for a lower risk of HF among light-to-moderate drinkers consistent with many earlier reports. They noted that these findings may be somewhat affected by the inability of the investigators to include data on the pattern of alcohol consumption (regular moderate intake versus periodic binge drinking of similar total amounts) to disease. It would be expected that the relations between alcohol intake and HF (as well as with total mortality) would be stronger for regular moderate drinkers than for those who consumed their alcohol in binges (even if the total weekly average intake was the same). This could be one reason why a “J-shaped” curve was not seen for the relation of alcohol intake to total mortality in this study.
While coronary artery disease (CAD) is known to be a major precursor of HF, it is not clear from the data presented if the alcohol-HF relation may have differed between subjects with and those without CAD. For the effects of current heavy drinking, the implications from this study are limited because of the small number of such drinkers in this cohort; this was especially the case for women. The authors do not discuss the potential effects on their results of under-reporting of alcohol intake among their subjects; other studies have suggested means for identifying such subjects and ways of adjusting for such.
This study adds support to other large studies, including one just released as a pre-publication (see Addendum), that suggest that moderate alcohol consumption may reduce the risk of the development of heart failure. Some of this putative protective effect surely relates to a decrease in the risk of coronary artery disease among moderate drinkers. Heavy alcohol intake, especially among alcoholics, may increase the risk of both heart disease and heart failure.
Reference: Gonḉalves A, Claggett B, Jhund PS, Rosamond W, Deswal A, Aguilar D, Shah AM, Cheng S, Solomon SD. Alcohol consumption and risk of heart failure: the Atherosclerosis Risk in Communities Study. European Heart Journal, 2015, pre-publication; doi:10.1093/eurheartj/ehu514.
Addendum
Following the preparation of this critique, the pre-publication version of another paper has appeared: Larsson SC, Orsini N, Wolk A. Alcohol consumption and risk of heart failure: a dose–response meta‐analysis of prospective studies. European Journal of Heart Failure 2015; January, 2015. 10.1002/ejhf.228. According to its abstract, this paper is based on “a meta-analysis that included eight prospective studies, with a total of 202,378 participants and 6,211 cases of HF.”
While the Forum has not yet had an opportunity for a careful review of this new paper, the authors’ conclusions appear to provide strong support for the paper by Gonḉalves et al. The authors of the Larsson et al paper conclude their abstract by stating that when carrying out a dose-response meta-analysis, they “observed a non-linear relationship between alcohol consumption and risk of HF. Compared with non-drinkers, the RRs (95% CI) across levels of alcohol consumption were 0.90 (0.84–0.96) for 3 drinks/week, 0.83 (0.73–0.95) for 7 drinks/week, 0.84 (0.72–0.98) for 10 drinks/week, 0.90 (0.73–1.10) for 14 drinks/week, and 1.07 (0.77–1.48) for 21 drinks/week. Alcohol consumption in moderation is associated with a reduced risk of HF.”
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 154: Effects of changes in alcohol consumption on risk of dementia among elderly women — 12 January 2015
A number of prospective studies have shown that moderate drinkers are at lower risk of developing dementia or cognitive impairment than abstainers or heavy drinkers; possible mechanisms of a putative beneficial effect could relate to a reduction in the risk of cerebral atherosclerosis, a direct effect on cognition through the release of acetylcholine in the hippocampus, the antioxidant effects of alcohol and polyphenols, or from the down-regulation of inducible nitric synthase and up-regulation of endothelial nitric oxide synthase.
The present study is based on 1,309 women who were aged 65 years or greater at the beginning of a 20-year follow up, during which they had at least two assessments of cognitive function. At baseline, 42.1% of the women reported that they were “light” drinkers (>0 – < 3 drinks/week, 13.8% reported “moderate” consumption (3-7 drinks/week), and 3.6% reported “heavy” consumption (> 7 drinks/week). By the 20th year of follow up, 17.5% of the previously normal women had developed dementia (by several standard tests, a previous diagnosis of dementia, or nursing home residence), and 22.7% had developed mild cognitive impairment (MCI). Thus, a total of 40.2% of the women had developed some degree of cognitive impairment.
In this paper, there was no suggestion that the small percentage of women (5%) who increased their intake changed their risk of cognitive impairment (fully adjusted OR=1.04, 95% CI 0.56, 1.95), when compared with women who did not change their intake or decreased it only slightly. However, for women who decreased their intake by > 0.5 drinks/week, the authors suggest that there was an increase in risk of cognitive impairment, with unadjusted results showing an OR of 1.34, 95% CI: 1.05-1.70. However, with full adjustment for confounders, the effect was attenuated: OR = 1.26, 95% CI 0.98, 1.61; p = 0.07.
Forum members noted that the reasons that some women changed their drinking habits could not be ascertained (as is usually the case in observational studies). Alzheimer’s dementia has a long prodromal period and latent pathology could precede/contribute to a decrease in drinking. They were also concerned about the lack of cognitive characterization of the cohort at baseline. Thus, Forum members had some difficulty in knowing how to interpret the finding of a lack of association of baseline drinking with risk of cognitive impairment 20 years later given that we are not told whether the groups defined on baseline drinking differed from each other in age or other health risk factors. For those who changed their intake, decreasing drinking by > 0.5 glasses/week may be very different for someone drinking > 7 drinks/week than in someone drinking < 1 drink/week. It would have been better if the authors somehow took baseline drinking into account when assessing effects of change in drinking.
There was also the concern that any observational study that relates the effects of changes in alcohol intake on the risk of a disease without somehow taking earlier drinking into account may give paradoxical results. (An example is the relation of obesity to cardiovascular disease; overall, there is an increase in risk for obese individuals but when changes in intake among older people are evaluated, the result is often no effect or even a protective effect: the “obesity paradox.”) The same has been shown for the relation of usual alcohol intake and changes in intake to other diseases.
Thus, while the analyses were done appropriately, Forum members had concerns about whether the findings presented in this paper justify the wisdom of the authors in stating in their conclusion that “Women in their ninth and tenth decade of life who decrease alcohol use may be at risk of cognitive impairment.” As one reviewer stated: “Knowing from other studies that light to moderate alcohol consumption is good for the heart and the head, I would not advise elderly people to stop drinking. However, the conclusions of the authors that this paper shows that decreasing alcohol consumption increases the risk of cognitive impairment in elderly women may be true, but are not justified because the design, analysis, and results of the study do not permit such a statement.”
Reference: Hoang TD, Byers AL, Barnes DE, Yaffe K. Alcohol Consumption Patterns and Cognitive Impairment in Older Women. Am J Geriatr Psychiatry 2014; 22:1663-1667.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 153: Moderate alcohol intake may lower the risk of developing diabetes among obese subjects — 11 December 2014
This case-control study compared the risk of having a high level of hemoglobin A1c, a measure of hyperglycemia, and of the waist/height ratio, a measure of obesity, according to reported alcohol consumption. Overall, subjects reporting an average alcohol intake between 22 and 44 g/day (the equivalent of between about 2 and 4 typical drinks) had lower levels of hemoglobin A1c and lower weight/height values. The author concludes: “The associations between obesity and hyperglycemia were weaker in light-to-moderate drinkers than in nondrinkers. Thus, light-to-moderate drinking may reduce the impact of obesity on the risk for diabetes.”
While Forum reviewers had some concerns about the first analytic approach given in the paper, they agreed that the second approach, in which specific levels of A1c were reported according to alcohol intake and measures of obesity, had merit. These latter data clearly indicate that hyperglycemia is affected both by obesity (which increases the risk) and alcohol intake (which decreases the risk); hyperglycemia is the leading factor associated with the development of diabetes mellitus.
A therapeutic implication of this study may be that obese subjects who are moderate drinkers should not be advised to stop their alcohol consumption. The results, along with a large amount of other research currently available, also suggest that obese subjects who do not drink and have no contraindications to alcohol consumption should be informed that consuming moderate amounts of alcohol may be associated with a reduction in their risk of developing diabetes.
Reference: Wakabayashi U. Light-to-Moderate Alcohol Drinking Reduces the Impact of Obesity on the Risk of Diabetes Mellitus. J Stud Alcohol Drugs 2014;75:1032–1038.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 152: Specific genetic factors modify the reduction in heart disease risk from alcohol consumption — 27 November 2014
It has long been known that genetic and other environmental factors modify the association between alcohol consumption and a variety of diseases, especially coronary heart disease (CHD). Foremost among these modifying factors are genes that affect alcohol metabolism, age (effects seen only in older individuals), and drinking patterns (regular moderate versus binge drinking). Also, certain cholesteryl ester transfer protein (CETP TaqIB) polymorphisms, that relate to HDL-cholesterol activity, may interact with alcohol consumption for their effects on the risk of CHD. In the present study, the investigators have carried out a population-based case-control study among subjects in southwest Sweden to determine if there was an interaction between CETP genotypes and alcohol consumption for its effects on the risk of CHD. The authors conclude that a significant reduction in the risk of CHD from moderate drinking was seen only among the 18.6% of their subjects who had a particular CETP polymorphism.
Forum members considered this to be an interesting paper, but had some questions about the selection of cases, as they included not only new cases of CHD but subjects “who had an exacerbation of previously diagnosed coronary heart disease;” this makes it somewhat difficult to compare their results with other papers. Further, despite a large number of potential “control” subjects from their base population, the controls chosen were considerably younger than the cases and had different medical histories. While they adjusted for some of these factors in their analysis, residual confounding remains possible.
The major concern of Forum members was the broad conclusion of the authors (that only a small proportion of the population will show any cardio-protective effects of moderate drinking) based on such a small number of subjects. For example, among their “intermediate” category of drinkers with the supposedly “protective” CETP polymorphism, there were only 13 cases of CHD. Further, a number of previous large studies have had quite conflicting results regarding the effects of CETP polymorphisms on the alcohol-CHD association. While this paper adds information on one (of many) factors that affect the association between alcohol consumption and CHD, larger studies in different populations will be needed to determine the overall importance of this particular genetic polymorphism.
Reference: Mehlig K, Strandhagen E, Svensson P-A, Rosengren A, Torén K, Thelle DS, Lissner L. CETP TaqIB genotype modifies the association between alcohol and coronary heart disease: The INTERGENE case-control study. Alcohol 2014;48:695e700.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 151: “Fetal alcohol syndromes” result from multiple maternal factors during pregnancy — 20 November 2014
Excessive maternal alcohol consumption during pregnancy (especially among women with alcohol dependency) is known to markedly increase the risk of the fetus showing a group of developmental disorders defined as fetal alcohol spectrum syndrome (FASD), with the most serious form being fetal alcohol syndrome (FAS). The present paper attempts to identify maternal risk factors for FASD and FAS, but the authors report that there were not enough data to carry out a formal meta-analysis. They do, however, describe important maternal risk factors that have been reported in the literature to relate to these syndromes. The more frequent maternal conditions related to the risk of FASD or FAS include older age of mother, lower educational level, family relatives who abuse alcohol, little prenatal care, and a more severe pattern of alcohol consumption in general and particularly during pregnancy. They emphasize that “FAS is a multifactorial condition, and it is potentiated by complex relationships among several factors, social and biological.”
Forum reviewers considered this to be a well-done analysis presenting important and balanced information on these syndromes. Forum members agreed that many genetic and environmental factors, in addition to heavy alcohol consumption, may contribute to the development of these syndromes (e.g., certain genetic polymorphisms, inadequate pre-natal care, poverty, low education, familial alcoholism, use of illicit drugs, etc.).
Given the permanent nature of many of the defects found in FASD and FAS, and limited therapeutic options, it is important that the focus should be on the prevention of these syndromes. If they are to be prevented, it will be necessary to intervene among high-risk women, either prior to or early during pregnancy. Better knowledge of all the factors involved will help facilitate interventions that may help prevent these serious conditions.
Reference: Esper LH, Furtado EF. Identifying maternal risk factors associated with Fetal Alcohol Spectrum Disorders: a systematic review. Eur Child Adolesc Psychiatry (2014) 23:877–889; DOI 10.1007/s00787-014-0603-2.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 150: A new meta-analysis on the relation of alcohol consumption to the risk of ischemic heart disease — 6 November 2014
This meta-analysis is from authors who in the past have tended to argue that the demonstrated inverse association between moderate alcohol consumption and ischemic heart disease (IHD) shown in most studies is due to confounding by other lifestyle factors. However, in this paper, they come to the conclusion (in their words): “Results from our quantitative meta-analysis showed that drinkers with average intake of < 30 g/day and no episodic heavy drinking had the lowest IHD risk (relative risk = 0.64, 95% confidence interval 0.53 to 0.71). Drinkers with episodic heavy drinking occasions had a risk similar to lifetime abstainers (relative risk = 1.12, 95% confidence interval 0.91 to 1.37).”
The conclusions of the authors thus not only support a “J-shaped” curve for alcohol consumption and IHD but provide additional support suggesting that the effect may be causal, i.e., related to the alcohol consumption and not to other associated lifestyle factors. They state: “For drinkers having one to two drinks per drinking day without episodic heavy drinking, there is substantial and consistent evidence from epidemiological and short-term experimental studies for a beneficial association with IHD risk when compared to lifetime abstainers. The alcohol-IHD relationship fulfills all criteria for a causal association proposed by Hill.”
It is clear from epidemiologic studies that moderate drinkers may exhibit moderation in other lifestyle factors (such as not smoking, eating a healthy diet, etc.). Indeed, there is aggregation of healthy lifestyle factors that must be considered when judging how a single factor (such as moderate drinking) relates to disease outcomes. This meta-analysis suggests that other lifestyle factors do not explain the lower risk of IHD found to occur among moderate drinkers. In fact, increasingly, moderate drinking is found to be an independent (and rather important) lifestyle factor that lowers the risk of cardiovascular disease, regardless of other factors. Such protection is not seen when drinking is more than moderate, defined in this paper as an average of 30 grams or more of alcohol per day, the equivalent of about 2 ½ to 3 typical drinks.
Reference: Roerecke M, Rehm J. Alcohol consumption, drinking patterns, and ischemic heart disease: a narrative review of meta-analyses and a systematic review and meta-analysis of the impact of heavy drinking occasions on risk for moderate drinkers. BMC Medicine 2014;12:182.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 149: The association of alcohol consumption with the risk of death from colorectal cancer — 28 October 2014
Data from prospective cohort studies on the association between alcohol consumption and the occurrence of colorectal cancer (CRC) are conflicting, with some suggesting an increase in risk while others failing to show such an effect. There are little data on the effects of alcohol consumption on the risk of mortality from CRC. The present study is based on a meta-analysis of data from nine cohort studies (with a total of more than two million subjects) to judge how the level of alcohol intake relates to CRC mortality. A total of almost 4,000 deaths from CRC were recorded. The conclusions of the authors are that the consumption of ≥ 50 grams of alcohol (about 4 typical drinks or more) per day increases the risk of death from CRC modestly [RR 1.21 (95% CI 1.01, 1.46)], but “light” drinking (≤ 12.5 g/day) or “moderate” drinking (12.6-49.9 g/day) do not increase the risk of CRC death. In fact, they state that their data support a “J-shaped” relation between alcohol intake and CRC mortality (i.e., a slight decrease in mortality associated with light drinking but an increased risk with heavier drinking).
Forum members considered this to be a well-done analysis. They noted the inability of the authors to evaluate differences in effect according to type of beverage consumed, the pattern of drinking, or the underlying folate levels of subject, all of which probably modify such a relation. The results are in line with earlier reports on alcohol and breast cancer, where alcohol appears to increase the incidence of the disease but does not increase mortality. For most diseases, including colorectal cancer, there may a J-shaped effect on mortality: a reduction in risk for light-to-moderate drinking but an increase with heavier drinking.
Overall, the present meta-analysis supports a finding of increased risk of death from colorectal cancer from heavy drinking. However, it shows rather convincingly that light to moderate amounts of alcohol do not increase the risk of death from this disease, probably because of the protective effects of moderate drinking on cardiovascular disease, a more common cause of mortality.
Reference: Cai S, Li Y, Ding Y, Chen K, Jin M. Alcohol drinking and the risk of colorectal cancer death: a meta-analysis. European Journal of Cancer Prevention 2014;23:532–539.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 148: Alcohol and liver cancer — 24 September 2014
Hepatic cirrhosis frequently precedes the development of liver cancer, and excessive alcohol consumption is known to be one cause of cirrhosis. The investigators in the present study carried out a meta-analysis to evaluate the association of alcohol consumption with liver cancer. They used data from 19 prospectively studied cohorts with a large total number of cases: 4,445 incident cases and 5,550 deaths from liver cancer.
The analysis from this large study indicates that liver cancer is related to heavier alcohol intake, but not to light-to-moderate drinking (with the latter defined in this study as < 3 typical drinks per day). The authors conclude: “This systematic review suggests a moderate detrimental role of consumption of 3 or more alcoholic drinks per day on liver cancer, and a lack of association with moderate drinking.”
Forum reviewers considered this to be a well-done analysis with appropriate statistical methodology. While the authors were unable to test the potential effects of pattern of drinking (regular moderate versus binge drinking), the type of beverage (wine or other beverages), or potential effects of obesity (with the latter being a key factor associated with the most common type of liver disease in the US, non-alcoholic fatty liver disease), the results of this study support most other research indicating that more than moderate drinking increases the risk of cirrhosis and liver cancer. However, the findings of no effect from what the authors considered “moderate” drinking (< 3 drinks/day, which exceeds the guidelines for most countries), also fits with another recent meta-analysis showing no increase in risk of liver cancer to be associated with light drinking.
There are many adverse health effects of heavy alcohol consumption. Liver cirrhosis, which frequently precedes the development of liver cancer, is one such potential outcome. On the other hand, this study suggests that moderate alcohol intake does not increase the risk of liver cancer.
Reference: F. Turati, C. Galeone, M. Rota, C. Pelucchi, E. Negri, V. Bagnardi, G. Corrao, P. Boffetta, C. La Vecchia. Alcohol and liver cancer: a systematic review and meta-analysis of prospective studies. Annals of Oncology 2014; advance publication; doi:10.1093/annonc/mdu020
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 147: Association of alcohol intake with different types of breast cancer — 11 September 2014
The present study was based on a large number of women participating in a clinical trial (enhanced screening for certain cancers versus routine care) focusing on prostate, lung, colorectal, and ovarian cancer. During a follow-up period averaging about 9 years, a total of 1,905 women were diagnosed with invasive breast cancer. The analyses showed that an increase in cancer risk was associated with alcohol intake for estrogen and progestin positive (ER+/PR+) tumors, but not for other histologic types of breast cancer. The increased risk was predominantly seen among PR+ cancers, as there was no evidence of an increase in risk from alcohol for women with ER+/PR- tumors. An association with the highest category of alcohol intake was noted for ductal (the most prominent type), lobular, and mixed ductal/lobular tumors, but a clear dose-response curve was not present. The authors conclude that alcohol consumption is not associated with all breast cancer subtypes, and that future research should include precise definition of subtypes of cancer.
Forum reviewers considered this to be a well-done analysis. There were some questions about the characteristics of the participants in the study that could affect generalizability of the results. For example, the cohort of women in this study were more highly educated, more likely to have a positive family history of breast cancer, to be smokers, and perhaps more obese that the general population. Of more concern, however, was the lack of ability to evaluate a number of other potential risk factors for breast cancer: folate levels and other dietary factors, the pattern of drinking (regular versus binge), potential changes in drinking after the baseline measurement, type of beverage, or the HER2 status of tumors. The finding in the paper of an increase in breast cancer risk, in comparison with non-drinkers, even for women reporting less than ½ drink per week (RR 1.15, CI 0.97, 1.39) and 0.5 – < 1 drink per week (RR 1.25, CI 1.03, 1.53), suggests that residual confounding must also be considered; it is unlikely that such small amounts of alcohol would have a physiological effect.
Overall, the present study shows a significant increase in the risk of breast cancer among women in a cancer prevention trial who, at baseline, indicated that they were consuming even less than 1 drink/week. The increase was exclusively in ER+/PR+ tumors, but not in ER+/PR- or ER-/PR- tumors.
In future research on this association, information on folate levels and drinking pattern, and especially on type of beverage consumed and on evidence of under-reporting of alcohol intake, will be important in better defining how alcohol consumption relates to the risk of breast cancer. While the results of this study are important in studying the etiology of breast cancer (as alcohol appears to relate only to hormone receptor positive tumors), the findings may not necessarily help individual women know how their alcohol consumption by itself may relate to their overall risk of the disease.
Reference: Falk RT, Maas P, Schairer C, Chatterjee N, Mabie JE, Cunningham C, Buys SS, Isaacs C, Ziegler RG. Alcohol and Risk of Breast Cancer in Postmenopausal Women: An Analysis of Etiological Heterogeneity by Multiple Tumor Characteristics. Am J Epidemiol 2014; advance access; DOI: 10.1093/aje/kwu189.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 146: Alcohol and the risk of abdominal aortic aneurysm — 4 September 2014
The large majority of prospective epidemiologic studies on the effects of alcohol consumption and the risk of coronary heart disease and stroke have shown a significant reduction in risk for moderate drinkers. There have been few studies relating alcohol intake to the development of abdominal aortic aneurysm (AAA), and results have been inconsistent. The present study is based on two very large population-based cohorts in Sweden that were followed prospectively for the clinical development of AAA (identified by radiography, surgical repair, or death resulting from rupture). There were more than 1,200 cases identified during a 14-year follow-up period. The results of this study suggest that moderate drinking is associated with a lower risk of AAA, with the beneficial effects primarily among consumers of beer or wine.
Forum reviewers were unanimous in considering this to be a well-done analysis, with unbiased estimates of effect of alcohol on the risk of aneurysm. The reduced risk of AAA among moderate drinkers was similar to that seen for common manifestations of atherosclerosis, especially coronary heart disease and ischemic stroke. Reviewers were uncertain why only consumers of wine and beer showed a beneficial effect, but not consumers of spirits: this could be explained by the polyphenols present in wine and beer that have been shown to be anti-inflammatory, anti-oxidant, and anti-platelet aggregation (all mechanisms that may relate to the development of AAA). However, residual confounding could also play a role.
It was noted that the percentage of the population with hypertension, probably the most important risk factor for AAA, was much lower than is common in most industrialized countries, but the degree to which this affected the results cannot be known. While alcohol is known to increase blood pressure, some large studies suggest that an increase occurs only with more than light-to-moderate drinking. Further, there were few very heavy drinkers (the highest category of alcohol was an average consumption of ≥1 drink/day among women and ≥2 drinks/day among men), so this study could not assess whether or not large amounts of alcohol might increase risk of AAA.
There have been a very limited number of studies on alcohol intake and aortic aneurysm. While this study suggests a slight decrease in occurrence of AAA with moderate wine and beer intake, it will be important for other large studies to evaluate this association. Additional studies on polyphenol intake and occurrence of AAA will also be useful.
Reference: Stackelberg O, Björck M, Larsson SC, Orsini N, Wolk A. Alcohol Consumption, Specific Alcoholic Beverages, and Abdominal Aortic Aneurysm. Circulation 2014;130:646-652.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 145: Alcohol consumption and brain structure on MRI scans — 25 August 2014
While numerous prospective epidemiologic studies have provided evidence that light-to-moderate amounts of alcohol reduce the risk of dementia and heavy drinking increases the risk, there are few studies on the effects of alcohol on brain structure assessed by magnetic resonance imaging (MRI). The present study is a cross-sectional evaluation between reported alcohol intake and MRI-assessed brain structure among 589 multi-ethnic community residents of New York. Total brain volume (TBV), white matter hyperintensity volume (WMHV), and presence of infarcts were derived from MRI scans when subjects were, on average, 80 years of age..
A key finding of this analysis is that, in comparison with non-drinkers, light-to-moderate alcohol intake (up to an average of 1 drink/day for women or 2 drinks/day for men, which was reported in 31% of their subjects) was associated with larger TBV (i.e., less brain atrophy). The effect was primarily among consumers of wine rather than of beer or liquor. Significant associations were not found for alcohol or for specific beverages for other measures of brain structure (WMHV or presence of infarcts).
Forum reviewers considered this to be an appropriate analysis that was able to consider many of the potential confounders of such an association. On the other hand, it was not a large study and was based on a cross-sectional analysis; thus it cannot be used to judge causation (e.g., it is possible that people with larger brains to begin with were more likely to consume wine or total alcohol, rather than their alcohol intake increasing their brain size).
Data from many previous studies have shown that moderate alcohol intake lowers the risk of developing clinical signs of cognitive decline and of dementia. Such a finding has led Forum members to be of the opinion that instructing the elderly to refrain from light-to-moderate amounts of alcohol may not be wise. Although prospective studies may show that the decrease in the risk ratio for dementia (comparing drinking with abstainers) tends to be less among the elderly than among middle-aged subjects, the absolute risk of dementia increases markedly with age. Thus, any intervention that lowers the risk of cognitive impairment will have a much greater impact in older people as compared with younger people.
Given the inconsistences in previous reports on the effects of alcohol on brain structure, we must conclude that while this study suggests that there might be a beneficial association between alcohol (especially wine intake) and brain size, such a relation is not definitive. An inverse relation between moderate drinking and clinical evidence of dementia, however, has received support from a large number of prospective epidemiologic studies; it may be a better association for us to use when advising the elderly regarding alcohol consumption.
Overall, scientific data indicate that, for elderly subjects without contraindications to alcohol, small amounts of wine or other alcoholic beverage consumed regularly may reduce the risk of dementia and other diseases of ageing. As stated by Michel de Montaigne many centuries ago: “ . . . drinking is the almost last pleasure that the years steal from us.”
Reference: Gu Y, Scarmeas N, Eaton Short E, Luchsinger JA, DeCarli C, Stern Y, Manly JJ, Schupf N, Mayeux R, Brickman AM. Alcohol intake and brain structure in a multiethnic elderly cohort. Clinical Nutrition 2014;33:662e667.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 144: Alcohol consumption and risk of endometrial cancer — 18 August 2014
Most epidemiologic studies have shown that moderate alcohol consumption does not increase the risk of uterine cancer, and some have suggested an inverse or J-shaped relation. In a new analysis from the Nurses’ Health Study, with 68,067 female participants aged 34–59 years in 1980, investigators have related repeatedly assessed long-term alcohol intake, and related the cumulative average intake over time to the risk of invasive uterine cancer. A total of 794 cases of invasive endometrial adenocarcinoma were identified over a 30 year follow-up period.
The authors report an inverse association among alcohol drinkers (multivariable RR=0.81; 95% CI: 0.68–0.96) compared with nondrinkers. Women with an intake of <5 g per day (an average of approximately one-half drink per day) had a 22% lower risk of endometrial cancer (multivariable RR=0.78; 95% CI: 0.66–0.94), with no further decrease evident from larger amounts of alcohol. In comparison with non-drinkers, the relative risk was similarly reduced for consumers of more than 30 grams of alcohol per day, but the number of subjects in this category was small, and a potential increase in risk from heavy drinking could not be adequately assessed in this study.
Forum members considered this to be a very well-done prospective study, with clear and biologically plausible results. By having repeated assessments of alcohol, an estimate of long-term average consumption was possible. The approximately 20% lower risk of uterine cancer among subjects with light alcohol intake remained statistically significant after multivariate adjustments for known potential confounders. Reviewers agreed with the authors that a potential mechanism for the association could be a reduction in insulin concentrations and improved insulin sensitivity that have been shown to occur with moderate alcohol consumption. Further, the frequently demonstrated inverse relation for alcohol with obesity may also play a mechanistic role. Overall, this study adds to accumulating scientific data showing that moderate drinking does not increase the risk of uterine cancer, and probably is associated with a reduction in risk
Reference: Je Y, DeVivo I, Giovannucci E. Long-term alcohol intake and risk of endometrial cancer in the Nurses’ Health Study, 1980–2010. British Journal of Cancer 2014;111:186–194; doi: 10.1038/bjc.2014.257.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 143: A Mendelian randomization assessment of alcohol and cardiovascular disease — 20 July 2014
Using a very large dataset from subjects of European descent, the authors have carried out a Mendelian randomization analysis to estimate the effects of alcohol consumption on cardiovascular disease (CVD), using as the instrumental variable an uncommon allele affecting alcohol metabolism, the ADH1B rs1229984 variant. People with this variant are unusually sensitive to alcohol (developing flushing and other uncomfortable symptoms from alcohol) and it has been well demonstrated that they are less likely than people without this variant to consume alcohol, and are unlikely to be heavy drinkers. The authors conclude that since the 7% of their subjects with the uncommon allele had less cardiovascular disease, this indicates that alcohol consumption is unrelated to CVD.
Forum members agree that the analyses were done correctly, but strongly disagree with the premise of the study and the conclusions of the authors, and consider the genetic factor chosen as inappropriate to use as the instrumental variable in Mendelian randomization. The gene studied explains only a fraction of alcohol consumption in the population (not stated in the paper) and it may have effects on CVD beyond those explained by alcohol consumption. Thus, this ADH1b allele violates the assumptions required for a variable for Mendelian randomization and would be inappropriate for judging the effects of alcohol on CVD. Further, in the present study, the authors report little relation of their estimate of alcohol consumption with HDL-cholesterol, while essentially all observational studies, clinical trials, and experimental studies have shown that alcohol is an important determinant of HDL. This further suggests that the use of the ADH1B allele provides an inadequate estimate of alcohol consumption.
Even without the weakness of the allele chosen to reflect alcohol effects, conclusions derived from Mendelian randomization in general are heavily dependent on the assumption that the instrumental chosen is appropriate, of which you can rarely be confident. Forum reviewers consider this method to be a very blunt instrument and subject to considerable bias for variables that are weakly correlated with exposure and not true instruments.
Some reviewers were concerned by the conclusion of the authors that this Mendelian randomization paper shows that all persons should drink less; this does not necessarily mean for people to completely avoid drinking. The protection of moderate drinking against CVD that is generally observed shows a non-linear gradient: it is better manifested at a low alcohol consumption, while it is less strong as the consumption levels rise above optimum and finally disappears and is transformed into harm with heavy alcohol consumption. This would be in agreement with the conclusions of most prospective studies and meta-analyses that drinking alcohol at low doses offers the best protection against CVD, as there is a J-shaped curve.
Reference: Holmes MV, Dale CE, Zuccolo L, et al (a total of 155 authors). Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. BMJ 2014;349:g4164 doi: 10.1136/bmj.g4164.
For the full critique of this study by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 142: A large study of alcohol consumption and mortality — 14 July 2014
The large European Prospective Investigation into Cancer and Nutrition Study (EPIC) has released a new analysis of the relation of alcohol consumption to mortality. The study concluded that alcohol use was positively associated with overall mortality, alcohol-related cancers, and violent death and injuries, but marginally to cardiovascular disease, and that absolute risks of death observed in EPIC suggest that alcohol is an important determinant of total mortality.
There is no question that heavy alcohol consumption, especially when associated with smoking, increases the risk of a number of upper aero-digestive cancers that are commonly referred to as “alcohol-related cancers.” In the present study, the authors have also included in this group a number of other cancers that may be related less directly to the effects of alcohol; these include colorectal cancer and female breast cancer which, because they are so much more common, make up the large majority of cancers “related to alcohol.” Forum members consider the EPIC study to be an important source of data on cancer, but had a number of questions about the analysis and especially about the conclusions of the authors.
Major weaknesses of the study are that an assessment of alcohol intake was obtained only at a baseline visit, with no further assessments during a follow-up period averaging 12 years, and especially, no information was available on the pattern of drinking of subjects (e.g., regular moderate versus binge drinking). Further, Forum members noted that there was no discussion of the effects of under-reporting of alcohol, which has been shown to markedly affect health effects of alcohol intake in epidemiologic studies. In fact, recent large studies show that most of the cases of cancer that appear to relate to “light-to-moderate drinking” actually relate to underreporting of consumption by subjects who are found, from other collected medical data, to be heavy users or abusers of alcohol.
The authors focus on “extreme drinkers,” which consist of women who consume (≥30 g/day) or men who consume ≥60 g/day. They do not point out that only 2.4% of the women in this study consumed at this level, and little attention is given to the fact that almost all of the women were non-drinkers or light-moderate drinkers. From the data presented in the paper, there is a clear U-shaped curve among women: the highest risks for total mortality were in the abstainers (a 26% increase over the referent group of light drinkers) and the very small number of women in the highest drinking category (a 27% increase).
For men, 8.2% were in the highest drinking category, reporting an average consumption of ≥ 60 g/d (5 – 6 typical drinks). For men, there was generally a U-shaped curve, with lower death rates for light to moderate drinkers. However, the heaviest drinkers had the highest risk of death for overall mortality and for deaths from cancers and other causes of death. For both men and women, at every level of drinking, smokers had an increased risk of death in comparison with non-smokers.
Some reviewers were also concerned about the unusual categorization of alcohol intake used in the study. Referring to subjects reporting 0.1 – 4.9 g/day as “moderate drinkers” is a strange designation for an alcohol intake that in most other studies would be named as light or very modest, and may lead to confusion in interpreting results. (Most studies would define 5 – 14.9 g/day as light to moderate drinkers, and this group is not given a name in this study).
Overall, this study tends to show a U-shaped relation between alcohol consumption and mortality. The data presented focus primarily on the highest categories of drinking, levels that are well known to relate to many diseases and mortality. For truly light-to-moderate consumption, however, there is overwhelming epidemiologic data that such drinking relates to lower mortality risks, and the present study does not contradict such an association.
Reference: Ferrari P, Licaj I, Muller DC, et al (36 other authors). Lifetime alcohol use and overall and cause-specific mortality in the European Prospective Investigation into Cancer and nutrition (EPIC) study. Pre-publication; BMJ Open 2014;4:e005245. doi:10.1136/bmjopen-2014-005245
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 141: A world-wide study of alcohol consumption and the risk of myocardial infarction — 3 July 2014
The authors report on data collected in the INTERHEART Study, a large international collaborative project of individuals with a first myocardial infarction (MI) and age- and sex-matched controls from 52 countries in Asia, Europe, the Middle East, Africa, Australia, North and South America. Included were nations with very divergent lifestyles, religions, degrees of development, and drinking habits. The authors attempted to provide a “world-wide” overview of the relation of alcohol consumption to the risk of myocardial infarction (MI). However, they were forced to use a case-control design, a type of study with many opportunities for bias and one that prevents determination of a causal relation. Further, the lack of detailed data on the amount of alcohol consumed by individuals weakens their results.
While the authors state that their study shows that low levels of alcohol use are associated with a moderate reduction in the risk of MI, they point out differences in results in different countries. Forum members considered that these large differences severely limit their ability to use such a dataset to provide overall conclusions on alcohol and MI. For example, only 1% of the non-drinkers in this study came from W. Europe and 1% from North America, while more than 70% of the non-drinkers came from the Middle East or Asia. With such diversity (e.g., almost all the abstainers were from one area), it is not possible to adequately “adjust” for such regional differences in analysis.
The authors also studied how alcohol consumption shortly prior to (in the 24 hours before) the occurrence of a MI relate to the short-term risk of MI. While their results show an increased risk for heavy drinking immediately prior to an MI (a result that differs from that of some previous studies), they admit analytic problems, stating: “Thus there remains uncertainty over the risk of MI in the period immediately following alcohol intake.”
Previous large prospective cohort studies (a type of epidemiologic study that decreases the risk of recall bias regarding alcohol intake and certain types of confounding) have clearly shown an inverse relation between moderate alcohol consumption and MI. Most of the previous studies have provided much more detailed data on alcohol exposure than did the present study. The authors realized many of these problems, and warn against using their results to make overall conclusions about the association between alcohol and MI from their paper. They state: “The associations observed between alcohol use and MI may be accounted for by unmeasured confounders such as genetic differences between populations, variation in alcohol type or preparation, and heterogeneity of social context. The present analysis should therefore prompt further research to clarify the nature of the association between alcohol use and MI.” Unfortunately, the conclusions presented in the abstract and in the do not mention such problems.
Some Forum members worried that many readers of the paper will be left with a very misleading impression of the relation of alcohol consumption to myocardial infarction, and will not be aware that the conclusions trumpeted in the abstract are compromised by weak data. Overall, members considered that the present paper adds little to our knowledge about the risks and benefits of alcohol in relation to cardiovascular disease.
Reference: Leong DP, Smyth A. Teo KK, McKee M, Rangarajan S, Pais P, Liu L, Yusuf S, on behalf of the INTERHEART investigators. Patterns of Alcohol Consumption and Myocardial Infarction Risk: Observations from 52 Countries in the INTERHEART Case-Control Study. Circulation 2014 (pre-publication) DOI: 10.1161/CIRCULATIONAHA.113.007627.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 140: A meta-analysis shows that light alcohol consumption is associated with a reduced risk of stroke, while heavier drinking may increase risk — 5 June 2014
Most epidemiologic studies have shown a reduction in the risk of ischemic stroke (and total stroke, as ischemic stroke is by far the most common type in western countries) to be associated with light to moderate alcohol consumption. The present study, a meta-analysis, was based on 27 prospective studies; the authors categorized a reported intake of <15 g/day as light consumption, and 15-30 g/day as moderate consumption. The authors point out differences (greater smoking, larger amounts of alcohol) between Chinese subjects and those from other countries, which may explain some of the differences shown between alcohol’s effects in the different countries. They also point out that they had no data on the pattern of drinking (regular, moderate intake versus binge-drinking) or on the type of alcoholic beverage consumed.
The key results of the study are a significant 15% reduction in total stroke for low alcohol intake, no effect for moderate, and a 20% increased risk for heavy alcohol consumption (RR 1.20, 95% CI 1.01, 1.43). Analyses were also done according to type of stroke: for ischemic stroke and stroke mortality there were decreases for low alcohol intake, but no significant effects of either moderate or heavy intake. For hemorrhagic stroke, the RR for subjects reporting heavy alcohol intake was higher than that of abstainers, but none of the differences between drinkers and non-drinkers was statistically significant.
This meta-analysis supports previous findings of a decrease in the risk of most strokes with light drinking and possibly an increase in the risk for heavy drinking. Forum members generally agreed with the conclusions of the authors: “Low alcohol intake is associated with a reduced risk of stroke morbidity and mortality, whereas heavy alcohol intake is associated with an increased risk of total stroke. The association between alcohol intake and stroke morbidity and mortality is J-shaped. An alcohol intake of 0-20 grams/day is associated with decreased rates of stroke morbidity and mortality.”
Reference: Zhang C, Qin Y-Y,Chen Q, Jiang H, Chen X-Z, Xu C-L, Mao P-J, He J, Zhou Y-H. Alcohol intake and risk of stroke: A dose–response meta-analysis of prospective studies. Int J Cardiol 2014; pre-publication; http://dx.doi.org/10.1016/j.ijcard.2014.04.225.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 139: Does adjustment for stress levels explain the protective effect of moderate drinking on the risk of mortality? — 18 May 2014
An inverse association between moderate alcohol consumption and total mortality has been reported in most prospective epidemiologic studies, even after adjustments for all known potential confounders. The present analysis was carried out specifically to focus on the effects of psychosocial stressors on the association, using a large population-based German cohort from the WHO MONICA study. No alcohol intake was reported by 15.3% of males and 41.8% of females; “moderate drinking” was defined as an average intake of 0.1-39.9 g/day for men (making up 51.1% of the cohort) and 0.1 – 19.9 g/day for women (38.8% of the cohort). Although data are not presented, there were apparently few women in the higher drinking categories.
The authors related the effects of including, or not including, in their equations a large number of psychosocial stressors, including educational level, occupational status, several indices of social support, job strain symptoms, depressive symptoms, somatic symptoms, and self-perceived health status, in the estimation of the effects of alcohol consumption on risk of total mortality over an average follow-up period of 12 years. In their analyses, there was little effect on risk estimates for mortality when these factors were added to the multi-variable analysis. The authors conclude: “The observed protective effect of moderate drinking could not be attributed to misclassification or confounding by psychosocial stressors.”
The authors have demonstrated among men a “U-shaped” curve, with the risk for moderate drinkers being 25-30% lower than that of both non-drinkers and heavier drinkers. For women, there was a lower estimated mortality risk ratio for all drinkers than for non-drinkers, although the confidence intervals included 1.0 in all categories (perhaps, as the authors state, there were few women in their higher categories of alcohol intake).
Forum reviewers thought that this was a well-done analysis of a large population-based population. It did not support the hypothesis that social support, job strain, depressive symptoms, and other such psychosocial factors have a strong influence on the demonstrated inverse relation between moderate alcohol consumption and total mortality. Thus, this study provides additional evidence that the observed reduction in total mortality seen among moderate drinkers is not due to confounding by other lifestyle factors, including psychosocial stressors.
Reference: Ruf E, Baumert J, Meisinger C, Döring A, Ladwig K-H, and for the MONICA/KORA Investigators. Are psychosocial stressors associated with the relationship of alcohol consumption and all-cause mortality? BMC Public Health 2014, 14:312. http://www.biomedcentral.com/1471-2458/14/312.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 138: Underreporting of alcohol intake affects the relation of alcohol to the risk of cancer — 23 April 2014
Epidemiologists are often faced with reported adverse health effects of alcohol among subjects reporting very low levels of consumption, levels that physiologically should not cause diseases such as cancer. It is often assumed that at least some of the subjects reporting low levels of intake may be underreporting their actual intake, but heretofore it has been difficult to judge this.
In the present study, the authors used each subject’s computer-based data on conditions and diseases (including laboratory and social factors), related to alcohol misuse, collected over many years to identify subjects reporting “light-to-moderate” alcohol intake who were likely, or unlikely, to be underreporting their intake at a baseline examination. Overall, 18.4% of subjects were suspected of being underreporters while 46.5% had adequate data that suggested that they were not underreporters. (The remaining 35.1% of subjects had inadequate data stored in the computer to be classified.)
Among their cohort of more than 100,000 subjects, 14,880 developed cancer during an average follow-up period of 18 years. There were 23,363 subjects who reported that they were light (up to 1 drink/day) or moderate (1 to 2 drinks/day) drinkers. In all comparisons, subjects suspected of being underreporters of their alcohol intake had a higher risk of cancer than those not categorized as being underreporters. For example, among subjects reporting 1 to 2 drinks/day, in comparison with non-drinkers, the risk ratio of any type of cancer among those considered to not be underreporters was 0.98 (95% CI 0.87-1.09); in other words, no effect on cancer risk from alcohol. For those categorized underreporters, however, the relative risk of any cancer was 1.33 (95% CI 1.21–1.45). Similar results were seen for alcohol-related cancers as for any cancer. Also, the risk of breast cancer among women was less than one-half as high among moderate drinkers who were unlikely to be underreporters of their alcohol intake as among those considered likely to be underreporting their drinking.
Adjusting for confounding in prospective studies is an ever-present challenge for epidemiologists. One factor that has often been considered probable, but difficult to adjust for, is the underreporting of actual alcohol intake by subjects. Being able to adjust for such unerreporting would greatly improve studies relating alcohol consumption to the risk of cancer (and other chronic diseases). For epidemiologic studies that have extensive longitudinal data on all medical conditions (such as the Kaiser-Permanente Study, the basis for these analyses), the approach described in this paper could be an extremely valuable way of seeking the true relation between light-to-moderate alcohol intake and cancer as well as with a variety of other health outcomes. Based on the present study, an increase in the risk of cancer among light-to-moderate drinkers may occur primarily among those who underreport their alcohol intake.
Reference: Klatsky AL, Udaltsova N, Li Y, Baer D, Tran HN, Friedman GD. Moderate alcohol intake and cancer: the role of underreporting. Cancer Causes Control 2014; on-line publication; DOI 10.1007/s10552-014-0372-8 2014.
Potential Conflict of Interest: The first author of this paper, Dr. Klatsky, is a member of the International Scientific Forum on Alcohol Research. While he has not contributed to this critique, readers may wish to take this fact into account when interpreting the conclusions of the review.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 137: Alcohol intake prior to and during pregnancy and birth outcomes — 28 March 2014
The present analysis was carried out among 1,264 women from Leeds, UK, whose alcohol intake was estimated prior to and during pregnancy. The outcomes were birth weight of the infant and whether or not it was small for gestational age (SGA). In comparison with most previous research on this topic, this study is notable for being of a relatively small size. Further, it had a high percentage of women who consumed alcohol both prior to and during the first trimester, had a very low participation rate of eligible women (only 30%), failed to present estimated effects by ethnicity, and had some questions related to residual confounding. It is unclear how the results of this study increase our knowledge of maternal alcohol consumption and birth outcomes.
Forum members do not believe that the consumption of alcohol should be recommended for pregnant women. A certain percentage of newborns will be small for gestational age, have certain deformities, and have later emotional and behavioral abnormalities. If a woman has consumed any alcohol during the pregnancy, she (and perhaps even her doctor) may blame the abnormality on alcohol consumption, whether or not it had anything to do with it. Hence, the majority of Forum members agree that women should not be encouraged to consume alcohol during pregnancy.
Further, scientific data are very consistent on the potential risks of serious adverse health outcomes of the infant from heavy maternal drinking, especially among women who are alcoholics. Heavy-drinking women who become pregnant should be strongly urged to stop their drinking.
On the other hand, sound data indicating harmful effects on the fetus of light or occasional drinking by a pregnant woman are difficult to come by. Because of the epidemiologic concerns of the present paper, described in our Forum critique, we do not believe that this study adds materially to our understanding of the topic. The serious anxiety occurring among some women who may have ingested some alcohol prior to learning that they were pregnant seems, based on numerous studies, to generally be unnecessary; the need to abort a fetus because of previous light drinking by the mother cannot be justified.
There is a serious problem in interpreting all studies of prenatal alcohol exposure and the outcomes of pregnancy because of potential confounding, especially by ethnicity, education, smoking, coexisting use of illegal drugs, etc. Further, alcohol use by pregnant women has become an especially emotional and even a moral issue, and the entangled confounders make rational analysis most difficult. This means that there is a difficult challenge for epidemiologists and statisticians, as well as for public health officials and the general public, about how to interpret results of individual research projects. The literature can support varying views, from no alcohol at all for those who might soon be expectant mothers to being able to drink moderately throughout pregnancy.
Also, it should be pointed out that the potential health benefits of moderate alcohol consumption relate primarily to middle-aged and older people, so there is no reason for pregnant women to consume alcohol for its “health effects.” Thus, it is very reasonable that the majority of women choose to avoid alcohol during pregnancy. Further, heavy drinking during pregnancy has known potentially serious consequences, and should never be encouraged. Finally, there is insufficient scientific evidence that an occasional drink of alcohol during pregnancy leads to harm to the fetus, and should not cause undue alarm in a pregnant woman who may have consumed some alcohol before she realized she was pregnant.
Reference: Nykjaer C, Alwan NA, Greenwood DC, Simpson NAB, Hay AWM, White KLM, Cade JE. Maternal alcohol intake prior to and during pregnancy and risk of adverse birth outcomes: evidence from a British cohort. J Epidemiol Community Health 2014, pre-publication. doi:10.1136/jech-2013-202934
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 136: Alcohol’s effects on cardiovascular risk among subjects with diabetes mellitus — 18 March 2014
A U- or J-shaped curve for the relation of alcohol consumption to cardiovascular disease (CVD) among diabetics has been shown in most prospective epidemiologic studies for many years, and CVD is the leading cause of death among diabetics. A variety of potential mechanisms of protection against CVD have been described, including beneficial effects of moderate drinking on lipids, inflammatory markers, and insulin resistance. The current paper assesses the effects of alcohol use among participants in the Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified-Release Controlled Evaluation (ADVANCE) trial. It was based on more than 11,000 subjects with diabetes from 20 countries, including those in Eastern Europe, Asia, and established market economies in Western Europe, North America, and the Pacific region. The outcomes over 5 years of follow up were CVD events (death from CVD, non-fatal myocardial infarction, non-fatal stroke), microvascular disease (renal disease, diabetic eye disease), and all-cause mortality.
Key results of the analyses showed that during follow up, more than 1,000 subjects (about 10%) had a major CVD, with similar percentages experiencing a microvascular complication or dying. The authors report that “Compared with abstainers, any alcohol use was associated with a 17% lower risk of cardiovascular events, a 15% lower risk of microvascular complications, and a 13% lower risk of all-cause mortality.” While there were few heavy drinkers (<4% of subjects), their data indicated that there was no significant lowering of risk of the outcomes among such subjects. Subjects who consumed wine had lower estimates of cardiovascular disease outcomes and mortality than consumers of other beverages.
Forum reviewers considered this to be a well-done analysis based on a large cohort of subjects with diabetes mellitus, with an adequate number of non-drinkers to serve as a referent group. The results strongly support previous studies that have shown a lower risk of cardiovascular events and total mortality among diabetic subjects who consume moderate alcohol. The study also showed that the risks of microvascular complications (diabetic kidney disease, diabetic eye disease) were lower among moderate drinkers.
The Forum considers this to be an important message (to physicians and the public), as the vascular ravages of diabetes are very serious, and diabetes is such a common disease that is increasing throughout the world. Diabetic patients without contraindications to alcohol sorely need to know of the potential cardiovascular protection of moderate alcohol consumption.
Reference: Blomster JI, Zoungas S, Chalmers J, Li Q, Chow CK, Woodward M, Mancia G, Poulter N, Williams B, Harrap S, Neal B, Patel A, Hillis GS. The relationship between alcohol consumption and vascular complications and mortality in individuals with type 2 diabetes mellitus. Diabetes Care 2014; pre-publication: DOI: 10.2337/dc13-2727
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here
===============================================================================
Critique 135: Binge drinking greatly increases mortality risk among moderate drinkers — 11 March 2014
This study was based on a sample of “late-middle-aged” (55-65 years old at baseline) community residents who were recruited from the western part of the United States to participate in a study of late-life alcohol consumption and drinking problems. The present analyses evaluated association between episodic heavy drinking and total mortality among 446 adults who were considered to be “moderate” drinkers. The authors report that the 74 moderate drinkers who engaged in episodic heavy drinking (“binge drinking”) had more than two times higher odds of 20-year mortality than moderate drinkers who did not binge drink.
An association between binge drinking and health outcomes has been demonstrated in epidemiologic studies for decades. Many (but not all) studies have shown an approximately two-fold increase in the risk of adverse outcomes for binge drinkers, in comparison with moderate drinkers who do not binge drink. In reviewing the present study, Forum members commented on the small number of subjects (only 74 binge drinkers in the analysis), and some other analytic weaknesses (e.g., no data on potential changes in drinking habits over 20 years, inadequate control of some potential confounders, results not applicable to the general population as some subjects were recruited because of previous alcohol misuse). Nevertheless, the results of the study support adverse effects on mortality of such a drinking pattern.
There are now considerable scientific data indicating harmful health effects of episodic excessive drinking in terms of coronary heart disease, other diseases of ageing, and mortality. Simply knowing the average intake of subjects over a period of time is inadequate for classifying their alcohol consumption. For middle-aged and older subjects the drinking pattern that has been shown to be associated with the most favorable health outcomes (including greater longevity of life) is regular, light-to-moderate intake, especially when the alcoholic beverage is consumed with food.
Reference: Holahan CJ, Schutte KK, Brennan PL, Holahan CK, Moos RH. Episodic heavy drinking and 20-year total mortality among late-life moderate drinkers. Alcohol Clin Exp Res 2014; pre-publication; DOI: 10.1111/acer.12381.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 134: Comments on “Section 2.3, Alcohol Consumption,” from the “World Cancer Report 2014” issued by the World Health Organization – 11 February 2014
A recently released report by IARC (International Agency for Research on Cancer) of the World Health Organization, entitled “World Cancer Report 2014,” includes a section on alcohol consumption as a factor in the etiology of cancer. From reading this report, it is clear that the conclusion of the authors is that all alcohol consumption is harmful, regardless of the amount consumed, the type of beverage, or the pattern of drinking. The members of the International Scientific Forum on Alcohol Research (the Forum) have real concerns about the WHO report.
It appears that the authors have been very selective in choosing the data upon which they base their conclusions, often citing their own work and ignoring thousands of scientific articles relating alcohol consumption to cancer rates and mortality. The report fails to discuss potential lower risks of cancer associated with polyphenols in wine and some other beverages. It ignores the consistent finding in almost all prospective epidemiologic studies over many decades that total mortality rates are lower among light-to-moderate alcohol consumers (and recent evidence suggests that this may even be true among people with cancer).
Members of the Forum strongly agree that heavy alcohol consumption and “binge” drinking are associated with many adverse effects (and would never be advised by responsible agencies). However, the WHO report seriously undermines its credibility by publishing a report that seems to deliberately ignore overwhelming scientific evidence showing that light-to-moderate consumption of alcohol not only reduces overall mortality but is usually not associated with an increased risk of cancer.
Excessive and binge drinking in young people is a growing scourge in many parts of the world, and alcohol consumption (especially in conjunction with smoking) clearly increases the risk of upper aero-digestive cancers; further, even moderate consumption is associated with a slight increase in the risk of breast cancer in women. However, the scare tactics condemning all alcohol consumption in the WHO report tend to obscure those important messages.
It is the opinion of our Forum that WHO, in the alcohol section of its new publication World Cancer Report 2014, has not provided an objective statement on alcohol and cancer based on current scientific data. By doing so, WHO has lost credibility and, more importantly, has missed a key opportunity to convey important focused messages about alcohol and cancer that would be more likelty to improve the health of the public.
Reference: Rehm J, Shield K. Section 2.3, Alcohol Consumption, from World Cancer Report 2014, pp. 97-106, released 3 February 2014 by IARC (International Agency for Research on Cancer), of the World Health Organization.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 133: Alcohol intake may lower the risk of developing multiple sclerosis — 4 February 2014
Previous research has shown that alcohol consumption may be associated with a reduced risk of rheumatoid arthritis, lupus erythematosus, and other autoimmune diseases. There have also been reports that alcohol may lower the risk of multiple sclerosis (MS). The authors of the present paper have used data from two large Swedish case-control studies of MS to evaluate the relation of alcohol consumption to MS. Key results showed that in both of the case-control analyses, there was a dose-response inverse relation between alcohol consumption and the risk of developing MS. In comparison with subjects reporting no alcohol intake in the 5- or 10-year period during which the diagnosis of MS was first made, subjects in the highest alcohol consumption group (> 112 g/week, about 9 drinks per week for women; >168 g/week, about 14 drinks per week for men) had 30% to 50% lower risk of developing MS. A variety of potential confounders were included in the analysis, including smoking, education, and SES.
Forum members who reviewed this paper all thought that it reflected a well-done analysis. The main concerns were that, as are most studies of uncommon diseases, these were case-control comparisons (which may be associated with recall bias, reverse causation, and other potential confounding variables), and that the investigators could not determine if the “non-drinkers,” their referent group, were lifetime abstainers or former drinkers. Also, while earlier research has shown that the polyphenols in wine may provide protection beyond that of alcohol in combating inflammation, there were no data on beverage-specific results.
In general, however, Forum members welcomed this contribution to our knowledge on the subject, and thought that the authors did a good job in discussing the strengths and weaknesses of their study. There was a brief discussion of potential mechanisms by which alcoholic beverages could lower the risk of MS, but no discussion of the potential added effects related to polyphenolic substances. Forum members also thought that serum uric acid (which may increase with alcohol consumption) could play a role in an autoimmune disease, but this was not discussed by the authors.
Based on previous research and the results of this paper, it is probable that moderate alcohol intake, especially of wine, may lower the risk of developing MS, a neurological disease for which no cure is currently available. While MS is too uncommon a condition to use these findings to recommend alcohol consumption for the prevention of the disease, it would be useful if future research could help determine if, for subjects who already have MS, moderate drinking may affect the progression of their disease.
Reference: Hedström AK, Hillert J, Olsson T, Alfredsson L. Alcohol as a modifiable lifestyle factor affecting multiple sclerosis risk. JAMA Neurology 2014; doi:10.1001/jamaneurol.2013.5858; published online January 6, 2014.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 132: Pattern of alcohol consumption and cause of death in a large European prospective study — 21 January 2014
A large group of investigators participating in the European Prospective Investigation into Cancer and Nutrition (EPIC) study have reported on the association of alcohol consumption with disease-specific mortality over a 12-year period among a very large number of men and women. Alcohol intake over the past year (as well as estimates of earlier intake) was reported at baseline. A variety of approaches were used to identify deaths in the participating cohorts, but validation of the cause of death was not possible. No data were reported on certain key aspects of drinking pattern (frequency of alcohol intake, binge drinking, with meals, etc.) and beverage-specific effects were not reported.
The authors report that the risk of death from cardiovascular diseases was lower, and from cancer and certain other causes of death were higher, among drinkers than among their referent group of “lifetime light users” (men reporting ≤1 drink/week and women reporting ≤ 0.5 drinks/week). However, their graphs of alcohol intake and risk of total mortality (not included in the paper but in supplementary data they provide on the internet) show strong J-shaped curves for increasing alcohol intake for both men and women. For men, the risk among alcohol consumers of up to about 48 gr/day (the equivalent of approximately four “typical drinks”) was lower than that of the lifetime light users that made up the referent group; at higher intake, the risk increased above that of light drinkers. For women, the risk of total mortality for drinkers remained lower than that of the referent group at all reported levels of intake. Despite these findings, the entire paper focuses only on the increased risk of death from alcohol for certain diseases, and almost completely ignores the net, overall effects on total mortality.
Forum reviewers considered that while the analyses were done correctly, there were major weaknesses in the estimation of “lifetime alcohol intake,” no data on the pattern of intake, no validation of coexisting diseases and, especially, no validation of the specific cause of death, even though this was the primary outcome of the study. All of these factors weaken the strong assertions made by the authors in their conclusions.
Forum members were concerned that the authors seemed to obscure the total effects of light-to-moderate drinking (lower risk of all-cause mortality), and emphasize only the harmful effects. Some reviewers considered that the presentation appeared to be based more on ideology than on an unbiased assessment of the data, and one suggested that the paper appears to have been written starting from pre-conceived conclusions, then finding data to support them.
It is interesting that two Commentaries published with this article came to divergent views. One by Stockwell and Chikritzhs emphasized potential bias and confounding that cause concern when relating alcohol to mortality in observational studies. While they then pointed out how well the present authors adjusted for many of these factors, they nevertheless concluded their commentary repeating how such factors are difficult to control and stating that “ . . . a healthy dose of skepticism is warranted for the hypothesis that light/moderate alcohol consumption is beneficial to health.” (They do not mention that data on alcohol and mortality are far more robust that data supporting generally accepted beliefs of the beneficial effects of physical exercise, eating a healthy diet, maintaining a lean body mass, etc.)
On the other hand, the commentary on the present paper by Banks considered the data presented quite sound, and concluded: “If taken as causal, these findings are consistent with most public health advice about alcohol, except that most advice recommends an upper limit to alcohol consumption, but does not actually encourage drinking. In fact, the evidence goes further than this and indicates that, in later life, on average and bearing in mind the priorities and risks of specific individuals, drinking at least some alcohol, but not too much, is likely to minimize the overall risk of death.”
Reference: Bergmann MM, Rehm J, Klipstein-Grobusch K, et al (38 authors). The association of pattern of lifetime alcohol use and cause of death in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Int J Epidemiol 2013;42:1772-1790
Attached Commentaries:
Banks E. Commentary: Lifetime alcohol consumption and mortality: have some, but not too much. Int J Epidemiol 2013;42:1790–1792; doi:10.1093/ije/dyt218
Stockwell T, Chikritzhs T. Commentary: Another serious challenge to the hypothesis that moderate drinking is good for health? Int J Epidemiol 2013;42:1792–1794; doi:10.1093/ije/dyt217
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 131: Effects of alcohol consumption on the risk of gout — 23 December 2013
A new meta-analysis has been conducted to assess the effects of alcohol consumption on the risk of gout. A total of 12 articles with 17 studies involving 42,924 cases met the inclusion criteria. The authors report that the pooled RRs for light (≤1 drink/day), moderate (>1 to <3 drinks/day), and heavy drinking (≥3 drinks/day) vs. non/occasional alcohol drinking were 1.16 (95 % CI, 1.07–1.25), 1.58 (95 % CI, 1.50–1.66), and 2.64 (95 % CI, 2.26–3.09), respectively. The results suggested that alcohol consumption might be associated with increased risk of gout.
Forum reviewers agreed that the analytic methodology in this paper was appropriate. Considerable research has shown that alcohol intake, especially heavier drinking, increases serum uric acid levels and the risk of gout. There remain some questions about the relation of wine consumption with gout, and the present study did not have data to test beverage-specific responses.
Overall, data suggest that alcohol intake, especially heavier drinking, raises serum uric acid levels and may trigger an acute attack in persons with gout, especially those who are not controlling their disease with appropriate medication. A number of studies, including the present one, suggest that even light alcohol intake may increase the risk of developing gout. In any case, the risk appears to be rather low with light drinking, a level of alcohol intake that should reduce the risk of cardiovascular disease. Also, some studies suggest that the risk is lower for the consumption of wine than for the consumption of other beverages containing alcohol.
Reference: Wang M, Jiang X, Wu W, Zhang D. A meta-analysis of alcohol consumption and the risk of gout. Clin Rheumatol 2013;32:1641–1648.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 130: How alcohol consumption may interact with genetic factors that relate to health and disease — 10December 2013
Despite extensive research over the past few decades, our knowledge about the genes that underlie most chronic diseases remains incomplete. For example, even for alcohol-related diseases, it is not possible at present to determine how an individual person will respond over a lifetime to varying amounts of alcohol intake: not all heavy drinkers develop cirrhosis; not all moderate drinkers lower their risk of cardiovascular disease. While the underlying genetic pattern of a person undoubtedly plays a role in his/her health outcomes, environmental factors, including alcohol consumption, may modify the effects of genes. The modification of the effects of genes by environmental factors, such as alcohol intake, can be referred to as “epigenetics.”
A new paper on epigenetics, by a leading scientist who has worked at the National Institute of Alcohol Abuse and Alcoholism (NIAAA) for many years, provides important new insight into mechanisms by which alcohol intake, especially heavy consumption, may modify the activity of genes affecting health. Dr. Zakhari describes specific effects that heavy alcohol intake can have on the activities of enzymes involved in epigenetic modifications. In some cases, alcohol enhances genetically determined effects, in others it suppresses such activity. As stated by the author, “Metabolites, including those generated during ethanol metabolism, can impact disease states by binding to transcription factors and/or modifying chromatin structure, thereby altering gene expression patterns.”
Forum members consider this to be a very well-thought-out and well-done presentation of important new data. They agree with the author that these observations could help researchers to design model medications to treat or at least ameliorate alcohol-related organ damage, such as cirrhosis of the liver and alcohol-related cancers. While reviewers consider that these observations are important in our understanding of how alcohol affects health, they point out that they must be tested in further research, especially epidemiologic studies, to evaluate the extent that such interations between alcohol and genes actually affect health outcomes. Key problems that limit our ability to determine causality of disease from epidemiologic studies include not knowing the underlying genetic susceptibility of individual subjects and, as pointed out in the present paper, not accounting for environmental factors that may modify such genetic effects.
Reference: Zakhari S. Alcohol metabolism and epigenetics changes. Alcohol Research: Current Reviews 2013;35:9-16.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 129: Association of alcohol consumption with skin cancer; A report from the Women’s Health Initiative — 20 November 2013
A report from more than 59,000 women in the Women’s Health Initiative related reported alcohol consumption to the risk of melanoma (MM) and non-melanoma skin cancer (NMSC). This was a fairly large study, with 532 cases of melanoma and 9,593 cases of NMSC occurring over approximately 10 years of follow up. The key reported results were for a higher hazard of MM (HR 1.64) and NMSC (OR 1.23) for drinkers of 7 or more drinks/week, compared with non-drinkers. Lifetime alcohol consumption was also positively associated with hazard of MM and risk of NMSC, with the only significant increases for MM according to type of beverage being seen for women with a preference for white wine or liquor. As shown in many previous studies, the risk of these skin cancers was lower among smokers than among non-smokers.
Forum reviewers thought that this was a very well-done analysis. They did note that there were large decreases in the estimates of HRs related to alcohol consumption when adjustments were made for sun exposure and other known confounders. For example, the HR for MM decreased for total wine from 1.30 to 1.06 when adjusted; for red wine:1.71 to 1.34; for white wine: 1.93 to 1.52; for liquor: 1.87 to 1.65; for beer: 1.34 to 1.18. The magnitude of these changes, as well as the very different baseline characteristics of the women according to their drinking habits, raises the possibility that there may be residual confounding affecting the results. In addition, reviewer Zhang points out that by including subjects with these skin cancers prior to baseline in their main analyses, there could be a problems with bias in their results.
Forum member Klatsky has recently reported on this topic using several decades of follow-up data from the Kaiser-Permanente study, with more than 300,000 subjects and more than 1,000 cases of MM. In that study, he and his colleagues found that among persons preferring wine, the HR for MM at 3+ drinks per day was 1.7 (95% CI 1.2-2.5), while it was 1.2, 1.3, and 1.1 in persons with preference for liquor, beer, and no beverage type. However, at 1-2 drinks per day, wine drinkers had a HR of 0.9. Klatsky states “So maybe too much should not be made of the beverage type data in these analyses. However, the association with alcohol seems statistically solid.”
A previous study by Mukamal, with data from 300,000 subjects participating in a risk factor surveillance survey reports: “Approximately 33.5% of respondents reported a sunburn within the past year. Heavier average alcohol use and binge drinking were both positively associated with prevalence and number of sunburns within the past year. The adjusted odds ratios for prevalence and number of sunburns among binge drinkers were 1.39 (1.31-1.48) and 1.29 (1.20-1.38), respectively.” Klatsky wonders whether “possible confounding by sun is not only an artifact of SES and tropical vacations, but whether heavy imbibers at the beach may fall asleep when exposed or simply do not notice their sunburn until it is severe.” Other Forum reviewers also worry that there may be residual confounding in the present study from sun and ultraviolet exposure.
Klatsky adds: “However, even if the alcohol-melanoma association is due to confounding by sun exposure, the same explanation seems less plausible for the inverse association between smoking and melanoma. While there is obviously no public health utility in any ‘protective’ effects of smoking, that association is scientifically interesting and could be a clue to mechanisms.”
The bottom line is that there are considerable observational epidemiologic data suggesting that alcohol consumption may relate to an increase in the risk of MM and NMSCs. As mechanisms are not known, there is still concern that much of this relation may relate to residual confounding by ultraviolet sun exposure, the most important environmental factor for these diseases.
Rerference: Kubo JT, Henderson MT, Desai M, Wactawski-Wende J, Stefanick ML, Tang JY. Alcohol consumption and risk of melanoma and non-melanoma skin cancer in the Women’s Health Initiative. Cancer Causes Control 2013 (pre-publication) DOI 10.1007/s10552-013-0280-3
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 128: Little effect of alcohol consumption on breast cancer risk found among African-American women — 14 November 2013
Alcohol is known to be a risk factor for breast cancer in Caucasian women, but the evidence in African-American (AA) women is limited and results from previous studies are inconclusive. The present case-control study, based on 803 cases of breast cancer among African American women in the northeastern part of the USA, evaluated associations between recent and lifetime drinking and breast cancer risk. The authors report that there was no association between recent drinking and breast cancer risk, even when stratified by menopausal status or by hormone receptor status. Further, their analyses suggested a slight decrease in cancer risk with alcohol consumption among women who drank when under 20 years of age (OR = 0.65; 95% CI: 0.47–0.89), regardless of menopausal or hormone receptor status.
Forum reviewers point out that this was a case-control study of breast cancer, which always presents an opportunity for recall bias, and the number of cases was not large. Further, AA women generally drink very little, so it may be difficult to determine if larger amounts of alcohol may increase breast cancer risk.
On the other hand, the results were based on a very well-done and complete analysis, with appropriate control for known risk factors, similar results were obtained when recent (in last year) alcohol intake and long-term alcohol consumption were considered, and their finding of increased risk of breast cancer among subjects with a family history of breast cancer, a personal history of benign breast disease, and HRT use strengthen the results.
The results of this study are consistent with those from many previous studies showing little effect of alcohol consumption on breast cancer risk among AA women. However, given that few AA women in the USA drink alcohol, and those that do typically consume only small amounts, the study cannot estimate the potential effect on breast cancer among heavier drinkers. Further, Forum members believed that the decrease in the risk of breast cancer found in this study for drinking early in life (before age 20 years) may be due to residual confounding by socio-economic factors.
Overall, the present study supports previous research suggesting that the light alcohol consumption typically seen among AA women in the USA is not an important factor in their risk of breast cancer. On the other hand, this paper reports similar null results between alcohol and cancer risk among Caucasian women in their study. Current data do not necessarily indicate that there are ethnic differences in alcohol metabolism that may lead to differences between Caucasian and AA women in the association of alcohol consumption with breast cancer, and this study alone cannot be used to support such a premise.
Reference: Chandran U, Zirpoli G, Ciupak G, McCann SE, Gong Z, Pawlish K, Lin Y, Demissie K, Ambrosone CB, Bandera EV. Does alcohol increase breast cancer risk in African-American women? Findings from a case–control study. British J Cancer 2013;109:1945–1953 | doi: 10.1038/bjc.2013.513.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 127: Estimation of alcohol-attributable and alcohol-preventable mortality in Denmark — 6 November 2013
In an attempt to judge the harmful and beneficial health effects related to alcohol consumption, Danish scientists have carried out analyses comparing alcohol-attributable and alcohol-preventable mortality in Denmark. They have used estimates of the potentially harmful effects of alcohol use on more than 20 diseases, giving 100% values to “alcohol use disorders,” although the specific causes of death are not known for this category. Most of the other attributions for harm are realistic, but the alcohol preventable attributions for diabetes and ischemic heart disease appear to be low. The authors conclude that 5.0% of deaths among women and 9.5% of deaths among men were attributable to alcohol in Denmark in 2010, with the majority of all alcohol-attributable deaths caused by high consumption. They attribute only between 2 and 3% of deaths to be preventable by alcohol.
Previous estimates of alcohol-attributable and alcohol-preventable effects have varied widely, emphasizing the importance of the assumptions made by the investigators in any set of analyses. For example, an analysis of deaths in Germany by Konnopka et al (Konnopka A, Hans-Helmut König H-H. The health and economic consequences of moderate alcohol consumption in Germany 2002. Value in Health 2009;12:253-261) concluded that there were more alcohol-preventable deaths than alcohol-attributable deaths and a report from the UK also estimated much lower rates for alcohol-attributable deaths (White IR, Altmann DR, Nanchahal K. Mortality in England and Wales attributable to any drinking, drinking above sensible limits and drinking above lowest-risk level. Addiction 2004;99:749–756). Further, a previous report that included data for Denmark gave very different results for net alcohol effects, estimating that less than 1% of deaths were attributable to alcohol (Britton A, Nolte E, White IR, Gronbaek M, Powles J, Cavallo F, McPherson K. A comparison of the alcohol-attributable mortality in four European countries. Eur J Epidemiol. 2003;18:643–51). It is probable that different underlying assumptions of alcohol effects on various diseases are the prime reason for such differences.
There is no question that heavy alcohol consumption contributes to a large number of disease conditions, and the findings of this study emphasize the magnitude of the problem. On the other hand, if the potentially beneficial effects of moderate alcohol consumption on many common diseases are underestimated, a net unfavorable result, as in the present study, is unavoidable. It will be interesting to see what assumptions are made in other studies such as this, and how such assumptions affect the outcome of analyses.
Reference: Eliasen M, Becker U, Grønbæk M, Juel K, Tolstrup JS. Alcohol-attributable and alcohol-preventable mortality in Denmark: an analysis of which intake levels contribute most to alcohol’s harmful and beneficial effects. Eur J Epidemiol 2013; DOI 10.1007/s10654-013-9855-2
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 126: Moderate alcohol intake may lower the risk of rheumatoid arthritis — 11 October 2013
Moderate alcohol intake, compared with abstinence, has been related to lower inflammatory markers and a reduced risk of many auto-immune diseases, including rheumatoid arthritis (RA), systemic lupus erythematosus, autoimmure diabetes, and Graves hyperthyroidism. The present large meta-analysis relating alcohol to RA includes data from 5 prospective cohort studies and 3 nested case-control studies. Their analyses are based on prospective data from a total of almost 200,000 subjects, among whom 1,878 developed RA.
This meta-analysis concludes that low to moderate alcohol consumption is inversely associated with the development of RA. It suggests a “J-shaped” curve, with a lowered risk for an average intake of up to 15 g of alcohol (about 1 to 1 ½ typical drinks), in comparison with non-drinkers, and an increased risk for heavier drinking. While the immediate effects were greater for women in this study, for long-term effects the authors noted that “Regardless of sex, a consistent low to moderate alcohol consumption for a period of at least 10 years was found to have a 17% reduction in RA risk.”
Beneficial effects of alcohol on indices of inflammation have been shown repeatedly. The probable mechanism of alcohol’s effect on the risk of RA is down regulation of the immune response and a decrease in pro-inflammatory cytokines.
Reference: Jin Z, Xiang C, Cai Q, Wei X, He J. Alcohol consumption as a preventive factor for developing rheumatoid arthritis: a dose-response meta-analysis of prospective studies. Ann Rheum 2013. doi: 10.1136/annrheumdis-2013-203323
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 125: Effects of alcohol consumption on risk of colorectal cancer; potential modification by folate intake — 25 September 2013
Many epidemiologic studies have shown a small increase in the risk of breast cancer and colorectal cancer to be associated with alcohol consumption. Some have found that higher intakes of folic acid may attenuate such an increase in risk. The present study was designed to evaluate the influence of alcohol consumption on the risk of colorectal cancer according to folic acid fortification period in the United States. The relation of alcohol intake to colorectal cancer in two prospective studies (the Nurses’ Health Study and the Health Professionals Follow-up Study) was compared for a prefortification period (before 1998) with such risk estimates during the postfortification period, which began in 1998. A total of 2,793 cases of invasive colorectal cancer were documented.
The authors concluded that their data support an increase in colorectal cancer with high alcohol intake, and suggest that the risk may be lower in the postfortification period due to a higher folate intake in the US population. Forum reviewers had some concerns about these conclusions, as they point out that no dose-response relation between alcohol and colorectal cancer was shown in either period, and in data since 1998 no significant relation is seen between alcohol and such cancers. In fact, the authors of the present study state: “We also examined drinking pattern in relation to colorectal cancer risk; neither frequency of drinking nor quantity of drinking was associated with the risk of colorectal cancer;” they do not report their data upon which that statement is based.
Overall, the present paper does not answer the question as to the extent to which alcohol may relate to the risk of colorectal cancer, or if folate intake may modify any relation that may exist. Given that colorectal cancer (and breast cancer in women) are so common, it is important to evaluate how dietary folate and other nutrients may relate to such cancers. Further research on the relation of alcohol to these cancers, and potentially modifying factors, is greatly needed.
Reference: Nan H, Lee JE, Rimm EB, Fuchs CS, Giovannucci EL, Cho E. Prospective study of alcohol consumption and the risk of colorectal cancer before and after folic acid fortification in the United States. Annals of Epidemiology 2013;23:558-563.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 124: The J-shaped curve for the relation of alcohol consumption to mortality — 17 September 2013
An analysis based on data from more than 110,000 subjects in the USA, of whom 3,364 died during a follow-up period of up to 9 years, was used to evaluate the relation of “heavy drinking” and “nonheavy drinking” to the risk of all-cause mortality. The authors defined heavy drinking as 5 or more drinks/occasion, and recorded the frequency in which subjects consumed such amounts. Subjects consuming < 5 drinks/occasion were classified as nonheavy drinkers.
The key findings of the analyses were that there was a positive and linear increase in risk of mortality for subjects consuming heavy amounts of alcohol, with the risk increasing as drinking at this level was more frequent. For nonheavy drinkers, there was a J-shaped relation with mortality. The point at which the nonheavy drinkers’ risk of mortality exceeded that of abstainers was between 4 and 5 drinking occasions/week.
Forum reviewers thought that this was a well-done analysis that emphasizes the importance of the pattern of drinking, and not just the average weekly intake. Although the upper limits of drinks/occasion exceeded that usually considered as “moderate,” a J-shaped curve between alcohol and mortality for these drinkers was demonstrated. This is the pattern usually seen in prospective epidemiologic studies when “moderate” is defined at somewhat lower levels of alcohol intake.
Forum reviewers agreed with the conclusions of the authors regarding the importance of considering the pattern of drinking when evaluating the health effects of alcohol. The authors concluded: “Promoting less harmful drinking patterns by reducing heavy drinking frequency is an appropriate harm reduction strategy, and assessing drinking pattern by determining the frequency of heavy and nonheavy drinking is a simple and fast way to determine risk and promote less risky drinking behavior.”
Reference: Plunk AD, Syed-Mohammed H, Cavazos-Rehg P, Bierut LJ, Grucza RA. Alcohol consumption, heavy drinking, and mortality: Rethinking the J-shaped curve. Alcohol Clin Exp Res 2013;pre-publication: DOI: 10.1111/acer.12250
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 123: Alcohol consumption and lymphoid and myeloid neoplasms — 5 September 2013
Many prospective studies have shown that moderate drinkers are at lower risk of certain types of lymphoid cancer. For example, a report in 2009 from the Million Women’s Study in the UK found that alcohol consumption showed a significant inverse association with the occurrence of non-Hodgkin lymphoma (NHL). Further, a 2012 paper from that study based on 9,162 incident cases of haematological malignancy, including 7,047 lymphoid and 2,072 myeloid cancers, concluded: “Among predominantly moderate alcohol drinkers, higher intake was associated with lower risk of lymphoid malignancies.” Those investigators did not find a significant effect of alcohol on the risk of myeloid tumors, such as acute myeloid leukemia. Another 2012 paper based on almost 2,000 cases of Non-Hodgkin Lymphoma concluded: “In summary, findings from the prospective study presented here support the hypothesis that alcohol intake might be associated with a reduced risk of NHL.”
The authors of the present paper from the Netherlands, based on 17.3 years of follow up with 1,375 cases of lymphoid and 245 cases of myeloid neoplasms, did not find a statistically significant reduction in the risk of lymphoid cancers, and the authors suggest: “If any association between alcohol consumption and lymphoid neoplasms exists, our study suggests an increased risk rather than a decreased risk.”
While reasons for this difference in results of this study when compared with other recent studies may be used to better understand the association between alcohol and such cancers, Forum reviewers were concerned about a number of aspects of this study. For example, the authors had data on alcohol consumption only at baseline for this very long (17+ year) follow up, so changes (either increases or decreases in intake) were not known. Further, the key relations reported were not adjusted for a large number of potentially confounding variables, such as a positive family history of hematological cancer. (The authors state that they carried out such multivariable analyses but do not present the data.) Of even more concern was the apparent inverse effect of alcohol on cancer risk for a number of types of tumors when dose-response relations were shown.
Given the rather consistent findings in other very large studies of hematological malignancies that the risk of many types of lymphoid cancer may be reduced by alcohol, and inconsistencies in the results of the present analyses, it is difficult to conclude that the present paper should change our current interpretation of the association between alcohol and these types of cancer.
Forum members look forward to reports from other prospective studies on this topic. For the present, however, the overwhelming scientific evidence suggests that moderate alcohol consumption is associated with a decrease in the risk of many types of lymphoid malignancies, but has little effect on myeloid cancers.
Reference: Heinen MM, Verhage BAJ, Schouten LJ, Goldbohm RA, Schouten HC, van den Brandt PA. Alcohol consumption and risk of lymphoid and myeloid neoplasms: Results of the Netherlands cohort study. Int J Cancer 2013l133:1701–1713.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 122: Does moderate wine consumption lower the risk of developing depression? — 3 September 2013
There is a large literature relating heavy alcohol consumption to depression: most studies show that heavy drinkers tend to be depressed, and depressed people may self-medicate with large amounts of alcohol. This large prospective study of subjects at high risk of cardiovascular disease has shown that “moderate” drinkers, especially wine drinkers (the majority of their subjects), were at lower risk of developing depression during 7 years of follow up than were non-drinkers. An important aspect of this study is indeed that the analyses were based on moderate drinkers, as people exceeding certain amounts of alcohol or testing positive on the CAGE questionnaire (a measure of alcohol misuse) were excluded.
Strengths of the study include it being a large prospective study, with more than 5,000 subjects, aged 55-80 years at baseline, who were followed for up to 7 years for the initial development of clinical depression (which was diagnosed in 443 instances). Especially important was the ability of the investigators to have repeated assessments of alcohol consumption, every two years. A rather complete list of potentially confounding variables was available. The key findings of the study were that subjects reporting >5-15 grams/day of total alcohol intake, and wine drinkers of 2-7 drinks/week, were at a lower risk of developing depression than were non drinkers.
Some Forum members remained concerned that there may have been residual confounding by other lifestyle habits, and that the results may apply primarily to subjects who are also following a Mediterranean-type diet and lifestyle. Also, data were not available to evaluate the relation of heavy drinking or alcoholism to depression. However, the authors provide good scientific support for their conclusions that subjects reporting >5-15 grams/day of total alcohol intake (from about ½ to 1 ½ of a typical drink), and wine drinkers of 2-7 drinks/week, are at approximately 30% lower risk of developing depression than are abstainers of alcohol.
Reference: Gea A, Beunza JJ, Estruch R, et al (17 authors). Alcohol intake, wine consumption and the development of depression: the PREDIMED study. BMC Medicine 2013. Advanced publication, released 29 August 2013.
For the full critique of this paper by members of the International scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 121: Differences between wine and other alcoholic beverages in terms of adverse consequences of alcohol consumption – 22 August 2013
Questionnaire-based data on alcohol consumption were collected from more than 5,000 military recruits in Switzerland, who had a mean age of just over 19 years. There were very few drinkers who averaged more than 21 drinks/week, so the emphasis was on the effects of what is usually referred to as “binge drinking,” defined in this study as the consumption of 6 or more typical drinks (a drink containing 10-12 g of alcohol) on a single occasion. The “preference” of one particular type of beverage was based on the subject indicating that it made up more than two-thirds of his total alcohol consumption. The specific type of beverage preferred — beer, wine, or “other beverages” (the latter including apertifs, “pops,” chillers, and coolers) — was related to the pattern of drinking (frequency of binge drinking) and to the reported occurrence of adverse alcohol-related consequences (e.g., blackouts, driving after heavy drinking, missing work due to drinking, accidents, unprotected sex, encounters with police).
The authors report: “Preference for beer was associated with risky drinking patterns and, comparable with a preference for strong alcohol, with the use of illicit substances (cannabis and other illicit drugs). In contrast, a preference for wine was associated with low-risk alcohol consumption and a reduced likelihood of experiencing at least four negative alcohol-related consequences or of daily cigarette smoking.” More frequent binge drinking of any beverage was strongly associated with an increase in adverse alcohol-related consequences.
Forum reviewers thought that the adverse outcomes, especially those related to heavy beer intake, tend to characterize a particular subculture that demonstrates problematic substance use due to personal characteristics of the subjects. The unhealthy outcomes may be a feature more of the cultural habits of the subjects rather than just due to the type of beverage they consume most frequently.
The authors conclude that strategies for preventing problems with alcohol abuse should attempt to reduce excessive drinking of all types of beverages. However, they add: “to lessen the additional negative effects of beer and strong alcohol, which are particularly cheap in Switzerland, targeted strategies such as minimum pricing policies for these beverage types should be considered.” Forum members think that the extent to which such beverage-specific price restructuring would decrease unhealthy drinking practices among young people remains unclear.
Reference: Dey M, Gmel G, Studer J, Dermota P, Mohler-Kuo M. Beverage preferences and associated drinking patterns, consequences and other substance use behaviours. European Journal of Public Health 2013; advance access; doi:10.1093/eurpub/ckt109
For the full critique of this critique by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 120: Binge drinking impairs endothelial function in young people — 20 August 2013
The function of the vascular endothelium is a key process in the development of atherosclerosis and coronary heart disease, and extensive studies among middle-aged and elderly adults generally show beneficial effects of moderate drinking on vascular function. Whether or not alcohol consumption among young people has any lasting biological effects on cardiovascular risk is unclear: risk factors tend to track from childhood into adulthood, but specific long-lasting effects related only to drinking in young people are not known. Hence, data are currently not available to answer the question as to when during life people might consider beginning the moderate consumption of alcohol for the potential lowering of cardiovascular risk later in life.
The present study does not answer that question, as it only compares abstaining young people with binge drinkers, with the latter being defined as subjects reporting that they consumed ≥ 5 drinks in 2 hours for males, and ≥ 4 drinks in 2 hours for females. (The average number of binge-drinking episodes for these subjects was 6 ± 1 within the past month.) It does not compare abstainers with moderate drinkers. However, the paper does show that binge drinking among 18 – 25 year olds has adverse effects on endothelial function.
Forum reviewers were pleased to see this study, but point out that it is a cross-sectional analysis, and only compares binge drinkers with non-drinking young people. Further, inadequate data are presented to know the degree to which the results of the study may suffer from residual confounding from other factors.
The authors conclude that their study showed adverse effects on both microvascular and macrovascular function to be associated with frequent binge drinking in young people. It is hoped that these investigators, or others, will in the future provide data on the effects on vascular function of regular, moderate alcohol consumption among young people. It would also be interesting to learn if effects are different for high-polyphenol wine than for other beverages. Further, it will be important to determine how long beneficial or adverse effects on vascular function may persist, with or without continued alcohol intake.
Reference: Goslawski M, Piano MR, Bian J-T, Church EC, Szczurek M, Phillips SA. Binge drinking impairs vascular function in young adults. J Am Coll Cardiol 2013;62:201–207.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 119: A consensus statement on the association of moderate alcohol consumption and health — 13 August 2013
A group of Italian scientists has prepared a consensus paper to review the available evidence on the association between moderate alcohol use and health and disease. The report resulted from extensive discussions among 36 prominent Italian scientists, and provides a working document for the scientific and health professional communities. The report has been signed by 19 separate societies or federations in Italy, including societies in nutrition, cardiology, and general medicine, as well as organizations of scientists dealing with diabetes, hypertension, and obesity.
The consensus report ends with four conclusions:
“(1) In healthy adults and in the elderly, spontaneous consumption of alcoholic beverages within 30 g ethanol/d for men and 15 g/d for women is to be considered acceptable and do not deserve intervention by the primary care physician or the health professional in charge. In fact, there is no evidence to suggest complete abstention from alcohol drinking by moderate users.
(2) Patients with increased risk for specific diseases, for example women with familiar history of breast cancer, or subjects with familiar history of early CVD or cardiovascular patients should discuss their drinking habits with their physician.
(3) No abstainer should be advised to drink for health reasons.
(4) Alcohol use must be discouraged in specific physiological or personal situations or in selected age classes (children and adolescents, pregnant and lactating women and recovering alcoholics). Moreover, the possible interactions between alcohol and acute or chronic drug use must be discussed with the primary care physician.”
Forum reviewers considered this to be a well-done and generally well-balanced appraisal of the current literature on alcohol and health; it could help inform physicians and the general public about our current knowledge on this topic. However, Forum reviewers were concerned by several aspects of the report where it appeared that the conclusions were more “political” than “scientific” (perhaps necessary to gain the support of all of the societies endorsing the report).
The authors of the report provided good data to support their first two conclusions, and recent publications that were not available to the authors at the time they prepared their report strongly support these conclusions. However, Forum members found little data provided in the paper to support the third statement in their summary; in fact, the information the authors presented in the text would tend to support the opposite conclusion. Further, while it may be correct, their fourth conclusion was not supported by scientific data in the paper.
Forum members agreed that the importance of the effects of alcohol consumption on total mortality must always be considered, and agreed with the statement of the authors that “Low levels of alcohol intake (1-2 drinks per day for women and 2-4 drinks per day for men) are inversely associated with total mortality in both men and women.”
Key areas that the Forum believed could have been given more emphasis related to the association between alcohol and diabetes mellitus, where data strongly support an approximately 30% lower risk for moderate drinkers, in comparison with non-drinkers. And the risk of cardiovascular disease is considerably reduced among diabetics who consume alcohol moderately. And the potential effects of moderate drinking on reducing the risk of congestive heart failure, a rapidly increasing health problem related to ageing of the population, were not discussed. Forum members also wished that more emphasis had been given in the consensus report to the pattern of drinking: current data indicate that regular moderate drinking, rather than binge drinking, is the pattern associated with the most favorable health outcomes.
Overall, this consensus report is an important and useful addition to the scientific literature on the relation of moderate alcohol consumption to a variety of health outcomes. It could be of great values to physicians and policy makers when providing advice to the public regarding the effects of alcohol on health.
Reference: Poli A, Marangoni F, Avogaro A . . . de Gaetano G . . . et al (total of 36 authors). Moderate alcohol use and health: A consensus document. Nutrition, Metabolism, & Cardiovasular Disease 2013;23:487-504.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 118: Clustering of alcohol consumption with socioeconomic and biologic risk factors for cancer — 30 July 2013
It has been shown in most previous studies that moderate drinkers, especially those who generally consume wine, tend to have other “moderate” lifestyle factors. For example, they tend to be better educated, of higher socio-economic status, and generally are more active and eat a healthier diet than non-drinkers. An exception is cigarette smoking, which tends to be more common in drinkers than in abstainers. Epidemiologists studying alcohol and health are always striving to adjust appropriately for other lifestyle factors, attempting to assure that the difference in health outcomes among subjects relates to their drinking, and not to associated lifestyle factors.
In the present study, the investigators related alcohol consumption to a large number of socio-demographic and lifestyle factors that relate to the risk of cancer. They report that several factors were associated with alcohol consumption ≥10g/d in both genders: older age, smoking, higher socio-demographic category, higher income, and less healthy dietary intakes. Other factors were associated with alcohol consumption differently for men and women. The authors then report that the total number of such factors was higher among consumers of ≥10g/d of alcohol than among abstainers or lighter drinkers. They conclude: “The multiplicity of deleterious lifestyle behaviours combined with alcohol drinking must be taken into account in cancer prevention efforts. Gender-specific medical advice for people with personal or family history of alcohol-related diseases, including cancer, should be strengthened.”
While Forum reviewers found the data presented in this paper to be of interest, they did not believe that simply adding up all adverse risk factors provided useful information for the prevention of cancer. It is well known that smoking is a major risk factor for certain cancers, and in almost all studies alcohol consumers are more likely to be smokers; hence, drinkers should certainly be advised about the dangers of smoking. On the other hand, by simply summing the number of factors into a total score, the authors included a number of risk factors for which there is less of a scientific basis for their effect on cancer risk (e.g, the intake of supplements). Such factors should not be given the same weight as smoking as risk factors for cancer. Further, this study was carried out among computer-literate volunteers, so it may have limited relevance for the general population.
There have been extensive data showing that “healthy” and “unhealthy” lifestyle factors tend to cluster: for example, light-to-moderate drinkers tend to be leaner and eat a healthier diet than non-drinkers or heavy drinkers, as shown in this study. However, the prevention of chronic diseases relates to a large number of behaviors, and alcohol consumption cannot be considered as an isolated factor. Current epidemiologic data suggest that the combination of not smoking, being physically active, eating a healthy diet, avoiding obesity, and, unless contraindicated, regularly consuming small amounts of an alcoholic beverage, together make up what can be defined as a “healthy lifestyle.”
Reference: Touvier M, Druesne-Pecollo N, Kesse-Guyot E, Andreeva VA, Galan P, Hercberg S, Latino-Martel P. Demographic, socioeconomic, disease history, dietary and lifestyle cancer risk factors associated with alcohol consumption. Int J Cancer 2013;in press
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 117: Changes in alcohol intake modify levels of fibrinogen, an important risk factor for coronary heart disease — 18 July 2013
A prospective analysis of data from 2,520 subjects in the Coronary Artery Risk Development in Young Adults Study (CARDIA) cohort related reported alcohol intake at two examinations, 13 years apart, to levels of fibrinogen on the two occasions. Fibrinogen is a strong determinant of thrombosis, and is an important risk factor for coronary heart disease. The authors report that, in comparison with participants who never drank, those who became/stayed drinkers had smaller increases in fibrinogen, while those who quit drinking had the highest increase in fibrinogen over 13 years of follow-up. They conclude that lower levels of fibrinogen may be a key mechanism for the established protective effect of moderate alcohol intake on cardiovascular disease outcomes.
Forum reviewers considered this to be a potentially important paper, as the finding of higher fibrinogen among never drinkers and those who quit drinking may relate to the higher risk of coronary disease commonly reported from such subjects in prospective studies. However, the reviewers point out that the reasons that subjects quit drinking are not known (although the authors did adjust for conditions related to quitting drinking). Further, blood clotting factors other than fibrinogen may be affected by changes in alcohol consumption, and they were not reported in this paper. More research will be needed to determine if changes in fibrinogen levels are key elements in alcohol’s effects on cardiovascular disease.
Reference: Okwuosa TM, Klein O, Chan C, Schreiner P, Liu K, Green D. Long-term change in alcohol-consumption status and variations in fibrinogen levels: the coronary artery risk development in young adults (CARDIA) study. BMJ Open 2013;3:e002944. doi:10.1136/bmjopen-2013-002944
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 116: Effects of genetic factors on the metabolism of alcohol — 10 July 2013
A summary paper on genetically determined mechanisms related to the metabolism of alcohol and acetaldehyde describes numerous ways that the metabolism, especially of acetaldehyde, may be modified, both in the periphery of the body and in the brain. Individuals with a mutation of the aldehyde dehydrogenase gene (the ALDH2*2 allele), and certain other genetically determined enzymes, do not tolerate alcohol and are much less likely to become alcohol abusers. The authors state that their studies suggest possible therapeutic avenues in the treatment of alcoholism.
Reference: Israel Y, Rivera-Meza M, Karahanian E, Quintanilla ME, Tampier L, Morales P, Herrera-Marschitz M. Gene specific modifications unravel ethanol and acetaldehyde actions. Front Behav Neurosci 2013;7:80.doi:10.3389/fnbeh.2013.00080
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 115: Potential association of alcohol consumption with diverticulosis — 25 June 2013
The etiology of diverticulosis of the colon is poorly understood. Many, but not all, studies suggest that low fiber intake and obesity increase the risk; few studies have evaluated the relation of alcohol consumption and diverticulosis, with inconclusive results. This paper tests the cross-sectional association of alcohol consumption with diverticulosis among 746 asymptomatic consecutive subjects undergoing screening colonoscopies in Lebanon.
One-half of the subjects in this study were abstainers. Most of the “drinkers” stated that they consumed alcohol occasionally or < 1 drink/day; only about 10% reported 1 or more drinks/day, and no data on type of beverage or pattern of drinking were available. Nevertheless, from their analyses the authors conclude that alcohol consumption raises the risk of diverticulosis.
Forum members considered that this cross-sectional analysis provides little support for a causative effect of alcohol on the risk of diverticulosis. Most larger observational studies have not shown such an effect. In the present study, about 90% of subjects were either abstainers or consumed alcohol only occasionally or averaged < 1 drink/day. Further, the investigators did not evaluate the pattern of drinking (including binge drinking) and the results do not support an increase in risk with greater drinking (lack of a dose-response relation). Mechanisms for such an effect are largely unknown. Thus, few of the Hill criteria for “causality” are met.
The authors’ use of an inter-country comparison of per-capita alcohol intake and reported diverticulosis has no relevance: there are large cultural differences between nations with high and those with low per-capita alcohol intake, and alcohol use may well have been just a marker for a western-type culture. While the present study could be used to generate an hypothesis of a relation of alcohol intake to diverticulosis, attempts to validate such an association will require much additional research.
Reference: Sharara AI, El-Halabi MM, Mansour NM, Malli A, Ghaith OA, Hashash JG, Maasri K, Soweid A, Barada K, Mourad FH, El Zahabi L. Alcohol consumption is a risk factor for colonic diverticulosis. J Clin Gastroenterol 2013;47:420–425.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 113: Metabolic and biochemical mechanisms by which alcohol consumption affects health — 11 June 2013
A large study from Australia, that included a high percentage of current or former alcohol abusers, related alcohol consumption with a variety of metabolic and biologic parameters that relate to health. Included were markers of lipid function, inflammation, glucose metabolism, and liver function. As expected, there was a linear increase in HDL-cholesterol with increasing alcohol intake; somewhat surprisingly, there was a linear decrease in insulin levels with increasing alcohol consumption (which may relate to the typical finding of a significantly lower risk of diabetes mellitus among moderate drinkers). Essentially all of the other factors showed a “J-shaped” or “U-shaped” relation with alcohol: a decrease with small to moderate amounts of alcohol and an increase with larger intake.
In their association with alcohol, the lowest (most favorable) values of parameters varied by the measure: lowest triglycerides at about 1 to 2 drinks per day, lowest CRP at about 1 drink/day, lowest blood sugar and lowest alkaline phosphatase values at 1 to 3 drinks/day. Adverse effects on liver enzymes, blood glucose, and inflammatory markers showed a threshold level of intake that varied somewhat by marker. For example, reported non-drinkers had higher values of CRP, triglycerides, and alkaline phosphatase; among drinkers, significant increases were seen only in consumers of 40 or more drinks/week. Unfortunately, the investigators did not report on the pattern of drinking, which usually shows preferable results from regular, moderate intake of alcohol with no binge drinking.
The key findings of the study can be summarized as favorable effects of moderate alcohol intake on HDL-cholesterol and insulin levels, and for most other factors (including liver enzymes, triglycerides, blood glucose, and the inflammatory marker CRP), a “J-shaped” relation: lower values with light drinking and higher values with larger amounts of alcohol. For most of these, there was either no effect or a favorable effect until alcohol intake exceeded a “threshold value,” at which heavier drinking began to show adverse effects.
Forum reviewers agreed with the conclusion of the authors: “The pattern of potentially beneficial effects of alcohol on HDL-C and insulin increasing progressively as consumption increases, whereas the negative effects show thresholds, is consistent with net U- or J-shaped effects of alcohol on health.” While actual health outcomes were not evaluated in this study, overall it provides strong support for the results of most prospective epidemiologic studies that show lower rates of cardiovascular and other diseases among light-to-moderate drinkers than among abstainers or heavy drinkers.
Reference: Whitfield JB, Heath AC, Madden PAF, Pergadia ML, Montgomery GW, Martin NG. Metabolic and biochemical effects of low-to-moderate alcohol consumption. Alcohol Clin Exp Res 2013;37:575–586.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 112: Relation of alcohol intake to risk of dying from cancer — 23 May 2013
This paper presents a meta-analysis that related alcohol consumption to all-cancer mortality; it was based on almost 50,000 deaths reported in the literature from prospective cohort studies. Forum reviewers had some concerns about the conclusions of the paper, based on some discrepancies in the text, the lack of data on drinking pattern, no beverage-specific results, etc. Nevertheless, as expected, the reported average consumption of 50 or more grams of alcohol per day (equivalent to 4 or more typical drinks each day) was associated with an estimated 32% increased risk of dying from cancer.
However, there was no increase in the estimated risk of cancer death for subjects classified as “moderate” drinkers (defined by the authors using a wide range of intake: 12.6 to 49.9 grams/day, the equivalent of up to approximately 4 or more typical drinks). Further, Forum members were surprised that a slight but statistically significant decrease in cancer mortality risk was seen for “light” drinkers (those reporting an average of ≤ 12.5 grams/day, or about one typical drink). Forum members appreciated that misclassification of cause of death or residual confounding could have contributed to this latter result.
It is especially important that the only significant increase in risk in cancer mortality among the almost 50,000 cancer deaths reported in this meta-analysis was for consumers of 50 grams or more of alcohol. This suggests strongly that the overall risk of cancer mortality related to alcohol consumption is primarily (perhaps almost exclusively) from heavier drinking. Certainly, the findings from this study do not support the premise that “any amount of alcohol increases the overall risk of dying from cancer.”
Reference: Jin M, Cai S, Guo J, Zhu Y, Li M, Yu Y, Zhang S, Chen K. Alcohol drinking and all cancer mortality: a meta-analysis. Ann Oncol 2013;24:807-816. doi: 10.1093/annonc/mds508.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 111: Association of alcohol consumption with a measure of osteoporosis in elderly women — 7 May 2013
The density of bones, measured as bone mineral density (BMD), is strongly related to osteoporosis. Elderly women with osteoporosis, in particular, are at increased risk of fractures of the hip, arm, and spine; such fractures often relate to severe disability. With data on alcohol collected as part of a clinical trial on the prevention of osteoporosis, investigators in Finland have related alcohol consumption to changes over three years in BMD. After those excluded due to incomplete data, data on 300 women were available for analysis. The majority of women were abstainers or consumed little alcohol. Nevertheless, the results support much earlier research: regular, moderate drinking is associated with higher levels of BMD (i.e., lower risk of osteoporotic fractures) than is abstinence.
Forum reviewers, as did the authors, noted a number of limitations of the study: a rather small cohort with a very low intake of alcohol, a short duration of follow up, and rather small differences according to whether the women consumed alcohol or not.
Data from European surveys have shown that women in Finland tend to have high levels of osteoporosis and to drink very little; hence the increase in BMD associated with alcohol intake, even though slight, could be important in this population. Over the past three decades, there has been an increase in alcohol consumption in Finland, especially a marked increase in the consumption of wine. Hence, some Forum reviewers thought that the improvement in BMD among drinkers in this study may have been primarily from wine (which may have additional components, other than alcohol, that relate to BMD). However, the number of subjects was not large enough to test this hypothesis in the present study. Overall, this study supports the premise that moderate alcohol intake, along with an adequate calcium intake and vitamin D and exercise, may have a favorable influence on the risk of developing osteoporosis
Reference: Sommer I, Erkkilä AT, Järvinen R, Mursu J, Sirola J, Jurvelin JS, Kröger H, Tuppurainen M. Alcohol consumption and bone mineral density in elderly women. Public Health Nutr 2013;16:704-712. doi: 10.1017/S136898001200331X.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 110: Divergent effects of regular moderate and binge drinking – 30 April 2013
The present study relates alcohol consumption measured in young to middle-aged adults to mortality over a follow-up period of 20 years. The analyses are based on data from a large population in a region of Norway where the alcohol drinking pattern most commonly reported was binge drinking on infrequent occasions. Previous research has demonstrated that a very different drinking pattern – the frequent consumption of small amounts of alcohol – is generally considered to be the pattern associated with most health benefits.
In the present study, both men and women who reported consuming alcohol up to twice a month had about 20% lower mortality than did abstainers. All groups reporting binge drinking had higher mortality than non-binge drinkers (which was statistically significant for men and had a similar estimated effect among women). Cardiovascular and ischemic heart disease mortality had similar patterns as total mortality, being lower among drinkers but higher among those who reported binge drinking.
The key finding of this study is that there are divergent effects on mortality of the frequency of drinking and the amount of alcohol consumed per occasion. While the results for this study may reflect a certain Northern European pattern of drinking (not frequent but heavy on each occasion), they may not apply to other European or North American populations, where drinking is more frequent but binge drinking less common. Nevertheless, the results of this study support results typically found in more moderately drinking populations: more frequent drinking, but smaller amounts per occasion, is the pattern of alcohol consumption associated with the lowest risk of mortality. Both aspects of drinking must be considered when studying the relation of alcohol to mortality.
Reference: Graff-Iversen S, Jansen MD, Hoff DA, Høiseth G, Knudsen GP, Magnus P, Mørland J, Normann PT, Næss ØE, Tambs K. Divergent associations of drinking frequency and binge consumption of alcohol with mortality within the same cohort. J Epidemiol Community Health 2013;67:350-357. doi:10.1136/jech-2012-201564.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 109: In women developing breast cancer, moderate alcohol consumption before or after diagnosis does not increase breast cancer mortality and decreases total mortality — 16 April 2013
Most previous research has shown a slight increase in the risk of breast cancer (BrCa) among women who consume alcohol (versus nondrinkers), even among those whose average is only one drink/day. The association with death due to breast cancer is less clear, although overall total mortality among moderate drinkers is almost always lower than among non-drinkers; this reduction is generally attributed to a lower risk of cardiovascular disease.
The present study related alcohol consumption, both prior to the diagnosis of BrCa and after the diagnosis, with survival; deaths from BrCa and from cardiovascular disease, as well as total mortality, were related to alcohol intake. Specifically, in this study the authors assessed alcohol intake in a cohort of 22,890 women with incident invasive breast cancer (BrCa) who were residents of one of four US states and diagnosed at ages 20 to 79 years. During a median follow-up period of 11.3 years after diagnosis of BrCa, 7,780 deaths occurred, including 3,484 attributed to breast cancer.
Based on a quadratic analysis, moderate alcohol consumption before diagnosis showed a tendency towards lower risk of death from BrCa, and a significantly greater reduction in the risk of cardiovascular disease mortality and total mortality. Alcohol consumption after diagnosis was not associated with disease-specific survival, but was associated with a lower risk of total mortality. For women consuming alcohol prior to the diagnosis of BrCa, those who decreased their intake showed little effect on mortality, while those who increased their intake showed further lowering of their risk of cardiovascular and total mortality.
Forum reviewers considered this to be an excellent paper providing important new data on the association of alcohol consumption with survival after a diagnosis of invasive breast cancer. They thought that the statements of the authors accurately reflected their data, as they concluded: “Overall alcohol consumption before diagnosis was not associated with disease-specific survival, but we found a suggestion favoring moderate consumption. There was no evidence for an association with postdiagnosis alcohol intake and breast cancer survival. This study, however, does provide support for a benefit of limited alcohol intake for cardiovascular and overall survival in women with breast cancer.”
An accompanying editorial* agreed with the conclusions of the authors. The editorial stated, “Based on the best available evidence, including [the present report], it appears that modest alcohol consumption after breast cancer diagnosis, up to approximately one drink per day on average, may be associated with optimal overall survival, without compromising breast cancer-specific survival.”
*Demark-Wahnefried W. To your health: How does the latest research on alcohol and breast cancer inform clinical practice? jco.ascopubs.org/cgi/doi/10.1200/JCO.2013.490466),
Reference: Newcomb PA, Kampman E, Trentham-Dietz A, Egan KM, Titus LJ, Baron JA, Hampton JM, Passarelli MN, Willett WC. Alcohol consumption before and after breast cancer diagnosis: Associations with survival from breast cancer, cardiovascular disease, and other causes. J Clin Oncol 2013; pre-publication. Available at jco.ascopubs.org/cgi/doi/10.1200/JCO.2012.46.5765
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 108: An unusual paper relating alcohol consumption to the risk of stroke
Numerous well-done prospective epidemiologic studies have shown that while heavy drinking may increase the risk of stroke, light-to-moderate alcohol consumption is usually associated with a significant decrease in the risk of the most common type of stroke, ischemic stroke.
This paper from investigators in Finland states that it was designed to relate alcohol consumption and obesity to the risk of ischemic stroke. Unfortunately, even though it has clearly been shown that the amount and pattern of alcohol consumption strongly modify the effect on the risk of stroke, for some unknown reason the authors have grouped all consumers of alcohol into a single group. Specifically, there are no data given that describe the relation of light-to-moderate alcohol consumption with stroke. Hence, the conclusion of the authors that “alcohol increases the risk of stroke” is not supported by the data presented. In the opinion of members of the Forum, without reporting the effects according to the amount of alcohol consumed or the pattern of drinking, this is an unsupported and potentially dangerous statement to present in a scientific journal.
Reference: Rantakömi SH, Laukkanen JA, Sivenius J, Kauhanen J, Kurl S. Alcohol consumption and the risk of stroke among hypertensive and overweight men. J Neurol 2013;260:534–539. DOI 10.1007/s00415-012-6672-6
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 107: Little effect on child’s mental functioning associated with mother’s light, occasional drinking in early pregnancy – 25 March 2013
A new report from the prospective, population-based Avon Longitudinal Study of Parents and Children (ALSPAC) in the UK is based on investigation of the association between light drinking in pregnancy (<1 glass per week in the first trimester) and child mental health. Mental health was assessed in more than 6,000 children using both parent- and teacher-rated Strengths and Difficulties Questionnaires (SDQs) at age 11 years. Academic outcomes based on Key Stage 2 examination results were measured in more than 10,000 children.
Approximately 40% of women consumed some alcohol but less than 1 glass/week, while 16% reported consuming ≥1 glass per week during the first trimester. The authors report that after adjustment, relative to abstainers, there was no effect of light drinking on teacher-rated scores or examination results. In girls, although there was a suggestion of worse outcomes on the parent-rated total score in those exposed to light drinking compared to abstainers, no dose–response relationship was evident. The authors conclude: “Light drinking in pregnancy does not appear to be associated with clinically important adverse effects for mental health and academic outcomes at the age of 11 years.”
Forum reviewers considered this to be a well-done study, with a balanced assessment of results by the authors. Reviewers were surprised at the somewhat arbitrary separation of alcohol consumption: <1 drink per week versus ≥1 drink per week. Current guidance about alcohol consumption in pregnancy from the Department of Health in England (2009) allows for pregnant women to drink up to 1–2 units of alcohol once or twice a week, and it would have been preferable to have data presented for drinkers at this level.
Forum Co-Director Conibear considered that “The most important aspect of this study relates to the fact that 25% of babies in the UK are unplanned, and 17% of mothers do not know they are pregnant until eight weeks or more. Therefore balanced advice concerning the effect of alcohol use in early pregnancy is crucial to prevent unnecessary concern amongst this group of mothers to be. Although the best advice is to avoid alcohol if you are pregnant, the present research can reassure mothers who drank occasionally without realising that they were pregnant that they have not done long-term harm to their baby.”
Forum reviewer Stockley added: “I think that another important message is that if a woman decides to consume a small amount of alcohol during pregnancy, she should never binge drink or get drunk. This we know can have adverse effects on the developing fetus, especially in the first trimester, but interestingly, also in the third trimester of pregnancy.”
Reference: Sayal K, Draper ES, Fraser R, Barrow M, Davey Smith G, Gray R. Light drinking in pregnancy and mid-childhood mental health and learning outcomes. Arch Dis Child 2013;98:107–111. doi:10.1136/archdischild-2012-302436.
For the full critique of this publication by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 106: A clinical trial shows that glucose metabolism is improved more by red wine than by gin — 14 March 2013
To compare the effects of moderate consumption of red wine, dealcoholized red wine, and gin on glucose metabolism and the lipid profile, a group of Spanish investigators carried out a randomized control trial among 67 men at high cardiovascular risk. All received each of red wine (30 g alcohol/d), the equivalent amount of dealcoholized red wine, and gin (30 g alcohol/d) for 4 week periods, in a randomized order. While fasting glucose levels were not affected, mean adjusted plasma insulin and HOMA-IR decreased after red wine and dealcoholized red wine, but not after gin. HDL cholesterol, Apolipoprotein A-I and A-II increased after red wine and gin. Lipoprotein(a) decreased after the red wine intervention. The authors conclude that their results support a beneficial effect of the non-alcoholic fraction of red wine (mainly polyphenols) on insulin resistance, thus greater protective effects on cardiovascular disease from red wine than from other alcoholic beverages.
Forum members were unanimous in considering this to be a very well-done and important trial. It supports a huge amount of observational data from epidemiologic cohort studies that have shown that subjects who consume moderate amounts of alcohol tend to have much lower risk of developing diabetes. Further, patients with diabetes who drink moderately have much lower risk of subsequent cardiovascular disease and lower mortality. Studies such as this one help scientists understand the mechanisms by which moderate drinking, especially of wine, can reduce the risk of metabolic and vascular diseases.
Reference: Chiva-Blanch G, Urpi-Sarda M, Ros E, Valderas-Martinez P, Casas R, Arranz S, Guillén M, Lamuela-Raventós RM, Llorach R, Andres-Lacueva C, Estruch R. Effects of red wine polyphenols and alcohol on glucose metabolism and the lipid profile: A randomized clinical trial. Clinical Nutrition 2013. Pre-publication. dx.doi.org/10.1016/j.clnu.2012.08.022.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 105: For preventing cardiovascular disease, an unrestricted-calorie Mediterranean-type diet provides 30% more benefit than a low-fat diet: Results of a large population-based clinical trial — 6 March 2013
A large well-done clinical trial in Spain was carried out among 7,447 subjects at high-risk of cardiovascular disease (on the basis of diabetes, hypertension, dyslipidemia, and other risk factors). The trial compared the effects of two versions of an energy-unrestricted Mediterranean-type diet, one with large amounts of extra-virgin olive oil (EVOO) and one with a supplement of mixed nuts, with results among subjects in a “control group,” made up of subjects who were advised to follow a low-fat, low-cholesterol diet (that has typically been recommended for reducing the risk of cardiovascular disease).
Both of the groups advised to consume a Med-Diet showed an increase in total fat, from an average of 39.3 % of total calories to an average of more than 41%; the group advised to decrease their total fat lowered their intake from 39 to 37 % of calories. All three groups showed slight decreases in saturated fat and slight decreases in dietary cholesterol intake (but blood cholesterol levels were not reported). Only the Med-Diet + nuts group showed an increase in alpha-linolenic acid (ALA), the fatty acid related to the lowest risk of cardiovascular disease in the Cretan cohort of the Seven-Countries Study and in the Lyon Diet-Heart Study.
The large majority of subjects in all groups consumed wine at baseline, and about one-third of the Med-Diet groups and one-quarter of the control group reported consuming ≥ 7 glasses of wine/week during the trial. However, alcohol consumption was not evaluated specifically for its effects in the present study.
The study was ended early by its data and safety monitoring board due to marked advantages being shown in terms of the occurrence of the primary end-point (the occurrence of myocardial infarction, stroke, or death from cardiovascular causes) in both Med-Diet groups in comparison with the control group. The multivariable-adjusted hazard ratios were 0.70 and 0.72 for the Med-Diet with olive oil and the Med-Diet with added nuts, hence an approximately 30% decrease in risk among subjects assigned to a Med-Diet compared with those in the control group.
Forum members (as did the authors) had difficulty in determining which specific components of the Med-Diet may have been the primary reasons for its more favorable results, as significant dietary changes during the trial were mainly related to the supplementary olive oil or nuts given to subjects in the two Med-Diet groups. Among potential factors were increased mono-unsaturated fat and higher antioxidants from the added EVOO and an increase in ALA from the supplemental nuts. Forum members noted that the Med-Diet interventions apparently did not provide an increase in the intake of ALA, which could have led to even more protection against cardiovascular disease.
In any case, the striking reduction in risk shown in the study from the Med-Diet provide further evidence of the effectiveness of such a diet in reducing cardiovascular disease. It has been shown repeatedly that people advised to consume a Mediterranean-type diet tend to comply much better with such advice than do people advised mainly to decrease their intake of all fats and cholesterol. A very large amount of scientific data now support advice to follow a Mediterranean-type diet, one that does not restrict calories but encourages the intake of selected fats (which may include extra-virgin olive oil or canola oil), as well as more fruits, vegetables, grains, nuts, and wine; it may be the most effective dietary approach for reducing cardiovascular disease.
Reviewer Keil points out that many good prospective cohort studies have shown that an increase in adherence to components of a Mediterranean-type diet decreases the risk of many diseases and mortality. He adds: “The great thing about the present study is that when the skeptics raise their voice and argue that the proponents of the Mediterranean diet have only observational data available, we can now respond that we not only have RCT data on secondary prevention (Lyon Diet-Heart study) but also the present study on primary prevention of cardiovascular disease.”
Reference: Estruch R, Ros E, Salas-Salvadó J, Covas M-I, Corella D, Arós F, et al, for the PREDIMED Study Investigators. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 2013. DOI: 10.1056/NEJMoa1200303
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please clickhere.
===============================================================================
Critique 104: Moderate alcohol consumption is associated with a lower risk of diabetes — 26 February 2013
A population-based longitudinal study in Norway showed a lower risk of developing type II diabetes, and a tendency for less auto-immune diabetes, among subjects reporting moderate alcohol consumption. The lowest risk was among subjects reporting that they consumed alcohol 5-10 times during the previous two weeks or reporting a daily consumption of 10-15 grams of alcohol per day (slightly less than one to a little over one drink per day, using 12 g of alcohol per day as a “typical drink”).
The overall results from this study support most previous research showing a rather large (approximately 30% or more) reduction in the risk of Type II diabetes mellitus to be associated with moderate drinking. In this study, the strongest protective effect related to the consumption of wine, rather than beer or spirits. Unlike some previous research, the present study did not show an increased risk of diabetes among binge drinkers, heavier drinkers, those reporting episodes of intoxication, or those giving positive responses on a CAGE questionnaire (a measure of an alcohol use disorder). As it is likely that alcoholics were under-represented in the cohort, the ability to show the effects of very heavy drinking may have been limited.
While the numbers of subjects with auto-immune diabetes were small, there was a tendency seen for a similar reduction in risk with moderate drinking as with the much more common Type II diabetes. Overall, this study strongly supports much previous research showing that moderate alcohol consumption is associated with a lower risk of developing diabetes.
Reference: Rasouli B, Ahlbom A, Andersson T, Grill V, Midthjell K, Olsson L, Carlsson S. Alcohol consumption is associated with reduced risk of Type 2 diabetes and autoimmune diabetes in adults: results from the Nord-Trøndelag health study. Diabet Med 2013;30:56–64.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 103: Alcohol intake just prior to bed-time may affect your sleep patterns — 18 February 2013
A paper from experts in the science of sleep provides an excellent review of intervention studies since the 1980s on the effects of alcohol consumption on sleep. The study finds that the time required to fall asleep, and sleep patterns in the first part of the night, tend to be improved by alcohol. The authors conclude that “The onset of the first REM sleep period is significantly delayed at all doses and appears to be the most recognizable effect of alcohol on REM sleep, followed by the reduction in total night REM sleep.” Slow-wave sleep is more common and REM sleep less common after alcohol.
The studies reviewed in this report were intervention studies among mainly young normal subjects, not people with sleep disorders. Other studies have demonstrated that small amounts of alcohol given in the evening to the elderly may improve sleep, and reduce the need for sleep-inducing medications. Overall, the data reviewed in this paper suggest that small amounts of alcohol in the evening have few adverse effects on sleep, and relate to earlier onset of sleep and less awakening in the first part of the night. Larger amounts of alcohol tend to make the onset of sleep faster, but may have some adverse overall effects on sleep patterns, with a shorter duration of REM sleep throughout the night.
Reference: Ebrahim IO, Shapiro CM, Williams AJ, Fenwick PB. Alcohol and sleep I: Effects on normal sleep. Alcohol Clin Exp Res 2013;doi: 10.1111/acer.12006. [Epub ahead of print]
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Requested comments on paper by Nelson et al
by R. Curtis Ellison, MD, Professor of Medicine & Public Health,
Boston University School of Medicine
NOTE: These comments do not necessarily reflect the views of the members of the International Scientific Forum on Alcohol Research
Nelson DE, et al. Alcohol-attributable cancer deaths and years of potential life lost in the United States. Am J Pub Health, released February 14, 2013
We always welcome new scientific publications that help elucidate factors related to the development of cancer. The new paper by Nelson et al focuses on the role that alcohol consumption may play in the risk of a number of cancers.
Background: It has long been appreciated that there are a number of upper aero-digestive cancers, such as cancer of the mouth, throat, and esophagus, that occur much more frequently in heavy drinkers, especially alcoholics, than in abstainers. Physiologic studies suggest that these are not diseases of light to moderate drinkers, as a certain amount of alcohol is required to produce these diseases. Similarly, among people consuming enough alcohol to lead to liver cirrhosis, the risk of liver cancer is also markedly increased.
These “alcohol-related cancers” should be discussed separately from other more common cancers – especially colon cancer and female breast cancer – for which the risk may be only slightly increased by alcohol. In the case of breast cancer, there may be a slight increase in risk among some women consuming an average of only one drink/day (in some studies, such an increase in risk occurs primarily among women who binge drink, have an inadequate intake of folate, and/or are also on hormone replacement therapy.)
For these types of cancer, it is especially important to consider the net health effects of alcohol consumption. For example, it is estimated that if a woman at average risk of breast cancer (i.e., does not have such a cancer in a first-degree relative) decides to avoid drinking completely in hopes of reducing her risk of breast cancer, her risk of breast cancer would be expected to be slightly decreased, on average, by perhaps 5-10%; however, her risk would be increased of dying from much more common diseases such as heart attack, stroke, or other conditions for which small amounts of alcohol have been shown to reduce risk. And, importantly, her risk of dying of any cause (total mortality) would actually be increased by her avoiding light alcohol consumption.
The pattern of drinking has often been shown to be even more important than the average amount of alcohol consumed. A stronger association with beneficial effects is seen with the regular (up to daily) intake of small amounts of an alcoholic beverage; drinking larger amounts on fewer days (including binge drinking) is almost always associated with adverse health effects. For example, a man having up to 2 drinks each day would have an average of 14 drinks per week, generally considered to be within recommended guidelines. However, a man consuming 7 drinks on each of only two days each week, despite the same weekly average consumption, would not be considered to be a moderate drinker.
Comments on the present paper: There are a number of concerns about the analyses and conclusions of the authors of the present paper. These include the following:
(1) The authors have “corrected” the reported data on alcohol consumption to make up for presumed under-reporting, using a method not generally accepted by statisticians and other researchers. This means that even many “light” drinkers are listed as reporting greater amounts of alcohol.
(2) The authors do not clearly separate the effects of truly moderate drinking from heavier drinking in their conclusions. They use up to 20 grams of alcohol per day as their lowest drinking category; this is higher than the 14 g/day that is the current definition of responsible drinking for women in the US Guidelines. Further, as stated, if reported intakes are increased artificially, many more light drinkers would be bumped up into higher categories of drinking. The result of this mis-categorization is that bona fide moderate drinking, which has been shown by others to have no association with most types of cancer, is improperly associated in this study with increased cancer.
(3) The authors’ implications that even regular, moderate drinking increases the risk of many cancers is not consistent with most previous research. Further, by not having data on the pattern of drinking, the authors include binge drinkers in the same category as regular drinkers, further exaggerating the association of cancer with moderate drinking. Others have clearly shown that there are large differences in effect between these two patterns. (It is troubling also that in the paper, the estimated percentage of alcohol-attributable cancer risk among subjects reporting > 0 to 20 grams of alcohol per day is much higher than that of subjects reporting > 20 to 40 grams/day; while this partly relates to the large number of persons who drink only small amounts, such an association makes no sense biologically. It is difficult to understand who the subjects are in the lowest drinking group, but it may include a large percentage of ex-alcoholics or heavier drinkers underreporting their intake. However, this makes any conclusions in this paper regarding the risk of cancer among moderate drinkers highly suspect.)
(4) The authors do not point out the demonstrated effects of alcohol on total mortality; regular, light-to-moderate drinkers live longer. By focusing only on cancer risks, the authors fail to mention the effects on the risk of much more common conditions, such as coronary heart disease, stroke, dementia, other important health problems of ageing, and on total mortality. The study of the health benefits and problems of drinking is a very mature field — authors generally discuss their observations in the context of total mortality or other major diseases that would be affected by their experimental design. In nearly all cases, light drinking is shown to be beneficial; these studies are ignored here.
(5) Overall, a criticism of this paper relates to the failure of the authors to put their results into perspective. Statements such as “There is no safe threshold for alcohol and cancer risk” is more of a “scare” statement than a balanced discussion of their results. Given that almost all prospective studies show that regular moderate drinkers have better health as they age and live longer than lifetime abstainers, even papers focused on the effects of alcohol on any particular disease should present a balanced view on its net effects on health and disease.
(6) Finally, the authors of this paper have taken the results of their analyses (some of which are based on questionable assumptions) as “truth,” then expounding at length about the public health implications. There should always be a certain amount of doubt when presenting the results of an individual study, as no one analysis can possibly reveal everything about an association. (As stated by Voltaire: “Doubt is not a pleasant condition, but certainty is absurd!)
As the authors acknowledge, observational epidemiologic data can never reveal the full “truth” about the causation of disease from exposures, and each new study’s results must be interpreted taking into consideration previous research. However, the overall implications presented by the authors of this paper suggest that their goal may have been to support a presumed conclusion to discourage alcohol consumption, not to carefully interpret the available data to best advance the public health.
Key points of these comments
• There are a number of assumptions taken by the authors in their analyses that raise questions about their results. The authors present only “adjusted” data for reported alcohol intake (based on national sales, not on individual intake), making the relation of alcohol intake to the occurrence of cancer in individuals unclear.
• There is poor differentiation between regular moderate drinking and periodic heavy drinking (binge drinking) or alcoholism, although there are marked differences in health effects between these groups. Regular, moderate drinking is associated with net health benefits, whereas binge drinking and alcoholism have almost exclusively adverse effects (including increases in many types of cancer).
• There has been a huge amount of previous research in this field, but the authors do not put their own results into perspective or discuss the overall health effects of alcohol consumption. Previous data have clearly shown that regular moderate drinkers tend to have lower risk of cardiovascular disease, stroke, diabetes, and many other diseases, and have a lower overall risk of all-cause mortality.
Submitted by
R. Curtis Ellison, MD, Professor of Medicine & Public Health; Director, Institute on Lifestyle & Health;l Boston University School of Medicine
Co-Director, International Scientific Forum on Alcohol Research
===============================================================================
Critique 102: Possible prevention of myocardial infarction from alcohol’s effects on periodontal disease: An hypothesis — 6 February 2013
A cross-sectional analysis among more than 5,000 Norwegian men was designed to determine if the frequency of alcohol consumption related to the risk of myocardial infarction associated with infectious periodontal disease. The authors hypothesized that because it is bactericidal, frequent alcohol consumption would decrease periodontal infection and lower the risk of tooth extraction related to periodontal infection. The authors state that their main finding was that frequent drinking lowers the risk of MI associated with periodontal disease.
Forum reviewers had real concern about the paper and the conclusions of the authors. Some stressed that the per cent of alcohol in most “drinks” is too low to be really bactericidal, that the key exposures (alcohol and oral infections) were based exclusively on self report and did not have information on type of beverage or pattern of drinking, that many confounders (especially related to socio-economic status) were not adequately taken into consideration, and that the authors did not really test the results of their study with appropriate statistical testing.
Current scientific data show an increase in the risk of cardiovascular disease to be associated with periodontitis. Further, data consistently show a decrease in the risk of cardiovascular disease from moderate drinking, and a very large number of mechanisms have been identified. However, the present study does not confirm that alcohol consumption plays an important role in preventing heart disease through its effect on periodontitis.
Reference: Håheim LL, Olsen I, Rønningen KS. Oral infection, regular alcohol drinking pattern, and myocardial infarction. Medical Hypotheses 2012;79:725–730.
For the full critique of this article by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 101: A review of the association of alcohol consumption with the risk of developing hypertension — 22 January 2013
A meta-analysis from investigators at Columbia University in New York evaluated the risk of developing hypertension according to the level of alcohol consumption previously recorded. The analyses were based on data from 16 prospective studies. The paper’s main results are that among men, there is little effect of alcohol consumption up to 30 grams of alcohol per day (the equivalent of about 2 ½ “typical drinks” by US standards or more than 3 drinks by UK standards), but evidence of an increased risk of hypertension for the intake of greater amounts of alcohol. For women, light drinking appears to be associated with a slightly lower risk of hypertension, but more than 20 grams/day of alcohol may increase the risk.
While Forum members thought that the analyses were done well, they had some concerns about the conclusions of the authors, some of which appear to not be in line with the data they presented. For example, their statement that “heavier alcohol consumption >20 g⁄d is associated with the risk of development of hypertension in both women and men” is not consistent with their findings of a significant increased risk of hypertension only with an intake of 31 – 40 grams of alcohol per day.
Similarly, the authors conclude: “Even for light drinkers, vigilant blood pressure monitoring is necessary,” which may not be appropriate given that their data show that intake below 30 grams per day has no significant association with hypertension in men and may actually reduce the risk of hypertension in women.
Overall, the results of this study, in line with findings from most previous research, indicate that people who consume alcohol according to most current drinking guidelines (no more than 2 typical drinks/day for men or 1/day for women) do not show an increase in their risk of hypertension, but heavier drinking appears to increase the risk. Not discussed in this paper, but especially important in terms of health, is that light drinking is associated with a significant and rather large decrease in the risk of the most serious sequelae of hypertension: coronary heart disease and ischemic stroke.
Reference: Briasoulis A, Agarwal V, Messerli FH. Alcohol consumption and the risk of hypertension in men and women: A systematic review and meta-analysis. J Clin Hypertens 2012;14:792-798.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 100: The effects of moderate drinking on cognitive function and dementia: An update — 15 January 2013
A paper from a group of Italian scientists provides an extensive review of the available research relating alcohol consumption to cognitive function. It presents brief summaries of results from most key epidemiologic studies dealing with this topic between 1987 and 2011. The large majority of these studies, and recent meta-analyses, support a finding of a lower risk of cognitive impairment from ageing and of dementia to be associated with moderate drinking.
Reviewers praised the authors for pointing out difficulties caused by having to develop guidelines for alcohol consumption based only on observational data, and not having large clinical trials for judging effect. A further problem faced in judging the numerous studies on this topic is that many lack data on beverage type and most lack detailed information on the pattern of drinking, which may be especially important in judging the effects of drinking.
Some reviewers stated that the paper does not present anything new, as previous meta-analyses have clearly shown a potentially protective effect of moderate alcohol consumption on the risk of cognitive decline and dementia. Given that recent large meta-analyses have shown that moderate drinking, is comparison with abstention, is usually associated with 20-35% lower risk of cognitive decline and dementia, Forum reviewers thought that the conclusions of the authors of this review paper were unnecessarily cautious. Overall, current scientific data support a conclusion that moderate consumption of alcoholic beverages, especially of wine, is neuroprotective.
Reference: Panza F, Frisardi V, Seripa D, Logroscino G, Santamato A, Imbimbo BP, Scafato E, Pilotto A, Solfrizzi V. Alcohol consumption in mild cognitive impairment and dementia: harmful or neuroprotective? Int J Geriatr Psychiatry 2012;27:1218-1238.
For the full review of this critique by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 099: Alcohol and survival after postmenopausal diagnosis of breast cancer — 20 December 2012
This paper assessed the association of pre-diagnostic alcohol consumption with disease recurrence and survival in a prospective cohort study in Germany based on 2,522 postmenopausal breast cancer patients, aged 50–74 years. The authors report that alcohol consumption was non-linearly associated with increased breast cancer-specific mortality, but not with breast cancer recurrence. Results were independent of estrogen receptor status. The authors also report a non-significantly decreased risk of mortality due to other causes.
Forum reviewers considered this to be a well-done analysis that was limited, however, by the lack of data on drinking patterns prior to breast cancer diagnosis and because no data were available on drinking after the diagnosis (the latter limits the applicability of its results to women who have already developed breast cancer). The comparisons were primarily between non-drinkers/light drinkers and women in the highest alcohol category; the authors state that when ex-drinkers were removed from the referent category, their results regarding breast cancer-specific mortality were no longer statistically significant. The authors do not describe the potential effects on their main results that could result from what is known as “index event bias,” which may occur when an exposure (e.g., alcohol) relates to the development of a disease, breast cancer in this study, and may also relate to sequelae (e.g., recurrence or death) from the same disease.
Forum reviewers conclude that current scientific data show that alcohol consumption may increase the risk of developing breast cancer. However, they believe that the effects on subsequent survival after such a diagnosis remain unclear.
Reference: Vrieling A, Buck K, Heinz J, Obi N, Benner A, Flesch-Janys D, Chang-Claude J. Pre-diagnostic alcohol consumption and postmenopausal breast cancer survival: a prospective patient cohort study. Breast Cancer Res Treat 2012;136:195–207. DOI 10.1007/s10549-012-2230-2
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 098: Moderate alcohol consumption may lower the risk of developing depression — 13 December 2012
Analyses from a prospective study of more than 13,000 adults in Spain related baseline alcohol intake (mainly wine) with the development of depression, with the outcome based on a physician’s diagnosis or on the habitual use of anti-depressant drugs for four or more years. Reported depression was much higher among women than men. Among women, the estimated hazard ratios for groups reporting an average alcohol intake of < 5 g/day of alcohol, 5-15 g/day, and > 15 g/day were 0.97, 0.62, and 0.84 (in comparison with subjects reporting no alcohol). The difference was statistically significant (CI = 0.43-0.89) for the group reporting 5-15 g/day.
Few men reported a diagnosis of depression; among moderately drinking men, the estimated risks of depression were similar to those of women, but none of the differences were statistically different from those of non-drinkers. The investigators found no differences according to the type of alcoholic beverage consumed.
The merits of this study include that the data were collected prospectively, that there were repeated questionnaires seeking data on depression, and that there were a large number of subjects, all of whom were college graduates. There were few men reporting depression, and few heavy drinkers, so results apply only to moderately drinking women. Among these women (those consuming between about ½ drink/day to about 1 or 1 ½ drinks per day) there was evidence of a lower risk of depression during a follow-up period extending up to 10 years.
Forum reviewers thought that this was a well-done analysis, and the use of cut-points for drinking groups according to spline analyses was appropriate. Some reviewers cautioned that moderate drinkers, especially regular wine drinkers, tend to have a large number of other healthy lifestyle habits that could relate to the risk of depression. While many of the recognized potential confounders were included in the Cox regression analysis in this paper, it will be important to determine if future studies support the conclusions of the authors.
Reference: Gea A, Martinez-Gonzalez MA, Toledo E, Sanchez-Villegas A, Bes-Rastrollo M, Nuñez-Cordoba JM, Sayon-Orea C, Beunza JJ. A longitudinal assessment of alcohol intake and incident depression: the SUN Project. BMC Public Health 2012, 12:954 doi:10.1186/1471-2458-12-954
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 097: Per-capita alcohol intake and all-cause mortality in Australia — 4 December 2012
An ecologic analysis from a group in Australia has related trends in the per-capita consumption of alcohol in Australia with rates of all-cause mortality. Unfortunately, the authors do not have data on individual consumption of alcohol (and no way of knowing if the people who drink or do not drink are those who die) and do not have data on many key factors that relate to both alcohol consumption and mortality (e.g., education, income, diet, occupation, etc.). Especially, they have no data on the patterns of consumption of members of the population (regular moderate intake or binge drinking). They “adjust” for death rates in women but do not report sex-specific mortality rates.
This paper illustrates many of the dangers of the so-called “ecologic fallacy,” in which comparisons are made between aggregate population data and biologic outcomes. It has been shown that such comparisons may be of interest in generating hypotheses, but not for answering questions of causation, for which different types of studies are required. As stated in a leading textbook of epidemiology: “Ecologic analysis poses major problems of interpretation when making ecologic inferences and especially when making biologic inferences. In contemporary epidemiology, the ‘ecologic fallacy’ reflects the failure of the investigator to recognize the need for biologic inference and thus for individual-level data. This need arises even when the primary exposure of interest is an ecologic measure and the outcome of interest is the health status of entire populations.”
With such serious limitations from the use of ecologic comparisons, this paper does not provide data upon which alcohol policy can be based. The authors of this paper appear to have ignored previous research providing very different interpretations of an inverse association between per-capita alcohol intake and mortality. A plethora of studies based on alcohol intake among individuals, and especially patterns of consumption, provide data needed for such policy decisions.
Reference: Livingston M, Wilkinson C. Per-capita alcohol consumption and all-cause male mortality in Australia, 1911–2006. Alcohol and Alcoholism 2012. Pre-publication: doi: 10.1093/alcalc/ags123
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 096: Frequency of alcohol consumption and cardiovascular risk factors: implications for drinking guidelines — 20 November 2012
As stated by the authors, “many observational studies suggest that increased drinking frequency is associated with reduced mortality among those with low-dose alcohol consumption. The purpose of this paper was to examine whether frequent drinkers consume lower-risk amounts during drinking days or have favorable risk factor profiles compared with those who drink less frequently, and discuss implications for the larger debate about the limitations of non-randomized studies about ‘moderate’ drinking and the development of low-risk drinking guidelines.” Indeed, previous epidemiologic research has clearly shown that the healthiest outcomes occur among regular, moderate drinkers who do not binge drink. Further, almost all studies have adjusted for a large number of socio-economic factors that are known to be potentially confounding factors for evaluating the association of alcohol consumption with health outcomes.
As expected, the present study shows that regular drinkers tend to consume less alcohol per occasion, and are less likely to binge drink. Further, such individuals tend to have better socio-economic status and lower levels of most cardiovascular risk factors. Most previous researchers have interpreted the better educational status and economic levels of moderate drinkers to be important causes of their more moderate lifestyle factors (including avoiding abusive drinking). Further, most previous research, including many basic science interventions and limited trials in humans, have shown that the administration (intake) of moderate amounts of an alcoholic beverage leads to more favorable cardiovascular risk factors, and numerous mechanisms have been identified (higher HDL-cholesterol, improved vascular reactivity, improved platelet and other coagulation factors, etc.).
The authors of this paper take an unusual turn when it comes to discussing the implications of their results. They tend to down-play any potential health benefits that may be caused by alcohol or the pattern of drinking and infer instead that the favorable risk factors themselves may lead to the drinking pattern. Forum members disagreed with the implications of the authors on a number of factors: (1) the lack of randomized trials of low-dose alcohol consumption; (2) levels of evidence; (3) drinking frequency and alcohol intake; (4) clustering of lifestyle behaviors; (5) alcohol consumption and CVD-related biomarkers; (6) alcohol intake, cancer and total mortality. Further, Forum reviewers cite a large body of scientific research that refutes some of the conclusions of the authors, e.g., that regular moderate alcohol intake does not relate to improved cardiovascular risk factors.
Forum reviewers agree with a concluding statement of the authors about using caution before recommending drinking to the general public. However, they believe that the arguments presented in this paper are not based on a balanced appraisal of available scientific data, and should not be used to support changes in guidelines for the public.
Reference: Naimi TS, Xuan Z, Brown DW, Saitz R. Confounding and studies of ‘moderate’ alcohol consumption: the case of drinking frequency and implications for low-risk drinking guidelines. Addiction 2012; pre-publication. doi:10.1111/j.1360-0443.2012.04074.x.
For the complete critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
A Tribute to Francesco Orlandi
(1927 – 2012)
It is with sadness that we have learned of the death on 12 November 2012 in Ancona, Italy, of Francesco Orlandi, MD. Francesco was a founding member of our International Scientific Forum on Alcohol Research, and a frequent and valuable contributor to our critiques. He will be sorely missed, both as a friend and as a respected scientist. Besides his strong passion for science, he was an extraordinarily cultivated man, rich in his sense of humor, and a sincere friend of many members of our Forum.
Francesco Orlandi was Professor of Gastroenterology at the University of Ancona from 1975 to 1999 and Direttore, Dottorato di ricerca Alimenti e Salute, 1997-99. He also served as Professor on wine and health at the Corso di Laurea Specialistica in Scienze Viticole ed Enologiche at the University of Turin.
Francesco was counselor and coordinator of the “wine and health” group of the Accademia Italiana della Vite e del Vino, and an OIV expert at the Italian Ministry of Agricultural, Food and Forestry Policies in Rome. In addition, he served as Visiting Professor in the Department of Medicine, Albert Einstein College of Medicine, New York, in 1977-8.
Francesco was always interested in the study of the health risks and benefits of alcohol consumption. In the 1990’s, he performed a number of experimental studies in rats on the mechanisms of early ethanol-induced liver damage, with particular attention to apoptosis and cell proliferation.
More recently Francesco became increasingly interested in the beneficial effects of moderate alcohol consumption on human health. He became convinced that only by working in a multi-disciplinary context could young investigators contribute to a new renaissance of alcohol and wine research in Italy. This is why in June, 2011, he organized the first seminar on responsible drinking in the context of the Mediterranean Diet, which was held in the ancient Pontignano Abbey, near Siena. There he brought together all young Italian scientists involved in this field of research; the abstracts of this meeting have been published (Eur J Nutr 2011;50:489–498).
As stated by a Forum member, Francesco was much more than a great doctor and an outstanding scientist. He was an old style gentleman, able to use the right words in every social context. He was an extremely educated person, cultivating interests from art, music, and sailing to science with the emotional motivation, intellectual freedom, and motivated curiosity that usually only young talents can have. Francesco will remain forever a young enthusiastic scientist for all of us who had the fortunate chance of interacting with him.
These comments provided by members of the International Scientific Forum on Alcohol Research (www.bu.edu/alcohol-forum)
15 November 2012
===============================================================================
Critique 095: Effects of alcohol on lymphoma, leukemia, and other types of hematological cancers —- 13 November 2012
Many observational epidemiologic studies have found an inverse association between alcohol consumption and hematological cancers (such as lymphoma and leukemia). This study, based on the Million Women’s Study in the UK, is large enough to permit an evaluation of associations with various types of such cancers. Further, it takes into account newer coding systems for morphology so that diseases associated with the lymphatic system can be separated from those of the myeloid system.
The key findings are that alcohol consumption appears to lower the risk of several types of lymphoma and plasma cell neoplasms, but has little effect on the risk of myeloid tumors such as acute myeloid leukemia. Smoking is associated with an increase in risk for most such cancers.
Forum reviewers considered this to be a very well-done analysis, and the ability of the authors to separate the effects on lymphoid and myeloid cancers is important. Forum members emphasize the strong differences in effect of smoking (an increase) and alcohol consumption (a decrease) on the risk of these cancers. They support future research to discover the mechanisms by which moderate drinking may lower such risk.
Reference: Kroll ME, Murphy F, Pirie K, Reeves GK, Green J, Beral V, for the Million Women Study Collaborators. Alcohol drinking, tobacco smoking and subtypes of haematological malignancy in the UK Million Women Study. British Journal of Cancer 2012;107:879–887.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
A Tribute to Serge Renaud
(1927 – 2012)
It is with sorrow that we have learned of the death in France on 28 October 2012 of Professor Serge Renaud at 84 years of age. In addition to being a colleague and close friend of many of us, he was celebrated as a pioneer in scientific research on the prevention of cardiovascular and other diseases. His innovative mind opened up new fields of inquiry that have greatly broadened research into the role of wine, alcohol, fatty acids, and other nutrients in preserving health and preventing disease. For his many contributions to science, on July 14, 2005, Serge received France’s highest distinction, the Legion d’Honneur.
Over many decades, Professor Renaud was the scientist who initiated much of the work relating the consumption of wine and other types of alcohol to cardiovascular disease and other of the diseases associated with ageing. He was the scientist most associated with the role of red wine in protecting the French from coronary artery disease (the “French Paradox”), and a leading figure in studying how other dietary factors relate to health. His innovative concepts have sometimes taken many years to be appreciated by other scientists. He made a major contribution with his research demonstrating how alpha-linolenic acid, monounsaturated fats, and other components of the “Cretan-type Mediterranean Diet,” play key roles in promoting health.
Serge Renaud was born in Cartelègue, Haute Gironde, France, and after starting his medical training in France moved to Montreal, Canada, and later to Boston, Massachusetts, USA. He returned to France in 1973 and became director of the INSERM unit in Lyon, France, where much of his research was carried out.
In an excellent tribute to Renaud in the Lancet in 2000, Bruno Simini pointed out his major contributions investigating the association between wine, diet, and thrombosis. Simini quotes Serge as saying: “If I hadn’t lived with my grandparents and great-grandparents on a vineyard near Bordeaux, perhaps this idea wouldn’t have occurred to me. When you see people reach the age of 80 or 90 years, who have been drinking small amounts of wine every day, you don’t believe wine in low doses is harmful.”1
In 1991, Serge Renaud appeared on the popular US television program, “60 Minutes,” in a segment entitled the “French Paradox.” When asked by Morley Safer, the host, what was the real reason that the French have rates of coronary artery disease so much lower than those in other developed nations, Renaud replied: “I think it is the alcohol.” And when Morley Safer closed the segment holding a glass of red wine and saying, “The protection of the French from heart disease may rest in this inviting glass,” the response in the US was remarkable – nothing such as this had ever been stated in the country that earlier in the century had made any alcohol consumption illegal through nation-wide prohibition. Following the television program, sales of red wine rose immediately by 40 per cent!
In addition to his studies on wine and alcohol, Professor Renaud, noting the very low rates of heart disease among participants from Crete in the “Seven Countries Study,” initiated the Lyon Diet Heart Study in 1985 to determine the effects of a diet based on that of Crete on the course of disease among patients who already had coronary disease. There were very dramatic reductions in subsequent coronary problems and in total mortality among subjects given the “Cretan-type diet,” which contained increased levels of an omega-3 fatty acid (alpha-linolenic acid) to replace some of the fats from meat and dairy products.
As quoted in the Lancet tribute by Simini, Professor Renaud said the results of these studies on heart disease and cardiac arrhythmias made him “wonder about the origins of civilisations. It is intriguing that ancient Asian and Mediterranean civilisations used natural oils in cooking—colza and olive—with similar fatty acid compositions.” [Colza oil is closely related to the widely used rapeseed oil and canola oil.] And because of his belief in ancient wisdom when it comes to diet and health, Renaud ends his book Le régime santé2 with a warning: “Don’t look for a pill that replaces [the Cretan diet]. There is no such thing.”
People around the world have profited, and will continue to profit, from the lifelong scientific work of Serge Renaud. For those of us who knew and worked with him, we cherish our memories of Serge the person, and of Serge the consummate scientist. As stated so well by a Forum member, “We are all in debt to Serge for the lesson he gave to our scientific community: curiosity as the sole reason to investigate, diligence in observing the facts, unbiased stringency in interpreting results, and, definitely not least, the modesty that only a great man can have. We shall keep him in our memory as an example and a mentor of the meaning of being a scientist.”
References
1. Simini B. Serge Renaud: From French Paradox to Cretan miracle. The Lancet 2000;335:48. doi:10.1016/S0140-6736(05)71990-5.
2. Renaud S. Le régime santé. Odile Jacob, Paris, 1998.
These comments provided by members of the International Scientific Forum on Alcohol Research (www.bu.edu/alcohol-forum)
31 October 2012
===============================================================================
Critique 094: The complex association between moderate alcohol consumption and breast cancer — 23 October 2012
An excellent review article from two scientists at the National Institue on Alcohol Abuse and Alcoholism describes the epidemiologic and basic scientific evidence linking alcohol consumption to the risk of breast cancer. The authors point out deficiencies in the epidemiologic data, especially that the pattern of drinking (regular moderate versus binge drinking) has generally not been taken into consideration (and the latter pattern can be associated with much higher blood alcohol concentrations). Further, epidemiologic studies usually provide data for only a short period of time, while the development of cancer may relate to exposures over many decades. The authors also comment upon the effect that under-reporting of alcohol by study participants could exaggerate effects on cancer risk from light drinking. They discuss two hypotheses that could relate alcohol to breast cancer risk: alcohol as a breast tumor promoter, and alcohol as a weak cumulative breast carcinogen, and present evidence from epidemiology and basic science that would relate to each hypothesis.
Overall, Forum reviewers were enthusiastic about this review paper, considering that it clearly outlined some of the difficulties scientists have in determining the causes of cancer. They agreed with the authors’ statements regarding the necessity to consider the overall net effects of moderate drinking, including reductions in the risk of cardiovascular disease and total mortality. They also agreed that future epidemiologic studies should focus on the pattern of drinking (and not just the average weekly amount of alcohol), and with their suggestions for future animal studies. One Forum reviewer cautioned that our understanding of the causes of breast cancer is still very incomplete, limiting our ability to provide well-founded recommendations to the public regarding moderate drinking as it relates to breast cancer risk.
Reference: Brooks PJ, Zakhari S. Moderate alcohol consumption and breast cancer in women: From epidemiology to mechanisms and interventions. Alcohol Clin Exp Res 2012; pre-publication: DOI: 10.1111/j.1530-0277.2012.01888.x.
For the full critique of this article by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 093: Is moderate alcohol consumption associated with an increased risk of atrial fibrillation among patients with cardiovascular disease? — 8 October 2012
An analysis of the association of alcohol consumption with the development of atrial fibrillation (AF) among subjects with coronary heart disease, stroke, diabetes, or other manifestations of cardiovascular disease (CVD) was based on subjects in two large antihypertensive drug treatment trials. Previous research in the general population has suggested an increase in the risk of the development of AF for heavy drinkers, and the present study shows such an association among subjects who already have CVD.
Among subjects in this study (all of whom had previous CVD), the authors also report that even “moderate” drinkers had a higher risk of AF than low-alcohol consumers, although the risk of death during follow up of moderate drinkers (9.9%) was lower than that of subjects reporting low-levels of drinking(12.5%). Excluding binge drinkers, the estimated risk of AF was about 13% higher in moderate drinkers than among subjects classified as low-alcohol consumers.
While the multiple analyses in this paper were done appropriately, Forum reviewers were concerned about two aspects of this study. First, there was concern about the wide range the authors chose for the category of “moderate” drinkers, which included subjects reporting from 1 drink per week up through those reporting 21 drinks per week for men and 14 drinks per week for women. It would have been useful to present results also for subjects who met more common definitions for moderate drinking: no more than 14 drinks/week for men and 7 drinks/week for women, the values used to define moderate drinking in the United States, Australia, and many other countries. Unfortunately, there is a conspicuous absence of data in this paper of the effects on the risk of AF of subjects consuming alcohol “moderately” by these standards.
Another major concern about these analyses relates to potential bias in the estimates from what is known as index event bias or collider bias. Given that alcohol intake prior to enrollment in this study may well have related to subjects’ development of cardiovascular disease, it is problematic to judge the effects of alcohol after a cardiovascular event on the subsequent risk of AF, a condition frequently associated with CVD.
All subjects in these analyses had already developed CVD (the prerequisite for being in the present study). Thus, the study included those who consumed alcohol prior to the diagnosis of CVD or diabetes and those who did not drink prior to these diagnoses. Given that moderate alcohol consumption has been shown to reduce substantially the risk of both CVD and diabetes, it can be assumed that subjects in this study who developed CVD despite being drinkers had other risk factors contributing to the disease that overcame any “protection” afforded by alcohol consumption. Unless adjusted for, these other risk factors could well affect the subsequent course of subjects following the onset of CVD, including the development of AF. A similar phenomenon has been seen for obesity (the “obesity paradox”), aspirin use (the “aspirin paradox”), and other exposures, where the associations with CVD seen prior to the initial development of the disease differ from those seen after the development of CVD.
It is clear from many previous studies in the general population that heavy alcohol intake and binge drinking increase the risk of developing atrial fibrillation. This cardiac arrhythmia is a common component of the “holiday heart” syndrome that may occur after very heavy bouts of drinking. As for the effects on the risk of atrial fibrillation from moderate drinking, as studied in this paper, there were a number of concerns from Forum reviewers about the analyses and results. They raise questions about the conclusions of the authors that even “moderate” drinking results in an increased risk of atrial fibrillation after the development of cardiovascular disease. Especially when defined as no more than 14 drinks per week for men or 7 drinks per week for women, the association between “moderate” alcohol consumption and atrial fibrillation remains unclear.
Reference: Liang Y, Mente A, Yusuf S, Gao P, Sleight P, Zhu J, Fagard R, Lonn E, Teo KK; for the ONTARGET and TRANSCEND Investigators. Alcohol consumption and the risk of incident atrial fibrillation among people with cardiovascular disease. CMAJ 2012. DOI:10.1503/cmaj.120412.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 092: The association of alcohol and tobacco with age at diagnosis among subjects with pancreatic cancer — 2 October 2012
This analysis from a group of distinguished scientists supports previous research showing that smoking is associated with an earlier onset of pancreatic adenocarcinoma. Other research has shown that smoking may also be a causative factor in the development of this type of cancer. For alcohol, this study shows that heavy drinking also appears to be associated with earlier diagnosis; previous research from some epidemiologic studies has suggested further that heavy intake of alcohol may be associated with the development of pancreatic cancer.
Forum reviewers were concerned, however, about potential bias in regards to the time of diagnosis of such cancer, and about many other limitations of the study. For example, the inability to separate drinkers by the pattern of drinking (binge drinking versus regular, moderate intake), by the socioeconomic status of subjects, and by a lack of information on chronic pancreatitis, a known risk factor, weaken the implications of this paper. Forum members do not think that the results of this study will have a large impact on clinical practice, or on measures for the prevention of pancreatic cancer.
Reference: Anderson MA; Zolotarevsky E; Cooper KL; Sherman S; Shats O; Whitcomb DC; Lynch HT; et al. Alcohol and tobacco lower the age of presentation in sporadic pancreatic cancer in a dose-dependent manner: A multicenter study. Am J Gastroenterol 2012; advance online publication, doi: 10.1038/ajg.2012.288
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 091: Light drinking may relate to increase in risk for certain cancers — 18 September 2012
A meta-analysis by a distinguished group of scientists was designed to determine if “light drinking” (defined as an average of up to 1 drink per day) was associated with the risk of certain cancers that have been shown in previous studies to be associated with the risk of cancer. The authors concluded that while the risk of these cancers was only slightly increased from such drinking, there were detectable increases in cancers of the oral cavity and pharynx, esophagus and female breast. They report no increase in the risk of cancers of the colorectum, liver, and larynx to be associated with such drinking.
Forum reviewers were concerned about a number of aspects of this study. While the statistical methodology was correct and done appropriately, the fact that the investigators (1) included both ex-drinkers and never drinkers in the reference group; (2) could not separate the effects of regular light drinking from binge drinking; (3) had no data on the duration of alcohol consumption at different levels; (4) did not adjust their analyses according to geographic region or type of study (both of which had large estimated effects on cancer risk); and (5) did not adjust their estimates of effect by other lifestyle habits, including smoking. All of these factors tend to weaken the implications of their results.
Forum reviewers were also concerned that despite the acknowledged limitations of their data, the authors present conclusions indicating that even light drinking increases the risk of certain cancers without commenting on the net health effects. They present only the effects on cancer (which was the topic of the meta-analysis) but do not comment on the overall or net health effects of light drinking: a marked reduction in the risk of much more common diseases, especially cardiovascular diseases, and a longer lifespan. Further, the lack of data on genetic patterns, folate intake, and other lifestyle factors makes it difficult to apply their findings to individual subjects. The Forum considers that while their analyses may be helpful in understanding associations between alcohol and cancer, the many limitations of this study indicate that it can provide only incomplete information on light alcohol consumption to be used as a basis for making recommendations to the public.
Reference: Bagnardi V, Rota M, Botteri E, Tramacere I, Islami F, Fedirko V, Scotti L, Jenab M, Turati F, Pasquali E, Pelucchi C, Bellocco R, Negri E, Corrao G, Rehm J, Boffetta P, La Vecchia C. Light alcohol drinking and cancer: a meta-analysis. Pre-publication: Annals of Oncology 2012; doi:10.1093/annonc/mds337
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 090: Effects of stopping alcohol consumption on subsequent risk of esophageal cancer — 13 September 2012
This paper provides an evaluation of the time following cessation of alcohol consumption that the risk of esophageal cancer returns to that of non-drinkers; it is based on 17 studies providing such information, 9 of which provided data for a meta-analysis. The authors conclude that an alcohol-related increased risk of esophageal cancer is reversible following drinking cessation, most likely requiring up to 16 years. The authors estimate that about one-half of the reduction in risk of cancer may occur within in a much shorter time, perhaps within about 4 or 5 years.
Forum reviewers considered this to be a well-done analysis. Forum members emphasized, as did the authors, a number of limitations of the study. Adjustments for smoking may not have been adequate: most upper aero-digestive cancers show a strong interaction between smoking and alcohol consumption in relation to cancer risk. (For many “alcohol-related” cancers, there is little effect of alcohol consumption among non-smokers.)
Further, large differences in the alcohol-cancer association were shown in this study for different geographical regions (some associations being much higher in Asia than in Europe or North America), but such differences were not adjusted for in the main analyses. The fact that the authors of this paper did not have data permitting the separation of ex-drinkers and never drinkers (both groups being included in the “non-drinker” category), and their inability to judge the effects of the baseline pattern of drinking (regular versus binge drinking), may also be limitations to the interpretation of their results. Adjustment for such factors may have influenced the effects of stopping drinking on subsequent cancer risk, and markedly changed the calculated effects on the numbers of cancers prevented worldwide.
In any case, the fact that cessation of drinking may reduce the risk of esophageal cancer is of importance. Other studies suggest further that just reducing the amount of alcohol consumed, rather than the complete cessation of drinking, may be associated with lowering of cancer risk, and low-level alcohol intake has been shown to have beneficial health effects on cardiovascular disease, diabetes, and other medical conditions.
Reference: Jarl J, Gerdtham Ulf-G. Time pattern of reduction in risk of oesophageal cancer following alcohol cessation — a meta-analysis. Addiction, 107, 1234–1243. doi:10.1111/j.1360-0443.2011.03772.x
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 089: Combination of hormone treatments and alcohol consumption influences the risk of breast cancer in women — 29 August 2012
An analysis among more than 40,000 postmenopausal women who were in the California Teachers Study was carried out to determine if there were differences in risk of breast cancer among women consuming alcohol according to their previous or current use of hormone therapy (HT). In the cohort, 660 women were diagnosed with invasive breast cancer during follow up.
Results from multivariate Cox proportional hazards regression models showed an increase in risk of breast cancer among alcohol consumers of more than 20 grams of alcohol per day (about 1 ½ to 2 typical drinks) who were current users of HT but not among those who were ex-users of HT. The authors conclude: “Following the cessation of HT use, alcohol consumption is not significantly associated with breast cancer risk, although a non-significant increased risk was observed among women who never used HT. Our findings confirm that concurrent exposure to HT and alcohol has a substantial adverse impact on breast cancer risk. However, after HT cessation, this risk is reduced.”
Forum reviewers considered this to be a very well-done analysis on a large group of post-menopausal women with repeated assessments of alcohol consumption and HT use. However, results from even very large studies on the relation between alcohol, HT, and breast cancer risk have often been conflicting. Even with numerous studies on this topic, we still have very poor predictors of which women will develop breast cancer. There is some increase in risk for women with a family history of such cancers and those who are obese. However, the percentage increases in risk associated with HT, alcohol consumption, and other environmental factors are generally small (unlike the many-fold increase in the risk of lung cancer among smokers in comparison with never smokers). This may explain why the results of individual studies may reach apparently conflicting conclusions. While the present study suggests that women who consume alcohol may have a decrease in their risk of breast cancer if they stop taking hormone replacement therapy, our current understanding of factors affecting breast cancer risk remains quite inadequate.
Reference: Horn-Ross PL, Canchola AJ, Bernstein L, Clarke CA, Lacey JV, Neuhausen SL, Reynolds P, Ursin G. Alcohol consumption and breast cancer risk among postmenopausal women following the cessation of hormone therapy use: the California Teachers Study. Cancer Epidemiol Biomarkers Prev 2012. [Epub ahead of print]
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 088: Higher levels of alcohol intake may slightly increase risk of age-related macular degeneration, with no effect from moderate drinking 22 August 2012
An analysis based on the follow up of more than 20,000 participants recruited in 1990-1994 for the Melbourne Collaborative Cohort Study in Australia related alcohol consumption at baseline to the subsequent development of age-related macular degeneration (AMD), a common cause of blindness in the elderly. At a follow-up examination between 2003 and 2007, digital macula photographs of both eyes were taken and evaluated for early and late AMD signs; there were 2,663 cases of early AMD and 121 cases of late AMD identified.
The authors report: “Drinking more than 20 g of alcohol per day was associated with an approximate 20% increase in the odds of early AMD (odds ratio = 1.21, 95% confidence interval: 1.06, 1.38; P = 0.004) when compared with those who reported no alcohol intake at baseline.” (An average of 20 grams/day of alcohol is the equivalent of about 2 daily drinks by British standards or 1 ½ drinks by US standards.) The analyses show that the increased risk was almost exclusively among smokers, with no significant effect among non-smokers who consumed any amount of alcohol.
Forum reviewers had some concern that approximately one-half of this “population-based” study did not have measurements for AMD; these included those who had died during the follow-up period (and deaths were more common among non-drinkers than among drinkers). Further, the authors focus only on the slight increase in risk of AMD seen for heavier drinkers, but do not emphasize that among never smokers there was no increase in risk for consumers of any amount of alcohol. Their results suggest a possible interaction between smoking and alcohol consumption in the etiology of this disease.
The findings of no effect (either positive or negative) from drinking < 20 g/day of alcohol in this study does not support some earlier reports of reduced risk of AMD among moderate wine drinkers. In the present study, there were no detectable differences in effect between the consumption of wine or of beer. A key point of this study may be that never-smokers do not show increased risk of AMD with alcohol consumption.
Reference: Adams MKM, Chong EW, Williamson E, Aung KZ, Makeyeva GA, Giles GG, English DR, Hopper J, Guymer RH, Baird PN, Robman LD, Simpson JA. 20/20—Alcohol and age-related macular degeneration: The Melbourne Collaborative Cohort Study. Am J Epidemiol 2012;176:289-298.
For the full critique of this article by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 087: Smoking increases, while alcohol consumption may decrease, the risk of amyotrophic lateral sclerosis (ALS) — 8 August 2012
Reference: de Jong SW, Huisman MHB, Sutedja NA, van der Kooi, AJ, de Visser M, Schelhaas HJ, Fischer K, Veldink JH, van den Berg LH. Smoking, alcohol consumption, and the risk of amyotrophic lateral sclerosis:A population-based study. Am J Epidemiol 2012;176:233–239
A population-based case-control study of the rare but devastating neurological disease amyotrophic lateral sclerosis (ALS) has shown that the risk of such disease is increased among smokers, as has been shown previously. However, surprisingly, the risk of ALS was found to be markedly lower among consumers of alcohol than among abstainers.
Forum reviewers thought that this was a well-done and important paper, as it is a population-based analysis, with almost 500 cases of ALS, a very large number of cases for this rare disease. They were especially struck by the magnitude of the difference in risk of ALS between alcohol consumers and never drinkers: the risk among drinkers was about one half that of non-drinkers. Said one reviewer: “The results in this study are astonishing in this mysterious disease. One should expect that alcohol, as a toxic agent, rather should contribute to the development of ALS than to prevent it. The lower risk among drinkers compared with non-drinkers is remarkable”
Forum reviewers cautioned that the results of this paper should not be used to prompt people to consume alcohol just to prevent ALS, as it is such a rare disease. However, this paper presents important data that could help scientists understand the etiology of ALS and perhaps other more common diseases.
For the full critique of this paper by members of the International Scientientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 086: Mechanisms for a beneficial effect of moderate alcohol consumption on osteoporosis in women — 1 August 2012
Women after menopause tend to develop weaker bones from what is known as osteoporosis, which may lead to fractures (especially hip fractures) from falling. The weakness of the bones results from an imbalance between the normal resorption (a type of dissolving of old bone) and the laying down of new bone, an ongoing process for both men and women referred to as “bone turnover.” For poorly understood reasons, after menopause the resorption of old bone in women continues but new bone is laid down less well, leading to a decrease in the density of bone. A variety of substances (calcium, vitamin D, various medications) have been used in an attempt to prevent the development of osteoporosis; in epidemiologic studies, moderate drinking of alcohol has been shown to lower this risk.
An intervention trial evaluating the association of alcohol intake with indices of bone metabolism shows beneficial effects of moderate alcohol intake on factors that relate to osteoporosis in post-menopausal women. The authors state that excessive bone turnover, combined with an imbalance whereby bone resorption exceeds bone formation, is the principal cause of post-menopausal bone loss. This study among 40 healthy post-menopausal women investigated the hypothesis that moderate alcohol intake (an average of 19 grams per day, or approximately 1 and ½ typical drinks per day in this study) attenuates bone turnover after menopause. Measurements were carried out while the women were consuming alcohol, after they had stopped drinking as part of the trial, and following resumption of alcohol. The study showed that abstinence from alcohol resulted in increased markers of bone turnover (hence, higher risk of developing osteoporosis), whereas resumption of alcohol reduced bone turnover markers.
Forum reviewers considered this to be an innovative and well-done study. The key questions raised were how alcohol may affect bone metabolism in a longer period of time than was tested in this study. Reviewers realized that such long-term intervention trials are very difficult and expensive to carry out. On the other hand, many prospective epidemiologic studies in the elderly have shown greater bone mineral density and a lower risk of fractures among regular moderate drinkers than among abstainers. The most important aspect of this study may be that it has helped identify cellular mechanisms for the increased bone density observed in post-menopausal women who are moderate alcohol consumers.
Reference: Marrone JA, Maddalozzo GF, Branscum AJ, Hardin K, Cialdella-Kam L, Philbrick KA, Breggia AC, Rosen CJ, Turner RT, Iwaniec UT. Moderate alcohol intake lowers biochemical markers of bone turnover in postmenopausal women. Menopause 2012;19: DOI: 10.1097/gme.0b013e31824ac071
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research and other invited scientists, please click here.
(Note: an ADDENDUM to the original Forum critique has been added on 15 August 2012.)
===============================================================================
Critique 085: Moderate alcohol intake is associated with a lower risk of kidney cancer — 19 July 2012
A majority of previous epidemiologic studies have shown that moderate drinking is associated with a lower risk of kidney cancer, which may affect about 1% of the general population. In published prospective cohort studies, the risk for such cancer among moderate drinkers is usually about 25% less than the risk seen among non-drinkers.
This well-done meta-analysis supports these findings: for the more-reliable prospective cohort studies (rather than case-control studies) the current study finds a 29% lower risk for subjects in the highest category of alcohol consumption in comparison with subjects in the lowest alcohol category. The findings suggest similar effects among men and women, and for all types of alcohol beverages. The effects are seen at a level of about one drink/day, with little further reduction in risk for greater alcohol consumption.
Reference: Song DY, Song S, Song Y, Lee JE. Alcohol intake and renal cell cancer risk: a meta-analysis. British Journal of Cancer 2012;106:1881–1890.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 084: Moderate drinking lowers risk of developing rheumatoid arthritis in women — 17 July 2012
A follow-up study of more than 34,000 women in Sweden has shown that moderate drinkers, in comparison with abstainers, were at significantly lower risk of developing rheumatoid arthritis (RA), an often serious and disabling type of arthritis. RA is known to relate to inflammation, and it is postulated that this is blocked to some degree by the consumption of alcohol. In this study, women who consumed at least 4 drinks per week (with a drink being defined as containing 15 grams of alcohol) had 37% lower risk of developing RA than subjects reporting never drinking or consuming less than 1 drink/week.
This large study is important as few prospective studies are of adequate size to have sufficient cases of RA to evaluate factors related to its development. The study supports previous research showing a lower risk of developing RA, or milder severity of the disease, among moderate drinkers than among abstainers.
Reference: Di Giuseppe D, Alfredsson L, Bottai M, Askling J, Wolk A. Long term alcohol intake and risk of rheumatoid arthritis in women: a population based cohort study. BMJ 2012;345:e4230 doi: 10.1136/bmj.e4230 (Published 10 July 2012)
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 083: Higher indices of quality of life are seen among persistent moderate drinkers than among abstainers — 20 June 2012
Data from a nationally representative sample of 5,404 community-dwelling Canadians ages 50 and older at baseline (1994/1995) was used to estimate the effects of alcohol drinking patterns on indices of quality of life, at baseline (when subjects were aged ≥50 years) and after a follow-up period. Health-related quality of life was assessed with the Health Utilities Index Mark 3 (HUI3). The authors report that most participants showed stable alcohol-consumption patterns over 6 years. Persistent regular moderate drinkers had the highest indices of quality of life at baseline, but subsequent changes in HUI3 were similar in all groups except those reporting decreasing alcohol consumption. The investigators conclude that persistent moderate drinkers had higher initial levels of health-related quality of life than persistent nonusers and those in other groups. However, rates of decline over time were similar for all groups except those decreasing their consumption, which had a greater decline in their level of health-related quality of life than persistent moderate users. While Forum reviewers admired the intent of this study, there were concerns about some of the statistical and epidemiologic aspects. The reasons that some people stopped drinking or decreased their intake were not known; while the authors state that subjects decreasing their alcohol consumption had a more rapid decline in quality of life measures, it is not known what percentage of such subjects decreased alcohol intake due to the development of serious iseases. If this were the case, such diseases may have been more important in their subsequent adverse health than the change in their drinking habits.
Further, the “baseline” quality of life measures in this study were obtained when subjects were aged 50 or older; this baseline value of quality of life was higher in moderate drinkers. However, there are statistical problems if adjustments are made for this when quality of life is assessed subsequently and related to drinking pattern. Peto has described this problem as a “horse-racing effect.” He states that in prospective studies, the correlation between exposures (e.g., drinking pattern) and outcomes (e.g., quality of life) assessments during follow up are likely to be the same as the outcome at the end of follow up. As an analogy he uses a race between ‘slow’ and ‘fast’ horses; it is likely that the fast horses will be ahead at the mid-point of the race as well as at the end. Environmental effects on quality of life begin early in life, and if one adjusts for the mid-life value (as done and referred to as “baseline” in the present study), you may end up disregarding much of the effect of subsequent alcohol intake.
Overall, this study shows a positive relation between moderate alcohol intake and quality of life in middle-aged adults. The effects on the subsequent quality of life as one ages of continued alccohol consumption, or of decreasing intake, remain unclear.
Reference: Kaplan MS, Huguet N, Feeny D, McFarland BH, Caetano R, Bernier J, Giesbrecht N, Oliver L, Ross N. Alcohol Use Patterns and Trajectories of Health-Related Quality of Life in Middle-Aged and Older Adults: A 14-Year Population-Based Study. J. Stud Alcohol Drugs 2012;73:581–590.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 082: A statistical model attempting to estimate the level of alcohol consumption that is “optimal” for health — 6 June 2012
Scientists from Australia and Oxford University have carried out a complex analysis in an attempt to determine the “optimal” level of alcohol consumption that is associated with the lowest rates of chronic disease in the UK. They conclude that the intake of about one-half of a typical drink per day would result in the healthiest outcomes, and the authors conclude that the recommended alcohol intake for the UK should be reduced from the current advised level of drinking.
There were a number of concerns by Forum members about the paper. It is based on an extremely complex statistical model that requires many assumptions, most of which cannot be validated. The parameters chosen to use in such a model determine the results, and a number of instances were identified where the values used in this analysis do not reflect current scientific knowledge. Further, the conclusions of the authors are based exclusively on the lowest point of the “J-shaped” curve for alcohol and disease, and disregard the findings that the risk of death, in comparison with non-drinkers, remains lower for drinkers of alcohol of up to several drinks per day.
There were other aspects of the paper that were of particular concern: (1) focusing only on the average amount of alcohol consumed, while the pattern of drinking (regular moderate versus binge drinking) has the greatest effect on health outcomes; (2) giving a single recommended level of alcohol intake irrespective of age; the greatest risks and lowest expected benefits of alcohol intake are among the young, whereas most of the putative health benefits relate to the diseases of ageing; (3) giving a single value for both men and women, since women are known to react (both adversely and beneficially) to lower levels of alcohol than do men; (4) the use of their estimated value alone for making recommendations for the population; guidelines should be based on a large number of social and behavioral factors, not just on the results of one scientific study.
The level of alcohol that is most likely to be associated with the lowest risk of adverse health outcomes and the most likely health benefits varies markedly among individuals. Middle-aged men and post-menopausal women are most likely to demonstrate enhanced health (e.g., lower risk of cardiovascular diseases, diabetes, dementia) from moderate drinking. For all ages, binge drinking is associated with predominantly adverse outcomes. In general, women should drink less than men. While the analyses presented in this paper are of scientific interest, they alone do not support changes in the current population recommendations for alcohol consumption.
Reference: Nichols M, Scarborough P, Allender S, Rayner M. What is the optimal level of population alcohol consumption for chronic disease prevention in England? Modelling the impact of changes in average consumption levels. BMJ Open 2012;2:e000957. doi:10.1136/bmjopen-2012-000957.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 081: Alcohol intake in the elderly affects risk of cognitive decline and dementia — 22 May 2012
A well-done review paper on the association between alcohol consumption and cognition in the elderly provides an excellent summary of potential mechanisms by which alcohol may affect cognitive function and the risk of dementia, both adversely and favorably. Current scientific data indicate that heavy drinking is associated with an increased risk of neurological disease and dysfunction, while regular light-to-moderate alcohol intake seems to be associated with a reduced risk of such dysfunction, including a lower risk of developing Alzheimer’s disease.
At present, the mechanisms by which the moderate intake of wine and other alcoholic beverages reduces the risk of cardiovascular diseases are much better defined than they are for cognition. Forum members agree with the authors that further research is needed to evaluate a potential role that wine and other alcoholic beverages may play in reducing the risk of dementia. Forum members also agree that, at present, the specific mechanisms of such putative protection are not well defined, and it would be premature to recommend light-to-moderate drinking for reducing the risk of dementia. On the other hand, current epidemiologic and biomedical data suggest that most elderly subjects who are responsible and moderate drinkers would not benefit from being advised to stop their alcohol consumption.
Reference: Kim JW, Lee DY, Lee BC, Jung MH, Kim H, Choi YS, Choi I-G. Alcohol and Cognition in the Elderly: A Review. Psychiatry Investig 2012;9:8-16; On-line: http://dx.doi.org/10.4306/pi.2012.9.1.8
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 080: Modest alcohol intake is associated with less inflammation among patients with the most common type of liver disease, non-alcoholic fatty liver disease (NAFLD) — 15 May 2012
NAFLD (non-alcoholic fatty liver disease) is the most common type of liver disease in the developed world, affecting up to one-third of the US population. NAFLD is often associated with obesity and other parameters of the so-called “metabolic syndrome,” which is a major risk factor for the development of cardiovascular disease. In a well-done study among subjects with NAFLD, the investigators have demonstrated that modest alcohol consumption (an average of up to 20 grams of alcohol per day and no binge drinking) is associated with less evidence of inflammation of the liver (steatohepatitis), a condition known to markedly increase the risk of progression of liver disease to cirrhosis.
Given that NAFLD and other conditions associated with the metabolic syndrome are so common, and are major risk factors for developing cardiovascular disease, the results of the present study are important. They show that modest drinking is associated with decreased, not increased, inflammation of the liver. Further, even among subjects with NAFLD, cardiovascular disease is a much more common cause of death than liver disease. The authors suggest that intervention studies should be done to support their findings; if confirmed, subjects with NAFLD should not be advised to avoid all alcohol, which is the current advice usually given to such patients.
Reference: Dunn W, Sanyal AJ, Brunt EM, Unalp-Arida A, Donohue M, McCullough AJ, Schwimmer JB. Modest alcohol consumption is associated with decreased prevalence of steatohepatitis in patients with non-alcoholic fatty liver disease (NAFLD). Journal of Hepatology 2012 (pre-publication release)
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
A Tribute to Federico Leighton Puga, MD — 8 May 2012
Frederico Leighton Puga, MD, Professor and Director of the Center for Molecular Nutrition and Chronic Diseases of the Catholic University of Chile in Santiago, died on 27 April 2012 at the age of 74 years. Dr. Leighton was a valued member of the International Scientific Forum on Alcohol Research, and was noted for his seminal work in nutrition, antioxidants, the health aspects of moderate wine consumption, and public health approaches for the prevention of chronic diseases.
Many Forum members knew and had worked with Dr. Leighton through many decades. All feel a deep loss, of a great scientist, a loyal and good friend, and someone very concerned with the health of people everywhere. As stated by one Forum member, “Federico was a great scientist motivated by curiosity and the desire to be useful for his country. His culture and education and intellectual rigor were well integrated into his humanity and the sweetness of his character.” Said another: “Federico had in abundance that indefinable quality known as ‘class.’” The world has lost an honest and honorable scientist.
For the full tribute to Dr. Leighton by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 079: Moderate alcohol consumption both prior to, and following, a myocardial infarction is associated with lower risk of mortality — 17 April 2012
In a very well-done analysis based on the follow up of more than 50,000 subjects from The Health Professionals Follow-up Study (HPFS), 1,818 men were confirmed with incident non-fatal myocardial infarction (MI). Among MI survivors, 468 deaths were documented during up to 20 years of follow up. Repeated reports were obtained on alcohol consumption throughout follow up. Average alcohol consumption was calculated prior to and then following the MI.
The overall results show that, in comparison with no alcohol consumption, the pre-MI and the post-MI intakes of light (0.1-9.9 g/day) and moderate (10.0-29.9 g/d) amounts of alcohol were both associated with lower risk of all-cause mortality and cardiovascular morality among these men. The significant reductions in all-cause mortality risk (22% lower for 0.1-9.9 g/day and 34% lower for 10.0 – 29.9 g/day, in comparison with non-drinkers) were no longer present for consumers of ≥ 30 g/day; for this highest consumer group, the adjusted hazard ratio was 0.87 with 95% CI of 0.61-1.25.
There are a number of other informative and interesting results described from this study. First, there was little change in reported alcohol prior to and following the MI: drinkers tended to remain drinkers of similar amounts. Few non-drinkers began to drink after their MI; among heavier drinkers, there was a tendency to decrease the amount somewhat (but very few stopped drinking completely). Further there were no significant differences in outcome according to type of beverage consumed although, interestingly, lower hazard ratios were seen for consumers of beer and liquor than of wine. While the authors state that the effects of alcohol were stronger for the association with non-anterior MIs, the HRs for all-cause mortality were little different: among the moderately drinking men the HRs were 0.58 for anterior MI and 0.51 for other types of MI.
Even though exposures (such as alcohol) for cardiovascular events (such as MI and cardiovascular mortality) may be different after a person has an event than it was before the event, in this study the reductions in risk were almost the same. For example, both for alcohol intake reported prior to a MI, and that after a non-fatal MI, the risk of mortality was about 30% lower for moderate drinkers than it was for abstainers. This suggests that, in terms of reducing cardiovascular disease, alcohol may have relatively short-term effects. Frequent consumption (of moderate amounts) may result in the best health outcomes.
Reference: Pai JK, Mukamal KJ, Rimm EB. Long-term alcohol consumption in relation to all-cause and cardiovascular mortality among survivors of myocardial infarction: the Health Professionals Follow-up Study. European Heart Journal 2012;doi:10.1093/eurheartj/ehs047
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 078: An update on the association of alcohol consumption with risk of breast cancer — 10 April 2012
An excellent review paper on the relation of alcohol consumption to the risk of breast cancer concludes that, overall, there is a positive dose-response relation between alcohol drinking and the risk of breast cancer. The analysis shows that an increase in risk is seen even among women reporting an average of only about one drink/day. Given the high prevalence of such light drinking in most female populations, the authors estimate that up to 1 to 2% of breast cancers in Europe and North America may be attributable to light drinking alone. Thus, while alcohol appears to be a risk factor for breast cancer, it does not explain a very high percentage of cases.
Forum members considered this to be a well-done analysis, with a good review not only of epidemiologic studies but of potential mechanisms of effect of alcohol on breast cancer risk. An increase in estrogen levels from alcohol seems to be the physiologic mechanism most commonly suggested for the increase in risk.
The meta-analysis is noteworthy in presenting risks specifically for women who consume up to one drink/day, which is the common pattern for a high proportion of women in western cultures. On the other hand, the authors herefailed to discuss the potential modification of alcohol effects on cancer risk from folate in the diet; in many studies, high folate levels tend to diminish or eliminate an increase in risk from alcohol. Further, the paper does not provide a discussion of the net effects of moderate drinking on mortality. In older women, the decrease in the risk of cardiovascular disease (a much more common cause of death than breast cancer), greatly exceeds the potential increase in risk of death from breast cancer.
Reference: Seitz HK, Pelucchi C, Bagnardi V, La Vecchia C. Epidemiology and Pathophysiology of Alcohol and Breast Cancer: Update 2012. Alcohol and Alcoholism 2012; doi: 10.1093/alcalc/ags011
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 077: Swedish study supports a “U-shaped” association of alcohol consumption with risk of pre-diabetes and diabetes mellitus — 29 March 2012
Subjects in a cohort in Sweden, some of whom had been exposed to a community intervention program to prevent diabetes, were evaluated 8-10 years after baseline for the presence of diabetes mellitus or impaired glucose metabolism (“pre-diabetes”) in relation to a baseline report of alcohol consumption. Approximately 2,000 men and 3,000 women had a normal glucose tolerance test at baseline; of these 105 men and 57 women developed type II diabetes. Of subjects with pre-diabetes at baseline, 175 men and 98 women progressed to diabetes. The authors report that total alcohol consumption and binge drinking increased the risk of pre-diabetes and diabetes in men, while low consumption decreased diabetes risk in women. However, the authors did not discuss the fact that in essentially all comparisons, the highest risk of diabetes or pre-diabetes was among abstainers.
Forum reviewers had some concerns about the study. For example, the study included some subjects who had been exposed to an intervention trial to prevent diabetes, yet no information is given on potential effects of the intervention. It was not a population-based group. Also, the sample was “enriched” with subjects who had a positive family history of diabetes, which may make it more difficult to judge the effects of environmental factors. Ex-drinkers and never drinkers were included in the abstainer group.
It appears that the authors focused only on the “statistically significant” results rather than commenting on the overall pattern of association (lower risk of developing diabetes for moderate drinkers than for abstainers and heavier drinkers). Further, the number of subjects in many of the sub-groups was very small, making it difficult to define specific cut-points for effects of alcohol on risk.
Nevertheless, reviewers considered that, overall, these analyses support the usual findings from previous research of a “U-shaped curve” for alcohol and diabetes for both men and women. There appears to be a reduction in risk with moderate alcohol intake and possibly an increased risk for heavier drinking.
Reference: Cullmann M, Hilding A, Östenson CG. Alcohol consumption and risk of pre-diabetes and type 2 diabetes development in a Swedish population. Diabet Med 2012;29:441–452. DOI: 10.1111/j.1464-5491.2011.03450.x
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 076: Evaluating the association of alcohol intake with cognitive functioning using a Mendelian randomization study design — 22 March 2012
Many observational cohort studies have shown that moderate alcohol use is associated with better cognitive function. However, since such studies are vulnerable to residual confounding by other lifestyle and physiologic factors, the authors conducted a Mendelian randomization study, using aldehyde dehydrogenase 2 (ALDH2) genotype (AA, GA, or GG) as an instrumental variable in 2-stage least squares analysis. Cognitive function was assessed from delayed 10-word recall score (n = 4,707) and Mini-Mental State Examination (MMSE) score (n = 2,284) among men from the Guangzhou Biobank Cohort Study (2003–2008). The authors had previously reported an association between reported alcohol intake and cognitive function from a larger group of subjects from the same study finding that women reporting occasional alcohol intake and men reporting occasional or moderate intake had better scores related to cognitive function than did abstainers.1
In the present Mendelian study, the authors found no significant association between groups defined by the ALDH2 genotype (as an “unbiased” estimate of alcohol consumption) and the two measures of cognitive functioning. A problem with the present analysis is that ALDH2 genotypes explained only 3% of the variance in reported alcohol intake, which weakens the conclusions of the authors. Further, differences in the predominant type of beverage consumed (rice wine), and probably marked differences in drinking patterns between these subjects and Europeans and Americans, make it difficult to know what the implications of this study are for western industrialized societies.
We agree with the authors that “Causality should be thoroughly verified in a variety of settings using different kinds of evidence, including experimental or genetic studies, rather than relying on simple observations in a particular setting.” We strongly support future attempts at using Mendelian randomization studies, hopefully using better instruments for estimating alcohol intake. On the other hand, as stated by recent evaluations of various study designs for determining causality,3 we appreciate that Mendelian randomization sounds good, but it is not the “Holy Grail.”
Reference: Au Yeung SL, Jiang CQ, Cheng KK, Liu B, Zhang WS, Lam TH, Leung GM, Schooling CM. Evaluation of moderate alcohol use and cognitive function among men using a Mendelian randomization design in the Guangzhou Biobank Cohort Study. Am J Epidemiol 2012; pre-publication release. DOI: 10.1093/aje/kwr462
Please click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 075: Moderate drinking associated with lower risk of stroke in women — 15 March 2012
A well-done analysis from the Nurses’ Health Study shows that the risk of total stroke is slightly lower among light-to-moderate consumers of alcohol than among subjects reporting no alcohol intake. In comparison with non-drinkers, the estimated risk is 17-21% lower for women averaging up to 15 grams of alcohol per day (a little over one drink/day by US definitions of approximately 12 grams of alcohol for a typical “drink.”). For consumers of larger amounts of alcohol, the risk of stroke has a tendency to be slightly increased, but not statistically significantly so.
Data on the pattern of drinking (regularly, binge, etc.) were not reported. Among these predominantly light drinkers, there were no differences between effects on the risk of the most common type of stroke, ischemic stroke (due to atherosclerotic obstruction of a artery or an embolic clot) or the less-common hemorrhagic stroke (bleeding into the brain).
The results, with full adjustment for other factors that may affect risk, suggest a “J-shaped” curve for total stroke, with reductions in risk for light-to-moderate drinking and possibly an increase with greater amounts. In this study, the point at which the risk of drinkers exceeds that of non-drinkers was about 38 grams of alcohol per day (the equivalent of about 3 typical “drinks”), with a 95% confidence interval of 28 to 57 grams/day.
The study supports many previous reports from observational epidemiologic studies that have shown a slight reduction in risk of the ischemic type of stroke from moderate alcohol intake. Some, but not all previous studies, show an increase in hemorrhagic stroke for any amounts of alcohol, but that was not seen in this study, possibly because there were few heavy drinkers in this group of nurses.
Reference: Jimenez M, Chiuve SE, Glynn RJ, Stampfer MJ, Camargo Jr CA, Willett WC, Manson JE, Rexrode KM. Alcohol Consumption and Risk of Stroke in Women. Stroke 2012, pre-publication. http://stroke.ahajournals.org. DOI: 10.1161/STROKEAHA.111.639435
Please click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 074: Does moderate wine consumption improve lung function? — 8 March 2012
An analysis based on a prospective study in the Netherlands assessed the impact of wine and resveratrol intake on lung function. It also studied genetic factors (affecting sirtuin) that have been found to be mechanisms by which resveratrol relates to metabolism and longevity of life. The authors report that resveratrol intake was associated with higher lung volumes and that white wine intake (but not red wine intake) was associated with lower risk of airway obstruction. They report that the genetic factors studied did not relate to the associations found.
While several previous studies (as does this one) have reported that wine intake improves lung function, Forum reviewers were concerned about several aspects of the paper, and especially with the conclusions of the authors that resveratrol was the key factor in improved lung function. A reviewer stated: “Resveratrol may well be just the bystander of something else present in wine.” The beneficial effects on lung function are probably related to many compounds present in wine, and not just resveratrol.
Based on a number of scientific studies, moderate wine intake appears to have a favorable effect on lung function. The doses of resveratrol seen in these epidemiologic studies are in the physiological range that could be expected from moderate wine consumption, unlike the huge doses of resveratrol being evaluated as a potential life-extending drug in pharmaceutical studies.
Reference: Siedlinski M, Boer JMA, Smit HA, Postma DS, Boezen HM. Dietary factors and lung function in the general population: wine and resveratrol intake. Eur Respir J 2012; 39: 385–391; DOI: 10.1183/09031936.00184110
Please click here for the full critique by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 073: The association of alcohol consumption with osteoporosis — 5 March 2012
Osteoporosis is a key underlying factor in fractures among the elderly, which are increasingly a major health problem. A review paper from France on the association between alcohol consumption and bone metabolism states that heavy alcohol intake may adversely affect bone mineral density and increase the risk of osteoporosis. It states that lighter drinking may actually improve bone density, but presents very limited data to support this statement. Forum members were disappointed that the paper did not carry out a meta-analysis or other synthesis of the data; further, data from a number of key epidemiologic studies on the subject were not discussed in the paper.
The paper provides important information on the mechanisms by which alcohol may affect bone metabolism. The authors describe effects of alcoholic beverages on bone density, bone microarchitecture, bone remodeling, and other mechanisms, which help explain how alcohol and polyphenols and other constituents of beer and wine may relate to the risk of fractures in the elderly.
Unfortunately, despite what the authors’ conclude, the paper does not provide a summation of the scientific data upon which public health policy can be based. Overall, current scientific data suggest that bone mineral density and the risk of fractures are favorably affected by light-to-moderate drinking, but adversely affected by heavy drinking and alcoholism.
Reference: Maurel DB, Boisseau N, Benhamou CL, Jaffre C. Alcohol and bone: review of dose effects and mechanisms. Osteoporos Int (2012) 23:1–16; DOI 10.1007/s00198-011-1787-7.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 072: Obesity may modify the association between alcohol consumption and the risk of colorectal cancer. 23 February 2012
A case-control study from Newfound/Labrador has reported that greater alcohol intake may increase the risk of colorectal cancer among obese subjects, but not among non-obese subjects. This is not a particularly large study, and only 45-60% of subjects who were recruited by telephone ended up providing data. Further, it is a case-control comparison, rather than a cohort analysis, making bias in the results more likely.
In this study, there was no relation of alcohol with the risk of CRC when considering the entire population. However, when subjects were stratified by BMI (<30 versus ≥ 30), the data indicate an increase in CRC risk for obese subjects who were “drinkers” (OR=2.2, 95% CI 1.2-4.0), especially among subjects reporting 5 or more drinks/daily (OR=3.7, CI 1.5-9.0). On the other hand, even among obese subjects there was not a clear dose-response effect noted, i.e., there was not a step-wise increase in CRC risk with greater number of drinks/day For example, the odds ratio (OR) was 2.3 times that of non-drinkers for obese subjects reporting 1-2 drinks/daily and 1.3 for those reporting 3-4 drinks/daily.
It will be interesting to determine if other studies show that there is modification of the association between alcohol intake and colorectal cancer by obesity. If such is the case, it could help understand some of the mechanisms for the development of cancer and provide better guidelines for screening for CRC.
Reference: Zhao J, Zhu Y, Wang PP, et al. Interaction between alcohol drinking and obesity in relation to colorectal cancer risk: a case-control study in Newfoundland and Labrador, Canada. BMC Public Health2012, 12:94 doi:10.1186/1471-2458-12-94
Please click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 071: Forum Comments on proposed new dietary guidelines for Australia — 16 February 2012
Members of the International Scientific Forum on Alcohol Research have provided comments on the chapter related to alcohol intake that has been included in “A review of the evidence to address targeted questions to inform the revision of the Australian Dietary Guidelines,” by the Australian Government Department of Health and Ageing and National Health and Medical Research Council (NHMRC), November 2011, ISBN Online 1864965304.
Forum members considered that the authors of the report should be commended on their work. Criticisms are primarily about the restriction in the time frame of the review, and minimal consideration of key nuances, such as quantity of alcohol consumed and its relation to risk or benefit, patterns of drinking, the balance between risks and benefits, and making statements at all when the evidence is too weak. More details (e.g. considering cardiovascular mechanisms to widen the search) would have added weight to the conclusions.
For the full comments of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 070: Potentially important new mechanisms found for the anti-aging effects of resveratrol, a phenolic compound found in red wine — 9 February 2012
A well-conducted experimental study in mice has provided potentially important new insights into the association of the intake of resveratrol and like compounds with health benefits. Resveratrol is a constituent of red wine and other vegetable products, and is being evaluated in high-doses as a pharmaceutical. The biologic mechanisms demonstrated in this study could provide key new approaches for the prevention or treatment of a number of chronic diseases in humans, especially those related to vascular and metabolic diseases and to the risk of mortality.
More than two decades ago, particularly through publicity related to the so-called “French Paradox,” the public became aware of the potential reduction in the risk of coronary heart disease from the moderate consumption of red wine, and the media focused on a single constituent in red wine, resveratrol, as being the “key” factor. We now know that resveratrol is only one of hundreds of phenolic compounds in wine, many of which have been shown to have beneficial effects on vascular function, and that alcohol itself (present in wine, beer or spirits) also provides considerable protection against heart disease. Still, there has remained considerable attention paid to resveratrol, and extensive scientific research on resveratrol and related substances have shown that, in high doses, they may increase longevity of life and reduce metabolic diseases of aging.
In general, Forum reviewers thought that this was a very well-done study. Their concerns related to the dose used in these experiments; while the levels of resveratrol and like compounds might be accessible with pharmaceutical doses, the suggestion that similar levels could be connected with wine consumption is misleading. Further, in humans, resveratrol in the diet will interact with many other chemicals to achieve an effect, as whole plant extracts consist of many active and inactive micronutrients that may play a role in health and disease. To ascribe a specific effect on health from one chemical found in wine or other plant products could be misleading.”
Still, the reviewers believed that this paper was an important contribution to our knowledge about the mechanisms by which resveratrol and other chemicals may play a role in cardiovascular and other diseases. Such knowledge could help develop approaches for the prevention and treatment of human disease and for increasing the longevity of a healthy life.
Reference: Park S-J, Ahmad F, Philp A, Baar K, Williams T, Luo H, Ke H, Rehmann H, Taussig R, Brown AL, Kim MK, Beaven MA, Burgin AB, Manganiello V, Chung JH. Resveratrol ameliorates aging-related metabolic phenotypes by inhibiting cAMP phosphodiesterases. Cell 2012;148:421-433. DOI 10.1016/j.cell.2012.01.017.
Click here for the full critique of this paper by the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 069: Little effect of binge drinking on heart disease or mortality among moderate drinkers in Denmark — 2 February 2012
In a well-done, population-based analysis from Denmark, it was found that subjects who were overall “light-to-moderate” drinkers but reported an episode of “binge drinking” (consumption >5 drinks on an occasion) did not show differences in risk of ischemic heart disease (coronary disease) or total mortality than did other moderate drinkers who did not report such an episode. These results are somewhat different from results of many other epidemiologic studies that have shown increased risk of health problems (even higher risk of coronary disease) to be associated with what was referred to as “binge drinking.”
Why there were no adverse effects of such drinking in the present study has provoked considerable discussion among members of the Forum. The general consensus of opinion has to do with inconsistencies in the definition of “binge drinking.” The rapid consumption of more than 5 drinks on an empty stomach surely has different effects than the consumption of alcohol over several hours with food, such as during a prolonged dinner. The rate of consumption strongly affects the consequences of alcohol; in fact, some have suggested that the consumption of more than 2 or 3 drinks in less than two hours may constitute a better definition of binge that the total number of drinks.
The Forum continues to suggest that “binge drinking,” however defined, is not a healthy pattern of alcohol consumption. But the circumstances of consumption (rate of consumption, with or without food, etc.) may also be important in its definition and in judging its effects on health.
Reference: Skov-Ettrup LS, Eliasen M, Ekholm O, Grønbaek M, Tolstrup JS. Binge drinking, drinking frequency, and risk of ischaemic heart disease: A population-based cohort study. Scandinavian Journal of Public Health 2011;39:880–887.
Click here for the full critique of this study by the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 068. Heavier alcohol consumption may increase risk of colon cancer in people with a family history of such cancer — 30 January 2012
An analysis based on a large number of subjects being followed in the Nurses’ Health Study and the Health Professionals Follow-up Study, relates alcohol consumption to the risk of colon cancer according to whether or not the subjects had a positive family history of colon cancer. Their results indicate that subjects with a family history whose average alcohol intake was 30 or more grams per day (about 2 ½ typical drinks by US standards) have an increase in their risk of colon cancer; there was not a significant association between alcohol and colon cancer among subjects without a positive family history.
Forum reviewers were somewhat concerned that the pattern of drinking (regularly or binge drinking) was not assessed, and that there was not a clear dose-response curve between the level of alcohol consumption and the risk of cancer (i.e., there was not a consistent increase in risk of cancer with greater alcohol intake). Further, folate intake was found to modify the association, with the highest risk for subjects with a positive family history of colon cancer, low levels of folate, and in the highest category of alcohol consumption.
The present study provides some support for an association between higher levels of alcohol intake and the risk of colon cancer among subjects with a positive family history of such cancer. However, there have been changes in the guidelines for screening for cancer (by endoscopy, with removal of pre-malignant tumors) and other preventive measures for people with a positive family history of colon cancer. Such measures could modify the effects of all risk factors for colon cancer in future analyses.
Reference: Cho E, Lee JE, Rimm EB, Fuchs CS, Giovannucci EL. Alcohol consumption and the risk of colon cancer by family history of colorectal cancer. Am J Clin Nutr 2012;95:413–419.
Click here for the full critique of this paper by the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 067: Comparison of effects of red wine versus white wine on hormones related to breast cancer risk 19 January 2012
Aromatase inhibitors (AIs) prevent the conversion of androgens to estrogens, and could play a role in the development of breast cancer. This study of 36 pre-menopausal women consisted of a cross-over intervention trial to determine if there were differences between red wine and white wine in their effects on AIs. Subjects sequentially consumed eight ounces of red wine, followed by white wine (or vice versa), each beverage for a one-month period. The investigators concluded that red wine, but not white wine, was associated with significant effects on some indices of estrogen metabolism; free testosterone and luteinizing hormone were increased, but no significant differences were noted in estrogen levels.
Forum reviewers considered the results interesting and that they contribute to our understanding of the relation of wine to hormonal levels. On the other hand, they were concerned about methodological problems, including a lack of baseline data and variations in the timing during the menstrual period of blood sampling (which could affect estrogen levels). Also, no significant effect of the interventions was seen on blood levels of estradiol.
Further, the Forum thought that it should be pointed out that data are inconsistent on the relation of red wine consumption to the risk of breast cancer; many studies do not show beverage-specific effects on risk. More research will be needed to determine if the polyphenols in red wine can play a role in lowering the risk of breast cancer.
Reference: Shufelt C, Bairey Merz CN, Yang YC, Kirschner J, Polk D, Stanczyk F, Paul-Labrador M, Braunstein GD. Red versus white wine as a nutritional aromatase inhibitor in premenopausal women. J Women’s Health, 2011;DOI: 10.1089/jwh.2011.3001
Click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 066: Is it the alcohol or the polyphenols in red wine (or both) that decrease cardiovascular disease in wine drinkers? 16 January 2012
Human randomized intervention trials of wine and alcohol are not common. This randomized, cross-over study was based on 67 male volunteers in Spain who were considered to be at “high-risk” of cardiovascular disease. The subjects agreed to not consume any alcohol for a baseline period, then for three one-month periods consumed 30 g/day of alcohol as red wine or as gin, or an equivalent amount of phenolics from dealcoholized red wine. The effects of each intervention on a large number of adhesion molecules and chemokines that affect inflammation and relate to the development of vascular disease were evaluated.
The key results of the study were that both ethanol and nonalcoholic compounds in red wine have potentially protective effects that may reduce the risk of vascular disease. Specifically, the authors conclude that “the phenolic content of red wine may modulate leukocyte adhesion molecules, whereas both ethanol and polyphenols of red wine may modulate soluble inflammatory mediators in patients at high risk of cardiovascular disease.” Thus, this study provides important new mechanistic evidence that the reduced risk of cardiovascular disease among red wine drinkers observed in most epidemiologic studies may result from a combination of both the alcohol and the polyphenols in the wine.
Reference: Chiva-Blanch G, Urpi-Sarda M, Llorach R, Rotches-Ribalta M, Guillèn M, Casas R, Arranz S, Valderas-Martinez P, Portoles O, Corella D, Tinahones F, Lamuela-Raventos RM, Andres-Lacueva C, Estruch R. Differential effects of polyphenols and alcohol of red wine on the expression of adhesion molecules and inflammatory cytokines related to atherosclerosis: a randomized clinical trial. Am J Clin Nutr 2012. doi: 10.3945/ajcn.111.022889.
Click here for the full critique of this paper by members of the International Scientific Forum on Alcohol Research.
===============================================================================
Critique 065: Are there differences in mortality between people consuming wine and those consuming other types of alcoholic beverages? 20 December 2011
Wine consumers, especially in comparison with spirits drinkers, have been shown to have higher levels of education and income, to consume a healthier diet, be more physically active, and have other characteristics that are associated with better health outcomes. However, epidemiologic studies have been inconsistent in showing that, after adjustment for all associated lifestyle factors, consumers of wine have lower risk of cardiovascular disease and mortality than do consumers of other beverages.
A study based on the long-term follow up of a group of older Americans concluded that the associated lifestyle habits and environmental factors of wine consumers largely explained their better health outcomes. Forum reviewers were concerned about some of the methodological approaches used, and believed that the data presented in the paper were inadequate to support such a conclusion. This was a small study, had only a single estimate of alcohol intake (at baseline but not throughout 20 years of follow up), and the authors may have over-adjusted for large differences in lifestyle factors between what they termed as “low-wine” and “high-wine” consumers. The study did confirm a lower mortality risk for alcohol consumers than for non-drinkers.
Experimental studies have clearly indicated that the polyphenols and other constituents that are present in wine and some beers have independent protective effects against most cardiovascular risk factors. Whether or not such advantages are seen among moderate drinkers of wine (or beer) in epidemiologic studies is difficult to determine, as comparisons are not being made between wine, beer, and spirits but between humans who consume one or other such beverage. In almost all populations, drinkers of a specific beverage differ in many ways other than just the type of beverage they consume.
Reference: Holahan CJ, Schutte KK, Brennan PL, North RJ, Holahah CK, Moos BS, Moos RH. Wine consumption and 20-year mortality among late-life moderate drinkers. J Stud Alcohol Drug 2012; 73: 80–88.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 064: Association of lifestyle and environmental factors with the risk of cancer — 13 December 2111
It has been well established that certain lifestyle habits relate to the risk of certain cancers (e.g., smoking and lung cancer). In a well-done analysis, the authors estimate the proportion of cancer in the population associated with a variety of lifestyle and environmental factors. They find that smoking has, by far, the largest effect on the risk of cancer, with 19.4% of cancer cases in the UK attributable to tobacco use. A poor diet (less intake of fruits and vegetables and fiber and greater intake of meat and salt), obesity, and alcohol are the next most important factors that relate to cancer, with alcohol being calculated to relate to 4.0% of cancer cases in the UK.
Forum reviewers considered this to be a well-done paper that used epidemiologic methods that are preferable to those used in some previous such analyses. Generally, they disagreed with the authors that no alcohol consumption was the theoretical “optimum exposure level,” as the risk of certain cancers seems to increase primarily from heavy drinking. Further, they found reason to believe that the purported effects related to diet may have been over-estimated.
Nevertheless, this paper provides considerable new information on lifestyle and environmental factors that may relate to the risk of cancer. It puts into perspective the importance of targeting certain behaviors for the potential reduction in the risk of cancer.
Reference: Parkin DM, Boyd L, Walker LC. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. Summary and conclusions. British Journal of Cancer 2011;105:S77 – S81.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 063: Genes modify the risk of liver disease among alcoholics — 5 December 2011
It has been widely observed that only a small percentage of alcoholics develop cirrhosis of the liver, the most advanced form of alcoholic liver disease (ALD); the reason why all alcoholics do not develop such disease is not known. The present study from Spain, that includes original work and a meta-analysis, evaluates whether genetic polymorphisms that determine levels of glutathione-S-transferases (GST) relate to the risk of developing ALD among alcoholics. Alcoholics with certain genetic GST polymorphisms were found to be at significant excess risk for such liver disease in comparison with alcoholics without these polymorphisms.
As stated by the authors, the theory that these enzymes may affect risk is based on the ability of certain GST alleles to detoxify harmful ethanol metabolites in the liver by conjugating acetaldehyde and ROS to reduced glutathione. The specific polymorphisms that they found to be associated with increased liver disease are among those that would be expected to lower the activity of the corresponding GST enzymes; this would permit higher levels of toxic metabolites of alcohol and oxidative stress to be present for longer periods of time after excessive alcohol consumption.
Some Forum reviewers thought that while the study was well done, the authors were unclear as to how these data could directly lead to “potential therapeutic targets” for liver disease in alcoholics. Nevertheless, the original study and meta-analysis provide important data on how specific genetic factors relate to the development of liver disease among alcoholics and could theoretically lead to better strategies for the prevention and treatment of alcoholic liver disease.
Reference: Marcos M, Pastor I, Chamorro A-J, Ciria-Abad S, González-Sarmiento R, Laso F-J. Meta-analysis: glutathione-S-transferase allelic variants are associated with alcoholic liver disease. Aliment Pharmacol Ther 2011;34:1159–1172.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 062: Similar effects of beer and wine on the risk of cardiovascular disease and of total mortality — 22 November 2011
The authors carried out an updated meta-analysis on the relationship between wine, beer or spirit consumption and cardiovascular outcomes, using state-of-the-art statistical techniques. Their meta-analysis provides evidence of J-shaped relationships between both wine and beer intake and vascular risk, with maximal protection of about 33% at a level of 25 g/day of alcohol (approximately 2 drinks/day by US standards). A statistically significant association between spirits intake and vascular disease was not found.
The key result of this meta-analysis is the finding of a very similar inverse association between the consumption of beer and the consumption of wine in relation to cardiovascular outcomes. While a similar associationwas not seen for spirits consumption, the data presented do not permit the conclusion that the key effects on cardiovascular disease are primarily due to the polyphenols in beer and wine. Similarly, the results do not permit the conclusion that the effect on cardiovascular disease is due primarily to the alcohol in these beverages. The lack of a similar J-shaped association for spirits may have been due to different drinking patterns (e.g., more binge drinking among consumers of spirits), as the pattern of drinking was not included as a confounder in the analyses.
Reference: Costanzo S, Di Castelnuovo A, Donati MB, Iacoviello L, de Gaetano G. Wine, beer or spirit drinking in relation to fatal and non-fatal cardiovascular events: a meta-analysis. Eur J Epidemiol 2011;DOI 10.1007/s10654-011-9631-0
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
A response from the Alcohol Policy Coalition of Australia to the Forum Critique #058: “A misguided statement on alcohol and health from a coalition in Australia,” which was published on the Forum web-site on 28 September 2011.
The Alcohol Policy Coalition of Australia has provided a response to Forum critique #058, “A misguided statement on alcohol and health from a coalition in Australia,” that was published on the Forum web-site on 28 September 2011.
The original Forum critique is available under Recent Reviews, #058 (click Critique o58). A description of the Forum, its members, the goals of the Forum, a disclosure statement, etc., are available from the home page of the web-site.
The response from the Alcohol Policy Coalition is now published in full on our web-site, dated 18 November 2011. To read the response to our critique # 058 provided by the Alcohol Policy Coalition, please click here.
===============================================================================
Critique 061: The reduction in risk of coronary heart disease from alcohol consumption may involve mechanisms other than an increase in HDL-cholesterol. 10 November 2011
In a prospective, observational study of approximately 150,000 Norwegians, the investigators found that alcohol consumption was associated with a large decrease in the risk of death from coronary artery disease. For men, the fully adjusted hazard ratio for cardiac death was 0.52 (95% CI 0.39 – 0.69) when comparing subjects reporting more than one drink/week in comparison with those reporting never or rarely drinking; for women, it was 0.62 (0.32–1.23). There was little change in the hazard ratio when HDL-cholesterol (HDL) was added to the model, suggesting that very little of the lower risk of heart disease was due to an increase in HDL from alcohol consumption.
Forum members considered this a well-done analysis. They were surprised at the very low amounts of alcohol intake reported by the subjects, with only 16% of males and about 8% of females reporting more than one drink/week. It is possible that the low levels of drinking, or perhaps over-adjustment in the multivariable analysis, led to the lack of effect of HDL. Most other studies have shown a much larger proportion of the effect of alcohol on heart disease risk to be associated with an increase in HDL.
Reference: Magnus P, Bakke E, Hoff DA, Høiseth G, Graff-Iversen S, Knudsen GP, Myhre R, Normann PT, Næss Ø, Tambs K, Thelle DS, Mørland J. Controlling for High-Density Lipoprotein Cholesterol Does Not Affect the Magnitude of the Relationship Between Alcohol and Coronary Heart Disease. Circulation 2011;124: DOI: 10.1161/CIRCULATIONAHA.111.036491
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 060: A new analysis from the Nurses’ Health Study on the association of alcohol with risk of breast cancer 3 November 2011
In a well-done analysis using prospectively collected data from the Nurses’ Health Study, the risk of breast cancer was found to be modestly increased among consumers of alcohol, even those whose total alcohol consumption was reported to be in the range of 3 to 6 drinks/week. Similar small increases in the risk of breast cancer have been found from alcohol consumption in the majority of previous studies observational studies. A strength of this study was the very large number of subjects, permitting the investigators to attempt to determine if both the amount of alcohol and the frequency of consumption were important in this association; strong effects were not found for either. A weakness is the failure to report the effects of folate intake on the association between alcohol and cancer; the same investigators have previously shown that folate is a potential moderator of the effects of alcohol on breast cancer risk.
The authors describe well the dilemma that women face regarding alcohol intake, which may increase slightly the risk of breast cancer but markedly decrease the risk of other more common diseases, especially cardiovascular conditions. For example, the authors state that regarding breast cancer, “We did find an increased risk at low levels of use, but the risk was quite small.” Forum members agree with the statement of the authors that “An individual will need to weigh the modest risks of light to moderate alcohol use on breast cancer development against the beneficial effects on cardiovascular disease to make the best personal choice regarding alcohol consumption.”
Reference: Chen WY, Rosner B, Hankinson SE, Colditz GA, Willett WC. Moderate alcohol consumption during adult life, drinking patterns, and breast cancer risk. JAMA 2011;306:1884-1890.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 059: Association of quantity of alcohol and frequency of consumption with cancer mortality
20 October 2011
A paper from the National Institutes of Health in the United States attempts to evaluate the separate and combined effects of the frequency of alcohol consumption and the average quantity of alcohol per occasion as they relate to the risk of mortality from all cancers, as well as cancer-specific mortality. It is based on repeated administrations of the National Health Interview Survey in the United States, with a total of more than 300,000 subjects and over 8,000 deaths from cancer, and reports on total cancer deaths and deaths from lung, colorectal, prostate, and breast cancers.
For total alcohol consumption (frequency x quantity), the data indicate a significant reduction in the risk of all-site cancers (RR=0.87, CI 0.80-0.94) which, interestingly, is not emphasized by the authors and is not included in their abstract. Moderate drinking consistently shows no effect, and only heavier drinking is associated with an increase in all-site cancer risk. For site-specific cancers, an increase in risk of lung cancer was seen only for heavier drinkers, with a tendency for less cancer among light drinkers. There was no evidence of an effect of total alcohol consumption on colorectal, prostate, or breast cancer.
The authors excluded non-drinkers in a second analysis in which they used categories of usual daily quantity and of frequency of consumption in an attempt to investigate their separate effects. For all-site cancer and for lung cancer, these results again show an increase in risk only for drinkers reporting greater amounts of alcohol. The data also show an increase in cancer risk from more frequent drinking among women but not among men. For colorectal, prostate, and breast cancer, there is no clear pattern of an increase in risk from quantity of alcohol consumed. For frequency of drinking, again there is a suggestion of an increase in risk with more frequent drinking, although the trends are not statistically significant.
The overall message of this analysis is that light to moderate alcohol intake does not appear to increase the risk of all-site cancer (and light drinking was shown in this study to be associated with a significant decrease in risk). Similarly, light to moderate consumption was not associated with site-specific cancers of the lung, colorectum, breast, or prostate. Heavier drinking is known to be associated with a large number of adverse health effects, including certain cancers, as was shown in this study.
When considering cancer, alcohol consumption should not be considered in isolation, but in conjunction with, other lifestyle behaviors (especially smoking). We agree with the authors that both quantity and frequency of consumption need to be considered when evaluating the relation of alcohol to cancer; further, beverage-specific effects need to be further evaluated.
Reference: Rosalind A. Breslow RA, Chen CM, Graubard BI, Mukamal KJ. Prospective study of alcohol consumption quantity and frequency and cancer-specific mortality in the US population. Am J Epidemiol 2011; DOI: 10.1093/aje/kwr210.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 058: A misguided statement on alcohol and health from a coalition in Australia. 28 September 2011
A group known as the Alcohol Policy Coalition in Australia has released a document entitled Cancer, Cardiovascular Disease and Alcohol Consumption. Forum members agree that excessive alcohol use has many adverse effects on the individual and on society, and efforts to reduce such use are important. On the other hand, they were disturbed that the coalition statement was limited almost exclusively to the effects of abusive drinking, was based primarily on extremely limited sources of information (mainly position statements by other organizations, and not publications based on sound research), and indicated a strong bias against alcohol.
Forum members contend that the Australian report misrepresents the extensive scientific data available on alcohol and health. The report specifically ignores scientific data indicating that in all developed countries, moderate consumers of alcohol are at much lower risk of essentially all of the diseases of ageing: coronary heart disease, ischemic stroke, diabetes, and dementia. And conspicuously absent from the Australian report is a description of the lower total mortality among middle-aged and elderly people associated with moderate alcohol consumption, a finding that has been found consistently throughout the world. Further, there is no mention in the report of the key relevance of the pattern of drinking, although regular moderate drinking (versus binge drinking only on week-ends, even when the total volume of alcohol is the same) has been shown to be a strong determinant of beneficial effects of alcohol consumption.
Scientific data over many decades have shown that while excessive or irresponsible alcohol use has severe adverse health and societal effects, regular moderate drinking is associated with beneficial effects on health. And a very large number of experimental studies, including results from human trials, have described biological mechanisms for the protective effects of both alcohol and the polyphenolic components of wine.
There have been a number of comprehensive meta-analyses published that Forum members believe can provide much more accurate, up to date, and scientifically balanced views of the current status of the health effects of alcohol consumption. Such documents are better sources of data upon which policy decisions should be based.
Reference: Alcohol Policy Coalition Position Statement. “Cancer, Cardiovascular Disease and Alcohol Consumption.” Released in Australia, September 2011.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 057: Differences in effects on atherosclerosis of regular moderate drinking and binge drinking. An experimental study in mice. 20 September 2011
An excellent study among experimental animals has reported very dramatic differences between the effects of alcohol administered in moderation on a daily basis and the same total weekly amount of alcohol administered on only two days of the week: binge drinking. The mice used in the study that were given regular moderate amounts of alcohol showed no weight gain, improved lipid values, and much less development of atherosclerosis than did control animals. However, those given alcohol in a binge-drinking pattern showed worse outcomes than control animals, and much worse outcomes than those given regular moderate alcohol.
This experimental study provides strong support for the frequent finding among humans in epidemiologic studies: benefits from regular moderate drinking, adverse effects from binge drinking. It is especially important since, being an experimental study, the potential confounding effects of other lifestyle habits are not an issue, as is always the case for observational studies among humans.
Reference: Liu W, Redmond EM, Morrow D, Cullen JP. Differential effects of daily-moderate versus weekend-binge alcohol consumption on atherosclerotic plaque development in mice. Atherosclerosis 2010, doi:10.1016/j.atherosclerosis.2011.08.034
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 056: Relation of alcohol consumption to colorectal cancer 13 September 2011
A meta-analysis of case-control and cohort studies on the association of alcohol consumption with colorectal cancer was carried out, based on 22 studies from Asia, 2 from Australia, 13 from Western Europe, and 24 from North America. The paper provides evidence that alcohol, at least at higher levels of consumption, is associated with an increase in the risk of colorectal cancer. Overall, there was no increase in the risk for consumers reporting an average intake of up to 1 drink per day, but a modest increase (of 21%) for what the authors defined as “moderate drinking” (averaging up to 49.9 g of alcohol, or about 4 typical drinks, per day). The increase in risk was greater (52%) for consumers of 50 or more grams of alcohol per day.
Forum reviewers thought that this was, in general, a very well-done study that used appropriate statistical techniques for meta-analysis. There were some key concerns, however, including the following: (1) the authors’ definition of “moderate drinking” extended well above the usual recommended limits for sensible drinking; effects of consumption in categories of 1 to 2 drinks/day, 2 to 3 drinks/day, etc., were not given; (2) no results were provided according to type of beverage even though many previous studies have shown differences between health effects for consumers of wine, or wine/beer, and other beverages; and (3) no data were available on the pattern of drinking. Many studies have shown that regular, moderate drinking on most days of the week has very different health outcomes than drinking only on week-ends or binge drinking.
Despite these concerns, Forum members agreed that current data indicate that alcohol intake, especially heavier drinking, is associated with an increase in the risk of colorectal cancers. Future studies are needed to help determine if there is a threshold level of alcohol that increases the risk, if there are differences by type of beverage, and if the pattern of drinking (regular versus binge drinking) affects the risk.
Reference: FedirkoV, Tramacere I, Bagnardi V, Rota M, Scotti L, Islami F, et al. Alcohol drinking and colorectal cancer risk: an overall and dose–response meta-analysis of published studies. Annals of Oncology 22: 1958–1972, 2011, doi:10.1093/annonc/mdq653
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 055. Alcohol intake and “successful ageing” 8 September 2111
Among 13,894 women in the Nurses’ Health Study, investigators prospectively examined alcohol use assessed at midlife in relation to “successful ageing,” which was defined as survival to age 70 years, not having a major chronic disease (such as coronary disease, cancer, stroke, diabetes), and having no major cognitive impairment, physical impairment, or mental health problems. Only 11% of the women met these criteria.
The results indicate that moderate drinkers, especially those consuming wine and drinking regularly, were more likely to exhibit successful ageing. For average amount consumed, the largest benefit (an increase of 28%) was among women who reported 15.1 – 30 g of alcohol per day (an average of just over 1 to 2 ½ drinks per day), when compared with non-drinkers. The frequency of drinking was especially important: in comparison with nondrinkers, women who drank only on 1 to 2 days per week had little increase in their risk of successful ageing, but those drinking on at least 5 days per week had almost a 50% greater chance of successful ageing.
Forum reviewers had some questions about the definition of “successful ageing” used in this study. It is believed that a much greater percentage of people who may not meet these criteria make huge contributions to society and should be considered “successful.”
In summary, these results support the findings of earlier studies showing that many aspects of successful ageing, in addition to just survival, are favorably affected by regular, moderate consumption of alcohol.
Reference: Sun Q, Townsend MK, Okereke OI, Rimm EB, Hu FB, Stampfer MJ, Grodstein F. Alcohol consumption at midlife and successful ageing in women: A prospective cohort analysis in the Nurses’ Health Study. PLoS Med 8(9): e1001090. doi:10.1371/journal.pmed.1001090
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 054. Role of alcohol intake and smoking on upper aerodigestive cancers – 6 September 2011
This paper provies an extensive analysis of the proportion of the risk of upper aero-digestive tract (UADT) cancers in the population (the population attributable risk) may be due to alcohol consumption and/or smoking. The analyses provide strong evidence that smoking is the most important factor in the risk of these cancers, and the risk is enhanced among those who also consume 2 or more drinks per day. Alcohol alone (i.e., among non-smokers) has little effect on the risk.
The authors state that their observations “are consistent with the hypothesis that alcohol acts as a carcinogen primarily because of its promoting effect on tobacco smoke.” In terms of the population-attributable risk, the authors conclude that “Our findings confirm that tobacco and alcohol together explain 73% of total UADT cancer burden in Europe.” Overall, tobacco use alone explained 28.7%, the combination of smoking and drinking 43.9%, and alcohol use alone only 0.4% of the population attributable risk. Among women, the risk of these cancers was higher among smokers than among those who both smoked and consumed alcohol; this perhaps suggests that the moderate intake of wine, the most common beverage among European women, may play a role in reducing the risk associated with smoking.
Forum reviewers thought that this was a very good paper, but hoped that in the future we would have more studies that evaluated the effects on risk of varying levels of alcohol consumption, differential effects of various beverages, and even differential effects according to subjects’ genetically determined differences in alcohol metabolizing enzymes.
Reference: Anantharaman D, Marron M, Lagiou P, Samoli E, Ahrens W, Pohlabeln H, et al. Population attributable risk of tobacco and alcohol for upper aerodigestive tract cancer. Oral Oncology 2011;47:725–731.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 053: An extensive review of the effects of alcohol consumption on the risk of cognitive impairment and dementia 25 August 2011
The authors of this paper have carried out an excellent review of the relation of alcohol consumption to the risk of cognitive impairment and dementia. They reviewed a total of 143 previous publications on the topic. There were 74 studies, based on a total of more than 250,000 subjects, that provided risk estimates for varying levels of alcohol consumption which allowed the investigators to include them in a comprehensive meta-analysis. These papers were published mainly after 1998, were predominantly among older subjects (92% were ≥ 55 years of age and 70% ≥ 65 years of age), and almost all employed mental status examinations to define cognitive impairment/dementia.
As stated by the authors, “These studies overwhelmingly found that moderate drinking either reduced or had no effect on the risk of dementia or cognitive impairment.” Overall, in the new meta-analysis based on these studies, the average ratio of risk for cognitive risk associated with moderate drinking of alcohol was 0.77, with nondrinkers as the reference group. This estimate is close to the estimates of reduction in the risk of cognitive dysfunction (RR of 0.73 and 0.74) seen in other recent selective meta-analyses. The present study found that both light and moderate drinking provided a similar benefit, but heavy drinking was associated with non-significantly higher cognitive risk for dementia and cognitive impairment.
Forum reviewers of this paper were particularly pleased that the authors attempted to answer a number of specific questions on this topic that have been raised from previous research. Their results included finding no appreciable differences whether or not “sick quitters” were included in the reference group, little effect from adjustments for other lifestyle factors, and no significant differences between alcohol’s effects on dementia, Alzheimer’s dementia, or vascular dementia (but, based on a small number of studies, no significant reduction in risk of cognitive decline over time). The investigators concluded that there were no differences between results in men and women. Their analyses also led to the conclusion that wine is associated with more beneficial effects on cognition than beer or spirits, but the authors caution that these results are based on a limited number of reports, and that many studies show no significant differences according to type of beverage.
Forum reviewers agreed with the conclusions of the authors that “Overall, light to moderate drinking does not appear to impair cognition in younger subjects and actually seems to reduce the risk of dementia and cognitive decline in older subjects.”
Reference: Neafsey EJ, Collins MA. Moderate alcohol consumption and cognitive risk. Neuropsychiatric Disease and Treatment 2011:7:465–484.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 052: Does moderate alcohol consumption increase body weight? 16 August 2011
A paper from Spain provides an extensive review of the association between alcohol consumption and body weight. It includes descriptions of cross-sectional and prospective studies (and a few small intervention studies) among subjects who varied in age (adolescence to old age), culture (from Americans and Europeans to Asians), and principal type of beverage consumed and pattern of drinking. The authors state that many of the studies they reviewed appear to be contradictory in their results. However, based on their review, they conclude that “as positive associations between alcohol and weight gain were mainly found in studies with data on higher levels of drinking, it is possible that an effect on weight gain or abdominal adiposity may only be experienced by heavy drinkers.” A second conclusion of the authors is that “the type of alcoholic beverage might play an important role in modifying the effect of alcohol consumption on weight gain,” with more favorable effects generally seen among consumers of wine. A formal meta-analysis is not provided. Forum members were uncertain whether the higher risk seen for spirits drinkers in this study was due to the beverage they chose or to their consumption of larger amounts of alcohol.
The overall conclusions of the authors is that it is currently unclear whether alcohol consumption a risk factor for weight gain, but if so it appears to occur mainly among heavier drinkers. They also state that “light-to-moderate alcohol intake, especially of wine, may be more likely to protect against, rather than promote, weight gain.”
Forum reviewers agreed with most of the conclusions of the authors, especially that current data do not clearly indicate if moderate drinking increases weight; further, the biologic mechanisms relating alcohol to changes in body weight are not well understood. The Forum review comments on the strong protective effects of moderate drinking on the risk of metabolic syndrome and diabetes, both of which relate to increasing obesity. And some studies suggest that even very obese people may be at lower risk of diabetes if they are moderate drinkers. Forum members also reviewed some of the distinctive mechanisms by which alcohol is metabolized in the body (it provides calories that are rapidly absorbed and are not stored in fat) that could explain differences in the effects of calories from alcohol and from other foods.
Forum members agree with the authors of this paper that future research efforts should be directed towards assessing the specific roles of different types of alcoholic beverages, taking into account drinking patterns, and perhaps including in the analysis the propensity of individual subjects to gain weight in the past. For now, there is little evidence that someone consuming small to moderate amounts of alcohol on a regular basis is increasing his or her risk of becoming obese.
Reference: Sayon-Orea C, Martinez-Gonzalez MA, Bes-Rastrollo M. Alcohol consumption and body weight: a systematic review. Nutrition Reviews 2011;69:419-431.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 051: Types of alcohol in relation to acute pancreatitis 11 August 2011
A very well-done analysis from scientists in Sweden has related the type of alcoholic beverage, and the amount consumed per occasion, to the risk of acute pancreatitis. The study suggests that a greater number of drinks per occasion (“binge drinking”) of spirits increases the risk of acute pancreatitis, but no such relation was seen for the consumption of beer or wine. Forum reviewers suggested that a faster rate of drinking, with a greater rise in BAC, for spirits drinkers may be an important factor in the observed higher risk of pancreatitis; the increased risk may not necessarily be due to lower levels of antioxidants or to the presence of other toxic substances in spirits.
In any case, the average total alcohol consumption did not affect the risk of pancreatitis; instead, it was the number of drinks consumed per occasion (of spirits, in this study) that was associated with an increase in risk. Residual confounding by the pattern of drinking, diet, or by other lifestyle factors could still be operating, and it will require replication of these results in other studies to support the conclusions of the authors.
Reference: Azodi OS, Orsini N, Andrén-Sandberg Å, Wolk A. Effect of type of alcoholic beverage in causing acute pancreatitis. Brit J Surgery 2011;DOI: 10.1002/bjs.7632.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 050: Multiple maternal risk factors for fetal alcohol disorders 7 August 2011
An extremely well researched and written review on the relation of maternal drinking during pregnancy to adverse fetal outcomes has been published by scientists from the University of New Mexico Center on Alcoholism, Substance Abuse, and Addictions. It covers many factors (host, agent exposure, and environment) that have been found to relate to the occurrence of fetal alcohol spectrum disorders (FASD). Such factors modify the risk associated with alcohol consumption during pregnancy, although the risk of abnormalities is clearly increased with frequent consumption of large amounts of alcohol, and is greater among women who are alcoholics. While current data do not show that light or occasional alcohol consumption during pregnancy increases the risk of FASD, Forum members do not believe that pregnant women should be encouraged to drink.
Forum members agree with the authors that “More research is needed to more clearly define what type of individual behavioral, physical, and genetic factors are most likely to lead to having children with FASD.” Evaluating these multidimensional factors should help identify women at particular risk for having a child with FASD and lead to interventions to prevent such fetal abnormalities.
Reference: May PA, Gossage JP. Maternal risk factors for fetal alcohol spectrum disorders. Not as simple as it might seem. Alcohol Research & Health 2011;34:15-26.
For the full critique of this article by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 049: Effects of smoking and alcohol use on risk of upper aero-digestive cancers 1 August 2011
A case-control analysis from subjects living in areas of South America with high rates of upper aero-digestive tract cancers showed that both alcohol consumption and smoking tended to increase the risk of such cancers. However, the predominant cause of these cancers was the combination of smoking and alcohol consumption, with much higher risk than either exposure alone. The effects on risk were greater for smoking than for alcohol: for non-smokers, there was little effect of alcohol on risk. For non-drinkers, the risk of cancer associated with smoking was still increased, but was lower than it was for current drinkers.
An especially important finding in this study was that, among ex-drinkers and former smokers, the increased risks associated with alcohol and tobacco use decreased steadily as the time since quitting increased. As stated by the authors, most of these cancers “could be prevented by quitting the use of either of these two agents.”
Reference: Szymańska K, Hung RJ, Wűnsch-Filho V, Eluf-Neto J, Curado MP, Koifman S, Matos E, Menezes A, Fernandez L, Daudt AW, Boffetta P, Brennan P. Alcohol and tobacco, and the risk of cancers of the upper aerodigestive tract in Latin America: a case–control study. Cancer Causes Control (2011) 22:1037–1046. DOI 10.1007/s10552-011-9779-7
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 048: A new report on drinking guidelines and the association of alcohol with risk of cancer. 18 July 2011
The Canadian Medical Association Journal has published a commentary by some French scientists relating drinking guidelines to the association between alcohol and cancer. They conclude that the current guidelines for sensible drinking for the general population are not adequate for the prevention of cancer, and revisions and eventual exclusion of such guidelines are needed.
Forum reviewers agree that alcohol consumption, especially heavy intake, increases the risk of certain types of cancer. However, they consider that the opinions of the authors in the paper (labeled as an “Analysis” rather than an editorial or comments) do not reflect current sound scientific data, that the report is highly selective in citing a small number of papers that support their opinions, and that the authors have ignored a huge amount of recent data from more scientifically sound research that have largely discredited such studies. Further, the report provides no mention of the consistent finding from studies around the world that moderate drinkers tend to have lower all-cause mortality risk than do abstainers.
Scientific data over many decades have shown that excessive or irresponsible alcohol use has severe adverse health effects, including an increase in the risk of certain cancers. On the other hand, moderate drinking is associated with lower risk of cardiovascular disease and many other diseases of ageing and with all-cause mortality. A very large number of experimental studies, including results from human trials, have described biological mechanisms for the protective effects of alcoholic beverages against such diseases. A number of comprehensive meta-analyses provide much more accurate, up to date, and scientifically balanced views than does the current paper; such documents may be better sources of data upon which guidelines to the public regarding alcohol consumption should be based.
Reference: Latino-Martel P, Arwidson P, Ancellin R, Druesne-Pecollo N, Hercberg S, Le Quellec-Nathan M, Le-Luong T, Maraninchi D. Alcohol consumption and cancer risk: revisiting guidelines for sensible drinking. CMAJ 2011. DOI:10.1503. /cmaj.110363
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 047: Overall health effects of alcohol consumption. Comments on a WHO report 10 July 2011
The World Health Organization (WHO) has released its global status report on alcohol and health for 2011. Forum members largely agreed with the discussion in the report of the serious health and societal problems associated with the misuse of alcohol, which contributes to accidents, many diseases, and premature deaths. On the other hand, Forum members were disturbed that the report was limited almost exclusively to abusive drinking, was based primarily on out-dated information, and minimized the beneficial health effects associated with moderate drinking. The report ignored a massive amount of scientific data indicating that in all developed countries, moderate consumers of alcohol are at much lower risk of essentially all of the diseases of ageing: coronary heart disease, ischemic stroke, diabetes, dementia, and osteoporosis. And conspicuously absent from the WHO report is a description of the decrease in total mortality among middle-aged and elderly people associated with moderate alcohol consumption, a finding that has been found consistently throughout the world.
Epidemiologic studies over many decades have shown that while excessive or irresponsible alcohol use has severe adverse health and societal effects, moderate drinking is associated with lower risk of cardiovascular disease and other diseases of ageing. And a very large number of experimental studies, including results from human trials, have described biological mechanisms for the protective effects of both alcohol and the polyphenolic components of wine. A number of comprehensive meta-analyses are cited by Forum reviewers which they consider to provide much more accurate, up to date, and scientifically balanced views of the current “status” of the health effects of alcohol consumption. Such documents are better sources of data upon which policy decisions should be based.
Reference: Global status report on alcohol and health. World Health Organization 2011. ISBN 978 92 4 156415 1 (NLM classification: WM 274)
For the full critique of this publication by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 046: All-cause mortality rates are lower among moderate drinkers than among abstainers. 4 July 2011
The author of this paper set out to determine the extent to which potential “errors” in many early epidemiologic studies led to erroneous conclusions about an inverse association between moderate drinking and coronary heart disease (CHD). His analysis is based on prospective data for more than 124,000 persons interviewed in the U.S. National Health Interview Surveys of 1997 through 2000 and avoids the pitfalls of some earlier studies. He concludes that the so-called “errors” have not led to erroneous results, and that there is a strong protective effect of moderate drinking on CHD and all-cause mortality.
The results of this analysis support the vast majority of recent well-done prospective studies. In the present paper, non-drinkers had much higher risk of death than did almost all categories of subjects consuming alcohol. The author contends that these results lend credence to the argument that the relationship between alcohol and mortality is causal.
While some Forum reviewers felt that this analysis only replicates what has been shown in many other papers, it appears that erroneous information continues to be used by some policy groups. Thus, most reviewers believe that this new analysis provides important information on potential health effects of moderate drinking.
Reference: Fuller TD. Moderate alcohol consumption and the risk of mortality. Demography 2011. DOI 10.1007/s13524-011-0035-2
For the full review of this publication by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 045: Alcohol drinking in the elderly: Risks and benefits. 26 June 2011
The Royal College of Psychiatrists of London has published a report related primarily to problems of unrecognized alcohol misuse among the elderly. The report provides guidelines for psychiatrists and family physicians on how to find and how to treat elderly people with misuse of alcohol and drugs. The report also mentions lower “sensible limits” for older people in comparison with younger people. The Forum reviewers point out, however, inherent difficulties in providing guidelines for a very non-homogenous group of individuals whose only criterion for inclusion is being above the age of 65 years. Such a group includes individuals varying from marathon runners to very sick, frail people. Forum reviewers thought that advice to lower limits of drinking for everyone in this age group is not based on reliable research, and would certainly not apply to all in this age group.
The Forum reviewers were also struck by the absence in the Royal College report of any discussion of the strong positive effects of moderate drinking on most of the diseases of ageing, especially cardiovascular diseases, diabetes, and dementia, which are leading causes of morbidity and mortality in this age group. For healthy moderate and responsible drinkers, advice to reduce or stop all alcoholic beverage intake would not be in the best health interests of such individuals.
Reference: Royal College of Psychiatrists, London. Our invisible addicts. First Report of the Older Persons’ Substance Misuse Working Group of the Royal College of Psychiatrists, College Report CR165. June 2011
For the full review of this publication by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 044: The association of alcohol drinking with migraine headache 12 June 2011
An excellent paper from a headache center in Italy summarizes the scientific data relating alcohol ingestion to migraine headaches. The factors that trigger an attack of migraine, or of other headaches as well, are poorly understood. While retrospective studies tend to include alcohol as a trigger for an attack, the authors describe that in a recent prospective study (in which information on the factors that could potentially trigger an attack were collected prior to the migraine attack), menstruation, stress, and fatigue were found most commonly to relate to a subsequent attack, but not alcohol consumption (in fact, beer consumption on the previous day reduced the risk of a migraine attack). In the present paper, the authors reviewed the role and mechanism of action of alcohol or other components of alcoholic drinks in relation to alcohol-induced headache. They conclude from their review that reports overestimate the role of alcohol, as well as other foods, in the triggering of migraine.
Forum members thought that this was a very balanced review of the subject, and that it provided straightforward and sensible advice. Although some individuals surely have the onset of a migraine or other type of headache after the consumption of wine or alcohol, the findings are not consistent. Forum members suggest that given that subjects reporting migraine headaches have been found to be at increased risk of cardiovascular disease, it would not be appropriate to advise all such sufferers to avoid alcohol. As suggested by the authors of this paper, it may be reasonable for those subjects who had a desire to consume alcohol to drink small amounts of specific beverages to see if each beverage was tolerated or not. After seeing the effects, and factoring in symptoms versus potential benefits from moderate drinking, a reasonable discussion can be carried out with respect to continued alcohol use by subjects with migraine.
Reference: Panconesi A, Bartolozzi ML, Guidi L. Alcohol and migraine: What should we tell patients? Curr Pain Headache Rep 2011;15:177–184. DOI 10.1007/s11916-011-0184-4.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 043: Frequent moderate drinking of alcohol is associated with a lower risk of fatty liver disease. 23 May 2011
In a large study of men in Japan, the presence of fatty liver disease by ultrasonography showed an inverse association with the frequency of alcohol consumption; there was some suggestion of an increase in fatty liver disease with higher volume of alcohol consumed per day. Moderate drinkers had lower levels of obesity than did non-drinkers, and both obesity and metabolic abnormalities were positively associated with fatty liver disease.
These findings support the results of a number of other recent studies showing that moderate drinking does not increase the risk of this common type of liver disease; instead, it is associated with a lower risk of its occurrence. We agree with the implications of these studies as stated by the authors: “These results suggest that lifestyle modifications aimed at fighting central obesity and metabolic abnormalities should be the most important recommendations for the management of fatty liver. In addition, it seems unlikely that the risk of fatty liver can be reduced by the discontinuation and/or reduction of alcohol consumption alone.”
Reference: Hiramine Y, Imamura Y, Uto H, Koriyama C, Horiuchi M, Oketani M, Hosoyamada K, Kusano K, Ido A, Tsubouchi H. Alcohol drinking patterns and the risk of fatty liver in Japanese men. J Gastroenterol 2011 46:519–528. DOI 10.1007/s00535-010-0336-z.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 042: An increase in risk of certain types of gastric cancer from heavy drinking, but no increase from moderate alcohol consumption 17 May 2011
A very well-done meta-analysis supports other data generated on the risk of alcohol consumption and gastric cancer – that is – that the risk may be real for heavy alcohol consumption but not for moderate intake. The type of gastric cancer relating to heavier alcohol intake in this study tended to be tumors involving the noncardia, but differences between the association with tumors of the gastric cardia were not significant.
There was no increased risk of gastric cancer from alcohol among Asians; this may be due to lower alcohol intake; there is a greater prevalence among Asians of the inactive ALDH2 genotype that is associated with flushing and other adverse effects of alcohol, and such subjects tend to drink less alcohol. However, a number of studies have shown higher risk for upper aero-digestive cancers for subjects with this ALDH2 genotype, so the overall reason for the lower risk among Asians in this study remains unclear. The main outcome of the study is that there is no increase in the risk of gastric cancer associated with the moderate intake of alcohol.
Reference: Tramacere I, Negri E, Pelucchi C, Bagnardi V, Rota M, Scotti L, Islami F, Corrao G, La Vecchia C, Boffetta P. A meta-analysis on alcohol drinking and gastric cancer risk. Ann Oncology 2011;doi:10.1093/annonc/mdr135
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 041: Estimated health effects of changes in advice for alcohol consumption between the 2005 and 2010 Dietary Guidelines for Americans 6 May 2011
This paper from the National Institute on Alcohol Abuse and Alcoholism in the US suggests that the changes in wording of the alcohol recommendations in the Dietary Guidelines for Americans between 2005 and 2010 indicate that some at-risk drinkers could be classified as moderate drinkers. The authors carried out an analysis using data from a large, nationally representative sample of U.S. adults to estimate differences between subjects following the 2005 recommendations and a “gray zone” of subjects who exceed the 2005 recommendations but fall within the moderate guidelines according to the 2010 recommendations. The differences between these two groups were minimal; other than the gray zone subjects having an increased risk of alcohol dependence (which is unlikely to relate to their slight differences in consumption), the only other differences between the two groups related to alcohol-related interpersonal relations and job loss. And, as the authors state, “There were no associations with medical conditions or mental disorders.”
More importantly, the authors state that “Moreover, of the gray area drinkers who experienced incident alcohol dependence and interpersonal problems, 89% of the former and 94% of the latter had moved out of the gray area and into the highest-risk consumption group over the course of the follow-up interval.” Problems were thus very rare in those who remained in the gray zone of drinking during follow up.
Obviously, drinking 3 or 4 drinks/day (other than doing so only occasionally) should not be considered a healthy way to consume alcohol. But if, as the authors state, almost all of the estimated effects on health are due to subjects who increase their drinking above this “gray zone,” there is little support for their argument that the changes in guidelines make a difference.
Reference: Dawson DA, Grant BF. The “Gray Area” of consumption between moderate and risk drinking. J Stud Alcohol Drugs 2011;72:453–458.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 040: Lower risk of coronary heart disease from alcohol, even with heavy drinking 27 April 2011
Using data from The 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions study (the NESARC study, n = 43,093), the authors of this paper conclude that alcohol may have cardioprotective effects not only in moderate drinkers, but also in individuals with patterns of use traditionally considered as “hazardous.” While such a finding has been shown in some population studies, there were questions by Forum reviewers as to the adequacy of the method for diagnosing coronary artery disease: self-report, with most subjects listing angina pectoris, a “soft” criterion for coronary disease.
In addition, the categories of drinking used in this study were very broad: rare or only occasional drinkers were combined with regular drinkers up to 7 or 14 drinks per week in the “moderate” category; the “hazardous” category included a broad range of drinkers, from a minimal increase over the recommended limits to very heavy drinkers. The pattern of drinking (especially the number of days per week that alcohol was consumed) was not reported, making it difficult to separate regular from heavy week-end drinkers. The effects of heavier drinking on other conditions (such as alcohol-related liver disease, mortality, etc.) were not included in this analysis.
It is physiologically possible that even hazardous use of alcohol, like moderate use, may well lead to cleaner arteries and therefore lower rates of coronary artery disease. If this is the case, an explanation for the increases in cardiovascular mortality reported for heavy drinkers in many studies may relate not directly to coronary artery disease, but to conditions such as cardiomyopathy or cardiac arrhythmias. However, the rates of accidents, suicide and other morbidity associated with hazardous alcohol use may well overcome any protective effects on coronary disease.
Reference: Le Strat Y, Gorwood P. Hazardous drinking is associated with a lower risk of coronary heart disease: Results from a national representative sample. Am J Addict 2011;20:257–263.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 039: The role that alcohol drinking may play in the risk of cancer 17 April 2011
A large group of distinguished scientists have published a very detailed and rather complex paper describing the association between alcohol consumption and cancer. It is based on data from the EPIC study in Europe, with a mean follow up of 8.8 years for more than 300,000 subjects. The authors describe an increase in risk of many cancers from alcohol intake, but do not give data permitting the detection of a threshold of intake for an adverse effect on cancer risk. The investigators conclude that “In western Europe, an important proportion of cases of cancer can be attributable to alcohol consumption, especially consumption higher than the recommended upper limits.”
Members of the Forum were concerned that the authors did not separate moderate consumption from heavy consumption for their main analyses, ignored the demonstrated benefits of moderate drinking on total mortality, and did not point out other environmental influences (such as smoking, diet, obesity, etc.) that often have much larger effects on the risk of many cancers than does alcohol consumption. The authors make statements such as alcohol has negative effects on total mortality that are not supported by the data presented in their paper, and are contradicted by most large-scale population-based studies. Overall, while this paper supports the well-known association between heavy drinking and an increased risk of upper aero-digestive and certain other cancers, it adds little information useful for the prevention of most types of cancer.
Reference: Schűtze M, Boeing H, Pischon T, et al, Alcohol attributable burden of incidence of cancer in eight European countries based on results from prospective cohort study. BMJ 2011; 342:d1584 doi: 10.1136/bmj.d1584 (Published 7 April 2011)
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 038: Effects of a large reduction in alcohol prices on mortality in Finland 7 April 2011
Time series intervention analysis modeling was applied to the monthly aggregations of deaths in Finland for the period 1996–2006 to assess the impact of a reduction in alcohol prices in 2004. The authors report that alcohol-related deaths increased in men aged 40–49 years, and in men and women aged 50–69 years: the mean rate of alcohol-related mortality increased by 17%, 14%, and 40%, respectively, which implies 2.5, 2.9 and 1.6 additional monthly deaths per 100,000 person-years following the price reduction. In contrast to alcohol-related mortality, CVD and all-cause mortality decreased among men and women in the highest age category. The changes were consistent with 19 and 25 fewer monthly deaths per 100,000 person-years for CVD and 42 and 69 fewer monthly deaths for all-cause mortality.
Forum members agreed that both potentially harmful and beneficial effects resulting from changes in alcohol intake should be considered when estimating population effects. They were unsure whether all of the reported effects in the elderly should be attributed to changes in alcohol intake, as decreases in CVD and all-cause mortality rates were occurring prior to the change in alcohol intake.
Reference: Herttua K, Mäkelä P, Martikainen P. An evaluation of the impact of a large reduction in alcohol prices on alcohol-related and all-cause mortality: time series analysis of a population-based natural experiment. Int J Epidemiol 2011;40:441-454; doi:10.1093/ije/dyp336.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 037: Genes found to relate to level of alcohol consumption among Asians 27 March 2011
In a study of 1,721 Korean male drinkers aged 40–69 y in an urban population–based cohort, and another sample of 1,113 male drinkers from an independent rural cohort, information on average daily alcohol consumption was collected and DNA samples were collected for genotyping. In a genome-wide association (GWA) study, 12 single-nucleotide polymorphisms (SNPs) on chromosome 12q24 had genome-wide significant associations with alcohol consumption. These polymorphisms were closely related to genes that determine levels of ALDH, low levels of which relate to flushing after even small amounts of alcohol. Such enzymes are much more common among Asians than among westerners. Further, associations were tested only with the weekly amount of alcohol consumed, not the pattern of drinking; hence, these findings are not direct measures of alcoholism.
The editorial by Freedman et al states “epidemiologic literature suggests that those who begin drinking at an early age may be at greater risk for a maladaptive and more genetically pronounced form of alcohol consumption, and other environmental milieus affect the risk of alcoholism.” It will be important to investigate the interplay of genes and environmental factors when seeking the determinants of alcohol abuse. Despite the findings of this study, our understanding of factors associated with alcoholism remains very limited.
Reference: Baik I, Cho NH, Kim SH, Han B-G, Shin C. Genome-wide association studies identify genetic loci related to alcohol consumption in Korean men. Am J Clin Nutr 2011;93:809–816.
Accompanying Editorial: Agrawal A, Freedman ND, Bierut LJ. Genome-wide association studies of alcohol intake—a promising cocktail? Am J Clin Nutr 2011;93:681–683.
For the full critique of this article by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 036: Alcohol consumption after age 75 associated with lower risk of developing dementia
7 March 2011
A population-based study of elderly Germans, aged 75 and older, evaluated the association between alcohol consumption and incident overall dementia and Alzheimer dementia over 3 years. There was good ascertainment of the development of dementia, even among subjects who died during follow up.
Of 3,202 subjects free of dementia at baseline, 217 subjects met criteria of dementia during follow up. Subjects consuming alcohol had approximately 30% less overall dementia and 40% less Alzheimer dementia than did non-drinking subjects. Unlike many previous studies showing greater effects of wine on reducing risk of dementia, no significant differences were seen according to the type of alcoholic beverage consumed. Overall, these results are similar to several previous studies in the very elderly and suggest that moderate drinking is associated with less dementia, even among individuals aged 75 years and older.
Reference: Weyerer S, Schaufele M, Wiese B, Maier W, Tebarth F, van den Bussche H, Pentzek M, Bickel H, Luppa M, Riedel-Heller SG, for the German AgeCoDe Study Group (German Study on Ageing, Cognition and Dementia in Primary Care Patients). Current alcohol consumption and its relationship to incident dementia: results from a 3-year follow-up study among primary care attenders aged 75 years and older. Age and Ageing 2011; 0: 1–7; doi: 10.1093/ageing/afr007.
For the full critique of this article by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 035: A review of the association of alcohol consumption with cardiovascular disease outcomes 5 March 2011
In an excellent summary, the authors of this paper have synthesized results from longitudinal cohort studies comparing alcohol drinkers with non-drinkers for the outcomes of overall mortality and mortality from cardiovascular disease (CVD), incident coronary heart disease (CHD), mortality from CHD, incident stroke, and mortality from stroke. They conclude that light to moderate alcohol consumption is associated with a reduced risk of multiple cardiovascular outcomes. Further, they suggest that current scientific data satisfy Hill criteria indicating causality, that alcohol intake is the cause of the lower risk of cardiovascular disease among moderate drinkers.
Forum members thought that this was a very well-done, comprehensive summary of a large number of studies on alcohol and cardiovascular disease. Some believed that two topics were not adequately discussed: (1) greater benefits from wine than from other beverages, a result seen in many studies, and (2) the importance of the pattern of drinking on the health effects of alcohol. However, Forum members welcomed the discussion in the paper as to causality and regarding future directions in research, with more emphasis into how physicians and individual patients might respond to encouragement to consume alcohol for its potentially beneficial effects on cardiovascular disease. Most believe that there is no substitute for balanced judgment by a knowledgeable, objective health professional when discussing alcohol intake, and this requires is a synthesis of common sense and the best available scientific facts as they apply to the individual.
Reference: Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 2011;342:d671; doi:10.1136/bmj.d671
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 034: A review of interventional studies in humans showing effects of alcohol on risk factors for cardiovascular disease 5 March 2011
A summary paper on the effects of alcohol consumption on biologic mechanisms associated with coronary heart disease provides an excellent review of a large number of intervention studies in humans. Appropriate analyses were done and the results are presented in a very clear fashion, although there was little discussion of the separate, independent effects of alcohol and polyphenols on risk factors.
The trials the authors reviewed have demonstrated that the moderate intake of alcoholic beverages leads to increases in HDL-cholesterol, apolipoprotein A1, and adiponectin and decreases in fibrinogen, all factors associated with a lower risk of heart disease. The findings described in this paper strengthen the case for a causal link between alcohol intake and a reduced risk of coronary heart disease, suggesting that the lower risk of heart disease observed among moderate drinkers is caused by the alcoholic beverage itself, and not by other associated lifestyle factors.
Reference: Brien SE, Ronksley PE,Turner BJ, Mukamal KJ, Ghali WA. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ 2011;342:d636; doi:10.1136/bmj.d636.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 033: Moderate-to-heavy alcohol intake may increase risk of atrial fibrillation 12 February 2011
A number of well-done studies have shown an increase in the risk of atrial fibrillation to be associated with heavy alcohol intake or with alcoholism. Most previous studies suggest little if any increase in risk from light-to-moderate drinking. The present study was a meta-analysis based on 14 studies from Europe or North America. It showed an increase in risk with alcohol, but there were limited dose-response data to determine if there was a threshold above which the risk was increased.
Overall, the scientific evidence from many studies suggests that at least heavy drinking may increase the risk of atrial fibrillation, although whether light-to-moderate intake increases the risk seems unlikely. Previous basic scientific data of mechanisms of atrial fibrillation have suggested that alcohol has little effect on this arrhythmia.
Reference: Kodama S, Saito K, Tanaka S, Horikawa C, Saito A, Heianza Y, Anasako Y, Nishigaki Y, Yachi Y, Iida KT, Ohashi Y, Yamada N, Sone H. Alcohol consumption and risk of atrial fibrillation. A meta-analysis. J Am Coll Cardiol 2011;57:427–436.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 032: Comments on alcohol in newly released Dietary Guidelines for Americans, 2010 9 February 2011
The United States has released new Dietary Guidelines for Amercans, 2010. While the Key Recommendations regarding alcohol remain similar to those of earlier guidelines, there were some changes in the text that reflect increasing scientific data indicating potential health benefits of moderate drinking. The key recommendation is as follows:
“If alcohol is consumed, it should be consumed in moderation—up to one drink per day for women and two drinks per day for men—and only by adults of legal drinking age.”
Within the main body of the guidelines, comments on alcohol include the following:
“The consumption of alcohol can have beneficial or harmful effects, depending on the amount consumed, age, and other characteristics of the person consuming the alcohol. Alcohol consumption may have beneficial effects when consumed in moderation. Strong evidence from observational studies has shown that moderate alcohol consumption is associated with a lower risk of cardiovascular disease. Moderate alcohol consumption also is associated with reduced risk of all-cause mortality among middle-aged and older adults and may help to keep cognitive function intact with age. However, it is not recommended that anyone begin drinking or drink more frequently on the basis of potential health benefits because moderate alcohol intake also is associated with increased risk of breast cancer, violence, drowning, and injuries from falls and motor vehicle crashes.”
Reference: www.cnpp.usda.gov/Publications/DietaryGuidelines/2010/PolicyDoc/Chapter3.pdf
To see a copy of the section on alcohol from the new Dietary Guidelines, click here.
===============================================================================
Critique 031: Wine polyphenols have a variety of beneficial effects on health 30 January 2011
Much of the protection against cardiovascular disease attributed to wine intake may relate not only to the alcohol in wine, but to its polyphenolic constituents. This review article summarizes research into the chemistry, bioavailability, metabolism and excretion of polyphenols as well as mechanisms of their action. As stated by the authors, “These protective effects could be due to one or many components of the complex mixture of bioavailable and bioactive compounds present in red wine including ethanol, resveratrol, flavonols, flavan-3-ols, anthocyanins, phenolic acids as well as their metabolites formed either in the tissues or in the colon by the microflora.” The authors describe their cardioprotective effects, effects on vascular function and atherosclerosis, anti-platelet effects, effects on myocardial ischemia, and anti cancer and anti-diabetic effects.
The authors conclude that “Polyphenols are the most abundant antioxidants in the diet and are widespread constituents of wine, fruits and vegetables.” Their review provides an extensive scientific literature on polyphenols in wine; it suggests multiple mechanisms by which such substances may have beneficial effects on health.
Reference: Rodrigo R, Miranda A, Vergara L. Modulation of endogenous antioxidant system by wine polyphenols in human disease. Clin Chim Acta 2011;412:410-424
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research please click here.
===============================================================================
Critique 030: Young rats given red wine polyphenols show less deterioration in endothelial function with ageing. 30 January 2011
The gradual decrease in endothelial function over time is a key factor in the development of diseases associated with ageing, especially cardiovascular disease (CVD). Many epidemiologic studies suggest greater protection against CVD from wine than from other beverages containing alcohol, with at least one factor being the polyphenols in red wine (RWPs).
The present study in rats found that the administration of red wine polyphenols protected against ageing-induced endothelial dysfunction. As stated by the authors: “The present findings indicate that regular intake of RWPs in the drinking water starting at young age (16 week-old) prevented the aging-related endothelial dysfunction most likely by reducing the excessive oxidative stress in the arterial wall.” They further suggest an important role of NADPH oxidase and possibly also the angiotensin system in the abnormal vascular response in aging. Their study showed that, “RWPs intake had also a physiological beneficial effect since it improved the physical exercise capacity of old rats.”
Forum members thought that this was an excellent paper, as it begins to delve into mechanisms by which polyphenols improve health. A mechanism is addressed and results are consistent with the working hypothesis of a specific interaction between polyphenols and peculiar enzymes. There is a satisfying agreement between basic mechanisms and pathophysiology.
Some scientists believe that interventions to improve endothelial function (such as the consumption of red wine or other sources of polyphenols) should begin earlier in life to slow down the endothelial dysfunction that occurs with ageing. This study in rats tends to support such a belief.
Reference: Dal-Ros S, Zoll J, Lang AL, Auger C, Keller N, Bronner C, Geny B, Schini-Kerth VB. Chronic intake of red wine polyphenols by young rats prevents aging-induced endothelial dysfunction and decline in physical performance: Role of NADPH oxidase. Biochem Biophys Res Commun 2011;404:743-749
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 029: Differing opinions on the message to the public regarding alcohol consumption 16 January 2011
A Letter to the Editor entitled “What should we advise about alcohol consumption?” was recently published by Maurizio Ponz de Leon in Intern Emerg Med.1 Dr. de Leon argues that the message of health benefits of moderate drinking “seems to me hazardous and extremely dangerous to diffuse in the general population.” His reasons included (1) many people may be unable to distinguish between low–moderate and high consumption of wine, beer or spirits, and alcohol metabolism may differ remarkably from one subject to another; (2) alcohol remains a frequent cause of car crash, and governments (in almost all western countries) try to convince or force people to abstain from drinking before driving; and (3) to consider alcohol as a medication whose consumption may contribute to improved health is another source of concern. Dr. de Leon asks: “Are we truly at the point of prescribing alcohol consumption in order to reduce the risk of stroke and coronary damage?” He concluded that “more studies are needed before we can give sensible recommendations on alcohol consumption to the general population.”
The de Leon editorial has prompted considerable response from other scientists, including further Letters to the Editor of the journal by Di Castelnuovo, Costanzo, Donati, Iacoviello, and de Gaetano,2 and by Estruch and Lamuela-Raventos.3 In addition, the original editorial has stimulated considerable debate among members of the International Scientific Forum on Alcohol Research. Among key arguments presented by the Forum members, all experts in scientific research on alcohol, are that messages to the public should not be “paternalistic” (we will tell you what is best for you since you are not smart enough to understand the facts), and that guidelines must always be based on sound, balanced scientific data rather than on uninformed opinion. Forum members emphasized that there are certain people who should not drink at all (including former abusers of drugs or alcohol, people with certain medical conditions, children and adolescents, and people with religious or moral proscriptions against alcohol), and there can never be a general recommendation for everybody to consume alcohol. On the other hand, physicians should not withhold from their patients and the public scientifically sound and balanced data on alcohol and health. And the data are extremely strong supporting a role for moderate alcohol intake, for appropriate adults, for the reduction in risk of coronary artery disease and other diseases of ageing.
Several Forum members pointed out that it was unfortunate that the journal had chosen to publish the original letter that castigates alcohol from an author with good scientific credentials, but little to no apparent research expertise in the subject of alcohol and health. Many Forum members disagreed with the statement of de Leon that “Many people may be unable to distinguish between low–moderate and high consumption of wine, beer or spirits.” A leading scientist dealing with this subject for decades, Dr. Arthur Klatsky, has written: “Most people know very well what the difference is between light to moderate drinking and binge or excessive drinking. While some patients may rationalize their heavy drinking because of its purported health effects, I have yet to find someone who had developed alcohol abuse because of messages about the health effects of moderate drinking.” Medical practitioners, in his view, “have a ‘solemn duty’ to tell the truth about alcohol consumption, as they understand it, to all of their patients.” While pointing out that certain individuals will not benefit from the consumption of alcohol, several Forum members believed that it would be unethical for physicians to withhold from middle-aged or elderly subjects at risk of cardiovascular disease information on the potential benefits of light-to-moderate drinking
References:
1. Maurizio Ponz de Leon. What should we advise about alcohol consumption? Intern Emerg Med, DOI 10.1007/s11739-010-0487-1.
2. Augusto Di Castelnuovo, Simona Costanzo, Maria Benedetta Donati, Licia Iacoviello, Giovanni de Gaetano. What should we advise about alcohol consumption? Reply letter by A. Di Castelnuovo. Intern Emerg Med, DOI 10.1007/s11739-010-0502-6.
3. Ramon Estruch • Rosa Ma Lamuela-Raventos. What should we advise about alcohol consumption: reply letter by R. Estruch. Intern Emerg Med; DOI 10.1007/s11739-010-0503-5.
For the full critique of these publications by members of the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 028: Changes over time in relation of social class to mortality from cirrhosis 9 January 2011
To explore the nature of the social class gradient of cirrhosis mortality in England and Wales across the 20th century, data on male cirrhosis mortality by social class were obtained from the Registrar General’s Decennial Supplements for the years 1921–1991. This paper describes a dramatic change during the 20th century in the association between social class and mortality from liver cirrhosis. While deaths from cirrhosis were more common among higher social classes in the early part of the century, the pattern changed so that deaths from cirrhosis were much more common among the lower social classes by the end of the century.
Suggested reasons for the lower current rates among subjects at higher social class include different patterns of alcohol consumption, with regular moderate consumption (especially of wine with meals) becoming more common with higher social class subjects while binge drinking (especially of beer and spirits) remaining more common in lower social classes. However, a number of other factors may relate to the class differences in rates of hepatic cirrhosis, including a less healthy diet and greater rates of obesity (associated with hepatic fatty liver and cirrhosis) among lower social class subjects and social class differences in hepatitis rates. Further, certain medications, coffee consumption, and many other lifestyle factors are associated with hepatic cirrhosis. The actual reasons for the changes over time reported in this paper remain unclear.
Reference: Crombie IK, Precious E. Changes in the social class gradient of cirrhosis mortality in England and Wales across the 20th century. Alcohol and Alcoholism 2011;46:80–82.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 027: Effects of resveratrol and quercetin on inflammation and insulin resistance – 20 December 2010
A study was carried out to examine the extent to which quercetin and trans-resveratrol (RSV) prevented inflammation or insulin resistance in primary cultures of human adipocytes treated with tumor necrosis factor-a (TNF-a)—an inflammatory cytokine elevated in the plasma and adipose tissue of obese, diabetic individuals. Cultures of human adipocytes were pretreated with quercetin and trans-RSV followed by treatment with TNF-a. Subsequently, gene and protein markers of inflammation and insulin resistance were measured. The authors report that quercetin, and to a lesser extent trans-RSV, attenuated the TNF-a–induced expression of inflammatory genes such as interleukin (IL)-6, IL-1b, IL-8, and monocyte chemoattractant protein-1 (MCP-1) and the secretion of IL-6, IL-8, and MCP-1.
Forum members were concerned about certain aspects of the study, especially the extrapolation of in vitro results to in vivo situations. The in vitro conditions the authors describe are minimally representative of an in vivo condition. In vivo, after consumption of quercetin or resveratrol, these compounds undergo extensive metabolism, leading to glucuronidated, sulphated or methylated compounds. In a previous study, quercetin 3-glucoside was transformed to 3,4-dihydroxyphenylacetic acid, acetate and butyrate in cells from human gut; only 3′-methylquercetin has been detected in human plasma, present at a concentration of 0.1 to 0.2 µM after 3 h. The authors of the current paper are using concentrations up to 60 µM, concentrations which have not been found in vivo.
There were also concerns with the work on cell uptake of quercetin and resveratrol. Primary adipocytes were incubated with the polyphenols, but it is not clear whether or not the concentrations used were subtoxic. Our current knowledge is limited about local concentration of the molecules we are studying in subcellular compartments, their interaction with alternative targets, and eventually their transformation into products that could be more or less active on a given specific pathway. The real difficult and important issue is the identification of a reasonable convergence — if not agreement — between data originating from extremely distant approaches. In this case, the notion that metabolic diseases are related to a homeostatic imbalance in adipose tissue, linked to a different redox status, linked to activation of specific pathways, and that different redox sensitive polyphenols do have a protective effect, encompasses the evidence produced by extremely distant approaches.
From a clinical point of view, the role of phytochemicals acting as antioxidants and anti-inflammatory agents could be extremely important in inflammation-associated chronic conditions such as cardiovascular disease, diabetes, and cancer. Quercetin and resveratrol may indeed play an important role in this regard, and need to be investigated further to establish the clinical importance of natural dietary compounds in the prevention of chronic degenerative conditions.
Reference: Chuang C-C, Martinez K, Xie G, Kennedy A, Bumrungpert A, Overman A, Jia W, McIntosh MK. Quercetin is equally or more effective than resveratrol in attenuating tumor necrosis factor-a–mediated inflammation and insulin resistance in primary human adipocytes. Am J Clin Nutr 2010;92:1511–1521.
For the full critique of this paper by the International Scientific Forum on Alcohol Research please click here.
===============================================================================
Critique 026: Chinese study suggests that alcohol increases angiographically significant coronary artery disease 8 December 2010
Among a large number of Chinese men presenting with chest pain or EKG changes, sequential subjects undergoing cardiac angiography were evaluated for obstructive coronary artery disease (CAD) lesions according to their reported recent alcohol intake. The study population consisted of 1,476 consecutive men 36 to 84 years of age; participants were categorized as nondrinkers, light drinkers, moderate drinkers, or heavy drinkers.
Adjusted odds ratios for angiographically proved CAD for light, moderate, and heavy drinking were 1.16 (95% confidence interval 0.68 to 1.94), 1.78 (1.35 to 2.27), and 2.18 (1.46 to 3.25). Compared to non-drinking, adjusted odds ratios were 1.03 (0.54 to 1.87) for drinking 0 to 15 years, 1.61 (1.28 to 2.14) for 16 to 30 years, and 1.98 (1.23 to 3.05) for >30 years. The authors concluded that moderate-to-heavy alcohol consumption increased the risk of CAD in Chinese men. CAD risk tended to increase with an increase in frequency and duration of drinking.
This was a very select group of patients (those presenting with chest pain or EKG changes), and not typical of the Chinese population. No information was available on drinking patterns or on previous alcohol intake. Further, a recent large population-based study from mainland China showed that consumers of alcohol were less likely to develop coronary disease, results similar to those in most Western populations. It is not possible from the present study to say that the association of alcohol intake with CAD is different between Chinese and Western populations, as the present study gives results only for a very select group of patients.
The most important outcome regarding CAD is the occurrence of clinical events (myocardial infarction, cardiac death, etc.). The detection of such events requires long-term follow-up studies to be able to judge the overall effects of alcohol drinking on CAD.
Reference: Zhou X, Li C, Xu W, Hong X, Chen J. Relation of alcohol consumption to angiographically proved coronary artery disease in Chinese men. Am J Cardiol 2010;106:1101–1103.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 025: Pattern of drinking and type of beverage affect the relation of alcohol intake to coronary heart disease 1 December 2010
Using cohort data from Belfast and France, investigators related weekly alcohol consumption, incidence of binge drinking (alcohol >50 g on at least one day a week), incidence of regular drinking (at least one day a week, and alcohol <50 g if on only one occasion), volume of alcohol intake, frequency of consumption, and types of beverage consumed to risk of coronary heart disease (CHD) events over a 10 year follow-up period. Overall, 60.5% of subjects from N. Ireland and 90.6% of French reported drinking alcohol at least once a week. Among drinkers, 12% of men in Belfast drank alcohol every day compared with 75% of men in France. Mean alcohol consumption was 22.1 g/ day in Belfast and 32.8 g/day in France. Binge drinkers comprised 9.4% and 0.5% of the Belfast and France samples, respectively.
Results showed that, after multivariate adjustment, the hazard ratio for hard coronary events compared with regular drinkers was 1.97 (95% CI 1.21 – 3.22) for binge drinkers, 2.03 (95% CI 1.41 – 2.94) for never drinkers, and 1.57 (95% CI 1.11 – 2.21) for former drinkers. The hazard ratio for hard coronary events in Belfast compared with in France was 1.76 (95% CI 1.37 to 2.67) before adjustment, and 1.09 (95% CI 0.79 to 1.50) after adjustment for alcohol patterns and wine drinking. Only wine drinking was associated with a lower risk of hard coronary events, irrespective of the country.
The authors conclude that regular and moderate alcohol intake throughout the week, the typical pattern in middle-aged men in France, is associated with a low risk of ischemic heart disease, whereas the binge drinking pattern more prevalent in Belfast confers a higher risk.
While a strong inverse association between moderate alcohol consumption and cardiovascular disease has been demonstrated for decades, more recent research has emphasized the importance of the pattern of drinking (regular moderate versus episodic or binge drinking). Further, there continues to be debate about the potential greater effect of wine versus other beverages containing alcohol. This study shows that regular moderate drinking (especially of wine) is associated with lower risk of MI, but episodic or binge drinking (especially of beer or whiskey) increases the risk. Lifetime abstinence has a similar adverse relation to CHD as does episodic or binge drinking.
Reference: Ruidavets J-B, Ducimetièere P, Evans A, Montaye M, Haas B, Bingham A, Yarnell J, Amouyel P, Arveiler D, Kee F, Bongard V, Ferrières J. Patterns of alcohol consumption and ischaemic heart disease in culturally divergent countries: the Prospective Epidemiological Study of Myocardial Infarction (PRIME). BMJ 2010;341:c6077 doi:10.1136/bmj.c6077.
For the detailed critique of this study by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 024: Moderate alcohol consumption lowers risk of metabolic diseases in a population with high mean alcohol intake. 28 November 2010
A cross-sectional analysis of data from subjects in Switzerland related varying levels of alcohol intake to the presence of diabetes mellitus, the “metabolic syndrome,” and an index of insulin resistance (HOMA-IR). The strengths of this paper include being population-based and having a large number of subjects who reported that they consumed 14 or more drinks/week. Also, there was a good percentage (27%) of subjects reporting no alcohol intake during the one week of assessment used for classifying subjects. Another strength is the careful confirmation of drinking status with state-of-the-art laboratory tests. In multivariate analysis, the prevalence of the metabolic syndrome, diabetes and mean HOMA-IR decreased with low-risk drinking and increased with high-risk drinking. No differences were noted according to the type of beverage consumed.
This is a cross-sectional analysis, so a causative relation between alcohol intake and the metabolic outcomes cannot be assessed. Still, the data support much that has been shown in prospective studies. Several Forum members commented on potential problems when considering a number of physiologic conditions as the “metabolic syndrome” and focusing therapy on the syndrome; they believed that each metabolic factor should be evaluated and treated singly.
Reference: Clerc O, Nanchen D, Cornuz J, Marques-Vidal P, Gmel G, Daeppen J-B, Paccaud F, Mooser V, Waeber G, Vollenweider P, Rodondi N. Alcohol drinking, the metabolic syndrome and diabetes in a population with high mean alcohol consumption. Diabet Med 2010;27:1241–1249.
For the detailed critique of this study by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 023: Evidence that PPAR-gamma is a mechanism for the effects of wine polyphenolics on cardiovascular risk. 27 November 2010
It is important that biological mechanisms are identified for the observed inverse relation between the moderate consumption of wine and cardiovascular disease shown in most epidemiologic studies. A paper by Zoechling et al is an elegant example of the needed effort to provide a biochemical mechanism for the biological effects of wine. Data on binding of different wine component were produced and this result is interpreted in light of epidemiological evidence.
It would have been appropriate to provide evidence also for the actual shift of gene expression primed by the same wine component in a cell or animal model. In this respect, results must be rated appropriate but still as preliminary; a ligand could have different effects. Further, biological evidence is not provided to support the contention that these polyphenols act through the PPAR-gamma receptor. The sort of evidence that should have been provided is a comparison with rosiglitazone in a cell population known to respond to PPAR-gamma agonists (e.g. adipocytes).
Further, the analytical data does not describe the amounts of any of the “active” substances. So while there is a lot of discussion of the active components, it is not possible to compare any wine’s “activity” with the amount of the key substances. Lacking such a comparison, it is very hard to conclude that these substances are in fact the responsible factors in the observed activity.
Nevertheless, this paper provides important data on potential mechanisms by which the constituents of wine and certain other beverages may act to reduce the risk of cardiovascular disease.
Reference: Zoechling A, Liebner F, Jungbauer A. Red wine: A source of potent ligands for peroxisome proliferator-activated receptor γ. Food & Function, Journal of the Royal Society of Chemistry, in press. DOI: 10.1039/c0fo00086h.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 022: Alcohol consumption decreases with the development of disease — 21 November 2010
In a cross-sectional study from the 2004 and 2007 Australian National Drug Strategy Household (NDSH) surveys, respondents were questioned about their current and past drinking, the presence of formal diagnosis for specific diseases (heart disease, type 2 diabetes, hypertension, cancer, anxiety, depression) and self-perceived general health status. The sample sizes for the 2004 and 2007 NDSH surveys were 24,109 and 23,356, respectively.
The authors report that respondents with a diagnosis of diabetes, hypertension, or anxiety were more likely to have reduced or stopped alcohol consumption in the past 12 months. The likelihood of having reduced or ceased alcohol consumption in the past 12 months increased as perceived general health status declined from excellent to poor (although the authors do not point out that lifetime abstainers were more likely than moderate drinkers to report less than excellent health status).
The authors conclude that the experience of ill health is associated with subsequent reduction or cessation of alcohol consumption (“sick quitters), which is consistent with most prospective epidemiologic studies. The authors also conclude that this may at least partly underlie the observed ‘J-shaped’ function relating alcohol consumption to premature mortality. On the other hand, most modern epidemiologic studies are careful not to include “sick quitters” within the non-drinking category, and relate health effects of drinkers with those of lifetime abstainers. Further, prospective studies in which alcohol intake is assessed at different times (rather than having “changes” based only on recall at one point in time, as was done in this study) usually indicate that subjects who decrease their intake are more likely to subsequently develop adverse health outcomes, especially related to cardiovascular disease, than those who continue moderate drinking.
Reference: Liang W, Chikritzhs T. Reduction in alcohol consumption and health status. Addiction 2010; in press (doi:10.1111/j.1360-0443.2010.03164.x).
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 021: Alcohol consumption affects risk of cataracts 25 October 2010
A population-based prospective study from Australia utilized repeated lens photographs over a period of 5 to 10 years to diagnose cataracts among more than 2,500 subjects. The investigators related the risk of their development, and the risk of cataract surgery, to the reported alcohol intake of subjects. Previous research has provided some biological mechanisms that make an association between alcohol and cataracts plausible.
Overall, the present study showed few statistically significant relations between alcohol and cataracts, although adjusted results suggested a “U-shaped” association between total alcohol intake and development of cataracts (a lower risk for moderate drinkers, higher risk for both abstainers and heavier drinkers). The U-shaped association with alcohol consumption was stronger for the risk of cataract surgery. These results are consistent with previous cohort studies. On inspection of the data presented, the potential reduction in risk of cataract was primarily for wine and beer. While some types of cataract may be reduced by moderate drinking, larger intake of alcohol may be associated with increased risk.
Reference: Kanthan GL, Mitchell P, Burlutsky G, Wang JJ. Alcohol Consumption and the Long-Term Incidence of Cataract and Cataract Surgery: The Blue Mountains Study. Am J Ophthalmol 2010;150:434–440.
For the full critique of this paper by members of the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 20: New data on effects of alcohol during pregnancy 12 October 2010
A very large population-based observational study from the UK found that at the age of 5 years, the children of women who reported light (no more than 1-2 units of alcohol per week or per occasion) drinking did not show any evidence of impairment on testing for behavioral and emotional problems or cognitive ability. There was a tendency for the male children of women reporting “heavy/binge” drinking during pregnancy (7 or more units per week or 6 or more units per occasion) to have poorer behavioral scores, but the effects were less clear among female offspring.
Scientific data continue to indicate that higher intake of alcohol during pregnancy may adversely affect the fetus, and could lead to very severe developmental or other problems in the child. However, most recent publications (as does this one) show little or no effects of occasional or light drinking by the mother during pregnancy. They also demonstrate how socio-economic, education, and other lifestyle factors of the mother may have large effects on the health of the fetus and child; these must be considered when evaluating the potential effects of alcohol during pregnancy.
Overall, current scientific data indicate that while drinking during pregnancy should not be encouraged, there is little evidence to suggest that an occasional drink or light drinking by the mother is associated with harm. Heavy drinking, however, may be associated with serious developmental defects in the fetus.
Reference: Kelly YJ, Sacker A, Gray R, Kelly J, Wolke D, Head J, Quigley MA. Light drinking during pregnancy: still no increased risk for socioemotional difficulties or cognitive deficits at 5 years of age? J Epidemiol Community Health 2010; doi:10.1136/jech.2009.103002
Addendum: After the above critique was prepared, a new paper has been published on the topic by O’Leary et al (O’Leary CM, Nassar N, Kurinczuk JJ, de Klerk N, Geelhoed E, Elliott EJ, Bower C. Prenatal Alcohol Exposure and Risk of Birth Defects Pediatrics 2010;126;e843-e850; DOI: 10.1542/peds.2010-0256). Overall, the results of that study are similar to those of the study by Kelly et al, with no increase in risk of birth defects in children born of women reporting low or moderate drinking during pregnancy but with an increased risk of defects among children of women reporting heavy drinking.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 019: Both alcohol and caffeinated coffee intake are associated with lower risk of diabetes in African-American women. 27 September 2010
In a very large cohort of African-American women in the US, the association between the consumption of alcohol, tea, and coffee was related to the development of type 2 diabetes mellitus over a follow-up period averaging 12 years. Tea and decaffeinated coffee showed no relation with diabetes, but the intake of both caffeinated coffee and alcohol showed a significant inverse association.
This paper is particularly important because some previous studies have not shown a strong association between alcohol and the risk of cardiovascular disease among African-Americans. African-Americans, especially women, tend to drink little alcohol, yet are at markedly increased risk of diabetes. In the present study, the approximately 30% lower risk for moderate alcohol drinkers was about the same in these African-American women as has been found in many previous studies of whites.
Reference
Boggs DA, Rosenberg L, Ruiz-Narvaez EA, Palmer JR. Coffee, tea, and alcohol intake in relation to risk of type 2 diabetes in African American women. Am J Clin Nutr 2010;92:960–966.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 018: Alcohol consumption following diagnosis of early-stage breast cancer may increase risk of recurrence of cancer but not total mortality risk 14 September 2010
In the Life After Cancer Epidemiology (LACE) study, 1,897 participants diagnosed with early-stage breast cancer between 1997 and 2000 and recruited on average 2 years post-breast cancer diagnosis were evaluated for the association between alcohol intake and breast cancer recurrence and death. The women, who were generally light drinkers, were followed for an average of 7.4 years. The study reported an increase in risk of breast cancer recurrence and breast cancer death, but no effect on total mortality, to be associated with consumption of 3 to 4 or more drinks per week when compared with women not drinking following their cancer diagnosis.
Previous research has been mixed on this topic. Almost all large studies have shown no increase in all-cause mortality for women who drink moderately following a diagnosis of breast cancer (as does this study). As for recurrence of breast cancer, most have shown no increase in risk, although one previous study of women with estrogen-receptor + tumors found an increased risk of a primary cancer developing in the contralateral breast to be associated with alcohol intake of more than 7 drinks per week.
Because of conflicting results among studies on this topic, further research will be needed to determine the extent to which alcohol following a diagnosis of breast cancer may relate to subsequent disease and death.
Reference: Kwan ML, Kushi LH, Weltzien E, Tam EK, Castillo A, Sweeney C, Caan BJ. Alcohol Consumption and Breast Cancer Recurrence and Survival Among Women With Early-Stage Breast Cancer:The Life After Cancer Epidemiology Study. J Clin Oncol 2010;28 (published ahead of print, 10.1200/JCO.2010.29.2730)
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, please click here.
===============================================================================
Critique 017: Moderate alcohol intake is associated with a lower risk of total mortality than are either abstinence or heavy drinking 5 September 2010
In a study based on data from 1,824 predominantly Caucasian Americans from the Western part of the United States, alcohol consumption at baseline was related to mortality risk during a 20-year follow-up period. Subjects were recruited into a longitudinal project that has examined late-life patterns of alcohol consumption and drinking problems. Lifetime abstainers were not included in the study, which focused on stress and coping processes among problem drinkers and non-problem drinkers. The sample at baseline included only subjects aged 55 to 65 years who had had outpatient contact with a health care facility in the previous 3 years.
The database at baseline included information on daily alcohol consumption, sociodemographic factors, former problem drinking status, health factors, and social-behavioral factors. Subjects who were not lifetime abstainers but did not report drinking at the time of the baseline examination were classified as “abstainers.” Data on potential changes in alcohol consumption during the course of the study were not collected. Death during follow up was confirmed primarily by death certificate.
The key results of the paper are that even when adjusting for sociodemographic factors, former problem drinking status, health factors, and social-behavioral factors, moderate drinking was associated with considerably lower risk of all-cause mortality. In comparison with “moderate drinkers” (subjects reporting up to 3 drinks/day), abstainers had 51 % higher mortality risk and heavy drinkers had 45% higher risk. The study supports most previous scientific studies showing that moderate drinking, in comparison with both abstinence and heavy drinking, is associated with lower risk of total mortality.
Reference: Holahan CJ, Schutte KK, Brennan PL, Holahan CK, Moos BS, Moos RH. Late-Life Alcohol Consumption and 20-Year Mortality. Alcoholism: Clinical and Experimental Research 2010;34:in press, November 2010
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 016: Association of alcohol with breast cancer risk varies according to subtype of tumor
29 August 2010
Most studies show a slight increase in the risk of breast cancer for women who consume alcohol. The association is thought to relate to alcohol’s effects on hormones, and alcohol use tends to be more strongly associated with hormonally sensitive breast cancers than tumors not sensitive to hormones. Few studies have evaluated how alcohol-related risk varies by breast cancer subtype. In the present study, follow-up data from 87,724 women in the Women’s Health Initiative Observational Study prospective cohort were evaluated for the relation of baseline alcohol consumption with subsequent breast cancer.
A total of 2,944 invasive breast cancer patients were diagnosed during follow up. In multivariable-adjusted analyses alcohol consumption was associated with an increase in the risk of lobular carcinoma (which makes up approximately 15-20% of breast cancers), but there was not a statistically significant association with the more-common ductal type of carcinoma. Hormone + cancers showed an association with alcohol intake, but not hormone – cancers. The findings support the importance of hormonal mechanisms in mediating the relation between alcohol use and breast cancer risk.
Reference Li CI, Chlebowski RT, Freiberg M, Johnson KC, Kuller L, Lane D, Lessin L, O’Sullivan MJ, Wactawski-Wende J, Yasmeen S, Prentice R. Alcohol consumption and risk of postmenopausal breast cancer by subtype: the Women’s Health Initiative Observational Study. J Natl Cancer Inst 2010 Aug 23. [Epub ahead of print]
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here : Critique 016.
===============================================================================
Critique 015: Moderate drinking does not appear to increase risk of breast cancer among women with a BRCA gene mutation 22 August 2010
A large study was carried out to assess the effects of alcohol consumption on breast cancer risk among women with a BRCA1 or a BRCA2 gene mutation, both of which markedly increase the risk of breast cancer. Comparisons were made between women with a gene mutation who had developed invasive breast cancer matched with women with the same gene mutation who had not developed breast cancer. After a number of appropriate exclusions, there were 1,480 matched pairs with BRCA1 mutations and 445 pairs with BRCA2 mutations.
Data from the study support an earlier report suggesting no increase in breast cancer risk from alcohol intake for women with either gene mutation. In the previous study on this topic, a slight lowering of breast cancer risk was noted with light drinking among women with the BRCA2 mutation but not among those with the BRCA1 mutation. In the present study, a possible reduction in risk of breast cancer was seen for moderately drinking women with the BRCA1 mutation, but not the BRCA2 mutation. Further, in the present study, the reduction is risk of breast cancer was seen only for wine consumers. While one should not over-interpret epidemiologic data in the absence of identified biologic mechanisms, there have been a very large number of experimental studies showing that certain polyphenols present in wine actively impede the initiation and growth of cancer cells.
Overall, current scientific data suggest that alcohol in moderation does not increase the risk of breast cancer among women with a BRCA mutation, and wine may be somewhat protective. If this is indeed the case and given the high risk associated with these genetic mutations, it would be important to inform women with such a mutation that moderate alcohol does not appear to increase their risk of breast cancer.
Reference: Dennis J, Ghadirian P, Little J, et al: The Hereditary Breast Cancer Clinical Study Group. Alcohol consumption and the risk of breast cancer among BRCA1 and BRCA2 mutation carriers. The Breast 2010; e-pub.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here.
=========================================================================
Critique 014: Moderate drinking, especially of wine, is associated with better cognitive function 13 August 2010
A large prospective study of men and women in northern Norway reported that moderate wine consumption was independently associated with better performance on cognitive tests after 7 years of follow up. There was no consistent association between consumption of beer or spirits and cognitive test results. The authors also reported that abstinence was associated with significantly lower cognitive performance in women. As noted by the authors, in any observational study there is the possibility of residual confounding by other lifestyle habits affecting cognitive function, and the present study was not able to adjust for certain ones (e.g., diet, income, or profession) but did adjust for age, education, body mass index, depression, and cardiovascular disease and its major risk factors.
The results of this study support findings from a number of observational, prospective studies that have shown that the moderate consumption of alcohol, especially of wine, may have favorable effects on cognitive function. Such effects could relate to the presence in wine of a number of polyphenols and other substances that reduce the risk of cognitive decline with ageing. Mechanisms that have been suggested for such protection against cognitive dysfunction include effects on atherosclerosis, coagulation, inflammation, as well as direct neuroprotective effects.
Reference: Arntzen KA, Schirmer H, Wilsgaard T, Mathiesen EB. Moderate wine consumption is associated with better cognitive test results: a 7 year follow up of 5033 subjects in the Tromsø Study. Acta Neurol Scandd 2010; Suppl 190:23-29.
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 013: Greater than moderate alcohol intake increases the risk of liver cirrhosis 27 July 2010
A new meta-analysis shows that alcohol consumption is a strong factor in the development of cirrhosis of the liver. The study also supports the theory that there is a threshold of drinking above which the risk is increased, as some of their analyses suggest that the risk increases only with intake of more than 24 grams/day of alcohol for women (about 2 typical drinks by US standards) and 36 grams/day of alcohol for men (about 3 typical US drinks).
Despite some concerns about the approach used, our Forum agrees that the present meta-analysis supports previous studies indicating a strong role of heavy alcohol drinking in the development of cirrhosis. The differences found by the investigators between the effects of moderate alcohol intake on cirrhosis morbidity and on cirrhosis mortality are difficult to explain, but may relate to misclassification of alcohol intake (heavy drinkers reporting less alcohol), always a problem in observational studies of the effects of alcohol.
The results related to morbidity suggest that small amounts of alcohol are not associated with an increased risk of cirrhosis, and may be associated with lower risk of disease. Thus, the data provide evidence for a “threshold effect” of alcohol intake for the development of cirrhosis. Limited previous data are available suggesting that wine consumption may be associated with lower risk of cirrhosis than the intake of other beverages, but essentially all studies show heavy drinking of any type of beverage increases the risk.
Reference: Rehm J, Taylor B, Patra SM, Irving H, Baliunas D, Patra J, Roerecke M. Alcohol as a risk factor for liver cirrhosis: A systematic review and meta-analysis. Drug and Alcohol Review 2010,29,437–445. DOI: 10.1111/j.1465-3362.2009.00153.x
For the detailed critique of this paper by the International Scientific Forum on Alcohol Research, click here.
===============================================================================
Critique 012: Moderate drinking in the elderly is associated with lower total mortality 23 July 2010
The effects of alcohol consumption in the elderly may be modified by a decreased ability to metabolize alcohol, an altered volume of distribution due to reduced lean body mass and total body water, and an increased prevalence of co-morbid conditions. These factors make this study of the net effects of drinking among a large number of community-dwelling elderly men and women especially important.
In large prospective studies from Australia of men aged 60-79 and women aged 70-75 years of age, men consuming up to 4 drinks/day and women up to 2 drinks/day had considerably lower risk of dying (total mortality) than did non-drinkers. For subjects reporting 1-2 drinks/day, their total mortality risk was about 20-30% lower than that of abstainers.
While the authors concluded that not consuming alcohol on 1 or 2 days per week was associated with better outcomes, this conclusion is not in accordance with their own data. The benefit of one or two “alcohol-free” days per week has never been substantiated with solid evidence from any large epidemiological study.
Our Forum review concludes that in terms of total mortality risk, recommendations for very low levels of drinking among the elderly may be overly restrictive, as this study showed lower total mortality for up to 4 drinks/day for elderly men and 2 drinks/day for elderly women. Further, this study does not provide support for the conclusion that mortality is lower for people who have 1 or 2 “alcohol-free” days per week.
Reference: McCaul KA, Almeida OP, Hankey GJ, Jamrozik K, Byles JE, Flicker L. Alcohol use and mortality in older men and women. Addiction 2010. On-line prior to publication: doi:10.1111/j.1360-0443.2010.02972.x
For the full critique of this paper by the International Scientific Forum on Alcohol Research, click here
===============================================================================
Critique 011: A Review of the Proposed New US Dietary Guidelines 14 July 2010
Members of our International Scientific Forum on Alcohol Research have submitted a detailed review of the draft recently circulated by the United States Department of Agriculture for proposed new US Dietary Guidelines for 2010. In general, Forum members were very pleased with the alcohol recommendations in the proposal, finding them interesting, balanced, and accurate. Many commented that, rather than just focusing on warnings against heavy drinking, the new Guidelines appear to take into account the large amount of recent epidemiologic and experimental data that support many potential beneficial health effects of moderate drinking.
Among specific recommendations from the Forum were the following:
■ A stronger statement is needed of the effects of light-to-moderate drinking on total mortality, in that recent prospective studies show a considerably lower of risk of death for moderate drinkers.
■ Additional emphasis is needed on the reduced risk of developing diabetes for moderate drinkers, and the much lower risk of cardiovascular disease among diabetics who consume some alcohol.
■ Further information should be presented on the consistent scientific data showing that women who drink moderately are at reduced, not increased, risk of weight gain in adult life.
There were a number of topics not discussed in the draft Guidelines that members of the Forum thought deserved consideration for inclusion.
■ Recent reports have consistently shown that among people who have already had a myocardial infarction or other cardiovascular event, moderate drinking is associated with a reduced risk of further cardiovascular events and death.
■ More emphasis in the Guidelines should be put on the pattern of drinking (regular moderate rather than occasional binge drinking) and also on the much lower blood alcohol levels after drinking when the beverage is consumed with food, rather than on an empty stomach.
■ It was also suggested to the Guidelines Committee that the beneficial effects on cardiovascular risk of polyphenols and other substances in wine and certain beers, in addition to alcohol, be discussed more adequately.
There were also some suggestions from ISFAR regarding future research needs in the field.
■ The Forum strongly supports the need for further research on the risks and benefits of light-to-moderate alcohol consumption, rather than focusing research only on alcohol abuse.
■ The Forum proposed emphasis on future research dealing with targeting recommendations for groups of people according to age, gender, other behaviors, etc., although there was some disagreement among Forum members as to whether or not moderate drinking has strong health effects in the young and not just in middle-aged and older adults.
■ ISFAR considers moderate drinking, unless contraindicated by certain conditions (e.g, former abuse, some types of severe liver disease), to be an important aspect of a healthy lifestyle. It should be a complement, not an alternative, to other lifestyle factors such as not smoking, getting exercise, eating a healthy diet, and avoiding obesity.
The draft of the proposed new Dietary Guidelines is available at http://www.cnpp.usda.gov/DGAs2010-DGACReport.htm.
For the full ISFAR critique of the proposed new Guidelines, click here
===============================================================================
Summary Critique 010 30 June 2010
Should moderate alcohol consumption be advised following a heart attack?
There has been considerable recent interest in the effects of alcohol consumption following an acute myocardial infarction (AMI). In an observational study among 325 subjects who were moderate drinkers prior to an AMI, 84% continued to drink and 16% quit. While most of the outcome measures showed no statistically significant effects between the two groups of patients, all outcomes showed a tendency towards better physical and mental health outcomes for persistent drinkers in comparison with those who quit drinking.
A key problem with this analysis, and with all observational epidemiologic studies on this topic, is that the reason that some subjects stopped drinking after having an AMI, while others continued to drink, is not known. Even though adjustments were made for many known related factors, there is always the possibility that subjects who stopped drinking were “sicker” in many ways than those who persisted in their alcohol consumption.
It may well require a randomized trial, in which some subjects having an AMI are randomly advised to continue to drink and others advised to stop drinking, to be able to determine reliably the effects on the clinical course of the persistence of alcohol intake following an AMI.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: Critique 010
===============================================================================
Summary: Critique 009 25 June 2010
Should moderate alcohol consumption be advised for its health effects?
A report from a conference that took place at the Medicine Grand Rounds at Beth Israel Deaconess Medical Center, Boston, Massachusetts, on January 15, 2009 has recently been published in the Journal of the American Medical Association, JAMA. It provides a discussion by an epidemiologist with a broad knowledge in the field in response to a theoretical question, as from a middle-aged patient, as to the advisability of consuming some alcohol “for his health.”
The paper provides an excellent discussion of a theoretical question about drinking and health. It focuses on the potential risks and benefits associated with moderate drinking for a middle-aged male patient. Most members of the International Scientific Forum on Alcohol Research (ISFAR) were pleased with the discussion of the topic. It was noted how uncommon it is that such knowledgeable, detailed, and mostly objective data appear in the mainstream medical literature. It was thought to be “readable, informative and thoughtful.”
The ISFAR critique points out a number of topics that were covered incompletely in the paper, including inadequate information on the importance of the pattern of drinking: moderate regular consumption versus binge drinking. Further, there was a notable lack of information on the beneficial effects on many pathophysiologic processes of polyphenols and other non-alcohol substances present in wine and certain other foods and beverages.
Overall, it was believed that the paper provided important information for physicians who may be discussing alcohol consumption with their patients.
Reference
Clinical Crossroads: Conferences with patients and doctors. A 42-year-old man considering whether to drink alcohol for his health. Kenneth J. Mukamal, MD, MPH, Discussant. JAMA 2010;303:2065-2073. (doi:10.1001/jama.2010.550)
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: Critique 009.
===============================================================================
Summary: Critique 008: 13 June 2010
Further evidence that moderate alcohol consumption may play a role in the prevention of Alzheimer’s Disease
In a case-control study from Spain on the effects of smoking and alcohol use on the risk of Alzheimer’s Disease (AD), the authors found that the risk of AD was unaffected by any measure of tobacco consumption. On the other hand, alcohol consumers showed a 47% lower risk of developing AD than did never consumers, with effects mainly among women and among never smokers. No differences were noted by type of alcoholic beverage consumed. The authors conclude that mean daily total consumption of alcohol showed increasingly protective dose-response relationships in women.
The numbers in this analysis were rather small, and there is always the possibility of confounding by other lifestyle factors. Still, the study supports a number of previous epidemiologic studies showing a lower risk of developing AD for moderate consumers of alcohol.
Reference
García AM, Ramón-Bou N, Porta M. Isolated and joint effects of tobacco and alcohol consumption on risk of Alzheimer’s Disease. Journal of Alzheimer’s Disease 2010;20:577–586. (DOI 10.3233/JAD-2010-1399).
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: Critique 08.
===============================================================================
Summary: Critique 007 9 June 2010
People may change to a “healthier” pattern of drinking as they age
In a prospective longitudinal study of a cohort of Americans in the “Baby Boomer” generation, subjects’ drinking habits were assessed at two points, when they were approximately 53 years of age and again when they were approximately 64 years of age. As the subjects got older, they began to consume fewer drinks per occasion but to consume alcohol more frequently; the net effect was little change in total alcohol intake for women but a slight increase for men.
In most epidemiologic studies, regular moderate drinking is the pattern associated with lower risk of many chronic diseases; hence, the described change in drinking pattern in this study (smaller amounts on more frequent occasions) can be considered a “healthy” change. Most long-term observational studies show a decrease in total alcohol intake with ageing, although reasons for such are poorly understood.
This paper emphasizes the importance of knowing the pattern of drinking, and not just the total number of drinks consumed over a week, when evaluating the impact of alcohol consumption on health and disease.
Reference
Molander RC, Yonker JA, Krahn DD. Age-related changes in drinking patterns from mid- to older age: results from the Wisconsin Longitudinal Study. Alcoholism: Clinical and Experimental Research 2010;34 (Published early online 7 May 2010).
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: Critique 07.
===============================================================================
Summary: Critique 006 2 June 2010
For patients who already have cardiovascular disease, continued moderate alcohol consumption may reduce their risk of death
This review paper in Circuation summarizes data from 8 epidemiologic studies of subjects with cardiovascular disease (CVD) as to their subsequent mortality (both CV and total-mortality) according to their alcohol consumption. Most studies showed significantly lower risk of both CV and total mortality for patients with CVD who were consumers of alcohol.
Despite these clear-cut findings, the authors were very cautious in their conclusions, focusing on the dangers of excessive drinking and not encouraging cardiovascular patients who do not drink to start regular drinking. They state that moderate consumers of alcohol who have CV disease should not be advised to stop drinking, but should be advised to not consume alcohol more heavily.
It is interesting that these authors published the meta-analysis upon which this review is largely based in the Journal of the American College of Cardiology earlier in 2010. In that paper, their conclusions were less restrained: “Cardiologists should be aware that regular, moderate alcohol consumption, in the context of a healthy lifestyle (increased physical activity, no smoking), dietary habits (decreased dietary fat intake, high consumption of fruit and vegetables), and adequate drug therapy, would put their patients at a level of cardiovascular or mortality risk substantially lower than either abstainers or heavy or binge drinkers.”
Reference
Costanzo S, Di Castelnuovo A, Donati MB, Iacoviello L, de Gaetano G. Contemporary Reviews in Cardiovascular Medicine. Cardiovascular and overall mortality risk in relation to alcohol consumption in patients with cardiovascular disease. Circulation 2010;121;1951-1959.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 006.
===============================================================================
Summary: Critique 005 27 May 2010
Alcohol in young women may increase their risk of benign breast disease
Among more than 6,000 young women being followed in a longitudinal study, 67 confirmed cases of benign breast disease (BBD) were diagnosed. Alcohol consumption was reported on 57 women who developed BBD when they were 16 – 23 years of age, with all but 8 subjects being 18 or older when they reported alcohol intake, and no data were presented on potential exposures earlier following menarche. A significant increase in the risk of BBD was associated with alcohol intake, although many key factors that have been shown to relate to BBD were not reported in the paper. Hence, while the number of cases is small, and a number of potential risk factors are not included, this study suggests that BBD may be increased by alcohol consumption in young women.
Reference
Berkey CS; Willett WC; Lindsay Frazier A; Rosner B; Colditz GA; Rockett RH; Helaine RM. Prospective study of adolescent alcohol consumption and risk of benign breast disease in young women. Pediatrics 2010;125:e1081-e1087.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 005.
===============================================================================
Summary: Critique 004 24 May 2010
Moderate alcohol consumption is associated with other healthy lifestyle factors
An analysis based on a very large number of subjects in France demonstrates, as have most other studies, that moderate consumers of alcohol have many associated healthy lifestyle habits: lower levels of body mass index, blood glucose, heart rate, stress and depression scores; higher subjective health status, HDL-cholesterol values, levels of physical activity and social status. The authors suggest that alcohol is not related causally to any of these factors, and that the other lifestyle factors, not alcohol consumption, are the reason that moderate drinkers have less cardiovascular disease. They chose a very narrow group of citations from the literature to support this contention.
The authors ignore a large number of well-conducted prospective epidemiologic studies showing that moderate drinkers are at lower risk over time of developing certain risk factors. Further, the authors of this paper ignore an immense basic science literature that suggests that alcohol is an important factor in the development of biological risk factors, atherosclerosis, and cardiovascular disease. Further, they do not describe a number of studies that have shown specifically that moderate drinking is associated with less cardiovascular disease and diabetes among subjects who are otherwise very healthy (non-smokers, not obese, physically active, and on a healthy diet).
There is no doubt that confounding by associated lifestyle factors can play a role in the lower risk of chronic diseases among moderate drinkers, who tend to also have other healthy behaviors. However, there is now a large body of scientific evidence that indicates that alcohol is an important factor in the lower rates of such diseases; current scientific data do not support the conclusions of the authors of this paper.
Reference
Hansel B, Thomas F, Pannier B, Bean K, Kontush A, Chapman MJ, Guize L, Bruckert E. Relationship between alcohol intake, health and social status and cardiovascular risk factors in the urban Paris-Ile-De-France Cohort: is the cardioprotective action of alcohol a myth? European J Clin Nutrition, advance online publication, doi:10:1038/ejcn.2010.61.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 004.
===================================================================================
Summary: Critique 003 17 May 2010
Moderate alcohol consumption markedly reduces the risk of diabetes mellitus, even among subjects with otherwise very healthy lifestyles
In a very well-done analysis from a large Dutch population, it was shown that moderate drinking considerably lowers the risk of developing type 2 diabetes even among subjects who are otherwise following a healthy lifestyle (not obese, non-smokers, physically active, eating a healthy diet). Thus, it indicates that the effect of moderate drinking on lowering the risk of diabetes cannot be explained by other healthy lifestyle habits of such drinkers. Moderate drinking should be considered as a complement, and not as an alternative, to other healthy lifestyle habits that lower the risk of chronic diseases such as diabetes and coronary heart disease.
Reference
Joosten MM, Grobbee DE, van der A DL, Verschuren WWM, Hendriks HFJ, Beulens JWJ. Combined effect of alcohol consumption and lifestyle behaviors on risk of type 2 diabetes. Am J Clin Nutr 2010;91: 1777-1783.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 003.
===============================================================================
Summary: Critique 002 26 April 2010
Red wine, but not other types of alcohol, improve endothelial function in a randomized trial
The healthy state of cells that form the lining of arteries, assessed by indices of endothelial function, is a key factor associated with preventing the development and progression of atherosclerosis and coronary heart disease. In a randomized trial among healthy young adults, the daily consumption of about 3 ounces of red wine for three weeks led to significant improvement in endothelial function. Such improvements were not seen with the consumption of water, or of beer or vodka containing similar amounts of alcohol.
Further, in a series of in-vitro studies, the authors showed very similar effects from red wine and from a high concentration of resveratrol (but not from beer or ethanol) on factors associated with improved endothelial function. The study supports many epidemiologic and animal experiments suggesting that certain non-alcoholic constituents of red wine have additional beneficial effects on cardiovascular risk over those of just the alcohol itself.
Reference
Huang PH, Chen YH, Tsai HY, Chen JS, Wu TC, Lin FY, Sata M, Chen JW, Lin SJ. Intake of red wine increases the number and functional capacity of circulating endothelial progenitor cells by enhancing nitric oxide bioavailability. Arteriosclerosis Thrombosis and Vascular Biology 2010;30:869-877.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 002.
===============================================================================
Summary: Critique 001 24 April 2010
Genetic effects on alcohol metabolism modify the relation of alcohol to breast cancer
A study from Germany compared the association between alcohol and breast cancer risk according to genetic variations affecting levels of alcohol dehydrogenase, an enzyme that clears alcohol from the blood stream. The authors conclude that genetic factors associated with the slow clearance of alcohol are associated with increased risk of breast cancer for drinkers; an increase in cancer risk was not seen for drinkers with genetic factors leading to fast clearance of alcohol. Such a finding would suggest that alcohol itself is the cause of an increase in breast cancer risk among drinkers.
Unfortunately, some previous studies have shown the opposite, that an increase in breast cancer risk occurs only among women who have genes associated with fast, rather than slow, alcohol metabolism. Overall, current scientific data indicate that breast cancer’s relation to drinking is not resolved, remaining murky and conflicted, and perhaps overemphasized. This facet of that murkiness is itself also conflicted. As of now, it is unclear the degree to which genes affecting alcohol dehydrogenase modify the association between alcohol and the risk of breast cancer and other diseases.
Reference
Larsen SB, Vogel U, Christensen J, Hansen RD, Wallin H, Overvad K, Tjønneland A, Tolstrup I. Interaction between ADH1C Arg272Gln and alcohol intake in relation to breast cancer risk suggests that ethanol is the causal factor in alcohol related breast cancer. Cancer Letters, 2010, in press.
For the full critique of this paper by the International Scientific Forum on Alcohol Research, please click here: CRITIQUE 001.
===============================================================================
